Abstract
Introduction
Coronal deformities are commonly encountered in paediatric orthopaedics and surgical treatment is indicated for severe deformities causing pain, function and cosmetic problems. In a growing bone, major surgical intervention like osteotomy with internal or external fixation can be avoided by growth modulation (hemiepiphysiodesis) using 8-plates. Our aim is to review the published literature on the use of 8-plates for deformity correction.
Methods
We conducted a systematic review on 8-plate growth modulation for coronal deformity correction. We carried out detailed literature search on PubMed, Google Scholar, EMBASE, and Cochrane databases. We analysed selected studies for patient demographics, rate of deformity correction, clinical outcome and complications.
Results
We identified seven studies using 8-plate for deformity correction involving 215 patients (350 Limbs). The mean age was 9.5 years (2–16 years M/F Ratio 1.1:1); underlying aetiology was Idiopathic in 33% and Pathological 67% cases. The deformities were successfully corrected in 196/215 patients (91.2%) and partial/no correction in 19/215 patients (8.8%). The mean time to correction was 15.3 Months (10.3–25) and follows up of 18.9 months (12.4–24). The deformity corrected at 1.28 °/month (0.93–1.53), lateral distal femoral angle changed at 0.87°/month (0.65–1.0) and medial proximal tibial angle changed at 0.72 (0.5–1). Complications were reported in 12/215 patients (5.6%) including hardware failure in 5, overcorrection/leg length difference in 5, infection 1 and stiffness 1. The rebound was reported in 8 patients (3.7%).
Conclusion
Growth modulation with 8-plates has high efficacy and low complications for deformity correction; and has been used widely across all paediatric age groups and aetiology. The literature is mostly retrospective and heterogeneous to develop age and aetiology specific recommendations.
Keywords: Genu varum, Genu valgum, Hemiepiphysiodesis, Growth modulation, Guided growth, 8- plate, Tension band plate, Deformity correction
1. Introduction
Coronal deformity is most commonly encountered in paediatric orthopaedic practice. The physiological deformities are treated conservatively, but severe deformities causing pain, function and cosmetic concerns, requires surgical intervention. In a growing bone, major surgical intervention with osteotomy and internal or external fixation can be avoided by growth modulation. Manipulation of growing bone by operative or non-operative method is old concept and widely used in paediatric orthopaedic practice for example in Pavlik harness treatment of DDH.1 Permanent hemiepiphysiodesis with open or percutaneous ablation of the physis for angular correction requires accuracy with timing and close follow up to avoid residual deformity or over-correction.
Temporary hemiepiphysiodesis with instrumentation is an attractive concept as allows for correction of deformity without above problems. There is ample evidence in literature to suggest that bone remodelling and growth can be modulated by mechanical forces.2 The physis works normally under optimum load conditions but lower and higher load leads to stimulation of growth at physis.3 The complex interactions of hormonal and mechanical forces across physis is not fully understood, therefore there are variable results reported to different methods of growth modulation.
The term “guided growth” was first described by Stevens when used a hardware construct with extraperiosteal plate and 2 screws.4 Stevens used this plate as tension band restraining the growth of the physis to overcome previous hardware problems of breakage with other constructs. This construct is commonly used for deformity correction by growth modulation of the physis without possibly causing permanent growth arrest. 8-plate appears to have superseded the options of using transphyseal screw or staple, due to its simplicity of construct, ease of application and rehabilitation.5 The evidence for safety and efficacy of implant is limited to retrospective studies and an experimental study.6 According to experimental study, there was statistically significant earlier effect on angle of correction and implant displacement was significantly lower when compared with Blounts staple.7
The obvious advantage of 8-plates is reversibility but duration for which these can be applied without losing reversibility remains unclear. There was also concern regarding surgical treatment of pathological physis and younger patients with guided growth due to problems with rebound or risk of permanent growth arrest. There is limited evidence on the use of growth modulation to correct deformities in these conditions.
We carried out a systematic review on growth modulation using 8-plate construct to evaluate demographics, clinical outcome, rate of correction, complication and rebound deformity in the literature. Our aim was to understand and develop the evidence base for the use of this construct. To the best of our knowledge, there is no systematic review in the published literature on this topic.
