Abstract
Background
Expedited partner therapy (EPT) is an effective strategy for partner management of sexually transmitted infections. Some states, including Wisconsin, allow EPT prescriptions to be filled without a patient name. This study determined the refusal rates of nameless EPT prescriptions in Milwaukee pharmacies.
Methods
In this cross-sectional study, three trained research assistants of different age, gender and race posed as ‘patients’ and visited 50 pharmacy locations from one pharmacy chain in Milwaukee County, WI to fill nameless EPT prescriptions. A Chi-square test was used to compare demographics of patients, pharmacists, and pharmacies. Multiple logistic regression was used to identify factors associated with prescription refusal.
Results
29 (58%) of 50 nameless EPT prescriptions were refused. Univariate analysis showed prescriptions were more likely to be refused if the pharmacy was in the suburbs (77%) compared to Milwaukee city (43%), p=0.01, if the pharmacist was older than the patient (82%) compared to being younger (46%) or within the same age group (33%), p=0.01 for both, and if the patient was white (78%) compared to non-white (47%), p=0.03. Multivariable regression revealed significantly higher refusals for pharmacies located in suburbs compared to city (OR: 5.3; 95% CI: 1.4–20.3, p=0.03) and in patients who were white compared to non-white (OR: 4.8; 95% CI: 1.2–19.8, p=0.01).
Conclusion
Over half of nameless EPT prescriptions were refused in Milwaukee county pharmacies, more frequently at suburban pharmacies and for white patients. Increased pharmacist education regarding EPT is essential to help combat the sexually transmitted infection crisis.
Keywords: Expedited partner therapy, prescriptions, pharmacists, chlamydia, gonorrhea
Introduction
Sexual transmitted infections (STIs) are a significant healthcare crisis, with 20 million new STIs occurring in the United States each year.1 Chlamydia and gonorrhea, the two most commonly reported STIs, can progress to pelvic inflammatory disease potentially causing infertility and other lifelong health complications if left untreated. It is imperative to provide appropriate treatment to patients and their partners to prevent future health complications. Expedited partner therapy (EPT) is effective at preventing reinfection of chlamydia and gonorrhea.2 EPT allows providers to give their patients diagnosed with chlamydia or gonorrhea prescriptions or medications to give directly to their partner, thus the partner does not need to see a healthcare provider.2 It should be used if the partner is unlikely to seek care. EPT has been recommended by the Centers for Disease Control and Prevention (CDC) since 2006 because it reduces the risk of persistent or re-infection of chlamydia and gonorrhea compared to standard referral.2 It has also been endorsed by the American Academy of Pediatrics, the American Academy of Family Physicians, the American Congress of Obstetricians and Gynecologists, and the Society of Adolescent Health and Medicine.3–6
Despite recommendations for EPT by numerous medical organizations, as of publication, it is currently protected by law in only 41 states and specifically against the law in two.7 In the remaining seven states EPT is potentially allowable meaning there are no specific statutes addressing EPT or EPT is subject to additional policies.7 Additionally, laws governing allowable EPT prescribing practices vary by state. For example, in Wisconsin EPT has been legal since 2009 and laws allow EPT prescriptions to be ‘nameless’ if the patient does not know or will not disclose the partner’s name.8,9 The provider can simply write “expedited partner therapy” on the prescription.2
EPT is especially important in Wisconsin because the most recent available CDC data ranked Milwaukee first for rate of gonorrhea and fourth for chlamydia in the US.1 Milwaukee County has nearly 1 million residents and is highly segregated with the suburbs being predominately white and the city predominately non-white.10,11 Minorities in Milwaukee are disproportionally affected by STIs, with blacks having over 9 times the rate of chlamydia and 20 times the rate of gonorrhea compared to whites.12
The success of prescription EPT requires action on the part of the provider, patient, partner and pharmacist. While many studies demonstrate that providers lack knowledge of and underutilize EPT,13–15 there is little literature regarding pharmacist knowledge and use of EPT. A New York City survey conducted in 2012, and repeated in 2014, consistently showed less than half of pharmacists knew EPT was legal.16 There are no known studies accessing the pharmacist acceptance of EPT, defined by actual observation of whether pharmacists fill EPT prescriptions.
The objective of this study was to determine the percentage of nameless EPT prescriptions that Milwaukee County pharmacists refused to fill through ‘secret shopper’ interactions. Because of the racial segregation in Milwaukee County and racial disparities of STIs, our hypotheses were that nameless EPT prescriptions were more likely to be refused at pharmacies located in the suburbs compared to the city of Milwaukee and more likely to be refused if the patient was non-white.
