Abstract
This study was designed to assess the accuracy of point-of-care ultrasound in determining the position of double-lumen tubes (DLTs).
A total of 103 patients who required DLT intubation were enrolled into the study. After DLTs were tracheal intubated in the supine position, an auscultation researcher and ultrasound researcher were sequentially invited in the operating room to conduct their evaluation of the DLT. After the end of their evaluation, fiberscope researchers (FRs) were invited in the operating room to evaluate the position of DLT using a fiberscope. After the patients were changed to the lateral position, the same evaluation process was repeated. These 3 researchers were blind to each other when they made their conclusions. Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy were obtained by statistical analysis.
When left DLTs (LDLTs) were used, the accuracy of ultrasound (84.2% [72.1%, 92.5%]) was higher than the accuracy of auscultation (59.7% [45.8%, 72.4%]) (P < .01). When right DLTs (RDLTs) were used, the accuracy of ultrasound (89.1% [76.4%, 96.4%]) was higher than the accuracy of auscultation (67.4% [52.0%, 80.5%]) (P < .01). When LDLTs were used in the lateral position, the accuracy of ultrasound (75.4% [62.2%, 85.9%]) was higher than the accuracy of auscultation (54.4% [40.7%, 67.6%]) (P < .05). When RDLT were used, the accuracy of ultrasound (73.9% [58.9%, 85.7%]) was higher than the accuracy of auscultation (47.8% [32.9%, 63.1%]) (P < .05).
Assessment via point-of-care ultrasound is superior to auscultation in determining the position of DLTs.
Keywords: anesthesiology, fiberoptic bronchoscopy, point-of-care ultrasound
1. Introduction
The lung isolation technique has been widely used for thoracic surgery, minimally invasive cardiac surgery, and so on.[1,2] Single-lumen tubes, bronchial blockers, and double-lumen tubes (DLTs) have been primarily used for pulmonary sequestration techniques. However, DLTs are still the major and popular method, which has been used for lung isolation. The proper placement of DLTs was been regarded as one of the basis of anesthetic management. Clinical methods such as auscultation could lead to many problems, and were believed to be not reliable.[3,4]
Fiberoptic bronchoscopy (FB) has been regarded as the golden standard for its visualization of DLTs in the trachea and bronchia.[5,6] The study conducted by Smith has revealed that the misplacement of DLTs was approximately 48% when performed through blind methods.[7] However, there are still some problems that require more concern such as high costs, fragility, and cross-infection.
Point-of-care ultrasound (POCU) has gained much development in recent years, especially in Anesthesiology and the Intensive Care Unit (ICU). At present, this technique has gained much attention in clinical anesthesia, such as nerve blocks, vascular puncture, transesophageal echocardiography (TEE), and so on. The judgment of the depth of the tracheal catheter is significantly important to patients, which would be helpful in avoiding complications. Many studies have reported that POCU could provide important information on the depth of the tube in patients such as in pediatrics and those who need emergent tracheal intubation.[8–11] However, most of these studies were based on the pleural gliding sign t technique. The gliding of the pleura could be easily observed by ultrasound. According to the presence of pleural gliding, it could be confirmed whether ventilation is present or not.[12–14]
The movement of the diaphragm and pleura, which could be quickly and efficiently observed by ultrasound, has been regarded as indirect quantitative and qualitative indicators of lung expansion.[15,16] The so-called “lung gliding” sign can easily be identified by ultrasound with an intercostal ultrasonographic view.[17]
The good positioning of DLTs is of great importance during an operation. However, few studies have used this technique to determine the position of DLTs. Including a quick ultrasound examination protocol to clinical assessments can ensure the more precise placement of left DLTs (LDLT)s compared with clinical assessment alone.[18] Another study also revealed that lung ultrasound was superior to clinical methods in confirming the adequate position of DLTs.[19]
LDLTs are more popular than right DLTs (RDLTs) for well-known reasons. However, there are no conclusions on whether POCU could be successfully used in the positioning of RDLTs. Furthermore, there was still no evidence on whether POCU is more accurate than auscultation when RDLTs were used. In most situations, the body position should be changed after anesthesia. The positioning can easily to be misplaced through changes in body position. In these cases, anesthesiologists have to readjust the tubes. Hence, more studies are needed to determine whether POCU would be effective for these cases.
