Abstract
Background
Depression is highly comorbid with anxiety in youth. It is frequently reported that anxiety precedes depression; however, evidence surrounding the temporal precedence of anxiety over depression is mixed. Many studies of anxiety-depression co-occurrence lump distinct forms of anxiety, obscuring information regarding trajectories of specific anxiety syndromes. This study sought to more accurately describe the development of anxiety and depression over time by moving beyond the question of temporal precedence to investigate a developmentally dynamic model of anxiety-depression co-occurrence.
Methods
A community sample of 665 youth (M=11.8, SD=2.4; 55% female) completed repeated self-report measures of depression and anxiety (social, physical, and separation anxiety) over a 3-year longitudinal study. Prospective associations between distinct syndromes of anxiety with depression were analyzed using an autoregressive cross-lagged path model over four time points.
Results
Physical symptoms and depression symptoms reciprocally predicted each other, above and beyond the stability of either domain. Social anxiety and depression symptoms similarly predicted each other in a systematic pattern.
Limitations
Our study is limited in its generalizability to other forms of anxiety, like worry. Additional research is needed to determine whether similar patterns exist in clinical populations, and whether these processes maintain symptoms once they reach diagnostic levels.
Conclusions
The development of syndromes of depression, physical, and social anxiety during childhood and adolescence occurs in a predictable, systematic reciprocal pattern, rather than sequentially and unidirectionally (i.e., anxiety syndromes precede depression). Results are clinically useful for predicting risk for disorder, and demonstrate the necessity of tracking symptom levels across domains.
Introduction
It is well established that depression is highly comorbid with anxiety during childhood and adolescence (Brady & Kendall, 1992). Estimates suggest that half of depressed individuals have a comorbid anxiety disorder (Kessler et al., 2003). Comorbidity is associated with greater symptom and diagnostic severity, and worse social functioning (Queen & Ehrenreich-May, 2014). It has been frequently reported that anxiety precedes depression (e.g., Cole, Peeke, Martin, Truglio, & Seroczynski, 1998; Keenan, Feng, Hipwell, & Klostermann, 2009; Avenevoli, Stolar, Li, Dierker, & Merikangas, 2001).
However, there are significant, unresolved questions regarding the temporal and longitudinal relations between anxiety and depression. While it has been established that youth who experience symptoms of anxiety are at heightened risk for later experiencing symptoms of depression (Kessler et al., 2005; Merikangas et al., 2010; Rohde, Lewinsohn, & Seeley, 1991; Cole et al., 1998), other research shows that those who experience symptoms of depression are similarly at greater risk for later symptoms of anxiety (Moffitt et al., 2007; Pine, Cohen, Gurley, Brook, & Ma, 1998; Merikangas et al., 2003). To date, most research has focused on a “which comes first” question regarding diagnostic patterns of depression and anxiety comorbidity. More recently, researchers have suggested that the temporal ordering between anxiety and depression may not be as straightforward as has been commonly presumed (Cummings, Caporino, & Kendall, 2014; Moffitt et al., 2007). The present study sought to advance knowledge on the temporal patterning of different forms of anxiety and depression by moving beyond the question of temporal precedence (i.e., “which comes first”) to investigate a more developmentally dynamic model of anxiety-depression co-occurrence over time.
An important issue that may obscure meaningful findings in the study of anxiety-depression co-occurrence is the lumping together of distinct forms of anxiety. In their “multiple pathways” model of anxiety-depression co-occurrence, Cummings and colleagues highlight the need for empirical work that does not treat anxiety as a single, isomorphic class of symptoms and disorder (Cummings et al., 2014). Anxiety disorders and their core defining features (e.g., generalized anxiety, social anxiety, panic, separation anxiety) are heterogeneous in their age of onset, longitudinal trajectories (Copeland, Angold, Shanahan, & Costello, 2014; Kessler et al., 2005), and symptom expression (Weems & Costa, 2005). Moreover, the rate of co-occurrence of these heterogeneous forms of anxiety with depression and other psychopathologies varies (Hankin et al., 2016; Angold, Costello, & Erkanli, 1999). Further, the degree of co-occurrence of different forms of anxiety with depression may vary by age and gender, based on the prevalence of each syndrome across childhood and adolescence for boys and girls (Cummings et al., 2014).
The current study longitudinally examined the reciprocal associations of depressive symptoms with different anxiety syndromes. Our main purpose was to investigate whether particular anxiety syndromes predict, and are predicted by, depression, in a systematic manner in youth, as theoretical work has emphasized the importance of examining interactive processes resulting in anxiety-depression co-occurrence (e.g., Cummings et al., 2014). A secondary goal was to examine whether developmental patterns of anxiety and depression co-occurrence are moderated by age and/or gender. To explore these descriptive questions, we assessed depression and different anxiety syndromes (social anxiety, panic, separation anxiety) using a multi-wave prospective design over a three-year follow-up across different age cohorts with community youth1. This study aims to contribute to a more nuanced, accurate picture of anxiety-depression co-occurrence over time in childhood and adolescence than the study of temporal precedence alone. By establishing a descriptive pattern of how different forms of anxiety relate to depression among youth, we can better understand processes that may explain why particular anxiety syndromes predict, and are predicted by, depression over time in a systematic manner.
Developmental Progression of Anxiety-Depression Co-Occurrence
A large body of research has investigated the temporal patterns of different forms of anxiety with depression (Cummings et al., 2014) with the goal of addressing the question of “which comes first.” Most prior work finds that anxiety, when broadly conceptualized and measured, predicts depression (e.g., Kouros, Quasem, & Garber, 2013; Kessler et al., 2005; Merikangas et al., 2010; Rohde et al., 1991; Cole et al., 1998). Much of this work combines multiple anxiety syndromes into a broad “anxiety symptoms” scale. However, this conclusion that anxiety precedes depression may depend on the specific anxiety syndromes examined as predictors of depression. We focus here on the association of syndromes of social anxiety, panic, and separation anxiety with depression. While much of the prior literature on anxiety-depression co-occurrence focuses on comorbidity at the disorder level, we focus on syndromes, as predictors of disorders (Gerhardt, Compas, Connor, & Achenbach, 1999). Existing models further emphasize the importance of studying anxiety-depression co-occurrence at the symptom- or syndrome-level, as youth with subclinical levels of these syndromes experience significant distress and impairment (Epkins & Heckler, 2011).