Materials and Methods
This was a cross-sectional study conducted at one local pharmacy chain in Milwaukee County. All 50 pharmacies locations within the county were included. Three trained research assistants who varied in gender, age, and race posed as ‘patients’. Patient ‘A’ was a <30 year old white female, patient ‘B’ was a <30 year old non-white male, and patient ‘C’ was a >50 year old non-white female. Each pharmacy location was visited once by one patient with nameless prescriptions for azithromycin and cefixime, the recommended oral medications to treat chlamydia and gonorrhea. The encounters were semi-scripted. At each pharmacy, the patient asked to speak directly with a pharmacist. The patient then presented the nameless EPT prescription to the pharmacist and asked if it could be filled. If the pharmacist agreed to fill the prescription, the patient requested the prescription back insisting they changed their mind and wished to instead speak with their physician first, thus ending the encounter. If the pharmacist refused, the patient asked the reason for prescription refusal and offered solutions to troubleshoot. For example, if told the issue was insurance/cost, the patient offered to pay out of pocket. If the pharmacist told the patient they needed a name, the patient said their partner’s physician said a name would not be needed. After troubleshooting and offering solutions, a second attempt was made and the pharmacist either agreed to fill or continued to refuse the prescription (Figure 1). No medications were dispensed during the entirety of the study. Encounters occurred over six days in December 2016. This study was approved by the Medical College of Wisconsin’s IRB as a deception study requiring the approval of the pharmacy’s regional supervisor with assurance that no staff employment would be jeopardized should they not fill the prescriptions. After each site was visited, the IRB required a letter sent to each site manager notifying them of the study and allowing them a chance to have their site’s data withdrawn from the study.
Figure 1.
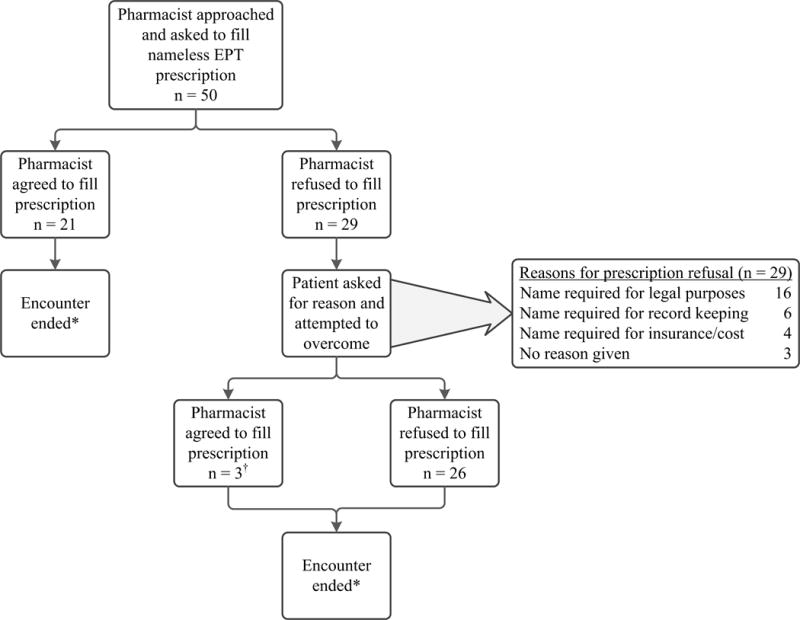
Flow diagram of the patient-pharmacist encounter.
*In total, after first and second attempt, 26 (52%) nameless EPT prescriptions were refused, while 24 (48%) were accepted.
†All three prescriptions came from the insurance/cost category after the patient offered to pay out of pocket.
After leaving the pharmacy, the patients immediately recorded the outcome of prescription refusal and refusal reason. Additional data collected included pharmacy location (categorized as Milwaukee city vs suburban), 24 hour pharmacy status, day of encounter (categorized as weekend vs weekday), time of encounter (categorized as morning, afternoon or evening), and perceived pharmacist characteristics including gender, age group (<30 years old, 30–50 years old, and >50 years), and race (white or non-white). We recorded whether the pharmacist refused to fill the prescription on the first and second requests. The primary outcome was refusal on the first request, and we analyzed characteristics associated with refusal on first request. We chose refusal on first request as the primary outcome because in real circumstances, patients may not ask why their prescription was refused, therefore, the encounter may not progress to allow a second chance for refusal. Chi-square test and Fisher’s Exact test were used to compare categorical variables, using an alpha of 0.05. Multiple logistic regression using stepwise selection and an alpha of 0.05 was used to identify factors associated with prescription refusal. Effects considered for inclusion in the model were: pharmacy location; 24-hour pharmacy status; day of encounter; perceived pharmacist gender, age and race; patient gender, age and race; and pharmacist-patient gender, age and race comparisons, along with two-way interactions. Statistical analysis was done using SAS V 9.2 (SAS, Cary, NC).