The present study was designed to attempt to evaluate the ability of DLT positioning by POCU compared with auscultation. FB was designed as the gold standard.
2. Materials and methods
2.1. Participants
This study was performed at Department of Anesthesiology in Henan Provincial People's Hospital from April 2016 to December 2016. This research was approved by the Ethics Committee of the hospital. A signed informed consent was provided by the patients or their family members. After approval, a total of 132 elective thoracic patients were enrolled into this study. All patients were endotracheally intubated by DLTs. Generally, 35-Fr DLT and 37-Fr DLT were chosen for female and male patients, respectively. Inclusion criteria: patients who underwent elective thoracic surgery requiring lung isolation. Exclusion criteria: patients with a history of thoracic surgery, and no pleural gliding under ultrasound before anesthesia induction.
2.2. Study Protocol
2.2.1. Overview
In order to guarantee the blind principle of this study, 4 researchers were included into the study. Four roles were assigned to each of these researchers: the ultrasonic evaluation researcher (UR), in charge of the positioning of DLTs by ultrasound; the auscultation evaluation researcher (AR), in charge of the positioning of DLTs using a stethoscope; the fiberscope evaluation researcher (FR), in charge of the positioning DLTs using a fiberscope; the primary anesthesiologist (PR), responsible for the patients throughout the study.
2.3. The evaluation process
2.3.1. Supine position
After patients were delivered to the operating room, they were initially evaluated by the UR and AR. In order to ensure the balance between groups, a fixed point was located for research. The location points used by all the 3 evaluators were same, which was fixed at the crossing point between the second rib gap and the collarbone midline, the crossing point between the fifth rib gap, and the collarbone midline. The detection of the gliding lung sign, lung pulse, and diaphragmatic excursion can accurately detect the main stem bronchial intubation and the bronchial obstruction.[13]
The PR was in charge of these patients. All patients were ventilated by pressure controlled ventilation, the peak pressure was set at 20 cm H2O, and respiratory rate was set at 16 times/min.
Immediately after the DLTs were inserted, the position of the DLTs was evaluated by the AR. The satisfactory isolation standard decided by the AR were as follows: both 2 points of the independent lung had no breath sounds, while there were clear breath sounds in the dependent lung. If there were sounds in one point and no sounds in the other point, the isolation was judged not good. The result of the AR was recorded by the PR, and would be asked to leave the operating room.
After the evaluation by the AR, the UR would inter the operating room and conduct the evaluation. The positioning point was the same as that of the AR. Standard: Pleural gliding could be easily observed on the side of the dependent lung during one-lung ventilation (OLV), while there were no such signs on the independent lung. Hence, the UR would be judged as good.
The ultrasound device (Model: S-Nerve, HFL38x 13–6 MHz; Sono-Site) was prepared before intubation. The linear probe was used in the present study. Longitudinal section of the lib was adopted to make the pleura gliding sign clearly observed, as shown in Fig. 1. During the examination of each point, 3 breath cycles were needed. The typical pleural gliding sign was defined as clear pleural gliding in the ultrasound devices, especially when the B line was visible, as shown in Fig. 2A and B. When the M model was used, a beach sign could be observed when there was a pleural gliding sign, as shown in Fig. 2C; and the barcode sign could not be observed when there was no pleural gliding sign, as shown in Fig. 2D. The presence of a pleural gliding sign was considered to denote that there was ventilation of the lung, while no pleural gliding sign was believed to denote that there was no ventilation of the lung.
Figure 1.
