Abstract
Introduction
Modified-risk tobacco products are expected to reduce exposure to harmful and potentially harmful constituents of cigarette smoke, and ultimately reduce the health burden of smoking-related diseases. Clinically relevant risk markers of smoking-related diseases inform about the risk profile of new tobacco products in the absence of in-market epidemiological data. The menthol Tobacco Heating System 2.2 (mTHS) is a modified-risk tobacco product in development as an alternative to cigarettes (conventional cigarettes [CCs]).
Methods
In this parallel-group study, Japanese adult smokers (23–65 years; ≥10 mCCs/day) were randomized to mTHS, menthol CCs (mCC), or smoking abstinence (SA) for 5 days in confinement and 85 days in ambulatory settings. Endpoints included biomarkers of exposure to harmful and potentially harmful constituents and clinically relevant risk markers of smoking-related diseases.
Results
One-hundred and sixty participants were randomized to the mTHS (n = 78), mCC (n = 42), and SA (n = 40) groups. Switching to the mTHS was associated with reductions in biomarkers of exposure compared with continuing mCCs. Reductions in 8-epi-prostaglandin F2α (biomarker of oxidative stress), 11-dehydro-thromboxane B2 (biomarker of platelet activation), soluble intracellular adhesion molecule-1 (biomarker of endothelial function), and an increase in high-density lipoprotein cholesterol (biomarker of lipid metabolism) and forced expiratory volume in 1 second (biomarker of lung function) occurred in the mTHS group compared with the mCC group. The changes in the mTHS group approached those in the SA group.
Conclusions
Switching from mCCs to mTHS was associated with improvements in clinically relevant risk markers linked to mechanistic pathways involved in smoking-related diseases.
Implications
In this three-way randomized study, switching from menthol cigarettes to mTHS for 5 days in confinement and 85 days in ambulatory settings was associated with reductions in biomarkers of exposure to cigarette smoke, and changes were observed in clinically relevant biomarkers of oxidative stress (8-epi-prostaglandin F2α), platelet activity (11-dehydro-thromboxane B2), endothelial function (soluble intracellular adhesion molecule-1), lipid metabolism (high-density lipoprotein cholesterol) and lung function (forced expiratory volume in 1 second), similar to the SA group. The results suggest that switching to the mTHS has the potential to reduce the adverse health effects of conventional cigarettes.
Introduction
There is an increasing focus on developing harm reduction strategies to address the health risks of conventional cigarettes (CCs). In 2012, the US Food and Drug Administration (FDA) issued draft guidance for industry on the regulatory application of modified-risk tobacco products (MRTP).1 In this draft guidance, the FDA stated that the application “must provide scientific evidence regarding the effect of the product on the health of individuals.” As part of this application, the applicant must conduct a variety of studies to “[…] enable FDA to fully assess—whether using clinical risk endpoints in the case of a risk modification order or exposure risk endpoints in the case of an exposure modification order—the health risks of the tobacco product as compared with other consumer behaviors.”
The evidentiary standard for assessing MRTPs, as expressed in the FDA’s draft guidance, endorses the public health perspective for evaluating the population benefit-risk profile using CCs as a default comparator with a known risk profile. At the level of individual risk, ineffectiveness and lack of acceptance of the candidate MRTP nullifies the potential population benefit of the MRTP. In the context of MRTP assessment, nonclinical and clinical measures of relevance to long-term smoking-related disease that are sensitive to smoking cessation can be used to define the risk profile in premarketing settings, especially in the absence of long-term epidemiological and health outcome studies.
In the first stage of this process, it is important to conduct in vitro, in vivo, and clinical studies to first examine whether the candidate MRTP does in fact reduce exposure to harmful and potentially harmful constituents (HPHCs) of cigarette smoke, and to assess the potential toxicological effects.2
Quitting smoking is known to reduce the excess risk of severe diseases, like chronic obstructive pulmonary disease, ischemic heart disease, and cerebrovascular disease.3–5 By switching to an MRTP associated with reduced exposure to HPHCs of cigarette smoke, we might expect to see similar reductions in clinically relevant risk markers for these diseases, as observed with smoking cessation.
A recent Japanese cross-sectional study revealed marked differences in a variety of biomarkers of cardiovascular disease between smokers and nonsmokers; some were lower in smokers, such as high-density lipoprotein (HDL) cholesterol (a biomarker of lipid metabolism), and others were higher in smokers, such as fibrinogen, total white blood cell count (WBC) (biomarkers of inflammation); 8-epi-prostaglandin F2α (8-epi-PG-F2α; a biomarker of oxidative stress); and 11-dehydro-thromboxane B2 (11-DTX-B2; a biomarker of platelet activation).6 The same clinical risk endpoints were examined in this study in smokers who switched to menthol THS 2.2 (mTHS) or abstained from smoking mCC.
With the objective to develop and commercialize reduced risk products, the Tobacco Heating System 2.2 (THS) (Philip Morris International, Neuchâtel, Switzerland) was designed to reduce the formation of HPHCs by heating rather than burning tobacco. The aerosol generated by the system delivers nicotine and flavor to the user. Several studies have examined the impact of the THS (and its prototypes) on biomarker of exposure levels in non-clinical and clinical studies, and demonstrated that the system markedly reduces exposure to HPHCs from THS aerosol compared with cigarette smoke.7–10
Some studies have also investigated the impact of the THS on biologically relevant risk markers, and confirmed that this system was associated with favorable changes in biomarkers reflective of lipid metabolism and other risk markers associated with cardiovascular disease both in vitro and in vivo.8,11,12 However, results obtained in laboratory settings may not apply to humans; therefore, it is essential to verify whether switching to the THS is associated with improvements in relevant risk markers in humans, that is, with changes approaching those upon quitting all tobacco product use.
The present study was performed to examine the impact of switching to mTHS after 5 days of confinement and a further 85 ambulatory days in Japanese smokers. We conducted a three-way parallel-group study in which eligible participants were randomized to switching to mTHS, continuing menthol CCs (mCCs), or abstaining from smoking as the gold-standard for reducing the risk of smoking. The ambulatory period was included to examine the use and effects of mTHS under real-life conditions. This study was part of a clinical assessment program which assesses both the regular and the menthol variant of THS. The regular version was assessed first in two short term reduced exposure studies in confinement similar to the first part of the study reported here (NCT01959932 and NCT01970982). In addition, the assessment of the regular variant in ambulatory conditions is part of a 6-month Exposure Response study, currently underway in the United States (NCT02396381).
The primary and secondary objectives were to compare the changes in biomarkers of exposure to HPHCs. These results are described in a related article (Part 1). As part of the development of the THS and considering the FDA’s draft guidance, we also investigated its impact on biologically and clinically relevant risk markers. These results are presented in this article.
