Abstract
Background
We noticed that most of active sports children with low back pain (LBP) have muscle tightness around the pelvis and reduced trunk flexibility. Abnormalities in short-time inversion recovery (STIR) images on magnetic resonance imaging (MRI) can show stress fracture. Therefore, we investigated the associations among LBP, trunk flexibility, and lumbar stress fractures.
Methods
A total of 130 patients under the age of 18 years complained of LBP were investigated in STIR MRI images. Among these 130 patients, 65 cases of lumbar stress fracture were diagnosed and 65 cases were not diagnosed as a lumbar stress fracture. We compared between a group suspected of stress fracture (suspected group) and a group of stress fracture(stress fracture group)about their trunk flexibility. These groups were investigated about their initial trunk flexibility about below items; Finger floor distance (FFD), Heel to buttock distance (HBD), straight leg raising (SLR).
Results
Significant differences were observed between suspected group and stress fracture group about every items; SLR (P < 0.001), FFD (P < 0.01), HBD (P < 0.002). Most cases of stress fracture group had reduced trunk flexibility, and low flexibility in pelvic area muscles was observed in 93.8% (61/65) of cases at the initial examination. Otherwise, that of suspected group was 73.8%(48/65).
Conclusions
Most patients of lumbar stress fracture had reduced trunk flexibility, and their reduced trunk flexibility might not be caused by LBP. In the early diagnosis of lumbar stress fractures using STIR MRI images, there were indicated that reduced trunk flexibility was one of helpful item for lumbar stress fracture.
Keywords: STIR MRI images, Lumbar stress fracture, Trunk flexibility, Low back pain
1. Introduction
We noticed that most of active sports children with low back pain (LBP) have muscle tightness around the pelvis and their reduced trunk flexibility. If they continue vigorous exercise while having muscle tension around the pelvis, we may be doubted that the possibility that repeated stress accumulates somewhere in their body. If no abnormal sign is identified on radiography or on clinical assessment in these children, we tend to diagnose them with unknown lumbar pain. However, we believe that the diagnosis depends on the cause of LBP. According to a previous report, on magnetic resonance imaging (MRI), abnormal findings in short-time inversion recovery (STIR) and T1 images indicate the stage before the occurrence of a stress fracture.1 We applied this principle to the lumbar vertebrae and found abnormalities in STIR MRI images. In addition, some previous studies have reported a relationship between LBP and hip flexibility.2, 3, 4, 5, 6 We doubted that stress fracture might have occurred as a result of repeated stress to the lumbar vertebrae. Perhaps reduced trunk flexibility might be compensated by changes in the lumbar vertebrae. Hence, we generally performed MRI examination in active sports children with flexion or extension lumbar pain or reduced trunk flexibility, despite the absence of a fracture sign on radiography, to confirm the existence of a stress fracture.
The present study aimed to investigate the associations among reduced trunk flexibility, and lumbar stress fracture. Additionally, we considered detail of trunk flexibility item about stress fracture group, and the prevention and treatment of stress fracture during the growth period is discussed.
2. Materials and methods
2.1. Patients
This is a case control study. Eligibility criteria were patients with low back pain during the growth period under the age of 18 years between June 2007 and November 2016. 65 cases which diagnosed as a stress fracture and 65cases which suspected stress fracture. 65 cases which were diagnosed lumbar stress fracture (55 cases in boys and 10 cases in girls; mean patient age, 14.0 + − 1.60 years [range, 8–17 years]) were defined as a stress fracture group. 65 cases which were not diagnosed lumbar stress fracture (31 cases in boys and 34 cases in girls; mean patient age, 14.0 + −1.84 years [range, 10–18 years]) were defined as a suspected group.
This study was approved by the institutional review boards of the concerned institutions. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from the parents/guardian of the children included in the study.
