Abstract
We investigated the effects of varus-valgus alignment on the long-term outcomes after cementless total hip arthroplasty (THA) using a porous coated version of Bi-Metric® femoral stems. The Kaplan-Meier survival analysis was performed in 71 hips. The survival rate with femoral revision for aseptic loosening as the end point was 100% at 17 years. Nevertheless, the initial stem alignment was more valgus in patients with the Engh grade III–IV stress shielding than patients with the Engh grade I–II. Our results suggest that valgus misalignment of cementless Bi-Metric stem might be a potential risk factor for the progression of stress shielding.
Keywords: Cementless THA, Femoral stem, Survival rate, Stem alignment, Stress shielding
1. Introduction
Cementless total hip arthroplasty (THA) is becoming increasingly popular due to a marked improvement of femoral stem components in regard to material property, surface treatment (porous coating), and shape conformity to various types of medullary cavity morphology.1, 2, 3, 4 Bi-Metric® total hip system (Biomet, Inc., Warsaw, IN) has been clinically introduced since 1985 in US and 1987 in Japan, which consists of a femoral stem made of forged titanium alloy (Ti-6Al–4 V) with a plasma-sprayed porous coating on its proximal one-third portion.
Several authors reported promising short to mid-term outcomes of cementless Bi-Metric stems.5, 6, 7, 8 Nevertheless, there are a few reports concerning about stress shielding and bone resorption. One study performed by Robertsen et al.5 showed that calcar remodeling was present in 90% of the patients (88% atrophy and 2% hypertrophy) only at 2.9 year follow-ups after 50 primary THAs using collared type Bi-Metric stems. Meding et al.8 reported that patients experienced a severe stress shielding classified as the Engh grades III (prevalence rate, 53%) and IV (17%) at 10.4 year follow-ups after receiving collarless type Bi-Metric stems (105 hips).
The stem malpositioning is a potential risk factor for the progression of stress shielding, which is often associated with a distal press-fit of stems and a reduced load transfer at a proximal part of femur.9, 10 In this context, we hypothesized that varus-valgus positioning of cementless Bi-Metric stem (even in the small variation) has a significant adverse effect on the fixation stability. In the present study, we conducted the 12–17 year long-term follow-up of 71 cementless THAs using a porous-coated version of Bi-Metric stems at a single institution, and analyzed the effects of varus-valgus misalignment on the long-term clinical and radiological outcomes.
2. Methods
This retrospective study was approved by the Institutional Review Board (IRB) of our institute. Between March 1997 and July 2002, 95 primary THAs were performed in 89 patients with the use of a collarless, proximally porous-coated, cementless Bi-Metric® femoral stems (Biomet, Inc., Warsaw, IN) without hydroxyapatite coating. All the operations were performed by four surgeons (TS, TM, TT, KY) at a single center. 10 patients (10 hips) died during the study period due to causes unrelated to THA. 14 patients alive either had changed hospital (2 patients, 2 hips) or were lost to followup (12 patients, 12 hips). Thus, 65 patients (71 hips) were included for clinical and radiographic analyses (Table 1). Of these patients, there were 11 males and 54 females with underlying diseases, including osteoarthritis (63 hips), osteonecrosis of femoral heads (7 hips), and rheumatoid arthritis (1 hip). Their mean age and body mass index (BMI) at the time of surgery were 60 years (range, 33–83 years) and 24.9 kg/m2 (range, 17.5–39.0 kg/m2). The mean follow-up period was 14.0 years (range, 12–17 years).
Table 1.
Patient demographics.
| Variable | Value |
|---|---|
| Number of hips | 71 |
| Number of patients | 65 |
| Number of women | 54 |
| Initial diagnosis (number of hips) | |
| Osteoarthritis | 63 (89%) |
| Osteonecrosis | 7 (10%) |
| Rheumatoid arthritis | 1 (1%) |
| Age at surgery (years) | 60 (range, 33–83) |
| BMI (kg/m2) | 24.9 (range, 17.5–39.0) |
| JOA hip score | 48 (range, 22–72) |
| Follow-up period (years) | 14 (range, 12–17) |
BMI: body mass index; JOA: Japanese Orthopaedic Association.