Methods
This study was performed in accordance with International Conference on Harmonization, Good Clinical Practice, the Declaration of Helsinki guidelines,13,14 national regulations, and was approved by the local Institutional Review Board in July 2013 before starting the study. The study was conducted at the Tokyo Heart Center Osaki Hospital and registered at ClinicalTrials.gov (identifier NCT01970995).
Participants
Japanese male and female smokers aged 23–65 years with a body mass index of 18.5–32 kg/m2 who reported having smoked ≥10 commercially available mCCs per day for ≥4 weeks, and had smoked for ≥3 years were eligible. Individuals with clinically relevant diseases or a history of alcohol and/or drug abuse, and pregnant or breastfeeding females or females unwilling to use acceptable methods of effective contraception were excluded from the study. Additional eligibility criteria are listed in Table 1.
Table 1.
Eligibility Criteria
| Inclusion criteria |
|---|
| Provided signed informed consent and could understand the subject information sheet |
| Age 23–65 y |
| Body mass index 18.5–32 kg/m2 |
| Japanese ethnicity |
| Healthy smoker, as judged by the principal investigator based on data collected at the screening visit |
| Smoked ≥10 mCCs per day with a maximum ISO yield of 1 mg for the previous 4 weeks (self-reported) and had smoked for ≥3 consecutive years |
| No plan to quit smoking in the next 3 months |
| Ready to stop smoking for up to 90 days |
| Ready to use the mTHS 2.2 |
| Exclusion criteria |
| The principal investigator judged the participant to be unable to participate for any reason (medical, psychiatric, and/or social reason) |
| Legally incompetent, physically or mentally incapable of giving consent |
| Medical condition requiring smoking cessation, or clinically relevant disease |
| Medical condition that required or would have required in the course of the study a medical intervention (eg, start of treatment, surgery, or hospitalization), which would have interfered with study participation and/or study results |
| Use of nicotine-containing products (other than mCCs) or electronic cigarettes/similar devices within 4 weeks prior to enrollment |
| Administration of drugs likely to affect CYP1A2 or CYP2A6 activity within 14 days or five half-lives of the drug (whichever was longer) before Day −2 |
| Administration of drugs within 14 days of Day −2 that the principal investigator thought was likely to interfere with the study objectives or the participant’s safety |
| Concomitant use of non-steroidal anti-inflammatory drugs (NSAIDs) or acetylsalicylic acid |
| Positive alcohol test and/or history of alcohol abuse that could have interfered with participation in the study |
| Positive urine drug test |
| Positive serology test for human immunodeficiency virus 1/2, hepatitis B, or hepatitis C virus |
| Donation/receipt of whole blood/blood products within 3 months prior to admission |
| Current or former employee of the tobacco industry, or of their first-degree relatives (parent, sibling, or child) |
| Employee of the investigational site, or any other parties involved in the study, or of their first-degree relatives (parent, sibling, or child) |
| Participation in a clinical study within 3 months before screening |
| Participation in the same study at a different time (ie, each subject could be included in the study population only once) |
| Pregnant/breast feeding women |
| Women who were unwilling to use an acceptable method of contraception |
ISO = International Organization for Standardization; mCC = menthol cigarettes; mTHS = menthol Tobacco Heating System 2.2.
Products
The mTHS (2.62 mg/stick menthol, 1.21 mg/stick nicotine and 3.94 mg/stick of glycerin used as aerosol former, obtained under Health Canada Intense smoking regimen, maximum heating temperature 350°C) was used in this study. Reference products were mCCs of the participant’s preferred commercially available brand.
Study Design and Interventions
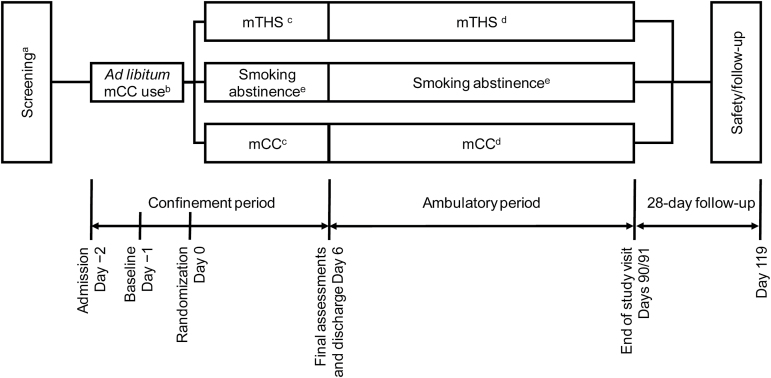
The study comprised a 4-week screening period (Days −30 to −3), an 8-day confinement period (Days −2 to Day 6), an 85-day ambulatory period (Days 6 to 91), and a 28-day safety follow-up period (Figure 1). On Day −2, the participants were admitted to the confinement unit to confirm eligibility, and were enrolled after trying the mTHS and reporting their willingness to use it during the study. Baseline assessments were made on Days −1 and 0 during which the participants smoked their own brand of mCCs. On Day 1, the participants were randomized (in a 2:1:1 ratio) to switch to mTHS (mTHS group), to continue smoking mCCs (mCC group), or to smoking abstinence (SA), with the randomization stratified by sex and daily average mCC consumption (10–19 vs. > 19 mCCs/day) over the previous 4 weeks. Between Days 1 and 5, participants in the mTHS and mCC groups exclusively used the allocated product ad libitum during the designated smoking hours (06:30 AM to 11:00 PM) while participants in the SA group completely abstained from smoking. Participants were discharged on Day 6 after clinical and safety assessments. During the 85-day ambulatory period, the participants returned to the study site and stayed overnight on the Day 30, 60, and 90 visits.
Figure 1.
Study design. aThe screening visit was scheduled 1–4 weeks before enrollment, and included trial use of the mTHS. bThe participants continued using their preferred mCCs. cmTHS and mCC dispensed to the participant according to the product allocation; ad libitum use was allowed. dThe participants used the mTHS or mCC according to the product allocation for ad libitum use. Dual use of mTHS and mCC was possible in the mTHS group, but not in the mCC group. eThe participants were asked to abstain from smoking and were provided with psychological support during the period of abstinence. The use of mTHS was strictly forbidden for participants in the SA group for the whole study duration. mCC = menthol cigarettes; mTHS = menthol Tobacco Heating System 2.2.
