Abstract
Background:
Fentanyl has been suggested to be effective for controlling airway and hemodynamic responses to tracheal extubation. This study was performed to compare the effects of oxycodone and fentanyl on airway and hemodynamic responses and postoperative pain during the recovery period in patients undergoing laparoscopic cholecystectomy.
Methods:
Ninety patients aged 18 to 65 years were randomly allocated to 1 of 3 groups: fentanyl, oxycodone, and control. Coughing responses (incidence and severity), hemodynamic responses during the recovery period, and acute postoperative pain were assessed.
Results:
The incidence of cough was decreased in the fentanyl and oxycodone groups compared with that in the control group at the points of awareness and extubation, and no significant difference was observed between the 2 treatment groups. Severe cough response was decreased in the fentanyl and oxycodone groups compared with that in the control group at the point of extubation, and no significant change was observed in cough severity between the 2 treatment groups. Postoperative pain scores were lower in the fentanyl and oxycodone groups than those in the control group at 5 and 30 minutes postoperatively, and no significant difference was observed between the 2 treatment groups. Hemodynamic responses did not differ among the 3 groups during the recovery period.
Conclusion:
Oxycodone treatment before tracheal extubation reduced cough response and was as effective as fentanyl treatment for improving extubation quality. Furthermore, single boluses of fentanyl and oxycodone showed equal effectiveness in attenuating acute postoperative pain in patients undergoing laparoscopic cholecystectomy.
Keywords: fentanyl, laparoscopic cholecystectomy, oxycodone, tracheal extubation
1. Introduction
One of the major concerns related to tracheal extubation is prevention of respiratory complications such as coughing, laryngospasm, breath holding, desaturation, and pulmonary edema.[1] Moreover, tracheal extubation can cause hypertension and tachycardia as a result of sympathetic stimulation.[2] Many drugs and techniques have been used to attenuate airway and hemodynamic responses with varying efficacy.
Fentanyl is a synthetic opioid that is commonly used to control moderate or severe pain. It has a rapid onset and provides 30 to 60 minutes of analgesia following a single intravenous injection,[3] making it useful for acute pain management during the perioperative period. In addition to this advantage, hemodynamic stability and a favorable recovery profile during and after extubation have been associated with the efficacy of fentanyl.[4,5]
Oxycodone is a strong semisynthetic opioid and although its onset time is similar to that of fentanyl, oxycodone has a longer analgesic duration (2–5 hours).[6] Recently, many studies have shown that the analgesic effects of oxycodone are better than those of fentanyl in treating postoperative pain.[7,8] Oxycodone has also been effectively utilized to attenuate hemodynamic changes during intubation.[9]
Therefore, we hypothesized that oxycodone could reduce airway responses and prevent detrimental hemodynamic changes following tracheal extubation as effectively or potentially more effectively than fentanyl. This study was performed to compare the effects of oxycodone and fentanyl on airway and hemodynamic responses and postoperative pain during the recovery period in patients undergoing laparoscopic cholecystectomy.
2. Materials and methods
2.1. Study population and anesthesia
This study was approved by the Institutional Review Board committee of the Yeungnam University Hospital, Daegu, Republic of Korea. Written informed consent was obtained from all the patients. This study was registered at clinicaltrials.gov (NCT03204045). We included patients aged 18 to 65 years with an American Society of Anaesthesiologists physical status classification of I or II who were scheduled for elective laparoscopic cholecystectomy. The exclusion criteria were allergies to either fentanyl or oxycodone, a history of chronic use of other opioids or analgesics, a history of smoking, a history of cardiac, hepatic, respiratory, or renal disease, current respiratory tract infection, other comorbid conditions, cognitive impairment, or a body mass index greater than 35 kg/m2.