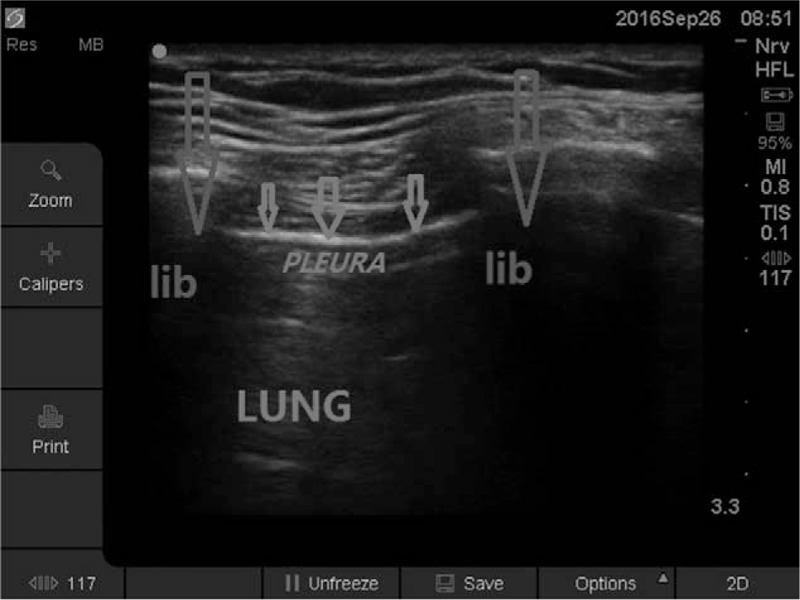
Lung, rib, and pleura were shown in the figure. Pleura were easily shown by the ultrasound which was recognized as a highlight line between the ribs and above the lungs. The pleura sling signs were mainly evaluated from the motion tracks of the pleura. It indicated that the wall sliding between the parietal pleura and visceral pleura.
Figure 2.
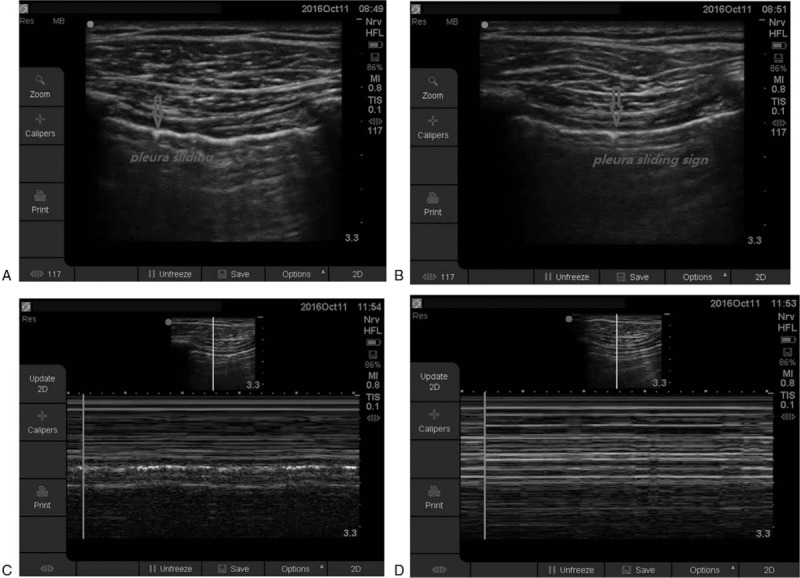
A and B: Pleura sliding sign were shown in these 2 pictures. In picture A, the point indicated by the red arrows showed one point of the pleura at the end of the expiratory. In picture B, this point was sliding to another location next to it at the end of respiratory. The 2 pictures clearly showed how the pleura sliding sign happened. C and D: Lung ventilations were shown in the ultrasound by the M model. In picture C, signs were seen which indicated there were ventilation under the probe. Barcode signs were seen in picture D, which indicated there was no ventilation under the probe. That means, if there were pleura sliding signs, lung ventilation were true under the probe, and beach signs will be seen clearly when using the M mode. M mode ultrasound was a good supplement in our study besides the sliding signs.
The distance between the skin and pleura were recorded. The results provided by the UR were recorded by the PR, and the evaluator would be instructed to leave the operating room.
After the evaluation by the UR, the FR would enter the operating room and commence the evaluation. Standard: When LDLTs were used, the proximal of blue capsule should be set below the promontory, and the 2 lobes of the left lung could be easily observed.
When RDLTs were used, the proximal of the blue capsule was set below the promontory, the middle and lower lobe of the right lung could be observed via the distal opening of the tube, and the upper lobe could also be observed via the lateral opening of the tube. The results of the evaluation conducted by the FR were recorded by the PR.
After the evaluation by the FR, the PR would readjust the DLT according to the result of the FR, if needed.
Lateral position: After the 3 researchers completed their evaluation, the patients were changed into the lateral position. The AR, UR, and PR would sequentially reevaluate the position of the DLT, similar to what they did when the patient was in the supine position.