All participants purchased their own mCCs throughout the study and were asked to bring sufficient mCCs to last during the confinement period. The participants were not reimbursed for the costs of their mCCs. The mTHS and mCCs were dispensed to the participants during the confinement period and the number of items dispensed was logged. During the ambulatory period, participants were provided with anticipated amounts of mTHS to cover the period until the next study visit. Participants in the mTHS group were asked to return any empty or partially used packs for study accountability during the ambulatory period. Participants were encouraged to adhere to their allocated product but dual use of mTHS and mCCs was possible in the mTHS group during the ambulatory period. Participants in the mCC and SA groups were prohibited from using mTHS, the latter being provided psychological support, if requested. For compliance assessment, daily tobacco product use was recorded in a log (confinement period with strict product dispensation) and in electronic diaries (ambulatory period), and exhaled CO was measured in SA group participants throughout the study. In the SA group, full abstinence required no use of any tobacco product and CO levels not exceeding 10 ppm, the use of nicotine replacement therapy being allowed.
Endpoints and Study Measures
Table 2 lists the clinically relevant risk markers reported in this article, as well as relevant demographic and exposure variables, including the times at which each variable was recorded. The following clinically relevant risk markers were measured: Oxidative stress—8-epi-PGF2α; platelet activity—11-DTX-B2; endothelial function—soluble intracellular adhesion molecule-1 (sICAM-1); lipid metabolism—HDL cholesterol, low-density lipoprotein (LDL) cholesterol, triglycerides, and total cholesterol; inflammation—total WBC; cardiovascular risk/function—homocysteine, high-sensitivity C-reactive protein (hs-CRP), fibrinogen, systolic blood pressure, and diastolic blood pressure; and metabolic syndrome—blood glucose, hemoglobin A1c (HbA1c), body weight, and waist circumference. All clinical laboratory endpoints were measured at independent contract laboratories, blinded to the randomized group allocation.
Table 2.
List of Clinically Relevant Risk Markers Reported in the Present Manuscript and Timing of Measurement
| Variable | Matrix | Screening | Confinement period | Ambulatory period | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Day −30 to −3 | −2 | −1 | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 30 | 31 | 60 | 61 | 90 | 91 | ||
| Safety-related variables | |||||||||||||||||
| Vital signs | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ||||
| Body height and weight | ● | ● | ● | ● | ● | ● | |||||||||||
| Waist circumference | ● | ● | |||||||||||||||
| Hematology, clinical chemistry, urinalysis | Blood/urine | ● | ● | ● | ● | ● | ● | ||||||||||
| Biomarkers of exposure | |||||||||||||||||
| COHb | Blood | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ||||||
| Urinary biomarkers of exposure | Urine | ● | ● | ● | ● | ● | ● | ● | ● | ● | ● | ||||||
| Risk markers and other clinical markers | |||||||||||||||||
| hs-CRP, fibrinogen, homocysteine, LDL cholesterol, HDL cholesterol | Blood | ● | ● | ● | ● | ||||||||||||
| sICAM-1 | Blood | ● | ● | ● | ● | ● | |||||||||||
| HbA1c | Blood | ● | ● | ||||||||||||||
| 8-epi-PGF2α and 11-DTX-B2 | Urine | ● | ● | ● | ● | ● | |||||||||||
COHb = carboxyhemoglobin; HbA1c = hemoglobin A1c; HDL = high-density lipoprotein; hs-CRP = high-sensitivity C-reactive protein; LDL = low-density lipoprotein; sICAM-1 = soluble intercellular adhesion molecule-1; 8-epi-PGF2α = 8-epi-prostaglandin F2α; 11-DTX-B2 = 11-dehydro-thromboxane B2. The other variables assessed in this study are listed in the accompanying publication. Only results at baseline (Day 0) and Day 90/91 are reported here.
Lung function was assessed spirometrically as the forced expiratory volume in 1 second (FEV1). Spirometry with and without a short-acting bronchodilator was performed at the screening visit at least 1 hour after smoking to evaluate inclusion/exclusion criteria (ie, post-bronchodilator function) with the testing done without a bronchodilator first. Furthermore, spirometry without a bronchodilator was performed prior to product use on Day 0 (baseline), and on Day 6, and at the Day 90 visit (Day 91) for comparison with the baseline values. For spirometry testing the 2005 testing and quality recommendations by the American Thoracic Society/European Respiratory Society Joint Task Force on the standardization of spirometry along with the electronic data submission and documentation processes were followed. Spirometry predicted values were standardized to the NHANES III predicted set. All personnel performing spirometry testing were appropriately trained. The FEV1 and forced vital capacity (FVC) were recorded and the ratio of FEV1/FVC calculated.
Statistical Analysis
The sample size was calculated based on the expected mTHS:mCC ratios of the concentrations of biomarkers of exposure, as observed in previous studies of heated tobacco products (NCT01780714 [unpublished data] and NCT01780688). A sample size of 160 participants randomized 2:1:1 to the mTHS, mCC, and SA groups, respectively, was considered sufficient to attain 80% power to show reductions of ≥50% in the biomarkers of exposure chosen as the primary endpoints (Total 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol [Total NNAL], COHb, monohydroxybutenyl mercapturic acid [MHBMA], 3-hydroxypropylmercapturic acid [3-HPMA], and S-phenylmercapturic acid [S-PMA]) in the mTHS group compared with the mCC group, using a one-sided test with 2.5% alpha level.
The primary analysis was conducted in the per-protocol (PP) set, which comprised all randomized subjects who were compliant to their randomized group, had not been mis-randomized, and had no major protocol deviations impacting evaluability. PP criterion in the mTHS and SA groups was no use of more than two CCs during a single day and no average daily use of more than 0.5 CCs. Missing values for the biomarkers were imputed using last observation carried forward. Non-normally distributed variables were natural log-transformed before analysis, and the results were back-transformed for presentation. Urine markers were analyzed adjusted for creatinine. The risk markers measured at baseline were summarized and Day 90 values were compared among the three groups by analysis of covariance adjusting for the baseline value, sex, and daily average mCC consumption at baseline. The least square (LS) mean differences (mTHS − mCC) or ratios (mTHS:mCC), 95% confidence intervals as well as, for descriptive purposes, p-values were calculated without adjustment for multiple comparisons.
Results
Participants
A total of 670 individuals were screened at two study sites, of which 231 tried the mTHS and 216 were enrolled and randomized. Of these, one subject was discontinued for meeting an exclusion criterion and 55 were discontinued following the closure of one of the two study sites due to non-compliance with sample collection and data recording procedures. The study was conducted and completed between August 2013 and July 2014 at the Tokyo Heart Center Osaki Hospital, Tokyo, Japan.
The full analysis set comprised 160 participants, with 78, 42, and 40 participants randomized to the mTHS, mCC, and SA groups, respectively. Two, one, and two participants in the mTHS, mCC, and SA groups, respectively, voluntarily discontinued.