All the patients received standard proximal profile (SPP) Bi-Metric stems with a 3° proximal-to-distal taper, 0° anteversion, and 135° stem-neck (CCD) angle, and Ti-6Al-4V plasma-sprayed porous coated cups with 4 fins on the rims (Mallory-Head®, Biomet, Inc.). The acetabular liners were 33-kGy γ-irradiated conventional ultra-high molecular weight polyethylene (PE) (ArCom®, Biomet, Inc.), which were captured by the cups with a Ring-Loc® mechanism (Biomet, Inc.). The counterfaces used were cobalt chrome alloy or monolithic zirconia (3Y-TZP) femoral heads with the diameter of 28 mm. A posterior approach without trochanteric osteotomy was adopted in all hips. Radiographs were taken before and immediately after THA, and the follow-up radiography was then performed weekly within one month. Subsequently, patients were evaluated at every 3 or 6 months at the first postoperative year, and at every 6 months or 1 year after the second year.
The preoperative and postoperative outcomes were assessed according to the Japanese Orthopaedic Association (JOA) score (100 points is the maximum score).11, 12 Stress shielding was classified as grade I–IV according to the criteria of Engh et al. [13]. The grade I–II and III–IV were regarded as mild and severe shielding in this study. Radiolucent lines at bone-implant interfaces were classified using three acetabular zones of DeLee and Charnley14 (zones I–III) and seven femoral zones of Gruen15 (zones 1–7). Distal cortical hypertrophy of bone on medial and lateral portion of femur was evaluated. The fixation and stability of the stems were assessed by the Engh’s scoring system (the maximum scores of fixation and stability are 10 and 17 points, respectively).16 The Kaplan-Meier analysis of the survival of the stem components was conducted in all hips. The stem failure was defined as aseptic loosening, and revision for any reason.
Radiological loosening was defined as 2 mm or more of radiolucency around the entire prosthesis17 or any migration of the implant.16 The total and annual linear wear18 of PE acetabular liners were assessed to correlate with aseptic loosening. Stem alignment was determined as the angle between the longitudinal axes of the femoral intramedullary canal and the femoral component stem on anteroposterior radiographs.19 Statistical analysis was performed with the Mann-Whitney U test to investigate the relationship between osteolysis and liner wear, as well as stress shielding and stem alignment. The analysis was conducted using software package SPSS (SPSS, version 17, Chicago, IL, USA). Statistical significance was set at a confidence level of P < 0.05.
3. Results
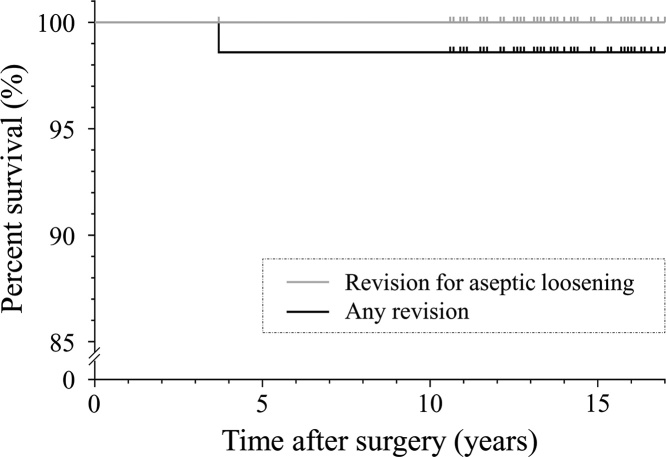
The mean JOA hip score improved from 48 points (range, 22–72 points; SD, 11) preoperatively to 93 points (range, 78–100 points; SD, 5) at final follow-up, and there were no patients remaining thigh pain after six months from the operation. The postoperative complications included: a late infection, and recurrent dislocation. One hip was revised as a result of periprosthetic infection. The Kaplan-Meier analysis with aseptic loosening of the stem as the end point showed 100% survival at 17 years (Fig. 1). On the other hand, the Kaplan-Meier analysis with revision of the stem for any reason (infection) as the end point showed 98.6% survival at 17 years (Fig. 1).