Social anxiety and depression are related during childhood and adolescence (Epkins & Heckler, 2011; Hamilton et al., 2016; Ranta, Kaltiala-Heino, Rantanan, & Marttunen, 2009); however, their temporal association has been debated. Cummings et al. (2014) proposed that social anxiety may predict depression, and vice versa, as impairment in one domain results in an increase in symptoms in the other domain. Many studies show that social anxiety predicts depression across the lifespan (e.g., Aune & Stiles, 2009; Last, Perrin, Hersen, & Kazdin, 1992; Beesdo et al., 2007). Others find that depression predicts social anxiety during adolescence, but that social anxiety did not predict depression (Hamilton et al., 2016). However, most of these studies have not repeatedly assessed social anxiety and depression with more than three time points. With three time points or fewer, it cannot be determined whether prediction from one symptom domain to another happened only once, or whether both temporal sequences exist as part of a larger pattern of mutually reinforcing symptom escalation (i.e., social anxiety predicts, and is predicted by, depression over time). This possibility has yet to be examined empirically.
Studies of adults find that panic is a risk factor for depression (Horn & Wuyek, 2010). However, National Comorbidity Survey data (Kessler et al., 1998) show of those individuals who reported both depressive episodes and panic attacks, 43.4% reported their first panic attack occurred before their first depressive episode, whereas 31.1% reported the reverse sequence. A review similarly found that panic precedes depression in one third of adults, depression precedes panic in another third, and panic and depression develop concurrently in the last third (Johnson & Lydiard, 1998). As panic has a later age of onset than social and separation anxiety, it may be more likely to temporally follow depression than either social or separation anxiety (Lewinsohn, Zinbarg, Seeley, Lewinsohn, & Sack, 1997). Thus, the precise temporal patterning between panic and depression symptoms is not well understood, especially among youth.
Most research has focused on separation anxiety as a risk factor for depression, and has found separation anxiety precedes depression (e.g., Lewinsohn et al., 1997). The median age of onset of separation anxiety disorder is younger than that of social anxiety and panic disorder across samples (Kessler et al., 2005; Last et al. 1992). Therefore, the temporal patterning of separation anxiety and depression may differ from that of other forms of anxiety with depression, such that separation anxiety may be most likely to precede depression symptoms. The heterogeneous ages of onset for different anxiety syndromes, combined with different temporal patternings of particular anxiety manifestations with depression, support the use of an analytical approach that can parse the independent associations of specific forms of anxiety with depression over time.
Moderators of Anxiety-Depression Co-occurrence
Age and gender may moderate the temporal associations of anxiety and depression. Depression and anxiety are more prevalent among girls than boys (Hankin et al., 1998; Costello et al., 1996; Axelson & Birmaher, 2001), and anxiety-depression co-occurrence is more common in girls (Cummings et al., 2014). Research finds greater heterotypic continuity from anxiety to depression, and vice-versa, for girls than for boys (Costello, Mustillo, Erkanli, Keeler, & Angold, 2003; McGee, Feehan, Williams, & Anderson, 1992). However, findings have been equivocal on whether gender moderates the development of anxiety and depression symptoms. Some studies have found stronger associations between anxiety and depression for girls over time (Merikangas et al., 2003), whereas others have not found that gender moderates developmental trajectories of anxiety and depression (McLaughlin & King, 2015; Hamilton et al., 2016). Relatedly, there are well-established age differences in both depression and certain forms of anxiety (Kessler et al., 2005), which have been proposed to lead to different patterns of comorbidity by age (Cummings et al., 2014). Few studies have examined whether age moderates trajectories of anxiety and depression across time.
Methodological Considerations
Much of the existing research has been limited to two- or three-point prospective designs (e.g., Avenevoli et al., 2001; Keenan et al., 2008; Pine et al., 1998), or to retrospective studies relying on participants’ recall of anxiety and depressive symptoms, which underestimate comorbidity rates (Angold et al., 1999; Moffitt et al., 2010). These designs were not structured to test for reciprocal associations in the developmental interplay of anxiety and depression. Important methodological considerations relevant to this issue can be drawn from the cascade model literature (e.g., Masten et al., 2005; Cole & Maxwell, 2003). Cascades refer to the process by which symptoms from one domain spill over to other domains, resulting in elevated symptom levels across domains over time (Masten & Cicchetti, 2010). Consistent with the cascade model literature, accurate delineation of the descriptive patterning of the temporal associations between different anxiety syndromes and depression benefits from a minimum of four time points with adequate spacing between follow-ups. This allows for change to occur in symptoms, and enables reliable prediction of co-occurring internalizing syndromes after controlling for the autoregressive stability of a particular internalizing syndrome (e.g., social anxiety) over time (Cole & Maxwell, 2003; Burt et al., 2008). The current study uses a multi-wave prospective design in which anxiety syndromes and depression were assessed across three years, and the repeated measures data analyzed across four assessment waves.
The Current Research
This study used data from a prospective longitudinal study of 3rd, 6th, and 9th graders recruited from the community to examine and more accurately describe the co-occurring temporal patternings and reciprocal effects of different anxiety syndromes and depression. We move beyond the question of “which came first” and examine the possibility of reciprocal effects in anxiety syndromes and depression to investigate how different anxiety syndromes and depression temporally relate to each other. Especially important to accurately delineating their longitudinal co-occurrence is distinguishing between syndromes of anxiety, given the established heterogeneity in anxiety. We also tested for moderation of the model by age and gender.
Method
Participants
Youth were recruited at the University of Denver and Rutgers University. Informational letters were sent home to families with a child in 3rd, 6th, or 9th grades in the broader Denver and central New Jersey areas. Of the families to whom letters were sent, 1,108 parents called the laboratory for more information. Parent report established that the parent and child were fluent in English, the child did not have an autism spectrum disorder, psychotic disorder, or intellectual disability. Of the families who initially contacted the laboratory, 665 (60%) qualified as study participants. The remaining 498 (40%) were nonparticipants for the following reasons: 4 (1%) were excluded because the parents reported that their child had an autism spectrum disorder or low IQ; 13 (3%) were non-English speaking families; 330 (71%) declined after learning about the study’s requirements; 113 (25%) were scheduled but did not arrive for assessment.
The final sample consisted of 665 youth from 7–17 years (M = 11.8, SD = 2.4). The sample was comparable to the community and school districts from which it was recruited. 62.2% of participants identified their race and ethnicity as white, 11.3% as African American, 7.5% as Latino/a, 9.6% as Asian or Pacific Islander, and 9.3% as another race or ethnicity. Median annual family income was $86,500. For additional details, see Hankin et al. (2015).
