Abstract
Introduction
With the increasing rates of total hip replacements being performed worldwide, there is an increasing incidence of periprosthetic fractures. As our patients’ demographics change to include older patients with multiple medical co-morbidities, there is a concurrent increase in morbidity and mortality rates. This leads to longer hospital stays and increasing hospital costs. In the current economic climate, the cost of treating periprosthetic fractures must be addressed and appropriate resource and funding allocation for future provision of services should be planned.
Materials and methods
All periprosthetic hip fractures that were admitted to a single trauma unit over a three-year period were reviewed. Independent chart review, haematological and radiological review was undertaken. All patients with a periprosthetic fracture associated with a total hip arthroplasty or hemiarthroplasty were included. Follow up data including complications were collated. Data from the hospital inpatient database and finance department was utilized for cost analysis. All statistical analysis was preformed using Minitab version 17.
Results
48 patients were identified who met the inclusion criteria for review. The majority of participants were female with a mean age of 73.5 years. The mean time to fracture was 4.5 years (9 months–18.5 years). Periprosthetic fracture was associated with total hip arthroplasty in 24 cases and a Vancouver B2 classification was most common at n = 20. The majority of patients had revision arthroplasty, with a mean length of stay of 24 days for the whole cohort (9–42). Vancouver B3 fractures had the longest inpatient stay at a mean of 26 days. The mean cost of for a full revision of stem with additional plate and cable fixation was over €27000 compared to €14,600 for ORIF and cable fixation based on length of hospital stay.
Conclusion
The prolonged length of stay associated with Vancouver B2 and B3 fractures leads to increased costs to the healthcare service. Accurately calculating the costs of total treatment for periprosthetic fractures is difficult due to a lack of transparency around implant and staffing costs. However, as we can expect increasing incidence of periprosthetic fractures presenting in the coming years it is paramount that we make financial provisions within healthcare budgets to ensure we can treat these patients appropriately.
Keywords: Periprosthetic fracture, Cost, Length of stay
1. Introduction
The national joint registries worldwide put the incidence of periprosthetic hip fractures at 25.3 per 1000 total hip replacements preformed.1 The incidence of periprosthetic hip fractures has been predicted to be up to 21% by 2020 in a paper by Frenzel et al.2 Not only are the numbers of people undergoing primary hip arthroplasty increasing, but the patient demographic is also changed. Now increasing body mass index, patient age and post-operative activity demands are all different. With these changes, patients and clinicians all have high expectations for clinical outcomes. However, as BMI increases and younger patients have higher activity levels, periprosthetic fractures can be expected at all our institutions.3 Due to the complex reconstruction and revision arthroplasty procedures needed to deal with periprosthetic fractures, these patients can often have lengthy and ultimately costly stays in hospital. No literature from the Republic of Ireland to date has looked at the costs of periprosthetic hip fractures in our current economic climate.
2. Patients and methods
In order to assess the economic impact of periprosthetic hip fractures a review of the current literature was undertaken. Analysis of the cost to the health service in one major trauma unit over a three-year period for all patients treated for periprosthetic fractures was also undertaken. As the Vancouver classification is widely used for stratification of periprosthetic fractures, we used this as method to assess the difference in hospital stay between groups.
Between 2013 and 2015, all patients who presented with a periprosthetic fracture surrounding a hip prosthesis were reviewed. All patients treated operatively were included in the analysis. A retrospective review of all patients who underwent either open reduction internal fixation or revision hip arthroplasty were included for analysis. Total hip arthroplasty and hemiarthroplasty cases were collated. The hospital notes were reviewed and all data collected using a standardised proforma to ensure accurate collection of information for analysis. Collection of all data including all haematological and radiological investigations. The hospital length of stay was collated to facilitate analysing the cost. All patients were classified on presentation as per the Vancouver classification of periprosthetic hip fractures. If required the Vancouver classification was modified based on intra-operative findings.