The rates of compliance to the allocated interventions were high; 70 (89.7%), 41 (97.6%), and 37 (92.5%) of randomized participants in the mTHS, mCC, and SA groups, respectively, were included in the PP set at Day 90. Dual use of mTHS and mCC during the ambulatory period was very limited, and the daily use of mCC was low (mean 0.1 mCCs/day) in the mTHS group during the ambulatory period.
As described in the co-publication (Part 1), exposure to HPHCs was markedly lower in the mTHS group than in the mCC group. Of note, the total 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol, carboxyhemoglobin, monohydroxybutenyl mercapturic acid, 3-hydroxypropylmercapturic acid, and S-phenylmercapturic acid concentrations (primary endpoints) were 56%, 55%, 87%, 49%, and 89% lower, respectively, in the mTHS group than in the mCC group on Day 5. These reductions were maintained until the end of the ambulatory period. The changes in these biomarkers of exposure in the mTHS group were similar to those in the SA group.
Oxidative Stress
Table 3 shows the biomarker concentrations at baseline and on the Day 90 visit. At baseline, the 8-epi-PGF2α concentrations were similar in all three groups. The 8-epi-PGF2α concentration at Day 90 was 12.7% lower in the mTHS group than in the mCC group. The LS mean values were similar in the mTHS and SA groups.
Table 3.
Changes in Risk Markers (Part 1)
| mTHS | mCC | Smoking abstinence | mTHS vs. mCC | mTHS vs. SA | |
|---|---|---|---|---|---|
| Geometric mean (95% CI) | Geometric mean (95% CI) | Geometric mean (95% CI) | LS mean ratio (%) (95% CI) [p] | LS mean ratio (%) (95% CI) [p] | |
| Endothelial dysfunction | |||||
| sICAM-1 (ng/ml) | |||||
| Baseline | 222.92 (205.10; 242.28) | 198.70 (171.01; 230.86) | 207.89 (176.09; 245.42) | ||
| Day 90 | 188.43 (176.13; 201.59) | 188.40 (163.69; 216.83) | 174.07 (149.35; 202.88) | 91.28 (85.06; 97.95) [.0116] | 102.41 (95.24; 110.12) [.5180] |
| Oxidative stress | |||||
| 8-epi-PGF2α (pg/mg Cr) | |||||
| Baseline | 201.95 (186.30; 218.92) | 202.65 (183.33; 224.00) | 198.47 (176.89; 222.68) | ||
| Day 90 | 194.40 (177.99; 212.32) | 222.48 (203.07; 243.75) | 206.59 (178.59; 238.98) | 87.29 (78.19; 97.45) [.0159] | 92.78 (82.80; 103.96) [.1947] |
| Platelet activation | |||||
| 11-DTX-B2 (pg/mg Cr) | |||||
| Baseline | 580.41 (531.09; 634.32) | 533.13 (487.32; 583.24) | 604.77 (540.20; 677.06) | ||
| Day 90 | 498.22 (447.54; 554.63) | 515.18 (466.99; 568.35) | 450.76 (398.12; 510.37) | 91.02 (80.48; 102.94) [.1327] | 112.89 (99.47; 128.12) [.0603] |
| Cardiovascular risk factors | |||||
| Fibrinogen (mg/dL) | |||||
| Baseline | 279.19 (266.68; 292.28) | 276.16 (259.93; 293.40) | 284.47 (268.74; 301.12) | ||
| Day 90 | 275.91 (262.37; 290.14) | 286.14 (267.36; 306.24) | 277.63 (262.27; 293.88) | 94.58 (87.87; 101.80) [.1360] | 99.39 (91.98; 107.40) [.8764] |
| Homocysteine (µmol/L) | |||||
| Baseline | 10.39 (9.30; 11.61) | 10.94 (9.39; 12.75) | 11.34 (9.41; 13.68) | ||
| Day 90 | 11.57 (10.37; 12.90) | 12.05 (10.31; 14.08) | 12.89 (10.74; 15.46) | 100.66 (93.35; 108.54) [.8638] | 97.03 (89.75; 104.91) [.4463] |
| hs-CRP (mg/L) | |||||
| Baseline | 0.20 (0.15; 0.25) | 0.17 (0.13; 0.23) | 0.22 (0.14; 0.34) | ||
| Day 90 | 0.24 (0.18; 0.32) | 0.25 (0.16; 0.37) | 0.23 (0.16; 0.33) | 93.59 (62.23; 140.75) [.7487] | 110.74 (72.67; 168.76) [.6328] |
| Metabolic syndrome | |||||
| Glucose (mg/dL) | |||||
| Baseline | 84.9 (83.0; 86.9) | 85.4 (83.5; 87.3) | 85.3 (82.9; 87.8) | ||
| Day 90 | 89.8 (87.7; 91.8) | 91.1 (89.1; 93.1) | 87.6 (85.1; 90.1) | 98.98 (96.42; 101.60) [.4370] | 102.80 (100.06; 105.61) [.0447] |
CI = confidence interval; Cr = creatinine; hs-CRP = high-sensitivity C-reactive protein; mCC = menthol cigarettes; mTHS = menthol Tobacco Heating System 2.2; SA = smoking abstinence; sICAM-1 = soluble intercellular adhesion molecule-1; 8-epi-PGF2α = 8-epi-prostaglandin F2α; 11-DTX-B2 = 11-dehydro-thromboxane B2.
Platelet Activity
The baseline 11-DTX-B2 concentrations differed slightly between the three groups at baseline, with the lowest mean values initially observed in the mCC group with slightly lower values than in the mTHS and SA groups (Table 3). 11-DTX-B2 on Day 90 was 9.0% lower in the mTHS group than in the mCC group, although the concentration remained higher in the mTHS group than in the SA group (Table 3).
Endothelial Dysfunction
The sICAM-1 concentration was slightly lower in the mCC group than in the other groups at baseline (Table 3). On Day 90, the sICAM-1 concentration was 8.7% lower in the mTHS group than in the mCC group, and a similar reduction was observed in the SA group.
Lipid Metabolism
Markers of lipid metabolism included HDL cholesterol, LDL cholesterol, total cholesterol, and triglycerides. As shown in Table 4, the baseline concentrations of these lipids were similar among the three groups, except for triglycerides, which was lower in the SA group than in the other groups. The LS mean HDL cholesterol concentration on Day 90 was 4.5 mg/dL higher in the mTHS group than in the mCC group. The magnitude of the increase in the mTHS group was slightly less than that in the SA group (LS mean difference mTHS − SA: −1.8 mg/dL). The triglyceride concentration decreased between baseline and Day 90 in the mTHS group but increased in the mCC and SA groups, resulting in LS mean differences of −6.3 mg/dL (mTHS−mCC) and −18.7 mg/dL (mTHS − SA). Total cholesterol decreased similarly in the mTHS and mCC groups, but increased in the SA group. There were no marked differences in LDL cholesterol, total cholesterol, and triglycerides concentrations between the mTHS and mCC groups (Table 4).
