Abstract
HIV and other sexually transmitted infections (STIs) are important public health challenges in the US. Adverse childhood experiences (ACEs), including abuse (emotional, physical or sexual), witnessing violence among household members, may have an effect on sexual behaviors, which increase the risk of HIV/STIs. The aim of this study was to examine the sex differences in the role of posttraumatic stress disorder (PTSD), major depression (MD), substance use disorders (SUDs), early sexual debut, and intimate partner violence (IPV) perpetration as mediators in the association between ACEs and HIV/STIs. Data were obtained from Wave 2 (2004–2005) of the National Epidemiologic Survey on Alcohol and Related Conditions. Structural equation modeling was used to determine the role of PTSD, MD, SUDs, early sexual debut, and IPV perpetration as mediators in the relationships between ACEs and HIV/STIs. Differences and similarities existed in the mediational roles of psychopathology and sexual behaviors. For example, among men, MD fully mediated physical/psychological abuse (β = 0.0002; p = 0.012) and sexual abuse (β = 0.0002; p = 0.006), and HIV/STIs while among women, MD fully mediated physical/psychological abuse (β = 0.0005; p < 0.001) and parental violence (β = −0.0002; p = 0.012). Among men, IPV perpetration fully mediated sexual abuse (β = −0.0005; p = 0.012) and HIV/STIs while among women, IPV perpetration was not a statistically significant mediator. HIV/STI prevention and intervention programs should use a life course approach by addressing adverse childhood events among men and women and consider the sex differences in the roles of psychopathology and sexual behaviors.
Keywords: Child abuse, HIV, Sexually transmitted diseases, Mediation, Men, Women
Introduction
HIV and other sexually transmitted infections (STIs) are important public health challenges in the United States (US). The Centers for Disease Control and Prevention (CDC) estimates that 1.2 million people are living with HIV in the US, and approximately one in eight are unaware of their infection [1]. Twenty million STIs occur in the US each year [2]. Some of the most common STIs among the US population include human papillomavirus (HPV), chlamydia, gonorrhea, and syphilis. Multiple adverse health outcomes may arise as a result of STIs, including cancer, adverse pregnancy outcomes, such as low birth weight and preterm delivery, and death [3–5]. Transmission of STIs from mother to child can result in fetal and neonatal death [6], and HPV infection may result in death from cervical cancer [7].
Adverse childhood experiences (ACEs) are also important public health issues and are defined as the negative events that a child may experience, including abuse (emotional, physical or sexual), witnessing violence among household members, losing a parent due to death or divorce, or residing in a household with someone who has mental illness, substance abuse or is engaging in criminal behavior [8, 9]. Recent estimates suggest that 63.1 % of adults in the US have been exposed to at least one ACE [10].
ACEs may have an effect on sexual risk behaviors, which increase the risk of STIs [11]. Childhood sexual abuse and having a family member who had a mental illness are associated with sexual risk behaviors such as sex at age 16 or younger, having multiple partners and pregnancy at age 18 or younger [12]. Psychological abuse, physical and psychological neglect, and parental separation were also associated with having multiple partners [12]. A child’s mother being treated violently was also associated with pregnancy before or at age 18 [12].
ACEs are also associated with psychiatric outcomes such as post-traumatic stress disorder (PTSD) [13], depression (MD) [14–17] and substance use disorders (SUDs) [14, 15, 18–20], and with sexual health outcomes such as early age at sexual debut [12] and IPV perpetration [21–23], which may lead to an increase in HIV/STI infections. Depression [24, 25] and substance use [24–26] have been shown to be positively associated with HIV seroconversion. Loneliness, one of the major tenets of depression, may lead to risky sexual behavior such as condomless sex [25], which is a risk factor for HIV/STIs. Substance use is also linked to a higher likelihood of unprotected sexual intercourse and condom failure [24], which are risk factors for contracting HIV and/or other STIs. PTSD has also been shown to be positively linked to risk factors such as anal sexual intercourse [27], exchange sex for money and/or drugs [27, 28], multiple sexual partners [28], and having sex with a risky partner [28, 29], which are determinants of contracting HIV and/or other STIs.
The Traumagenic Dynamics model proposed by Finkelhor and Browne offers a viable framework to investigate sexual health consequences associated with childhood sexual abuse [30, 31]. The four traumagenic dynamics, which may help in the understanding of the relationship between sexual abuse and sexual health outcomes are: traumatic sexualization, betrayal, powerlessness and stigmatization [31]. In relation to the current study, we also propose that the latter three components of the Traumagenic Dynamics model (betrayal, powerlessness and stigmatization) may be used to understand the sexual health consequences associated with other ACEs. For example, in experiencing ACEs such as neglect, and physical or psychological abuse, there may be a sense of betrayal that is felt by the child as someone who they trusted has caused them harm by abuse and/or neglect [32, 33]. Witnessing violence in the home [34], or living with someone who had been incarcerated [35] or had mental illness [36] can result in a child feeling powerless or helpless, as he/she may not be able to help during these specific events. By experiencing any, some or all of these adverse events, neglect [37], physical or psychological abuse [37], sexual abuse [37–39], witnessing parental violence [40] or living with someone who was incarcerated [35] or had a mental illness [41], a child may feel stigmatized or ashamed. These feelings of betrayal, powerlessness and stigmatization may persist into adulthood. In addition, research has shown that feelings of powerlessness can be a factor contributing to engaging in risky sexual behavior [42]. We also propose that feelings of betrayal and stigmatization that may occur due to these adverse events may contribute to mental health disorders and maladaptive behaviors, and hence, an increase in the likelihood of being diagnosed with HIV and/or an STI.
The aim of this study was to examine the sex differences in the role of PTSD, MD, SUDs, early sexual debut, and intimate partner violence (IPV) perpetration as mediators in the association between ACEs and HIV/STIs. We also used varying components of the Traumagenic Dynamics model (traumatic sexualization, betrayal, powerlessness, and stigmatization) as a framework to understand the relationship, not only between sexual abuse, but also between other ACEs (psychological/physical abuse, witnessing parental violence, parental incarceration and psychopathology) and HIV/STIs, and the potential mediational roles of PTSD, MD, SUDs, early sexual debut, and IPV perpetration.
Methods
Ethics Statement
The Virginia Commonwealth University Institutional Review Board deemed the current study exempt as de-identified, secondary data were used.
Data Source and Sample Population
Data were obtained from Wave 2 (2004–2005) of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). The NESARC was designed to study psychiatric and substance use disorders [43]. The NESARC sample is a nationally representative sample of the non-institutionalized adult population of the U.S., including the District of Columbia, Alaska, and Hawaii. Adults age 18 years and older living in the US were surveyed [44]. The “Group Quarters Inventory” from the US Bureau of Census 2000 was used to obtain information from military personnel living off base, boarding houses, rooming houses, nontransient hotels and motels, shelters, facilities for housing workers, college quarters, and group homes [44]. The survey also oversampled Black and Hispanic households [44], and included Spanish speakers [45]. Sample weights were available for each observation.
Operationalization of Adverse Childhood Experiences
ACEs were operationalized by 23 questions asking about experiences during childhood [46]: (1) If a respondent was left alone or unsupervised before age 10, (2) Went without things needed (clothes, school supplies), (3) Went hungry, or (4) Failed to get medical treatment; (5) If a parent or caregiver insulted or said hurtful things, (6) Threatened to hit or throw something at the respondent, (7) Made the respondent fear that he/she would be physically hurt, (8) Pushed, grabbed, shoved, slapped or hit the respondent, or (9) Hit the respondent causing marks, bruises or injury; (10) If an adult or other person had touched the respondent sexually, (11) Had the respondent touched him/her sexually, (12) Attempted to have sexual intercourse or (13) Had sexual intercourse with the respondent; (14) If the respondent witnessed his/her father or another adult male push, grab, slap, or throw something at his/her mother, (15) Hit mother with a fist or something hard, (16) Repeatedly hit mother for at least a few minutes, or (17) Threaten mother with a knife/gun or use it to hurt her. These ACEs were analyzed in a Likert Scale format: “Very often”, “Fairly often”, “Sometimes”, “Almost never” and “Never”. However, some ACEs, which had relatively few respondents in some categories were recoded to Very often/Fairly often/Sometimes/Almost never versus Never (sexual abuse categories) or Very often/Fairly often versus Sometimes/Almost never versus Never (witnessing parental violence categories) [22]. Other ACEs were determined from questions asking if, before 18 years old, the respondent had lived with a parent or other adult who (18) Was a problem drinker, (19) Had abused drugs, (20) Had been incarcerated, (21) Had a mental illness, or (22) Had attempted and/or (23) Had committed suicide, each coded with a dichotomous (Yes vs. No) response [46]. Due to the distinct categorization of ACEs in our previous research [46], ACEs were then categorized as: neglect (items 1–4), physical/psychological abuse (items 5–9), sexual abuse (items 10–13), parental violence (items 15–17), and parental incarceration and psychopathology (items 18–23). The constructs capture by the ACE questions in the NESARC are consistent with those covered by other widely used ACE questionnaires, such as the Adverse Childhood Experiences International Questionnaire (ACE-IQ), implemented by the World Health Organization [47], and the Adverse Childhood Experience Study Scale [48]. This consistency provides support for the construct validity of the NESARC ACE questionnaire. The questions used in the ACE questionnaire in NESARC also cover adverse events that have been used in several studies examining ACEs [49–53].
Operationalization of HIV/STI Diagnosis
There were three questions on HIV/STI diagnosis: “In the last 12 months, did you test positive for HIV, the virus that causes AIDS?”; “In the last 12 months, did you have AIDS?”; and “In the last 12 months, did you have any other sexually transmitted diseases?” Therefore, HIV/STI diagnosis was operationalized by answering “Yes” to any of the three questions versus answering “No” to all three questions.
Potential Mediators—Posttraumatic Stress Disorder, Substance Use Disorders, Major Depression, Intimate Partner Violence Perpetration, Early Sexual Debut
PTSD, MD, and SUDs were determined by questions asking about symptoms of PTSD, major depressive episode, and SUDs since Wave 1 interview (2001–2002) but before the past year. SUDs considered were abuse of and/or dependence on alcohol, nicotine, sedatives, tranquilizers, opioids, amphetamines, cannabis, hallucinogens, cocaine, and heroin [46]. PTSD, MD, and SUDs were diagnosed using the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria [54] and the Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version (AUDADIS-IV) [55, 56].