Procedure
Parents visited the laboratory for the baseline assessment and provided informed written consent. Youth provided informed written assent. Youth completed questionnaires assessing their depressive and anxious symptoms at baseline. Follow-up assessments evaluating child-reported symptoms of depression and anxiety occurred every 3 months after baseline for three years, for a total of 13 assessments. For purposes of the present investigation, these assessments were combined into four composite time points using averages: T1, T2, T3, and T4 (see the data analytic plan for further details regarding T1-T4). The Institutional Review Boards at both sites approved all procedures. Youth were compensated monetarily for their participation.
Measures
Depressive symptoms
The Children’s Depression Inventory (CDI; Kovacs, 1992) is a widely-used measure of depressive symptoms in youth that was administered at baseline and at each 3-month assessment. A total score, ranging from 0 to 54, is generated by summing all items. Higher scores indicate higher levels of depressive symptoms. The CDI has sound psychometric properties, including good internal consistency and construct validity (Klein, Dougherty, & Olino, 2005). In the current sample, internal consistency (α) was between 0.79 and 0.90 across all assessments.
Anxious symptoms
The Multidimensional Anxiety Scale for Children (MASC; March, Parker, Sullivan, Stallings, & Conners, 1997), a widely-used measure of anxious symptoms in youth, was administered at baseline and at each 3-month assessment. The MASC assesses physical symptoms of anxiety, harm avoidance, social anxiety, and separation anxiety, and shows good reliability and validity (March et al., 1997). The present study included the physical panic symptoms, social anxiety, and separation anxiety subscales, which are associated with risk for their specific disorders and demonstrate discriminant validity (van Gastel & Ferdinand, 2008; Wei et al., 2014; March et al., 1997). Subscale scores for physical symptoms, social anxiety, and separation anxiety were created by computing a mean score of the items in each subscale. Higher scores indicate higher levels of anxious symptoms. Internal consistency was adequate for all subscales across all time points in the present sample (α > .80 for physical symptoms, α > .80 for social anxiety, and α >.69 for separation anxiety) and was comparable to the internal consistency found in similar community samples of youth (e.g., March et al., 1997; Muris, Merckelbach, Ollendick, King, & Bogie, 2002; Ivarsson, 2006).
Data Analytic Plan
Analyses were conducted using Mplus (Muthen & Muthen, 2008). “Good fit” was defined as confirmatory fit index (CFI)≥.95 and standardized root mean square residual (SRMR)≤.08; “acceptable fit” was defined as CFI≥.90 (Hu & Bentler, 1999). Hu and Bentler (1999) recommend using a combination of two relative fit indices (e.g., CFI and SRMR). Given several statisticians’ recommendations to treat these values as guidelines, rather than as strict cutoffs, we prioritized the convergence across these two fit indices over reliance on any one particular measure of fit (Kenny, 2015; Barrett, 2007).
We modeled the prospective associations between physical panic symptoms, social anxiety, and separation anxiety with depression symptoms in an autoregressive cross-lagged path model over four time points: T1, T2, T3, and T4. T1 was the average of scores from participants’ 3, 6, and 9 month assessments; T2 was the average of scores from 12, 15, and 18 months; T3 was the average of 21, 24, and 27 months; T4 was the average of 30, 33, and 36 months. We created our composites from the average of 3 time points as it has been demonstrated that three or more assessments results in more reliable, sensitive longitudinal analyses (Little, 2013). Average scores improve the reliability of the estimate of each construct and account for outliers (Little, 2013). Baseline symptoms were excluded, as meta-analytic work has found the first administration of repeated measures self-report data, particularly the CDI, is elevated (Twenge & Nolen-Hoeksema, 2002). This approach allowed us to test cross-prediction from one syndrome domain to another across 4 time points, with equal assessments contributing to each time point in analyses, with equal spacing across time, and making use of all the data collected.
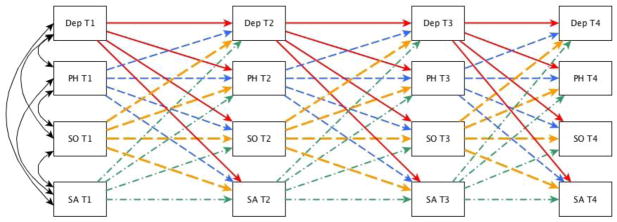
The general model (Figure 1) included correlations between CDI score and individual MASC subscale scores at each of the four time points, paths linking CDI score with subsequent MASC subscale scores, and MASC subscale scores with subsequent CDI scores and with each other. We allowed depressive symptoms to predict subsequent depressive symptoms, and each form of anxiety symptoms to predict itself at subsequent time points, to model the stability of depressive and anxious syndromes over time and enable prospective prediction of change in different internalizing syndromes (e.g., social anxiety to later depression). Therefore, the cross-lagged paths provide the incremental estimate of how much one internalizing syndrome (e.g., social anxiety) predicts future change in another internalizing syndrome (e.g., depression) after accounting for autoregressive stabilities and earlier influences of all forms of internalizing syndromes included in the model. Finally, we explored moderation of pathways in the general autoregressive cross-lagged model by age and gender. If a pathway was significant in the general model, an interaction term was added to that specific regression to examine whether that pathway was moderated by age/gender.
Figure 1.
Autoregressive cross-lagged path model. Note. All four symptom domains were allowed to correlate within time at all four time points; these paths are included in the figure at T1, but are omitted from the figure at T2, T3, and T4 for simplicity. DEP: depression; PH: physical symptoms; SO: social anxiety; SA: separation anxiety.
Data were missing completely at random across each of the four time points for the CDI, and across each of the four time points for the MASC subscales (Little’s MCAR test; CDI: χ2=31.96, df=27, p=0.23; physical symptoms: χ2=36.93, df=27, p=0.10; social anxiety: χ2=28.01, df=27, p=0.41; separation anxiety: χ2=16.77, df=27, p=0.94). Missing data were addressed using full information maximum likelihood (FIML) estimation (Graham & Schafer, 2002).
Results
Descriptive Statistics
The means and standard deviations of each anxiety syndrome and depressive symptoms, separated by gender, are reported in Table 1. Mean levels of physical symptoms, social anxiety, separation anxiety, and depression symptoms were within the range typically observed in community samples of youth of these ages. The pattern of gender differences in our sample was consistent with prior literature on symptom levels for girls and boys across development. Girls reported higher mean levels of depression symptoms than boys at each time point.
Table 1.