The patients were assigned to 1 of 3 groups by computer-generated randomization: the fentanyl group, the oxycodone group, or the control group. None of the patients were premedicated. After applying routine hemodynamic monitoring (electrocardiography, noninvasive blood pressure, capnography, and pulse oximetry), general anesthesia was induced with propofol (1.5–2.5 mg/kg) and remifentanil at an initial target concentration of 3 to 4 ng/mL using target-controlled infusion (TCI) devices (Orchestra Base Primea, Fresenius Vial, France). After intravenous injection of rocuronium (0.6–0.8 mg/kg), intubation was performed using an endotracheal tube with an internal diameter of 7.5 mm for females and 8.0 mm for males. Anesthesia was maintained with 6 to 9 vol% end-tidal concentration of desflurane in 50% oxygen with air and a continuous infusion of remifentanil (fixed target concentration of 2–3 ng/mL), which were adjusted to maintain acceptable hemodynamic parameters and a bispectral index (BIS) of 40 to 60. When carbon dioxide gas was desufflated, desflurane was titrated to a 0.6 MAC, and remifentanil was discontinued. After all surgical procedures were completed, desflurane was discontinued. Ten minutes prior to the completion of the operation, the patients received a 2 mL mixture of fentanyl (1 μg/kg) or oxycodone (0.08 mg/kg) in isotonic saline intravenously according to their allocated study groups by an anesthesiologist who was blinded to the group-treatment allocation. Residual neuromuscular blockade was antagonized by intravenous pyridostigmine (0.2 mg/kg) and glycopyrrolate (0.01 mg/kg). Oral suction was gently performed. Tracheal extubation was smoothly performed when the patients opened their eyes in response to a verbal request and spontaneous ventilation was adequate.
2.2. Study assessments
Airway reflex responses, including coughing, breath holding, bucking, and laryngospasm, were recorded at the point of awareness (eye opening in response to verbal commands), extubation, and 3 minutes after tracheal extubation. Hemodynamic responses were recorded at the completion of surgery (T1), at the point of awareness (T2), at the point of extubation (T3), and 3 min after tracheal extubation (T4). All assessment parameters were evaluated by a different anesthesiologist who was blinded to the group randomization. Extubation time (from discontinuation of desflurane until extubation) was recorded for all the patients.
Coughing severity was assessed using a 5-point scale (0 = no coughing; 1 = smooth extubation, minimal coughing (1–2 times); 2 = moderate coughing (3–4 times); 3 = severe coughing (5–10 times) and straining; 4 = poor extubation, very uncomfortable (laryngospasm and coughing > 10 times).[4] Scores of 3 and 4 were considered clinically severe. Breath holding was defined as desaturation and not breathing for ≥ 20 seconds, resulting in a > 5% decrease in SpO2 from baseline. The mean blood pressure (MBP), heart rate (HR), and SpO2 were also measured at the same time point.
In the recovery room, hemodynamic responses were evaluated every 5 minutes for 30 minutes. Postoperative pain intensity was assessed at 5 and 30 minutes in the postanesthetic care unit (PACU) using a numerical rating scale (NRS) ranging from 0 (no pain) to 10 (worst possible pain). When the pain score was ≥ 5 or the patient asked for rescue analgesics, 30 mg of ketorolac was injected intravenously. The sedation score was also recorded at the same time points using a scale of 1 to 5, where 1 indicates that the patient is asleep but easily roused, and 5 represents somnolent and minimal or no response to stimulation.[10] Any adverse reactions (nausea, vomiting, dizziness, hypotension, and respiratory depression) in the recovery room were also recorded. All data were assessed by an anesthesiologist who was blinded to the study.
2.3. Statistical analyses
Based on our preliminary study, the coughing response rate after laparoscopic cholecystectomy was 70%. A 50% reduction in the incidence of coughing responses in the fentanyl or oxycodone group was considered clinically relevant, and 30 patients were required per group (α = 0.05, power = 80%). Therefore, 33 patients were selected for each group to account for dropouts. The data are expressed as numbers (%) or means (SD). Statistical analysis was performed using SPSS software (IBM, Chicago, IL). After assessing the normality of the data with the Shapiro–-Wilk test and Kolmogorov–Smirnov test, categorical variables were analyzed using the χ2 test or Fisher exact test, followed by Z tests with Bonferroni correction, and continuous variables were analyzed using ANOVA. A value of P < .05 was considered statistically significant.