2.2. Study protocol
Patients who complained of LBP at the first medical examination and fulfilled any of the following criteria underwent MRI: 1) aggravation of LBP during standing (anteflexion) or during the one-leg extension test;7, 8, 9, 10 2) reduction in trunk and lower limb flexibility indicated with reduced results in a straight-leg-raising angle (SLR), finger-to-floor distance (FFD), or heel-to-buttock distance (HBD) test; and 3) bone sclerosis or bone resorption in the pars interarticularis in oblique radiographs.
Coronal and transverse T1-weighted images and STIR images were obtained using a 0.3T AIRIS Vento open MRI system (Hitachi Medical Corporation, Chiyoda, Tokyo). All MRI images from the initial examination to the final examination were assessed by the same doctor.
2.3. Assessment of trunk flexibility (muscle tightness)
The SLR, HBD, and FFD tests were used as indices of flexibility. The following standard values were set for these muscle tightness tests: SLR, 70°; FFD, 0 finger’s breadth [fb]; and HBD, 0 cm. This standard was used as a criterion for pass of flexibility. Joint laxity was not assessed in the present study, as it can be influenced by sex and age.
2.4. Treatment methods and protocols
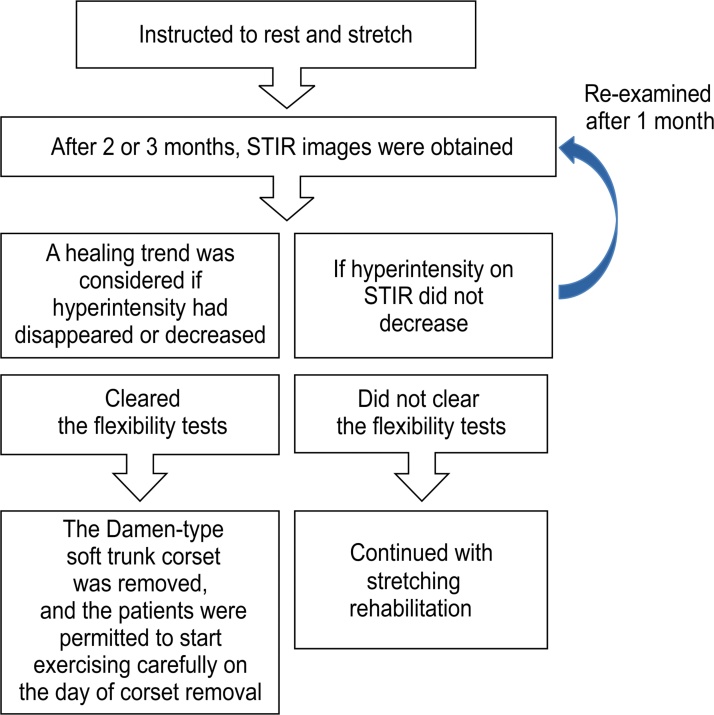
Physical therapy was continued until all patients achieved the standard values set for the SLR, FFD, and HBD tests. When hyperintensity was observed in STIR MRI images, patients were fitted with a Damen-type soft trunk corset, were instructed to rest, and were taught to stretch according to the methods described by Sairyo et al. 11 Radiographic changes were assessed every month to confirm whether a fracture was present near the hyperintense area. After 2–3 months, STIR MRI images were obtained, and patients were considered to be in a healing trend if the hyperintensity disappeared or decreased in the MRI images (Fig. 1).1 In patients who were considered to be in a healing trend and who achieved the pass standard of trunk flexibility, the Damen-type soft trunk corset was removed, and these patients were permitted to start exercising carefully on the day of corset removal. The level of exercise was increased gradually to avoid LBP or discomfort, and if the patients did not experience any problems for approximately 2 weeks, medical follow-up was discontinued. Patients who did not achieve the standard values of the muscle tightness tests continued with stretching rehabilitation. Additionally, patients who did not show a decrease in hyperintensity in STIR MRI images were re-examined after 1 month (Fig. 2).