IPV perpetration was operationalized by six questions taken from the Conflict Tactic Scales [57], which have been validated in a population-based sample [58]. These questions were used to ask respondents about use of force with partners in the past year: [22] 1) Pushing, grabbing or shoving; 2) Slapping, kicking, biting or hitting; 3) Threatening his/her partner with a weapon like a knife or gun; 4) Cutting or bruising partner; 5) Forcing partner to have sex; and 6) Injuring partner enough so that he/she needed medical attention. Each IPV perpetration variable was categorized into a binary construct, Once/2 to 3 times/Once a month/More than once a month versus Never, as has been used in previous studies [58–61], before being used as a latent variable in structural equation modeling (SEM) [46]. The use of latent variables allows for the reduction of a large number of observed variables into an overall theme. In addition, IPV perpetration is more proximal to HIV/STI infection in comparison to the other mediator variables considered.
Age at sexual debut was determined by the question “How old were you when you first had sex/sexual intercourse, or have you never had sexual intercourse?” Debut was categorized into <15 and ≥15 [62]. Self-reported age at sexual debut has been used in several prior studies [62–65].
Confounders
Potential confounders considered were associated with ACEs and HIV/STI diagnosis. Previous studies suggest that age, race/ethnicity, income, marital status and insurance status differences are associated with ACEs [66]. Diagnosis of STIs was independently associated with race/ethnicity and low income [67]. A previous study examining the association between ACEs and STI diagnosis adjusted for age at interview and race [11]. Marital status [68–70] and socioeconomic risk factors [68, 69] such as education [70] in prior studies were associated with STIs. Therefore, the following potential sociodemographic confounders were considered: age, race/ethnicity (White (reference), Black, Other, Hispanic), income (<$25,000, $25,000–<$50,000, ≥ $50,000 (reference), education (less than high school, high school, greater than high school education), marital status (married/cohabiting, widowed/divorced/separated, never married (reference)) and insurance status (insured (reference) and not insured).
Analytic Approach
Respondents were excluded if they answered “Don’t know” to questions on ACEs and HIV/STI diagnosis (n = 262). Therefore, the resultant sample size was 34,391. The distribution of sociodemographic characteristics overall, across populations exposed and unexposed to ACEs, and populations diagnosed and not diagnosed with HIV/STIs were examined using SAS version 9.4 (SAS Institute, Cary, NC). The prevalence estimates of mediator variables were also obtained among the overall study population, and by ACE exposure and HIV/STI diagnosis.
Overall Structural Equation Modeling Approach
Structural equation modeling (SEM) was used to determine appropriate latent factor(s) for ACEs and IPV perpetration. Exploratory factor analysis (EFA) was used to explore the possible latent structures of the observed variables for ACEs and IPV perpetration. Confirmatory factor analysis (CFA) was used to confirm the latent structures and to determine if the models obtained from the EFA were an appropriate fit for the data [71]. A mediation model was used to determine the roles of PTSD, MD, SUDs, early sexual debut (as observed variables), and IPV perpetration (as a latent variable) between ACE factors and HIV/STIs (an observed variable) (Fig. 1). Survey weights were used in analyses. SEM and mediational analyses were performed in Mplus (Muthén & Muthén, Los Angeles, CA).
Fig. 1.
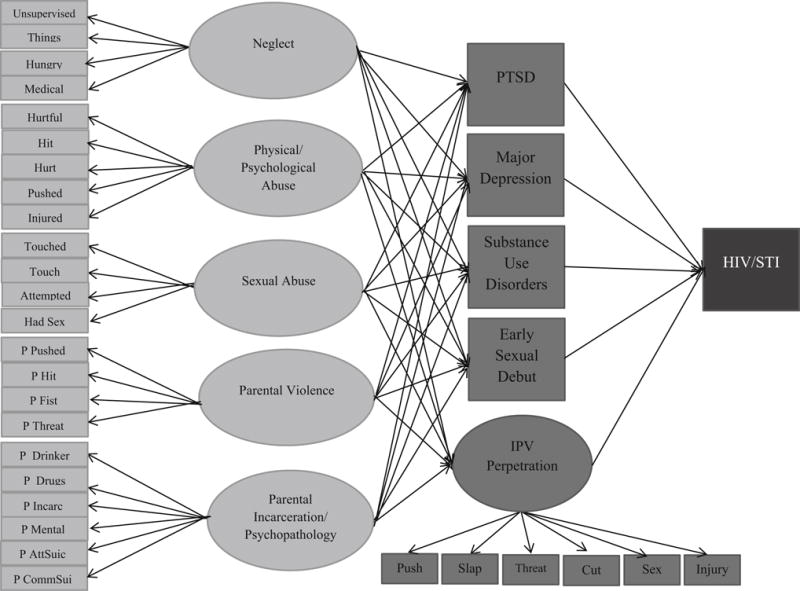
Mediational model showing hypothesized indirect associations between adverse childhood experiences and HIV/STIs. Direct associations between ACE factors and HIV/STIs are not shown. Abbreviations: Adverse childhood experiences: Attempted Adult/other person attempted to have sex with respondent; Had sex Adult/other person had sex with respondent; Hit Parent/caregiver threatened to hit or throw something at the respondent; Hungry Respondent went hungry; Hurt Parent/caregiver made respondent fear they would be physically hurt; Hurtful Parent/caregiver insulted or said hurtful things to the respondent; Injured Parent/caregiver hit respondent that caused marks/bruises/injury; Medical Respondent failed to get medical treatment; P_AttSuic Respondent lived with a parent/other adult who attempted suicide; P_CommSuic Respondent lived with a parent/other adult who committed suicide; P_Drinker Parent/other adult living in the home was a problem drinker; P_Drugs Parent/other adult had problems with drugs; P_Fist Father/other adult male hit mother with a fist or something hard; P_Hit Father/other adult male repeatedly hit mother for at least a few minutes; P_Incarc Respondent lived with a parent/other adult who was incarcerated; P_Mental Parent/other adult was treated/hospitalized for mental illness; P_Pushed Father/other adult male push, grab, slap or throw something at mother; P_Threat Father/other adult male threaten mother with a knife/gun or use it to hurt her; Pushed Parent/caregiver pushed/grabbed/shoved/slapped or hit respondent; Things Respondent went without things needed (clothes, supplies); Touch Adult/other person had respondent touched them sexually; Touched Adult/other person touched respondent sexually; Unsupervised Respondent was left alone or unsupervised before age 10; Mediator: PTSD posttraumatic stress disorder; Intimate partner violence perpetration: Cut Respondent cut/bruise spouse or partner; IPV Intimate partner violence; Injury Respondent injured spouse/partner enough that they needed medical care; Push Respondent pushed/grabbed/shoved spouse/partner; Sex Respondent force spouse/partner to have sex; Slap Respondent slapped/kicked/bit/hit spouse/partner; Threat Respondent threatened spouse/partner with a weapon like a knife or gun; HIV/STI HIV/sexually transmitted infection
Model Building
Measurement invariance by sex was tested for ACE factors and IPV perpetration. Configural invariance and strong measurement invariance would indicate that parameters (factor loadings and thresholds) were freely estimated or fixed across groups, respectively [72]. The Chi square difference test of measurement invariance is limited as it is highly influenced by sample size [73–75]. Due to the large sample size of the study population, the change in the Comparative Fit Index (ΔCFI) (CFIconstrained − CFIunconstrained) was used as an alternative goodness-of-fit index, where a value of ≤0.01 indicates that the null hypothesis of measurement invariance should not be rejected [76].
Results
Weighted Descriptive Statistics
Table 1 shows the distribution of sociodemographic characteristics, overall and by ACE exposure and HIV/STI diagnosis, and shows ACE exposure by HIV/STI diagnosis and HIV/STI diagnosis by ACE exposure. Overall, about six in ten respondents reported being exposed to ACEs (60.9 %) and only 0.9 % reported an HIV/STI diagnosis in the past year.
Table 1.
Distribution of characteristics overall, across respondents exposed and unexposed to ACEs and reporting or not reporting HIV/STIs
| Overall % (N) | ACEs % (N) | No ACEs % (N) | p value % (N) | HIV/STIs % (N) | No HIV/STIs % (N) | p value | |
|---|---|---|---|---|---|---|---|
| Sex | |||||||
| Men | 47.9 (14,453) | 49.5 (9236) | 45.4 (5217) | <0.0001 | 45.1 (145) | 48.0 (14,308) | 0.0693 |
| Women | 52.1 (19,938) | 50.4 (12,018) | 54.6 (7920) | 54.9 (220) | 52.0 (19,718) | ||
| Age | |||||||
| 18–34 | 25.5 (7988) | 24.8 (4885) | 26.5 (3103) | 39.2 (130) | 25.3 (7858) | ||
| 35–49 | 31.1 (10,966) | 33.4 (7253) | 27.5 (3713) | 42.6 (154) | 31.0 (10,812) | ||
| 50+ | 43.4 (15,437) | 41.7 (9116) | 46.0 (6321) | <0.0001 | 18.3 (81) | 43.6 (15,356) | <0.0001 |
| Race/ethnicity | |||||||
| White, nH | 71.0 (20,025) | 71.2 (12,383) | 70.7 (7642) | <0.0001 | 62.7 (182) | 71.1 (19,843) | <0.0001 |
| Black, nH | 11.0 (6541) | 11.4 (4158) | 10.5 (2383) | 19.3 (110) | 11.0 (6431) | ||
| Other, nH | 6.4 (1520) | 6.1 (906) | 6.9 (614) | 5.0 (13) | 6.4 (1507) | ||
| Hispanic, any race | 11.6 (6305) | 11.4 (3807) | 11.9 (2498) | 13.0 (60) | 11.6 (6245) | ||
| Income | |||||||
| <$25,000 | 26.3 (10,826) | 25.3 (6369) | 27.8 (4457) | 39.7 (171) | 26.2 (10,655) | ||
| $25,000–<$50,000 | 27.8 (9758) | 27.5 (6034) | 28.4 (3724) | 26.8 (90) | 27.9 (9668) | ||
| ≥$50,000 | 45.9 (13,807) | 47.1 (8851) | 43.8 (4956) | <0.0001 | 33.5 (104) | 46.0 (13,7003) | <0.0001 |
| Education | |||||||
| <High school | 14.0 (5452) | 13.1 (3116) | 15.3 (2336) | 15.9 (62) | 14.0 (5390) | ||
| High school | 27.5 (9377) | 26.7 (5618) | 28.6 (3759) | 28.6 (109) | 27.5 (9268) | ||
| >High school | 58.6 (19,562) | 60.1 (12,520) | 56.1 (7042) | <0.0001 | 55.5 (194) | 58.6 (19,368) | 0.1001 |
| Insurance | |||||||
| Yes | 87.7 (30,034) | 88.0 (18,634) | 87.3 (11,400) | 0.0029 | 85.0 (302) | 87.7 (29,732) | 0.0006 |
| No | 12.3 (4325) | 12.0 (2601) | 12.7 (1724) | 15.0 (63) | 12.3 (4262) | ||
| Marital status | |||||||
| Married/cohabiting | 63.8 (18,752) | 64.3 (11,633) | 63.1 (7119) | 0.0004 | 44.4 (125) | 64.0 (18,627) | <0.0001 |
| Widowed/Div/Sep | 18.8 (9058) | 18.6 (5537) | 19.1 (3521) | 22.6 (101) | 18.8 (8.957) | ||
| Never married | 17.36 (6581) | 17.0 (4084) | 17.8 (2497) | 32.9 (139) | 17.2 (6442) | ||
| ACE exposure | |||||||
| Yes | 60.9 (21,254) | – | – | 72.2 (273) | 60.8 (20,981) | ||
| No | 39.1 (13,137) | 27.8 (92) | 39.2 (13,045) | <0.0001 | |||
| HIV/STI | |||||||
| Yes | 0.9 (365) | 1.1 (273) | 0.7 (92) | – | – | ||
| No | 99.1 (34,026) | 98.9 (20,981) | 99.3 (13,045) | <0.0001 |
There were statistically significant differences in ACE exposure by sex, age, race/ethnicity, yearly income category, education, insurance, marital status, and by HIV/STI diagnosis. Among respondents reporting ACEs, approximately 50 % were women while among those reporting no exposure to ACES, approximately 55 % were women. Approximately one-third (33.4 %) of respondents reporting ACEs were aged 35–49 while 27.5 % of those reporting no exposure to ACEs were in the same age group. The percentages of White and Black respondents reporting ACEs were slightly higher compared to the percentages of White and Black respondents who did not report ACE exposure (White: 71.2 % reporting ACEs vs. 70.7 % reporting no ACEs; Black: 11.4 % reporting ACEs vs. 10.5 % reporting no ACEs). Among those reporting ACEs, approximately a quarter (25.3 %) of respondents reported earning less than $25,000 per year in comparison to about 28 % reporting no exposure to ACEs. With regards to educational differences, among respondents who reported at least one ACE, approximately 13.1 % had less than a high school education compared to 15.3 % of those reporting no ACEs. Majority of respondents reporting ACEs and not reporting ACEs, 88 and 87 % respectively, reported having health insurance. Approximately, 64 and 63 % of respondents reporting and not reporting ACEs, respectively, were married/cohabiting. Majority of respondents reporting ACEs and not reporting exposure to ACEs did not report being diagnosed with HIV/STIs, 98.9 and 99.3 %, respectively.