3. Results
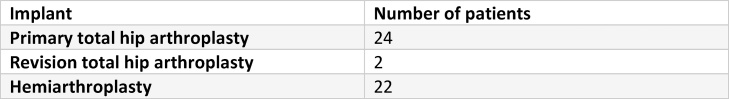
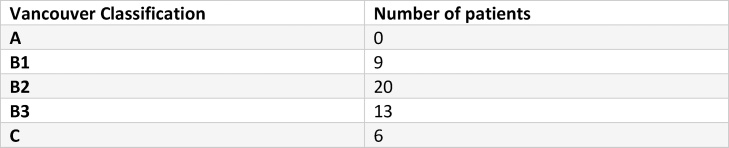
Over a two-year period, 48 patients were identified who had periprosthetic fractures needing operative intervention. The median age of the cohort was 73.5 years (53–88) and predominantly female, n = 30. The median time to fracture was 4.5 years, however this ranged from 9 months to 18.5 years. Periprosthetic fractures associated with both primary and revision total hip arthroplasty and hemiarthroplasty were included for analysis. Primary total hip arthroplasty had most femoral fractures, n = 24 (Fig. 1). Fig. 2 shows the stratification of the Vancouver classification among the study cohort. The majority were found to have Vancouver B2 fractures at time of the operation (n = 20).
Fig. 1.
Table: Implant associated with periprosthetic fracture.
Fig. 2.
Table: Vancouver Classification.
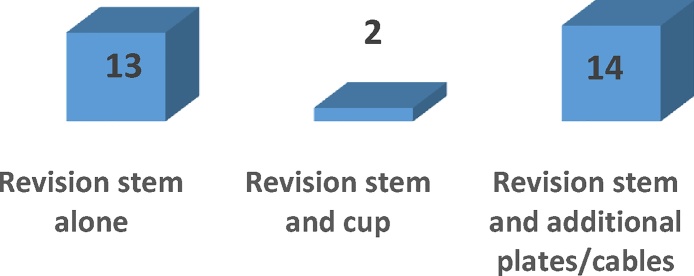
The majority of patients underwent revision arthroplasty, n = 29, with the femoral component being replaced in all cases. Open reduction internal fixation was undertaken in 19 cases, particularly those who had well fixed femoral stems or who were deemed medically unsuitable to undergo a full revision arthroplasty. Fig. 3, shows the type of revision operative intervention undertaken, including revision of the femoral stem with additional cables or plate cable constructs.
Fig. 3.
Revision operative intervention.
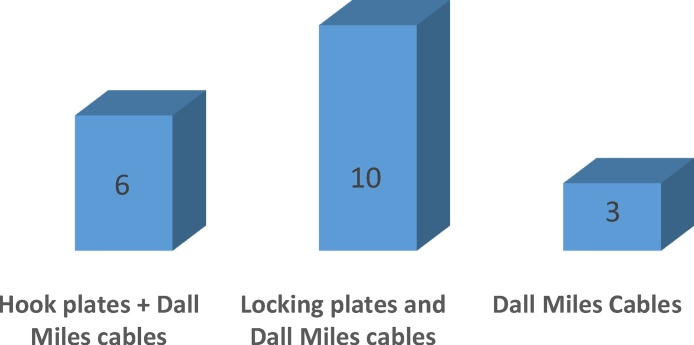
The open reduction internal fixation methods undertaken included hook plate, locking plate and cable fixation. Fig. 4 shows a graphical representation of this. The majority of patients who had ORIF fixation had a locking plate and cable construct.
Fig. 4.
ORIF operative constructs undertaken.
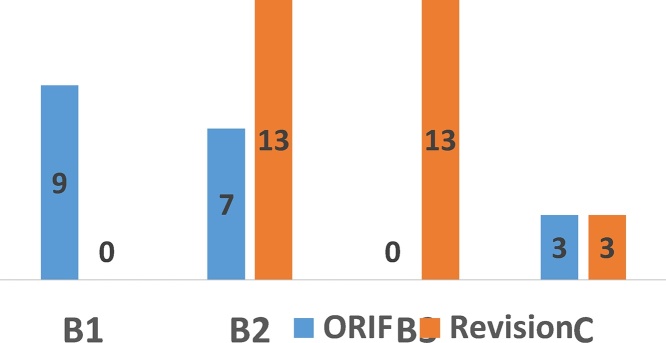
All Vancouver B3 fractures underwent revision arthroplasty. 13 B2 classified fractures underwent revision arthroplasty and 7 B2 fractures underwent ORIF fixation. We acknowledge that ORIF fixation in the setting of a loose stem is controversial. However, each patient was assessed with regards to medical and anaesthetic suitability for a revision arthroplasty. If the risks precluded them from a full revision, a decision for ORIF was made. Fig. 5 shows the graphical representation of the operative intervention based on Vancouver classification.
