Abstract
Radiotherapy is a reliable method to cure cervical cancer patients, but it could cause serious urological complications after the treatment due to the anatomical location of the cervix. The main purpose of this retrospective analysis is to study the incidence, latency, and therapeutic efficacy of urological complications caused by radical hysterectomy with postoperative radiotherapy or radiotherapy alone in patients with cervical cancer.
A retrospective analysis was conducted on patients with cervical cancer who received radical hysterectomy with postoperative radiotherapy or radiotherapy alone at the First Hospital of Jilin University between January 2010 and May 2016. The urological complications were confirmed by clinical manifestation, ultrasound, computed tomography (CT), nuclear scintigraphy, and assessment of renal function. All the patients with urological complications received conventional treatment, including conservative, electrosurgery, ureteral stents, nephrectomy, and neoplasty. The onset time of radiation injury symptoms was confirmed according to the medical history and follow-up. The surveillance for the therapeutic effects for these complications was accomplished by cystoscopy, imaging, and laboratory assessment.
The overall rate of urological complications after treatment was 3.26%, comprising 2.12% ureteral obstruction, 0.98% radiocystitis, and 0.16% vesicovaginal fistula. The incidence of ureteral obstruction in patients treated with radical hysterectomy with postoperative radiotherapy and radiotherapy alone was not statistically significant (2.18% vs 1.59%, P > .05). The median onset time of radiocystitis and ureteral obstruction was 10 months (0–75 months) and 12 months (2–66.3 months), respectively. The onset time of vesicovaginal fistula was 3.5 months. After the appropriate treatment, the majority of the complications were under control.
The incidence of urological complications is acceptable. There was no statistical difference in the risk between patients treated with radical hysterectomy with postoperative radiotherapy and radiotherapy alone. The latency period between radiotherapy and the manifestation of urological complications may be relatively long. So it is crucial to underline long-term follow-up after radiotherapy. The majority of urological complications were alleviated after symptomatic treatment and the patients with cervical cancer achieved long-term remissions or cures.
Keywords: cervical cancer, radiation cystitis, radiotherapy, ureteral obstruction, urological complications
1. Introduction
Cervical cancer is the second most common malignancy of women worldwide.[1] In the United States, there are estimated 12,820 new cases and 4210 deaths in 2017.[2] The treatment for cervical cancer includes surgery, radiation and chemotherapy, or different combinations of the 3 approaches.[3] According to the International Federation of Gynecology and Obstetrics (FIGO) clinical staging system, early tumor stages (IB-IIA) generally require surgery or definitive radiotherapy, while patients with more advanced disease are usually treated with primary (chemo-) radiotherapy.[4] Radiotherapy tends to be a proper treatment strategy for invasive cervical cancer in all stages.[5] The definitive radiotherapy in patients with stage IB1 or stage IIA1 cervical cancer has been confirmed to be associated with an improvement in overall survival (OS).[6] Postoperative radiotherapy significantly reduces locoregional recurrences in high risk cases[7] and decreases the risk of disease progression.[8] When assessing the results of a particular therapeutic method, not only the probability of tumor control but also the toxicity of the therapy should be considered. Due to the anatomical location of the cervix, the patients who received radiotherapy or combined radical surgery could suffer from serious urological complications, such as radiation-related cystitis, chronic renal failure, ureter obstruction, and sexual disorders.[9–11] These complications bring great agony and inconvenience to the lives of patients. The present report is a retrospective analysis to evaluate the morbidity of urological complications after cervical cancer radiotherapy. We present the crude incidence and latency of urological complications in cervical cancer patients, and assess the effectiveness of symptomatic treatment for complications.