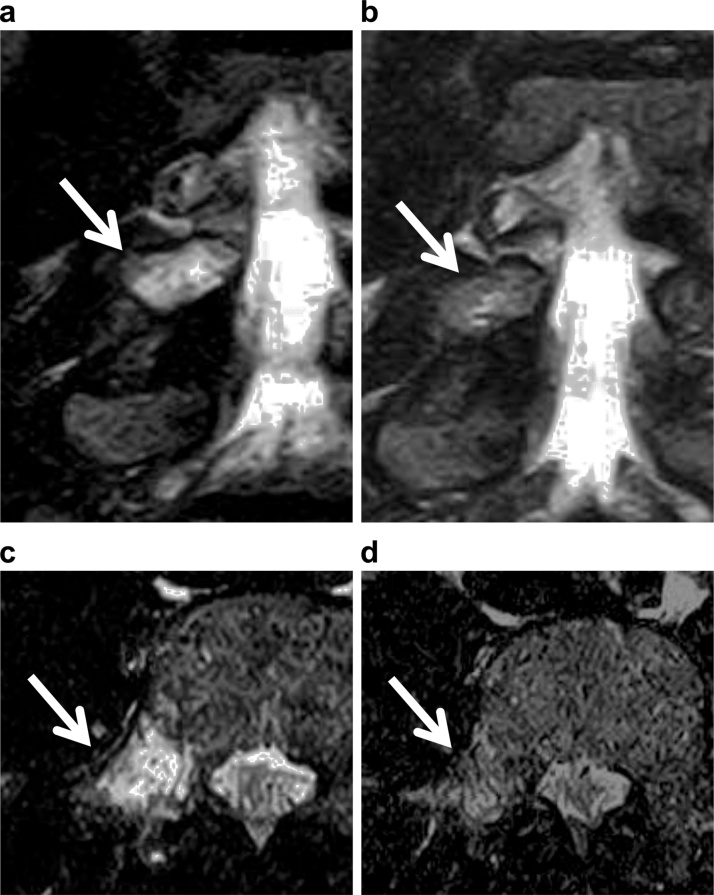
Fig. 1.
Disappearance of hyperintensity. A clear area of hyperintensity (white arrow) is observed on magnetic resonance imaging (MRI) (a) at the initial examination from the L5 vertebral arch to the pedicle; however, it is not observed on MRI (b) at the final examination. Upper/coronal view, lower/axial view.
Fig. 2.
Treatment protocol.
2.5. Outcome measures
In the stress fracture cases, we examined the treatment period; proportion of patients with reduced results in the SLR, HBD, and FFD tests at the initial examination; change in these test results at the final examination; time taken to achieve flexibility; rate of return to sports; and changes in the STIR MRI images.
2.6. Statistical analysis
We compared between a suspected group and a stress fracture group about their trunk flexibility. These groups were examined for their initial trunk flexibility about below items using the Welch’s t-test; FFD, HBD, SLR. We used the Wilcoxon signed-rank test to determine whether changes in the SLR, HBD, and FFD test results (non-continuous and non-normally distributed data) were significant.
All statistical analyses were performed using SPSS, version 22.0 for Windows (IBM Corp., Armonk, NY). A P-value ≤0.05 was considered statistically significant.
3. Results
Significant differences were observed between suspected group and stress fracture group about every item; SLR (P < 0.00001), FFD (P < 0.01), HBD (P < 0.002) (Table 1). Most cases of stress fracture group had reduced trunk flexibility, and low flexibility in pelvic area muscles was observed in 93.8% (61/65) of cases at the initial examination. On the other hands, it was 73.8% (48/65) in the suspected group.