Fig. 5.
Operative intervention based on Vancouver classification.
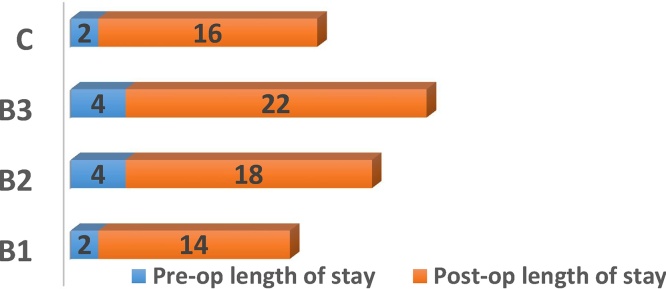
The mean length of stay for the cohort of patients was 24 days (9–42 days). The ORIF cohort had a shorter mean length of stay of 19 days (9–29 days) compared to the revision cohort of 29 days (9–42 days). This length of stay excluded rehabilitation or convalescence stays. When analysing the length of stay based on Vancouver classification, B3 fractures have the longest mean length of stay at 28 days. There was a 2–4 day delay to the index revision operation (Fig. 6).
Fig. 6.
Length of stay based on fracture classification.
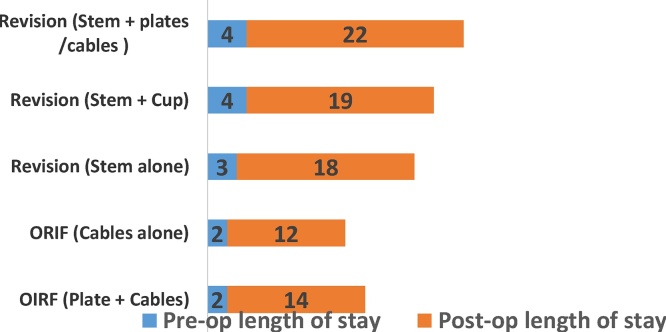
Length of stay based on operative technique was analysed. It was found that those who had a revision stem with plate and cable fixation had on average 26 days compared to 14 days for ORIF with cable fixation alone. Fig. 7 shows the length of stay based on operative technique.
Fig. 7.
Length of stay based on operative technique.
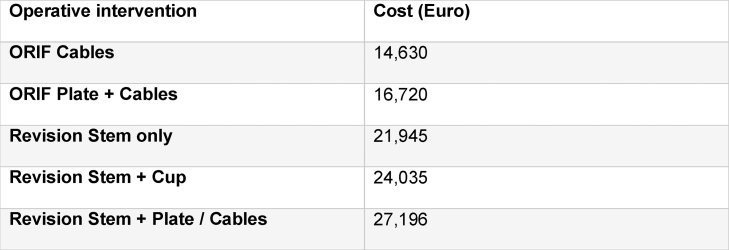
The average cost of an overnight stay in an Orthopaedic ward in a trauma unit is €1045 per night.4 Excluding the costs of theatre time, revision prosthesis implants and staff, the costs to the healthcare service ranges from €14000 to €27000 as shown below. Fig. 8 shows the costs of hospital stay based on the operative procedure undertaken.
Fig. 8.
Cost of hospital stay based on operative procedure.
Delayed discharges have major cost implications, as the average age of this cohort is 73.5 years, rehabilitation and convalescence is often needed to ensure patients can regain mobility. Patients stayed on average 15 days (5–21 days) in an acute trauma hospital while awaiting a rehabilitation bed. A delay of this magnitude can add additional costs up to €21,945.
A review of the clinical outcomes of this cohort was also undertaken. Results collated showed a dislocation rate of 4% (n = 2), superficial infection 6%(n = 3) and a periprosthetic fracture of 4% (n = 2). Both dislocation and periprosthetic fractures occurred in the Vancouver B3 group who underwent revision stem and plate, cable construct. No DVT or PE was identified. The mortality rate was 0% at 3 months and 14% (n = 7) within 1 year.