2. Material and methods
This systematic review was performed in line with PRISMA-P 2015 checklist.8 The Pubmed, Google Scholar, EMBASE, and Cochrane database was searched for all relevant articles against search criteria from 2006 to 2016. The keywords used for search are summarised in Table 1.
Table 1.
Keyword searches for identifying articles.
| Keyword and Boolean Searches | ||
|---|---|---|
| Coronal Deformity | AND | Paediatric |
| Hemiepiphysiodesis | AND | Eight plate |
| Hemiepiphyseodesis | AND | Children |
| Guided growth | AND | Coronal deformity |
| Growth Modulation | AND | Angular deformity |
| Genu Varum | AND | Deformity correction |
| Genu Valgum | AND | Deformity correction |
| Eight Plate | AND | Angular deformity |
| 8-Plate | AND | Deformity correction |
| Tension Band Plate | AND | Paediatric |
The author performed literature searches on electronic databases with above keywords and reviewed articles. The abstracts meeting the inclusion criteria were reviewed by both authors. The inclusion criterion was Randomised Controlled Trials; Prospective or retrospective case studies on the Coronal deformity correction by growth modulation using 8-plate. Growth modulation with other methods like percutaneous hemiepiphysiodesis; staple and transphyseal screw was excluded from the study. For studies comparing two different methods; only patient data using 8-plate was included in the analysis. The studies not published in English literature or with incomplete data were excluded from the study.
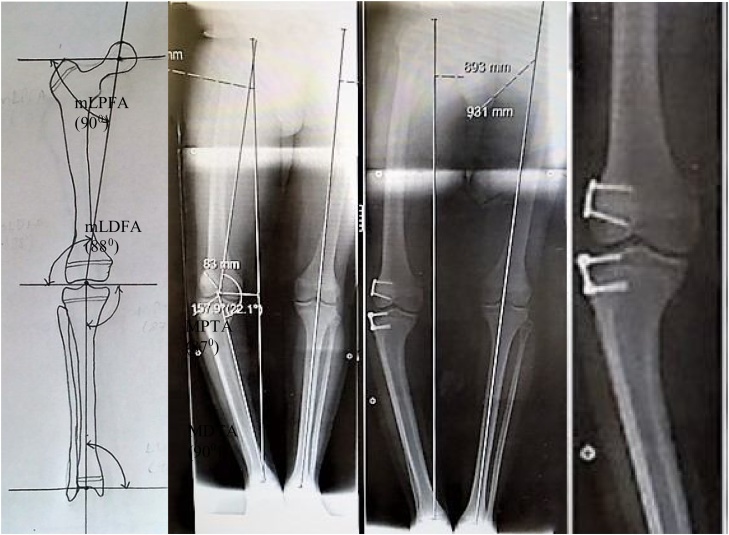
We collected patient data including number of patients and limbs operated, age, sex of patients, follow up duration. Rate and time taken for deformity correction was documented. We also recorded aetiology of coronal deformity, follow up duration, complications and rebound deformity following removal of plate. We recorded percentage of deformities corrected by this method and successfully avoided the need for osteotomy. The angles for measurement of deformity were as described by Paley et al. and shown in Fig. 1.9
Fig. 1.
A) Radiographical Angles, B) Preoperative and C, D) postoperative images of 8-plate.
Statistical Analysis: SPSS (IBM Statistical Package for the Social Sciences, Version 24) and differences with p-value <0.05 was considered statistically significant. Patient data was extracted from each article for analysis and summarised using Microsoft excel spreadsheet (Microsoft Corporation USA)
2.1. Surgical technique
Surgery was performed as day stay in most studies except one where patients were admitted for inpatient hospital stay. Surgical technique of application of 8- plate was described in publication by Stevens.4 It was recommended to place the plate just posterior to sagittal axis under fluoroscopic guidance to avoid risk of developing recurvatum. Two or three cm incision centred over physis to apply plate following meticulous surgical dissection in sub-muscular plane. Damage to periosteum and perichondrial ring should be carefully avoided. The placement of tension band plate should be confirmed under fluoroscopy. Postoperatively patient was mobilised full weight bearing and early return to full activities was recommended. Patient followed with serial radiographs to monitor progress with deformity correction. Screw and plate was removed once deformity was corrected and achieved neutral mechanical axis.