3. Results
Of the 99 enrolled patients, 90 were randomized into the 3 groups and were eligible for analysis; 4 did not meet the inclusion criteria, and 5 did not want to participate in the study (Fig. 1). No significant differences were found among the 3 groups with respect to demographic data and anesthetic characteristics of the patients (Table 1). The incidence of cough was significantly decreased in the fentanyl and oxycodone groups compared with that of the control group at the points of awareness (P =.039 for both) and extubation (P =.028 and P =.015, respectively), and no significant difference was observed between the fentanyl and oxycodone groups. The incidence of bucking and breath holding was not different among the 3 groups (Table 2). The severity of cough significantly differed among the 3 groups at the points of awareness and extubation (P =.035 and P =.002, respectively). Post hoc tests with Bonferroni correction showed that the incidence of severe cough was lower in the oxycodone group than in the control group at the point of awareness and that the incidence of severe cough was decreased in the fentanyl and oxycodone groups compared with that in the control group at the point of extubation. No significant change was observed in cough severity between the fentanyl and oxycodone groups (Table 3). Hemodynamic responses did not differ among the 3 groups at any time points (T1–T5) during the recovery period (Fig. 2).
Figure 1.
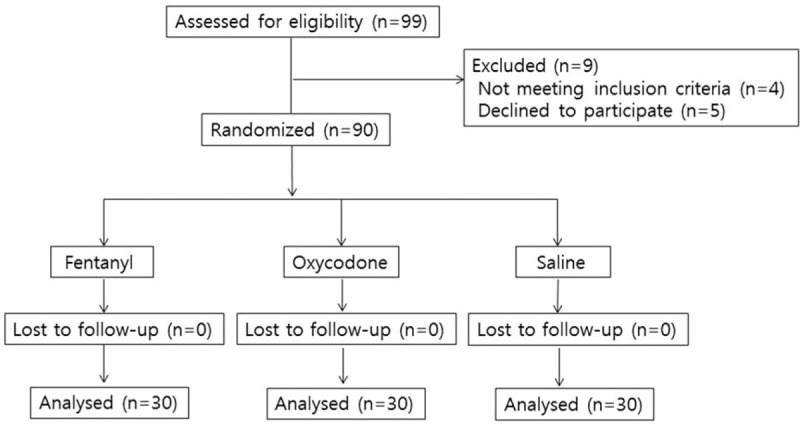
Flow diagram of the study design and patient selection.
Table 1.
Demographic data.
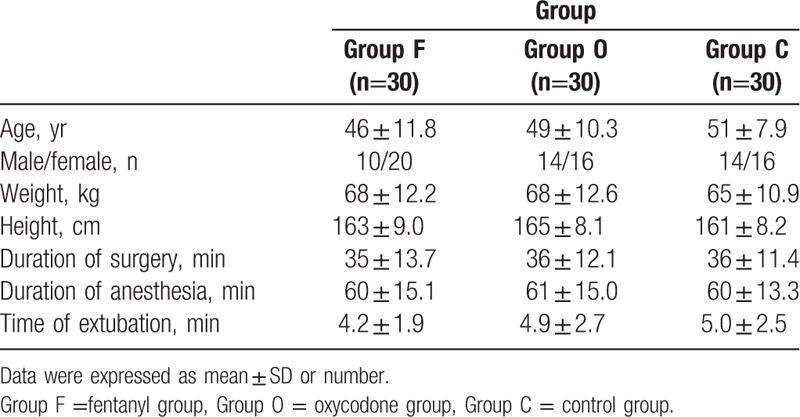
Table 2.
Extubation quality.
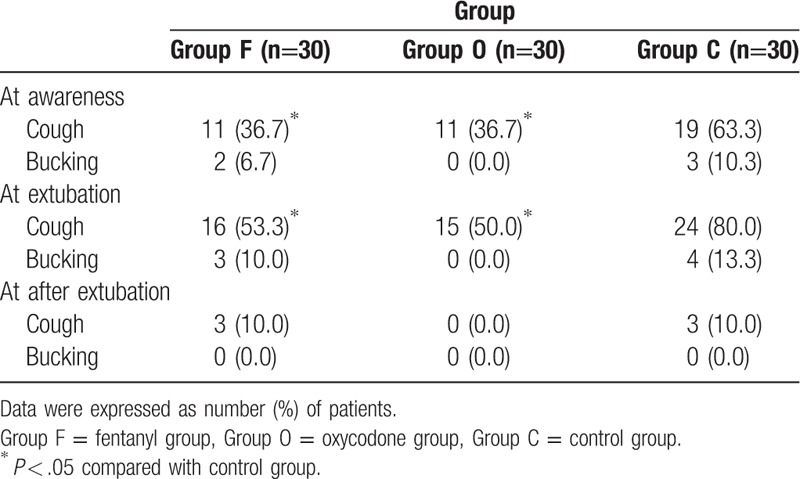
Table 3.
