Abstract
Objective
To investigate the state-specific prevalence, regional differences, and correlates of hookah use among U.S. adults.
Methods
We analyzed the most recent nationally representative data of adults from the National Adult Tobacco Survey (NATS) 2012–2013 (n = 60192). State-specific prevalence of lifetime and current hookah use was calculated and mapped. Multivariate logistic regression was performed to determine the association between sociodemographic characteristics, regional differences, and hookah use.
Results
Among U.S. adults (≥18 years), overall prevalence of lifetime hookah use was 12.3%, while current use was 3.9%. Mapping of state-specific prevalence revealed that the West tended to have higher rates of use, while the South tended to have lower ones. In the adjusted model, we observed that current hookah use was positively associated with younger adults, males, non-Hispanic adults, those with higher education and income statuses, being single, those living in the West, and current cigarette use.
Conclusion
The prevalence of hookah use varies by state, region, and sociodemographic characteristics among adults. Future research, including longitudinal studies, are needed to identify geographic and sociodemographic characteristics and trends among hookah users, investigate hookah-related health outcomes, and evaluate targeted public health efforts aimed at this emerging threat.
Implications
This study investigates state-level prevalence, regional differences, and sociodemographic characteristics of hookah use among U.S. adults, using the most recent NATS. Hookah use was positively associated with younger adults and those living in the West. This study adds to the understanding of the geographic and sociodemographic factors underlying hookah use, which can be used to develop much needed evidence-based regulations and programs that are responsive to the needs of different risk groups.
Introduction
Hookah, also called a waterpipe, hubble-bubble, shisha, narghile, or argileh, is a traditional apparatus for the smoking of tobacco and other combustible materials that is popular throughout the Middle East, and more recently, throughout the world.1 Hookah use has increased rapidly in the United States, especially among adolescents, among whom use has increased by 5.3% from 2011 to 2014, although cigarette use has decreased significantly by 6.6% in recent years.2 According to the Centers for Disease Control and Prevention (CDC), the reduction in cigarette consumption might be due to the increased use of other forms of tobacco, including hookahs.3 Hookah creates very large amounts of secondhand smoke, 4,5 and hookah smoking is thus likely to affect bystanders, even more than cigarette smoking does6,7 while at the same time having significant negative effects on those who smoke it themselves.6,8
Studies have found that hookah use is addictive9,10 and causes similar health effects11,12 as cigarettes. Hookah smoke contains high levels of toxic chemicals, such as carbon monoxide (CO), tar, heavy metals, benzene, and other cancer-causing chemicals13,14, and has been associated with dramatically greater smoke exposure than cigarette smoke.12 Moreover, people who use hookahs inhale substantially more smoke than cigarette smokers.5 Possible adverse health outcomes of hookah use include lung cancer,15 periodontal disease,1 respiratory illnesses,16 and low-birth-weight infants.17 In addition, sharing mouthpieces contributes to the spread of infectious diseases, such as hepatitis C, tuberculosis, influenza, and herpes.18 Despite these negative health effects, hookah smoking is generally perceived to be a less harmful, less addictive alternative to cigarettes.19–21
The World Health Organization (WHO) and the World Bank have reported that comprehensive tobacco control policies are the most effective way to curb the tobacco use epidemic, impacting both the demand for and supply of tobacco products.22,23 A recent review of hookah-related legislation and policies, however, revealed that there are very few smoke-free policies at the state and local levels that have addressed hookah smoking.20 Additionally, there is virtually no legislation in any of the 50 states and the District of Columbia that addresses any of the text on hookah packaging or the need to provide information on the negative health impacts of hookah use either on the packaging or in establishments where hookah use is allowed. Existing policies do not necessarily discourage current users or directly inform the public about the hazards of hookah-related secondhand smoke in other venues (eg homes) and do not explicitly reference hookah bars and lounges, leading to varying interpretations.24
Despite the emerging literature demonstrating adverse health consequences of hookah use, little is known about the regional patterns of such use. Also, most studies that have addressed the epidemiology of hookah use have been international in scope, thereby utilizing samples with demographics that are not necessarily representative of hookah users in the United States, such as university students in other countries25,26 and use as a result of cultural practices specific to individual cultures.27,28 Moreover, public policy regarding hookah use, advertising and sales lag far behind those existing for cigarettes, although they are receiving increased attention at the local and federal levels as evidenced by bans on hookah lounges in a number of cities and the recent Food and Drug Administration (FDA) report concerning national concerns and policies.29 Assessments of the geographic use of hookahs across U.S. states can serve as an exploratory tool or a basis for future epidemiological research and evidence-based policymaking.
In this study, therefore, we analyzed a nationally representative sample of U.S. adults to assess the state-specific prevalence of hookah use and to determine its association with regional and sociodemographic characteristics using the most recent National Adult Tobacco Survey (NATS) data. Findings from this research can inform interventions focused on reducing hookah use among population subgroups in the United States.
Methods
Sample
Data from the cross-sectional, nationally representative NATS 2012–2013 were analyzed. A detailed description of the NATS methodology is available elsewhere.30 Briefly, the NATS was designed as a stratified, national random-digit dialed landline and cell phone survey of 60192 noninstitutionalized adults aged 18 years and older, residing in the 50U.S. states or the District of Columbia. For the 2012–2013 survey wave, the response rate to the survey was 44.9% (landline, 47.2%; cellular, 36.3%).