Based on previous experiments,[4,20,21] the hypothesis of this study was that there would be a 20% difference between auscultation and ultrasound in terms of the accuracy of the evaluation of the DLT position. In order to detect this difference with a power of 80% and a P-value of .05, the power calculation indicated that a sample size of at least 35 experimental subjects and 35 control subjects is needed to reject the null hypothesis, in which the failure rates for the experimental and control subjects are equal, with a probability (power) of .8 and a type I error of 0.05.
2.3.2. Data Acquisition
Sex, age, body mass index, height, and the distance from the skin to the pleura were recorded. The results provided by the FR were regarded as the gold standard. The results provided by the AR and UR were scored as “Yes” or “No.”
2.3.3. Statistical Analysis
All data were present as means ± standard deviation. These experimental results were analyzed using SPSS 17.0 software (SPSS, Inc., Chicago, IL). The differences among groups were assessed by one-way analysis. A P-value <.05 was considered statistically significant.
3. Results
Signed informed consents were provided by the 132 subjects. Among these subjects, 14 subjects were excluded for the reason of no clear breath sounds before anesthesia, and 15 subjects were excluded for the reason of no clear pleural siding signs before anesthesia. A total of 103 subjects were finally enrolled into the study.
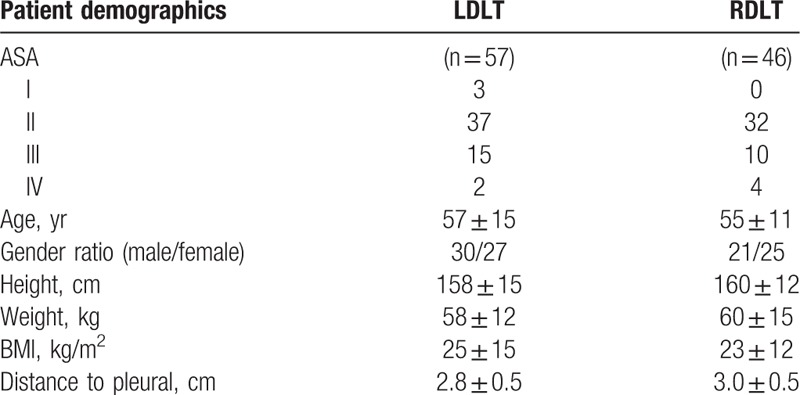
No significant differences were found among the general data such as sex ratio, age, body mass index, height, distance from skin to pleura, and type of surgery, as shown in Table 1.
Table 1.
General data of patient demographics.
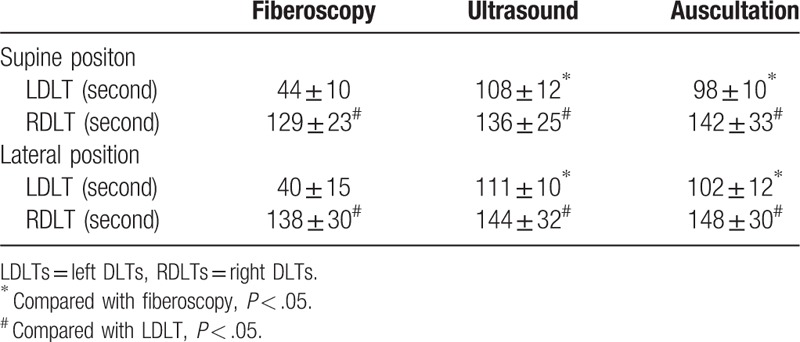
The total time for fiberscopic examination was shorter than those for ultrasound and auscultation examinations. Furthermore, the evaluation time of the UR was slightly longer than the AR, but there were no statistical differences. In addition, no differences were found between the supine position and lateral position, as shown in Table 2.
Table 2.
Time consumed by auscultation and ultrasound in determination of DLT location.
The main results of the present study were as follows: the accuracy of ultrasound was higher than the accuracy of auscultation. Compared with auscultation, ultrasound was recommended by the results of the present study, as shown in Table 3.
Table 3.
Test characteristics and results of auscultation versus ultrasound.