Cough severity.
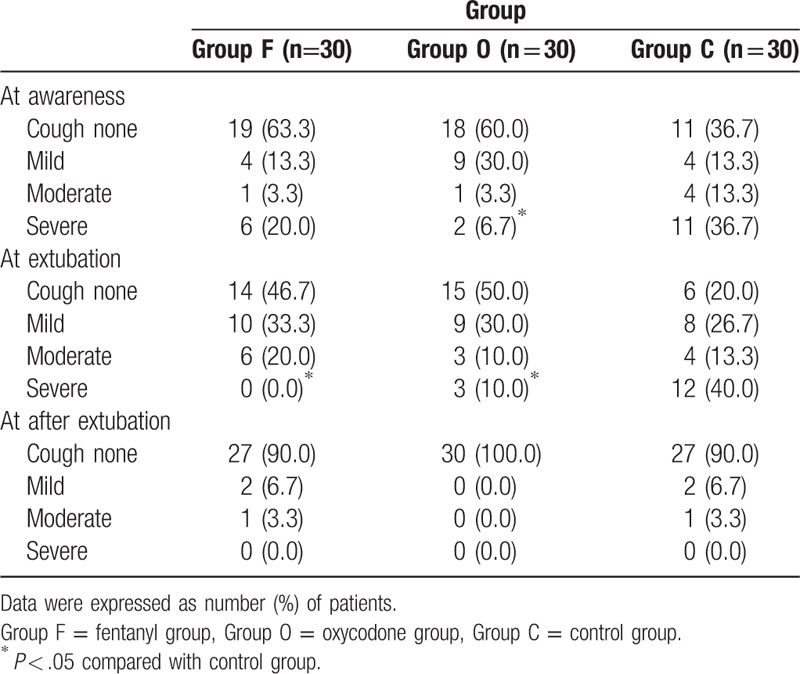
Figure 2.
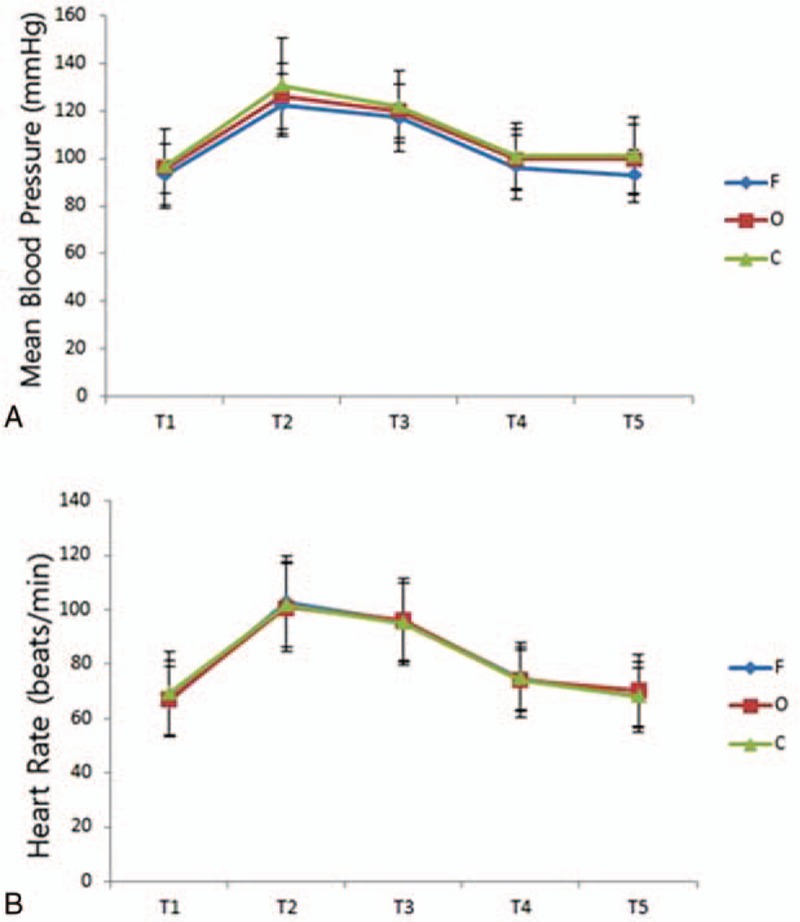
Hemodynamic change in 3 groups. T1: completion of surgery; T2: point of extubation; T3: 3 min after tracheal extubation; T4 and T5; 5 and 30 min in PACU. F = fentanyl group, O = oxycodone group, C = control group.