There were also statistically significant differences in reporting HIV/STIs by age, race/ethnicity, yearly income category, insurance, marital status and ACE exposure but no statistically significant differences by sex and by education. Approximately four in ten (42.6 %) of respondents reporting HIV/STIs were 35–49 compared to approximately three in ten (31.0 %) of respondents of that age group not reporting an HIV/STI diagnosis. White respondents accounted for majority of respondents reporting and not reporting HIV/STIs, 62.7 and 71.1 %, respectively. Close to four in ten (39.7 %) of respondents reporting HIV/STI infection earned less than $25,000 while approximately one in four (26.2 %) among those not reporting HIV/STI infection were in the same income category. Majority of respondents who reported and did not report HIV/STIs had insurance, 85.0 and 87.7 %, respectively. However, close to one in three (32.9 %) respondents reporting HIV/STIs and 17.2 % of respondents not reporting HIV/STIs were never married. Approximately seven in ten (72.2 %) respondents reporting HIV/STIs and about six in ten respondents (60.8 %) not reporting an HIV/STI diagnosis also reported exposure to at least one ACE.
Weighted Prevalence of Mediators
Table 2 shows the weighted prevalence estimates of PTSD, MD, SUDs, early sexual debut and IPV perpetration overall, by ACE exposure and HIV/STI diagnosis. Overall, 6.4 % of the population reported PTSD, 7.0 % reported MD, and 15.1 % reported SUDs. Approximately one in ten (9.9 %) of the study population reported having a sexual debut at less than 15 years old and 5.6 % reported IPV perpetration in the past year. There were statistically significant differences in ACE exposure and HIV/STI diagnosis for all mediator variables. For example, the percentages of respondents reporting ACEs and reporting PTSD, MD, SUDs, early sexual debut, and IPV perpetration were two to three times the percentages of respondents not reporting ACEs but reporting the mediator variable. A similar pattern was seen for the mediator variables by HIV/STI diagnosis. The percentages of respondents reporting HIV/STIs and reporting PTSD, MD, SUDs, early sexual debut, and IPV perpetration were more than twice the percentages of respondents not reporting an HIV/STI diagnosis but reporting each mediator.
Table 2.
Prevalence of mediator variables overall and by adverse childhood experience and HIV/STI exposure
| Mediator | Overall % (N) | ACEs % (N) | No ACEs % (N) | HIV/STIs % (N) | No HIV/STIs % (N) |
|---|---|---|---|---|---|
| PTSD | |||||
| Yes | 6.4 (2457) | 8.7 (2033) | 2.9 (424) | 15.7 (56) | 6.4 (2401) |
| No | 93.6 (31,934) | 91.3 (19,221) | 97.1 (12,713) | 84.3 (309) | 93.6 (31,625) |
| Major depression | |||||
| Yes | 7.0 (2479) | 9.1 (1985) | 3.6 (494) | 19.4 (60) | 6.8 (2419) |
| No | 93.0 (31,912) | 90.9 (19,269) | 96.4 (12,643) | 80.6 (305) | 93.2 (31,607) |
| Substance use disorders | |||||
| Yes | 15.1 (4952) | 18.9 (3842) | 9.2 (1110) | 35.7 (109) | 14.9 (4843) |
| No | 84.9 (29,439) | 81.1 (17,412) | 90.8 (12,027) | 64.3 (256) | 85.1 (29,183) |
| Early sexual debut | |||||
| <15 | 9.9 (3317) | 12.4 (2589) | 5.8 (728) | 22.0 (73) | 9.8 (3244) |
| ≥15 | 90.1 (28,445) | 87.6 (17,428) | 94.2 (11,017) | 78.0 (282) | 90.2 (28,163) |
| IPV perpetration | |||||
| Yes | 5.6 (1679) | 7.2 (1379) | 2.8 (300) | 12.5 (44) | 5.5 (1635) |
| No | 94.4 (23,923) | 92.8 (14,972) | 97.2 (8951) | 87.5 (225) | 94.5 (23,698) |
Comparisons of ACE exposure and non-exposure, and HIV/STI diagnosis and no diagnosis were statistically significant for all mediator variables with p < 0.001
ACE adverse childhood experience, IPV intimate partner violence, PTSD posttraumatic stress disorder, STI sexually transmitted infection
Evaluation of Measurement Models
Supplemental Table 1 shows the standardized model results for measurement models with strong invariance from the confirmatory factor analysis (CFA) models for ACEs and IPV perpetration. Model fit statistics for the CFA for the ACE measurement model were: χ2(df = 497) = 10,169.475, p < 0.0001; χ2 for men = 4007.798; χ2 for women = 6161.677; CFI = 0.989; TLI = 0.989; RMSEA = 0.034; 90 % CI (0.033–0.034), WRMR = 5.771. Model fit statistics for the CFA for the IPV measurement model were: χ2(df = 22) = 157.238, p < 0.0001; χ2 for men = 54.680; χ2 for women = 102.558; CFI = 0.991; TLI = 0.988; RMSEA = 0.019; 90 %CI (0.016–0.022), WRMR = 2.410. The model fit statistics indicate that the ACE and IPV perpetration measurement models were a good fit for the data.
Measurement Invariance
There were statistically significant differences comparing configural invariance (factor loadings and thresholds were freely estimated) and strong invariance (holding factor loadings and thresholds equal across groups) models for ACE and IPV perpetration factors. The CFI difference comparing the constrained and unconstrained models was −0.001 for ACEs and 0.005 for IPV perpetration, which are both <0.01. As a result, structural models accounted for strong invariance for ACEs and IPV perpetration across sex groups and we were able to compare findings for men and women.
Evaluation of Structural Model
Direct Relationships Between ACEs and HIV/STIs
Tables 3 and 4 show the direct associations between ACEs, mediators, (PTSD, depression, substance abuse, early sexual debut, and IPV perpetration) and HIV/STIs. There were no statistically significant direct associations seen between ACEs and HIV/STIs. However, PTSD, MD, SUDs, and early sexual debut were associated with HIV/STIs in both men and women, but IPV perpetration was associated with HIV/STIs in men only.
Table 3.
Unstandardized estimates for associations between HIV/STIs, PTSD, major depression, and substance use disorders and adverse childhood experiences among men and women, national epidemiologic survey on alcohol and related conditions, 2004–2005
| HIV/STIs
|
PTSD
|
Major depression
|
Substance use disorders
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est. | SE | p value | Est. | SE | p value | Est. | SE | p value | Est. | SE | p value | |
| Men | ||||||||||||
| Neglect | −0.003 | 0.002 | 0.224 | 0.010 | 0.006 | 0.105 | −0.012 | 0.007 | 0.106 | −0.047 | 0.016 | 0.003** |
| Phys/Psy | 0.002 | 0.002 | 0.396 | 0.019 | 0.005 | <0.001*** | 0.032 | 0.006 | <0.001*** | 0.085 | 0.013 | <0.001*** |
| Sexual | 0.002 | 0.002 | 0.337 | 0.023 | 0.004 | <0.001*** | 0.019 | 0.005 | <0.001*** | 0.034 | 0.010 | <0.001*** |
| PV | 0.000 | 0.002 | 0.847 | −0.006 | 0.004 | 0.125 | −0.007 | 0.005 | 0.163 | −0.016 | 0.011 | 0.156 |
| PIP | 0.002 | 0.001 | 0.269 | 0.008 | 0.003 | 0.006** | 0.009 | 0.003 | 0.013* | 0.022 | 0.008 | 0.008** |
| HIV/STI* | 0.009 | 0.003 | 0.001** | 0.010 | 0.003 | <0.001*** | 0.012 | 0.002 | <0.001*** | |||
| Women | ||||||||||||
| Neglect | 0.001 | 0.003 | 0.605 | −0.005 | 0.008 | 0.530 | −0.022 | 0.009 | 0.022* | −0.043 | 0.010 | <0.001*** |
| Phys/Psy | 0.000 | 0.002 | 0.886 | 0.037 | 0.007 | <0.001*** | 0.056 | 0.008 | <0.001*** | 0.051 | 0.008 | <0.001*** |
| Sexual | 0.001 | 0.002 | 0.591 | 0.048 | 0.036 | 0.190 | 0.031 | 0.024 | 0.197 | 0.028 | 0.022 | 0.197 |
| PV | 0.001 | 0.002 | 0.454 | 0.007 | 0.005 | 0.113 | −0.017 | 0.006 | 0.003** | 0.002 | 0.006 | 0.672 |
| PIP | 0.001 | 0.002 | 0.410 | −0.003 | 0.005 | 0.581 | 0.012 | 0.006 | 0.052 | 0.017 | 0.006 | 0.009** |
| HIV/STI* | 0.004 | 0.002 | 0.035* | 0.009 | 0.002 | <0.001*** | 0.009 | 0.002 | <0.001*** | |||
Note Direct associations between ACE factors and mediators (PTSD, depression, substance abuse), between mediators and HIV/STIs, and between ACE factors and HIV/STIs
Est. unstandardized estimate, Phys/Psy physical/psychological abuse, PIP parental incarceration/psychopathology, PTSD posttraumatic stress disorder, PV witnessing parental violence, SE standard error
HIV/STI on PTSD, depression, substance abuse;
Bolded numbers are statistically significant at
p < 0.05,
p < 0.01,
p < 0.001
Table 4.