Means and standard deviations of symptoms of anxiety and depression by gender
| Total Sample | Boys | Girls | Gender Difference | ||||
|---|---|---|---|---|---|---|---|
| Variable | Mean | SD | Mean | SD | Mean | SD | t–value |
| T1 (n=524) | |||||||
| DEP | 4.79 | 4.14 | 4.42 | 3.66 | 5.08 | 4.48 | −1.87 |
| PH | 8.12 | 5.00 | 7.66 | 4.78 | 8.50 | 5.16 | −1.95 |
| SO | 8.89 | 4.75 | 8.06 | 7.72 | 9.57 | 4.67 | −3.68*** |
| SA | 7.03 | 4.03 | 6.39 | 3.81 | 7.55 | 4.14 | −3.36*** |
| T2 (n=510) | |||||||
| DEP | 4.28 | 4.02 | 3.92 | 3.80 | 4.56 | 4.16 | −1.83 |
| PH | 7.02 | 4.75 | 6.51 | 4.56 | 7.42 | 4.82 | −2.17* |
| SO | 7.91 | 4.75 | 6.85 | 4.29 | 8.743 | 4.94 | −4.59*** |
| SA | 6.30 | 3.84 | 5.70 | 3.47 | 6.76 | 4.05 | −3.17** |
| T3 (n=420) | |||||||
| DEP | 3.77 | 4.00 | 3.37 | 3.26 | 4.08 | 4.47 | −1.98* |
| PH | 6.94 | 5.08 | 6.20 | 4.51 | 7.49 | 5.41 | −2.62** |
| SO | 8.22 | 4.89 | 7.28 | 4.54 | 8.89 | 5.02 | −3.36*** |
| SA | 5.71 | 3.44 | 5.25 | 3.15 | 6.04 | 3.62 | −2.33* |
| T4 (n=433) | |||||||
| DEP | 4.15 | 4.26 | 3.54 | 3.33 | 4.61 | 4.79 | −2.74** |
| PH | 6.75 | 5.51 | 6.02 | 4.80 | 7.30 | 5.94 | −2.49* |
| SO | 7.92 | 5.22 | 6.83 | 4.82 | 8.73 | 5.38 | −3.86*** |
| SA | 5.04 | 3.55 | 4.27 | 3.18 | 5.61 | 3.70 | −4.05*** |
Note. Gender = male (1) or female (−1). DEP: depression; PH: physical symptoms; SO: social anxiety; SA: separation anxiety
Significant at the .05 level, 2-sided independent samples t-test;
Significant at the .01 level, 2-sided independent samples t-test;
Significant at the .001 level, 2-sided independent samples t-test.
Correlations within and across domains are reported in Table 2. Within time at T1, T2, T3, and T4, symptoms of depression were moderately to strongly correlated with physical and social anxiety symptoms. Symptoms of depression were weakly correlated with separation anxiety symptoms within time.
Table 2.
Intercorrelations among primary study variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.DEP_T1 | |||||||||||||||
| 2.PH_T1 | .58** | ||||||||||||||
| 3.SO_T1 | .48** | .55** | |||||||||||||
| 4.SA T1 | .12** | .43** | .44** | ||||||||||||
| 5.DEP_T2 | .71* | .46** | .45** | .05 | |||||||||||
| 6.PH_T2 | .43** | .76** | .50** | .35** | .53** | ||||||||||
| 7.SO_T2 | .45** | .45** | .77** | .31** | .55** | .54** | |||||||||
| 8.SA_T2 | .10* | .36** | .35** | .81** | .10* | .43** | .36** | ||||||||
| 9.DEP_T3 | .57** | .43** | .45** | .12* | .78* | .50** | .51** | .10* | |||||||
| 10.PH_T3 | .39** | .69** | .41** | .29** | .45** | .75** | .41** | .28** | .57** | ||||||
| 11.SO_T3 | .41** | .42** | .67** | .26** | .50** | .47** | .74** | .24** | .61** | .58** | |||||
| 12.SA_T3 | .11* | .29** | .27** | .73** | .08 | .32** | .24** | .78** | .13* | .35** | .27** | ||||
| 13.DEP_ T4 | .53** | .41** | .38** | .09 | .65** | .46** | .47** | .06 | .76** | .51** | .51** | .03 | |||
| 14.PH_T4 | .37** | .65** | .41** | .22** | .42** | .71** | .40** | .26** | .51** | .81** | .48** | .24** | .62** | ||
| 15.SO_T4 | .26** | .36** | .61** | .28** | .39** | .43** | .72** | .26** | .53** | .46** | .81** | .21** | .55** | .53** | |
| 16.SA_T4 | .02 | .27** | .29** | .67** | .06 | .31** | .23** | .76** | .13** | .25** | .23** | .79** | .13** | .35** | .362** |
Note. DEP: depression; PH: physical symptoms; SO: social anxiety; SA: separation anxiety
- Correlation is significant at the 0.01 level (2-tailed).
- Correlation is significant at the 0.05 level (2-tailed).
General autoregressive cross-lagged model results
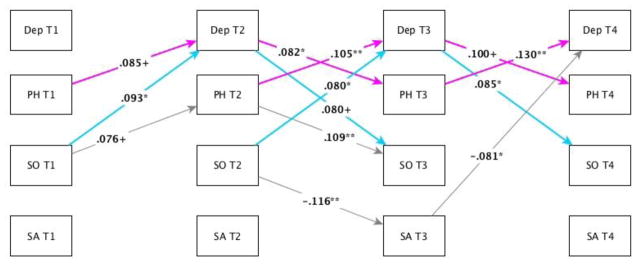
Figure 2 shows the model and main findings. Model fit was good by SRMR and acceptable by CFI (SRMR=.07, CFI=.93; χ2 = 475.65, df = 55, p<.001).
Figure 2.
Significant pathways in the autoregressive cross-lagged path model. Note. Autoregressive stability paths are not depicted in the figure for simplicity. All stability paths were significant, p<.05. * Significant at p<.05; ** Significant at p<.01; + Significant at trend level, p≤.08. DEP: depression; PH: physical symptoms; SO: social anxiety; SA: separation anxiety.
Physical panic and depression
Levels of physical symptoms of anxiety at T1 predicted variance in depression symptoms at T2 (β=.085, p=.055). Levels of depression at T2 predicted variance in physical symptoms at T3 (β=.082, p=.045). Physical symptoms at T3 predicted variance in depression symptoms at T4 (β=.130, p=.003). A reciprocal relationship comprising T2, T3, and T4 was also found from physical symptoms to depression beginning with physical symptoms at T2. Although depression symptoms at T1 did not predict physical symptoms T2 (β=−.027, p=.495), levels of physical symptoms at T2 predicted variance in depression at T3 (β=.105, p=.01), and levels of depression at T3 predicted variance in physical symptoms at T4 (β=.100, p=.08).
