Abstract
Objective
Individuals with substance use disorders are at high risk for hospital readmission. This study examined whether targeted follow-up services received within 14 days postdischarge from an inpatient hospital stay or residential detoxification reduced readmissions within 90 days, among Medicaid beneficiaries who had an index substance use disorder diagnosis.
Methods
Claims data were analyzed for Medicaid beneficiaries aged 18–64 years with a substance use disorder diagnosis coded as part of an inpatient hospital stay or residential detoxification in 2008 (N=30,439). Follow-up behavioral health services included residential, intensive outpatient, or outpatient treatment, and/or medication-assisted treatment (MAT). Analyses included 10 states or fewer based on a minimum number of index admissions and prevalence of follow-up services or MAT. Survival analyses with time-varying independent variables were used to test the association of follow-up services and MAT with behavioral health readmissions.
Results
Two-thirds of individuals with an index admission had no follow-up services within 14 days. Behavioral health admissions 90 days postdischarge were present for 29% of individuals with an index admission. Survival analyses showed that MAT and residential treatment were associated with reduced risk of behavioral health admission in the 90 days postdischarge. However, outpatient was associated with increased risk of readmission, as was intensive outpatient in one model.
Conclusions
Provision of MAT or residential treatment for substance use disorders after an inpatient or detoxification stay may help prevent future readmissions. Medicaid programs should be encouraged to reduce barriers to MAT and residential treatment to prevent future behavioral health admissions.
INTRODUCTION
Reducing hospital readmissions is an increasing focus of health care quality improvement and cost-reduction strategies.1 Readmission rates for individuals with substance use disorders are relatively high (18–26%).2 Having a substance use disorder is linked to greater complexity of care and hospital-related complications, longer lengths of stay, and greater likelihood of readmissions even when addiction treatment is not the reason for hospitalization.3–8 Further, they are associated with other health consequences and higher health services costs.3,9,10 Among Medicaid beneficiaries, alcohol and drug use disorders were among the top ten conditions with the most all-cause 30-day readmissions.2 For Medicaid beneficiaries with a mental disorder, a comorbid substance use diagnosis is a major predictor of readmissions.11–14
Medicaid patients and providers have identified inadequate planning and unsuccessful follow-up care as root causes of high readmission rates.10,15 For individuals with a substance use disorder, prompt receipt of follow-up treatment services or medication-assisted treatment (MAT) after an inpatient hospital discharge or a detoxification stay could be expected to reduce readmission rates. Residential, intensive outpatient and outpatient addiction treatment services are effective in reducing substance use and its consequences.16–19 Less is known about their impact on readmissions.
Medicaid beneficiaries with comorbid mental and substance use disorders had a reduced likelihood of readmission in hospitals where a higher proportion of patients received outpatient mental health treatment within 7 days after hospital discharge.12 Receiving addiction treatment soon after discharge is associated with reduced detoxification readmission,20,21 with stronger findings for residential than outpatient.21
This study examined whether Medicaid beneficiaries with a substance use disorder diagnosis who received targeted follow-up services (outpatient, intensive outpatient, or residential treatment) or MAT after an index hospital inpatient stay or residential detoxification had a lower likelihood of postdischarge behavioral health hospital or detoxification admission within 90 days than individuals who did not receive follow-up services. Findings from this study should be valuable as decisions are made about which services Medicaid and other payers should cover and how to improve care for their enrollees.
METHODS
Data
Data were from four component files of the 2008 Medicaid Analytic eXtract data set:22 personal summary (PS) for beneficiary characteristics and enrollment status, inpatient (IP) for hospital services, other therapy (OT) for detoxification and follow-up services, and prescription (RX), linked by a unique beneficiary identifier by state. Although data were from 2008, the relationship between follow-up services and postdischarge behavioral health readmissions is not expected to change over time. Analyses used de-identified data, thus were exempt from IRB review.
Sample
The first (index) inpatient hospital admission with a substance use disorder diagnosis or residential detoxification admission, between 4/1/2008 and 9/1/2008, was included for individuals aged 18–64 years (N=30,439). Presence of a substance use disorder was determined by an ICD-9 diagnostic code for substance abuse or dependence in any position for an inpatient hospital admission or by a residential detoxification. All diagnoses (not just primary) were considered because with serious co-occurring disorders, it is not always clear which would be designated as primary; further, stigma may lead to a decision not to put substance use disorder diagnoses as primary. If substance use disorder is noted at all, it is important given common medical complications, as well as the need for addiction treatment services. Of the 30,439 admissions in the sample, 30.8% had a substance use disorder as the primary diagnosis.
Excluded were individuals enrolled in both Medicaid and Medicare or enrolled in managed care plans (because of likely incomplete claims data). Also excluded were individuals not continuously enrolled in Medicaid 90 days before and after their index admission, and who only had substance use disorder diagnoses of nicotine/tobacco use disorder, marijuana abuse, or hallucinogen abuse.
Data were included from 10 states based on a minimum number of index admissions and prevalence of follow-up services or MAT: Connecticut, Illinois, Indiana, Minnesota, Missouri, North Carolina, New York, West Virginia, Wisconsin and Vermont. Thirty-seven states were excluded that had fewer than 650 index admissions, indicating no or few fee-for-service claims; 3 states were excluded in which none of the follow-up services were received by at least 5% of index admissions. In the 10 states that remained, an average of 82% Medicaid enrollees were excluded due to their dual Medicaid/Medicare eligibility or participation in managed care plans23 (see Appendix for details by state).