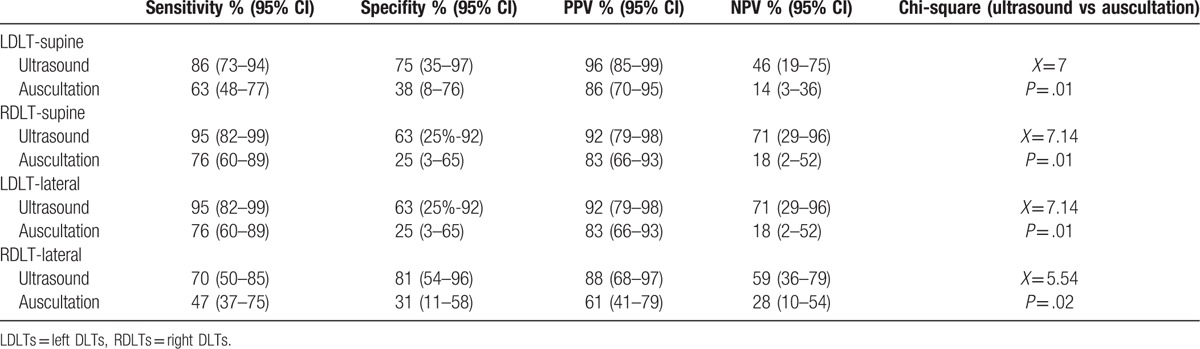
3.1. Supine position
When LDLTs were used, sensitivity and specificity for auscultation was 63.3% (48.3%–76.6%) and 37.5% (8.5%–75.5%), respectively, and sensitivity and specificity for ultrasound was 85.7% (72.8%–94.1%) and 75.0% (34.9%–96.8%), respectively. The accuracy of ultrasound (84.2% [72.1%–92.5%]) was higher than the accuracy of auscultation (59.7% [45.8%–72.4%]) (P = .0082 < .01).
When RDLTs were used, sensitivity and specificity for auscultation was 76.3% (59.8%–88.6%) and 25.0% (3.2%–65.1%), respectively, and sensitivity and specificity for ultrasound was 94.7% (82.3%–99.4%) and 62.5% (24.5%–91.5%), respectively. The accuracy of ultrasound (89.1% [76.4%–96.4%]) was higher than the accuracy of auscultation (67.4% [52.0%–80.5%]) (P = .0075 < .01).
3.2. Lateral position
When LDLTs were used, sensitivity and specificity for auscultation was 60.0% (43.3%–75.1%) and 41.2% (18.4%–67.1%), respectively, and sensitivity and specificity for ultrasound was 80.0% (64.4%–91.0%) and 64.7% (38.3%–85.8%), respectively. The accuracy of ultrasound (75.4% [62.2%–85.9%]) was higher than the accuracy of auscultation (54.4% [40.7%–67.6%]) (P = .0186 < .05).
When RDLTs were used, sensitivity and specificity of auscultation was 56.7% (37.4%–74.5%) and 31.3% (11.0%–58.7%), respectively, and sensitivity and specificity of ultrasound was 70.0% (50.6%–85.3%) and 81.3% (54.4%–96.0%), respectively. The accuracy of ultrasound (73.9% [58.9%–85.7%]) was higher than the accuracy of auscultation (47.8% [32.9%–63.1%]) (P = .02 < .05).
4. Discussion
The positioning of LDLTs and RDLTs differed significantly due to anatomical differences. For these reasons, the type of DLT and position of the body have to be taken into consideration. Our evaluation was based on the consideration of 4 factors: LDLT, RDLT, supine position, and lateral position.
From the results in the present study, we could draw a conclusion that ultrasound was better than auscultation. Ultrasound could become a better method compared with auscultation.
A total of 4 researchers were involved in this study: AR, UR, FR, and PR. Each of them has at least 8 years of experience in clinical anesthesia and at least 3 years of experience in DLT intubation. Each researcher was responsible for evaluating only 1 factor. The evaluation was performed in the operating room, except for the PR, in which the evaluations performed by the AR, UR, and FR were independent, and none of them knew about the conclusions made by the other researchers.
There were no significant differences in the general data. The distance from the skin to the pleura was an important characteristic. If the distance is too long, the breath sound by the AR and the pleural gliding by the UR would be easily disturbed. The evaluation point was located at the second and fifth lib, and was distant from the breast, allowing it not to be easily disturbed.