Unstandardized estimates for associations between early sexual debut, IPV perpetration and adverse childhood experiences among men and women, national epidemiologic survey on alcohol and related conditions, 2004–2005
| Latent variable | Early sexual debut
|
IPV perpetration
|
||||
|---|---|---|---|---|---|---|
| Est. | SE | p value | Est. | SE | p value | |
| Men | ||||||
| Neglect | −0.036 | 0.011 | 0.001** | −0.120 | 0.094 | 0.201 |
| Phys/Psy | 0.041 | 0.009 | <0.001*** | 0.087 | 0.069 | 0.211 |
| Sexual | 0.056 | 0.007 | <0.001*** | 0.232 | 0.050 | <0.001*** |
| PV | 0.007 | 0.008 | 0.387 | 0.055 | 0.053 | 0.306 |
| PIP | 0.011 | 0.006 | 0.048* | 0.016 | 0.052 | 0.746 |
| HIV/STI* | 0.006 | 0.002 | 0.004** | 0.002 | 0.001 | 0.007** |
| Women | ||||||
| Neglect | −0.012 | 0.007 | 0.065 | −0.170 | 0.085 | 0.046* |
| Phys/Psy | 0.005 | 0.005 | 0.315 | 0.252 | 0.095 | 0.008** |
| Sexual | 0.066 | 0.050 | 0.187 | 0.120 | 0.103 | 0.242 |
| PV | 0.004 | 0.004 | 0.254 | 0.041 | 0.042 | 0.320 |
| PIP | 0.009 | 0.004 | 0.031* | 0.042 | 0.044 | 0.345 |
| HIV/STI* | 0.017 | 0.003 | <0.001*** | −0.002 | 0.001 | 0.267 |
Direct associations between ACE factors and mediators (early sexual debut, and IPV perpetration), between mediators and HIV/STIs, and between ACE factors and HIV/STIs
Est. unstandardized estimate, IPVP intimate partner violence perpetration, Phys/Psy physical/psychological abuse, PIP parental incarceration/psychopathology, PTSD posttraumatic stress disorder, PV witnessing parental violence, SE standard error
HIV/STIs on early sexual debut and IPV perpetration
Bolded numbers are statistically significant at
p < 0.05,
p < 0.01,
p < 0.001
Mediation Results Among Men
Mediation results among men are shown in Table 5 and Fig. 2. PTSD fully mediated the relationship between physical/psychological abuse (β = 0.0002; p = 0.012), sexual abuse (β = 0.0002; p = 0.003), parental incarceration/psychopathology (β = 0.0001; p = 0.032) and HIV/STIs. MD fully mediated physical/psychological abuse (β = 0.0003; p = 0.004), sexual abuse (β = 0.0002; p = 0.006) and HIV/STIs. SUDs fully mediated neglect (negative mediation) (β = −0.0006; p = 0.008), physical/psychological abuse (β = 0.001; p = <0.001), sexual abuse (β = 0.0004; p = 0.002), parental incarceration/psychopathology (β = 0.0000, p = 0.015) and HIV/STIs. Early sexual debut fully mediated neglect (β = −0.0002; p = 0.031), physical/psychological abuse (β = 0.0002; p = 0.015), sexual abuse (β = 0.0003; p = 0.007) and HIV/STIs. IPV perpetration fully mediated sexual abuse (β = 0.0005; p = 0.012) and HIV/STIs.
Table 5.
Unstandardized estimates of mediation pathways of adverse childhood experiences and HIV/STI diagnosis via posttraumatic stress disorder, major depression, substance use disorders, early sexual debut and intimate partner violence perpetration among men and women
| Latent variable | Posttraumatic stress disorder
|
Major depression
|
Substance use disorders
|
Early sexual debut
|
IPV perpetration
|
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| Est.a | p value | Est.a | p value | Est.a | p value | Est.a | p value | Est.a | p value | |
| Men | ||||||||||
| Neglect | 0.0001 | 0.145 | −0.0001 | 0.142 | −0.0006 | 0.008** | −0.0002 | 0.031* | −0.0002 | 0.247 |
| Physical/psychological abuse | 0.0002 | 0.012* | 0.0003 | 0.004** | 0.0010 | <0.001*** | 0.0002 | 0.015* | 0.0002 | 0.263 |
| Sexual abuse | 0.0002 | 0.003** | 0.0002 | 0.006** | 0.0004 | 0.002** | 0.0003 | 0.007** | 0.0005 | 0.012* |
| Parental violence | −0.0001 | 0.166 | −0.0001 | 0.209 | −0.0002 | 0.167 | 0.0000 | 0.411 | 0.0001 | 0.336 |
| Parental incarceration/psychopathology | 0.0001 | 0.032* | 0.0002 | 0.058 | 0.0000 | 0.015* | 0.0001 | 0.100 | 0.0000 | 0.766 |
| Women | ||||||||||
| Neglect | 0.0000 | 0.549 | −0.0002 | 0.052 | −0.0004 | 0.003** | −0.0002 | 0.078 | 0.0003 | 0.266 |
| Physical/psychological abuse | 0.0001 | 0.053 | 0.0005 | <0.001*** | 0.0005 | <0.001*** | 0.0001 | 0.317 | −0.0005 | 0.235 |
| Sexual abuse | 0.0002 | 0.267 | 0.0003 | 0.218 | 0.0003 | 0.216 | 0.0110 | 0.194 | −0.0018 | 0.388 |
| Parental violence | 0.0000 | 0.207 | −0.0002 | 0.012* | 0.0000 | 0.675 | 0.0001 | 0.267 | −0.0001 | 0.415 |
| Parental incarceration/psychopathology | 0.0000 | 0.596 | 0.0001 | 0.084 | 0.0002 | 0.028* | 0.0002 | 0.043* | −0.0001 | 0.462 |
Est. unstandardized estimate, PTSD posttraumatic stress disorder, SE standard error
Bolded numbers are statistically significant at
p < 0.05,
p < 0.01,
p < 0.001
Standard errors for all estimates are < 0.001
Fig. 2.
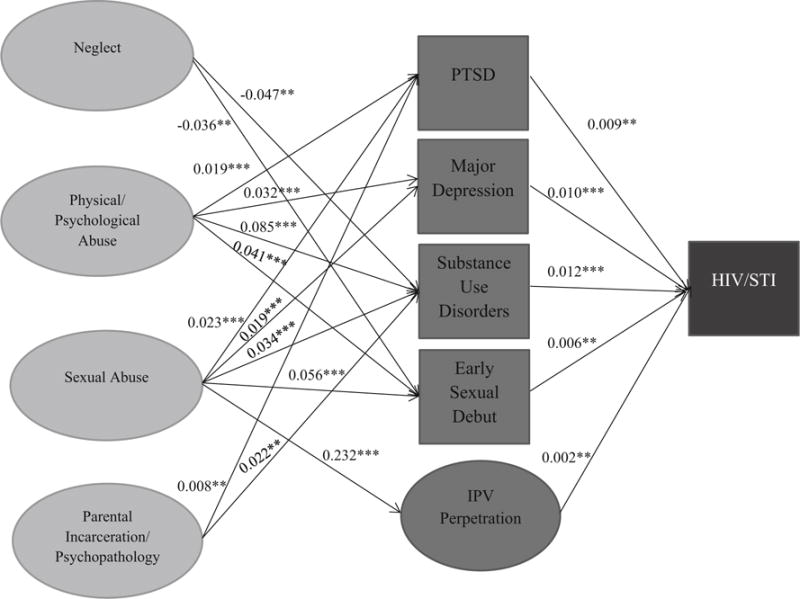
Model showing statistically significant mediational associations between adverse childhood experiences and HIV/STIs among Men. β estimates are statistically significant at *p < 0.05, **p < 0.01, ***p < 0.001. Mediator: PTSD posttraumatic stress disorder, IPV intimate partner violence; Outcome: HIV/STI HIV/sexually transmitted infection
Mediation Results Among Women
Mediation results among women are shown in Table 5 and Fig. 3. PTSD was not a statistically significant mediator between any ACE and HIV/STIs. MD fully mediated physical/psychological abuse (β = 0.0005; p = <0.001), parental violence (negative mediation) (β = −0.0002; p = 0.012) and HIV/STIs. SUDs fully mediated neglect (negative mediation) (β = −0.0004; p = 0.003), physical/psychological abuse (β = 0.0005; p = <0.001), parental incarceration/psychopathology (β = 0.0002; p = 0.028) and HIV/STIs. Early sexual debut fully mediated parental incarceration/psychopathology (β = 0.0002; p = 0.043) and HIV/STIs. IPV perpetration was not a statistically significant mediator between any ACE and HIV/STIs.
Fig. 3.