Variables
The outcome was time to a behavioral health admission in the 90 days following discharge from the index admission. For all follow-up services, eligible diagnoses were broadened to include both substance use and mental disorders, given overlap in clinical needs and treatment approaches. A postdischarge behavioral health admission was thus defined as an inpatient admission with a primary diagnosis of a substance use or mental disorder or a residential detoxification admission. For readmission, only primary diagnosis was used, to emphasize a behavioral health admission and better indicate the effect of follow-up services on the substance use disorder itself.
Four key independent variables were created, each within 14 days of discharge from the index admission; a 14-day period indicates good clinical care by minimizing time outside of treatment.21 Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes, place of service, and primary substance use or mental disorder diagnosis were used to identify residential behavioral health treatment (RES), excluding detoxification; partial hospital or intensive outpatient program (IOP); outpatient behavioral health services (OP); and MAT, defined as a prescription fill of buprenorphine, disulfiram, acamprosate, or naltrexone or a HCPCS service code for methadone, buprenorphine, or naltrexone.
The number of days to the first follow-up service received within 14-days postdischarge was calculated. Service receipt could begin on the day of discharge (day 0). Because follow-up services could occur at any point in the 14-day window, the opportunity to observe a postdischarge behavioral health readmission varied. To address this, each follow-up service was coded as a series of time-varying independent variables from day 0 to day 14 for the survival analysis models. Once a follow-up service was received, the remainder of the 14 days was coded as having received that service. For the few who received 2 or 3 follow-up service types (excluding MAT), an episode approach coded only the most intensive service (RES then IOP then OP), starting on the first day of any services received.
Covariates were basis of Medicaid eligibility (disability vs. other), demographics (age, sex, race/ethnicity), mental or physical comorbidities at index admission, type of substance use disorder (alcohol only, any opioid use disorder), index admission length of stay (days), and use of behavioral health services or MAT in the 90 days prior to index admission.
Analyses
Available follow-up services varied by state, depending on Medicaid coverage in that state. Three models were run to account for each pattern of services: Model 1 - OP and MAT in all 10 states; Model 2 - OP, MAT and IOP in Indiana, Missouri, Connecticut, Vermont, and Minnesota only; and Model 3 - OP, MAT, IOP and RES in Connecticut, Vermont, and Minnesota only. Index admission was the unit of analysis.
Cox proportional hazards regression models were used to estimate the effect of follow-up services and MAT on time to a behavioral health admission after discharge, with censoring at 90 days. Hazard ratios (HRs) are interpreted similarly to odds ratios, showing at any point in time in the 90 days after discharge whether an individual receiving the follow-up service within 14 days was more (HR >1) or less (HR < 1) likely to have a behavioral health admission than an individual not receiving the service within 14 days. Models included all covariates. State was included as a fixed effect, to account for differences in population, Medicaid eligibility, other Medicaid covered services, and other unobserved variations. Analyses were conducted in SAS v9.3.
RESULTS
Characteristics of Sample and Index Admissions
Table 1 describes the sample and highlights the often-wide variations across states as indicated by the minimum and maximum percentages by state (see Appendix for by-state findings). Comorbid mental disorders were prevalent in about half of admissions and physical comorbidities in about two-thirds. Medicaid eligibility was usually due to a disability (66.6%) overall, but this varied widely across states (24.5% to 97.5%). A substantial minority of index admissions (21.1%) had only an alcohol use disorder coded without any drug use disorder, and 27.3% had an opioid use disorder coded, regardless of other substance use disorder diagnoses. Behavioral health service use 90 days prior to the index admission was fairly uncommon for MAT (5.1%) and inpatient (13.1%); however, over a quarter used outpatient in that time period. The mean index admission length of stay was 6.0 days (not shown).
Table 1.
Characteristics of Medicaid Patients with Substance Use Disorders and Their Index Admissions
| Total | By statea | ||||
|---|---|---|---|---|---|
|
| |||||
| Characteristic | N | % | Mean % | Min % | Max % |
| Total patients with an index admission (N) | 30,439 | 100.0 | |||
| Sex | |||||
| Male | 17,114 | 56.2 | 52.0 | 38.7 | 66.6 |
| Female | 13,325 | 43.8 | 48.0 | 33.4 | 61.3 |
| Race/ethnicity | |||||
| White | 13,121 | 43.1 | 59.2 | 29.5 | 94.3 |
| Black | 11,939 | 39.2 | 25.2 | 1.2 | 57.2 |
| Hispanic | 3,733 | 12.3 | 6.9 | .1 | 25.3 |
| Other | 590 | 1.9 | 3.1 | .1 | 16.1 |
| Unknown | 1,056 | 3.5 | 8.3 | .5 | 49.0 |
| Age | |||||
| 18–39 | 10,174 | 33.4 | 37.3 | 25.1 | 61.7 |
| 40–59 | 18,527 | 60.9 | 56.9 | 34.8 | 67.2 |
| 60–64 | 1,738 | 5.7 | 5.8 | 3.5 | 8.2 |
| Comorbidities | |||||
| Mental disorder | 15,438 | 50.7 | 53.6 | 39.0 | 65.3 |
| Physical | 20,519 | 67.4 | 66.0 | 34.2 | 79.4 |
| Basis of Medicaid eligibility | |||||
| Disability | 20,276 | 66.6 | 73.4 | 24.5 | 97.5 |
| Other | 10,163 | 33.4 | 26.6 | 2.5 | 75.5 |
| Substance use diagnosis at index | |||||
| Alcohol only | 6,427 | 21.1 | 25.3 | 17.1 | 34.3 |
| Any opioid use disorder | 8,300 | 27.3 | 22.6 | 11.1 | 35.8 |
| Prior behavioral health servicesb | |||||
| Medication-assisted treatment | 1,547 | 5.1 | 8.0 | 1.9 | 22.9 |
| Inpatient | 4,000 | 13.1 | 9.3 | 4.6 | 17.0 |
| Outpatient | 7,882 | 25.9 | 25.4 | 18.5 | 35.1 |
Percentages calculated by state, then mean %, minimum % and maximum percent calculated across the 10 states.