3. Observations and results
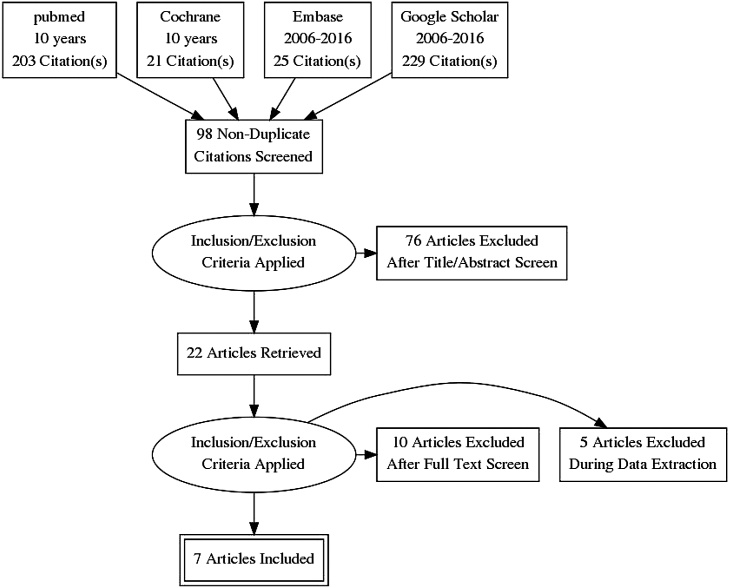
The preliminary searches of the literature with the above keywords identified articles as shown in PRISMA flow diagram. Articles were screened against inclusion and exclusion criteria as described in methods (Fig. 2).
Fig. 2.
PRISMA flow diagram.
We identified seven studies using 8-plate for deformity correction involving 215 patients (350 limbs). The mean age at the time of correction was 9.5 years (range 2–16 years), and male to female ratio approximately 1.1:1 (Male 114, Female 101). The underlying aetiology was documented in six studies (190 patients) as Idiopathic in 33% cases (62/190) and Pathological in 67% (128/190). The pathological conditions included skeletal dysplasia, pseudo-achondroplasia, hereditary osteodystrophy, Blount’s disease, rickets, post-traumatic sequalae, other congenital and acquired disorders. The demographic information is provided in Table 2.
Table 2.
Demographic information and aetiological diagnosis.
| References | year and study | No of pts | Limbs | Diagnosis | Patient age | Age Range (Yrs) | Ratio (M:F) | |
|---|---|---|---|---|---|---|---|---|
| 1 | Boero et al10 | Retrospective 2010 | 58 | 108 | Idio 30, Patho 28 | 10.83 | 2.25–14.9 | M30, F28 |
| 2 | Kulkarni et al11 | Case series 2015 | 24 | 40 | Idio 1, Patho 23 | 5.3 | 2–9.1 | M11, F13 |
| 3 | Ballal et al12 | Prospective 2009 | 25 | 37 | NA | 11.6 | 5.5–14.9 | M15, F10 |
| 4 | Burghardt et al13 | Case series 2010 | 43 | 51 | Idio 9, Patho 34 | 9.6 | 4–14.2 | M24, F19 |
| 5 | Jelinek et al14 | Retrospective 2011 | 17 | 33 | Idio 12, Patho 5 | 11.6 | 2.9–16 | M8, F9 |
| 6 | Kumar et al15 | Prospective 2016 | 19 | 31 | IdIo 10, Patho 9 | 7.8 | 4–12 | M8, F11 |
| 7 | Yilmaz et al16 | case series 2014 | 29 | 50 | patho 29 | 10 | 4–15.4 | M18, F11 |