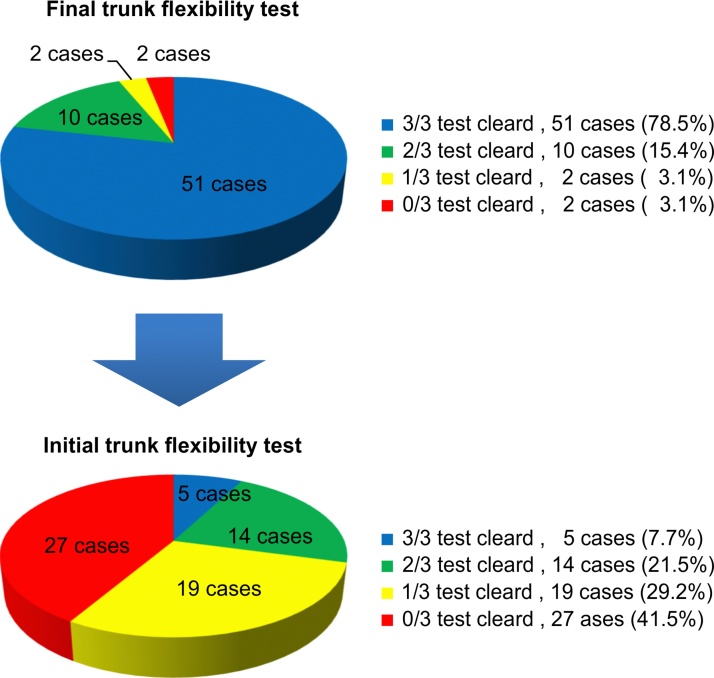
In the stress fracture group, five cases (7.7%) reached the pass level and 60 cases (92.3%) did not reach the pass level. 14 cases passed 2 out of the 3 items (SLR, FFD, HBD) [21.5%], 19 passed 1 out of 3 items [29.2%], and 27 did not pass any item [41.5%] at the initial medical examination (Fig. 3). At the final examination, 51 of the 65 cases (78.5%) reached the pass level of trunk flexibility and 14 did not reach the pass level (Fig. 3). In 14 cases which did not reach the pass level, 10 cases passed 2 out of 3 items (15.4%), 2 cases passed 1 out of 3 items (3.1%), 2 patients did not pass any item (3.1%) (Fig. 3).
Fig. 3.
Initial final trunk flexibility comparison.
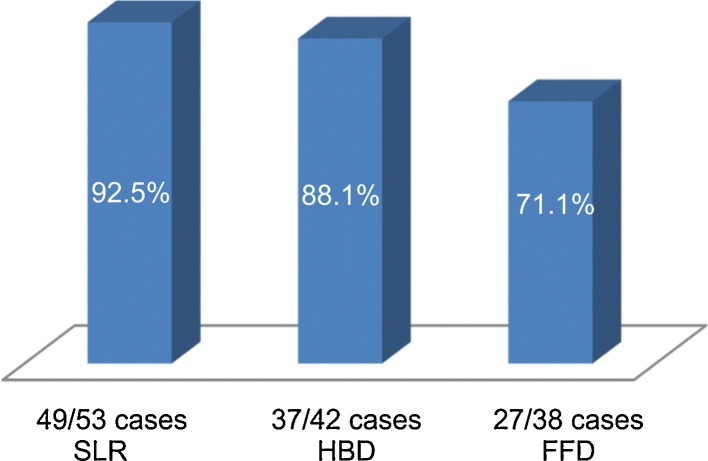
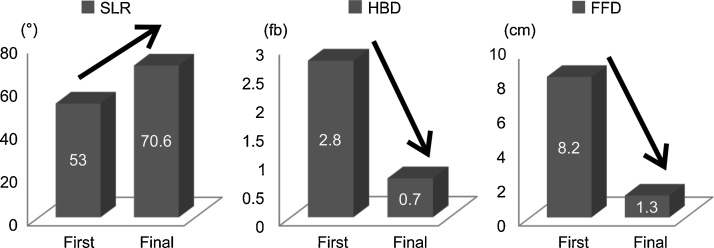
The rates of improvement in the results of the SLR, HBD, and FFD tests at the final examination were 92.5% (49/53 cases), 88.1% (37/42), and 71.1% (27/38), respectively (Fig. 4).