Results
Of the 50 encounters, 29 (58%) patients were initially refused and 21 (42%) were able to fill the prescription on the first attempt (Figure 1). No pharmacies opted to withdraw data. Reasons for refusal were categorized and are listed in Figure 1. After troubleshooting, only three additional prescriptions were accepted (all from the insurance/cost category), therefore 26 (52%) of EPT prescriptions were refused by pharmacists (Figure 1).
Perceived pharmacy and pharmacist characteristics are included in Table 1. Prescriptions were more likely to be refused if the pharmacy was located in the suburbs (77%) compared to the city of Milwaukee (43%), p=0.01. No pharmacist characteristics were associated with prescription refusal. Analysis of patient characteristics, also in Table 1, showed the prescription was more likely to be refused if the patient was white (78%) compared to non-white (47%), p=0.03. Comparisons between the pharmacist and patient are presented in Table 2. The prescription was more likely to be refused if the pharmacist was older than the patient (82%), compared to the pharmacist being younger than the patient (46%) or within the same age group (33%), p=0.01.
Table 1.
Characteristics of pharmacy, pharmacists and patients for all 50 encounters and percentage of refusals for each characteristic.
| Total N=50 n (%) |
Refused to fill on first request* | p-value# | |
|---|---|---|---|
| Pharmacy location | 0.01 | ||
| Milwaukee city | 28 (56) | 43% | |
| Suburban | 22 (44) | 77% | |
| 24 hour pharmacy | 0.49 | ||
| Yes | 11 (22) | 46% | |
| No | 39 (78) | 62% | |
| Day of encounter | 0.14 | ||
| Weekend | 9 (18) | 33% | |
| Weekday | 41 (82) | 63% | |
| Time of encounter | 0.30 | ||
| Morning | 21 (42) | 62% | |
| Afternoon | 3 (6) | 100% | |
| Evening | 26 (52) | 50% | |
| Perceived pharmacist gender | 0.20 | ||
| Male | 28 (56) | 50% | |
| Female | 22 (44) | 68% | |
| Perceived pharmacist age | 0.29 | ||
| <30 | 21 (42) | 48% | |
| 30–50 | 23 (46) | 61% | |
| >50 | 6 (12) | 83% | |
| Perceived white pharmacist | 0.72 | ||
| Yes | 37 (74) | 60% | |
| No | 13 (26) | 54% | |
| Patient gender | 0.39 | ||
| Male | 18 (36) | 50% | |
| Female | 32 (64) | 63% | |
| Patient age | 0.18 | ||
| <30 | 36 (72) | 64% | |
| >50 | 14 (28) | 43% | |
| Patient white | 0.03 | ||
| Yes | 18 (36) | 78% | |
| No | 32 (64) | 47% | |
Percentage calculated by the number of refusals divided by the number of encounters for that category.
Chi-square test used to compare proportions of refusal to fill on first request for each category.
Table 2.
Pharmacist and patient comparisons for all 50 encounters and percentage of refusals for each characteristic.
| Total N=50 n (%) |
Refused to fill on first request* | p-value# | |
|---|---|---|---|
| Gender Comparison | 0.89 | ||
| Different gender | 22 (44) | 59% | |
| Same gender | 25 (56) | 57% | |
| Age Comparison | 0.01 | ||
| Pharmacist older than patient | 22 (44) | 82% | |
| Pharmacist younger than patient | 13 (26) | 46% | |
| Same age group | 15 (30) | 33% | |
| Race Comparison** | 0.24 | ||
| Different race | 31 (62) | 52% | |
| Same race | 19 (38) | 68% | |
Percentage calculated by the number of refusals divided by the number of encounters for that category.
Chi-square test used to compare proportions of refusal to fill on first request for each category.
Race categorized as white and non-white.