Services that were received in the 90 days before the index admission.
Source: 2008 Medicaid Analytic eXtract (MAX)
Follow-up Services Within 14 Days of Discharge
Three-quarters of individuals with an index admission had no RES, IOP or OP service in the 14 days postdischarge (Table 2), but this varied by state (49.9% to 83.4%). Few individuals received postdischarge RES (8.3%) or IOP services (5.5%) in the states that offered them; OP services were received by 22.8% of individuals and MAT by 10.4%. The proportions receiving specific services also ranged across states. When including receipt of MAT, two thirds of individuals with an index admission did not have either a follow-up service or MAT within the 14-day window. See Appendix for by-state findings.
Table 2.
Characteristics of Behavioral Health Follow-Up Services Within 14 Days of Discharge and Inpatient Admissions Within 90 Days of Discharge
| Total | By state | ||||
|---|---|---|---|---|---|
|
| |||||
| Characteristic | N | % | Mean % | Min % | Max % |
| Total patients with an index admission (N) | 30,439 | 100.0 | |||
| Follow-up services 14 days postdischarge | |||||
| RESb | 276 | 8.3 | 11.7 | 2.1 | 29.1 |
| IOPb | 372 | 5.5 | 4.9 | 2.0 | 7.8 |
| OP (excludes IOP) | 6,929 | 22.8 | 20.1 | 15.4 | 27.6 |
| No RES, IOP or OP service | 22,862 | 75.1 | 73.9 | 49.9 | 83.4 |
| Follow-up MAT 14 days postdischarge | 3,155 | 10.4 | 10.8 | 3.2 | 26.2 |
| No RES, IOP, OP or MAT service | 20,599 | 67.7 | 67.3 | 38.7 | 79.6 |
| Time to first follow-up service (RES, IOP, OP or MAT)c | |||||
| 0 day | 1,944 | 6.4 | 7.4 | 3.1 | 12.5 |
| 1 day | 1,554 | 5.1 | 6.0 | 3.0 | 22.6 |
| 2 day | 981 | 3.2 | 2.8 | 1.5 | 5.5 |
| 3 day | 802 | 2.6 | 2.3 | 1.0 | 3.9 |
| 4 day | 829 | 2.7 | 2.4 | 1.0 | 5.2 |
| 5 day | 682 | 2.2 | 1.8 | .8 | 3.5 |
| 6 day | 729 | 2.4 | 2.0 | .8 | 3.8 |
| 7 day | 400 | 1.3 | 1.4 | .8 | 2.2 |
| 8 day | 353 | 1.2 | 1.1 | .6 | 1.6 |
| 9 day | 303 | 1.0 | 1.0 | .3 | 1.7 |
| 10 day | 296 | 1.0 | 1.0 | .6 | 1.3 |
| 11 day | 258 | .8 | 1.0 | .5 | 1.8 |
| 12 day | 231 | .8 | .8 | .4 | 1.1 |
| 13 day | 248 | .8 | .9 | .6 | 1.3 |
| 14 day | 230 | .8 | .9 | .6 | 1.4 |
| Inpatient admission 90 days postdischarge | |||||
| Any | 14,702 | 48.3 | 42.1 | 32.9 | 54.8 |
| Behavioral health | 8,918 | 29.3 | 23.9 | 13.5 | 36.7 |
| Time to behavioral health inpatient admission | |||||
| < 7 days | 3,764 | 12.4 | 10.3 | 2.6 | 27.2 |
| 7–14 days | 1,103 | 3.6 | 2.7 | 1.2 | 4.7 |
| 15–30 days | 1,429 | 4.7 | 3.7 | 2.2 | 6.3 |
| 31–60 days | 1,589 | 5.2 | 4.2 | 2.0 | 6.2 |
| 61–90 days | 1,033 | 3.4 | 3.0 | 1.7 | 4.3 |
| No inpatient admission | 21,521 | 70.7 | 76.1 | 63.3 | 86.5 |
Abbreviations: IOP, intensive outpatient; MAT, medication-assisted treatment; OP, outpatient; RES, residential
Percentages calculated by state, then mean %, minimum % and maximum percent calculated across the 10 states.
Denominator for Total % is total admissions across states with service
For the few individuals who received more than one of the IOP, OP, or RES follow-up services (excluding MAT), an episode approach was used where only the most intensive service was coded.
Source: 2008 Medicaid Analytic eXtract (MAX)
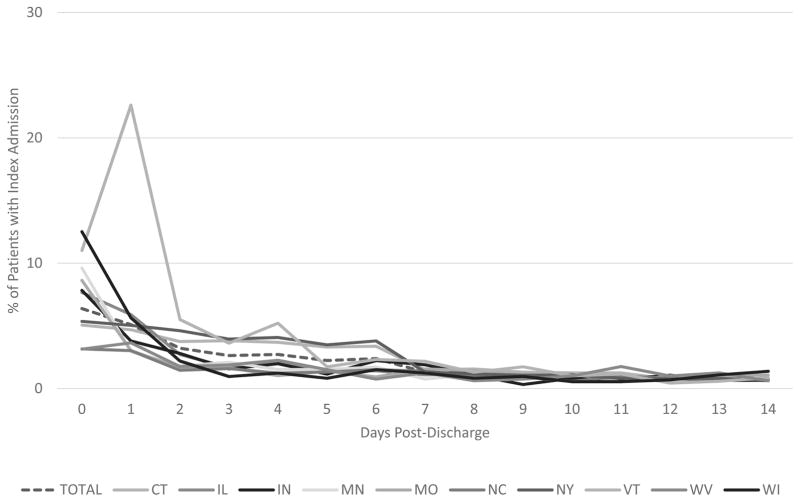
Of those who received a service, it most frequently started on the day of discharge or the two days following, with frequency of first service use declining each day thereafter. Figure 1 illustrates the time to first behavioral health follow-up service, overall (dotted line) and by state. The most variation by state occurs in the first 2 days postdischarge.