The evaluation of pleural gliding signs needs a duration of ventilation and working knowledge of the operators.[12,13,20] When LDLTs were used, the evaluation time of the FR was significantly shorter than the AR and UR. The evaluation time for ultrasound in the present study was shorter than that reported by Ramsingh, which was 162 ± 38 seconds.[3] These differences were probably related to the method ever used: Ramsingh not only detected the pleural gliding sign, but also the cricothyroid membrane and ETT cuff. These prolonged the evaluation time. Furthermore, there were no differences in evaluation time between the AR and UR. The evaluation point of these 2 researchers was the same. At least 3 breath cycles and 2-lung evaluations were needed no matter what type of DLT was used. Further studies also indicated that compared with LDLTs, the positioning time of RDLTs was longer, and there were no differences among these 3 researchers. These results may be related to the process of finding the opening of the right upper lobe. Usually, the opening of the right upper lobe was slightly hard to find when evaluated by the FR due to its anatomical variations. Hence, we conclude that when LDLTs were used, the evaluation time by FR was shorter than the AR and UR. However, no differences were found when RDLTs were used.
Changes in body position would influence the effect of DLTs, and subsequently, the results. Discussing only the evaluation in the supine position would not be sufficient enough, since thoracic surgery is usually achieved in the lateral position, and the readjustment of the position of the DLT is often necessary. Therefore, the conclusion drawn only from results in supine is not sufficient. For this reason, after the evaluation was performed in the supine position, we conducted further research in the lateral position. The methods used were the same as that in the supine position.
Our results revealed that the sensitivity and specificity of auscultation were both lower than those of ultrasound. Furthermore, the accuracy of ultrasound was significantly higher than the accuracy of auscultation. Auscultation has been known as the standard for the determination of tracheal intubation.[21] However, the sensitivity of auscultation to distinguish tracheal intubation and bronchial intubation was as low as 60% to 65%.[22,23] Hence, auscultation is not a reliable tool for the positioning of DLTs.[24,25] In the present study, although the auscultation was performed by a fixed researcher and a fixed stethoscope, the evaluation of the breath sound was easily affected by many factors, such as the voice from the contra-lateral lung breath sounds, the environment of the operating room, the noise in the operating room, the physiological state of the operator, and so on. The process of auscultation has some subjectivity. Compared with auscultation, ultrasound had more advantages. The pleural gliding sign, lung pulse, and diaphragmatic excursion can be easily displayed on the screen by ultrasound.[13,26] The M-mode ultrasound was also helpful: the beach sign appears only when pleural gliding exists, and the barcode sign appears when the pleural gliding sign is not present. Therefore, ultrasound is more objective and less susceptible to interference. Auscultation could be replaced by ultrasound to position the DLT.
This study is the first to discuss the accuracy of ultrasound both in the supine and lateral positions. Most previous studies have only revealed the evaluation of DLTs in the supine position. However, most thoracic operations are performed in the lateral position. The accuracy of ultrasound declined from the supine position to the lateral position. These results revealed that changes in body position induced the accuracy decline both in auscultation and ultrasound. The reason was thought to be associated with 2 factors: first, thoracic and lung compliances were declined in the lateral position compared with the supine position, affecting the evaluation of breath sounds and pleural gliding; second, the relative location of the lung tissue and trajectory would be changed, increasing the difficulty of the evaluation.
Although this technique is still not commonly used in clinical practice, POCU continuous to show more advantages in many areas. On one hand, more training programs were needed to allow more doctors master this technique.[27,28] On the other hand, the ultrasound itself needs to be further revolutionized, while lowering its cost.
Overall, the present study shows that POCU is more accurate than auscultation in the positioning of DLT. Further studies have shown that accuracy declined from the supine to the lateral position. However, POCU was still accurate and reliable in the lateral position. Hence, POCU is recommended for the positioning of DLTs.
There are still several limitations in our study that deserves attention:
-
(1)
Our conclusions were made based on the patients enrolled in our study, who met the criteria. However, the conclusions that could have been drawn from patients excluded from our study remain unknown. Further studies are needed for patients with chronic obstructive pulmonary disease (COPD), pleural adhesion and pneumothorax, whose breath sounds and/or pleural gliding are not obvious
-
(2)
The ideal position of DLTs should be as follows: When one lung is ventilated, the contra-lateral side should have no breath sounds or pleural gliding; and vice versa. However, in the present study, we only evaluated one of these, that is: the dependent lung that needs ventilation during the operation had breath sounds or pleural gliding signs, while the independent lung had none of the signs above. This criterion could ensure the need for an operation, the lung isolation would be considered to be good, and the collapse of the independent lung would be defined as satisfactory by the surgeons. Our standard may not be absolutely satisfactory for the re-inflation of the independent lung, and this usually occurs in clinical practice.