Social anxiety and depression
Levels of social anxiety symptoms at T1 predicted variance in depression symptoms at T2 (β=.093, p=.036). Levels of depression at T2 predicted variance in social anxiety symptoms at T3 (β=.080, p=.055). Additionally, social anxiety symptoms at T2 predicted variance in depression symptoms at T3 (β=.080, p=.04). Levels of depression at T3 also predicted variance in social anxiety symptoms at T4 (β=.085, p=.033).
Separation anxiety and depression
Levels of separation anxiety symptoms at T3 predicted variance in depression symptoms at T4 (β=.081, p=.03). Separation anxiety and depression were not prospectively associated at any other time points above and beyond the stability of either syndrome from one time point to the next, and the prospective contributions of other syndromes.
Moderation by age or gender
Age moderated the path from depression symptoms at T2 to physical symptoms at T3 (β=.465, p=.023). Gender moderated the relation of physical symptoms at T1 to depression at T2 (β=−.104, p=.033); this pathway was stronger for girls than for boys. Neither age nor gender moderated any other pathways.
Discussion
The temporal patterning of the development of co-occurring syndromes of anxiety and depression during childhood and adolescence has long been a topic of debate. The current study found physical panic symptoms and depression symptoms, as well as social anxiety and depression symptoms, longitudinally and reciprocally predicted each other over the three-year prospective follow-up, above and beyond the stability of either domain from one time point to the next. The results of the current study suggest that the development of syndromes of depression, physical and social anxiety during childhood and adolescence occurs in a predictable and systematic reciprocal pattern, rather than strictly sequentially and unidirectionally (i.e., anxiety syndromes precede depression). This is the first study, to our knowledge, to investigate temporal dynamics relating the unique contributions of multiple specific anxiety syndromes to the development of depression over time. That is, by entering depression and all three syndromes of anxiety in our model simultaneously and across all four time points, we were able to parse the degree to which each individual internalizing syndrome separately predicted unique variance in cross-domain symptom levels.
An extensive literature has examined anxiety-depression co-occurrence (e.g. Conway, Zinbarg, Mineka, & Craske, 2017; Hamilton et al., 2016; McLaughlin & King, 2015). While the preponderance of evidence indicates that most forms of anxiety precede depression (Kessler et al., 2005; Merikangas et al., 2010; Rohde et al., 1991; Cole et al., 1998), another body of research suggests that depression may precede anxiety (Moffitt et al., 2007; Pine et al., 1998; Merikangas et al., 2003) or that the two may develop in parallel (Cummings et al., 2014). The results of the current study suggest that the traditional view that anxiety precedes depression is an oversimplification of a more nuanced, dynamic process, and support a “multiple pathways” framework of anxiety-depression co-occurrence (Cummings et al., 2014). The present work can help to explain inconsistencies in the sequential comorbidity literature regarding the temporal precedence of anxiety relating to depression.
Our study benefits from the use of four time points assessed longitudinally over three years. Most previous work has used three time points to investigate the prospective associations of syndromes of anxiety with depression (e.g. McLaughlin & King, 2015; Avenevoli et al., 2001; Pine et al., 1998). However, with three time points or fewer, it is not clear whether an escalation from one symptom domain to another happened only once (e.g. social anxiety at T1 predicts depression at T2, without being able to see the opposite thread in the dynamic pattern), or whether the escalations were part of a larger pattern of mutually reinforcing escalations unfolding over time, as seen here. Such a pattern, as observed in the present investigation, is consistent with a cascade model conceptualization of anxiety-depression co-occurrence, whereby symptom change in one domain “spills over” into another domain, in a series of bidirectional associations over time (Masten et al., 2005; Cole & Maxwell, 2003).
The current study most directly builds upon work by McLaughlin & King (2015), who used an autoregressive cross-lagged panel model to examine trajectories of anxiety and depression co-occurrence over a 12-month period with three assessments. Their model provides important contributions to understanding anxiety-depression co-occurrence over time. However, their approach left particular questions unanswered, as separate models were created for each anxiety syndrome studied. Thus, as these separate models did not parse the covariance between anxiety syndromes, the relative contributions of each form of anxiety to depression symptoms are unclear. The present work, in contrast, simultaneously modeled physical, social, and separation anxiety with depression, and parsed the unique variance in depression symptoms prospectively predicted by each form of anxiety on its own. Such a distinction is crucial in identifying potential mechanisms via which these longitudinal bi-directional patterns develop and are maintained.
Separation anxiety symptoms were not predicted over time by depression, physical, or social anxiety symptoms. The only consistent predictor of separation anxiety symptoms at a given time point was separation anxiety at the previous time point. Separation anxiety has a younger median age of onset than panic disorder and social anxiety, and is less common in older adolescents (Kessler et al., 2005). In a younger sample of children, separation anxiety and depression may have predicted variance in each other over time. Separation anxiety and depression may also develop independently of one another over time across development via unique mechanisms. This provides additional evidence that lumping distinct forms of anxiety together obscures meaningful differences in the temporal sequencing of syndromes of depression and anxiety, as these patterns vary by symptom type.
The pattern of findings in the current study raises questions about potential mechanisms that may account for these relations. Peer and social mechanisms may help explain the reciprocal association between depression and social anxiety symptoms over time. Peer relationships become increasingly important and intimate during adolescence, and these relationships have a strong influence on depression and social anxiety symptoms during this time (Somerville, 2013). Individuals with higher levels of depression engage in behaviors that expose them to more interpersonal stressors, such as withdrawal from social relationships, excessive reassurance seeking, and irritability (Liu & Alloy, 2010; Hamilton et al., 2013; Hammen, 1991). Increased interpersonal stress may reinforce social anxiety symptoms, and anxiety-related behaviors (e.g. avoidance of social situations) may in turn lead to escalations in depression symptoms as individuals withdraw further from their social networks (Caldwell, Rudolph, Troop-Gordon, & Kim, 2004). Similar mechanisms may account for the relationship between physical anxiety and depression symptoms. Physical symptoms of anxiety are closely associated with panic disorder (van Gastel & Ferdinand, 2008; Wei, et al., 2014). Avoidance of situations associated with panic attacks is a key feature of panic disorder, particularly in panic disorder with agoraphobia (Craske, Sanderson, & Barlow, 1987). This avoidance may lead individuals to become isolated, which may lead to escalations in depression symptoms. Further empirical study is necessary to explore these possibilities.
Exploratory analyses to examine age and gender as moderators of these longitudinal reciprocal patterns suggested that results applied similarly to both girls and boys, as well as to youth of different ages, almost without exception. Mean level differences in syndromes of anxiety and depression are well-established between boys and girls and across development (Hankin & Abramson, 2001), which was reflected in this study. The lack of moderation by gender in our findings is consistent with prior work that did not find evidence for moderation of developmental trajectories of anxiety or depression (McLaughlin & King, 2015; Hamilton et al., 2016) or of cross-domain covariance (Conway et al., 2017) as a function of gender, suggesting that boys and girls follow the same trajectories of symptom development.