Figure 1.
Days to first behavioral health follow-up service (OP, IOP, RES, or MAT), overall and by state
Inpatient Readmissions Within 90 Days of Discharge
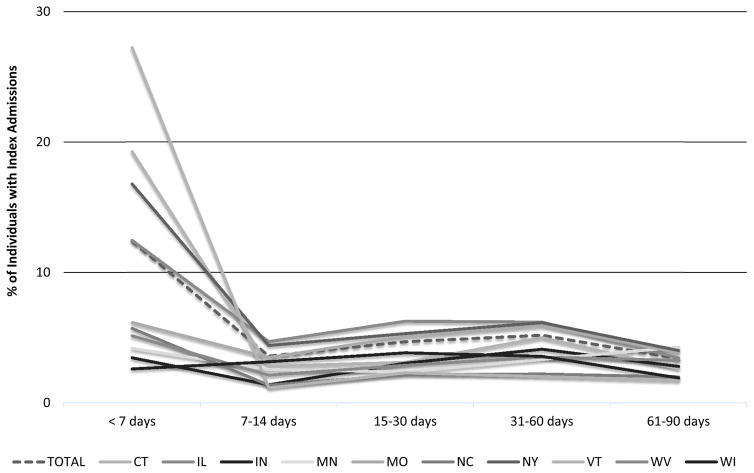
Hospital readmissions for any cause were common (48.3%) in the 90-day postdischarge period (Table 2) as were readmission rates when considering only readmissions with a primary behavioral health diagnosis (29.3%). Postdischarge readmissions occurred throughout the 90-day period, though were most likely within the first week postdischarge. As shown in Figure 2, in several states a substantial proportion of individuals had behavioral health readmissions within the first 7 days, whereas in other states behavioral health readmissions occurred more evenly throughout the time period studied. About 70% of individuals overall had no behavioral health readmission in the 90 days postdischarge.
Figure 2.
Time to behavioral health inpatient admission or detoxification 90 days post-discharge, overall and by state
Hazard of Behavioral Health Admission Within 90 Days of Discharge
Table 3 reports the hazard of a behavioral health admission within 90 days of discharge. Model 1 includes all 10 states and only OP and MAT services. OP receipt in the 14 days postdischarge is associated with a higher hazard of readmission in the 90 days postdischarge (HR=1.40, p<.001). MAT is associated with a lower hazard of readmission (HR=.61, p<.001). As expected, states were significant predictors of a behavioral health admission 90 days postdischarge. Most covariates were significant, with the exception of Medicaid eligibility and race/ethnicity is Hispanic, other or unknown.
Table 3.
Hazard ratios for the time to a behavioral health admission within 90 days postdischarge, by available followup services
| Model #1: OP, MAT (N=30,439) | Model #2: OP, MAT, IOP (N=6,787) | Model #3: OP, MAT, IOP, RES (N=3,339) | ||||
|---|---|---|---|---|---|---|
| Independent variables | Hazard ratio | 95% confidence interval | Hazard ratio | 95% confidence interval | Hazard ratio | 95% confidence interval |
| Follow-up servicesb | ||||||
| OP | 1.40** | 1.32–1.48 | 1.40** | 1.21–1.61 | 1.45* | 1.15–1.81 |
| MAT | .61** | .56–.67 | .60** | .48–.74 | .54** | .41–.73 |
| IOP | 1.06 | .84–1.35 | 1.45* | 1.03–2.04 | ||
| RES | .50** | .33–.76 | ||||
|
| ||||||
| State (reference: VT) | ||||||
| CT | .96 | .82–1.12 | 1.10 | .92–1.31 | 1.09 | .90–1.31 |
| IL | .75** | .65–.87 | -- | -- | -- | -- |
| IN | .41** | .34–.51 | .44** | .36–.56 | -- | -- |
| MN | .47** | .39–.58 | .53** | .42–.67 | .63** | .49–.80 |
| MO | .52** | .45–.61 | .55** | .46–.66 | -- | -- |
| NC | .39** | .33–.46 | -- | -- | -- | -- |
| NY | 1.00 | .87–1.15 | -- | -- | -- | -- |
| WI | .44** | .34–.55 | -- | -- | -- | -- |
| WV | .47** | .38–.58 | -- | -- | -- | -- |
|
| ||||||
| Basis of Medicaid eligibility is other than disabled (reference: disabled) | .99 | .94–1.04 | .86 | .74–1.00 | .86 | .72–1.01 |
|
| ||||||
| Female (reference: male) | .79** | .76–.83 | .76** | .68–.84 | .75** | .66–.86 |
|
| ||||||
| Age (reference: 40–59) | ||||||
| 18–39 | .98 | .93–1.03 | 1.11 | 1.00–1.25 | 1.07 | .92–1.24 |
| 60–64 | .68** | .60–.77 | .48** | .34–.68 | .47** | .31–.72 |
|
| ||||||
| Race/ethnicity (reference: white) | ||||||
| Black | 1.13** | 1.08–1.19 | .90 | .79–1.03 | .87 | .72–1.06 |
| Hispanic | 1.05 | .98–1.13 | .76* | .62–.95 | .82 | .66–1.02 |
| Other | .91 | .76–1.10 | .82 | .57–1.20 | .81 | .55–1.19 |
| Unknown | .95 | .83–1.09 | .88 | .59–1.33 | .92 | .53–1.57 |
|
| ||||||
| Comorbidities | ||||||
| Mental disorder | 1.29** | 1.23–1.35 | 1.04 | .93–1.16 | .75** | .64–.88 |
| Physical | .57** | .54–.59 | .51** | .46–.57 | .40** | .34–.46 |
|
| ||||||
| Index admission length of stay | .95** | .95–.96 | .95** | .93–.96 | .95** | .93–.97 |
|
| ||||||
| Substance use diagnosis at index | ||||||
| Alcohol only | 1.25** | 1.19–1.33 | 1.27** | 1.13–1.44 | 1.50** | 1.26–1.78 |
| Any opioid use disorder | 1.34** | 1.27–1.41 | 1.29** | 1.13–1.47 | 1.36** | 1.14–1.62 |
|
| ||||||
| Prior behavioral health services | ||||||
| Medication-assisted treatment | 1.11* | 1.01–1.22 | 1.08 | .90–1.29 | .99 | .81–1.21 |
| Inpatient | 2.81** | 2.68–2.95 | 2.49** | 2.20–1.82 | 2.10** | 1.74–2.55 |
| Outpatient | 1.20** | 1.14–1.26 | 1.29** | 1.15–1.44 | 1.33** | 1.16–1.54 |
Two dashes (--) indicate that the services was not included in the available data for that state.
Cox proportional hazards regression models