2. Methods
2.1. Patients
The records for consecutive patients with cervical cancer, who received radical hysterectomy followed by radiotherapy or radiotherapy alone in the First Hospital of Jilin University between January 2010 and May 2016 were reviewed. Histologically, the patients were diagnosed with squamous cell carcinoma or adenocarcinoma between IB to IIIB stages. The FIGO evaluation procedures for staging were limited to colposcopy, biopsy, conization of the cervix, cystoscopy, and proctosigmoidoscopy. Patients were eligible for participation if: received radical hysterectomy followed by radiotherapy; treated by radical radiotherapy; normal transaminases, urine creatinine, and urine nitrogen; blood hemoglobin ≥ 9 g/dL, leucocytes ≥ 3000/mm3, and platelets ≥ 100,000/mm3. Patients were excluded because of: bladder irritation symptoms, hydronephrosis, and glandular cystitis before treatment with radical radiotherapy alone or concomitant radical hysterectomy; ureteral obstruction was proved to be caused by cervical cancer recurrence or metastasis; loss to follow-up. Eventually, 614 patients were eligible for this retrospective analysis. According to the selection of different treatments, the patients were divided into 2 groups. One group underwent radical hysterectomy with postoperative radiotherapy (RH + RT, n = 551), while the other group received radiotherapy alone (RT, n = 63). The median age of all patients at presentation was 47 years (26–77 years). All these 614 patients were followed-up by medical history and physical examination, cervical/vaginal cytology tests, imaging and laboratory assessment after discharging from hospital.
2.2. Treatment
Before brachytherapy (BT), all patients underwent external beam radiotherapy (EBRT). The median external irradiation dose was 46 Gy (40–48 Gy) in daily fractions of 2 Gy, 5 d/wk. EBRT was delivered by an 8-MV linear accelerator using a 4-field technique. Shielding was used to minimize dose to the bladder and kidney. The first intracavitary treatment was delivered within 1 to 2 weeks after completion of the initial external radiotherapy in most patients. BT was administered at a dose of 3 Gy per fraction, 3 times a week and given 8–15 fractions to point A. The median intracavitary brachytherapy dose to point A was 35 Gy (24–45 Gy). RT was normally started 7 to 10 days after radical hysterectomy.
Urological complications were identified by clinical manifestation, ultrasound, computed tomography (CT), nuclear scintigraphy, and measurement of renal function. The onset time of symptoms from radiation injury was confirmed according to the medical history and follow-up. Toxicities occurred during treatment or within 90 days after the end of treatment were defined as acute toxicity. Toxicities experienced after 90 days of treatment completion were regarded as late toxicity.[12]
The patients with radiation cystitis were managed with conservative treatments, such as indwelling catheterization, intermittent catheterization, anti-inflammatory therapy, or hemostatic drugs. Severe hemorrhagic cystitis patients were treated by transurethral electrocautery. For patients with hydronephrosis, ureteral stenting was the prime consideration. When the treatment failed or patients developed acute obstructive renal failure, the percutaneous nephridium puncturing ostomy under the B-ultrasound guiding was performed as life-saving treatment. If nuclear scintigraphy showed a functionless kidney, nephrectomy should be performed. The neoplasty was done for patients with vesicovaginal fistula at the 6 month after radiotherapy.
2.3. Follow-up
The recommended surveillance is based on the patients’ complications. Cystoscopy is recommended for patients with radiation cystitis every 3 to 6 months for 2 years, and then annually. Imaging (ultrasound, CT, or nuclear scintigraphy) is recommended for surveillance in patients with hydronephrosis or functionless kidney every 3 to 6 months. For patients with renal failure, laboratory assessment (blood urea nitrogen, creatinine) should be completed more frequently (e.g., every 1–2 months).
2.4. Statistical analysis
SPSS software package was used for statistical analyses. Pearson's chi-square tests were used for comparisons. A P value < .05 was considered statistically significant.
3. Results
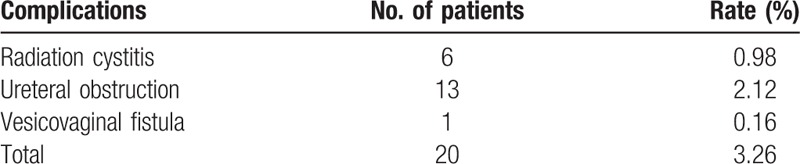
A total of 614 patients with cervical cancer FIGO stage IB-IIIB were candidates for this analysis. Urological complications occurred in 20 (3.26%) of all patients, which included 6 cases of radiation cystitis (0.98%), 13 cases of ureteral obstruction (2.12%) and one case of vesicovaginal fistula (0.16%) (Table 1).
Table 1.
The rate of urological complications.