Fig. 4.
Improvement ratio of flexibility at the final examination. SLR, straight-leg-raising angle; FFD, finger-to-floor distance; HBD, heel-to-buttock distance.
The mean values in the SLR, HBD, and FFD tests improved from 53.0° to 70.6°, 2.8 fb to 0.7 fb, and 8.2 cm to 1.3 cm, respectively (Fig. 5). An improvement in flexibility was observed in 61 cases, while 4 cases did not exhibit improvement. The Wilcoxon signed-rank test showed that the SLR test value increased significantly between the initial and final examinations (P < 0.001), and that the HBD and FFD test values decreased significantly between the initial and final examinations (P < 0.001).
Fig. 5.
Overall flexibility improvement rates in the groups. SLR, straight-leg-raising angle; FFD, finger-to-floor distance; HBD, heel-to-buttock distance.
LBP disappeared approximately 21 days after instructing the patients to rest, and flexibility was achieved at a mean of 37.6 days. The median treatment period was 119 days (range, 53–1105 days), and all the patients returned to usual sporting activities. The rate of return to sports was 100%.
Hyperintensity in STIR MRI images disappeared in 51 of the 65 cases (78.5%), decreased in 8 cases (12.3%), and increased in 6 cases (9.2%). The onset site was bilateral, right, and left in 23, 25, and 17 cases, respectively.
4. Discussion
Repeated microtrauma and excessive stress at the lumbar vertebra have been reported to be involved in the onset of lumbar stress fractures,12, 13, 14 although only few studies have examined the causes in detail. Some studies have reported the influence of trunk flexibility on LBP.2, 3, 4, 5, 6 Hence, we considered that a reduction in trunk flexibility might be associated with repeated micro-trauma and excessive stress at the lumbar vertebra as a bone stress reaction.15 We focused on a reduction in the flexibility of pelvic area muscle groups, as an essential aspect of compensation for a reduction in trunk flexibility.8, 9 Considering a reduction in flexibility as the basis for treatment in patients with lumbar stress fracture,7, 10 we implemented therapies that improve trunk and lower limb flexibility,16 and examined the change in these values at the final examination and the time taken to achieve flexibility without pain. Although the symptoms of LBP disappeared within 3 weeks in all cases, the time taken to acquire trunk flexibility was over 3 weeks. Thus, we proved that a reduction in trunk flexibility was not caused by LBP, as the reduction in trunk flexibility existed even after the LBP resolved.
In the present study, among the 65 cases of stress fracture group, only 5 (7.7%) cleared all the muscle tightness tests and 60 (92.3%) did not clear all the tests, suggesting that a reduction in trunk flexibility exists in patients with lumbar stress fractures during the growth period. In almost all patients with lumbar stress fractures, a reduction in hamstring flexibility7, 10 or an FFD test result of 0 has been reported.12 Although we could not investigate the general reduction in trunk flexibility without low back pain during the growth period, we noted a high incidence of reduction in trunk flexibility among patients with lumbar stress fractures. Hence, we regarded a reduction in trunk flexibility as one of the reasons for a lumbar stress fracture, and rehabilitation stretching was continued during the rest period to prevent recurrence.
Studies have indicated that 47% of young individuals presenting to hospitals with at least a 3-week history of LBP experience a lumbar stress fracture or spondylolysis during the growth period.17, 18 Thus, a stress fracture should always be considered in patients with LBP during the growth period.