In a multivariate analysis, prescriptions were more likely to be refused if the pharmacy was located in the suburbs compared to the city of Milwaukee (OR: 5.3; 95% CI: 1.4–20.3, p=0.03) and if the patient was white compared to non-white (OR: 4.8; 95% CI: 1.2–19.8, p=0.01). Not significant were 24 hour pharmacy status; day of encounter; perceived pharmacist gender, age and race; patient gender and age; and pharmacist-patient gender, age and race comparisons.
Discussion
This is the first known study that assesses the acceptance or refusal of nameless EPT prescription through in-person encounters. Although prescription and medication EPT is a legal practice in Wisconsin since 2009, in this study over half of the nameless EPT prescriptions were refused. The most common reason cited for refusal was a lack of name for legal purposes. Since in Wisconsin a name is not required for legal purposes and the law protects providers and pharmacists from liability, the need for improved knowledge about the specific name details of EPT was highlighted through this study. Even after our patients encouraged the pharmacists by stating the prescribing physician said a name was not required, no pharmacist sought to look up the EPT law or allowed the prescription to be filled. The only three prescriptions that were allowed after ‘troubleshooting’ were for insurance/cost reasons, still over half were refused.
In this study, no pharmacist characteristics were associated with EPT refusal, including perceived age group. This finding suggests that pharmacist understanding of EPT guidelines does not vary depending on when they received their training. We were not surprised by the increased refusal in suburban pharmacies. We hypothesized this because the rates of STIs are significantly higher in minorities and Milwaukee is one of the most segregated areas in the US, with most minorities residing in the city compared to the suburbs.1,17 Because STI rates are higher in the city, it is likely pharmacists located in Milwaukee have encountered EPT more frequently and would thus be more likely to fill the prescription. We had also hypothesized pharmacists would be more likely to refuse nameless prescriptions from non-white patients compared to white patients. This was based on many studies including a systemic review by Hall showing healthcare workers have an implicit bias of negative attitudes towards non-whites and positive attitudes towards whites.18–20 However, in our study the prescription was more likely to be refused when the patient was white. A possible explanation is higher expectations/standards for patients who are white, thus disapproval when EPT is requested.21 The etiology of the known racial disparities of STIs is multi-factorial and should be further investigated. Additional EPT education for pharmacists would increase overall awareness of EPT and ultimately the ability for patients to fill prescriptions.
This study has limitations. The patient always first asked to speak directly with a pharmacist. This was necessary to determine pharmacist understanding of EPT guidelines, but eliminated the initial interaction with the pharmacist technician who may have less knowledge of EPT. Therefore, it is plausible that our study resulted in a lower refusal rate than might be encountered by actual patients. Further studies would be needed to assess if further EPT training for pharmacist technicians would also be beneficial. Also, this study was limited to one pharmacy chain in one county. However, the pharmacy chain is among the largest in the county and is nationally available.
In conclusion, although a legal practice in Wisconsin, nameless EPT prescriptions are refused more than half the time at the pharmacy. While it is imperative that medical providers have increased knowledge and utilization of nameless EPT prescriptions, without increased acceptance of these prescriptions at pharmacies, nameless EPT will never be successful at reducing re-infection rates of chlamydia/gonorrhea in the real world. It is important to increase pharmacist awareness and educate about EPT to ultimately increase success of EPT.
Short Summary.
This was a ‘secret shopper’ study in which over half of nameless expedited partner therapy prescriptions were refused at local pharmacies.
Acknowledgments
We would like to acknowledge our pharmacy regional supervisor for his generous effort which allowed this study to be possible. To keep the integrity of this study, he must remain un-identified.
Funding Source: This study was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number 8UL1TR000055.
Footnotes
Financial disclosure: The authors have no financial relationships relevant to this article to disclosure.
Conflict of interest: The authors have no conflicts of interest to disclose.