-
(3)
Our data shows that ultrasound was a reliable tool for the evaluation of DLTs. However, it could not completely rule out subjective factors. Pleural gliding signs were not so obvious in some cases, and accordingly, the decision may not be absolutely objective. In future studies, there is a need to conduct a hierarchical analysis for the degree of pleural gliding signs.
-
(4)
In the present study, we only evaluated the position with YES or NO. However, the true reason of the malposition was not defined and analyzed; and through ultrasound, we could not determine how to re-adjust the DLTs when the positioning is not good.
Author contributions
Conceptualization: W. Zhang, W-C. Hu.
Data curation: L. Xu, L. Wei, Q. Zhang, W-C. Hu.
Formal analysis: L. Wei, Q. Zhang, W-C. Hu.
Investigation: L. Xu, W-C. Hu.
Methodology: W. Zhang, W-C. Hu.
Project administration: W. Zhang.
Resources: L. Xu, L. Wei, Q. Zhang.
Software: L. Xu, L. Wei, Q. Zhang.
Validation: W. Zhang.
Writing – original draft: L. Wei, W-C. Hu.
Writing – review & editing: L. Xu, Q. Zhang, W. Zhang.
Footnotes
Abbreviations: AR = auscultation evaluation researcher, COPD = chronic obstructive pulmonary disease, DLTs = double-lumen tubes, FB = fiberoptic bronchoscopy, FR = fiberscope evaluation researcher, FRs = fiberscope researchers, ICU = intensive care unit, LDLTs = left DLTs, OLV = one-lung ventilation, POCU = point-of-care ultrasound, PR = primary anesthesiologist, RDLTs = right DLTs, TEE = transesophageal echocardiography, UR = ultrasonic evaluation researcher.
Fundings: Science and Technology Project of Henan Province (182102310167) and Medical Science Research Project of Henan Province (201602227).
The authors declare that they have no competing interests.
References
- [1].Bahk JH, Lim YJ, Kim CS. Positioning of a double-lumen endobronchial tube without the aid of any instruments: an implication for emergency management. J Trauma 2000;49:899–902. [DOI] [PubMed] [Google Scholar]
- [2].Moloney JT, Fowler SJ, Chang W. Anesthetic management of thoracic trauma. Curr Opin Anaesthesiol 2008;21:41–6. [DOI] [PubMed] [Google Scholar]
- [3].Ramsingh D, Frank E, Haughton R, et al. Auscultation versus point-of-care ultrasound to determine endotracheal versus bronchial intubation: a diagnostic accuracy study. Anesthesiology 2016;124:1012–20. [DOI] [PubMed] [Google Scholar]
- [4].Seymour AH, Prasad B, McKenzie RJ. Audit of double-lumen endobronchial intubation. Br J Anaesth 2004;93:525–7. [DOI] [PubMed] [Google Scholar]
- [5].Cohen E. Double-lumen tube position should be confirmed by fiberoptic bronchoscopy. Curr Opin Anaesthesiol 2004;17:1–6. [DOI] [PubMed] [Google Scholar]
- [6].Klein U, Karzai W, Bloos F, et al. Role of fiberoptic bronchoscopy in conjunction with the use of double-lumen tubes for thoracic anesthesia: a prospective study. Anesthesiology 1998;88:346–50. [DOI] [PubMed] [Google Scholar]
- [7].Smith GB, Hirsch NP, Ehrenwerth J. Placement of double-lumen endobronchial tubes. Correlation between clinical impressions and bronchoscopic findings. Br J Anaesth 1986;58:1317–20. [DOI] [PubMed] [Google Scholar]
- [8].Hiruma M, Watanabe T, Baba H. Using lung ultrasound in an infant to detect bronchial intubation not previously identified by auscultation. Can J Anaesth 2015;62:1121–2. [DOI] [PubMed] [Google Scholar]
- [9].Abbasi S, Farsi D, Zare MA, et al. Direct ultrasound methods: a confirmatory technique for proper endotracheal intubation in the emergency department. Eur J Emerg Med 2015;22:10–6. [DOI] [PubMed] [Google Scholar]
- [10].Tessaro MO, Salant EP, Arroyo AC, et al. Tracheal rapid ultrasound saline test (T.R.U.S.T.) for confirming correct endotracheal tube depth in children. Resuscitation 2015;89:8–12. [DOI] [PubMed] [Google Scholar]