| 215 | 350 | 9.5 | 2–16 |
3.1. Data analysis
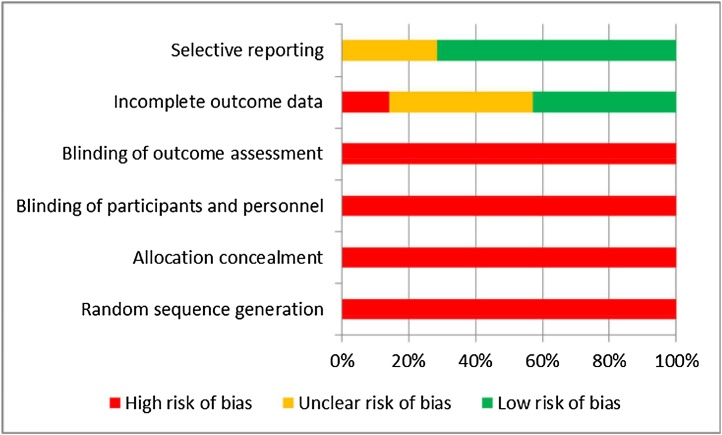
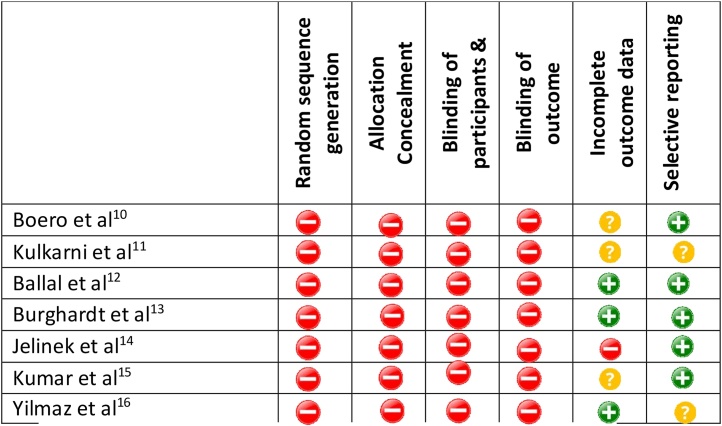
Author’s assessment of risk of bias is given in Fig. 3, Fig. 4. There were two prospective studies, two retrospective studies and three case series. There is high risk of selection and performance bias in retrospective studies. There was no randomisation of patient selection in all studies involved in this review.
Fig. 3.
Cochrane risk of bias graph.17
Fig. 4.
Summary of author’s assessment on risk of bias.
3.2. Clinical outcome
The mean time to correction was 15.3 Months (10.3–25) and follows up duration 18.9 months (12.4–24). The rate of deformity correction was 1.28 °/month (0.93–1.53), lateral distal femoral angle changed at 0.87°/month (0.65–1.3) and medial proximal tibial angle changed at 0.72 (0.5–1). Further details are provided in Table 3.
Table 3.
Mean time to correction and rate of correction of deformity, mLDFA (mechanical distal femoral angle) and mMPTA (mechanical Medial Proximal Tibial Angle).
| S No | References | year of study | Mean time correction mths | Follow up post correction mths | Combined (Deg/mth) |
|
|---|---|---|---|---|---|---|
| mLDFA deg/mth | mMPTA deg/mth | |||||
| 1 | Boero et al10 | 2010 | 14 | 21 | 0.93 | |
| 2 | Kulkarni et al11 | 2015 | 15.6 | 21 | 1.53 | |
| 3 | Ballal et al12 | 2009 | 16.1 | 12.4 | 0.7 | 0.5 |
| 4 | Burghardt et al13 | 2010 | 14.2 | 16 | 0.65 | 0.58 |
| 5 | Jelinek et al14 | 2011 | 11.9 | NA | 1 | 1 |
| 6 | Kumar et al15 | 2016 | 10.3 | 24 | 1.3 | 0.8 |
| 7 | Yilmaz et al16 | 2014 | 25 | NA | 0.72 | – |
| Mean | 15.3 | 18.9 | 0.87 | 0.72 | ||
The deformities were successfully corrected in 91.2% (196/215) cases and partial/no correction in 8.8% (19/215). Table 4 has information on the number of cases.
Table 4.