Fig. 1.
Kaplan-Meier survival curves for cementless Bi-Metric femoral components at a mean of 14 years.
The average cup inclination and anteversion were measured as 41° and 19.1° in the postoperative AP radiographs. The average total and annual linear wear of PE acetabular liners were assessed as 1.25 ± 0.75 mm and 0.090 ± 0.049 mm/year, respectively. Pelvic osteolytic lesions were noted in acetabular zones I–III, and these prevalences were 35, 30, and 9% of 69 hips (excluding one infected hip and one dislocated hip), respectively.
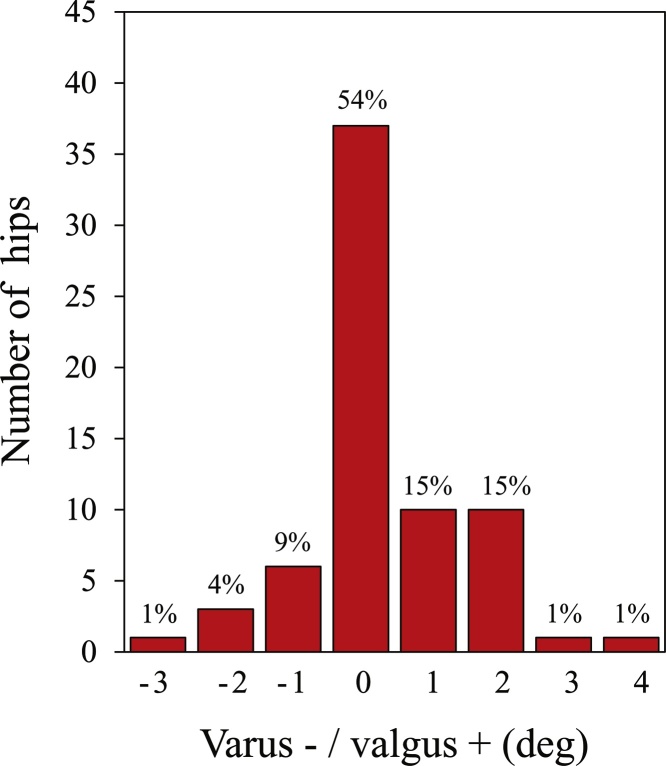
All stems were placed within ±4° from neutral alignment (Fig. 2). There were no measureable changes in varus-valgus positioning for any stems at any follow-up. The femoral stems were placed within ±1° from neutral alignment in 77% of 69 hips. The average Engh’s scores for stem fixation and stability were both favorable (9.6 points [range, 5–10 points, SD, 1] and 16.9 points [range, 14.5–17 points, SD, 1]), suggesting the successful bone ingrowth in all patients.
Fig. 2.
Relationship between number (percentage) of the hips and the initial stem alignment.