These findings have several clinical implications. First, this model is clinically useful for predicting risk for disorder. CDI scores predict the onset of depression (Mattison, Handford, Kales, Goodman, & McLaughlin, 1990), and MASC subscale scores predict their respective disorders (van Gastel & Ferdinand, 2008; Wei, et al., 2014). As amplifications within these domains predicted cross-domain escalations over time, this suggests increased susceptibility to eventual disorder. Second, the current model demonstrates the necessity of tracking symptom levels across domains. If clinicians limit their assessment to an individual diagnostic category, they may miss important sub-clinical cross-domain symptom changes. Finally, the developmental trajectories of anxiety and depression syndromes occur in systematic, predictable patterns of bi-directional effects over time. This supports a reconceptualization of assessments and interventions, which assume that for the majority of youth, anxiety simply precedes depression. For many children and adolescents, depression and anxiety may oscillate in symptom severity in predictable ways over the course of development. Clinicians can use this knowledge to more accurately and effectively conceptualize and treat anxiety and depression in youth.
The current study has several methodological strengths that help to further knowledge of the development of co-occurring syndromes of anxiety and depression in youth. Using a four time point prospective longitudinal design spanning three years provided a rigorous investigation of longitudinal patterns in symptom development. Furthermore, by controlling for the stability of each symptom domain over time in the autoregressive cross-lagged model, and entering all four syndromes into the model simultaneously at all time points, associations across symptom domains from one time point to the next are not due merely to the stability or intercorrelations of these syndromes over time. Finally, these results were found in a large, racially and ethnically representative community sample of girls and boys. Therefore, the results of this study likely generalize to other youth populations.
The strengths of this study must be considered in light of several limitations. Our analyses focused on self-reported anxiety and depression symptoms, rather than on diagnoses. Although the MASC and CDI have been shown to predict the development of disorder (van Gastel & Ferdinand, 2008; Wei, et al., 2014; Klein et al., 2005), additional research is needed to determine whether similar developmental patterns exist in syndromes of anxiety and depression at diagnostic levels. Research with a psychiatric sample would be necessary to establish whether these patterns also apply in more severe clinically symptomatic populations and whether these processes maintain levels of anxiety and depression once they reach diagnostic thresholds. Additionally, the current study is limited in its ability to generalize to forms of anxiety, like generalized anxiety, that are not assessed by the MASC. This represents an important avenue for future research.
The present study expands extant understanding of the development of co-occurring depression with different forms of anxiety in youth by demonstrating that symptom development of some internalizing syndromes occurs in mutually reinforcing, reciprocal patterns across time. Physical symptoms and depression predict each other over time, above and beyond the stability of either syndrome over time, for boys and girls across all ages. Similarly, symptoms of social anxiety and depression are also mutually predictive over time, above and beyond the expected stability, for all ages and genders. The current study also emphasizes the importance of distinguishing between heterogeneous forms of anxiety in the study of anxiety-depression co-occurrence, as separation anxiety and depression were not reciprocally associated over time. Taken together, these results suggest that, rather than framing the development of co-occurring syndromes of anxiety and depression as a question of “which came first”, it is more informative and accurate to conceptualize the co-development of these syndromes as occurring in a series of systematic, predictable bi-directional patterns over time.
Highlights.
A model describing the development of anxiety-depression co-occurrence is proposed.
Physical panic and depression symptoms reciprocally predicted each other over time.
Social anxiety and depression symptoms also predicted each other systematically.
Anxiety-depression co-occurrence does not develop strictly unidirectionally.
Results are clinically useful for predicting risk and tracking symptoms.
Acknowledgments
Role of the Funding Source
The research reported in this article was supported by grants from the National Institute of Mental Health to Benjamin L Hankin, R01MH077195, R01MH105501, R21MH102210, MH109662, and to Jami F. Young, MH077178.
Funding Source:
The research reported in this article was supported by grants from the National Institute of Mental Health to Benjamin L Hankin, R01MH077195, R01MH105501, R21MH102210, MH109662, and to Jami F. Young, MH077178.
The authors appreciate the thoughtful feedback provided by Tina Schweizer, Dustin Haraden, Fatema Jivanjee, Julianne Griffith, and Elissa Hamlat on earlier drafts of this manuscript.
Footnotes
As the present investigation uses the Multidimensional Anxiety Scale for Children (MASC; March, Parker, Sullivan, Stallings, & Conners, 1997) as our measure of anxiety, we do not examine associations between generalized anxiety and depression. This represents an important avenue for future work.
Contributors
Erin Long was primarily responsible for data analysis and manuscript preparation. Erin Long and Dr. Benjamin Hankin conceived of the ideas and primarily drafted the paper. Drs. Jami Young and Benjamin Hankin were the co-principal investigators on this study, and were responsible for data collection. They assisted with data analysis and provided feedback on drafts of the manuscript.
