Abstract
The identification of epidural space with loss of resistance (LOR) is commonly performed. But it lacks specificity. Epidural pressure waveform analysis (EPWA) provides a simple confirmative adjunct for LOR. If the needle is located within the epidural space, measurement of the pressure at its tips shows a pulsatile waveform. Previous studies demonstrated satisfactory sensitivity and specificity of EPWA. However, success or failure of epidural injection was confirmed by the pinprick test, which is limited for patients in the setting of the pain clinic. In this study, we evaluated the sensitivity, specificity, as well as positive and negative predictive values of EPWA for cervical epidural steroid injection (CESI) confirmed by fluoroscopy.
One hundred and five CESIs of 75 patients suffering from neck and radicular arm pain of over 3 months duration were enrolled. The physician injected 5 mL of normal saline after a feeling of satisfactory LOR. Saline filled extension tubing, connected to a pressure transducer, was attached to the needle. A 3 mL bolus of contrast medium was injected to confirm the success of CESI.
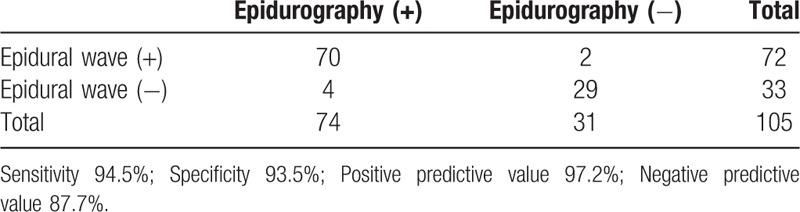
The incorrect identification of epidural space with LOR (false LOR) was 29.5%. Of these 31 failed CESIs, 2 showed epidural waveform and 29 did not. The sensitivity, specificity, positive and negative predictive value of EPWA was 94.5%, 93.5%, 97.2%, and 87.7%, respectively.
EPWA shows satisfactory reliability and is a simple adjunct to decrease false LOR for CESI. Further confirmative studies are required before its routine use in clinical practice.
Keywords: cervical, epidural waveform, loss of resistance
1. Introduction
Loss of resistance (LOR) is the most commonly used method to confirm the epidural space.[1] The advantage of LOR is its simplicity; only saline or air filled syringe is required. LOR is felt through the sudden decrease of pressure and this pressure gradient is generated when the needle is within the passage of interspinous ligament, ligamentum flavum, and epidural space. The presence of ligamentum flavum is crucial for the identification of epidural space by LOR.[2] However, gaps in ligamentum flavum, paravertebral muscle and cyst in interspinous ligament can modify this passage and a false LOR is generated consequentially.[1,3,4] The false positive rate of the lumbar and cervical area was reported to be 8.3% ∼ 17% and 30% ∼ 68%, respectively.[1,5,6] If the false positive rate is high, repeated attempts of epidural steroid injection (ESI) are required, with additional discomfort or pain to the patient.
The high rate of false LOR has prompted the design of adjunctive modalities.[1] Among these, epidural pressure waveform analysis (EPWA) using pressure transducer has been reported.[7–11] If the epidural needle or catheter is positioned accurately in the epidural space, a pulsatile wave coinciding with arterial pulsations can be seen through the monitor.[1,7–11] For the routine use of this EPWA as an adjunctive method, reliability studies have been reported. However, all the results were obtained from the patients before surgery or from women in labor via the thoracic and lumbar epidural injections.[7–9,11]
ESI of the cervical and lumbar area is a common method for the pain physician to manage patients experiencing chronic pain.[12–14] Most pain physicians routinely used fluoroscopy as a guidance tool. ESI using fluoroscopic guidance provides the benefit of accuracy and minimizes the delivery of medication to non-epidural space.[15] Before injecting steroid or other medications, a radiographic contrast medium is used to confirm the epidural space by fluoroscopic guidance. However, injection of contrast medium into non-epidural spaces can occur. Most of these injections occur due to false LOR. If the contrast medium is injected in non-epidural spaces, this false injection can interrupt the repeated attempts because the bony landmark needed for ESI is covered with previously injected contrast medium. As a result, the injection level should be changed or the injected contrast medium should be allowed to dissipate with time.