The 2012–2013 NATS comprised two sampling frames: one consisting of landline telephone users and one consisting of cellular telephone numbers. Each state consisted of three strata: a listed landline stratum, a nonlisted landline stratum, and a cellular phone stratum. The samples from each frame were stratified by state to provide adequate representation of each state and gather higher numbers of completed surveys from states with larger populations. The state goals targeted a minimum of 800 completed surveys: 600 landline (75%) and 200 cell-only (25%) from each state. Thirty states targeted more than 800 for 24000 of the 60000 target population. The top 20 most populous states with a goal above 800 accounted for the remaining 36000 surveys allocated across these states in approximate proportion to their population. The number of surveys conducted was very close to state goals, with a range of 97.6%–105.6%.30
Variables
Participants were identified to be current cigarette smokers if they answered “yes” to the question, “Have you smoked at least 100 cigarettes in your entire life?” and responded with “every day,” or “some days,” to the question, “Do you now smoke cigarettes every day, some days or not at all?” Participants who answered “yes” to the question, “Have you ever smoked tobacco in a hookah in your entire life?” were defined as ever users of hookahs. For current hookah use, individuals who responded with “rarely” were also included as current users, a practice consistent with previous literature.31–35 As this might boost the number of respondents classified as current hookah users, and as those who report rarely using hookahs may differ from those who smoke every day or some days, subgroup analyses were performed for (a) those who rarely smoked (n = 1103) and (b) for those who smoked every (n = 20) or some days (n = 149) for a total of 169 subjects in this group.
Sociodemographic variables included age (18–24, 25–34, 35–44, 45–54, 55–64, and 65≥), gender, race/ethnicity (non-Hispanic White, non-Hispanic Black, non-Hispanic Asian, Hispanic, and non-Hispanic other), educational attainment (less than high school diploma, high school graduate, some college or associate degree, bachelor’s degree or higher), annual household income (<$20000, $20000–$49999, $50000–$99999, and ≥$100000), marital status (married/living with a partner, divorced/widowed/separated/single/never marry/not living with partner), and U.S. region (Northeast, Midwest, South, and West). All 50U.S. states and the District of Columbia were also included in the analyses. Current cigarette smoking status also was included as a covariate and characteristics of cigarette smokers were also assessed for purposes of comparison.
Statistical Analyses
Data were analyzed using the –survey– module of Stata 14.0 (StataCorp, College Station, TX) to account for complex sample design and responses. The landline data were weighted by probability of selection of a respondent’s telephone number, nonresponse, number of landlines in the household, and number of adults in the household. The cell phone data were weighted to adjust for probability of selection of the telephone number and nonresponse. To adjust for undercoverage and nonresponse bias, final weights were calculated using a raking method, with state, age, gender, race/ethnicity, marital status, educational attainment, and phone category.36
Estimates of lifetime and current hookah use were calculated for each state. For lifetime hookah use, state-specific prevalence was assessed and mapped by gender. The ArcGIS 10.0 software (ESRI, Redlands, CA) was used for GIS mapping. A descriptive analysis of all variables included in this study was performed using weighted percentages and confidence intervals (CIs). Multivariate logistic regression was performed to assess the association between sociodemographic characteristics, region, and hookah use. A significance level of α = 0.05 was used in the analysis.
Results
For current hookah use, presented results include analyses of individuals who reported using hookah rarely, on some days, or every day. Not shown are separate analyses for (a) those who rarely use hookah and (b) those who use hookah on some days or every day, as results were virtually identical to those analyses conducted with “current hookah use” including those who reported smoking hookah rarely, on some days, or every day. Among U.S. adults, the overall prevalence of lifetime hookah use was 12.3% (95% CI: 11.9–12.7), while the rate of current use was 3.9% (95% CI: 3.6–4.1). Table 1 presents estimates of current and lifetime hookah use among U.S. adults for each state, categorized by the four geographic regions. The prevalence varied substantially by state. Estimates of current hookah use ranged from 0.8% (95% CI: 0.2–2.6) in Mississippi to 10.3% (95% CI: 5.7–17.9) in the District of Columbia. For lifetime hookah use, the prevalence ranged from 4.4% (95% CI: 2.6–7.1) in Mississippi to 27.1% (95% CI: 20.8–34.6) in the District of Columbia (Table 1). Lifetime hookah use was more prevalent among males than females in all 50 states and the District of Columbia and the geographic distribution of use by gender varied somewhat by state (Table 1). Among males, the highest prevalence of lifetime hookah use was in the District of Columbia (36.3%), followed by Nevada (24.3%), New Mexico (23.6%), and California (22.2%). Among females, the highest rates were observed in the District of Columbia (20.0%), Arizona (14.4%), Nevada (13.6%), and Colorado (13.1%).
Table 1.