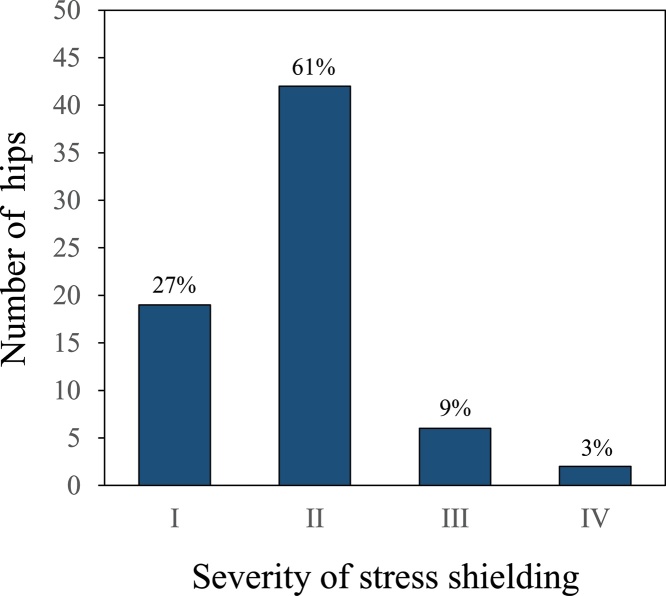
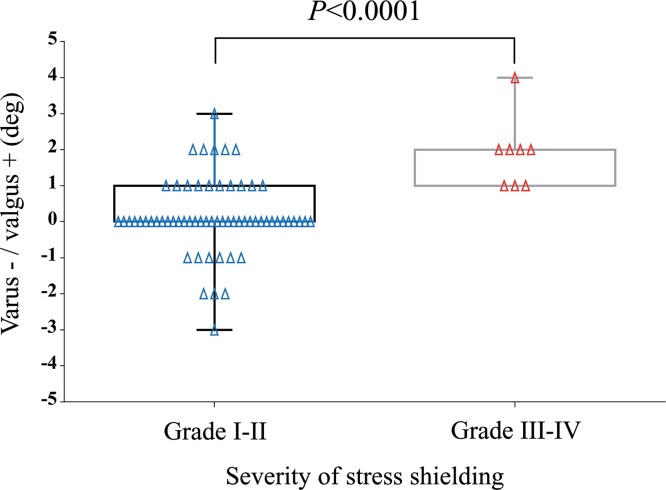
Stress shielding of the Engh grade I, II, III and IV was noted at 27, 61, 9, and 3%, respectively, and 88% of 69 hips (excluding one infected hip and one dislocated hip) were mild grade I–II (Fig. 3). A cortical hypertrophy was noted in 6 hips (9%). The initial stem alignment was more valgus in patients with the Engh grade III–IV stress shielding than patients with the Engh grade I–II (P < 0.0001). (Fig. 4). The femoral osteolysis was observed at the proximal zones (13, 7, 11% of 69 hips in zones 1, 6, 7), but no femoral components were revised for osteolysis.
Fig. 3.
Relationship between number (percentage) of the hips and the stress shielding grades defined by Engh et al. [13].
Fig. 4.
Relationship between the initial stem alignment and the stress shielding grades defined by Engh et al. [13].
4. Discussion
The small variation of varus-valgus misalignment did not compromise the long-term survivorship of a porous coated version of Bi-Metric stem. No femoral component had evidence of loosening, and the Kaplan-Meier analysis for aseptic loosening showed a 100% survival rate at 17 years (Fig. 1). Although osteolytic lesions were noted within the proximal femur (Gruen zones 1, 6, and 7), these were not reached to the distal area of the stem, suggesting the protective effect of the proximal porous coating on polyethylene wear debris migration.
Some other authors also reported excellent long-term survivals (96–100%) of Bi-Metric stems.20, 21 One study by Davies et al.20 showed the 100% survivorship for aseptic loosening at mean follow-up of 15.2 years after 64 primary THAs. Mäkelä et al.21 performed a follow-up study of 5379 patients from Finnish Arthroplasty Register, and reported the high survival for aseptic loosening of 99.0, 99.0, 96.0% at 7, 10, 15-years, respectively. Meding et al.22 showed the 100% survivorship for aseptic loosening at mean follow-up of 20 years after 157 primary THAs. Sueyoshi et al.23 also reported 100% survivorship with stem revision as the endpoint for more than 20 years (range, 0–26 years; mean, 7.9 years).