Clinical outcome of cases in each publication.
| S No | References | Full correction | Partial Correction | No correction | Total | complications | Rebound |
|---|---|---|---|---|---|---|---|
| 1 | Boero et al10 | 52 | 5 | 1 | 58 | 0 | 2 |
| 2 | Kulkarni et al11 | 22 | 2 | 0 | 24 | 3 | 2 |
| 3 | Ballal et al12 | 24 | 1 | 0 | 25 | 2 | 1 |
| 4 | Burghardt et al13 | 39 | 0 | 4 | 43 | 1 | 2 |
| 5 | Jelinek et al14 | 17 | 0 | 0 | 17 | 3 | 0 |
| 6 | Kumar et al15 | 17 | 2 | 0 | 19 | 2 | 0 |
| 7 | Yilmaz et al16 | 25 | 0 | 4 | 29 | 1 | 1 |
| 196 | 10 | 9 | 215 | 12 | 8 |
3.3. Complications
Complications were reported in 12/215 cases treated (5.6%) including hardware problems in 5, overcorrection or leg length difference 5, infection 1 and stiffness in 1. The rebound of deformity was reported in 8/215 cases (3.7%).
4. Discussion
Coronal deformities are commonly presented in children and growth modulation using 8-plate to correct deformity is an attractive concept in skeletally immature patients. This has rapidly gained popularity, but evidence available in literature is limited and many questions remain unanswered. The evidence is based on mostly retrospective studies and an experimental study. The experimental study has shown that 8-plate is more effective than Blount staples for deformity correction by guided growth after temporary hemiepiphysiodesis.6,7 Our main aim for this systematic review was to evaluate published literature on growth modulation using 8-plate hemiepiphysiodesis for coronal deformity correction, with regards to age, aetiology, time to correction, clinical outcome and complications.
Stevens first described the procedure and shown to have prevented 97% osteotomies with this procedure in his prospective study on 34 patients.4 He used plate widely across paediatric age groups and aetiology, but shown rebound of deformity in four patients (8 femora) younger than 11 years with idiopathic genu valgum. There was no permanent or premature physeal closure or limb length discrepancy identified, but longer follow up needed. One randomised controlled trial and two retrospective comparative studies compared 8-plate with Blounts staple and shown to be at least as effective as staple. Retrospective study has shown shorter implantation time of 8-plate, otherwise comparable results with respect to treatment time, rate of correction and complications.14 Higher complications were observed with pathological physis and unacceptable failure rate (44%) in patients with Blount disease was observed by Schroerlucke et al.18
Boero et al. compared idiopathic versus dysplasia/syndrome group and recommended early intervention in osteochondral dysplasia/syndrome group as correction time is longer.10 Other authors have also used the plate in younger patients (Age <10) and pathological physis and shown to be effective in deformity correction and low risk of physeal damage.16 There is tendency towards faster correction in young patients and two plates when compared with one plate.
4.1 Limitations
This systematic review has limitations because of type and nature of studies included in the review. There were two prospective studies and most other publications were retrospective on relatively small number of patients from single unit. These studies do not have control group, any blinding and randomisation, and therefore as such are prone to allocation, selection and randomisation bias. The patients, surgeons and personnel collecting data were aware about the operative intervention, resulting in performance and detection bias. We analysed these studies for completeness of patient information on rate and time of deformity correction, clinical outcome and complications.
There was heterogeneity with regards to measurement of radiographic angles and other parameters of deformity correction across all studies. The age group and aetiology also differed across these studies, making it difficult to isolate results of surgical intervention. There were inconsistencies in reporting of rebound deformity following correction or further surgery and reported in five out of seven studies included in the review. Only one study reported radiographic follow up of 10 patients for 16 months following plate removal for monitoring recurrence of deformity and shown rebound of 1.0 mm/month indicating reversibility. There was variability in the level of data reporting of radiological parameters, making it impossible to perform descriptive statistics.
5 Conclusion
Growth modulation with 8-plates has high efficacy and low complication rate for deformity correction and avoiding the need for osteotomy. This systematic review shows that 8-plates have been used widely across all paediatric age groups and aetiology. The methodological quality of studies was low and limited available evidence to develop aetiology and age specific recommendations. There is need for high quality multi-centre study with longer follow up on large number of patients.
Conflict of interest
The authors have none to declare.
Funding information
The authors have no funding source.