Followup service represents behavioral health treatments that occurred within 14 days of discharge from the index admission
p<.05,
p<.001
Source: 2008 Medicaid Analytic eXtract (MAX)
Model 2 adds IOP, covered only by 5 states. OP and MAT services remain significant as in Model 1, but IOP is not a significant predictor of behavioral health admission in the 90 days postdischarge. State and covariate effects were similar to Model 1.
Model 3 includes all four services (OP, MAT, IOP, RES), covered only by 3 states. OP and MAT services remain significant as in Models 1 and 2. IOP is significantly related to higher risk of readmission (HR=1.45, p<.05). RES is significantly related to lower risk of readmission (HR=.50, p<.001). As before, most covariates are significant.
To determine if the patterns held when the included states were constant across models, sensitivity analyses examined Models 1 and 2 using only the same 3 states as in Model 3. With fewer states, IOP was significantly associated with higher risk or readmission in Model 2 as well as Model 3 (not shown).
DISCUSSION
This analysis found strong support for the value of rapid follow-up with MAT or residential treatment services to reduce risk of a behavioral health admission in the 90 days postdischarge from an index admission. These results are consistent with studies showing an association between MAT and residential services and improved outcomes.16,18,19 Most behavioral health admissions, however, had no follow-up service in the 14 days postdischarge.
Surprisingly, outpatient treatment services (and in one model, intensive outpatient) were associated with an increased risk of readmission. On the surface this seems contradictory to expectations, but possible explanations arise. Patients’ discharge plans may refer to an inappropriate level of care – that is, outpatient treatment may be insufficient to meet addiction needs yet residential treatment might not be recommended by the discharge team, readily available, or covered under Medicaid. Studies have shown that poor treatment matching leads to poorer substance use outcomes,24–26 thus readmission is more likely. These findings suggest that no outpatient care is better than outpatient care (controlling for other services). Perhaps presence of a referral to follow-up care or return to pre-existing treatment for substance use or mental disorders indicates a greater need for services following discharge. Further, with residential services sometimes scarce, people who would have been appropriate for residential might go to outpatient or IOP in order to receive any care. This study could not test these scenarios; claims data do not include nuanced measures of severity or needed level of care.
The concept of follow-up services following discharge has clear face validity, but it may be difficult to show the benefit empirically. Challenges discussed below include access to postdischarge services, range in quality and coordination of inpatient and postdischarge services, and data concerns.
First, difficulties accessing behavioral health treatment arise for a variety of reasons.27 Geographic and financial barriers are common, especially for more intensive levels of care. Fourteen days may be insufficient if individuals who are referred to care and intend to use it are unable to obtain appointments within this short window.28,29 Medicaid clients had a 16–22% increase in likelihood of follow-up treatment in a licensed mental health clinic when 30 days were allowed rather than 7 days postdischarge from a mental hospitalization.30 However, a longer follow-up window also allows more time in which relapse might happen.
Second, quality and coordination of postdischarge treatment may vary widely. For example, inpatient providers in one state, prior to a Medicaid quality improvement effort, had low rates of communication with outpatient providers, arranging for follow-up behavioral health care, and referring individuals for physical health care.30 Claims data cannot capture whether communication occurs between inpatient and postdischarge clinicians, level of attention paid to substance use disorders during the inpatient stay, or whether the substance use disorder was addressed adequately or at all. If the major reason for hospitalization was a general medical condition, addiction may have been a side issue. Postdischarge services might not mitigate an initial lack of attention or adequate attention to the individual’s substance use issues.