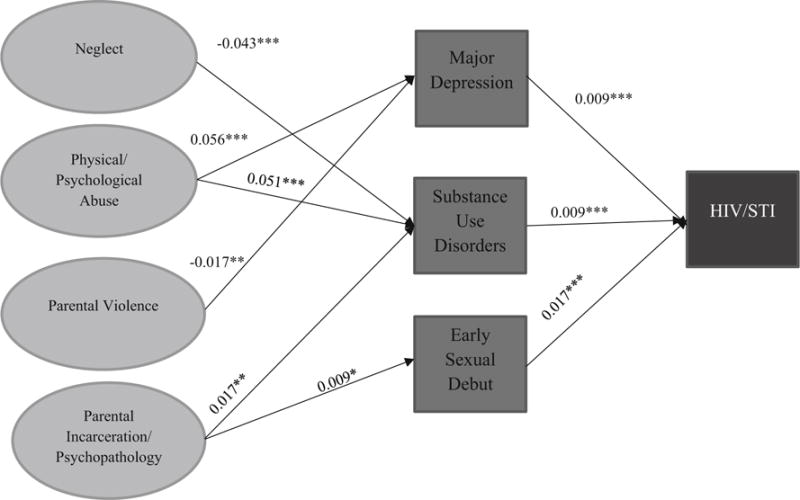
Model showing statistically significant mediational associations between adverse childhood experiences and HIV/STIs among women. β estimates are statistically significant at *p < 0.05, **p < 0.01, ***p < 0.001. Outcome: HIV/STI HIV/sexually transmitted infection
Discussion
The primary finding of this study was that the mediational roles of psychopathology and sexual behaviors in the associations between ACEs and HIV/STIs varied by sex. The non-statistically significant results between ACEs and HIV/STIs in the mediation model suggest that the effect of ACEs was explained fully through the statistically significant mediators in the model: PTSD and IPV perpetration for men, and MD, SUDs, and early sexual debut for men and women. Our results support previous findings that IPV perpetration is associated with HIV/STI diagnosis among men [77, 78]. However, there were no direct effects observed between ACEs and HIV/STIs in the mediation model, which also conflicts prior research showing that new HIV infections have been shown to be common in women who were exposed to childhood emotional [15], sexual [15, 79] and physical abuse [15, 79] but may be a function of the low prevalence estimate of HIV/STIs in the current sample.
Direct Associations Between Mediators and HIV/STIs
PTSD, MD, and SUDs were associated with HIV/STIs among women and men in the current study. These findings support previous studies, which found that depression and PTSD are associated with STI symptoms [80]. Psychological disorders may be associated with HIV/STI through their link with risky sexual behavior [81]. For example, depression, has been independently linked with risky sexual behavior [81]. Some research has shown that PTSD has not been independently linked to risky sexual behavior [81], while other studies have shown positive associations with risky behaviors such as exchange sex [27, 28], and having multiple sexual partners [28]. The current study also confirms that substance use disorders are positively associated with HIV/STI diagnosis [82–84]. It is possible that risky sexual behaviors may be used as a coping mechanism to deal with mental health and substance use disorders.
Mediational Role of Posttraumatic Stress Disorder
In the current study, the indirect effects between sexual abuse and HIV/STIs via PTSD was statistically significant among men. Victims of sexual abuse may be at risk for peritraumatic dissociation, the dissociation (the disruption or disturbance in a person’s thoughts, awareness, identity, consciousness or memory [85]) that occurs during and immediately after a traumatic exposure [86–89]. This increased risk may result in further vulnerability to PTSD [86] and consequent risk for HIV/STI diagnosis. PTSD has been found to be associated with HIV risk behavior including lack of condom use [81, 90] and using intravenous drugs, being treated for an STI, exchanging sex for money/drugs [81].
PTSD also mediated the associations between physical/psychological abuse, parental incarceration/psychopathology and HIV/STIs among men. These findings support prior research showing that PTSD mediates child trauma and adverse behavioral outcomes in men [46, 91]. In the current study, PTSD mediation of ACEs and HIV/STIs were not found in women. Cross et al., found that gender was a moderator in assessing the mediational role of PTSD between childhood trauma and alcohol and substance use, which are also risk factors for HIV/STIs. This study found that while PTSD mediated childhood trauma and alcohol and substance use for men and women, the mediation effect was stronger in men. The difference in the mediational effect of PTSD among men and women suggests that mental health consequences associated with ACEs may differ among men and women, and PTSD may play a bigger role in the structural pathway between ACEs, specifically abuse and parental incarceration/psychopathology, and HIV/STIs for men compared to women.
Mediational Role of Depression
MD mediated the relationship between sexual abuse and HIV/STIs for men but this association was not statistically significant for women. Kendler et al., showed that childhood sexual abuse had a stronger effect on MD in men compared to women [92]. The current study supports these findings as sexual abuse was statistically significantly associated with MD in men but this relationship was not significant in women. The current findings also suggest that sexual abuse may also have a stronger effect on PTSD and SUDs among men compared to women due to the direct associations between childhood sexual abuse and these disorders, as well as the mediational role of PTSD, MD, and SUDs in the association between sexual abuse and HIV/STIs.
MD also mediated physical/psychological abuse and HIV/STIs among men and women but negatively mediated witnessing parental violence and HIV/STIs among women only. Research has shown that emotional abuse was associated with depression and anxiety among men and women [93], and psychological distress has been shown to be positively associated with decreased [94] and inconsistent condom use [95], and an increase in the number of sex partners [94], which are risk factors for HIV/STIs. The negative mediation of MD between witnessing parental violence and HIV/STIs among women was driven by the negative statistically significant association between witnessing parental violence and depression. The association between witnessing parental violence and depression was not statistically significant among men. These findings differ from results from a previous study, which found a positive association between witnessing parental violence and depression among men and women [96]. However, the difference in findings could have been due to the difference in populations as the current study examined a nationally representative sample in the U.S. while Nicodimos et al., examined college students in Ethiopia. In addition, in the current study, data collected on witnessing parental violence in the current study only included violence towards the mother in the home. Therefore, witnessing violence towards the maternal figure in the home may be associated with depression more so among women than men as women are more likely to internalize their traumatic experiences.
Mediational Role of Substance Use Disorders
SUDs played a significant mediational role for men and women. SUDs significantly mediated physical/psychological abuse among men and women with positive associations between physical/psychological abuse and SUDs, and between SUDs and HIV/STIs. Research has shown that physical and emotional abuse are positively associated with drug overdose [97]. Maternal and paternal drug use, which have been linked to childhood emotional and physical abuse, respectively, are associated with earlier drug use [98].
SUDs also mediated the relationships between sexual abuse and HIV/STIs among men, and parental incarceration/psychopathology and HIV/STIs among men and women. Fuller-Thomson and colleagues found that participants who reported sexual abuse were almost three times and twice as likely to have drug and alcohol dependence, respectively, compared to participants who did not report sexual abuse [49]. Also, living with someone who has been incarcerated and who has mental health issues may be linked to substance use in adulthood as family members who were incarcerated or experienced mental health issues may have been more likely to abuse substances. This familiarity with substance use for children who were exposed to this environment may also play a role in personal substance use [99].
However, SUDs negatively mediated neglect and HIV/STIs in both groups. There was a negative association between neglect and SUDs, which contradicts previous studies. Neglect, as assessed by reporting inadequate food, clothing, medical care, inadequate supervision, and inappropriate chores was shown to be associated with substance abuse [100]. The current neglect factor did not include inappropriate chores, which may have explained the disparate findings. However, childhood maltreatment, including neglect may also be associated with resilience (experiencing adversity and then showing better emotional well-being than expected [101]) [102], which may be a protective factor of SUDs. A positive association was observed between SUDs and HIV/STI diagnosis, which has been previously established [82, 103, 104].
Mediational Role of Early Sexual Debut
Early sexual debut mediated abuse (physical/psychological and sexual) and HIV/STIs among men. The current study showed that there was a positive association between physical/psychological abuse and early sexual debut among men. Previous research has shown that sexual [105] and physical abuse [105] have been linked to early sexual debut. Prior research has also shown that early sexual debut is associated with an STI diagnosis among men [106], which supports the current study’s findings. Early sexual debut was not a statistically significant mediator between physical/psychological or sexual abuse, and HIV/STIs among women, which conflicts previous research showing a positive association between abuse and early sexual debut among women [105]. The differences in findings could have been due to the way age of sexual debut was operationalized. In the current study, age of sexual debut was operationalized as a binary variable (<15, ≥15), while in previous research, it was operationalized as a continuous variable [105].
Early sexual debut also negatively mediated neglect and HIV/STIs among men and positively mediated parental incarceration/psychopathology among women. Among men, there was a negative association between neglect and early sexual debut and a positive association between early sexual debut and HIV/STIs. Men who were neglected were more likely to have a later sexual debut compared to men who were not neglected. This finding could have been due to resilience as a result of neglect and not engaging in sexual intercourse at younger ages. Early sexual debut was not a statistically significant mediator among women as the association between neglect and early sexual debut was not statistically significant. Prior research has shown that men who are maltreated (and who may experience more neglect compared to women) may show higher resilience compared to women (who may be more likely to experience other forms of ACEs such as sexual abuse [107]. The availability of social and emotional resources plays a moderational role among men where the experience of neglect may only cause maladjustment among men if these resources are low [107]. However, among women, early sexual debut mediated parental incarceration/psychopathology. Not having parents around or having household members who may have a mental illness may result in women internalizing the loss of a loved one, which may lead to earlier sexual relationships.
Mediational Role of IPV Perpetration
IPV perpetration mediated sexual abuse and HIV/STIs among men but not among women. Among men, there were statistically significant relationships between sexual abuse and IPV perpetration, and between IPV perpetration and HIV/STIs. However, these relationships were not statistically significant among women. Previous studies have found that childhood sexual abuse is positively associated with IPV perpetration among men and women but the relationship has been found to be stronger for men [108]. Research has suggested that men, who are victims of childhood sexual abuse may be more likely to show aggression and violence against others, while women may be less likely to externalize their experience in the form of aggression and may be more likely to internalize their childhood sexual abuse experiences [108]. Male perpetrators of physical and sexual IPV tend to engage in risky sexual behavior, including main partner infidelity [109], paying money for sex [109], less condom use [110], and are more likely to be diagnosed with HIV/STIs [77, 78]. This perpetration of IPV, may result from the exertion of power over partners due to feelings of powerlessness that may have been experienced during episodes of sexual abuse during childhood. However, research is lacking in this area among women. The lack of association between IPV perpetration and HIV/STIs among women in the current study could be due to perpetration of IPV not being a significant factor in HIV risk behavior such as inconsistent condom use for women as was shown in other studies for men [109, 110].
Traumagenic Dynamics Model
The Traumagenic Dynamics model, which includes traumatic sexualization, betrayal, powerlessness and stigmatization, may help in understanding the relationship between sexual abuse and sexual health outcomes. Therefore, this model may help to explain the mediational role of PTSD, MD, SUDs, early sexual debut, and IPV perpetration between sexual abuse and HIV/STIs among men. Men who have been exposed to childhood sexual abuse, may undergo traumatic sexualization, feelings of betrayal, and stigmatization, which may result in PTSD, depression, substance abuse, early sexual relationships, and perpetration of IPV. The tendency to perpetrate IPV may be one way of exuding power due to feelings of powerlessness that resulted during childhood sexual abuse. A modified version of the Traumagenics Dynamics model including the latter three components, betrayal, powerlessness, and stigmatization, may also be used to understand the mediational role of MD, SUDs, and early sexual debut between other ACEs and HIV/STIs among men and women. Men and women may feel betrayed, powerless and may feel stigmatized due to physical and/or psychological abuse experienced during childhood, which may result in a higher likelihood of depression, substance abuse, and earlier sexual relationships, resulting in a higher likelihood to be diagnosed with HIV/STIs.