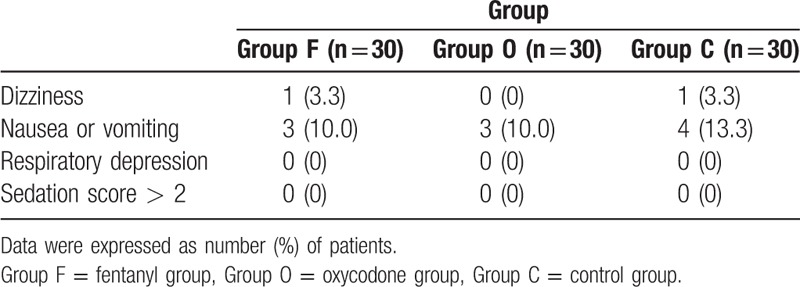
The postoperative pain score was significantly lower in the fentanyl and oxycodone groups than in the control group at 5 (P < .001 for both) and 30 minutes postoperatively (P =.034 and P =.002, respectively). The requirement for rescue analgesics was greater in the control group than in the oxycodone group (P =.028), but there was no difference between the fentanyl group and the control group (Table 4). The 3 groups did not show significant differences regarding the prevalence of dizziness, nausea, vomiting, and sedation. Respiratory depression did not occur in any of the groups (Table 5).
Table 4.
Severity of postoperative pain.
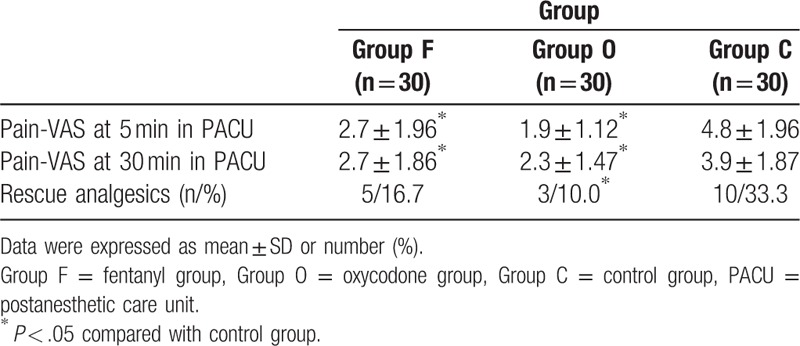
Table 5.
Incidence of adverse events.
4. Discussion
In this study, oxycodone treatment before tracheal extubation reduced the coughing response and was as effective as fentanyl treatment in relieving airway reflexes and improving extubation quality, without an accompanying increase in side effects. Furthermore, single bolus of fentanyl and oxycodone were found to have equal effectiveness in attenuating acute postoperative pain in patients undergoing laparoscopic cholecystectomy.
During recovery from general anesthesia, smooth emergence and hemodynamic stability are important. In particular, airway reflex caused by endotracheal extubation may elicit various complications such as coughing, bucking, breath holding, and laryngospasm,[1,11] and stimulation of the sympathetic nervous system can result in severe hypertension and tachycardia.[12] These distressing adverse events can significantly increase morbidity (airway obstruction, pulmonary edema, arrhythmia, myocardial ischemia, and surgical bleeding) and generate considerable costs (drugs, nursing cares, unanticipated reintubation, and delayed discharge). Deep extubation (defined as tracheal extubation while a patient is deeply sedated to blunt the laryngeal reflex) may be preferable to avoid these undesirable outcomes; however, this alternative technique may not be suitable for nonfasting patients due to the risk of aspiration or for patients undergoing airway surgeries due to potential airway complications.[2] Therefore, although various therapeutic strategies have been implemented to attenuate airway and hemodynamic responses during extubation, no treatment has been demonstrated to be completely successful.