A previous study reported that stress fractures are common in girls during the growth period, as many hormonal changes occur during this period.19 However, a goodness-of-fit test of the lumbar stress fractures in the present study showed that the incidence of lumbar stress fractures was 5 times over greater in boys than in girls (P < 0.001), and our result was similar to that reported in the study by Morita et al.13
The presence of pain only on extension and not on flexion has been reported previously.18, 20, 21 However, in actual practice, we found that LBP varied in severity during flexion when muscular tension around the lower lumbar vertebrae was observed at the initial diagnosis and positive STIR MRI findings were noted. In the present study, we did not identify a difference between extension pain and flexion pain.22
MRI images are helpful for the early detection and diagnosis of lumbar stress fractures. Hyperintensity on STIR MRI images is indicative of bone marrow edema and bleeding; therefore, it is considered important for the early detection of a lumbar stress fracture.11, 23, 24 When T1-weighted images are also used, old stress fractures can be evaluated as well.11 Thus, in STIR and T1-weighted MRI images, low intensity is normal, whereas hyperintensity indicates the presence of a stress fracture. Many cases of classical spondylolysis that can be clearly determined from plain radiographs are at the end-stage, and therefore, synostosis is difficult. However, considering the MRI grading of spondylolysis by Hollenberg et al.25 when hyperintensity is observed in STIR MRI images, the inflammatory response is not complete and a minor response remains; hence, there is a possibility of synostosis. If hyperintensity disappears, the case can be considered an old case, wherein the inflammatory response has disappeared. In such cases, traditional methods of muscle strength training and exercise according to the pain level are considered logical approaches.26, 27 We believe that these evaluation guidelines may help prevent prolonging therapy by only instructing the patient to rest.
Based on these findings, we used STIR MRI images as an early evaluation index and determined healing according to a decrease in inflammation and improvements in stretching. Moreover, we obtained monthly oblique and lateral radiographs, which were closely observed for any bone changes. We believe that treatment strategies should be determined by evaluating STIR MRI images over time, and this approach was effective at our clinic.
The disappearance or decrease of hyperintensity in STIR MRI images was observed in 90.1% of the cases at the final examination. The patients who showed an increase in hyperintensity had not followed instructions to rest and continued participating in sports activities, although all of them had agreed to rest at the initial examination.
Opinions are divided regarding the use of a hard trunk corset, semi-hard trunk corset, soft trunk corset, or no corset.28, 29, 30 It is difficult to ensure that children who are very active in sports take rest, if the use of a corset is not indicated during the resting period. The patient’s cooperation is important, and therefore, we recommend the use of a soft lumbar corset for 2–3 months during bone recovery.
There may be some doubts about whether the economics in this study were realistic; however, we wonder whether the economical results of the cases that could not start treatment would have been the same if we had not detected the fracture earlier.
4.1. Limitations
The present study had some limitations. In cases of severe LBP, we could not perform the muscle tightness tests appropriately. Further multi-centre studies with a large number of patients are needed to confirm our findings.
4.2. Conclusions
In our study, after LBP subsided, reduced trunk flexibility remained, and among those patients, many had stress fractures. Though most patients with LBP might have reduced trunk flexibility, their reduced trunk flexibility might not be caused by LBP. Hence, reducing repeated microtrauma and excessive stress to the lumbar vertebra by early detection and early acquisition of trunk flexibility might be important in the treatment of stress fractures during the growth period.
In the treatment of lumbar stress fractures, early diagnosis using STIR MRI images, trunk fixation, and stretching of the pelvic area muscles are considered important.
Conflict of interest
None
Funding
None.
Ethical approval
This study was approved by the institutional review boards of the concerned institutions KOSSMOS Medical Corporation (KE-002), Kyorin University (H26-065 NO.528), Japan Community Health Care Organization Yamanashi Hospital (JMA-IIA00189) dated August 7th, 2014.
Informed consent was obtained from the parents/guardian of the children included in the study.