State-Specific Estimatesa of Lifetime and Current Hookah Use Among U.S. Adults: NATS 2012–2013 (n = 60192)
| Total, Nb | Ever used hookahc | Current hookah used | |||
|---|---|---|---|---|---|
| Overall | Male | Female | Overall | ||
| Northeast | |||||
| Connecticut | 774 | 11.9 (8.8, 16.0) | 16.6 (11.2, 23.9) | 7.1 (4.3, 11.5) | 3.1 (1.7, 5.6) |
| Maine | 774 | 8.9 (6.4, 12.3) | 9.2 (5.9, 14.0) | 8.4 (5.0, 13.6) | 3.2 (1.7, 5.9) |
| Massachusetts | 1038 | 14.2 (11.1, 18.2) | 17.5 (12.3, 24.3) | 11.0 (7.6, 15.6) | 4.3 (2.2, 8.0) |
| New Hampshire | 756 | 10.1 (7.3, 13.7) | 11.5 (7.5, 17.1) | 8.7 (5.2, 14.2) | 3.9 (2.2, 6.8) |
| New Jersey | 1246 | 9.7 (7.4, 12.6) | 11.1 (7.7, 15.7) | 8.1 (5.2, 12.5) | 3.6 (2.1, 6.0) |
| New York | 2867 | 12.7 (11.0, 14.5) | 15.0 (12.6, 17.9) | 9.2 (7.2, 11.8) | 4.6 (3.6, 5.9) |
| Pennsylvania | 1903 | 9.8 (8.2, 11.7) | 12.4 (9.8, 15.5) | 7.1 (5.1, 9.6) | 3.5 (2.5, 4.8) |
| Rhode Island | 772 | 11.2 (8.2, 15.1) | 14.1 (9.0, 21.3) | 7.0 (4.3, 11.2) | 4.5 (2.5, 8.1) |
| Vermont | 756 | 10.2 (7.4, 13.9) | 13.6 (9.0, 20.2) | 6.2 (3.7, 10.3) | 3.0 (1.4, 6.4) |
| Midwest | |||||
| Indiana | 969 | 12.3 (9.5, 15.7) | 13.4 (9.4, 18.9) | 11.2 (7.5, 16.2) | 5.1 (3.2, 7.9) |
| Illinois | 1954 | 12.8 (10.8, 15.1) | 15.5 (12.4, 19.1) | 9.4 (7.0, 12.6) | 4.1 (3.0, 5.7) |
| Iowa | 814 | 10.4 (7.5, 14.2) | 14.1 (9.4, 20.6) | 6.9 (4.1, 11.4) | 2.8 (1.4, 5.5) |
| Kansas | 781 | 12.7 (9.6, 16.8) | 15.4 (10.4, 22.1) | 9.4 (5.9, 14.8) | 3.0 (1.7, 5.4) |
| Michigan | 1540 | 12.8 (10.6, 15.4) | 15.4 (12.0, 19.6) | 9.4 (6.9, 12.8) | 3.7 (2.5, 5.3) |
| Minnesota | 856 | 14.3 (11.5, 17.7) | 19.4 (14.9, 24.7) | 9.8 (6.5, 14.4) | 4.3 (2.8, 6.6) |
| Missouri | 906 | 11.8 (9.2, 15.0) | 16.1 (11.8, 21.7) | 6.9 (4.4, 10.7) | 3.5 (2.1, 5.7) |
| Nebraska | 804 | 9.3 (6.7, 12.9) | 10.0 (6.1, 15.8) | 8.6 (5.3, 13.7) | 4.2 (2.3, 7.5) |
| North Dakota | 778 | 9.8 (5.6, 16.7) | 12.8 (5.7, 26.3) | 7.0 (4.1, 11.7) | 2.3 (1.1, 4.7) |
| Ohio | 1705 | 9.0 (7.3, 11.1) | 10.1 (5.4, 13.4) | 6.6 (4.7, 9.3) | 3.4 (2.3, 4.9) |
| South Dakota | 790 | 7.3 (5.2, 10.3) | 10.9 (7.0, 16.4) | 3.8 (2.1, 6.6) | 3.9 (2.4, 6.3) |
| Wisconsin | 869 | 11.8 (9.2, 15.2) | 12.9 (9.3, 17.5) | 10.7 (7.0, 16.1) | 4.4 (2.7, 7.1) |
| South | |||||
| Alabama | 840 | 7.6 (5.3, 10.8) | 10.7 (6.9, 16.3) | 5.2 (2.7, 9.6) | 1.9 (0.9, 4.2) |
| Arkansas | 771 | 6.9 (4.6, 10.3) | 9.2 (5.7, 14.7) | 4.7 (2.1, 10.0) | 2.1 (1.0, 4.5) |
| Delaware | 781 | 7.9 (5.4, 11.5) | 10.5 (6.7, 16.0) | 5.8 (2.8, 11.7) | 1.6 (0.8, 3.5) |
| District of Columbia | 656 | 27.1 (20.8, 34.6) | 36.3 (25.1, 49.1) | 20.0 (13.8, 27.9) | 10.3 (5.7, 17.9) |
| Florida | 2841 | 13.1 (11.5, 15.0) | 16.4 (13.7, 19.5) | 9.9 (7.9, 12.2) | 3.8 (2.9, 5.0) |
| Georgia | 1532 | 13.6 (11.2, 16.4) | 17.2 (13.5, 21.7) | 10.3 (7.3, 14.4) | 4.2 (2.9, 6.2) |
| Kentucky | 781 | 8.1 (5.6, 11.6) | 11.5 (7.4, 17.6) | 5.4 (2.8, 10.1) | 1.4 (0.6, 3.4) |
| Louisiana | 805 | 8.6 (6.1, 12.2) | 10.5 (6.4, 16.8) | 6.1 (3.6, 10.1) | 2.0 (0.9, 4.2) |
| Maryland | 921 | 12.6 (10.1, 15.6) | 16.6 (12.5, 21.6) | 8.9 (6.0, 12.9) | 4.0 (2.6, 6.0) |
| Mississippi | 815 | 4.4 (2.6, 7.1) | 6.9 (3.6, 12.7) | 2.0 (0.8, 4.8) | 0.8 (0.2, 2.6) |
| North Carolina | 1523 | 8.7 (7.0, 10.7) | 12.3 (9.4, 15.8) | 5.0 (3.3, 7.5) | 2.6 (1.7, 4.0) |