References
- 1.Centers for Disease Control and Prevention. Sexually transmitted disease surveillance. Atlanta: U.S. Department of Health and Human Services; 2015. https://www.cdc.gov/std/stats15/default.htm. Updated 2016. Accessed March 29, 2017. [Google Scholar]
- 2.Centers for Disease Control and Prevention. Expedited partner therapy in the management of sexually transmitted diseases. Atlanta, GA: US Department of Health and Human Services; https://www.cdc.gov/std/treatment/eptfinalreport2006.pdf. Updated 2006. Accessed 2017, February 3. [Google Scholar]
- 3.American Academy of Pediatrics. Statement of endorsement—expedited partner therapy for adolescents diagnosed with chlamydia or gonorrhea. Pediatrics. 2009;124:1264. [Google Scholar]
- 4.American Academy of Family Physicians. AAFP policies. American Academy of Family Physicians; Web site. http://www.aafp.org/about/policies/all/partner-therapy.html. Updated 2012. Accessed July 28, 2015. [DOI] [PubMed] [Google Scholar]
- 5.American College of Obstetricians and Gynecologists. Expedited partner therapy in the management of gonorrhea and chlamydia. Committee opinion no. 632. Obstet Gynecol. 2015;125:1526–1528. doi: 10.1097/01.AOG.0000466366.67312.8c. [DOI] [PubMed] [Google Scholar]
- 6.Burstein GR, Eliscu A, Ford K, et al. Expedited partner therapy for adolescents diagnosed with chlamydia or gonorrhea: A position paper of the society for adolescent medicine. J Adolesc Health. 2009;45(3):303–309. doi: 10.1016/j.jadohealth.2009.05.010. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Legal status of expedited partner therapy. Atlanta: U.S. Department of Health and Human Services; http://www.cdc.gov/std/ept/legal/default.htm. Accessed February 5, 2013. [Google Scholar]
- 8.2009 Wisconsin Act 280.
- 9.Division of Public Health Wisconsin Department of Health Services. Expedited partner therapy for Chlamydia tachomatis infection, Neisseria gonorrhoeae infection and Trichomoniasis: Guidance for health care professionals in wisconsin. Wisconsin Department of Health Services Web site. https://www.dhs.wisconsin.gov/publications/p0/p00253.pdf. Updated 2013. Accessed July 28, 2015.
- 10.United States Census Bureau. Quick facts. https://www.census.gov/quickfacts/fact/table/milwaukeecountywisconsin,US/PST045216. Updated 2016. Accessed August 8, 2017.
- 11.Maternowski M. Measuring black/white segregation in metro Milwaukee. WUWM Milwaukee Public Radio: NPR News in Milwaukee Web site. http://wuwm.com/post/measuring-blackwhite-segregation-metro-milwaukee#stream/0. Updated 2017. Accessed August 8, 2017.
- 12.Division of Public Health Wisconsin Department of Health Services. Sexually transmitted disease in Wisconsin 2014. Wisconsin Department of Health Services Web site. https://www.dhs.wisconsin.gov/publications/p00415-2014-milw.pdf. Updated 2015. Accessed October 15, 2015.
- 13.Pickett ML, Melzer-Lange MD, Miller MK, Menon S, Visotcky AM, Drendel AL. Physician adherence to CDC guidelines for sexually active adolescents in the pediatric emergency setting. Pediatr Emerg Care. 2016 doi: 10.1097/PEC.0000000000000873. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hsii A, Hillard P, Yen S, Golden NH. Pediatric residents’ knowledge, use, and comfort with expedited partner therapy for STIs. Pediatrics. 2012;130(4):705–711. doi: 10.1542/peds.2011-3764. [DOI] [PubMed] [Google Scholar]
- 15.Rosenfeld E, Marx J, Terry M, et al. Perspectives on expedited partner therapy for chlamydia: A survey of health care providers. Int J STD AIDS. 2016;27(13):1180–1186. doi: 10.1177/0956462415610689. [DOI] [PubMed] [Google Scholar]
- 16.Reid A, Rogers ME, Arya V, Edelstein ZR, Schillinger JA. Pharmacists’ knowledge and practices surrounding expedited partner therapy for Chlamydia trachomatis, New York City, 2012 and 2014. Sex Transm Dis. 2016;43(11):679–684. doi: 10.1097/OLQ.0000000000000520. [DOI] [PubMed] [Google Scholar]
- 17.Social Science Data Analysis Network. Censusscope: Your portal to census data. http://www.censusscope.org/. Accessed January 29, 2017.
- 18.FitzGerald C, Hurst S. Implicit bias in healthcare professionals: A systematic review. BMC Medical Ethics. 2017;18(1):19. doi: 10.1186/s12910-017-0179-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maina IW, Belton TD, Ginzberg S, Singh A, Johnson TJ. A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Soc Sci Med. 2017 doi: 10.1016/j.socscimed.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 20.Hall WJ, Chapman MV, Lee KM, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: A systematic review. Am J Public Health. 2015;105(12):e60–e76. doi: 10.2105/AJPH.2015.302903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Biernat M, Kobrynowicz D. Gender-and race-based standards of competence: Lower minimum standards but higher ability standards for devalued groups. J Pers Soc Psychol. 1997;72(3):544. doi: 10.1037//0022-3514.72.3.544. [DOI] [PubMed] [Google Scholar]