Third, the necessary omission of states with managed care, which likely carved out behavioral health services resulting in omitted data, means that the states analyzed may not be representative. Replication that includes managed care and carve-out data would give fuller confidence in these findings. Yet, there might be reasons that managed care organizations would have different service arrays and procedures for preventing readmissions than the relatively unmanaged fee-for-service population, which might lead to different patterns of findings. In addition, although the states in this study had the strongest data, few beneficiaries received any follow-up services. Individuals may have received services in settings that have block grant funding or larger residential treatment programs that were ineligible for Medicaid payment based on the IMD exclusion,31 thus are not in Medicaid claims. Even if a state offers a service, it may limit which enrollees may access it (e.g., pregnant women or people with serious mental illness).32 The relatively few individuals meeting inclusion criteria may also reflect under-identification of people with substance use disorders within claims data.33
Medicaid is an increasingly larger payer of behavioral health services,34 particularly under health care reform.31 However, states vary by Medicaid eligibility, behavioral health services covered, spending on behavioral health services,31,35,36 and contracting with specialty managed care organizations for behavioral health benefits. A true national study would have been ideal, but the vast variability amongst states in services available and financing approaches made this prohibitive.
Successful recovery from any diagnosis depends on many factors: quality of care in the index admission, overall health status, demographics, ability to purchase medications, etc. Similarly, a complex variety of factors are associated with readmissions.37 Systematic reviews of interventions to reduce 30-day medical rehospitalization report that no single intervention was regularly associated with reduced risk38 and effective interventions are complex and seek to enhance patient capacity to reliably access and enact postdischarge care.39 A recent project reduced 30-day readmission rates and increased MAT for patients admitted for alcohol dependence by implementing a discharge planning protocol.40
These analyses relied on Medicaid claims data. One cannot tell, for instance, if referrals were made at the time of discharge, or if an individual had difficulties accessing services postdischarge. Individuals dually eligible for Medicaid and Medicare were excluded, which may omit some individuals with severe mental illness. Some services or populations are excluded by states, thus resource availability may play a role in these findings. Services could be obtained with other funding such as block grants, so follow-up service receipt may be underestimated. Findings apply to those who sought Medicaid-funded care. We controlled for disability as the basis of admission, but the definition of disability varies across states. The original admission allowed a behavioral health diagnosis in any position, but the readmissions variable required a primary diagnosis. This omitted some readmissions, but allowed a focus on the impact of behavioral health services on a clearly defined behavioral health readmission. However, this may lead to an underestimate of readmissions that are ultimately related to behavioral health, as this is often not the primary diagnosis but may still be a key factor in an admission. This analysis did not examine the number of services or other aspects of the follow-up care episode, if received.
The generalizability of these findings may be limited. The exclusion criteria reduced the analytic sample to only 10 states. Further, in those 10 states, due to omission of enrollees who were dually eligible for Medicaid and Medicare and those in managed care plans, on average only 18% of Medicaid enrollees were represented in the data. The findings thus are most applicable to people who are in fee-for-service or other plans that have low use of treatment management approaches, or conversely, low use of additional supports to reduce readmissions. As a Medicaid sample, the findings are likely most applicable to people who are low-income or otherwise Medicaid-eligible.
Future research could use alternative methods to delve into open questions raised by these limitations and discussed above as challenges. In particular, research is needed to confirm, and if confirmed, disentangle the perplexing outpatient finding. The discussion above suggests potential pathways to understanding the results, but careful study would be necessary to thoroughly analyze the relationship. Further, it would be important to expand the populations for whom these findings hold, by testing the hypotheses in Medicaid managed care populations, where data are available, as well as privately insured populations.
CONCLUSIONS
In a time of change in the health care system, the question of how to reduce readmissions is potent. A high proportion of patients readmitted to hospitals within a short time frame may indicate inadequate quality of hospital care or lack of appropriate coordination of postdischarge care. Under the ACA, financial penalties have been established for hospitals with excessive Medicare readmissions within 30 days after acute care hospitalizations for several diagnoses.1,41 Other payers likely will follow suit. However, concerns have risen about holding hospitals accountable when they cannot exert control over patient behavior and provider performance after acute care.
It is important to continue to delve into readmissions and follow-up after treatment, given the heightened understanding of how substance use and mental disorders affect health and recovery, the likelihood of readmission, and the high stakes related to health care in this population. Future research should further investigate how MAT and residential treatment may be useful in improving outcomes after an inpatient stay and the counterintuitive outpatient results.
These findings highlight several policy implications. Most individuals had no follow-up services within the 14-day window; if services are not received, they cannot improve outcomes. Policies implemented after the time period of these admissions, including the ACA and federal parity, should increase access to behavioral health services under Medicaid. Further, Medicaid programs should be encouraged to ensure that a range of substance use disorder treatment benefits are offered to all Medicaid beneficiaries. This may require a renewed focus on how to best allocate scarce resources, especially for more expensive services such as residential treatment. States should ensure that barriers to use of MAT are reduced, for example by omitting prior authorization requirements, or by developing models such as hub-and-spoke to increase access to MAT in the community, or by specifically encouraging training for and adoption of MAT among Medicaid providers. Efforts are needed such as focused discharge planning, follow-up phone calls, coordination with primary care providers, use of performance measures (e.g., follow-up after hospitalization for mental illness42), and better linkages between hospitals and specialty addiction treatment providers. Solutions that focus on benefit design should be combined with efforts targeted at referral processes to ensure that more individuals who are discharged from inpatient treatment receive appropriate and timely follow-up services.
Supplementary Material
References
- 1.Centers for Medicare & Medicaid Services. [Accessed June 22, 2015];Readmissions Reduction Program. n.d http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html.