Nevertheless, we found that the small valgus misalignment significantly affected the severity of stress shielding (Fig. 4). Biomechanically, varus-valgus malalignment of femoral stems has been recognized to induce different load transmission patterns than in neutral alignment.24 In contrast to a clear statement of the adverse effect of malalignment on cemented stems,25, 26, 27 there were few reports on uncemented stems. Min et al.28 observed no adverse effects of varus-valgus position on clinical and radiological results of cementless THA using a tapered-wedge femoral stem (CLS, Zimmer) after a mean follow-up of 7.7 years (range, 5–11 years). Panisello et al.29 showed that malalignment did not affect clinical and radiological outcomes on an anatomic femoral stem (ABG II, Stryker) at 3 years follow-up. However, they observed that valgus stems had significantly more cortical atrophy in zone 7 than the neutral stems because of shifting of the load transmission to the lateral and distal medial cortical area. Khalily et al.19 reported on an Alloclassic prosthesis (Sulzer) with a press-fit tapered, dual-wedge design in which there were no problems related to varus malalignment at 5–11 years follow-up. In the present study, valgus malalignment affected the degree of stress shielding in Bi-Metric stem although there were no problems in clinical outcomes up to 17 years follow-up. In the above contexts, the significance of stem alignment and the related sensitivity to stress shielding can be dependent on component designs. Bi-Metric is often described as double-wedged taper (the proximal part has wedge-shaped profiles in the AP and lateral views),30 but its proximal AP width is relatively narrow and lateral profile is nearly straight. These features may be rather close to a tapered round stem.
On the acetabular side, the stable fixation was achieved by using the plasma-sprayed porous coated Mallory-Head cups, and none of our cases experienced any failure in the locking mechanism. However, result of PE wear was not satisfactory in this study (average total wear, 1.25 ± 0.75 mm) due to the implantation of conventional uncrosslinked PE liners (ArCom), although it was a comparable wear level to other publications.31, 32, 33 In more recent years (since 2007), as an alternative material to the conventional liners, vitamin-E diffused highly cross-linked PE liners (E1, Biomet, Warsaw, IN, USA) with the improved oxidation and wear resistance34 have been clinically available for the Mallory-Head cups. The use of E1 would contribute to further improved outcome of the total hip system used in this study.
This study had limitations. The unmatched numbers in the subjects between men and women were examined (11 males and 54 women), and the study involved their broad age ranges (33–83). In addition, an activity level, femoral morphology, and bone quality in the each patient were not evaluated. Despite the above limitations, our results suggest that valgus misalignment of the Bi-Metric stem design may be a potential risk factor for the progression of stress shielding although there were no problems in the long-term survivorship up to 17 years.
Conflict of interests
The authors have none to declare.
Funding
No funds have been received for this study.
Ethical approval
This study was performed in accordance with ethical standards of the institutional and/or national research committee and with 1964 Helsinki Declaration and its later amendments or comparable ethical standards. It was conducted after approval of the university ethical committee, and written approval statement was collected from all the included subjects before surgery.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Aldinger P.R., Breusch S.J., Lukoschek M., Mau H., Ewerbeck V., Thomsen M. A ten- to 15-year follow-up of the cementless spotorno stem. J Bone Jt Surg Br. 2003;85(2):209–214. doi: 10.1302/0301-620x.85b2.13216. [DOI] [PubMed] [Google Scholar]