- [11].Hoffmann B, Gullett JP, Hill HF, et al. Bedside ultrasound of the neck confirms endotracheal tube position in emergency intubations. Ultraschall Med 2014;35:451–8. [DOI] [PubMed] [Google Scholar]
- [12].Weaver B, Lyon M, Blaivas M. Confirmation of endotracheal tube placement after intubation using the ultrasound sliding lung sign. Acad Emerg Med 2006;13:239–44. [DOI] [PubMed] [Google Scholar]
- [13].Blaivas M, Tsung JW. Point-of-care sonographic detection of left endobronchial main stem intubation and obstruction versus endotracheal intubation. J Ultrasound Med 2008;27:785–9. [DOI] [PubMed] [Google Scholar]
- [14].Chun R, Kirkpatrick AW, Sirois M, et al. Where's the tube? Evaluation of hand-held ultrasound in confirming endotracheal tube placement. Prehosp Disaster Med 2004;19:366–9. [DOI] [PubMed] [Google Scholar]
- [15].Gerscovich EO, Cronan M, McGahan JP, et al. Ultrasonographic evaluation of diaphragmatic motion. J Ultrasound Med 2001;20:597–604. [DOI] [PubMed] [Google Scholar]
- [16].Müller NL. Imaging of the pleura. Radiology 1993;186:297–309. [DOI] [PubMed] [Google Scholar]
- [17].Lichtenstein DA, Menu YA. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding. Chest 1995;108:1345–8. [DOI] [PubMed] [Google Scholar]
- [18].Sustić A, Protić A, Cicvarić T, et al. The addition of a brief ultrasound examination to clinical assessment increases the ability to confirm placement of double-lumen endotracheal tubes. J Clin Anesth 2010;22:246–9. [DOI] [PubMed] [Google Scholar]
- [19].Álvarez-Díaz N, Amador-García I, Fuentes-Hernández M, et al. Comparison between transthoracic lung ultrasound and a clinical method in confirming the position of double-lumen tube in thoracic anaesthesia. A pilot study. Rev Esp Anestesiol Reanim 2015;62:305–12. [DOI] [PubMed] [Google Scholar]
- [20].Williamson JP, Grainge C, Parameswaran A, et al. Thoracic ultrasound: what non-radiologists need to know. Curr Pulmonol Rep 2017;6:39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Guidelines for cardiopulmonary resuscitation and emergency cardiac care. Emergency Cardiac Care Committee and Subcommittees, American Heart Association. Part I. Introduction. JAMA 1992;268:2171–83. [PubMed] [Google Scholar]
- [22].Vezzani A, Manca T, Brusasco C, et al. Diagnostic value of chest ultrasound after cardiac surgery: a comparison with chest X-ray and auscultation. J Cardiothorac Vasc Anesth 2014;28:1527–32. [DOI] [PubMed] [Google Scholar]
- [23].Sitzwohl C, Langheinrich A, Schober A, et al. Endobronchial intubation detected by insertion depth of endotracheal tube, bilateral auscultation, or observation of chest movements: randomised trial. BMJ 2010;341:c5943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Fischer GW, Cohen E. An update of anesthesia for thoracoscopic surgery. Curr Opin Anaesthesiol 2010;23:7–11. [DOI] [PubMed] [Google Scholar]
- [25].Parab SY, Divatia JV, Chogle A. A prospective comparative study to evaluate the utility of lung ultrasonography to improve the accuracy of traditional clinical methods to confirm position of left sided double lumen tube in elective thoracic surgeries. Indian J Anaesth 2015;59:476–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Sustić A. Role of ultrasound in the airway management of critically ill patients. Crit Care Med 2007;35:S173–7. [DOI] [PubMed] [Google Scholar]
- [27].Ramsingh D, Rinehart J, Kain Z, et al. Impact assessment of perioperative point-of-care ultrasound training on anesthesiology residents. Anesthesiology 2015;123:670–82. [DOI] [PubMed] [Google Scholar]
- [28].Ramsingh D, Fox JC, Wilson WC. Perioperative point-of-care ultrasonography: an emerging technology to be embraced by anesthesiologists. Anesth Analg 2015;120:990–2. [DOI] [PubMed] [Google Scholar]


