Abstract
Aim
It has been suggested that the use of a pilot-hole may reduce the risk of fracture to the lateral cortex. Therefore the purpose of this study was to determine the effect of a pilot hole on the strains and occurrence of fractures at the lateral cortex during the opening of a high tibial osteotomy (HTO) and post-surgery loading.
Materials and Methods
A total of 14 cadaveric tibias were randomized to either a pilot hole (n = 7) or a no-hole (n = 7) condition. Lateral cortex strains were measured while the osteotomy was opened 9 mm and secured in place with a locking plate. The tibias were then subjected to an initial 800 N load that increased by 200 N every 5000 cycles, until failure or a maximum load of 2500 N.
Results
There was no significant difference in the strains on the lateral cortex during HTO opening between the pilot hole and no-hole conditions. Similarly, the lateral cortex and fixation plate strains were not significantly different during cyclic loading between the two conditions. Using a pilot hole did not significantly decrease the strains experienced at the lateral cortex, nor did it reduce the risk of fracture.
Conclusions
The nonsignificant differences found here most likely occurred because the pilot hole merely translated the stress concentration laterally to a parallel point on the surface of the hole.
Cite this article: K. Bujnowski, A. Getgood, K. Leitch, J. Farr, C. Dunning, T. A. Burkhart. A pilot hole does not reduce the strains or risk of fracture to the lateral cortex during and following a medial opening wedge high tibial osteotomy in cadaveric specimens. Bone Joint Res 2018;7:166–172. DOI: 10.1302/2046-3758.72.BJR-2017-0337.R1.
Keywords: Lateral cortex, Tibial osteotomy, Fracture, High Tibial Osteotomy, Lateral Cortical Strains, Fixation Plate
Article focus
A medial opening wedge high tibial osteotomy is an effective procedure to mitigate the effects of uni-compartmental osteoarthritis
The lateral cortical hinge is at risk of fracture during this surgery
It has been suggested that the use of a pilot-hole near the lateral cortex will prevent cortical fracture
Key messages
A pilot hole does not reduce lateral cortical bone strains during high tibial osteotomy (HTO) opening.
The use of a pilot hole did not lower the risk of lateral cortical fracture during HTO opening.
Caution should be practiced when using HTO fixation systems that use a pilot hole.
Strengths and limitations
Controlled laboratory study
Investigation of strains experienced during and post-surgery following instrumentation
Use of cadaveric specimens
Introduction
Unicompartental osteoarthritis most commonly affects the knee joint, with malalignment being identified as one of the primary causes.1 While a partial or total knee arthroplasty is a common surgical option, these implants have a limited life span (approximately 5% to 20% have poor outcomes at ten years),2-4 and as such these may not be a viable option for younger active patients. A medial opening wedge high tibial osteotomy (mHTO) procedure is used to correct varus malalignment and reduce the symptoms experienced by the patient.5,6 During a mHTO, an oblique medial-to-lateral surgical cut is made in the proximal tibia, effectively creating a lateral cortical bone hinge. The wedge is then opened about this hinge until the desired correction/opening is achieved and then the bone is commonly stabilized with a fixation plate.6
Disruption (e.g. fracture) of the lateral cortical hinge has been reported to occur in 16% to 25% of patients.7-12 The ‘hinge’ is a common failure location because the apex of the osteotomy produces stress concentrations6,7 that are commonly formed at the edges of cracks, notches, or sharp corners.13,14 Disruption of the lateral cortical hinge can result in loss of stability, delayed- or non-union, or recurrent varus deformity;8,11,12 this can lead to increasing pain and a longer time to full, pain-free weight bearing. Furthermore, the extra recovery time associated with the more severe fractures (e.g. type II and type III where the fracture reaches the distal portion of the proximal tibiofemoral joint or compromises the tibial plateau, respectively)10,11 can result in greater length of time for return to work and resumption of normal activities of daily living;15 this can subsequently lead to decreased quality of life and increased indirect healthcare costs.