Table 4.
Changes in Risk Markers (Part 2)
| mTHS | mCC | SA | mTHS vs. mCC | mTHS vs. SA | |
|---|---|---|---|---|---|
| Arithmetic mean (95% CI) | Arithmetic mean (95% CI) | Arithmetic mean (95% CI) | LS mean difference (95% CI) [p] | LS mean difference (95% CI) [p] | |
| Inflammation | |||||
| WBC (GI/L) | |||||
| Baseline | 5.90 (5.60; 6.19) | 5.76 (5.34; 6.20) | 6.40 (5.75; 7.04) | ||
| Day 90 | 5.54 (5.24; 5.83) | 6.04 (5.54; 6.54) | 5.94 (5.44; 6.44) | −0.57 (−1.03; −0.1) [.0173] | −0.16 (−0.65; 0.33) [.5113] |
| Lipid metabolism | |||||
| LDL Cholesterol (mg/dL) | |||||
| Baseline | 121.3 (113.0; 129.7) | 123.3 (111.3; 135.2) | 111.1 (102.6; 119.6) | ||
| Day 90 | 113.4 (104.7; 122.1) | 114.1 (104.7; 123.6) | 110.5 (102.3; 118.7) | 0.9 (−6.6; 8.3) [.8162] | −4.7 (−12.5; 3.0) [.2270] |
| HDL Cholesterol (mg/dL) | |||||
| Baseline | 56.9 (53.8; 60.0) | 60.0 (55.0; 65.1) | 58.4 (53.8; 63.0) | ||
| Day 90 | 60.3 (56.5; 64.2) | 58.5 (53.8; 63.3) | 63.5 (58.4; 68.6) | 4.5 (1.1; 7.9) [.0084] | −1.8 (−5.3; 1.7) [.2944] |
| Triglycerides (mg/dL) | |||||
| Baseline | 139.5 (123.1; 156.0) | 131.5 (115.3; 147.7) | 112.8 (98.8; 126.8) | ||
| Day 90 | 138.5 (120.4; 156.7) | 137.2 (123.0; 151.5) | 133.1 (110.5; 155.7) | −6.3 (−21.2; 8.7) [.4095] | −18.7 (−34.4; −2.9) [.0199] |
| Total cholesterol (mg/dL) | |||||
| Baseline | 197.5 (188.9; 206.1) | 201.4 (188.2; 214.6) | 184.4 (174.8; 194.0) | ||
| Day 90 | 191.1 (181.9; 200.3) | 192 (181.7; 202.3) | 189.9 (180.8; 199.1) | 2.0 (−6.7; 10.7) [.6499] | −8.3 (−17.35; 0.75) [.0719] |
| Metabolic syndrome | |||||
| Hemoglobin A1c (%) | |||||
| Baseline | 5.17 (5.10; 5.25) | 5.23 (5.14; 5.32) | 5.22 (5.13; 5.32) | ||
| Day 90 | 5.17 (5.09; 5.26) | 5.20 (5.09; 5.32) | 5.18 (5.08; 5.27) | 0.02 (−0.06; 0.10) [.5866] | 0.04 (−0.04; 0.12) [.2981] |
| Body weight (kg) | |||||
| Baseline | 62.35 (59.70; 65.01) | 62.01 (58.74; 65.29) | 62.24 (58.56; 65.91) | ||
| Day 90 | 62.67 (60.00; 65.34) | 62.41 (59.12; 65.71) | 63.79 (60.05; 67.53) | −0.09 (−0.75; 0.57) [.7926] | −1.24 (−1.92; −0.56) [.0004] |
| Waist circumference (cm) | |||||
| Baseline | 87.1 (81.0; 93.1) | 91.0 (81.3; 100.7) | 86.0 (77.6; 94.4) | ||
| Day 90 | 81.0 (77.6; 84.5) | 80.2 (77.9; 82.6) | 80.8 (77.5; 84.1) | 1.6 (−2.4; 5.6) [.4251] | 0.1 (−4.0; 4.2) [.9684] |
| Cardiovascular risk factors | |||||
| Systolic blood pressure (mmHg) | |||||
| Baseline | 110.2 (107.4; 112.9) | 111.0 (107.8; 114.2) | 104.7 (102.2; 107.3) | ||
| Day 90 | 104.2 (101.5; 106.9) | 105.5 (101.3; 109.6) | 102.2 (99.3; 105.2) | −0.59 (−3.80; 2.62) [.7157] | −0.76 (−4.16; 2.65) [.6607] |
| Diastolic blood pressure (mmHg) | |||||
| Baseline | 67.0 (64.8; 69.3) | 67.5 (65.2; 69.8) | 64.0 (62.0; 66.0) | ||
| Day 90 | 62.8 (60.7; 64.9) | 63.9 (61.0; 66.8) | 62.7 (60.5; 64.9) | −0.68 (−3.04; 1.69) [.5705] | −1.68 (−4.16; 0.79) [.1800] |
| Lung function | |||||
| FEV1 (%pred) | |||||
| Baseline | 94.08 (92.25; 95.92) | 93.46 (89.94; 96.96) | 92.65 (89.46; 95.84) | ||
| Day 91 | 95.54 (93.63; 97.44) | 94.02 (91.18; 96.85) | 94.18 (90.38; 97.97) | 1.91 (−0.14; 3.97) [.0669] | −0.02 (−2.15; 2.11) [.9848] |
CI = confidence interval; FEV1 = forced expiratory volume in 1 second; HDL = high-density lipoprotein; LDL = low-density lipoprotein; mCC = menthol cigarettes; mTHS = menthol Tobacco Heating System 2.2; SA = smoking abstinence; WBC = white blood cell count.
Inflammation
Although there was some variability at baseline, WBC decreased in the mTHS group and increased in the mCC group, resulting in a LS mean difference of −0.57 GI/L at Day 90 (Table 3). The reduction in WBC was slightly smaller in the mTHS group than in the SA group.
Cardiovascular Risk and Function
Several markers of cardiovascular risk and function were examined, including hs-CRP, fibrinogen, homocysteine, and blood pressure. As shown in Table 3, the hs-CRP concentration on Day 90 was 6.4% lower in the mTHS group than in the mCC group, but was 10.7% higher in the mTHS group than in the SA group (mTHS:mCC and mTHS:SA ratios). There were no apparent differences in fibrinogen, homocysteine (Table 3), or blood pressure (Table 4) among the three groups.