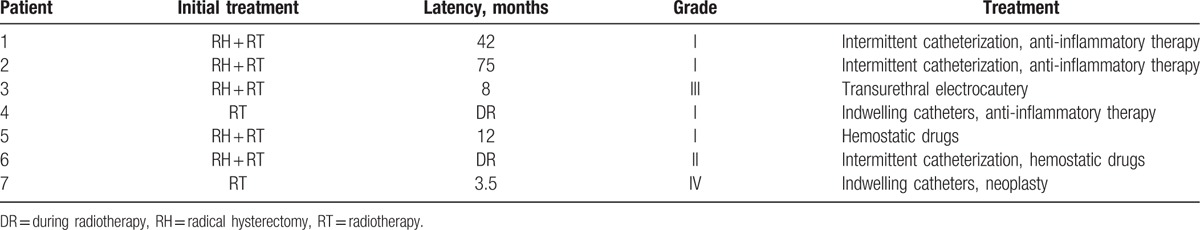
In 7 cases of bladder injury, 6 cases were radiation cystitis and 1 case was vesicovaginal fistula. Of these 7 patients, 2 suffered from acute toxicities and 5 suffered from late toxicities. The median onset time of radiation cystitis was 10 months (0–75 months). The urinary irritation symptoms of 5 patients were cured by conservative management, such as indwelling catheterization, intermittent catheterization, anti-inflammatory therapy, and hemostatic drugs. However, 1 patient with hematuria was considered as severe complication (Grade III). The patient was treated with transurethral electrocautery intervention. The onset time of vesicovaginal fistula was 3.5 months. The vesicovaginal fistula acquired satisfied therapeutic effect through neoplasty (Table 2).
Table 2.
Patients with bladder injury.
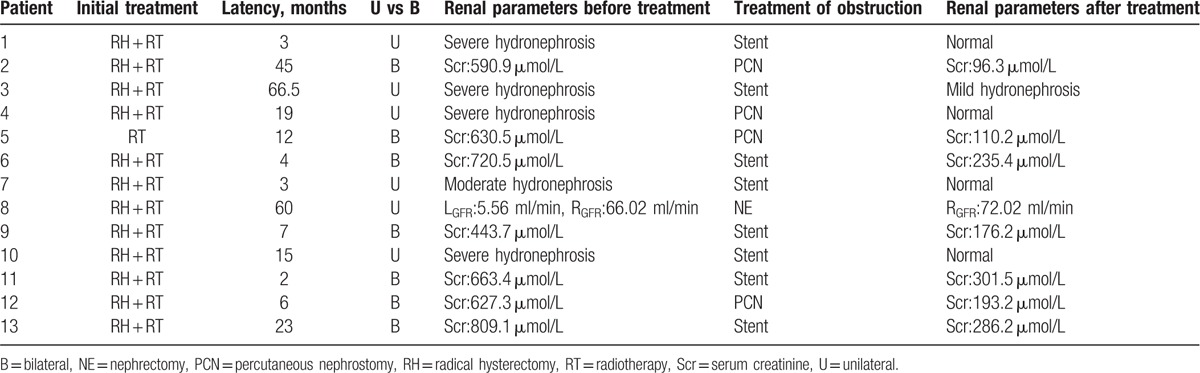
Thirteen cases (2.12%) developed ureteral obstruction, which occurred in 12 of 551 patients (2.18%) who received radical hysterectomy followed by radiotherapy and only in 1 of 63 patients (1.59%) who received radiotherapy alone. There were no significant differences in rates of ureter obstruction between these 2 groups (P > .05) (Table 3).
Table 3.
Frequency of ureteral obstruction in patients with different treatments.

The median onset time of ureteral obstruction was 12 months (2–66.3 months). Only 1 patient suffered acute toxicities. Six patients with unilateral ureter obstruction developed hydronephrosis. Ureteral stents were used for the treatment of hydronephrosis. One of these 6 patients underwent percutaneous nephrostomy drain under the B-ultrasound guiding after failure of indwelling ureteral stent. When unilateral hydronephrosis was accompanied with calculus and nonfunctioning kidney, laparoscopic nephrectomy was necessary.