In a recent report, Ogawa et al9 identified gap opening distance and osteotomy sufficiency (i.e. the extent of the osteotomy’s involvement with the anterior and posterior proximal cortical bone) as being significantly associated with a fracture to the lateral cortical hinge. Furthermore, Nakamura et al12 suggested that the position of the hinge may influence the risk of fracture to the lateral aspect of the tibia, and developed a classification system to describe safe zones for the hinge. A relatively new technique that is purported to reduce stress concentrations produced at the apex of the osteotomy is to introduce a pilot hole at this location; theoretically, the hole will distribute the stresses over the larger area of the round walls of the hole.13 Surgical techniques have been developed that include a pilot hole at the apex of the osteotomy prior to opening the gap,16,17 and the use of a pilot hole has been shown to be safe for a 3o increase in correction.16 However, although this technique is being used clinically,16,17 to the authors’ knowledge, there has not been an investigation into the effectiveness of a pilot hole in reducing the risk of intra- or postoperative lateral cortex hinge fractures associated with mHTO.
Therefore, the purpose of this laboratory investigation was to determine the effectiveness of a pilot hole in reducing the strains at the lateral cortical hinge during mHTO opening and in response to cyclic loading. We hypothesized that including a pilot hole would reduce the stress concentration of the lateral cortex, thereby reducing the strains measured at the lateral cortex during opening, and in response to cyclic loading postoperatively. We also hypothesized that the redistribution of the stress in response to the pilot hole would reduce the loading experienced by the fixation plate.
Materials and Methods
HTO opening protocol
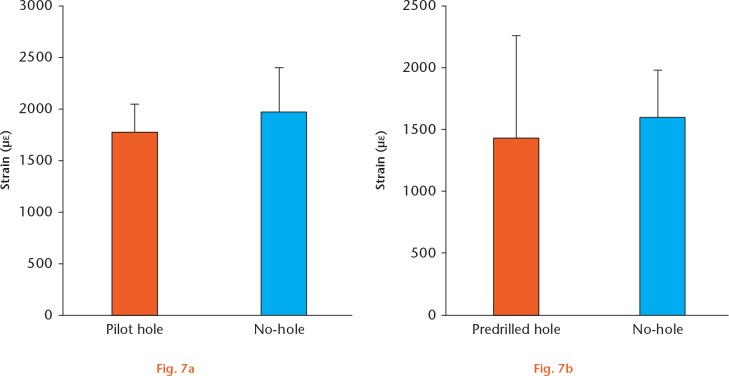
A total of 7 paired (n = 14; both tibiae from a single donor) fresh-frozen cadaveric tibias (all male with a mean age of 48 years (sd 4.5), mean weight of 76 kg (sd 20), and mean height of 1.8 m (sd 0.07) were used for testing in the current study. The specimens were screened for bone affecting disorders (e.g. kidney disease, metastatic cancers) and were scanned using dual radiograph absorptiometry to rule out osteoporosis. All the surgical procedures described were performed by a fellowship-trained orthopaedic surgeon (AG) with expertise in performing high tibial osteotomy (HTO). The paired specimens were randomized using a random number generator (Microsoft Excel, Microsoft, Redmond, Washington) to either a pilot hole condition (n = 7) or a no-hole (n = 7) condition. A 20 mm × 1.5 mm oscillating saw (0.5 teeth per mm, ConMed Corporation, Utica, New York) was used to create an oblique cut, without irrigation, that was initiated 4 cm below the medial tibial plateau and extended to 1 cm from the lateral cortex and 1.5 cm below the lateral tibial plateau (Fig. 1).17 For the specimens in the pilot hole group, an additional step was included in the process. Following the osteotomy cut, a proprietary guide (SBM Inc, Winchester, Massachusetts) was placed over the apex (Fig. 1a) that allowed for the accurate placement and drilling of a 3.4 mm diameter hole (Figs 1a and 1b). All the osteotomy procedures for both groups were performed under the guidance of fluoroscopic imaging.
Fluoroscopic images of a) the resulting osteotomy cut and b) the pilot hole.
Prior to the opening of the osteotomy, a uniaxial strain gauge (Vishay Intertechnology, Inc., Malvern, Pennsylvania) was attached to the mid-lateral cortex of the tibia aligned with the longitudinal axis of the bone and in line with the surgical cut. The bone was prepared for the strain gauges through two rounds of sanding and surface cleaning/degreasing (M-prep 6% phosphoric acid conditioner (Vishay Intertechnology, Inc.) and M-prep 0.02% ammonium hydroxide, 0.05% trisodium phosphate, and 0.01% sodium tetraborate pentahydrate neutralizer (Vishay Intertechnology, Inc)) followed by gauge attachment using a single drop of strain gauge adhesive (M-bond 200; Vishay Intertechnology, Inc.) and a protective polyurethane coating (M-Coat; Vishay Intertechnology, Inc.). Once the strain gauge was attached, the osteotomy in both groups was slowly opened as is performed in the clinical setting (at the surgeon’s discretion) with a laminar spreader to 9 mm of medial wedge height/correction. The opening was then stabilized with a HTO compression fixation plate (Otis-C-Plus, SBM Inc, Winchester, Massachusetts) and secured in place with four locking screws (Fig. 2). To isolate the effect of the pilot hole, no posteromedial wedge or any type of bone graft was used to provide extra structural support to the construct.