Strengths and Limitations
The study had several strengths. To date, this study is the first to examine the association between ACEs and HIV/STIs using an SEM modeling approach. Using SEM allows for the use of latent variable constructs based on a larger number of indicator variables, and testing among variables while accounting for measurement error. This study is also the first study to examine the role of mediators in the association between ACEs and HIV/STI. In considering psychosocial and behavioral mediators, this study has helped to determine key factors that may need to be considered in HIV/STI prevention program planning, such as early sexual debut and long-term social, environmental and familial events that occurred during childhood [11] as well as psychiatric and SUDs, and IPV perpetration that may have occurred with the past year.
The findings of this study should be considered with some limitations. First, the low prevalence of HIV/STIs reported may have resulted in estimates biased towards the null. Furthermore, due to the nature of the survey, we were unable to consider biomarkers for HIV/STI diagnosis. Although self-reported measures of sexual behavior and HIV/STI diagnosis have questionable validity [111, 112], reporting of STIs was found to have good reliability, excellent specificity and moderate sensitivity [113]. Second, one study suggested that ACEs are underreported among STI populations [114]. Therefore, it is possible that ACEs might have been underreported among those who were diagnosed with HIV/STI. This additional underreporting may have also contributed to biased estimates towards the null. Third, we were unable to consider potential effect measure modifiers such as sexual orientation as previous research has shown that men who have sex with men (MSM) are at increased risk for STIs [115] due to the small sample sizes of sexual minorities and of those diagnosed with HIV/STI in the study sample. Therefore, the findings presented in the current study may be more generalizable to heterosexual populations more so than sexual minority populations.
Conclusions
The main finding was that the role of psychopathology and sexual behaviors as mediators in the relationship between ACEs and HIV/STIs varied by sex. HIV/STI prevention and intervention programs should use a life course approach by addressing adverse events that may have occurred during childhood, recent depression, and substance abuse among men and women. While programs for men and women should address neglect, physical/psychological abuse, sexual abuse (and the peritraumatic dissociation that may occur as a result), parental violence, and parental incarceration/psychopathology, PTSD, depression, substance abuse, early sexual debut, and recent IPV perpetration, our findings suggest that men may also benefit greatly from prevention efforts with a focus on sexual abuse, PTSD, and IPV perpetration. Future research may include examining the association between ACEs and HIV/STIs using longitudinal studies and larger samples of respondents who have been diagnosed with HIV/STIs. Future studies should also examine the mediational roles in the relationship between ACEs and HIV/STIs by race/ethnicity and sexual orientation.
Supplementary Material
Acknowledgments
The authors would like to thank Dr. Victor Heh for his support in preparation of the manuscript.
Funding The National Epidemiologic Survey on Alcohol and Related Conditions was funded by the National Institute on Alcohol Abuse and Alcoholism with support from the National Institute on Drug Abuse. B. Mezuk is supported by the National Institute of Mental Health (K01-MH093642).
Footnotes
Electronic supplementary material The online version of this article (doi:10.1007/s10461-016-1553-0) contains supplementary material, which is available to authorized users.
Compliance with Ethical Standards
Conflict of Interest There are no potential conflicts of interest to disclose for any author.
Ethical Approval The Virginia Commonwealth University Institutional Review Board deemed the current study exempt as de-identified, secondary data were used.
Informed consent Informed consent was obtained from all individual participants included in the study.
References
- 1.Centers for Disease Control and Prevention (CDC) HIV/AIDS: basic statistics. Available at: http://www.cdc.gov/hiv/pdf/statistics_basics_factsheet.pdf. Accessed July 29, 2016.
- 2.Centers for Disease Control and Prevention (CDC) Sexually transmitted diseases (STDs): adolescents and young adults. Available at: http://www.cdc.gov/std/life-stages-populations/adolescents-YoungAdults.htm. Accessed July 29, 2016.
- 3.Centers for Disease Control and Prevention (CDC) Human papillomavirus (HPV)-associated cancers. Available at: http://www.cdc.gov/cancer/hpv/. Accessed July 29, 2016.
- 4.Ebrahim SH, Peterman TA, Zaidi AA, Kamb ML. Mortality related to sexually transmitted diseases in US women, 1973 through 1992. Am J Public Health. 1997;87:938–44. doi: 10.2105/ajph.87.6.938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta NK, Bowman CA. Managing sexually transmitted infections in pregnant women. Womens Health (Lond Engl) 2012;8:313–21. doi: 10.2217/whe.12.16. [DOI] [PubMed] [Google Scholar]
- 6.Newman L, Kamb M, Hawkes S, et al. Global estimates of syphilis in pregnancy and associated adverse outcomes: analysis of multinational antenatal surveillance data. PLoS Med. 2013;10:e1001396. doi: 10.1371/journal.pmed.1001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.International Agency for Research and Cancer. All cancers (excluding non-melanoma skin cancer): estimated incidence, mortality, and prevalence worldwide in 2012. Available at: http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx. Accessed July 29, 2016.
- 8.Centers for Disease Control and Prevention (CDC) Adverse childhood experiences reported by adults—five states, 2009. MMWR Morb Mortal Wkly Rep. 2010;59:1609–13. [PubMed] [Google Scholar]
- 9.Anda RF, Butchart A, Felitti VJ, Brown DW. Building a framework for global surveillance of the public health implications of adverse childhood experiences. Am J Prev Med. 2010;39:93–8. doi: 10.1016/j.amepre.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 10.Brown MJ, Cohen SA. Association between abusive and non-abusive adverse childhood experiences and diagnosis of cancer in Wisconsin. USA: 2013. pp. S2–008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hillis SD, Anda RF, Felitti VJ, Nordenberg D, Marchbanks PA. Adverse childhood experiences and sexually transmitted diseases in men and women: a retrospective study. Pediatrics. 2000;106:E11. doi: 10.1542/peds.106.1.e11. [DOI] [PubMed] [Google Scholar]
- 12.Ramiro LS, Madrid BJ, Brown DW. Adverse childhood experiences (ACE) and health-risk behaviors among adults in a developing country setting. Child Abuse Negl. 2010;34:842–55. doi: 10.1016/j.chiabu.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 13.Swopes RM, Simonet DV, Jaffe AE, Tett RP, Davis JL. Adverse childhood experiences, posttraumatic stress disorder symptoms, and emotional intelligence in partner aggression. Violence Vict. 2013;28:513–30. doi: 10.1891/0886-6708.vv-d-12-00026. [DOI] [PubMed] [Google Scholar]
- 14.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14:245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 15.Jewkes RK, Dunkle K, Nduna M, Jama PN, Puren A. Associations between childhood adversity and depression, substance abuse and HIV and HSV2 incident infections in rural South African youth. Child Abuse Negl. 2010;34:833–41. doi: 10.1016/j.chiabu.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. J Affect Disord. 2004;82:217–25. doi: 10.1016/j.jad.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 17.Pickles A, Aglan A, Collishaw S, Messer J, Rutter M, Maughan B. Predictors of suicidality across the life span: the Isle of Wight study. Psychol Med. 2010;40:1453–66. doi: 10.1017/S0033291709991905. [DOI] [PubMed] [Google Scholar]
- 18.Oladeji BD, Makanjuola VA, Gureje O. Family-related adverse childhood experiences as risk factors for psychiatric disorders in Nigeria. Br J Psychiatry. 2010;196:186–91. doi: 10.1192/bjp.bp.109.063677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Strine TW, Dube SR, Edwards VJ, et al. Associations between adverse childhood experiences, psychological distress, and adult alcohol problems. Am J Health Behav. 2012;36:408–23. doi: 10.5993/AJHB.36.3.11. [DOI] [PubMed] [Google Scholar]
- 20.Wu NS, Schairer LC, Dellor E, Grella C. Childhood trauma and health outcomes in adults with comorbid substance abuse and mental health disorders. Addict Behav. 2010;35:68–71. doi: 10.1016/j.addbeh.2009.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duke NN, Pettingell SL, McMorris BJ, Borowsky IW. Adolescent violence perpetration: associations with multiple types of adverse childhood experiences. Pediatrics. 2010;125:e778–86. doi: 10.1542/peds.2009-0597. [DOI] [PubMed] [Google Scholar]
- 22.Roberts AL, McLaughlin KA, Conron KJ, Koenen KC. Adulthood stressors, history of childhood adversity, and risk of perpetration of intimate partner violence. Am J Prev Med. 2011;40:128–38. doi: 10.1016/j.amepre.2010.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miller E, Breslau J, Chung WJ, Green JG, McLaughlin KA, Kessler RC. Adverse childhood experiences and risk of physical violence in adolescent dating relationships. J Epidemiol Community Health. 2011;65:1006–13. doi: 10.1136/jech.2009.105429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koblin BA, Husnik MJ, Colfax G, et al. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20:731–9. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- 25.Reisner SL, Mimiaga MJ, Skeer M, et al. Clinically significant depressive symptoms as a risk factor for HIV infection among Black MSM in Massachusetts. AIDS Behav. 2009;13:798–810. doi: 10.1007/s10461-009-9571-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Celentano DD, Valleroy LA, Sifakis F, et al. Associations between substance use and sexual risk among very young men who have sex with men. Sex Transm Dis. 2006;33:265–71. doi: 10.1097/01.olq.0000187207.10992.4e. [DOI] [PubMed] [Google Scholar]