- 2.Pospischill M., Knahr K. Cementless total hip arthroplasty using a threaded cup and a rectangular tapered stem. J Bone Jt Surg Br. 2005;87(2):1210–1215. doi: 10.1302/0301-620X.87B9.16107. [DOI] [PubMed] [Google Scholar]
- 3.Berend K.R., Lombardi A.V., Mallory T.H., Dodds K.L., Adams J.B. Cementless double-tapered total hip arthroplasty in patients 75 years of age and older. J Arthroplasty. 2004;19(3):288–295. doi: 10.1016/j.arth.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Pieringer H., Labek G., Auersperg V., Böhler N. Cementless total hip arthroplasty in patients older than 80 years of age. J Bone Jt Surg Br. 2003;85(5):641–645. [PubMed] [Google Scholar]
- 5.Robeltsen K., Gaarden M., Teichert G., Langhoff O. Results of the total bi-metric cementless hip adthroplasty. Orthopedics. 1996;19(8):673–674. doi: 10.3928/0147-7447-19960801-11. [DOI] [PubMed] [Google Scholar]
- 6.Lybäck C.C., Lybäck C.O., Kyrö A., Kautiainen H.J., Belt E.A. Survival of Bi-Metric femoral stems in 77 total hip arthroplasties for juvenile chronic arthritis. Int Orthop. 2004;28(6):357–361. doi: 10.1007/s00264-004-0584-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lazarinis S., Kärrholm J., Hailer N.P. Effects of hydroxyapatite coating on survival of a cementless femoral stem. Acta Orthop. 2011;82(4):399–404. doi: 10.3109/17453674.2011.597699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meding J.B., Keating E.M., Ritter M.A., Faris P.M., Berend M.E. Minimum ten-year follow-up of a straight-stemmed, plasma-sprayed, titanium-alloy, uncemented femoral component in primary total hip arthroplasty. J Bone Jt Surg Am. 2004;86(1):92–97. doi: 10.2106/00004623-200401000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Huiskes R. The various stress patterns of press-fit, ingrown, and cemented femoral stems. Clin Orthop Relat Res. 1990;261:27–38. [PubMed] [Google Scholar]
- 10.Otani T., Whiteside L.A. Failure of cementless fixation of the femoral component in total hip arthroplasty. Orthop Clin North America. 1992;23(2):335–346. [PubMed] [Google Scholar]
- 11.Imura S. The Japanese orthopaedic association: evaluation chart of hip joint fuctions. J Jpn Orthop Assoc. 1995;69:864–867. in Japanese. [Google Scholar]
- 12.Yamamoto K., Imakiire A., Shishido T. Cementless total hip arthroplasty using porous-coated Biomet acetabular cups (Hexloc and Ringloc types) J Orthop Sci. 2003;8(5):657–663. doi: 10.1007/s00776-003-0689-8. [DOI] [PubMed] [Google Scholar]
- 13.Engh C.A., Bobyn J.D., Glassman A.H. Porous-coated hip replacement. The factors governing bone ingrowth, stress shielding, and clinical results. J Bone Jt Surg Br. 1987;69(1):45–55. doi: 10.1302/0301-620X.69B1.3818732. [DOI] [PubMed] [Google Scholar]
- 14.DeLee J.G., Charnley J. Radiological demarcation of cemented ockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 15.Gruen T.A., McNeice G.M., Amstutz H.C. Modes of failure of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 16.Engh C.A., Massin P., Suthers K.E. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;257:107–128. [PubMed] [Google Scholar]
- 17.Clohisy J.C., Harris W.H. The Harris-Galante cementless femoral component in primary total hip replacement at 10 years. J Arthroplasty. 1999;14(8):915–917. doi: 10.1016/s0883-5403(99)90003-7. [DOI] [PubMed] [Google Scholar]
- 18.Livermore J., Ilstrup D., Morrey B. Effect of femoral head size on wear of the polyethylene acetabular component. J Bone Jt Surg Am. 1990;72(4):518–528. [PubMed] [Google Scholar]
- 19.Khalily C., Lester D.K. Results of a tapered cementless femoral stem implanted in varus. J Arthroplasty. 2002;17(4):463–466. doi: 10.1054/arth.2002.32171. [DOI] [PubMed] [Google Scholar]