| Oklahoma | 783 | 10.5 (7.9, 13.9) | 14.0 (9.8, 19.5) | 7.8 (4.8, 12.4) | 2.7 (1.5, 5.0) |
| South Carolina | 788 | 8.5 (6.0, 11.8) | 10.4 (6.7, 15.8) | 7.2 (4.1, 12.1) | 1.1 (0.4, 3.0) |
| Tennessee | 951 | 9.4 (7.0, 12.5) | 12.2 (8.2, 17.9) | 7.1 (4.7, 10.6) | 2.2 (1.2, 4.0) |
| Texas | 3772 | 11.3 (9.9, 12.8) | 12.6 (10.5, 15.0) | 9.7 (8.0, 11.7) | 3.4 (2.6, 4.5) |
| Virginia | 1264 | 12.8 (10.4, 15.6) | 15.3 (12.0, 19.4) | 10.6 (7.5, 14.7) | 5.0 (3.5, 7.1) |
| West Virginia | 767 | 7.0 (4.9, 10.0) | 8.0 (4.8, 13.1) | 5.9 (3.4, 10.0) | 2.0 (1.0, 3.9) |
| West | |||||
| Alaska | 781 | 10.3 (7.5, 14.0) | 12.8 (8.2, 19.4) | 8.1 (5.4, 12.1) | 2.6 (1.0, 6.8) |
| Arizona | 991 | 17.5 (14.5, 21.0) | 20.0 (15.5, 25.4) | 14.4 (10.5, 19.2) | 6.5 (4.5, 9.2) |
| California | 5783 | 17.0 (15.6, 18.4) | 22.2 (19.9, 24.6) | 12.0 (10.4, 13.7) | 5.4 (4.6, 6.4) |
| Colorado | 845 | 15.5 (12.4, 19.1) | 17.7 (12.9, 23.8) | 13.1 (9.5, 17.8) | 5.3 (3.4, 8.2) |
| Hawaii | 776 | 9.8 (7.2, 13.2) | 12.2 (8.3, 17.6) | 6.8 (3.9, 11.7) | 2.0 (1.1, 3.8) |
| Idaho | 806 | 13.7 (10.1, 18.3) | 15.8 (10.7, 22.6) | 11.7 (7.0, 18.8) | 5.1 (2.8, 9.2) |
| New Mexico | 809 | 15.9 (12.4, 20.3) | 23.6 (17.4, 31.3) | 8.0 (5.1, 12.4) | 4.4 (2.7, 7.2) |
| Montana | 778 | 9.8 (7.3, 13.2) | 14.7 (10.3, 20.6) | 4.7 (2.7, 8.1) | 3.8 (2.2, 6.4) |
| Oregon | 862 | 16.0 (12.8, 19.7) | 20.3 (15.2, 26.5) | 11.7 (8.1, 16.6) | 2.2 (1.2, 4.3) |
| Nevada | 823 | 19.1 (15.5, 23.3) | 24.3 (18.7, 31.0) | 13.6 (9.4, 19.2) | 6.5 (4.3, 9.5) |
| Utah | 786 | 12.5 (9.5, 16.2) | 14.9 (10.2, 21.2) | 10.3 (6.8, 15.2) | 5.5 (3.5, 8.6) |
| Washington | 1134 | 12.2 (9.9, 14.9) | 16.3 (12.6, 20.8) | 8.5 (5.9, 12.0) | 2.4 (1.5, 4.0) |
| Wyoming | 775 | 11.8 (8.5, 16.2) | 16.3 (10.7, 23.9) | 7.2 (4.1, 12.1) | 4.5 (2.6, 7.6) |
NATS = National Adult Tobacco Survey.
aPercentages are weighted (95% confidence interval).
bUnweighted sample sizes.
cThe question, “The next question asks you about smoking tobacco in a hookah. A hookah is a type of water pipe. Have you ever smoked tobacco in a hookah in your entire life?” was used to identify ever hookah use.
dThe question, “Do you now smoke tobacco in a hookah every day, some days, rarely or not at all?” was used to determine current use of hookah. Respondents who answered “every day,” “some days,” or “rarely” were considered current hookah user.
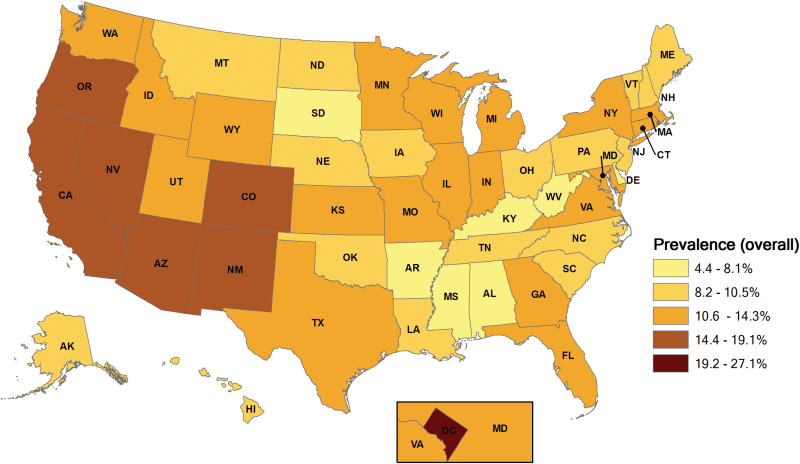
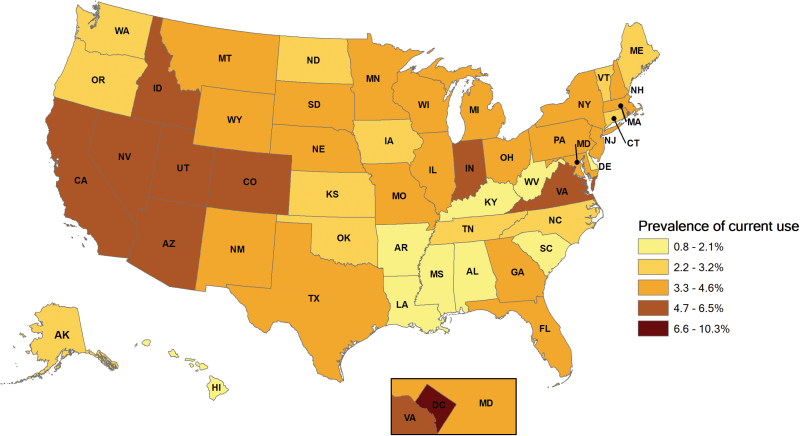
For both current and lifetime hookah use, the West tended to have higher rates, while the South tended to have lower ones. The maps in Figures 1 and 2 show the weighted percentage of lifetime and current hookah use with darker shading indicating a higher prevalence of hookah use. Classifications are based on quintiles. Nine states had rates of current hookah use greater than or equal to 5%: Arizona, California, Colorado, the District of Columbia, Idaho, Indiana, Nevada, Utah, and Virginia. Seven states had rates of lifetime use greater than or equal to 15%: Arizona, California, Colorado, the District of Columbia, Nevada, New Mexico, and Oregon. The distributions of the prevalence of current and lifetime hookah use appeared to be similar.