During emergence, opioids have been widely used to attenuate the sympathetic stimuli of tracheal extubation and postoperative pain. Many studies have identified the analgesic effects of fentanyl and oxycodone on postoperative pain.[7,10,13] Koch et al[10] reported that oxycodone had a better analgesic effect than fentanyl on postoperative pain after laparoscopic cholecystectomy, while Xie et al showed that oxycodone was not superior to fentanyl in improving postoperative pain. However, studies comparing the 2 drugs in terms of hemodynamic effects and airway responses to tracheal extubation are rare. Fentanyl has a short onset time and high lipid solubility. Its analgesic effect peaks in 5 minutes, reflecting rapid and extensive redistribution in the body.[10,14] The timed administration of fentanyl can somewhat offset hemodynamic responses resulting from endotracheal intubation or extubation.[15,16] Oxycodone, a newly developed semisynthetic opioid, is structurally analogous to morphine, with 1:1 analgesic strength in controlling postoperative pain.[17] The onset time of oxycodone is similar to that of fentanyl; however, it has a longer duration of action compared with fentanyl.[6] Lee et al[9] showed that oxycodone and fentanyl comparably attenuated the hemodynamic response following endotracheal intubation during surgery for nasal bone fracture. The present study showed that fentanyl (1 μg/kg) and oxycodone (0.08 mg/kg) had no attenuating effect on increases in BP and HR following extubation. The treatment doses of the 2 drugs may have been insufficient to maintain hemodynamic stability. However, regarding postoperative pain control, the clinical efficacy of oxycodone was comparable to that of fentanyl at equianalgesic doses.
Among the various airway reflex responses related to the presence of an endotracheal tube, coughing is the most common.[18] The cough reflex during emergence from anesthesia is evoked by the activation of the ascending vagus nerve in the airway by chemical and mechanical irritations.[19] Coughing on emergence is a physiologic airway reflex, and appropriate activation of the cough reflex may have a protective effect in terms of prevention of aspiration and airway obstruction during breathing. However, coughing can induce serious complications such as cardiovascular instability, bleeding at the surgical site, laryngospasm, and increased intracranial and intrathoracic pressure, which can cause detrimental effects. Therefore, various medications are used (lidocaine, propofol, dexmedetomidine, and remifentanil) to inhibit coughing during anesthetic recovery.[20–23] Short-acting opioids are widely used for smooth extubation, and recent studies have reported that fentanyl administration resulted in a more comfortable emergence and recovery.[5,16,24] Conversely, fentanyl-induced cough can be harmful to patients, although it is mostly transient and limited.[25,26] This adverse event occurs frequently following anesthetic induction with high doses (greater than 2 μg/kg intravenously) of fentanyl and rapid injection rates. Therefore, we elected to administer fentanyl (1 μg/kg intravenously) to suppress airway irritation during anesthetic emergence, and compared its effects with those of oxycodone. To the best of our knowledge, no studies have reported the effect of oxycodone on attenuating the cough response to tracheal extubation. In this study, a single dose of oxycodone was as effective as fentanyl in attenuating airway reflexes during recovery from general anesthesia, although the mechanism of the beneficial effects of fentanyl and oxycodone on airway reflex remains unknown.
While opioid drugs may be useful for facilitating smooth emergence, they are associated with additional side effects such as delayed emergence, sedation, dizziness, nausea, vomiting, and respiratory depression. In this study, no difference in the incidence of side effects was observed between the 2 treatment groups or between the treatment groups and the control group.