Conflict of Interest
The authors declare that they have no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40(1):57–87. [PubMed] [Google Scholar]
- Aune T, Stiles TC. The effects of depression and stressful life events on the development and maintenance of syndromal social anxiety: Sex and age differences. Journal of Clinical Child and Adolescent Psychology. 2009;38(4):501–512. doi: 10.1080/15374410902976304. [DOI] [PubMed] [Google Scholar]
- Avenevoli S, Stolar M, Li J, Dierker L, Merikangas K. Comorbidity of depression in children and adolescents: Models and evidence from a prospective high-risk family study. Biological Psychiatry. 2001;49:1071–1080. doi: 10.1016/s0006-3223(01)01142-8. [DOI] [PubMed] [Google Scholar]
- Axelson DA, Birmaher BB. Relation between anxiety and depressive disorders in childhood and adolescence. Depression and Anxiety. 2001;14(2):67–68. doi: 10.1002/da.1048. [DOI] [PubMed] [Google Scholar]
- Baldwin JS, Dadds MR. Reliability and validity of parent and child versions of the Multidimensional Anxiety Scale for Children in community samples. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(2):252–260. doi: 10.1097/01.chi.0000246065.93200.a1. [DOI] [PubMed] [Google Scholar]
- Barrett P. Structural equation modeling: Adjusting model fit. Personality and Individual Differences. 2007;42:815–824. [Google Scholar]
- Beesdo K, Bittner A, Pine DS, Stein BM, Höfler M, Lieb R, Wittchen H. Incidence of social anxiety disorder and the consistent risk for secondary depression in the first three decades of life. Arch Gen Psychiatry. 2007;64(8):903–912. doi: 10.1001/archpsyc.64.8.903. [DOI] [PubMed] [Google Scholar]
- Brady EU, Kendall PC. Comorbidity of anxiety and depression in children and adolescents. Psychological Bulletin. 1992;111(2):244–255. doi: 10.1037/0033-2909.111.2.244. [DOI] [PubMed] [Google Scholar]
- Burt KB, Obradovic J, Long JD, Masten AS. The interplay of social competence and psychopathology over 20 years: Testing transactional and cascade models. Child Development. 2008;79(2):359–374. doi: 10.1111/j.1467-8624.2007.01130.x. [DOI] [PubMed] [Google Scholar]
- Caldwell MS, Rudolph KD, Troop-Gordon W, Kim DY. Reciprocal influences among relational self-views, social disengagement, and peer stress during early adolescence. Child Development. 2004;75:1140–1154. doi: 10.1111/j.1467-8624.2004.00730.x. [DOI] [PubMed] [Google Scholar]
- Cole DA, Maxwell SE. Testing meditational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology. 2003;112(4):558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- Cole DA, Peeke L, Martin J, Truglio R, Seroczynski A. A longitudinal look at the relation between depression and anxiety in children and adolescents. Journal of Consulting and Clinical Psychology. 1998;66(3):451–460. doi: 10.1037//0022-006x.66.3.451. [DOI] [PubMed] [Google Scholar]
- Conway CC, Zinbarg RE, Mineka S, Craske MG. Core dimensions of anxiety and depression change independently during adolescence. Journal of Abnormal Psychology. 2017;126(2):160–172. doi: 10.1037/abn0000222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland WE, Angold A, Shanahan L, Costello EJ. Longitudinal patterns of anxiety from childhood to adulthood: The Great Smoky Mountains Study. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;53(1):21–33. doi: 10.1016/j.jaac.2013.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, Worthman CM. The Great Smoky Mountains Study of youth: Goals, designs, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry. 1996;53(12):1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60(8):837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Craske MG, Sanderson WC, Barlow DH. The relationships among panic, fear, and avoidance. Journal of Anxiety Disorders. 1987;1:153–160. [Google Scholar]
- Cummings CM, Caporino NE, Kendall PC. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychological Bulletin. 2014;140(3):816–845. doi: 10.1037/a0034733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epkins CC, Heckler DR. Integrating etiological models of social anxiety and depression in youth: Evidence for a cumulative interpersonal risk model. Clinical Child and Family Psychology Review. 2011;14(4):329–376. doi: 10.1007/s10567-011-0101-8. [DOI] [PubMed] [Google Scholar]
- Gerhardt CA, Compas BE, Connor JK, Achenbach TM. Association of a mixed anxiety-depression syndrome and symptoms of major depressive disorder during adolescence. Journal of Youth and Adolescence. 1999;28(3):305–323. [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7(2):147. [PubMed] [Google Scholar]
- Grills-Taquechel AE, Ollendick TH, Fisak B. Reexamination of the MASC factor structure and discriminant ability in a mixed clinical outpatient sample. Depression and Anxiety. 2007;25(11):942–950. doi: 10.1002/da.20401. [DOI] [PubMed] [Google Scholar]
- Hamilton JL, Potter CM, Olino TM, Abramson LY, Heimberg RG, Alloy LB. The temporal sequence of social anxiety and depressive symptoms following interpersonal stressors during adolescence. Journal of Abnormal Child Psychology. 2016;44:495–509. doi: 10.1007/s10802-015-0049-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton JL, Stange JP, Shapero BG, Connolly SL, Abramson LY, Alloy LB. Cognitive vulnerabilities as predictors of stress generation in early adolescence: Pathway to depressive symptoms. Journal of Abnormal Child Psychology. 2013;41:1027–1039. doi: 10.1007/s10802-013-9742-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100(4):555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY. Development of gender differences in depression: An elaborated cognitive vulnerability-transactional stress theory. Psychological Bulletin. 2001;127(6):773–796. doi: 10.1037/0033-2909.127.6.773. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998;107(1):128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Snyder HR, Gully LD, Schweizer TH, Bijtterbier P, … Vasey MW. Understanding comorbidity among internalizing problems: Integrating latent structural models of psychopathology and risk mechanisms. Development and Psychopathology. 2016;28:987–1012. doi: 10.1017/S0954579416000663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankin BL, Young JF, Abela JRZ, Smolen A, Jenness JL, … Oppenheimer CW. Depression from childhood into late adolescence: Influence of gender, development, genetic susceptibility, and peer stress. Journal of Abnormal Psychology. 2015;124(4):803–816. doi: 10.1037/abn0000089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn PJ, Wuyek LA. Anxiety disorders as a risk factor for subsequent depression. International Journal of Psychiatry in Clinical Practice. 2010;14:244–247. doi: 10.3109/13651501.2010.487979. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Ivarsson T. Normative data for the Multidimensional Anxiety Scale for Children (MASC) in Swedish adolescents. Nordic Journal of Psychiatry. 2006;60(2):107–113. doi: 10.1080/08039480600588067. [DOI] [PubMed] [Google Scholar]
- Johnson MR, Lydiard RB. Comorbidity of major depression and panic disorder. Journal of Clinical Psychology. 1998;54(2):201–210. doi: 10.1002/(sici)1097-4679(199802)54:2<201::aid-jclp9>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Keenan K, Feng X, Hipwell A, Klostermann S. Depression begets depression: Comparing the predictive utility of depression and anxiety symptoms to later depression. Journal of Child Psychology and Psychiatry. 2009;50(9):1167–1175. doi: 10.1111/j.1469-7610.2009.02080.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Hipwell A, Feng X, Babinski D, Hinze A, Rischall M, Henneberger A. Subthreshold symptoms of depression in preadolescent girls are stable and predictive of depressive disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47(12):1443–1442. doi: 10.1097/CHI.0b013e3181886eab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DA. Measuring model fit. 2015 Nov 24; Retrieved from davidakenny.net/cm/fit.htm.