Figure 1.
State-specific weighted prevalence of hookah lifetime use among adults in the United States: National Adult Tobacco Survey, 2012–2013.
Figure 2.
State-specific weighted prevalence of hookah current use among adults in the United States: National Adult Tobacco Survey, 2012–2013.
Table 2 describes the sociodemographic characteristics of current and lifetime hookah users, and how these characteristics were independently associated with hookah use. Cigarette use was included for comparison. In the multivariate logistic regression model, significant regional differences were observed, with adults in the West having increased levels of both lifetime (odds ratio [OR] = 1.6; 95% CI: 1.4–1.9) and current (OR = 1.4; 95% CI: 1.1–1.8) use of hookahs compared with adults in the Northeast. Conversely, adults living in the West were less likely to be current cigarette smokers than those living in the Northeast (OR = 0.8; p < .05).
Table 2.
Estimates and Multivariate Logistic Modela of Factors Associated With Use of Hookah and Cigarettes Among U.S. Adults Aged ≥18 years, NATS 2012–2013 (n = 60192)
| Ever used hookah (n = 4929) | Current use of hookahd (n = 1272) | Current use of cigarettese (n = 8163) | ||||
|---|---|---|---|---|---|---|
| % (95% CI) | aOR (95% CI) | % (95% CI) | aOR (95% CI) | % (95% CI) | aOR (95% CI) | |
| Age (years) | ||||||
| 18–24 | 36.4 (34.5, 38.4) | 7.2 (6.1, 8.5)** | 18.3 (16.8, 19.9) | 15.1 (10.8, 21.2)** | 18.5 (17.0, 20.1) | 0.6 (0.5, 0.8)** |
| 25–34 | 24.8 (23.5, 26.1) | 3.5 (3.1, 4.0)** | 6.3 (5.6, 7.1) | 4.1 (2.9, 5.7)** | 24.0 (22.6, 25.4) | 1.2 (1.1, 1.4)* |
| 35–44 | 9.0 (8.2, 9.9) | Referent | 1.4 (1.1, 1.9) | Referent | 20.0 (18.4, 21.0) | Referent |
| 45–54 | 5.1 (4.6, 5.7) | 0.6 (0.5, 0.7)** | 0.6 (0.4, 0.8) | 0.4 (0.2, 0.6)** | 21.5 (20.4, 22.6) | 1.0 (0.9, 1.1) |
| 55–64 | 3.2 (2.8, 3.6) | 0.3 (0.3, 0.4)** | 0.2 (0.1, 0.3) | 0.1 (0.1, 0.3)** | 16.8 (15.9, 17.7) | 0.7 (0.6, 0.8)** |
| ≥65 | 1.5 (1.3, 1.7) | 0.2 (0.2, 0.3)** | 0.1 (0.02, 0.1) | 0.06 (0.02, 0.2)** | 7.8 (7.3, 8.3) | 0.2 (0.2, 0.3)** |
| Gender | ||||||
| Male | 15.3 (14.7, 16.0) | 1.7 (1.6, 1.9)** | 4.8 (4.4, 5.2) | 1.5 (1.3, 1.8)** | 20.6 (19.8, 21.3) | 1.5 (1.4, 1.6)** |
| Female | 9.2 (8.7, 9.7) | Referent | 2.7 (2.4, 3.1) | Referent | 14.5 (13.9, 15.1) | Referent |
| Race/ethnicity | ||||||
| White, non-Hispanic | 11.7 (11.3, 12.2) | Referent | 3.6 (3.3, 3.9) | Referent | 17.2 (16.6, 17.7) | Referent |
| Black, non-Hispanic | 7.5 (6.4, 8.8) | 0.6 (0.5, 0.7)** | 2.0 (1.5, 2.7) | 0.4 (0.3, 0.7)** | 19.5 (17.9, 21.3) | 0.8 (0.7, 0.9)** |
| Asian, non-Hispanic | 16.2 (13.5, 19.2) | 0.7 (0.6, 1.0)* | 5.0 (3.4, 7.3) | 0.6 (0.4, 1.0) | 7.5 (5.5, 10.2) | 0.6 (0.4, 0.8)* |
| Hispanic | 14.1 (12.8, 15.4) | 1.0 (0.9, 1.2) | 4.6 (3.9, 5.4) | 0.8 (0.6, 1.1) | 14.5 (13.2, 15.9) | 0.4 (0.4, 0.5)** |
| Other, non-Hispanic | 17.6 (15.7, 19.5) | 1.2 (1.0, 1.4)* | 5.6 (4.5, 6.9) | 1.1 (0.8, 1.4) | 27.8 (25.7, 30.0) | 1.5 (1.3, 1.7)** |
| Education attainment | ||||||
| Less than high school diploma | 5.9 (4.9, 7.2) | 0.6 (0.4, 0.7)** | 2.1 (1.5, 2.9) | 0.7 (0.4, 1.0)* | 25.6 (23.8, 27.5) | 1.5 (1.3, 1.7)** |
| High school graduate | 11.1 (10.3, 12.0) | Referent | 4.0 (3.4, 4.6) | Referent | 21.8 (20.8, 22.8) | Referent |