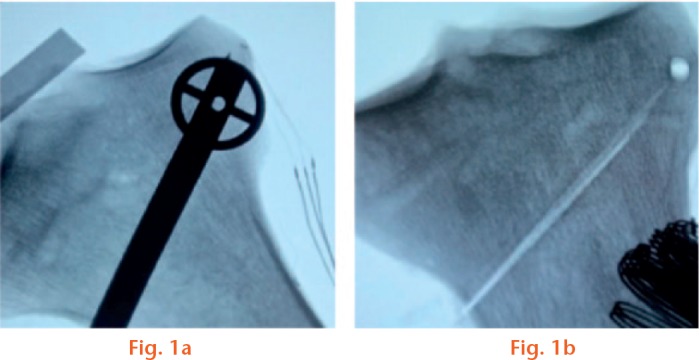
Fig. 2.
The tibia potted at 15° with respect to a composite femur (not shown) and with the osteotomy fixation plate shown on the medial aspect (inset). It should be noted that the white insert was only used to establish the width of the opening and was not left in for testing.
Once the osteotomy was performed, specimen preparation was continued by sectioning the distal end of the tibia and potting it into a section of polyvinyl chloride tubing using dental cement (Denstone Dental Cement, Hereaus Holdings GmbH, Hanau, Germany). The tibia was aligned at an angle of 15°, simulating 15° of knee flexion when aligned with a composite femur in the materials testing machine (Fig. 2). This angle was chosen as it has been shown to represent the position of peak external knee adduction moment.18 The strain gauge that was attached prior to the osteotomy opening remained on the lateral cortex to measure the lateral cortical hinge strains during cyclic loading. In addition, a second strain gauge was attached to the fixation plate aligned with the longitudinal axis of the plate. All gauges were wired independently into a quarter bridge completion circuit (National Instruments NI-PXI 1050 and SCXI 1010; National Instruments, Austin, Texas) and data was acquired at 10 kHz using a custom designed LabView data collection program (Labview, National Instruments).
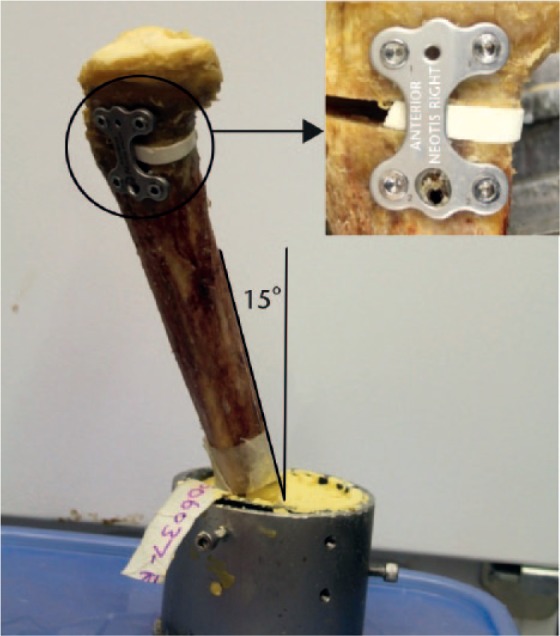
The potted tibias were rigidly secured to an Intsron materials testing machine (MTM) (Instron, Model 8874, Norwood, Massachusetts) via a previously designed multi-axis fixation jig.18 A standardized femoral template (Sawbones, Pacific Research Laboratories, Vashon Washington) was also potted and rigidly attached to the base of the MTM (Fig. 3). The tibia and femur were initially aligned visually, such that the medial and lateral condyles of the femur were in contact with the respective side of the tibial plateau when a 10 N load was applied. Small adjustments were then made by aligning a mark on the femur (midway between the condyles) with the middle of the intercondylar eminence of the tibia. Once the tibia was correctly positioned, the femur was adjusted to ensure that the tibia and femur articulating surfaces were aligned.