This study has some limitations. First, we used only a single dose of fentanyl or oxycodone to compare their effects on the cough response with tracheal extubation. The results did not have sufficient power to compare the differences between 2 drugs. Therefore, further studies involving timed titrations are required. Second, the sample size of this study was determined from the results of the power analysis in the planning stage of the study. However, if additional subjects had been enrolled for analysis, the effects of fentanyl and oxycodone on airway reflexes and hemodynamic responses could have been assessed more accurately. Third, we analyzed the data of the patients who eventually completed the study rather than the data of all initially enrolled patients. Intention-to-treat analysis, which involves the randomization of all participants, required for more conservative estimates to avoid various misleading biases. Fourth, the emergence response varies based on type of operation, and our results were limited to laparoscopic cholecystectomy. Therefore, cough suppression effects of fentanyl and oxycodone during tracheal extubation may not be generalizable to patients undergoing different procedure. Finally, the airway reflex assessment was limited to the first 3 minutes after extubation. Though adverse respiratory events typically occur shortly afterward tracheal extubation, a longer time interval should be considered for observation during recovery.
In conclusion, oxycodone and fentanyl were found to be beneficial for attenuating airway reflexes in response to tracheal extubation and for relieving immediate postoperative pain in patients undergoing laparoscopic cholecystectomy.
Author contributions
Conceptualization: S-J. Park.
Data curation: E.K. Choi, N. Kwon, S-J. Park.
Formal analysis: E.K. Choi, N. Kwon, S-J. Park.
Funding acquisition: E.K. Choi.
Investigation: E.K. Choi.
Methodology: S-J. Park.
Supervision: S-J. Park.
Visualization: S-J. Park.
Writing – original draft: E.K. Choi.
Writing – review & editing: S-J. Park.
Footnotes
Abbreviations: BIS = bispectral index, HR = heart rate, MBP = mean blood pressure, NRS = numerical rating scale, PACU = postanesthetic care unit, TCI = target controlled infusion.
This work was supported by the 2017 Yeungnam University Research Grant.
The authors have no conflicts of interest to disclose.
References
- [1].Padley SP, Downes MO. Case report: pulmonary oedema secondary to laryngospasm following general anaesthesia. Br J Radiol 1994;67:654–5. [DOI] [PubMed] [Google Scholar]
- [2].Hartley M, Vaughan RS. Problems associated with tracheal extubation. Br J Anaesth 1993;71:561–8. [DOI] [PubMed] [Google Scholar]
- [3].Michaloliakou C, Chung F, Sharma S. Preoperative multimodal analgesia facilitates recovery after ambulatory laparoscopic cholecystectomy. Anesth Analg 1996;82:44–51. [DOI] [PubMed] [Google Scholar]
- [4].Nishina K, Mikawa K, Maekawa N, et al. Fentanyl attenuates cardiovascular responses to tracheal extubation. Acta Anaesthesiol Scand 1995;39:85–9. [DOI] [PubMed] [Google Scholar]
- [5].Inagaki Y, Shindo H, Mashimo T, et al. The effects of epidural fentanyl on hemodynamic responses during emergence from isoflurane anesthesia and tracheal extubation: a comparison with intravenous fentanyl. Anesth Analg 1997;85:328–35. [DOI] [PubMed] [Google Scholar]
- [6].Leow KP, Cramond T, Smith MT. Pharmacokinetics and pharmacodynamics of oxycodone when given intravenously and rectally to adult patients with cancer pain. Anesth Analg 1995;80:296–302. [DOI] [PubMed] [Google Scholar]
- [7].Kim NS, Lee JS, Park SY, et al. Oxycodone versus fentanyl for intravenous patient-controlled analgesia after laparoscopic supracervical hysterectomy: a prospective, randomized, double-blind study. Medicine (Baltimore) 2017;96:e6286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Park JH, Lee C, Shin Y, et al. Comparison of oxycodone and fentanyl for postoperative patient-controlled analgesia after laparoscopic gynecological surgery. Korean J Anesthesiol 2015;68:153–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Lee YS, Baek CW, Kim DR, et al. Comparison of hemodynamic response to tracheal intubation and postoperative pain in patients undergoing closed reduction of nasal bone fracture under general anesthesia: a randomized controlled trial comparing fentanyl and oxycodone. BMC Anesthesiol 2016;16:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Koch S, Ahlburg P, Spangsberg N, et al. Oxycodone vs. fentanyl in the treatment of early post-operative pain after laparoscopic cholecystectomy: a randomised double-blind study. Acta Anaesthesiol Scand 2008;52:845–50. [DOI] [PubMed] [Google Scholar]