| Some college or associate degree | 14.3 (13.5, 15.1) | 1.6 (1.4, 1.8)** | 4.8 (4.3, 5.4) | 1.5 (1.2, 1.8)* | 19.0 (18.2, 19.8) | 0.9 (0.8, 0.9)* |
| Bachelor degree or higher | 14.1 (13.4, 14.7) | 2.3 (2.0, 2.7)** | 2.9 (2.6, 3.3) | 1.8 (1.4, 2.3)** | 6.8 (6.4, 7.3) | 0.3 (0.28, 0.35)** |
| Annual household income | ||||||
| <20000 | 10.1 (8.9, 11.4) | 1.0 (0.9, 1.2) | 3.4 (2.7, 4.2) | 1.1 (0.8, 1.5) | 26.3 (24.7, 28.0) | 1.1 (1.0, 1.2) |
| 20000–49999 | 11.5 (10.8, 12.3) | Referent | 3.6 (3.1, 4.1) | Referent | 22.6 (21.6, 23.6) | Referent |
| 50000–99999 | 13.1 (12.3, 14.0) | 1.2 (1.0, 1.3)* | 3.9 (3.4, 4.4) | 1.2 (1.0, 1.5) | 15.7 (14.8, 16.6) | 0.7 (0.6, 0.7)** |
| ≥100000 | 15.1 (14.1, 16.1) | 1.6 (1.4, 1.8)** | 3.9 (3.3, 4.5) | 1.5 (1.2, 1.9)* | 9.3 (8.5, 10.1) | 0.5 (0.4, 0.5)** |
| Marital status | ||||||
| Married/with a partner | 8.8 (8.4, 9.2) | Referent | 1.7 (1.5, 1.9) | Referent | 14.7 (14.2, 15.3) | Referent |
| Singleb | 16.5 (15.7, 17.3) | 1.4 (1.3, 1.6)** | 6.3 (5.8, 6.9) | 2.0 (1.6, 2.4)** | 21.0 (20.3, 21.8) | 1.3 (1.2, 1.5)** |
| U.S. regionc | ||||||
| Northeast | 11.5 (10.5, 12.5) | Referent | 4.0 (3.4, 4.7) | Referent | 16.6 (15.5, 17.7) | Referent |
| Midwest | 11.7 (10.9, 12.6) | 1.0 (0.9, 1.2) | 3.9 (3.4, 4.5) | 0.8 (0.6, 1.1) | 19.6 (18.6, 20.7) | 1.1 (0.9, 1.2) |
| South | 10.8 (10.2, 11.5) | 1.0 (0.9, 1.2) | 3.2 (2.8, 3.6) | 0.8 (0.6, 1.1) | 19.4 (18.6, 20.2) | 1.0 (0.9, 1.2) |
| West | 15.9 (15.0, 16.8) | 1.6 (1.4, 1.9)** | 4.9 (4.4, 5.5) | 1.4 (1.1, 1.8)* | 15.1 (14.3, 16.0) | 0.8 (0.7, 1.0)* |
| Current use of cigarettese | ||||||
| Yes | 21.2 (19.9, 22.5) | 2.6 (2.3, 2.9)** | 8.5 (7.7, 9.5) | 3.9 (3.2, 4.7)** | — | — |
| No | 10.4 (10.0, 10.8) | Referent | 2.9 (2.6, 3.1) | Referent | — | — |
aOR = adjusted odds ratio; CI = confidence interval; NATS = National Adult Tobacco Survey.
aAdjusted for age, sex, ethnicity, educational level, income level, smoking status, marital status, and region.
bIncludes people those who divorced/widowed/separated.
cNortheast includes Connecticut, Maine, Massachusetts, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, and Vermont; Midwest includes Indiana, Illinois, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, and Wisconsin; South includes Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia; West includes Alaska, Arizona, California, Colorado, Hawaii, Idaho, New Mexico, Montana, Oregon, Nevada, Utah, Washington, and Wyoming.
dThe question, “Do you now smoke tobacco in a hookah every day, some days, rarely or not at all?” was used to determine current use of hookah. Respondents who answered “every day,” “some days,” or “rarely” were considered current hookah users.
eRespondents who reported smoking at least 100 cigarettes during their lifetime and now smoked “every day” or “some days.”
*p < .05. **p < .001.
A number of characteristics of individuals were also associated with hookah use, and the associations were similar for lifetime and current hookah use. Age was significantly associated (p < .001) with hookah use, with adults younger than 35 being more likely to use them and adults older than 44 less likely. Of note, young adults aged 18 to 24 years were more likely to be current hookah smokers than those aged 35 to 44 years (OR = 15.1; 95% CI: 10.8–21.2), and less likely to be current cigarette smokers (OR = 0.6; 95% CI: 0.5–0.8).