Fig. 3.
The experimental setup, including the multi-axis fixation jig within the materials testing machine.
Cyclic loading protocol
Once the specimens were secured in the MTM, they were subjected to a staircase cyclic loading protocol. The system initially applied a sinusoidal waveform between 200 N and 800 N at 1.8 Hz that was incrementally increased by 200 N every 5000 cycles, until failure or to a maximum force of 2400 N.19,20 The lower loads were used to simulate the mean ground reaction forces obtained from in vivo patient data,18 while the higher forces were used to determine the extreme values. Failure was defined as a breakage of the plate, the lateral cortical hinge, or a complete fracture that resulted in segmental separation. A custom designed data collection program (LabVIEW 2008, National Instruments) collected axial force and strain data at a sampling rate of 10 Hz (National Instruments NI-PXI 1050 and SCXI 1010).
Data analysis and statistics
The peak strains were extracted from the strain-time profiles during the opening of the wedge. For the cyclic loading protocol, the peak strains during the 800 N cycle and the cycle at failure were also extracted. In addition, the strain rate during HTO opening was calculated to verify a standardized opening protocol between specimens had occurred. A one-tailed, paired student’s t-test was used to compare the strains and strain rates produced by the pilot hole and no-hole condition during the osteotomy procedure. The strains from the lateral cortex and fixation plate were compared between the pilot hole and no-hole conditions during the cyclic loading procedure, also with a paired student’s t-test. Statistical analysis was performed using SPSS statistical software (IBM SPSS statistics version 21, IBM Corp., Armonk, New York) and α was set at 0.05 for all tests. Finally, post-hoc effect sizes and power were calculated using the means and SD of each group (G*power 3.1; Universitat Kiel, Germany)
Results
Fracture patterns during HTO opening
Overall, four visible fractures were identified in the pilot hole tibiae and five were identified in the tibiae with no hole. A consistent pattern of fracture was noticed during the opening of the osteotomy, such that a crack travelled toward the lateral cortex (Fig. 4) with fractures most evident on the posterior aspect of the tibia.
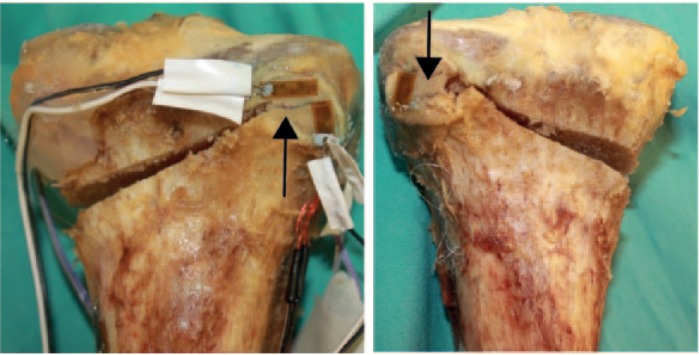
Examples of the common fracture patterns resulting from the opening of the osteotomy; a) no-hole condition and b) pilot hole condition. Both figures show the propagation of a crack from a) the apex of the cut and b) the edge of the hole laterally through the tibiofibular joint surface towards the cortical hinge.
Strains during HTO openings
Strain rates of 0.00238 (0.0020) ε/s and 0.0024 (0.0015) ε/s were calculated for the pilot hole and no-hole conditions, respectively; the difference between the groups was not significant (p = 0.376; Effect Size (ES) = 0.30; power = 0.27), confirming a consistent strain rate during opening between the groups. There was also no statistically significant difference between the mean strain measured at the lateral cortex when a pilot hole was used compared with the no-hole condition (Fig. 5) (p = 0.169; ES = 0.57; power = 0.68).
Fig. 5.
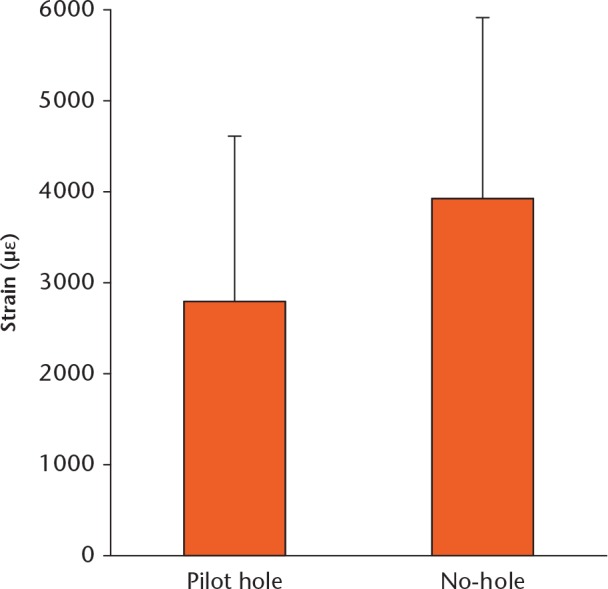
Comparison of the Mean (sd) lateral cortex strains during the opening of the high tibial osteotomy between the pilot hole (n = 7) and no-hole condition (n = 7).