Of the 7 patients with bilateral ureteral obstruction, 2 suffered from acute renal failure, 2 had azotemia, and 3 had mild hydronephrosis complicated by an upper urinary tract infection. The laboratory findings revealed that the serum creatinine and urea nitrogen of the 2 patients with acute renal failure were 590.9 μmol/L, 630.5 μmol/L, and 26.2 mg/dL, 36.39 mg/dL, respectively. They received percutaneous nephropyelostomy under the B-ultrasound guiding because of failure of ureteral stenting. The serum creatinine and urea nitrogen levels were then decreased. Patients with azotemia or mild hydronephrosis were treated with ureteral stenting to divert the urinary stream. The disease situations were effectively controlled. All patients with urological complications were relieved or recovered after treatment, which renal parameters were rechecked by B- ultrasound and laboratory examinations (Table 4).
Table 4.
Patients with ureteral obstruction.
The median follow-up time is 42 months (5–81 months). None of the patients died of complications during the follow-up. Through the appropriate treatment, the quality of life for the 20 patients has improved to various degrees.
4. Discussion
In this retrospective analysis, we reviewed the frequency of radiotherapy-related urological complications in patients with cervical cancer FIGO stage IB-IIIB treated with radical radiotherapy or concomitant radical hysterectomy. The overall rate of urological complication was 3.26%. Of these, 0.98% were presented as radiation cystitis, 2.12% as ureteral obstruction and 0.16% as vesicovaginal fistula. These results suggest that in patients with locally advanced cervical cancer, radiotherapy may produce relatively low and acceptable rates of toxicity. The incidence of complications may be reduced to some extent by careful dose planning and continuous observation of the patient during the irradiation.
Based on clinical symptoms, radiography and endoscopy, bladder complications were classified into 4 degrees of severity. Grade I: a single bleeding episode, hematuria, or several episodes of bleeding spaced at long intervals. Grade II: hematuria, which persists for months, with or without periods of normality. Grade III: severe hematuria that requires surgical intervention. Grade IV: fistulas.[13] In the present report, bladder injuries occurred in 7 patients. Severe complications including grades III and IV bladder injuries occurred in only 2 of the cases, representing 0.3% of all the recruited patients. This retrospective study is limited by the small size of sample, and makes it difficult to evaluate the toxicity, particularly grade I and II toxicities, which may not routinely be recorded by clinicians in the clinic. The urinary symptoms of these 7 patients were resolved and healed with homologous therapy. The temporary efficacy is noteworthy. However, young patients tend to have a greater lifetime risk after a recovery from the cervical cancer. This is attributed to the long latency period between radiotherapy and the manifestation of severe urological complications. Severe complications are extremely rare and can have a notoriously long latency period, for example bladder rupture and fistula formation.[14] Pandey et al[15] reported a case of extensive bladder necrosis with hydronephrosis and sepsis nearly 45 years after radiotherapy. Fortunately, after treatment, the patient recovered 6 months later with completely healed wounds and nearly normal renal parameters. In this study, the onset time of vesicovaginal fistula was 3.5 months, which was considered late toxicity. Thus, it is vital to pay attention to the past medical history of radiotherapy and observe for a long period.
It has been recognized that cervical cancer treatment increased the risk of developing ureteral obstruction.[16] The actual incidence of this complication is difficult to estimate. Our study demonstrated that the overall ureteral obstruction rate was 2.12%. We compared the morbidities of ureteral obstruction between patients treated with radical hysterectomy followed by radiotherapy and that received radiotherapy alone. There were no significant differences between the 2 groups, which was consistent with the previous study.[17] However, Elliott et al[18] reported that patients who underwent radiotherapy alone had a higher incidence of ureteral stricture than that of surgery with postoperative radiotherapy. The etiological factors of ureteral injury include damages by surgery or radiotherapy, tumor recurrence or metastasis and others. In the present study, in order to improve the accuracy of complication rate, we excluded patients with hydronephrosis or cervical cancer recurrence or metastasis before radiotherapy.
Previous investigators have reported that mean time of bladder injury to onset was 27 ± 21 months (3–94 months) following initiation of treatment,[19] while ureteral complications appeared later, between 25 and 30 years.[17] In the present study, the median onset time of radiation cystitis is 10 months (0–75 months), while that of ureteral obstruction is 12 months (2–66.5 months). The ureters could probably tolerate much higher doses of radiation, which make a contribution to explain the results mentioned above.