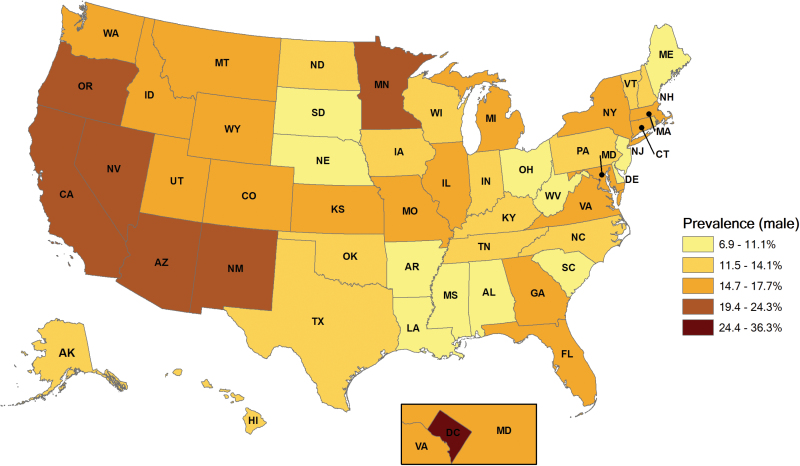
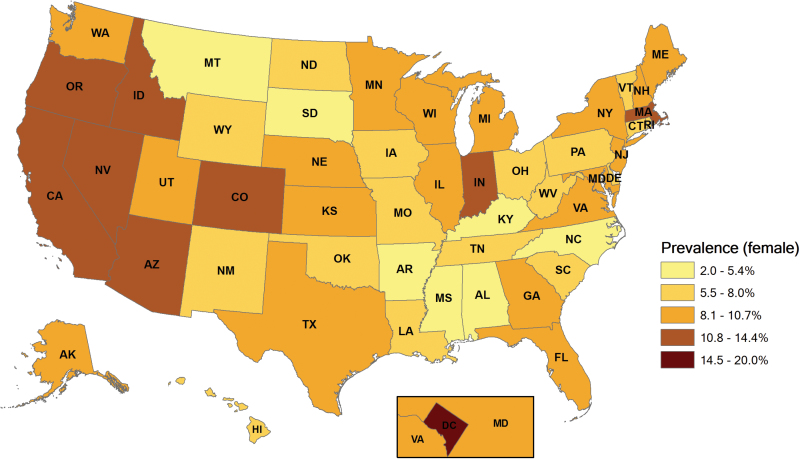
Being male and being single were also associated with increased current hookah use (OR = 1.5; 95% CI: 1.3–1.8, OR = 2.0; 95% CI: 1.6–2.4, respectively). Similarly, current cigarette smokers were also more likely to be male and single (OR = 1.5; 95% CI: 1.4–1.6, OR = 1.3; 95% CI: 1.2–1.5, respectively) (Figures 3 and 4). Non-Hispanic Black adults were negatively associated with both current hookah use and current cigarette use compared with White adults (OR = 0.4; 95% CI: 0.2–0.6; OR = 0.8; 95% CI: 0.7–0.9, respectively). In contrast to current cigarette use, individuals with a Bachelor’s degree or higher and those who earned more than $100000 in annual household income were more likely to be current hookah users (OR = 1.8; 95% CI: 1.4–2.3, OR = 1.5; 95% CI: 1.2–1.9, respectively) and less likely to be current cigarette users (OR = 0.3; 95% CI: 0.3–0.4, OR = 0.5; 95% CI: 0.4–0.5, respectively). Positive associations were observed between current cigarette smoking and lifetime and current hookah use. Individuals who were current cigarette smokers were more likely to be current hookah users than those who were not current cigarette smokers (OR = 3.9; 95% CI: 3.2–4.7).
Figure 3.
State-specific weighted prevalence of hookah lifetime use among men in the United States: National Adult Tobacco Survey, 2012–2013.
Figure 4.
State-specific weighted prevalence of hookah lifetime use among women in the United States: National Adult Tobacco Survey, 2012–2013.
Discussion
We investigated the regional and state-level prevalence of lifetime and current hookah use, and assessed the association between characteristics of individuals and hookah use, using the most recent nationally representative sample of adults from the United States with such information. The results demonstrate that the prevalence of current and lifetime hookah use varied substantially by state and region, with higher rates of use being reported in the West, although Washington DC had the highest prevalence of both lifetime and current use. In addition, a number of characteristics of individuals were independently associated with both current and lifetime use, with the characteristics among individuals in each hookah-use group being quite similar and markedly different from those of cigarette smokers. Current hookah use was positively associated with living in the West, younger adults, males, those with higher education and income statuses, single status, and current cigarette smoking.
This study builds on past research, demonstrating significant changes over a very short time period. Compared with a recently published study37 that used data from the 2009–2010 NATS, the prevalence rates for both lifetime and current hookah use have increased. Reported lifetime hookah use has increased from 9.8% to 12.3%, and current hookah use has increased from 1.5% to 3.3% in this very short timespan. Variations in rates of use by state also changed over this period. The highest prevalence of lifetime hookah use, which remained the same, was in the District of Columbia. However, the lowest prevalence of lifetime hookah use was in Mississippi, replacing West Virginia. Data presented here are also consistent with another prior study of 105012 students from 152U.S. universities that found hookah use was highest in the West.38
The current study also found that increased lifetime and current hookah use persisted in the West even after adjusting for multiple confounders—which Salloum et al.37 did not examine in the 2009–2010 wave. This suggests that the increased prevalence in the West may not be due to commonly studied sociodemographic factors such as race/ethnicity, education, or income, but may be related to as yet unmeasured or unidentified variables. Due to the paucity of state-level research on hookah environment characteristics such as number of hookah bars, methods of advertising, and comprehensive reports on regulations, it is difficult to determine what might be causing the increase in prevalence in the West. More research is needed to identify such potential causal factors and to create appropriate interventions to address them.