Fractures and strain during loading
Of the fourteen specimens, only six (three pilot hole specimens and three no-hole specimens) were subjected to cyclic loading, as the remaining eight all had substantial and visible fractures from the HTO opening phase of the study. Of these, three fractured within the first 15 cycles of the initial 800 N load cycle, while the three remaining tibias failed near the end of the first round of the loading protocol. There were two common fracture patterns seen in these specimens. The first was an assumed propagation of a pre-existing crack that was only visible on fluoroscopy at the time of osteotomy creation that extended through the lateral cortex (Fig. 6a), while the second was a shearing off of the lateral cortex (Fig. 6b).
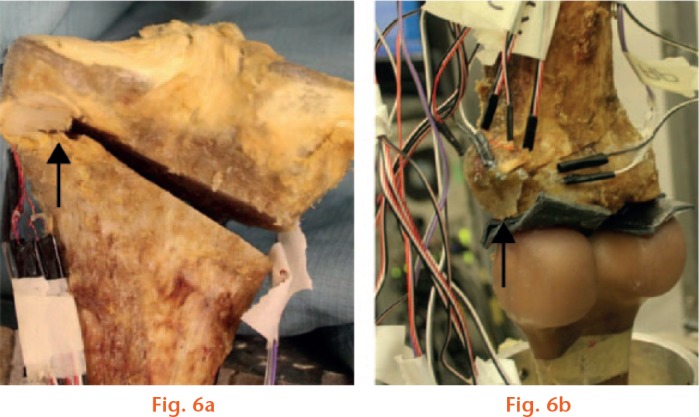
Typical fracture patterns after cyclic loading. a) Propagation of the crack through to the lateral cortex and b) shearing of the lateral cortex.
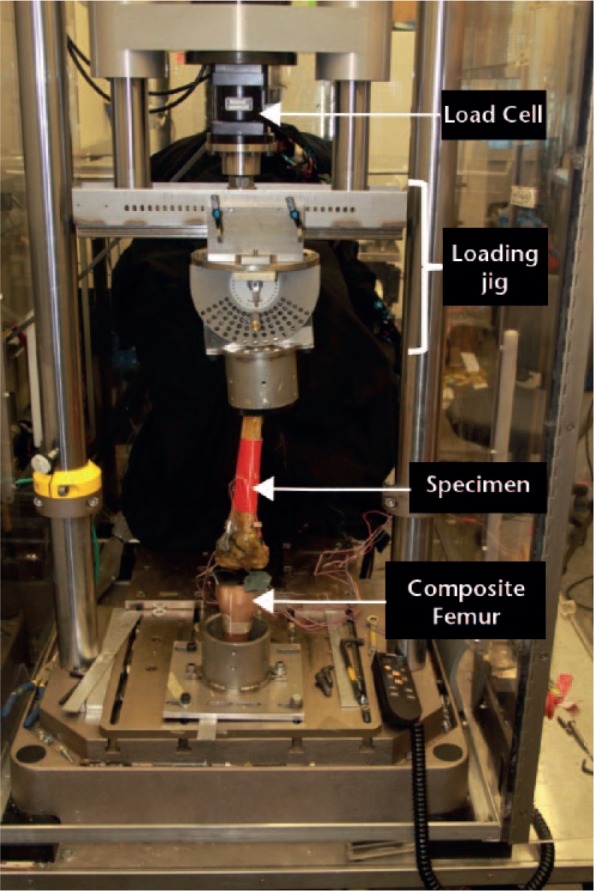
The mean axial strains at the lateral cortex (Fig. 7a) and the fixation plate (Fig. 7b), when exposed to the 800 N load cycle, were not significantly different between the pilot hole and no-hole conditions (cortex strains, p = 0.317; ES = 0.58; power = 0.38; fixation plate strains, p = 0.421; ES = 0.32; power = 0.19).