- 20.Davies H., Ollivere B., Motha J., Porteous M., August A. Successful performance of the Bi-Metric cementless femoral stem at a minimum follow-up of 13 years in young patients. J Arthroplasty. 2010;25(2):186–190. doi: 10.1016/j.arth.2008.11.105. [DOI] [PubMed] [Google Scholar]
- 21.Mäkelä K.T., Eskelinen A., Paavolainen P., Pulkkinen P., Remes V. Cementless total hip arthroplasty for primary osteoarthritis in patients aged 55 years and older. Acta Orthop. 2010;81(1):42–52. doi: 10.3109/17453671003635900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meding J.B., Ritter M.A., Keating E.M., Berend M.E. Twenty-year followup of an uncemented stem in primary THA. Clin Orthop Relat Res. 2015;473(2):543–548. doi: 10.1007/s11999-014-3763-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sueyoshi T., Meding J.B., Berend M.E., Brunsman M.J., Ritter M.A. Short-term outcomes with a second-generation uncemented stem in total hip arthroplasty. Orthopedics. 2016;39(2):e215–8. doi: 10.3928/01477447-20160201-01. [DOI] [PubMed] [Google Scholar]
- 24.Mollan R.A.B., Watters P.H., Steele R., McClelland C.J. Failure of the femoral component in the Howse total hip arthroplasty. Clin Orthop Relat Res. 1984;190:142–147. [PubMed] [Google Scholar]
- 25.Munuera L., Garcia-Cimbrelo E. The femoral component in low-friction arthroplasty after ten years. Clin Orthop Relat Res. 1992;279:163–175. [PubMed] [Google Scholar]
- 26.Jaffe W.L., Hawkins C.A. Normalized and proportionalized cemented femoral stem survivorship at 15 years. J Arthroplasty. 1999;14(6):708–713. doi: 10.1016/s0883-5403(99)90226-7. [DOI] [PubMed] [Google Scholar]
- 27.Gill T.J., Sledge J.B., Orler R., Ganz R. Lateral insufficiency fractures of the femur caused by osteopenia and varus angulation: a complication of total hip arthroplasty. J Arthroplasty. 1999;14(8):982–987. doi: 10.1016/s0883-5403(99)90014-1. [DOI] [PubMed] [Google Scholar]
- 28.Min B.W., Song K.S., Bae K.C., Cho C.H., Kang C.H., Kim S.Y. The effect of stem alignment on results of total hip arthroplasty with a cementless tapered-wedge femoral component. J Arthroplasty. 2008;23(3):418–423. doi: 10.1016/j.arth.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 29.Panisello J.J., Herrero L., Herrera A., Canales V., Martinez A., Cuenca J. Bone remodelling after total hip arthroplasty using an uncemented anatomic femoral stem: a three-year prospective study using bone densitometry. J Orthop Surg. 2006;14(1):32–37. doi: 10.1177/230949900601400108. [DOI] [PubMed] [Google Scholar]
- 30.Khanuja H.S., Vakil J.J., Goddard M.S., Mont M.A. Cementless femoral fixation in total hip arthroplasty. J Bone Jt Surg Am. 2011;93(5):500–509. doi: 10.2106/JBJS.J.00774. [DOI] [PubMed] [Google Scholar]
- 31.Triclot P., Grosjean G., El Masri F., Courpied J.P., Hamadouche M. A comparison of the penetration rate of two polyethylene acetabular liners of different levels of crosslinking: a prospective randomised trial. J Bone Jt Surg Br. 2007;89:1439–1445. doi: 10.1302/0301-620X.89B11.19543. [DOI] [PubMed] [Google Scholar]
- 32.Geerdink C.H., Grimm B., Ramakrishnan R., Rondhuis J., Verburg A.J., Tonino A.J. Crosslinked polyethylene compared to conventional polyethylene in total hip replacement: pre-clinical evaluation, in-vitro testing and prospective clinical follow-up study. Acta Orthop. 2006;77(2):719–725. doi: 10.1080/17453670610012890. [DOI] [PubMed] [Google Scholar]
- 33.Calvert G.T., Devane P.A., Fielden J., Adams K., Horne J.G. A double-blind, prospective, randomized controlled trial comparing highly cross-linked and conventional polyethylene in primary total hip arthroplasty. J Arthroplasty. 2009;24:505–510. doi: 10.1016/j.arth.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 34.Yamamoto K., Tateiwa T., Takahashi Y. Vitamin E-stabilized highly crosslinked polyethylenes: the role and effectiveness in total hip arthroplasty. J Orthop Sci. 2017;22(3):384–390. doi: 10.1016/j.jos.2017.01.012. [DOI] [PubMed] [Google Scholar]