References
- 1.Arendt E.A., Griffiths H.J. The use of MR imaging in the assessment and clinical management of stress reactions of bone in high-performance athletes. Clin Sports Med. 1997;16:291–306. doi: 10.1016/s0278-5919(05)70023-5. [DOI] [PubMed] [Google Scholar]
- 2.Corkery M.B., O'Rourke B., Viola S. An exploratory examination of the association between altered lumbar motor control, joint mobility and low back pain in athletes. Asian J Sports Med. 2014;5:e24283. doi: 10.5812/asjsm.24283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nagai T., Abt J.P., Sell T.C. Lumbar spine and hip flexibility and trunk strength in helicopter pilots with and without low back pain history. Work. 2015;52:715–722. doi: 10.3233/WOR-152192. [DOI] [PubMed] [Google Scholar]
- 4.Okamura S., Wada N., Tazawa M. Injuries and disorders among young ice skaters: relationship with generalized joint laxity and tightness. Open Access J Sports Med. 2004;5:191–195. doi: 10.2147/OAJSM.S63540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Radwan A., Bigney K.A., Buonomo H.N. Evaluation of intra-subject difference in hamstring flexibility in patients with low back pain: an exploratory study. J Back Musculoskelet Rehabil. 2014;8:61–66. doi: 10.3233/BMR-140490. [DOI] [PubMed] [Google Scholar]
- 6.Sung P.S. A kinematic analysis for shoulder and pelvis coordination during axial trunk rotation in subjects with and without recurrent low back pain. Gait Posture. 2014;40:493–498. doi: 10.1016/j.gaitpost.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Czaprowski D., Leszczewska J., Kolwicz A. The comparison of the effects of three physiotherapy techniques on hamstring flexibility in children: a prospective, randomized, single-blind study. PLoS One. 2013;8:e72026. doi: 10.1371/journal.pone.0072026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gauvin M.G., Riddle D.L., Rothstein J.M. Reliability of clinical measurements of forward bending using the modified fingertip-to-floor method. Phys Ther. 1990;70:443–447. doi: 10.1093/ptj/70.7.443. [DOI] [PubMed] [Google Scholar]
- 9.Mierau D., Cassidy J.D., Yong-Hing K. Low-back pain and straight leg raising in children and adolescents. Spine (Phila Pa 1976) 1989;1989(14):526–528. doi: 10.1097/00007632-198905000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Santonja Medina F.M., Sainz De Baranda Andújar P., Rodríguez García P.L. Effects of frequency of static stretching on straight-leg raise in elementary school children. Sports Med Phys Fitness. 2007;47:304–308. [PubMed] [Google Scholar]
- 11.Meyers S.P., Wiener S.N. Magnetic resonance imaging features of fractures using the short tau inversion recovery (STIR) sequence: correlation with radiographic findings. Skeletal Radiol. 1991;20:499–507. doi: 10.1007/BF00194246. [DOI] [PubMed] [Google Scholar]
- 12.Ciullo J.V., Jackson D.W. Pars interarticularis stress reaction, spondylolysis, and spondylolisthesis in gymnasts. Clin Sports Med. 1985;4:95–110. [PubMed] [Google Scholar]
- 13.Morita T., Ikata T., Katoh S. Lumbar spondylolysis in children and adolescents. J Bone Joint Surg Br. 1995;77:620–625. [PubMed] [Google Scholar]
- 14.Purcell L., Micheli L. Low back pain in young athletes. Sports Health. 2009;1:212–222. doi: 10.1177/1941738109334212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gregory P.L., Batt M.E., Kerslake R.W. Single photon emission computerized tomography and reverse gantry computerized tomography findings in patients with back pain investigated for spondylolysis. Clin J Sport Med. 2015;15:79–86. doi: 10.1097/01.jsm.0000152710.82225.3d. [DOI] [PubMed] [Google Scholar]