Comparison of the mean (SD) strains corresponding to the 800N cyclic loading protocol between the pilot hole (n = 3) and no-hole conditions (n = 3). Strains were measured at a) the lateral cortex and b) the fixation plate and there were no significant differences between conditions at either the lateral cortex or the fixation plate.
Discussion
The purpose of this investigation was to determine whether a pilot hole could reduce the strains and thus the risk of fracture at the lateral cortex hinge during the opening of an HTO and in response to cyclic loading. The data suggests that the implementation of a pilot hole at the apex of the osteotomy does not significantly reduce the strain at the lateral cortex hinge during HTO opening in either scenario. This is relevant as there are some commercial HTO systems that are currently utilizing this approach, despite the lack of quantitative evidence.
It is theorized that the implementation of a hole could reduce the stress concentration at the apex of the osteotomy by increasing the radius at the tip of the cut. Although this technique is a novel application in bone it is used routinely to prevent the propagation of a crack in glass (e.g. window panes).13 In the specimens where failure occurred during the opening of the osteotomies, the fracture was initiated at the lateral cortex and was directed laterally and distally (Fig. 4) toward the proximal tibiofibular joint; such a fracture is representative of a moderate severity, type II osteotomy fracture classification.10,11 This pattern is also consistent with the interpretation that the osteotomy is a crack in the bone and that, during the wedge opening, the crack continues to propagate in the direction of the applied force.14 However, contrary to the hypothesis, the pilot hole did not significantly reduce the strain at the lateral cortex, or the incidence of fracture during the wedge opening. This may have occurred because rather than reducing the stress at the apex of the osteotomy, the pilot hole merely translated the stress concentration laterally to a parallel point on the surface of the hole.14 The nonsignificant reduction in strain may have occurred because the pilot hole decreased the width of the lateral hinge (i.e. less bone material between the apex and cortex), thereby increasing the flexure and reducing the rigidity of the hinge;21 the thinner hinge aids to reduce the strain but weakens the lateral cortex when loaded.
In a previous study, Kessler et al16 could achieve an additional 3° of osteotomy closure when a pilot hole was used in a medial closing wedge osteotomy. However, during a closing wedge osteotomy, the pilot hole is subjected to primarily compressive loading, compared with the tensile loading experienced during an opening-wedge osteotomy, as investigated in the current work. It is well established that a hole improves the strength of a material in compression compared with tension.22 Furthermore, although it is commonly referred to as a hole,16,17 the osteotomy is cut into it forming a circular notch that, although it decreases the stress distribution marginally better than a sharp angled notch, does not reduce the stress concentration as well as a hole.23
During cyclic loading, all the specimens failed at the lateral cortex either due to a crack that was assumed to propagate or due to lateral cortex shearing (Fig. 6). The shearing of the lateral cortex presents a possible source of failure that may have been directly related to the implementation of the hole, as described above (i.e. the pilot hole infringes on the lateral cortex). Additionally, the purpose of a medial opening wedge HTO is to redistribute a portion of the patient’s body weight to the lateral aspect of the knee.24 Therefore, the extra load, coupled with the thin hinge, may have produced the shearing pattern in the failed HTOs. These patterns of failure are consistent with those presented by Stoffel et al,25 who tested a fixation system that employed a pilot hole.
The pilot hole resulted in an insignificant strain reduction at the lateral cortex and the fixation plate during cyclic loading, which could be due to the hole creating an environment in the bone similar to the environment that is created by the pores that are present in brittle, ceramic-like materials. Brittle materials are strong under compression because they tend to have large cracks or pores in their molecular structure that close when compression is applied.13 The collapsing of the hole recreates the notch at the lateral apex of the osteotomy, subsequently reproducing the stress concentration that the hole was intended to prevent.