- 2.Agency for Health Care Research and Quality. [Accessed June 22, 2015];Conditions with the Largest Number of Adult Hospital Readmissions by Payer, 2011. 2014 http://www.hcup-us.ahrq.gov/reports/statbriefs/sb172-Conditions-Readmissions-Payer.pdf. [PubMed]
- 3.Clark RE, Samnaliev M, McGovern MP. Impact of substance disorders on medical expenditures for Medicaid beneficiaries with behavioral health disorders. Psychiat Serv. 2009;60(1):35–42. doi: 10.1176/ps.2009.60.1.35. [DOI] [PubMed] [Google Scholar]
- 4.Ries RK, Fiellin DA, Miller SC, Saitz R, editors. The ASAM Principles of Addiction Medicine. 5. Philadelphia, PA: Wolters Kluwer; 2014. [Google Scholar]
- 5.Sterling S, Chi F, Hinman A. Integrating care for people with co-occurring alcohol and other drug, medical, and mental health conditions. Alcohol Res Health. 2011;33(4):338–349. [PMC free article] [PubMed] [Google Scholar]
- 6.Wancata J, Benda N, Windhaber J, Nowotny M. Does psychiatric comorbidity increase the length of stay in general hospitals? Gen Hosp Psychiatry. 2001;23(1):8–14. doi: 10.1016/s0163-8343(00)00110-9. [DOI] [PubMed] [Google Scholar]
- 7.Ahmedani BK, Solberg LI, Copeland LA, et al. Psychiatric comorbidity and 30-day readmissions after hospitalization for heart failure, AMI, and pneumonia. Psychiat Serv. 2015;66(2):134–140. doi: 10.1176/appi.ps.201300518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Becker MA, Boaz TL, Andel R, Hafner S. Risk of early rehospitalization for non-behavioral health conditions among adult Medicaid beneficiaries with severe mental illness or substance use disorders. J Behav Health Serv Res. 2016 doi: 10.1007/s11414-016-9516-9. [DOI] [PubMed] [Google Scholar]
- 9.Rockett IR, Putnam SL, Jia H, Chang CF, Smith GS. Unmet substance abuse treatment need, health services utilization, and cost: A population-based emergency department study. Ann Emerg Med. 2005;45(2):118–127. doi: 10.1016/j.annemergmed.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 10.Raven MC, Billings JC, Goldfrank LR, Manheimer ED, Gourevitch MN. Medicaid patients at high risk for frequent hospital admission: Real-time identification and remediable risks. J Urban Health. 2009;86(2):230–241. doi: 10.1007/s11524-008-9336-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fontanella CA. The influence of clinical, treatment, and healthcare system characteristics on psychiatric readmission of adolescents. Am J Orthopsychiatry. 2008;78(2):187–198. doi: 10.1037/a0012557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mark TL, Tomic KS, Kowlessar N, Chu BC, Vandivort-Warren R, Smith S. Hospital readmission among Medicaid patients with an index hospitalization for mental and/or substance use disorder. J Behav Health Serv Res. 2013;40(2):207–221. doi: 10.1007/s11414-013-9323-5. [DOI] [PubMed] [Google Scholar]
- 13.Prince JD, Akincigil A, Hoover DR, Walkup JT, Bilder S, Crystal S. Substance abuse and hospitalization for mood disorder among Medicaid beneficiaries. Am J Public Health. 2009;99(1):160–167. doi: 10.2105/AJPH.2007.133249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Regenstein M, Andres E. Reducing hospital readmissions among Medicaid patients: A review of the literature. Qual Manag Health Care. 2014;23(1):20–42. doi: 10.1097/QMH.0000000000000016. [DOI] [PubMed] [Google Scholar]
- 15.Raven MC, Carrier ER, Lee J, Billings JC, Marr M, Gourevitch MN. Substance use treatment barriers for patients with frequent hospital admissions. J Subst Abuse Treat. 2010;38(1):22–30. doi: 10.1016/j.jsat.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 16.Fullerton CA, Kim M, Thomas CP, et al. Medication-assisted treatment with methadone: assessing the evidence. Psychiat Serv. 2014;65(2):146–157. doi: 10.1176/appi.ps.201300235. [DOI] [PubMed] [Google Scholar]
- 17.McCarty D, Braude L, Lyman DR, et al. Substance abuse intensive outpatient programs: Assessing the evidence. Psychiat Serv. 2014;65(6):718–726. doi: 10.1176/appi.ps.201300249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reif S, George P, Braude L, et al. Residential treatment for individuals with substance use disorders: Assessing the evidence. Psychiat Serv. 2014;65(3):301–312. doi: 10.1176/appi.ps.201300242. [DOI] [PubMed] [Google Scholar]
- 19.Thomas CP, Fullerton CA, Kim M, et al. Medication-assisted treatment with buprenorphine: Assessing the evidence. Psychiat Serv. 2014;65(2):158–170. doi: 10.1176/appi.ps.201300256. [DOI] [PubMed] [Google Scholar]
- 20.Mark TL, Vandivort-Warren R, Montejano LB. Factors affecting detoxification readmission: Analysis of public sector data from three states. J Subst Abuse Treat. 2006;31(4):439–445. doi: 10.1016/j.jsat.2006.05.019. [DOI] [PubMed] [Google Scholar]
- 21.Lee MT, Horgan CM, Garnick DW, et al. A performance measure for continuity of care after detoxification: Relationship with outcomes. J Subst Abuse Treat. 2014;47(2):130–139. doi: 10.1016/j.jsat.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Medicare & Medicaid Services. [Accessed July 19, 2016];Medicaid Analytic eXtract (MAX) General Information. n.d https://www.cms.gov/research-statistics-data-and-systems/computer-data-and-systems/medicaiddatasourcesgeninfo/maxgeneralinformation.html.