4. Discussion
Total hip arthroplasty has resulted in great clinical success, improved quality of life and functional ability. It is widely accepted as a very cost effective intervention. The number of THA’s being undertaken continue to increase yearly, with a projection of a 174% increase in numbers in the next 25 years. 5, 6, 7 Those patients undergoing revision arthroplasty often tend to be older have concurrent medial co-morbidities and can have bone loss or complex fracture patterns making revision operations more technically demanding. Hence complications associated with revision surgery can increase the associated costs and hospital stay.8 Excluding implant costs, it is clear that more complex operations with longer mean operating times in older medically unfit patients can be expected to increase the costs to the health services.
Estimating the actual financial cost of treating patients with periprosthetic fractures is a complex undertaking. Within the health services of both the UK and Ireland, very little detail is available about the costings of prosthetic implants, theatre times and staffing costs. Thus any financial review an inexact science. However it is clear that length of hospital stay which has a definite price point is one area we can assess the differences between patient groups and look at the costs of prolonged admissions. This can allow identification of reasons for prolonged admissions and allow planning for the future. With regards to the Vancouver classification it is suggestive from published literature that patients who undergo ORIF have shorter length of stay and hospital costs.9, 10 However, from our review it is clear that patients who have extensive ORIF procedures that include plating and cables do indeed have a shorter length of stay but it is non-significant. We acknowledge that our numbers in this study are small, but we do feel it gives a representative picture that patients undergoing revision, be that a standard femoral stem revision or combination stem, plating and cable revision have similar length of stay post operatively. Thus revisions would incur similar costs with regards to hospital length of stay regardless of procedure performed.
As a result of the increasing number of primary arthroplasties being performed, we can expect an increasing number of patients presenting with periprosthetic fractures needing revision or ORIF acutely. The mortality rates associated with periprosthetic fracture revision surgery is high at 7.8%.6 When compared to the mortality rate associated with aseptic loosening revision at 0.9%, the difference is substantial and should be considered. Overall one-year mortality rates are between 7 and 18%.2, 11 Additional resources are often needed to manage these patients in the pre and post-operative period and increased length of stay and costs can be expected to manage the co-morbidities.
The economic burden of revision arthroplasty is very relevant in times of tight healthcare budgets. In 2012 a group from London reviewed the cost of revision arthroplasty for all causes of revision surgery.10 The mean length of stay for aseptic loosening or dislocation was significantly shorter than for a periprosthetic fracture, at 9.3 days compared to 17.8 days. Pre-operative investigation costs were higher in the cases associated with deep infection. There was no statistical difference in the mean implant costs between those undergoing revision for infection or periprosthetic fracture. The mean total cost for a patient with a periprosthetic fracture was £18,185 compared to £11,897 for aseptic loosening. Vanhegan et al. showed a statistical significance in the difference in costs to the health service between an aseptic loosening revision and a periprosthetic revision operation. Complications were also significantly higher in the periprosthetic revision group compared to the other groups, again adding to costs and hospital stay.10 Phillips et al. in 2011 reviewed the cost of treating periprosthetic hip fractures in a single unit. Over a 10 year period they had 146 patients treated for periprosthetic hip fractures. The total length of stay in this cohort was 39.3 days, and the mean cost for treatment was £23,469 per patient. Philips et al. completed a costing assessment, which showed that ward costs contributed the most to the overall cost at 80%.9 Using length of stay as a metric, they found that if inpatient stay exceeded 30 days the mean cost per patient was over £33,000 compared to £11,386 if less than 30 days.9
From the literature it is clear that the cohort of patients that have periprosthetic hip fractures have multiple medical co-morbidities.12, 13 These patients need increased allied health care professionals input, with regards to gait retraining and safety assessments to ensure they can be discharged safely. All of our patient cohort were referred to the Geriatric Medicine services for rehabilitation post operatively. As the average age of our patients continues to increase many units are experiencing difficulty with discharge planning. Requirements for additional rehabilitation beds and allied health professionals have not be met by the health services to date. Until additional rehab beds and services are made available, the length of stay of these patients in acute trauma beds will continue to be high and costly.