Limitations of the study include the fact that the cadaveric specimens used in the current investigation did not have a varus deformity prior to the osteotomy. Therefore, after the osteotomy procedure, the tibias were overcorrected. This problem was mitigated during the potting phase of the procedure, where the lateral aspect of the tibia was adjusted to create a level tibial plateau. With respect to the placement of the strain gauges, although the stress would most likely be concentrated at the apex of the osteotomy, during pilot testing it was revealed that the complex topography of the tibia in this region made it difficult and unreliable to place a strain gauge at this location. However, given that fracture during mHTO opening most commonly propagates towards, and ends at, the lateral aspect of the tibia, the placement of the strain gauges in the current investigation, combined with the observed fracture patterns, provide a relatively reliable assessment of the effect of pilot hole use. Furthermore, the current study made use of paired tibias to overcome the limitations associated with testing cadaveric bones. Although this was a relatively small sample, the calculated power (0.65) and effect size (0.57) for the strains during opening were moderate and large, respectively, and on their own might be suggestive of a meaningful difference. Furthermore, it should be noted that the reduction to six specimens for the cyclic loading may affect the application of the findings; these quantitative data should be analyzed carefully. However, these data should be interpreted in combination with the number and type of fracture patterns that were realized within each group. These numbers would further suggest that including a pilot hole is not an effective method for reducing the occurrence of complications during mHTO surgery such as lateral cortical fracture. In fact, including the pilot hole resulted in type II fracture patterns during HTO opening and type III patterns during cyclic loading,10-12 both of which are accompanied with additional complications.
There are also differences between cadaveric and in vivo tibias that should be considered. First, during this experiment there was no opportunity for tissue healing, which occurs in vivo. After an actual osteotomy, the patient would be advised to use assistive devices, reducing weight-bearing, and may not return to full activity for six months or longer.26 Therefore, the cyclic loading applied in the current investigation is representative of weight-bearing immediately post operation, which, depending upon the fixation device used, may not be entirely representative of the clinical scenario. Another consideration is that the testing was performed without the presence of the supporting structures of the knee, such as muscles, tendons, and ligaments, which help to increase knee joint stability.24 Therefore, the data presented here should be interpreted as a ‘worst-case scenario’, and offers a conservative estimate of the effect of these surgical procedures.
This study suggests that the implementation of a pilot hole does not significantly reduce the lateral strains during the opening of an osteotomy. The pilot hole was also not successful in decreasing the number of fractures that occurred at the lateral cortex. Therefore, caution should be taken when using HTO fixation systems that use a pilot hole near the lateral cortex.
Footnotes
Author Contributions: K. Bujnowski: Experimental Design, Data collection and Analysis, Manuscript preparation and revision.
A. Getgood: Experimental Design, Manuscript Preparation and Revision.
K. Leitch: Experimental Design, Manuscript Preparation and Revision.
J. Farr: Experimental Design, Manuscript Preparation and Revision.
C. Dunning: Experimental Design, Manuscript Preparation and Revision.
T. A. Burkhart: Experimental Design, Data collection and Analysis, Manuscript preparation and revision.
Conflict of Interest Statement: SBM provided in-kind support for this project
Funding Statement
The authors would like to thank the Canadian Institute of Health Research (CIHR) and the Natural Sciences and Engineering Council (NSERC) of Canada for providing funding for this project. The authors would also like to thank SBM Inc. (Winchester, Massachusetts) for their in-kind contribution of consumables for the study.
J. Farr and A. Getgood report funding received from several companies, none of which is related to this article.
References
- 1. Bombardier C, Hawker G, Mosher D. The Impact of Arthritis in Canada: Today and over the next 30 years. Artritis Alliance of Canada, 2011. [Google Scholar]