As regarding to the treatment of ureteral obstruction after radiotherapy, we prefer to operate percutaneous nephropyelostomy under the B-ultrasound guiding after failure of indwelling ureteral stent. Reimplantation of the ureters with an ureteroneocystostomy is not a reasonable choice when considering the long onset time of bladder complications. In addition, the reimplantation requires high surgical technical and may bring more postoperative complications. For the patients who have unilateral severe hydronephrosis without nonfunctional kidney, considering that the normal side ureter may narrow in months or years after complete irradiation, the nephrostomy is more effective than nephrectomy.
Data suggest that patients who undergo radiotherapy for pelvic cancers are at risk for radiation-induced second cancers, especially at radiated sites near the cervix. Therefore, careful surveillance is appropriate for these patients.[20,21] Salani et al[22] suggested that imaging was not routinely recommended for surveillance but might be indicated in patients with symptoms or findings that were suspicious for recurrence. Many other tests remained optional based on clinical indications, such as blood urea nitrogen and serum creatinine determinations. Our study suggested that imaging and laboratory assessment were essential for surveillance in patients with complications. B-ultrasound, nuclear scintigraphy, and laboratory assessment should be routine examination for the patients with urological complications during the follow-up. At follow-up, the majority patients achieved long-term remissions or recovery from urological complications, and the quality of life of the 20 patients has improved.
5. Conclusions
In conclusion, we found that the rate of urological complications was acceptable and the risk was similar for patients treated with radical hysterectomy with postoperative radiotherapy or radiotherapy alone. The onset time of the urological complications can be late, so it is crucial to follow-up for lifetime after radical hysterectomy with postoperative radiotherapy or radiotherapy alone. Though the treatment of the complications is challenging, the majority of urological complications have achieved long-term remissions or recovery. However, the nature of the retrospective study and the small size of samples with complications may attenuate our conclusion. Further prospective randomized clinical trials are necessary to confirm our findings.
Acknowledgments
The authors thank Professor Yuchuan Hou and our colleagues who provided insight and expertise that greatly assisted the research.
Author contributions
Investigation: H. Qiu.
Methodology: S. Liu.
Resources: C. Yang, K. Wang.
Software: C. Tang, Q. Zheng.
Writing – original draft: F. Li, H. Guo, Y. Hou.
Writing – review & editing: Y. Hou.
Footnotes
Abbreviations: B = bilateral, BT = brachytherapy, EBRT = external beam radiotherapy, FIGO = International Federation of Gynecology and Obstetrics, NE = nephrectomy, PCN = percutaneous nephrostomy, RH = radical hysterectomy, RT = radiotherapy, Scr = serum creatinine, U = unilateral.
Competing interests: The authors declare that they have no competing interests.
Ethics approval and consent to participate: The study protocol was approved by the medical center's ethical committee. All patients signed informed consents.
References
- [1].Brar H, Hogen L, Covens A. Cost-effectiveness of sentinel node biopsy and pathological ultrastaging in patients with early-stage cervical cancer. Cancer 2017;123:1751–9. [DOI] [PubMed] [Google Scholar]
- [2].Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin 2017;67:7–30. [DOI] [PubMed] [Google Scholar]
- [3].Steen R, Dahl AA, Hess SL, et al. A study of chronic fatigue in Norwegian cervical cancer survivors. Gynecol Oncol 2017;146:630–5. [DOI] [PubMed] [Google Scholar]
- [4].Koh W-J, Greer BE, Abu-Rustum NR, et al. Cervical cancer, version 2.2015. J Natl Compr Cancer Ne 2015;13:395–404. [DOI] [PubMed] [Google Scholar]