References
- 1.Pavlik A. The functional method of treatment using a harness with stirrups as the primary method of conservative therapy for infants with congenital dislocation of the hip. 1957. Clin Orthop Relat Res. 1992;281:4–10. [PubMed] [Google Scholar]
- 2.Ganley T.J., Spiegel D.A., Gregg J.R., Flynn J.M. Overuse injuries to the physes in young athletes: a clinical and basic science review. UPOJ. 1998;11(Spring):27–35. [Google Scholar]
- 3.Frost H.M. A chondral modeling theory. Calcif Tissue Int. 1979;28:181–200. doi: 10.1007/BF02441236. [DOI] [PubMed] [Google Scholar]
- 4.Stevens P.M. Guided growth for angular correction: a preliminary series using a tension band plate. J Pediatr Orthop. 2007;27/3(April/May):253–259. doi: 10.1097/BPO.0b013e31803433a1. [DOI] [PubMed] [Google Scholar]
- 5.Gottliebsen M., Shiguetomi-Medina J.M., Rahbek O., Møller-Madsen B. Guided growth: mechanism and reversibility of modulation. J Child Orthop. 2016;10:471–477. doi: 10.1007/s11832-016-0778-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanellopoulos A.D., Mavrogenis A.F., Dovris D. Temporary hemiepiphysiodesis with blount staples and eight-plates in pigs. Orthopedics. 2011;34(April (4)) doi: 10.3928/01477447-20110228-05. [DOI] [PubMed] [Google Scholar]
- 7.Blount W.P., Clarke G.R. Control of bone growth by epiphyseal stapling; a preliminary report. J Bone Joint Surg Am. 1949;31A(3):464–478. [PubMed] [Google Scholar]
- 8.Moher D., Shamseer L., Clarke M. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paley D., Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of multiapical frontal plane angular and bowing deformities of the femur and tibia. Clin Orthop Relat Res. 1992;(280):65–71. [PubMed] [Google Scholar]
- 10.Boero S., Michelis M.B., Riganti S. Use of the eight-plate for angular correction of knee deformities due to idiopathic and pathologic physis: initiating treatment according to etiology. J Child Orthop. 2011;5:209–216. doi: 10.1007/s11832-011-0344-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kulkarni R.M., Rushnaiwala F.M.I., Kulkarni G.S., Negandhi R., Kulkarni M.G., Kulkarni S.G. Correction of coronal plane deformities around the knee using a tension band plate in children younger than 10 years. Indian J Orthop. 2015;49(March–April (2)):208–218. doi: 10.4103/0019-5413.152484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ballal M.S., Bruce C.E., Nayagam S. Correcting genu varum and genu valgum in children by guided growth. J Bone Joint Surg [Br] 2010;92-B:273–276. doi: 10.1302/0301-620X.92B2.22937. [DOI] [PubMed] [Google Scholar]
- 13.Burghardt R.D., Herzenberg J.E. Temporary hemiepiphysiodesis with the eight-Plate for angular deformities: mid-term results. J Orthop Sci. 2010;15:699–704. doi: 10.1007/s00776-010-1514-9. [DOI] [PubMed] [Google Scholar]
- 14.Jelinek E.M., Bittersohl B., Martiny F., Scharfstädt A., Krauspe R., Westhoff B. The 8-plate versus physeal stapling for temporary hemiepiphyseodesis correcting genu valgum and genu varum: a retrospective analysis of thirty five patients. Int Orthop (SICOT) 2012;36:599–605. doi: 10.1007/s00264-011-1369-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kumar A., Gaba S., Sud A., Mandlecha P., Goel L., Nayak M. Comparative study between staples and eight plate in the management of coronal plane deformities of the knee in skeletally immature children. J Child Orthop. 2016;10:429–437. doi: 10.1007/s11832-016-0758-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yilmaz G., Oto M., Thabet A. Correction of lower extremity angular deformities in skeletal dysplasia with hemiepiphysiodesis: a preliminary report. J Pediatr Orthop. 2014;34:336–345. doi: 10.1097/BPO.0000000000000089. [DOI] [PubMed] [Google Scholar]
- 17.Higgins J.P.T., Altman D.G., Gøtzsche P.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schroerlucke S., Bertrand S., Clapp J., Bundy J., Gregg F.O. Failure of Orthofix eight-plate for the treatment of Blount Disease. J Pediatr Orthop. 2009;29:57–60. doi: 10.1097/BPO.0b013e3181919b54. [DOI] [PubMed] [Google Scholar]