We propose that the implementation of EPWA can decrease false contrast medium injection in the outpatient pain management clinic setting. To verify this proposal, a reliability study of EPWA under fluoroscopic guidance is needed. Previous reliability studies used the pinprick or cold ice test to confirm the success of epidural block, which is limited for patients in the setting of the pain management clinic.[7–9,11]
In this reliability study, we chose the cervical epidural space, which is reported to have a high false LOR [1,5,6] and which has never been studied related to the reliability of EPWA.
The primary purposes of this study are to provide data to calculate the sensitivity, specificity, and positive/negative predictive values under the confirmation of fluoroscopic image and to determine the incidence of false LOR of the cervical epidural area in the pain management clinic setting.
2. Material and methods
2.1. Study design
This study was a prospective, single pain management clinic, and blinded study. This study was approved by the institutional review board of our institution (05–037) and all participants provided written and informed consent. This trial was registered in the Clinical Trial Registry (NCT02838654).
2.2. Patients
One hundred and five cervical ESIs (CESIs) of 75 patients from July 2016 to June 2017 were enrolled. Inclusion criteria were neck and radicular arm pain of more than 3 months duration due to intervertebral disc herniation, spinal stenosis, facet arthropathy, or herpes zoster of cervical region. Exclusion criteria were refusal to participate in the study, laboratory findings suggesting coagulopathy, inflammation or infection, allergy to local anesthetics, steroids or contrast medium, coagulopathy, and previous surgery on the cervical spine. Patients were also excluded if they showed any signs of neurologic deficits.
One hundred and ten CESIs of 78 patients were initially enrolled. However, 1 patient was excluded due to not satisfying the inclusion criteria and 2 patients due to inadvertent intrathecal injections. Finally, 105 CESIs of 75 patients were enrolled.
2.3. Performance of CESIs
All epidural injections were carried out by 1 pain physician (JH) to provide a more homogenous condition. The midline approach at the C6-7 level, where fluoroscopic lateral images demonstrated minimal overlap with adjacent structures of shoulder in the prone position, was used. For the purpose of widening of the C6-7 interlaminar space, a pillow was placed under the chest of the patient to produce greater flexion of their necks in the prone position. After aseptic preparation and skin infiltration with 1% lidocaine, a 20-gauge Tuohy epidural needle (Tae-Chang Industrial Co., Kongju, Republic of Korea) was inserted under anteroposterior (AP) fluoroscopic guidance until the needle reached the superior border of the inferior laminar. If the bony contact was made with the superior border of the inferior lamina, further needle advance was performed with LOR technique using an air-filled syringe. When a satisfactory LOR was encountered, 5 mL of normal saline was injected through the epidural needle and saline filled sterile extension tubing connected to a pressure transducer (Edwards Lifesciences, Irvine, CA) was attached to the needle. The level of pressure transducer was adjusted to heart level. The pressure scale was set in a range of 0-30-mmHg on a portable monitor. To confirm the success of CESI, we injected 3 mL of contrast medium subsequently after recording the epidural waveform. After injection of the contrast medium, the AP and lateral views were saved to the hard disk of C-arm and they were transmitted to a picture archiving and communication system (PACS). An investigator not affiliated with the study assessed the image. This investigator was board certified in anesthesiology and pain medicine with more than 10 years of experience in fluoroscopy-guided injections. The success cervical epidurography was evaluated and recorded. Adverse events of intravascular, subdural, or intrathecal injection were also evaluated. A second investigator who was independent to the fluoroscopic image and performance of CESI assessed the epidural waveform. When the proper epidural waveform appeared in the monitor subsequently after LOR, this waveform was digitally captured using a mobile phone. This waveform was classified as strong, moderate, weak, and absent according to the amplitude. We determined the waveform according to the systolic part of pulsatile wave such as strong (20 ∼ 30 mmHg), moderate (15 mmHg), weak (beneath 15 mmHg), and absent.
Strong, moderate, and weak oscillations were considered having positive waveform, whereas absent oscillations were considered negative waveforms (Figs. 1A–D). We considered as a false LOR when an unsuccessful epidurograhy was obtained in spite of satisfactory LOR.
Figure 1.