- [5].Matsumoto Y, Mabuchi S, Kozasa K, et al. The significance of tumor-associated neutrophil density in uterine cervical cancer treated with definitive radiotherapy. Gynecol Oncol 2017;145:469–75. [DOI] [PubMed] [Google Scholar]
- [6].Haque W, Verma V, Fakhreddine M, et al. Addition of chemotherapy to definitive radiotherapy for IB1 and IIA1 cervical cancer: analysis of the National Cancer Data Base. Gynecol Oncol 2017;144:28–33. [DOI] [PubMed] [Google Scholar]
- [7].Wolf B, Ganzer R, Stolzenburg J-U, et al. Extended mesometrial resection (EMMR): surgical approach to the treatment of locally advanced cervical cancer based on the theory of ontogenetic cancer fields. Gynecol Oncol 2017;146:292–8. [DOI] [PubMed] [Google Scholar]
- [8].Rogers L, Siu SS, Luesley D, et al. Radiotherapy and chemoradiation after surgery for early cervical cancer. Cochrane Database Syst Rev 2012;5:CD007583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Wit EM, Horenblas S. Urological complications after treatment of cervical cancer. Nat Rev Urol 2014;11:110–7. [DOI] [PubMed] [Google Scholar]
- [10].Perrucci E, Lancellotta V, di Benedetto M, et al. Encrusted cystitis after definitive radiotherapy for cervical cancer: a case report. J Contemp Brachyther 2016;8:541–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Mendez LC, Weiss Y, D'Souza D, et al. Three-dimensional-guided perineal-based interstitial brachytherapy in cervical cancer: a systematic review of technique, local control and toxicities. Radiother Oncol 2017;123:312–8. [DOI] [PubMed] [Google Scholar]
- [12].Ring KL, Young JL, Dunlap NE, et al. Extended-field radiation therapy with whole pelvis radiotherapy and cisplatin chemosensitization in the treatment of IB2-IIIB cervical carcinoma: a retrospective review. Am J Obstet Gynecol 2009;201:109e101–6. [DOI] [PubMed] [Google Scholar]
- [13].Bosch A, Frias Z. Complications after radiation therapy for cervical carcinoma. Acta Radiol Ther Phys Biol 1977;16:53–62. [DOI] [PubMed] [Google Scholar]
- [14].Gellrich J, Hakenberg OW, Oehlschlager S, et al. Manifestation, latency and management of late urological complications after curative radiotherapy for cervical carcinoma. Onkologie 2003;26:334–40. [DOI] [PubMed] [Google Scholar]
- [15].Pandey A, Beier J, Dobkowicz L, et al. Extensive necrosis of the bladder with hypostatic abscess: a late complication after radiotherapy. Onkologie 2010;33:116–8. [DOI] [PubMed] [Google Scholar]
- [16].Nakamura K, Kitahara Y, Satoh T, et al. Analysis of the effect of adjuvant radiotherapy on outcomes and complications after radical hysterectomy in FIGO stage IB1 cervical cancer patients with intermediate risk factors (GOTIC Study). World J Surg Oncol 2016;14:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Mclntyre JF, Eifel PJ, Levenback C, et al. Ureteral stricture as a late complication of radiotherapy for stage IB carcinoma of the uterine cervix. Cancer 1995;75:836–43. [DOI] [PubMed] [Google Scholar]
- [18].Elliott SP, Fan Y, Jarosek S, et al. Propensity-weighted comparison of long-term risk of urinary adverse events in elderly women treated for cervical cancer. Int J Radiat Oncol Biol Phys 2015;92:586–93. [DOI] [PubMed] [Google Scholar]
- [19].Georg P, Boni A, Ghabuous A, et al. Time course of late rectal- and urinary bladder side effects after MRI-guided adaptive brachytherapy for cervical cancer. Strahlenther Onkol 2013;189:535–40. [DOI] [PubMed] [Google Scholar]
- [20].Chaturvedi AK, Engels EA, Gilbert ES, et al. Second cancers among 104,760 survivors of cervical cancer: evaluation of long-term risk. J Natl Cancer Inst 2007;99:1634–43. [DOI] [PubMed] [Google Scholar]
- [21].Kumar S, Shah JP, Bryant CS, et al. Radiation-associated endometrial cancer. Obstet Gynecol 2009;113:319–25. [DOI] [PubMed] [Google Scholar]
- [22].Salani R, Backes FJ, Fung MF, et al. Posttreatment surveillance and diagnosis of recurrence in women with gynecologic malignancies: Society of Gynecologic Oncologists recommendations. Am J Obstet Gynecol 2011;204:466–78. [DOI] [PubMed] [Google Scholar]