- 23.Centers for Medicare & Medicaid Services. [Accessed Dec 15, 2016];MAX 2008 Encounter Data Chartbook and Appendix Tables. n.d https://www.cms.gov/Research-Statistics-Data-and-Systems/Computer-Data-and-Systems/MedicaidDataSourcesGenInfo/MAX_Chartbooks.html.
- 24.McLellan AT, Grissom GR, Zanis D, Randall M, Brill P, O’Brien CP. Problem-service ‘matching’ in addiction treatment. A prospective study in 4 programs. Arch Gen Psychiatry. 1997;54(8):730–735. doi: 10.1001/archpsyc.1997.01830200062008. [DOI] [PubMed] [Google Scholar]
- 25.McLellan AT, Woody GE, Luborsky L, O’Brien CP, Druley KA. Increased effectiveness of substance abuse treatment. A prospective study of patient-treatment “matching”. J Nerv Ment Dis. 1983;171(10):597–605. doi: 10.1097/00005053-198310000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Sharon E, Krebs C, Turner W, et al. Predictive validity of the ASAM Patient Placement Criteria for hospital utilization. J Addict Dis. 2003;22(Suppl 1):79–93. doi: 10.1300/j069v22s01_06. [DOI] [PubMed] [Google Scholar]
- 27.Substance Abuse and Mental Health Services Administration. [Accessed July 19, 2016];Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. 2013 http://archive.samhsa.gov/data/NSDUH/2012SummNatFindDetTables/DetTabs/NSDUH-DetTabsTOC2012.htm.
- 28.Boyd JW, Linsenmeyer A, Woolhandler S, Himmelstein DU, Nardin R. The crisis in mental health care: a preliminary study of access to psychiatric care in Boston. Ann Emerg Med. 2011;58(2):218–219. doi: 10.1016/j.annemergmed.2011.03.053. [DOI] [PubMed] [Google Scholar]
- 29.Malowney M, Keltz S, Fischer D, Boyd JW. Availability of outpatient care from psychiatrists: a simulated-patient study in three U.S. cities. Psychiat Serv. 2015;66(1):94–96. doi: 10.1176/appi.ps.201400051. [DOI] [PubMed] [Google Scholar]
- 30.New York State Office of Mental Health. [Accessed June 22, 2015];New York State Behavioral Health Organizations Phase 1 Summary Report January 2012–June 2013. n.d https://www.omh.ny.gov/omhweb/special-projects/dsrip/docs/bho-2013-report.pdf.
- 31.Substance Abuse and Mental Health Services Administration. Medicaid Handbook: Interface with Behavioral Health Services. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. [Google Scholar]
- 32.Armed Forces Health Surveillance C. Arm and shoulder conditions, active component, U.S. Armed Forces, 2003–2012. Msmr. 2013;20(6):18–22. [PubMed] [Google Scholar]
- 33.Garnick DW, Horgan CM, Chalk M. Performance measures for alcohol and other drug services. Alcohol Res Health. 2006;29(1):19–26. [PMC free article] [PubMed] [Google Scholar]
- 34.Mark TL, Levit KR, Vandivort-Warren R, Buck JA, Coffey RM. Changes in US spending on mental health and substance abuse treatment, 1986–2005, and implications for policy. Health Aff (Millwood) 2011;30(2):284–292. doi: 10.1377/hlthaff.2010.0765. [DOI] [PubMed] [Google Scholar]
- 35.Robinson G, Kaye N, Bergman D, Moreaux M, Baxter C. [Accessed June 22, 2015];State profiles of mental health and substance abuse services in Medicaid. 2005 http://store.samhsa.gov/product/State-Profiles-of-Mental-Health-and-Substance-Abuse-Services-in-Medicaid/NMH05-0202.
- 36.Substance Abuse and Mental Health Services Administration. [Accessed July 19, 2016];National Expenditures for Mental Health Services and Substance Abuse Treatment Services, 1986–2005. 2010 http://store.samhsa.gov/shin/content//SMA10-4612/SMA10-4612.pdf.
- 37.Rosen AK, Chen Q, Shin MH, et al. Medical and surgical readmissions in the Veterans Health Administration: what proportion are related to the index hospitalization? Med Care. 2014;52(3):243–249. doi: 10.1097/MLR.0000000000000081. [DOI] [PubMed] [Google Scholar]
- 38.Hansen LO, Young RS, Hinami K, Leung A, Williams MV. Interventions to reduce 30-day rehospitalization: A systematic review. Ann Intern Med. 2011;155(8):520–528. doi: 10.7326/0003-4819-155-8-201110180-00008. [DOI] [PubMed] [Google Scholar]
- 39.Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095–1107. doi: 10.1001/jamainternmed.2014.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wei J, Defries T, Lozada M, Young N, Huen W, Tulsky J. An inpatient treatment and discharge planning protocol for alcohol dependence: efficacy in reducing 30-day readmissions and emergency department visits. Journal of general internal medicine. 2015;30(3):365–370. doi: 10.1007/s11606-014-2968-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Health Affairs. Health Policy Brief: Medicare Hospital Readmissions Reduction Program. [Accessed June 22, 2015];Health Affairs. 2013 http://healthaffairs.org/healthpolicybriefs/brief_pdfs/healthpolicybrief_102.pdf.
- 42.National Quality Forum. [Accessed June 22, 2015];Follow-up After Hospitalization for Mental Illness (FUH) n.d http://www.qualityforum.org/QPS/0576.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.