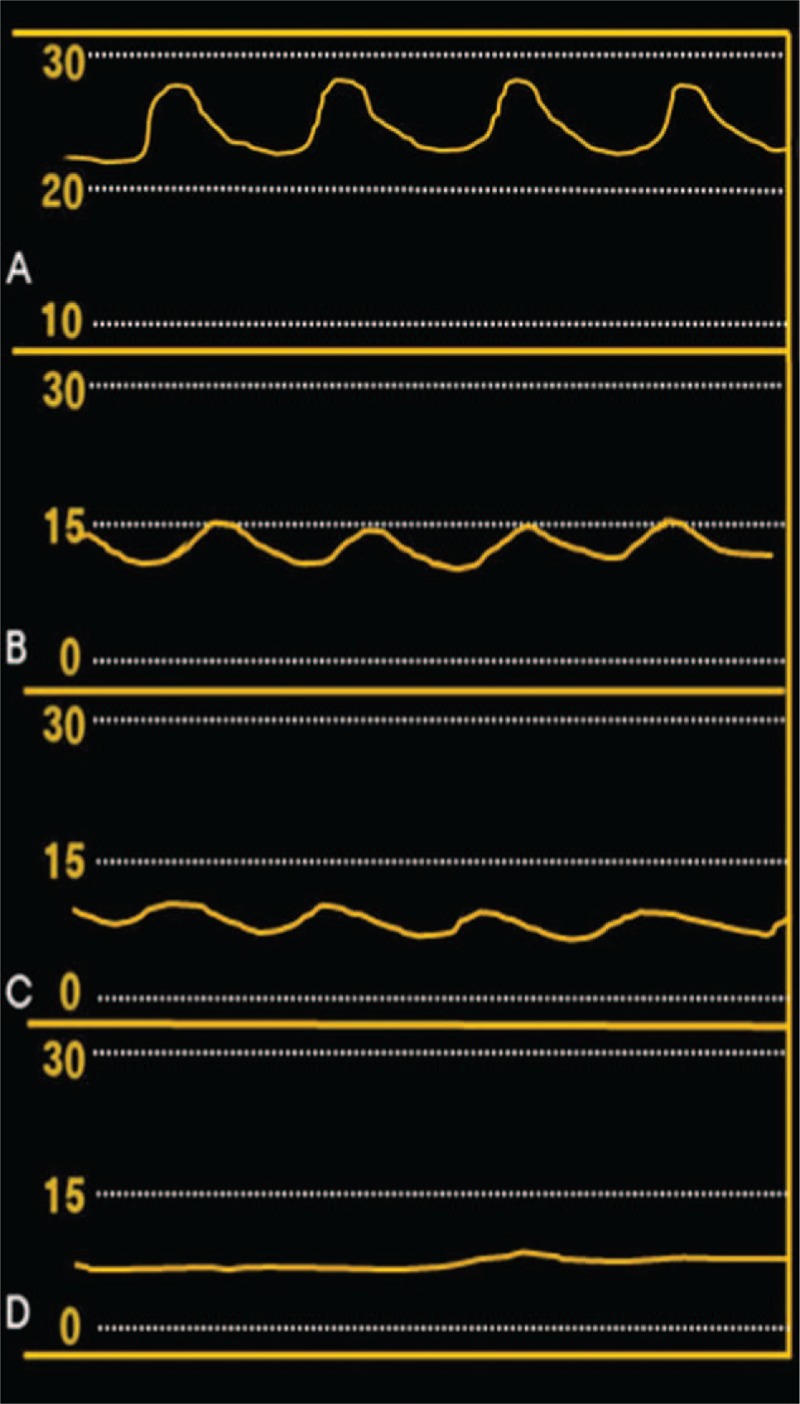
Illustration of epidural waveforms representing (A) strong, (B) moderate, (C) weak, and (D) absent. Waveform was presented according to the systolic part of pulsatile wave such as strong (20 ∼ 30 mmHg), moderate (15 mmHg), weak (beneath 15 mmHg), and absent.
Patients who completed the study were injected with 4 mL of 0.2% ropivacaine mixed with dexamethasone 5 mg.
Demographic data (age, gender, height, weight, duration of symptom, and type of disease) were obtained before CESI. During the performance of CESI, the incidence of false LOR and epidural pressure were also measured. Adverse events including subdural, intrathecal or intravascular injections were evaluated.