- 2. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 2010;468:57-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Khan M, Osman K, Green G, Haddad FS. The epidemiology of failure in total knee arthroplasty: avoiding your next revision. Bone Joint J 2016;98-B(suppl A):105-112. [DOI] [PubMed] [Google Scholar]
- 4. Von Keudell A, Sodha S, Collins J, et al. Patient satisfaction after primary total and unicompartmental knee arthroplasty: an age-dependent analysis. Knee 2014;21:180-184. [DOI] [PubMed] [Google Scholar]
- 5. Lee DC, Byun SJ. High tibial osteotomy. Knee Surg Relat Res 2012;24:61-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wright JM, Crockett HC, Slawski DP, Madsen MW, Windsor RE. High tibial osteotomy. J Am Acad Orthop Surg 2005;13:279-289. [DOI] [PubMed] [Google Scholar]
- 7. Martin R, Birmingham TB, Willits K, et al. Adverse event rates and classifications in medial opening wedge high tibial osteotomy. Am J Sports Med 2014;42:1118-1126. [DOI] [PubMed] [Google Scholar]
- 8. Bonasia DE, Dettoni F, Sito G, et al. Medial opening wedge high tibial osteotomy for medial compartment overload/arthritis in the varus knee: prognostic factors. Am J Sports Med 2014;42:690-698. [DOI] [PubMed] [Google Scholar]
- 9. Ogawa H, Matsumoto K, Akiyama H. The prevention of a lateral hinge fracture as a complication of a medial opening wedge high tibial osteotomy: a case control study. Bone Joint J 2017;99-B:887-893. [DOI] [PubMed] [Google Scholar]
- 10. Nakamura R, Komatsu N, Murao T, et al. The validity of the classification for lateral hinge fractures in open wedge high tibial osteotomy. Bone Joint J 2015;97-B:1226-1231. [DOI] [PubMed] [Google Scholar]
- 11. Takeuchi R, Ishikawa H, Kumagai K, et al. Fractures around the lateral cortical hinge after a medial opening-wedge high tibial osteotomy: a new classification of lateral hinge fracture. Arthroscopy 2012;28:85-94. [DOI] [PubMed] [Google Scholar]
- 12. Nakamura R, Komatsu N, Fujita K, et al. Appropriate hinge position for prevention of unstable lateral hinge fracture in open wedge high tibial osteotomy. Bone Joint J 2017;99-B:1313-1318. [DOI] [PubMed] [Google Scholar]
- 13. Groover MP. Fundamentals of Modern Manufacturing: materials, processes and systems. Fourth ed. Hoboken, NJ: John Wiley & Sons Inc, 2010. [Google Scholar]
- 14. Schijve J. Fatigue of Structures and Materials. Second ed. New York: Springer, 2009. [Google Scholar]
- 15. Lützner J, Kasten P, Günther KP, Kirschner S. Surgical options for patients with osteoarthritis of the knee. Nat Rev Rheumatol 2009;5:309-316. [DOI] [PubMed] [Google Scholar]
- 16. Kessler OC, Jacob HA, Romero J. Avoidance of medial cortical fracture in high tibial osteotomy: improved technique. Clin Orthop Relat Res 2002;395:180-185. [DOI] [PubMed] [Google Scholar]
- 17. Getgood A, Collins B, Slynarski K, et al. Short-term safety and efficacy of a novel high tibial osteotomy system: a case controlled study. Knee Surg Sports Traumatol Arthrosc 2013;21:260-269. [DOI] [PubMed] [Google Scholar]
- 18. Leitch KM. Biomechanical Investigations of Medial Opening Wedge High Tibial Osteotomy: Gait Analysis, Materials Testing and Dynamic Radiography. The University of Western Ontario, 2014, https://ir.lib.uwo.ca/etd/1981/ [Google Scholar]
- 19. Maas S, Diffo Kaze A, Dueck K, Pape D. Static and Dynamic Differences in Fixation Stability between a Spacer Plate and a Small Stature Plate Fixator Used for High Tibial Osteotomies: A Biomechanical Bone Composite Study. ISRN Orthop 2013;2013:387620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Agneskirchner JD, Freiling D, Hurschler C, Lobenhoffer P. Primary stability of four different implants for opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2006;14:291-300. [DOI] [PubMed] [Google Scholar]
- 21. Hibbeller RC. Mechanics of Materials. Eighth ed Boston, Massachusetts: Pearson, 2004. [Google Scholar]
- 22. Gibson RF. Fatigue of Composite Materials. Third ed Lancaster, Pennsylvania: DEStech Publications Inc, 2013. [Google Scholar]
- 23. Young WC, Budynas RG. Stress Concentration. In: Roarks’s Formulas for Stress and Strain. Eighth ed. Columbus, Ohio: McGraw Hill, 2002:259. [Google Scholar]
- 24. Birmingham TB, Kramer JF, Kirkley A, et al. Association among neuromuscular and anatomic measures for patients with knee osteoarthritis. Arch Phys Med Rehabil 2001;82:1115-1118. [DOI] [PubMed] [Google Scholar]
- 25. Stoffel K, Stachowiak G, Kuster M. Open wedge high tibial osteotomy: biomechanical investigation of the modified Arthrex Osteotomy Plate (Puddu Plate) and the TomoFix Plate. Clin Biomech (Bristol, Avon) 2004;19:944-950. [DOI] [PubMed] [Google Scholar]
- 26. Wolcott M, Traub S, Efird C. High tibial osteotomies in the young active patient. Int Orthop 2010;34:161–166. [DOI] [PMC free article] [PubMed] [Google Scholar]