- 27.Hutton HE, Treisman GJ, Hunt WR, et al. HIV risk behaviors and their relationship to posttraumatic stress disorder among women prisoners. Psychiatr Serv. 2001;52:508–13. doi: 10.1176/appi.ps.52.4.508. [DOI] [PubMed] [Google Scholar]
- 28.El-Bassel N, Gilbert L, Vinocur D, Chang M, Wu E. Posttraumatic stress disorder and HIV risk among poor, inner-city women receiving care in an emergency department. Am J Public Health. 2011;101:120–7. doi: 10.2105/AJPH.2009.181842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weiss NH, Tull MT, Borne ME, Gratz KL. Posttraumatic stress disorder symptom severity and HIV-risk behaviors among substance-dependent inpatients. AIDS Care. 2013;25:1219–26. doi: 10.1080/09540121.2013.764381. [DOI] [PubMed] [Google Scholar]
- 30.Lacelle C, Hebert M, Lavoie F, Vitaro F, Tremblay RE. Child sexual abuse and women’s sexual health: the contribution of CSA severity and exposure to multiple forms of childhood victimization. J Child Sex Abus. 2012;21:571–92. doi: 10.1080/10538712.2012.688932. [DOI] [PubMed] [Google Scholar]
- 31.Finkelhor D, Browne A. The traumatic impact of child sexual abuse: a conceptualization. Am J Orthopsychiatry. 1985;55:530–41. doi: 10.1111/j.1939-0025.1985.tb02703.x. [DOI] [PubMed] [Google Scholar]
- 32.Klest B, Freyd JJ, Foynes MM. Trauma exposure and post-traumatic symptoms in Hawaii: gender, ethnicity, and social context. Psychol Trauma. 2013;5:409–16. doi: 10.1037/a0029336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reichmann-Decker A, DePrince AP, McIntosh DN. Affective responsiveness, betrayal, and childhood abuse. J Trauma Dissociation. 2009;10:276–96. doi: 10.1080/15299730902956788. [DOI] [PubMed] [Google Scholar]
- 34.Cascardi M. From violence in the home to physical dating violence victimization: the mediating role of psychological distress in a prospective study of female adolescents. J Youth Adolesc. 2016;45:777–92. doi: 10.1007/s10964-016-0434-1. [DOI] [PubMed] [Google Scholar]
- 35.Bockneck EL, Sanderson J, Britner PA., IV Ambiguous loss and posttraumatic stress in school-age children of prisoners. J Child Fam Stud. 2009;18:323–33. [Google Scholar]
- 36.Widemalm M, Hjarthag F. The forum as a friend: parental mental illness and communication on open internet forums. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1601–7. doi: 10.1007/s00127-015-1036-z. [DOI] [PubMed] [Google Scholar]
- 37.Pinheiro PS. World report on violence against children. New York: United Nations; 2006. pp. 1–357. [Google Scholar]
- 38.Coffey P, Leitenberg H, Henning K, Turner T, Bennett RT. Mediators of the long-term impact of child sexual abuse: perceived stigma, betrayal, powerlessness, and self-blame. Child Abuse Negl. 1996;20:447–55. doi: 10.1016/0145-2134(96)00019-1. [DOI] [PubMed] [Google Scholar]
- 39.McElvaney R, Greene S, Hogan D. To tell or not to tell? Factors influencing young people’s informal disclosures of child sexual abuse. J Interpers Violence. 2014;29:928–47. doi: 10.1177/0886260513506281. [DOI] [PubMed] [Google Scholar]
- 40.Buckley H, Holt S, Whelan S. Listen to me! Children’s experiences of domestic violence. Child Abuse Rev. 2007;16:296–310. [Google Scholar]
- 41.Gladstone BM, Boydell KM, Seeman MV, et al. Children’s experiences of parental mental illness: a literature review. Early Interv Psychiatry. 2011;5:271–89. doi: 10.1111/j.1751-7893.2011.00287.x. [DOI] [PubMed] [Google Scholar]
- 42.Walsh K, Messman-Moore T, Zerubavel N, Chandley RB, Denardi KA, Walker DP. Perceived sexual control, sex-related alcohol expectancies and behavior predict substance-related sexual revictimization. Child Abuse Negl. 2013;37:353–9. doi: 10.1016/j.chiabu.2012.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grant BF, Dawson DA. Introduction to the national epidemiologic survey on alcohol-related conditions. Available at: http://pubs.niaaa.nih.gov/publications/arh29-2/74-78.htm. Accessed July 29, 2016.
- 44.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61:807–16. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 45.SAMSHA’s Co-Occuring Center for Excellence. The epidemiology of co-occurring substance use and mental disorders: Overview Paper. 2007;8:1–11. [Google Scholar]
- 46.Brown MJ, Perera RA, Masho SW, Mezuk B, Cohen SA. Adverse childhood experiences and intimate partner aggression in the US: sex differences and similarities in psychosocial mediation. Soc Sci Med. 2015;131C:48–57. doi: 10.1016/j.socscimed.2015.02.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.World Health Organization. Adverse childhood experiences international questionnaire (ACE-IQ) [online] Available at: http://www.who.int/violence_injury_prevention/violence/activities/adverse_childhood_experiences/questionnaire.pdf?ua=1. Accessed July 22, 2016.
- 48.Finkelhor D, Shattuck A, Turner H, Hamby S. Improving the adverse childhood experiences study scale. JAMA Pediatrics. 2013;167:70–5. doi: 10.1001/jamapediatrics.2013.420. [DOI] [PubMed] [Google Scholar]
- 49.Fuller-Thomson E, Roane JL, Brennenstuhl S. Three types of adverse childhood experiences, and alcohol and drug dependence among adults: an investigation using population-based data. Subst Use Misuse. 2016:1–11. doi: 10.1080/10826084.2016.1181089. [DOI] [PubMed] [Google Scholar]
- 50.Giovanelli A, Reynolds AJ, Mondi CF, Ou SR. Adverse childhood experiences and adult well-being in a low-income, urban cohort. Pediatrics. 2016;137 doi: 10.1542/peds.2015-4016. Epub 2016 Mar 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Glowa PT, Olson AL, Johnson DJ. Screening for adverse childhood experiences in a family medicine setting: a feasibility study. J Am Board Fam Med. 2016;29:303–7. doi: 10.3122/jabfm.2016.03.150310. [DOI] [PubMed] [Google Scholar]
- 52.Mouton CP, Hargreaves MK, Liu J, Fadeyi S, Blot WJ. Adult cancer risk behaviors associated with adverse childhood experiences in a low income population in the southeastern United States. J Health Care Poor Underserved. 2016;27:68–83. doi: 10.1353/hpu.2016.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Perez NM, Jennings WG, Piquero AR, Baglivio MT. Adverse childhood experiences and suicide attempts: the mediating influence of personality development and problem behaviors. J Youth Adolesc. 2016;45:1527–45. doi: 10.1007/s10964-016-0519-x. [DOI] [PubMed] [Google Scholar]
- 54.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Washington: DC: American Psychiatric Association; 2000. [Google Scholar]
- 55.Grant BF, Dawson DA, Hasin DS. The alcohol use disorder and associated disabilities interview schedule. DSM-IV National Institute on Alcohol Abuse and Alcoholism; Bethesda: 2001. [Google Scholar]
- 56.Ruan WJ, Goldstein RB, Chou SP, et al. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Straus M, Gelles R. Physical violence in American families: risk factors and adaptations to violence in 8,145 families. New Brunswick: NJ: Transaction Publishers; 2009. [Google Scholar]
- 58.Moffitt TE, Caspi A, Krueger RF, et al. Do partners agree about abuse in their relationship? A psychometric evaluation of interpartner agreement. Psychol Assess. 1997;9:47–56. [Google Scholar]
- 59.Finneran C, Stephenson R. Intimate partner violence, minority stress, and sexual risk-taking among US MSM. J Homosex. 2014;61:288–306. doi: 10.1080/00918369.2013.839911. [DOI] [PubMed] [Google Scholar]
- 60.Ramirez M, Paik A, Sanchagrin K, Heimer K. Violent peers, network centrality, and intimate partner violence perpetration by young men. J Adolesc Health. 2012;51:503–9. doi: 10.1016/j.jadohealth.2012.02.016. [DOI] [PubMed] [Google Scholar]
- 61.Reed E, Lawrence DA, Santana MC, et al. Adolescent experiences of violence and relation to violence perpetration beyond young adulthood among an urban sample of Black and African American males. J Urban Health. 2014;91:96–106. doi: 10.1007/s11524-013-9805-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hillis SD, Anda RF, Felitti VJ, Marchbanks PA. Adverse childhood experiences and sexual risk behaviors in women: a retrospective cohort study. Fam Plann Perspect. 2001;33:206–11. [PubMed] [Google Scholar]
- 63.Magnusson BM, Masho SW, Lapane KL. Adolescent and sexual history factors influencing reproductive control among women aged 18–44. Sex Health. 2011;8:95–101. doi: 10.1071/SH10007. [DOI] [PubMed] [Google Scholar]
- 64.Magnusson BM, Masho SW, Lapane KL. Early age at first intercourse and subsequent gaps in contraceptive use. J Womens Health (Larchmt) 2012;21:73–9. doi: 10.1089/jwh.2011.2893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.O’Donnell L, O’Donnell CR, Stueve A. Early sexual initiation and subsequent sex-related risks among urban minority youth: the reach for health study. Fam Plann Perspect. 2001;33:268–75. [PubMed] [Google Scholar]
- 66.Brown MJ, Thacker LR, Cohen SA. Association between adverse childhood experiences and diagnosis of cancer. PLoS ONE. 2013;8:e65524. doi: 10.1371/journal.pone.0065524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Harling G, Subramanian S, Ba¨rnighausen T, Kawachi I. Socioeconomic disparities in sexually transmitted infections among young adults in the United States: examining the interaction between income and race/ethnicity. Sex Transm Dis. 2013;40:575–81. doi: 10.1097/OLQ.0b013e31829529cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Adebowale AS, Titiloye M, Fagbamigbe AF, Akinyemi OJ. Statistical modelling of social risk factors for sexually transmitted diseases among female youths in Nigeria. J Infect Dev Ctries. 2013;7:17–27. doi: 10.3855/jidc.2272. [DOI] [PubMed] [Google Scholar]
- 69.Shendre MC, Tiwari RR. Social risk factors for sexually transmitted diseases. Indian J Dermatol Venereol Leprol. 2002;68:25–7. [PubMed] [Google Scholar]
- 70.Waight MT, Rahman MM, Soto P, Tran T. Sexually transmitted diseases during pregnancy in Louisiana, 2007–2009: high-risk populations and adverse newborn outcomes. J La State Med Soc. 2013;165:219–26. [PubMed] [Google Scholar]
- 71.Suhr DD. Exploratory or confirmatory factor analysis [online] Available at: http://www2.sas.com/proceedings/sugi31/200-31.pdf. Accessed July 30, 2016.