Metabolic Syndrome
The glucose concentrations increased similarly between baseline and Day 90 in all three groups (Table 3), and there were no apparent differences in HbA1c and waist circumference (Table 4) among the three groups at baseline or at Day 90.
Lung Function
At the Day 90 visit FEV1 showed an increase of 1.91 (−0.14, 3.97) %pred in the mTHS group compared to the mCC group, comparable to the values observed in the SA group (Table 4).
Discussion
This randomized, three-arm parallel-group study showed that switching from mCCs to mTHS was associated with improvements in clinically relevant risk markers, especially HDL-cholesterol, sICAM-1, 8-epi-PGF2α, 11-DTX-B2 and FEV1 as compared with continuing mCCs in Japanese adult smokers. The improvements in these markers approached those observed in the SA group which was included in this study as a gold-standard to evaluate the risk reduction associated with smoking cessation, and to examine whether the changes in the risk markers after switching to an MRTP mimic those associated with eliminating all tobacco product-related exposure. The changes in risk markers accompanied marked changes in biomarkers of exposure, which were apparent within 5 days of product use in confinement and were maintained for 85 days in ambulatory settings, as described in the co-publication (Part 1). As the analysis of clinical risk markers was descriptive, the findings require confirmation from separate clinical research.
The FDA highlights the assessment of clinical risk markers1 while the Institute of Medicine report refers to intermediate clinical effects.2 The clinical risk endpoints were selected from multiple clinical risk components across several biological processes, physiological systems, and mechanisms associated with smoking-related diseases, including inflammation, oxidative stress, platelet activation, lipid metabolism and lung function. Their selection was based on (1) epidemiological evidence suggesting a robust relationship between the clinical risk endpoint and at least one known smoking-related health outcome; (2) clinical evidence linking cigarette smoking to the clinical risk endpoint (consistent with the epidemiological evidence); and (3) clinical evidence linking smoking cessation to the reversibility of the endpoint. Many of the clinical risk markers evaluated in this study are described in the 2010 Surgeon General Report.15 (cf. Supplementary Material for a detailed list of references).
Several studies, including those by Miura et al.16 and Sakaguchi et al.,17 have evaluated the effects of MRTPs on biomarkers of exposure, but they did not examine the effects on clinical risk markers.
The present results are broadly consistent with those reported by Ogden et al., who compared tobacco-heating cigarettes, snus and ultra-low machine yield tobacco-burning cigarettes.18–20 Ogden et al. evaluated similar biomarkers of risk, and noted that switching to tobacco-heating cigarettes was associated with reductions in platelets, sICAM-1, and WBC, while (±)5-iPF2a-VI (another F2-isoprostane) decreased after switching to ultra-low machine yield cigarettes.20
In another study of relevance, Roethig et al. randomized adult smokers to either an electrically heated cigarette smoking system (EHCSS) or to continue CCs for 12 months.21 Similar to our study, they reported that switching to the EHCSS was associated with reductions in biomarkers of exposure, including nicotine equivalents, plasma cotinine, total 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol, total 1-hydroxypyrene, urine mutagenicity, 4-aminobiphenyl hemoglobin adducts, carboxyhemoglobin, and 3-hydroxypropylmercapturic acid, and these changes were accompanied by improvements in total white blood cell count, hemoglobin, hematocrit, 11-DTX-B2, and HDL-cholesterol.
A recent Japanese cross-sectional study showed that many clinically relevant risk markers were markedly elevated in smokers as compared to nonsmokers.6 Accordingly, the changes in risk markers observed in our study, and in the studies by Ogden et al.20 and Roethig et al.,21 suggest that reduced exposure to HPHCs after switching to an MRTP translated into improvements in risk markers similar to those associated with smoking cessation. The sensitivity of the majority of the risk markers to smoking status is further elucidated by reviewing the ratio and difference effects of nonsmokers versus smokers, based on the Japanese cross-sectional study publication,6 in conjunction with the corresponding mTHS versus mCC results of the present study. Across all risk markers investigated in both studies, the results were fully consistent in direction and largely in size, with no or small effects observed for homocysteine and LDL in both studies. The cross-sectional study effects of fibrinogen, hs-CRP and HDL were within the 95% confidence intervals of the present study. After 90 days of switching from mCC to mTHS, 11-DTX-B2 reached about one third and 8-epi-PGF2α, SICAM-1 and WBC about half of the corresponding effect observed in the cross-sectional comparison of nonsmokers and smokers.
Lung function is defined by ventilation capacity, airway resistance and gas exchange capacity and influenced by lung elasticity and lung surface tension. A main characteristic of chronic pulmonary diseases such as COPD is the loss of lung elasticity, which develops gradually as a consequence of increased inflammatory responses and structural abnormalities such as increased thickness of the airway walls.22–24 Airway resistance and a reduction in lung elasticity eventually lead to expiratory airflow limitation, the hallmark and earliest sign of COPD, resulting in delayed emptying and hyperinflation of the lung characterized by an increased residual volume (RV),25,26 ultimately resulting in a decrease in vital capacity and FEV1.27
Several studies have shown that subclinical inflammatory changes in small airways exist years before the advanced stages of COPD.23,28–31 Although relatively few longitudinal studies have assessed the effects of smoking cessation on inflammation in smokers without chronic respiratory symptoms, these studies demonstrated that the inflammatory response decreased rapidly within the first few months after smoking cessation. Considering these earlier findings, it seems likely that the favorable changes in lung function as assessed by FEV1 in the present study may be best explained by a decrease in the inflammatory state of the lung when switching from mCCs to mTHS, similar to the changes observed following smoking cessation.
With respect to risk reduction, including the risk of cardiovascular disease, the results of short-term studies, such as ours, cannot demonstrate whether switching to a candidate MRTP translates into disease risk reduction. However, it is important to measure surrogate markers which are fit for the purpose of MRTP risk assessment in short-term studies in order to predict the risk reduction profile and the potential effects of longer-term use32 compared to continued cigarette smoking. They can subsequently be supported by larger confirmatory studies. Such cumulative and consistent evidence, covering multiple clinically relevant endpoints and related biological processes, physiological systems, and mechanisms, will provide a strengthened empirical basis of a candidate MRTP evaluation.