It is clear from the literature that costs to the health services are increasing and quite substantial but specific costings are rarely reported. True data and costs incurred by the health service are difficult to elucidate from finance departments, true costs of implants also can vary between institutions pending on purchasing agreements between hospital groups and suppliers. It is imperative that costs of hospital stay, investigations and implants be made widely known, so that accurate analysis of the cost of treatment can be undertaken. This will facilitate future resource planning, budget allocation and also facilitate ‘money following the patient’ appropriately, as patients begin to be transferred for definitive treatment in specialist units.
Conflict of interest
None.
References
- 1.13th Annual report 2016, National joint registry for England, Wales, Northern Ireland and the Isle of Man UK 2016. http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/13th%20Annual%20Report/07950%20NJR%20Annual%20Report%202016%20ONLINE%20REPORT.pdf.
- 2.Frenzel S., Vecsei V., Negrin L. ‘Periprosthetic femoral fractures –incidence, classification problems and the proposal of a modified classification scheme’. Int Orthop (SICOT) 2015;39:1909–1920. doi: 10.1007/s00264-015-2967-4. [DOI] [PubMed] [Google Scholar]
- 3.Dixon T., Shaw M., Ebrahim S., Dieppe P. Trends in hip and knee joint replacement: socioeconomic inequalities and projections of need. Ann Rheum Dis. 2004;63:825–830. doi: 10.1136/ard.2003.012724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.2018. HSE Charges.https://www.hse.ie/eng/services/list/3/acutehospitals/hospitals/Hospitalcharges.html [Accessed online on 22 May, 17] [Google Scholar]
- 5.Healy W.L., Iorio R. Implant selection and cost for total joint arthroplasty: conflict between surgeons and hospitals. Clin Orthop. 2007;457:57–63. doi: 10.1097/BLO.0b013e31803372e0. [DOI] [PubMed] [Google Scholar]
- 6.Ong K.L., Mowat F.S., Chan N. Economic burden of revision hip and knee arthroplasty in Medicare enrollees. Clin Orthop. 2006;446:22–28. doi: 10.1097/01.blo.0000214439.95268.59. [DOI] [PubMed] [Google Scholar]
- 7.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg [Am] 2007;89(A):780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 8.Amenabar T., Rahman W.A., Avhad V.V., Vera R., Gross A.E., Kuzyk P.R. ‘Vancouver tuype B2 and B3 periprosthetic fractures treated with revision total hip arthroplasty’. Int Orthop (SICOT) 2015;39:1927–1932. doi: 10.1007/s00264-015-2957-6. [DOI] [PubMed] [Google Scholar]
- 9.Phillips J.R.A., Boulton C., Moran C.G., Manktelow A.R.J. ‘What is the financial cost of treating periprosthetic hip fractures?’. Injury Int J Care Injured. 2011;42:146–149. doi: 10.1016/j.injury.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 10.Vanhegan I.S., Malik A.K., Jayakumar P., Ul Islam S., Haddad F.S. ‘A financial analysis of revision hip arthroplasty: the Economic Burden in relation to the National Tarriff’. J Bone Joint Surg Br. 2012;94(B):619–623. doi: 10.1302/0301-620X.94B5.27073. [DOI] [PubMed] [Google Scholar]
- 11.Young S.W., Walker C.G., Pitto R.P. Functional outcome of femoral peri prosthetic fracture and revision hip arthroplasty: a matched-pair study from the New Zealand Registry. Acta Orthop. 2008;79:4834–8874. doi: 10.1080/17453670710015463. [DOI] [PubMed] [Google Scholar]
- 12.Riemen A.H.K., James D., Hutchison J.D. ‘The multidisciplinary management of hip fractures in older patients’. Orthop Trauma. 2016;30(Apr (2)):117–122. doi: 10.1016/j.mporth.2016.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith T.O., Hameed Y.A., Cross J.L., Henderson C., Sahota O., Fox C. Enhanced rehabilitation and care models for adults with dementia following hip fracture surgery. Cochrane Database Syst Rev. 2015;(6) doi: 10.1002/14651858.CD010569.pub2. [Art. No.:CD010569] [DOI] [PubMed] [Google Scholar]