- [11].Cranfield KA, Bromley LM. Minimum alveolar concentration of desflurane for tracheal extubation in deeply anaesthetized, unpremedicated children. Br J Anaesth 1997;78:370–1. [DOI] [PubMed] [Google Scholar]
- [12].Lowrie A, Johnston PL, Fell D, et al. Cardiovascular and plasma catecholamine responses at tracheal extubation. Br J Anaesth 1992;68:261–3. [DOI] [PubMed] [Google Scholar]
- [13].Choi YJ, Park SW, Kwon HJ, et al. Efficacy of early intravenous bolus oxycodone or fentanyl in emergence from general anaesthesia and postoperative analgesia following laparoscopic cholecystectomy: a randomized trial. J Int Med Res 2015;43:809–18. [DOI] [PubMed] [Google Scholar]
- [14].Channaiah VB, Kurek NS, Moses R, et al. Attenuation of hemodynamic response to laryngoscopy and endotracheal intubation with pre induction IV fentanyl versus combination of IV fentanyl and sub lingual nitroglycerin spray. Med Arch (Sarajevo Bosnia and Herzegovina) 2014;68:339–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Sawano Y, Miyazaki M, Shimada H, et al. Optimal fentanyl dosage for attenuating systemic hemodynamic changes, hormone release and cardiac output changes during the induction of anesthesia in patients with and without hypertension: a prospective, randomized, double-blinded study. J Anesth 2013;27:505–11. [DOI] [PubMed] [Google Scholar]
- [16].Aksu R, Akin A, Biçer C, et al. Comparison of the effects of dexmedetomidine versus fentanyl on airway reflexes and hemodynamic responses to tracheal extubation during rhinoplasty: a double-blind, randomized, controlled study. Curr Ther Res Clin Exp 2009;70:209–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Silvasti M, Rosenberg P, Seppala T, et al. Comparison of analgesic efficacy of oxycodone and morphine in postoperative intravenous patient-controlled analgesia. Acta Anaesthesiol Scand 1998;42:576–80. [DOI] [PubMed] [Google Scholar]
- [18].Soltani HA, Aghadavoudi O. The effect of different lidocaine application methods on postoperative cough and sore throat. J Clin Anesth 2002;14:15–8. [DOI] [PubMed] [Google Scholar]
- [19].Wilddicombe JG. Afferent receptors in the airways and cough. Respir Physiol 1998;114:5–15. [DOI] [PubMed] [Google Scholar]
- [20].Venkatesan T, Korula G. A comparative study between the effects of 4% endotracheal tube cuff lignocaine and 1.5 mg/kg intravenous lignocaine on coughing and hemodynamics during extubation in neurosurgical patients: a randomized controlled double-blind trial. J Neurosurg Anesthesiol 2006;18:230–4. [DOI] [PubMed] [Google Scholar]
- [21].Jung SY, Park HB, Kim JD. The effect of a subhypnotic dose of propofol for the prevention of coughing in adults during emergence from anesthesia with sevoflurane and remifentanil. Korean J Anesthesiol 2014;66:120–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Guler G, Akin A, Tosun Z, et al. Single-dose dexmedetomidine attenuates airway and circulatory reflexes during extubation. Acta Anaesthesiol Scand 2005;49:1088–91. [DOI] [PubMed] [Google Scholar]
- [23].Lee JH, Koo BN, Jeong JJ, et al. Differential effects of lidocaine and remifentanil on response to the tracheal tube during emergence from general anaesthesia. Br J Anaesth 2011;106:410–5. [DOI] [PubMed] [Google Scholar]
- [24].Kong CF, Chew ST, Ip-Yam PC. Intravenous opioids reduce airway irritation during induction of anaesthesia with desflurane in adults. Br J Anaesth 2000;85:364–7. [DOI] [PubMed] [Google Scholar]
- [25].Yeh CC, Wu CT, Huh BK, et al. Premedication with intravenouslow-dose ketamine suppresses fentanyl-induced cough. J Clin Anesth 2007;19:53–6. [DOI] [PubMed] [Google Scholar]
- [26].Sedighinejad A, Naderi Nabi B, Haghighi M, et al. Propofol is effective to depress fentanyl-induced cough during inductionof anesthesia. Anesth Pain Med 2013;2:170–3. [DOI] [PMC free article] [PubMed] [Google Scholar]