Some limitations of the present study warrant mentioning, including the potential for dual use (mTHS group) and restarting cigarette smoking (SA group) in the ambulatory phase, which may confound the results obtained in this period. However, the inclusion of a confinement period in which mTHS and mCC were distributed strictly according to randomization ensured that the products were used as allocated in this period. The same reduction in exposure observed under these very controlled conditions was sustained in an ambulatory, more real-life environment. Additionally, the product use recorded in the participants’ diaries, changes in exposure markers, and changes in the subjective effects of smoking (as reported in Part 1) indicate that dual use in the THS group was infrequent, and that the participants in the SA group showed good compliance to the intervention. Indeed, self-reported compliance with randomized allocation was high on Day 90, with the abstinence rate in the SA group > 90% and in the mTHS group 87.2% mostly mTHS users (≥70% THS use), 2.6% dual users (30% < THS use < 70%), and 3.8% mostly mCC smokers (≤30% THS use).
Another factor that warrants mentioning is that changes in the number of menthol tobacco sticks used per day and in smoking topography may influence some biomarkers of exposure, and potentially may influence the effects of MRTPs on risk markers. As described in Part 1, the participants in the mTHS group adapted their puffing behaviors through more puffs and similar total puff volumes relative to their mCC baseline puffing, resulting overall in similar nicotine concentrations in both groups. Accordingly, the changes in smoking topography or menthol sticks used are unlikely to contribute to the differences in exposure to cigarette smoke/aerosol and hence to the observed differences in biomarkers of exposure or clinical risk markers.
In one of the markers related to metabolic syndrome, waist circumference, an anomaly was observed at the level of summary statistics in that day 90 values were more than five centimeters short of the baseline values in all three groups. As the other metabolic markers, including weight, were virtually unchanged and since no causative explanation appeared even remotely plausible, we concluded that some change in measurement method had occurred between the two assessments, even though its nature could not be identified.
Finally, this study was primarily designed to establish the reduction in exposure to HPHCs. However, surrogate markers of smoking-related diseases were included in the analysis and the impact of mTHS compared to mCC on these markers resulted in changes which were consistent with those achieved by smoking cessation.
In spite of these restrictions, the weight of evidence in favor of the mTHS being a reduced risk tobacco product is compelling, and the available evidence can be gauged against the Hill criteria for product risk assessment purposes.33 The observed effects of switching from mCC to mTHS are generally consistent with the prior expectations and knowledge from smoking cessation in terms of the size and favorable direction of the observed effects, consistent with findings from previous clinical studies, specific and plausible with regard to the a priori specified disease pathways. Moreover, the totality of the effects of switching to mTHS approach those seen subsequent to abstinence, thus supporting the notion of a biological gradient (dose–response relationship). The accumulating evidence is coherent across different types of studies, including human data, experimental animal studies and in vitro models.
In summary, the findings support the presumption that the development of mTHS as consumer-acceptable inhaled nicotine delivery system would be an important advancement in pursuing harm reduction by converting adult smokers from mCC to mTHS. Analog to epidemiological information on health outcome-effects at the individual and population levels after smoking cessation, the examined clinical risk markers in this study are in line with clinical and biological effects expected with quitting combustible cigarettes.
Conclusions
Switching to mTHS was associated with improvements in clinically relevant risk markers linked to oxidative stress, endothelial dysfunction, lipid metabolism, inflammation, and lung function. The directions of these changes in the mTHS and SA groups were similar and clearly distinct from those seen in the mCC group. Further longer term studies are ongoing to confirm the present results, and to verify the clinical relevance of the improvements in the surrogate markers for modified risk tobacco products observed here.
Supplementary Material
Supplementary data are available at Nicotine & Tobacco Research online.
Funding
The study was funded by Philip Morris Products S.A.
Declaration of Interests
All authors are employees of Philip Morris Products S.A.
Supplementary Material
Acknowledgments
The authors would like to thank Dr. Masahiro Endo, MD, study Principal Investigator Tokyo Heart Center Osaki Hospital, LSI Medience Corporation, Tokiwa Chemical Industries Co. Ltd., Nicholas D. Smith, PhD (Edanz Group Ltd), for providing medical writing support, which was funded by Philip Morris Products S.A.. Covance Central Laboratory Services, Covance Japan Co. Ltd, BML Covance CLS and Celerion Inc. for laboratory processing of samples. Clinical trial registration: NCT01970995 (ClinicalTrials.gov).
References
- 1. U.S. Department of Health and Human Services, Food and Drug Administration, Center for Tobacco Products. Guidance for Industry: Modified Risk Tobacco Product Applications. Rockville, MD: Food and Drug Administration; 2012. [Google Scholar]
- 2. Committee on Scientific Standards for Studies on Modified Risk Tobacco Products, Board on Population Health and Public Health Practice, Institute of Medicine. Scientific Standards for Studies on Modified Risk Tobacco Products. Washington, DC: The National Academies Press; 2012. [Google Scholar]
- 3. Lee PN, Fry JS, Forey BA. Estimating the decline in excess risk of chronic obstructive pulmonary disease following quitting smoking - a systematic review based on the negative exponential model. Regul Toxicol Pharmacol. 2014;68(2):231–239. doi:10.1016/j.yrtph.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 4. Lee PN, Fry JS, Hamling JS. Using the negative exponential distribution to quantitatively review the evidence on how rapidly the excess risk of ischaemic heart disease declines following quitting smoking. Regul Toxicol Pharmacol. 2012;64(1):51–67. doi:10.1016/j.yrtph.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 5. Lee PN, Fry JS, Thornton AJ. Estimating the decline in excess risk of cerebrovascular disease following quitting smoking–a systematic review based on the negative exponential model. Regul Toxicol Pharmacol. 2014;68(1):85–95. doi:10.1016/j.yrtph.2013.11.013. [DOI] [PubMed] [Google Scholar]
- 6. Lüdicke F, Magnette J, Baker G, Weitkunat R. A Japanese cross-sectional multicentre study of biomarkers associated with cardiovascular disease in smokers and non-smokers. Biomarkers. 2015;20(6–7):411–421. doi:10.3109/1354750x.2015.1096303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gonzalez-Suarez I, Martin F, Marescotti D, et al. In vitro systems toxicology assessment of a candidate modified risk tobacco product shows reduced toxicity compared to that of a conventional cigarette. Chem Res Toxicol. 2016;29(1):3–18. doi:10.1021/acs.chemrestox.5b00321. [DOI] [PubMed] [Google Scholar]
- 8. Phillips B, Veljkovic E, Boue S, et al. An 8-month systems toxicology inhalation/cessation study in Apoe-/- mice to investigate cardiovascular and respiratory exposure effects of a candidate modified risk tobacco product, THS 2.2, compared with conventional cigarettes. Toxicol Sci. 2016;149(2):411–432. doi:10.1093/toxsci/kfv243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Picavet P, Haziza C, Lama N, Weitkunat R, Lüdicke F. Comparison of the pharmacokinetics of nicotine following single and ad libitum use of a tobacco heating system or combustible cigarettes. Nicotine Tob Res. 2015;18(5):557–563. doi:10.1093/ntr/ntv220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. van der Toorn M, Frentzel S, De Leon H, Goedertier D, Peitsch MC, Hoeng J. Aerosol from a candidate modified risk tobacco product has reduced effects on chemotaxis and transendothelial migration compared to combustion of conventional cigarettes. Food Chem Toxicol. 2015;86:81–87. doi:10.1016/j.fct.2015.09.016. [DOI] [PubMed] [Google Scholar]
- 11. Ansari S, Baumer K, Boué S, et al. Comprehensive systems biology analysis of a 7-month cigarette smoke inhalation study in C57BL/6 mice. Sci Data. 2016;3:150077. doi:10.1038/sdata.2015.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Phillips B, Veljkovic E, Peck MJ, et al. A 7-month cigarette smoke inhalation study in C57BL/6 mice demonstrates reduced lung inflammation and emphysema following smoking cessation or aerosol exposure from a prototypic modified risk tobacco product. Food Chem Toxicol. 2015;80:328–345. doi:10.1016/j.fct.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 13. World Medical Association (WMA). Ethical principles for medical research involving human subjects (Declaration of Helsinki). 2008. www.wma.net/en/30publications/10policies/b3/17c.pdf Accessed February 01, 2017. [Google Scholar]
- 14. ICH E6 (R1). Guideline for good clinical practice 1996. www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6/E6_R1_Guideline.pdf Accessed August 14, 2014.