- 72.Schroeders U, Wilhelm O. Equivalence of reading and listening comprehension across test media. Educ Psychol Measur. 2011;71:849–69. [Google Scholar]
- 73.Brannick MT. Critical comments on applying covariance structure modeling. Journal of Organizational Behavior. 1995;16:201–13. [Google Scholar]
- 74.Kelloway EK. Structural equation modeling in perspective. Journal of Organizational Behavior. 1995;16:215–24. [Google Scholar]
- 75.Meade AW, Lautenschlager GJ. A Monte-Carlo study of confirmatory factor analytic tests of measurement equivalence/invariance. Struct Equ Model. 2004;11:60–72. [Google Scholar]
- 76.Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Model. 2002;9:233–55. [Google Scholar]
- 77.Decker MR, Seage GR, 3rd, Hemenway D, Gupta J, Raj A, Silverman JG. Intimate partner violence perpetration, standard and gendered STI/HIV risk behaviour, and STI/HIV diagnosis among a clinic-based sample of men. Sex Transm Infect. 2009;85:555–60. doi: 10.1136/sti.2009.036368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Raj A, Reed E, Welles SL, Santana MC, Silverman JG. Intimate partner violence perpetration, risky sexual behavior, and STI/HIV diagnosis among heterosexual African American men. Am J Mens Health. 2008;2:291–5. doi: 10.1177/1557988308320269. [DOI] [PubMed] [Google Scholar]
- 79.Houston E, Sandfort TG, Watson KT, Caton CL. Psychological pathways from childhood sexual and physical abuse to HIV/sexually transmitted infection outcomes among homeless women: the role of posttraumatic stress disorder and borderline personality disorder symptoms. J Health Psychol. 2013;18:1330–40. doi: 10.1177/1359105312464674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Harbertson J, Grillo M, Zimulinda E, et al. Prevalence of PTSD and depression, and associated sexual risk factors, among male Rwanda Defense Forces military personnel. Trop Med Int Health. 2013;18:925–33. doi: 10.1111/tmi.12129. [DOI] [PubMed] [Google Scholar]
- 81.Marshall BD, Prescott MR, Liberzon I, Tamburrino MB, Calabrese JR, Galea S. Posttraumatic stress disorder, depression, and HIV risk behavior among Ohio Army National Guard Soldiers. J Trauma Stress. 2013;26:64–70. doi: 10.1002/jts.21777. [DOI] [PubMed] [Google Scholar]
- 82.Centers for Disease Control and Prevention (CDC) HIV and substance abuse in the United States [Online] Available at: http://www.cdc.gov/hiv/risk/behavior/substanceuse.html. Accessed July 30, 2016.
- 83.Colfax G, Shoptaw S. The methamphetamine epidemic: implications for HIV prevention and treatment. Curr HIV/AIDS Rep. 2005;2:194–9. doi: 10.1007/s11904-005-0016-4. [DOI] [PubMed] [Google Scholar]
- 84.Des Jarlais DC, Arasteh K, Perlis T, et al. Convergence of HIV seroprevalence among injecting and non-injecting drug users in New York City. AIDS. 2007;21:231–5. doi: 10.1097/QAD.0b013e3280114a15. [DOI] [PubMed] [Google Scholar]
- 85.National Alliance on Mental Illness. Mental Illness: Dissociative Disorders. Available at: http://www.nami.org/Content/NavigationMenu/Inform_Yourself/About_Mental_Illness/By_Illness/Dissociative_Disorders.htm. Accessed November 10, 2014.
- 86.Yiaslas TA, Kamen C, Arteaga A, et al. The relationship between sexual trauma, peritraumatic dissociation, posttraumatic stress disorder, and HIV-related health in HIV-positive men. J Trauma Dissociation. 2014;15:420–35. doi: 10.1080/15299732.2013.873376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Cloitre M, Scarvalone P, Difede JA. Posttraumatic stress disorder, self- and interpersonal dysfunction among sexually retraumatized women. J Trauma Stress. 1997;10:437–52. doi: 10.1023/a:1024893305226. [DOI] [PubMed] [Google Scholar]
- 88.Shearer SL. Dissociative phenomena in women with borderline personality disorder. Am J Psychiatry. 1994;151:1324–8. doi: 10.1176/ajp.151.9.1324. [DOI] [PubMed] [Google Scholar]
- 89.Zlotnick C, Zakriski AL, Shea MT, et al. The long-term sequelae of sexual abuse: support for a complex posttraumatic stress disorder. J Trauma Stress. 1996;9:195–205. doi: 10.1007/BF02110655. [DOI] [PubMed] [Google Scholar]
- 90.Pengpid S, Peltzer K. Mental health, partner violence and HIV risk among women with protective orders against violent partners in Vhembe district. South Africa. Asian J Psychiatr. 2013;6:494–9. doi: 10.1016/j.ajp.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 91.Machisa MT, Christofides N, Jewkes R. Structural pathways between child abuse, poor mental health outcomes and male-perpetrated intimate partner violence (IPV) PLoS ONE. 2016;11:e0150986. doi: 10.1371/journal.pone.0150986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kendler KS, Gardner CO. Sex differences in the pathways to major depression: a study of opposite-sex twin pairs. Am J Psychiatry. 2014;171:426–35. doi: 10.1176/appi.ajp.2013.13101375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rehan W, Antfolk J, Johansson A, Santtila P. Do single experiences of childhood abuse increase psychopathology symptoms in adulthood? J Interpers Violence. 2016 doi: 10.1177/0886260516647004. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 94.Elkington KS, Bauermeister JA, Zimmerman MA. Psychological distress, substance use, and HIV/STI risk behaviors among youth. J Youth Adolesc. 2010;39:514–27. doi: 10.1007/s10964-010-9524-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Brown LK, Tolou-Shams M, Lescano C, et al. Depressive symptoms as a predictor of sexual risk among African American adolescents and young adults. J Adolesc Health. 2006;39:444.e1–e8. doi: 10.1016/j.jadohealth.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 96.Nicodimos S, Gelaye BS, Williams MA, Berhane Y. Associations between witnessing parental violence and experiencing symptoms of depression among college students. East Afr J Public Health. 2009;6:184–90. doi: 10.4314/eajph.v6i2.51764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lake S, Hayashi K, Buxton J, et al. The effect of prescription opioid injection on the risk of non-fatal overdose among people who inject drugs. Drug Alcohol Depend. 2015;156:297–303. doi: 10.1016/j.drugalcdep.2015.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Taplin C, Saddichha S, Li K, Krausz MR. Family history of alcohol and drug abuse, childhood trauma, and age of first drug injection. Subst Use Misuse. 2014;49:1311–6. doi: 10.3109/10826084.2014.901383. [DOI] [PubMed] [Google Scholar]
- 99.VanderBroek L, Acker J, Palmer AA, de Wit H, MacKillop J. Interrelationships among parental family history of substance misuse, delay discounting, and personal substance use. Psychopharmacology. 2016;233:39–48. doi: 10.1007/s00213-015-4074-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Green JG, McLaughlin KA, Berglund PA, et al. Childhood adversities and adult psychiatric disorders in The national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. 2010;67:113–23. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Daniel B. Operationalizing the concept of resilience in child neglect: case study research. Child Care Health Dev. 2006;32:303–9. doi: 10.1111/j.1365-2214.2006.00605.x. [DOI] [PubMed] [Google Scholar]
- 102.McGloin JM, Widom CS. Resilience among abused and neglected children grown up. Dev Psychopathol. 2001;13:1021–38. doi: 10.1017/s095457940100414x. [DOI] [PubMed] [Google Scholar]
- 103.El-Bassel N, Wechsberg WM, Shaw SA. Dual HIV risk and vulnerabilities among women who use or inject drugs: no single prevention strategy is the answer. Curr Opin HIV AIDS. 2012;7:326–31. doi: 10.1097/COH.0b013e3283536ab2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sogaard OS, Lohse N, Ostergaard L, et al. Morbidity and risk of subsequent diagnosis of HIV: a population based case control study identifying indicator diseases for HIV infection. PLoS ONE. 2012;7:e32538. doi: 10.1371/journal.pone.0032538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Richter L, Komarek A, Desmond C, et al. Reported physical and sexual abuse in childhood and adult HIV risk behaviour in three African countries: findings from Project Accept (HPTN-043) AIDS Behav. 2014;18:381–9. doi: 10.1007/s10461-013-0439-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Buttmann N, Nielsen A, Munk C, Frederiksen K, Liaw KL, Kjaer SK. Young age at first intercourse and subsequent risk-taking behaviour: An epidemiological study of more than 20,000 Danish men from the general population. Scand J Public Health. 2014;42:511–7. doi: 10.1177/1403494814538123. [DOI] [PubMed] [Google Scholar]
- 107.Maples LA, Park SS, Nolen JP, Rosén LA. Resilience to childhood abuse and neglect in college students. J Aggress Maltreat Trauma. 2014;23(10):1001–19. [Google Scholar]
- 108.Cubellis MA, Peterson BE, Henninger AM, Lee D. Childhood sexual abuse and antisocial traits and behaviors: a gendered examination of the factors associated with perpetration of intimate partner violence. J Interpers Violence. 2016 doi: 10.1177/0886260516633692. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 109.Hembling J, Andrinopoulos K. Evidence of increased STI/HIV-related risk behavior among male perpetrators of intimate partner violence in Guatemala: results from a national survey. AIDS Care. 2014;26:1411–8. doi: 10.1080/09540121.2014.913766. [DOI] [PubMed] [Google Scholar]
- 110.Frye V, Ompad D, Chan C, Koblin B, Galea S, Vlahov D. Intimate partner violence perpetration and condom use-related factors: associations with heterosexual men’s consistent condom use. AIDS Behav. 2011;15:153–62. doi: 10.1007/s10461-009-9659-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Harrington KF, DiClemente RJ, Wingood GM, et al. Validity of self-reported sexually transmitted diseases among African American female adolescents participating in an HIV/STD prevention intervention trial. Sex Transm Dis. 2001;28:468–71. doi: 10.1097/00007435-200108000-00009. [DOI] [PubMed] [Google Scholar]
- 112.Gallo MF, Steiner MJ, Hobbs MM, Warner L, Jamieson DJ, Macaluso M. Biological markers of sexual activity: tools for improving measurement in HIV/sexually transmitted infection prevention research. Sex Transm Dis. 2013;40:447–52. doi: 10.1097/OLQ.0b013e31828b2f77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Fisher DG, Reynolds GL, Creekmur B, Johnson ME, Deaugustine N. Reliability and criterion-related validity of self-report of syphilis. Sex Transm Dis. 2007;34:389–91. doi: 10.1097/01.olq.0000245916.45429.ec. [DOI] [PubMed] [Google Scholar]
- 114.Marcus JL, Bernstein KT, Philip S, Klausner JD. Evidence of underreporting of adverse childhood experiences, San Francisco municipal STD clinic, 2007. Sex Transm Dis. 2009;36:422–4. doi: 10.1097/OLQ.0b013e31819d72ad. [DOI] [PubMed] [Google Scholar]
- 115.Centers for Disease Control and Prevention (CDC) Sexually Transmitted Diseases: Gay, Bisexual and Other Men who Have Sex with Men. Available at: http://www.cdc.gov/std/life-stages-populations/msm.htm. Accessed October 18, 2013.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