- 16.Sairyo K., Kawamura T., Mase Y. Jack-knife stretching promotes flexibility of tight hamstrings after 4 weeks: a pilot study. Eur J Orthop Surg Traumatol. 2013;23:657–663. doi: 10.1007/s00590-012-1044-6. [DOI] [PubMed] [Google Scholar]
- 17.Micheli L.J., Wood R. Back pain in young athletes: significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med. 1995;149:15–18. doi: 10.1001/archpedi.1995.02170130017004. [DOI] [PubMed] [Google Scholar]
- 18.d’Hemecourt P.A., Gerbino P.G., 2nd, Micheli L.J. Back injuries in the young athlete. Clin Sports Med. 2000;19:663–679. doi: 10.1016/s0278-5919(05)70231-3. [DOI] [PubMed] [Google Scholar]
- 19.Boden B.P., Osbahr D.C., Jimenez C. Low-risk stress fractures. Am J Sports Med. 2001;29:100–111. doi: 10.1177/03635465010290010201. [DOI] [PubMed] [Google Scholar]
- 20.McTimoney C.A., Micheli L.J. Current evaluation and management of spondylolysis and spondylolisthesis. Curr Sports Med Rep. 2003;2:41–46. doi: 10.1249/00149619-200302000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Simon L.M., Jih W., Buller J.C. Back pain and injuries. In: Birrer R.B., Griesemer B.A., Cataletto M.B., editors. Pediatric Sports Medicine for Primary Care. Lippincott Williams & Wilkins; Philadelphia, PA: 2002. pp. 306–325. [Google Scholar]
- 22.Masci L., Pike J., Malara F. Use of the one-legged hyperextension test and magnetic resonance imaging in the diagnosis of active spondylolysis. Br J Sports Med. 2006;40:940–946. doi: 10.1136/bjsm.2006.030023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sairyo K., Katoh S., Takata Y. MRI signal changes of the pedicle as an indicator for early diagnosis of spondylolysis in children and adolescents: a clinical and biomechanical study. Spine (Phila Pa 1976) 2006;31:206–211. doi: 10.1097/01.brs.0000195161.60549.67. [DOI] [PubMed] [Google Scholar]
- 24.Yamane T., Yoshida T., Mimatsu K. Early diagnosis of lumbar spondylolysis by MRI. J Bone Joint Surg Br. 1993;75:764–768. doi: 10.1302/0301-620X.75B5.8376435. [DOI] [PubMed] [Google Scholar]
- 25.Hollenberg G.M., Beattie P.F., Meyers S.P. Stress reactions of the lumber pars interarticularis: the development of a new MRI classification system. Spine (Phila Pa 1976) 2002;27:181–186. doi: 10.1097/00007632-200201150-00012. [DOI] [PubMed] [Google Scholar]
- 26.George S.Z., Delitto A. Management of the athlete with low back pain. Clin Sports Med. 2002;21:105–120. doi: 10.1016/s0278-5919(03)00060-7. [DOI] [PubMed] [Google Scholar]
- 27.Watkins R.G. Lumbar disc injury in the athlete. Clin Sports Med. 2002;21:147–165. doi: 10.1016/s0278-5919(03)00063-2. [DOI] [PubMed] [Google Scholar]
- 28.El Rassi G., Takemitsu M., Woratanarat P. Lumbar spondylolysis in pediatric and adolescent soccer players. Am J Sports Med. 2005;33:1688–1693. doi: 10.1177/0363546505275645. [DOI] [PubMed] [Google Scholar]
- 29.Sairyo K., Sakai T., Yasui N. Conservative treatment of lumbar spondylolysis in childhood and adolescence: the radiological signs which predict healing. J Bone Joint Surg Br. 2009;91:206–209. doi: 10.1302/0301-620X.91B2.21256. [DOI] [PubMed] [Google Scholar]
- 30.Standaert C.J., Herring S.A. Spondylolysis: a critical review. Br J Sports Med. 2000;34:415–422. doi: 10.1136/bjsm.34.6.415. [DOI] [PMC free article] [PubMed] [Google Scholar]