2.4. Statistics
We calculated the sample size of this study based on the specificity of EPWA. Leurcharusmee et al[11] reported a specificity of EPWA of 83.8%, whereas our preliminary study indicated a value of 95%. On the basis of an α error level of 0.05, a β error level of 0.2, and a 2-sided test, 105 injections were required as a total sample size with an 80% power.
3. Results
One hundred and five CESIs of 75 patients were evaluated. The reason for CESI was neck and radicular arm pain due to herpes zoster, herniated nucleus, spinal stenosis, and facet arthropathy. The rate of incorrect identification of epidural space with LOR (false LOR) was 29.5% (31/105). Of these 31 failed CESIs, 2 showed an epidural waveform and 29 did not. Overall, 72 cases of CESI showed epidural waveform. Among the 72 cases, more than half of the CESIs showed epidural waveform of weak oscillation. The measured epidural pressure was 15.5 ± 5.4 mmHg (Table 1, Fig. 1).
Table 1.
Patient characteristics and cervical epidural steroid injection measurements.
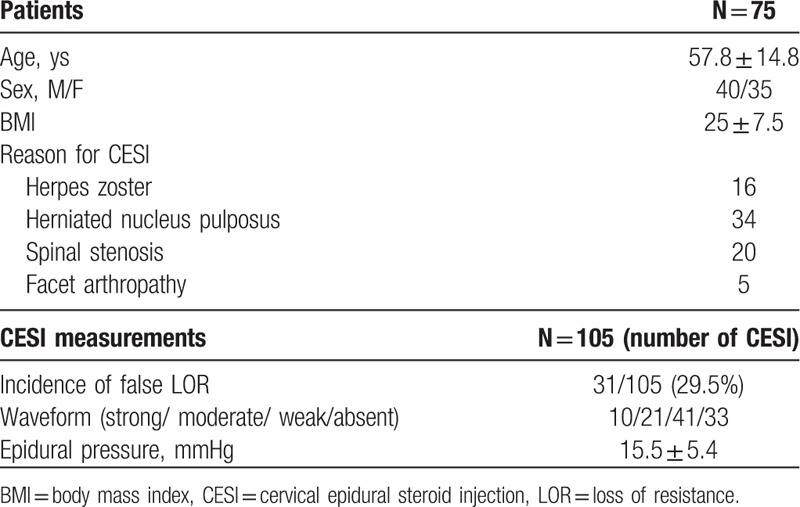
The sensitivity, specificity, positive and negative predictive value of EPWA was 94.5%, 93.5%, 97.2%, and 87.7%, respectively. False positive and false negative values were 6.4% and 5.4%, respectively (Table 2).
Table 2.
Comparison of epidural wave with epidurography.
Dural puncture occurred in 2 cases of CESI (1.9%). Epidural waveform was also observed in 2 cases of dural puncture. Two patients experienced a self-relieving paresthesia. Three cases of intravascular injection confirmed with fluoroscopy were found.
4. Discussion
It is postulated that the pulsatile wave shown in EPWA is transmitted from the pulsating spinal cord through the fluid-filled subarachnoid space and through the dura matter.[7]
This reliability study of EPWA at the cervical region showed 94.5% sensitivity, 93.5% specificity, 97.2% positive predictive value, and 87.7% negative predictive value. The high sensitivity and positive predictive value is similar to previous results.[7–9,11] However, our study should be differentiated from previous studies because we confirmed the success of epidural block using fluoroscopy. In another study, among 37 failed epidural blocks, 27 provided no sensory anesthesia at 10 minutes and 10 subjects was unable to be threaded with the catheter through the needle.[11] Success or failure can be uncertain in such patients who are not threaded with the catheter. In addition, the 27 patients confirmed to be a failure of epidural block due to no sensory anesthesia at 10 minutes would still have a possibility of success. A 10-minute delay might not be sufficient to show sensory anesthesia in a small number of patients. Previously, most epidural cases showed bilateral sensory anesthesia to ice within 10 minutes or less; however, 4% of patients required 12 to 15 minutes.[16] False positive rates were reportedly reduced by waiting more than 10 minutes before block.[11] Fluoroscopy or computed tomography is the gold standard criterion to confirm the success of epidural block. We could minimize the ambiguous cases of success or failure by confirming every CESIs using fluoroscopy.