- 15. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease. A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention; 2010. [PubMed] [Google Scholar]
- 16. Miura N, Yuki D, Minami N, Kakehi A, Futamura Y. A study to investigate changes in the levels of biomarkers of exposure to selected cigarette smoke constituents in Japanese adult male smokers who switched to a non-combustion inhaler type of tobacco product. Regul Toxicol Pharmacol. 2015;71(3):498–506. doi:10.1016/j.yrtph.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 17. Sakaguchi C, Kakehi A, Minami N, Kikuchi A, Futamura Y. Exposure evaluation of adult male Japanese smokers switched to a heated cigarette in a controlled clinical setting. Regul Toxicol Pharmacol. 2014;69(3):338–347. doi:10.1016/j.yrtph.2014.04.016. [DOI] [PubMed] [Google Scholar]
- 18. Ogden MW, Marano KM, Jones BA, Morgan WT, Stiles MF. Switching from usual brand cigarettes to a tobacco-heating cigarette or snus: part 2. Biomarkers of exposure. Biomarkers. 2015;20(6–7):391–403. doi:10.3109/1354750x.2015.1094134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ogden MW, Marano KM, Jones BA, Morgan WT, Stiles MF. Switching from usual brand cigarettes to a tobacco-heating cigarette or snus: part 1. Biomarkers of exposure. Biomarkers. 2015;20(6–7):391–403. doi:10.3109/1354750x.2015.1094133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ogden MW, Marano KM, Jones BA, Morgan WT, Stiles MF. Switching from usual brand cigarettes to a tobacco-heating cigarette or snus: Part 3. Biomarkers of biological effect. Biomarkers. 2015;20(6–7):404–410. doi:10.3109/1354750x.2015.1094135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Roethig HJ, Feng S, Liang Q, Liu J, Rees WA, Zedler BK. A 12-month, randomized, controlled study to evaluate exposure and cardiovascular risk factors in adult smokers switching from conventional cigarettes to a second-generation electrically heated cigarette smoking system. J Clin Pharmacol. 2008;48(5):580–591. doi:10.1177/0091270008315316. [DOI] [PubMed] [Google Scholar]
- 22. Hogg JC, Macklem PT, Thurlbeck WM. Site and nature of airway obstruction in chronic obstructive lung disease. N Engl J Med. 1968;278(25):1355–1360. doi:10.1056/nejm196806202782501. [DOI] [PubMed] [Google Scholar]
- 23. Cosio M, Ghezzo H, Hogg JC, et al. The relations between structural changes in small airways and pulmonary-function tests. N Engl J Med. 1978;298(23):1277–1281. doi:10.1056/nejm197806082982303. [DOI] [PubMed] [Google Scholar]
- 24. Yanai M, Sekizawa K, Ohrui T, Sasaki H, Takishima T. Site of airway obstruction in pulmonary disease: direct measurement of intrabronchial pressure. J Appl Physiol (1985). 1992;72(3):1016–1023. [DOI] [PubMed] [Google Scholar]
- 25. Ebert RV. Elasticity of the lung in pulmonary emphysema. Ann Intern Med. 1968;69(5):903–908. [DOI] [PubMed] [Google Scholar]
- 26. Corbin RP, Loveland M, Martin RR, Macklem PT. A four-year follow-up study of lung mechanics in smokers. Am Rev Respir Dis. 1979;120(2):293–304. [DOI] [PubMed] [Google Scholar]
- 27. Macklem PT. Therapeutic implications of the pathophysiology of COPD. Eur Respir J. 2010;35(3):676–680. doi:10.1183/09031936.00120609. [DOI] [PubMed] [Google Scholar]
- 28. Guy HJ, Prisk GK, Elliott AR, Deutschman RA, III, West JB. Inhomogeneity of pulmonary ventilation during sustained microgravity as determined by single-breath washouts. J Appl Physiol (1985). 1994;76(4):1719–1729. [DOI] [PubMed] [Google Scholar]
- 29. Pinkerton KE, Green FH, Saiki C, et al. Distribution of particulate matter and tissue remodeling in the human lung. Environ Health Perspect. 2000;108(11):1063–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Takizawa H, Tanaka M, Takami K, et al. Increased expression of inflammatory mediators in small-airway epithelium from tobacco smokers. Am J Physiol Lung Cell Mol Physiol. 2000;278(5):L906–L913. [DOI] [PubMed] [Google Scholar]
- 31. Verbanck S, Schuermans D, Meysman M, Paiva M, Vincken W. Noninvasive assessment of airway alterations in smokers: the small airways revisited. Am J Respir Crit Care Med. 2004;170(4):414–419. doi:10.1164/rccm.200401-037OC. [DOI] [PubMed] [Google Scholar]
- 32. Temple R. Are surrogate markers adequate to assess cardiovascular disease drugs?JAMA. 1999;282(8):790–795. [DOI] [PubMed] [Google Scholar]
- 33. Hill AB. The environment and disease: association or causation?Proc R Soc Med. 1965;58(5):295–300. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.