- Kessler R, Berglund P, Demler O, Jin R, Koretz D, Merikangas K, … Wang P. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication. Journal of the American Medical Association. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62(60):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Stang PE, Wittchen H, Ustun TB, Roy-Burne PP, Walters EE. Lifetime panic-depression comorbidity in the National Comorbidity Survey. Arch Gen Psychiatry. 1998;55:801–808. doi: 10.1001/archpsyc.55.9.801. [DOI] [PubMed] [Google Scholar]
- Klein DN, Doughtery LR, Olino TM. Toward guidelines for evidence-based assessment of depression in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34(5):412–432. doi: 10.1207/s15374424jccp3403_3. [DOI] [PubMed] [Google Scholar]
- Kouros CD, Quasem S, Garber J. Dynamic temporal relations between anxious and depressive symptoms across adolescence. Development and psychopathology. 2013;25(03):683–697. doi: 10.1017/S0954579413000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory (CDI) Manual. Toronto: Multi Health Systems; 1992. [Google Scholar]
- Last C, Perrin S, Hersen M, Kazdin A. DSM-III-R anxiety disorders in kids: Sociodemographic and clinical characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:1070–1076. doi: 10.1097/00004583-199211000-00012. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Zinbarg R, Seeley JR, Lewinsohn M, Sack WH. Lifetime comorbidity among anxiety disorders and between anxiety disorders and other mental disorders in adolescents. Journal of Anxiety Disorders. 1997;11(4):377–394. doi: 10.1016/s0887-6185(97)00017-0. [DOI] [PubMed] [Google Scholar]
- Little PTD. Longitudinal structural equation modeling. New York: Guilford Press; 2013. [Google Scholar]
- Liu RT, Alloy LB. Stress generation in depression: A systematic review of the empirical literature and recommendations for future study. Clinical Psychology Review. 2010;30:582–593. doi: 10.1016/j.cpr.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- March JS, Parker JDA, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(4):554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- Masten AS, Cicchetti D. Developmental cascades. Development and Psychopathology. 2010;22(3):491–495. doi: 10.1017/S0954579410000222. [DOI] [PubMed] [Google Scholar]
- Masten AS, Roisman GL, Long JD, Burt KB, Obradovic J, … Tellgen A. Developmental cascades: Linking academic achievement and externalizing and internalizing symptoms over 20 years. Developmental Psychology. 2005;41(5):733–746. doi: 10.1037/0012-1649.41.5.733. [DOI] [PubMed] [Google Scholar]
- Mattison RE, Handford HA, Kales HC, Goodman AL, McLaughlin RE. Four-year predictive value of the Children’s Depression Inventory. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1990;2(2):169–174. [Google Scholar]
- McGee R, Feehan M, Williams S, Anderson J. DSM-III disorders from age 11 to age 15 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31(1):50–59. doi: 10.1097/00004583-199201000-00009. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, King K. Developmental trajectories of anxiety and depression in early adolescents. Journal of Abnormal Child Psychology. 2015;43(2):311–323. doi: 10.1007/s10802-014-9898-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swanson SA, Avenevoli S, Cui L, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication - Adolescent Supplement. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Zhang H, Avenevoli S, Acharyya S, Neuenschwander M, Angst J. Longitudinal trajectories of depression and anxiety in a prospective community study: The Zurich Cohort Study. Arch Gen Psychiatry. 2003;60(10):993–1000. doi: 10.1001/archpsyc.60.9.993. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Journal of Psychological Medicine. 2010;40(6):899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Harrington H, Caspi A, Kim-Cohne J, Goldberg D, Gregory AM, Poulton R. Depression and generalized anxiety: Cumulative and sequential comorbidity in a birth cohort followed prospectively to age 21 years. Arch Gen Psychiatry. 2007;64(6):651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- Muris P, Merckelbach H, Ollendick T, King N, Bogie N. Three traditional and three new childhood anxiety questionnaires: Their reliability and validity in a normal adolescent sample. Behaviour Research and Therapy. 2002;40(7):753–772. doi: 10.1016/s0005-7967(01)00056-0. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthen BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthen & Muthén; 2012. [Google Scholar]
- Osman A, Williams JE, Espenschade K, Gutierrez PM, Bailey JR, Chowdhry O. Further evidence of the reliability and validity of the Multidimensional Anxiety Scale for Children (MASC) in psychiatric inpatient samples. J Psychopathol Behav Assess. 2009;31:202–214. [Google Scholar]
- Pine DS, Cohen P, Gurley D, Brook J, Ma Y. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch Gen Psychiatry. 1998;55(1):56–64. doi: 10.1001/archpsyc.55.1.56. [DOI] [PubMed] [Google Scholar]
- Queen AH, Ehrenreich-May J. Anxiety-disordered adolescents with and without a comorbid depressive disorder: Variations in clinical presentation and emotion regulation. Journal of Emotional and Behavioral Disorders. 2014;22(3):160–170. [Google Scholar]
- Ranta K, Kaltiala-Heino R, Rantanen P, Marttunen M. Social phobia in Finnish general adolescent population: Prevalence, comorbidity, individual and family correlates, and service use. Depression and Anxiety. 2009;26:528–536. doi: 10.1002/da.20422. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn P, Seeley J. Comorbidity of unipolar depression: II. Comorbidity with other mental disorders in adolescents and adults. Journal of Abnormal Psychology. 1991;100(2):214–222. [PubMed] [Google Scholar]
- Snyder HR, Gulley LD, Bijttebier P, Hartman CA, Oldehinkel AJ, Mezulis A, Young JF, Hankin BL. Adolescent emotionality and effortful control: Core latent constructs and links to psychopathology and functioning. Journal of Personality and Social Psychology. 2015;109(6):1–18. doi: 10.1037/pspp0000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville LH. The teenage brain: Sensitivity to social evaluation. Current Directions in Psychological Science. 2013;22(2):121–127. doi: 10.1177/0963721413476512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge JM, Nolen-Hoeksema S. Age, gender, race, socioeconomic status, and birth cohort difference on the children's depression inventory: A meta-analysis. Journal of Abnormal Psychology. 2002;111(4):578–588. doi: 10.1037//0021-843x.111.4.578. [DOI] [PubMed] [Google Scholar]
- van Gastel W, Ferdinand RF. Screening capacity of the Multidimensional Anxiety Scale for Children (MASC) for DSM-IV anxiety disorders. Depression and Anxiety. 2008;25(12):1046–1052. doi: 10.1002/da.20452. [DOI] [PubMed] [Google Scholar]
- Weems CF, Costa NM. Developmental differences in the expression of childhood anxiety symptoms and fears. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44(7):656–663. doi: 10.1097/01.chi.0000162583.25829.4b. [DOI] [PubMed] [Google Scholar]
- Wei C, Hoff A, Villabø MA, Peterman J, Kendall PC, … March J. Assessing anxiety in youth with the multidimensional anxiety scale for children. Journal of Clinical Child and Adolescent Psychology. 2014;43(4):566–578. doi: 10.1080/15374416.2013.814541. [DOI] [PMC free article] [PubMed] [Google Scholar]