We think that the main benefit of implementing EPWA during fluoroscopy guided ESI is to minimize the injection of contrast medium to the non-epidural space. The inadvertent injection of contrast medium to muscle or other ligamentous structure can interrupt further ESIs by limited visualization of the bony landmark. According to our study, the primary block failure rate (incidence of false LOR) was 29.5% (31/105). Of these 31 failed CESIs, which means epidurography (−), 2 (ie, false positive waveform) showed the epidural waveform whereas 29 (ie, true negative waveform) did not. This means that if we had implemented the EPWA, we could have prevented injection of the contrast medium to the 29 CESIs not showing epidural waveform. The 2 CESIs among the 31 failed CESIs showed epidural waveform even though the needle was not located in the epidural space. These epidural waveforms fluctuated with the pattern of respiration. We speculate that the 2 CESIs were falsely interpreted as positive waveforms due to this fluctuating waveform influenced by respiration. As the needle is inserted at lower neck (C6-7), which is not far from the chest, movement of the chest during respiration can be transmitted to the needle. However, in most cases, the appearance of waveform was evident whether it was pulsatile or fluctuating.
Among the 74 successful CESIs, which means epidurography (+), 4 (ie, false negative waveform) did not show any epidural waveform despite being in the epidural space. The results of prior study suggested the suboptimal volume of normal saline through the epidural needle before EPWA as a main reason of false negative rate.[11] Although our study used a 5 mL volume based on the results,[17] this volume provided positive waveforms in only 90% of their subjects.[17] Therefore, we suggest that the use of a greater volume of normal saline could decrease the rate of false negative waveforms. Another reason might be the technical error, that is, the failure of scale adjustment (0 ∼ 30 mmHg) before measurement of EPWA.
This study demonstrated the incidence of false LOR as 29.5% which is similar to previous results performed in cervical area, [1,5] and higher than the results of lumbar area.[1]
To reduce the false LOR, various methods including the use of contrast medium or epidrum to detect LOR have been studied.[5,6] We suggest that EPWA might be more valuable if it is applied to CESI which shows high false LOR rate and one adjunctive method to reduce the failure of CESI.
We encountered 2 cases of intrathecal injection during this study. The same pulsatile waveform during successful epidural injection was also observed in intrathecal injection. Therefore, EPWA should not be used in differentiating between intrathecal and epidural injection. Fluoroscopy or computed tomography should be the confirmative tool. Inadvertent cervical dural punctures attributed to CESI may lead to neurologic complication.[18]
Although we confirmed high sensitivity and specificity of EPWA, this method still lacks the popularity as an adjunctive tool of LOR. Further studies or follow-up trials including minimizing the cost of pressure transducer are required to gain popularity and be used broadly.
Our study was designed to show that EPWA can exclude false-positive LOR, therefore, its important role would be differentiating between false positive and true positive LOR (conclude that the needle is in the epidural space by positive epidural wave after LOR), the most important parameter is the positive predictive value. In this point of view, the sample size of this study was not enough. As we included only CESI, patients were limited and not so frequent compared to the lumbar area. Further reliable study with an enough sample size is required.
In summary, EPWA provided satisfactory sensitivity (94.5%), specificity (93.5%), as well as positive (97.2%) and negative (87.7%) predictive values for identification of the cervical epidural space. Although EPWA showed satisfactory results, further confirmative studies are required before its routine use in clinical practice.
Author contributions
Conceptualization: J.H. Hong.
Data curation: J.H. Hong.
Formal analysis: S. Jung.
Funding acquisition: J.H. Hong.
Investigation: J.H. Hong, S. Jung.
Resources: S. Jung.
Supervision: S. Jung.
Visualization: S. Jung.
Writing – original draft: J.H. Hong.
Writing – review & editing: J.H. Hong.
Footnotes
Abbreviations: CESI = cervical epidural steroid injection, EPWA = epidural pressure waveform analysis, LOR = loss of resistance.
This work was supported by the National Research Foundation of Korea (NRF) Grant funded by the Korea Government (MSIP) (No.2014R1A5A2010008).
The authors declare no conflicts of interest.
References
- [1].Tran DQ, Gonzalez AP, Bernucci F, et al. Confirmation of loss-of-resistance for epidural analgesia. Reg Anesth Pain Med 2015;40:166–73. [DOI] [PubMed] [Google Scholar]
- [2].Lirk P, Moriggl B, Colvin J, et al. The incidence of lumbar ligamentum flavum midline gaps. Anesth Analg 2004;98:1178–80. [DOI] [PubMed] [Google Scholar]
- [3].Lirk P, Kolbitsch C, Putz G, et al. Cervical and high thoracic ligamentum flavum frequently fails to fuse in the midline. Anesthesiology 2003;99:1387–90. [DOI] [PubMed] [Google Scholar]
- [4].Lirk P, Colvin J, Steger B, et al. Incidence of lower thoracic ligamentum flavum midline gaps. Br J Anesth 2005;94:852–5. [DOI] [PubMed] [Google Scholar]
- [5].Kim YU, Kim D, Park JY, et al. Method to reduce the false-positive rate of loss of resistance in the cervical epidural region. Pain Res Manag 2016;2016:9894054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lee JY, Lee SM, Sim WS, et al. False loss of resistance in cervical epidural injection: the loss of resistance technique compared with the epidrum guidance in locating epidural space. Pain Physician 2016;19:131–8. [PubMed] [Google Scholar]
- [7].Lennox PH, Umedaly HS, Grant RP, et al. A pulsatile pressure waveform is a sensitive marker for confirming the location of the thoracic epidural space. J Cardiothorac Vasc Anesth 2006;20:659–63. [DOI] [PubMed] [Google Scholar]
- [8].de Medicis E, Tetrault JP, Martin R, et al. A prospective comparative study of two indirect methods for confirming the localization of an epidural catheter for postoperative analgesia. Anesth Analg 2005;101:1830–3. [DOI] [PubMed] [Google Scholar]
- [9].Al-Aamri I, Derzi SH, Moore A, et al. Reliability of pressure waveform analysis to determine correct epidural needle placement in labouring women. Anesthesia 2017;72:840–4. [DOI] [PubMed] [Google Scholar]
- [10].Arnuntasupakul V, Van Zundert TC, Vijitpavan A, et al. A randomized comparison between conventional and waveform-confirmed loss of resistance for thoracic epidural blocks. Reg Anesth Pain Med 2016;41:368–73. [DOI] [PubMed] [Google Scholar]
- [11].Leurcharusmee P, Arnuntasupakul V, Chora De La Garza D, et al. Reliability of waveform analysis as an adjunct to loss of resistance for thoracic epidural blocks. Reg Anesth Pain Med 2015;40:694–7. [DOI] [PubMed] [Google Scholar]
- [12].Choi JW, Lim HW, Lee JY, et al. Effect of cervical interlaminar epidural steroid injection: analysis according to the neck pain patterns and MRI findings. Korean J Pain 2016;29:96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Manchikanti L, Nampiaparampil DE, Candido KD, et al. Do cervical epidural injections provide long-term relief in neck and upper extremity pain? A systematic review. Pain Physician 2015;18:39–60. [PubMed] [Google Scholar]
- [14].Shim E, Lee JW, Lee E, et al. Fluoroscopically guided epidural injections of the cervical and lumbar spine. Radiographics 2017;37:537–61. [DOI] [PubMed] [Google Scholar]
- [15].Stitz MY, Sommer HM. Accuracy of blind versus fluoroscopically guided caudal epidural injection. Spine (Phila Pa 1976) 1999;24:1371–6. [DOI] [PubMed] [Google Scholar]
- [16].Larsson J, Gordh TE. Testing whether the epidural works: too time consuming? Acta Anesthesiol Scand 2010;54:761–3. [DOI] [PubMed] [Google Scholar]
- [17].de Medicis E, Pelletier J, Martin R, et al. Technical report: optimal quantity of saline for epidural pressure waveform analysis. Can J Anesth 2007;54:818–21. [DOI] [PubMed] [Google Scholar]
- [18].Epstein NE. Neurological complications of lumbar and cervical dural punctures with a focus on epidural injections. Surg Neurol Int 2017;8:60. [DOI] [PMC free article] [PubMed] [Google Scholar]