This study also identified several sociodemographic correlates associated with hookah use in adults. Results show that males are more likely to use hookah than females, a finding corroborated by the study by Salloum et al. However, it should be noted that a recent paper by Villanti et al.39 found identical rates of use among males and females, albeit in a sample restricted to younger adults aged 18 to 24 years. In the present study, being married or having a partner was found to be negatively associated with hookah use. Although this was not studied by Salloum et al., being married has been shown to be associated with reduced hookah use in a different study of U.S. Air Force military recruits40 and has been linked to decreased cigarette use.41
In this study, higher income and education were positively associated with hookah use, in contrast to cigarette smoking, which is well recognized to be more common among those of lower socioeconomic status.42 This highlights the fact that different factors seem to be associated with cigarette and hookah use. These findings are also consistent with a recent study that found that high school students with higher parental education status and higher income were more likely to be hookah users.43 The cause or causes of this finding are, we believe, very important and currently unexplained. The diffusion of hookah use in the United States is coinciding with the proliferation of hookah bars.44 The use of these venues is often quite costly, which may be related to the fact that they are more affordable to higher income groups or more of a status symbol and a trending social activity among more affluent individuals. This clearly contrasts with cigarette smoking in the fact that cigarette use currently is stigmatized among the same demographic.33
Our study also showed that younger age was associated with greater hookah use, as has been found in other studies. In a national survey, the CDC reported a significant increase in hookah use among middle school- and high school-aged youth.45 Among high school students, current hookah use significantly increased from 4.1% to 9.4% from 2011 to 2014, although current cigarette use decreased from 15.8% to 9.2%45. In addition, a university-based study of young adults found that the prevalence of hookah use was 28.4%, whereas 19.6% of the participants smoked cigarettes at the time of the study46.
Studies have suggested that increased hookah use among younger adults is due mainly to harm perception, attitude, and social norms regarding its acceptability.47,48 Compared with cigarette smoking, college students tend to perceive hookah use as less harmful, addictive, and detrimental, and as having higher social approval.33,49 A longitudinal cohort study of university students indicated a significant association between positive attitudes toward hookah use and increased odds of initiation.50 Additionally, these misconceptions of hookah use may alter the social norms of other peers, potentially contributing to the increasing trend of hookah use among younger adults. Younger adults are more likely to use the internet or social media, such as Twitter and YouTube, and to share photos of their hookah use, including at bars and social events, potentially prompting peers who have never tried hookah to initiate use.51–53
Several limitations of this study are deserving of note. First, since the analyses were based on self-reported data, recall and social desirability biases may have affected the results. Second, we analyzed cross-sectional data; therefore, it was not possible to assess the causality of relationships or to perform long-term trend analyses. Additional longitudinal studies are essential to assess risk factors associated with hookah use and how they may be changing, changing regional variations in use, as well as potential health risks. Third, the majority (86.8%) of the sample of current hookah users reported “rarely” using hookah. However, accounting for the rarely group does not diminish the findings of this study, because even using hookah rarely might represent initiation of hookah use, as well as cause potential health risks at both the individual and population levels. Fourth, owing to the limitations of the questionnaire, we could not account for lifestyle factors, such as alcohol consumption, licit and illicit substance use, psychological factors, and religiosity, which have been found to be associated with hookah use in other studies.43,54,55 Although we described the overall state-level prevalence, we were not able to compare rural and urban differences and/or population characteristics across the states. Lastly, the paucity of information available concerning state and local regulations regarding hookah bars, use of hookahs in public outdoor spaces, hookah and shisha sales, and use of hookah-related advertising limits our ability to correlate geographic usage rates with public policies.
Despite these limitations, the data presented provide an estimate of the state-based prevalence of hookah use in the 50U.S. states and the District of Columbia, using the most recent nationally representative NATS data, and describe the individual and regional characteristics associated with lifetime and current hookah use. Since the characteristics of hookah users are different to those of cigarette smokers, the findings of this study should be useful for guiding the development of strategies to prevent hookah use, including those aimed at marketing and at regulating emerging alternative tobacco products. Another consideration that should be addressed in future studies is that of nonsmokers being exposed to secondhand hookah smoke. Hookah venues, including bars, lounges, restaurants, and cafés, are prevalent around university campuses and provide a gathering place for college students. Thus, the effect of such venues on the health of nonsmokers is also a significant consideration
Furthermore, although several states, as well as the District of Columbia regulate cigarette smoking in public places and workplaces, the Smoke-Free Air Act is often not applicable to hookah bars. Hookah bars have been able to take advantage of this exemption in certain states, often times creating unsafe environments with minimal ventilation. It is thus left up to local governments and organizations to advocate for increased awareness of this pressing health issue. Analysis of potential policy options to decrease hookah use and exposure has demonstrated that banning hookah bars would not only be politically infeasible but would also not significantly decrease the prevalence of hookah use.56 However, it would be possible to impose stricter regulations on hookah bars and hookah packaging that increase the visibility of the harmful nature of the product as has been done for cigarettes.57,58 Given the existing state-level autonomy in developing hookah sensitive regulations, continuous monitoring of state-level hookah-related policies and prevalence of use could help explicate “what works” within the U.S. context at the state level. Such monitoring can help guide the development, implementation, and evaluation of evidence-based targeted interventions for the prevention of hookah use that are responsive to the state-level policy and regulatory context.
Funding
This work was supported by the National Cancer Institute at the National Institutes of Health (3 P30 CA016087-33S1), the NYU College of Global Public Health Affinity Grant to MW, the National Institute on Drug Abuse (1K24DA038345-01), NYU CTSA Grant (UL1TR000038) from the National Center for Advancing Translational Sciences to SES, and NYU/Abu Dhabi Public Health Research Center to MW, SES, and JAS.
Declaration of Interests
None declared.
References
- 1. Akl EA, Gaddam S, Gunukula SK, Honeine R, Jaoude PA, Irani J. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. Int J Epidemiol. 2010;39(3):834–857. [DOI] [PubMed] [Google Scholar]
- 2. Arrazola RA, Singh T, Corey CG, et al. Tobacco use among middle and high school students—United States, 2011–2014. MMWR Morb Mortal Wkly Rep. 2015;64(14):381–385. [PMC free article] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention. Drop in Cigarette Consumption Offset by Increases in Other Forms of Smoked Tobacco. 2012. [Google Scholar]
- 4. Katurji M, Daher N, Sheheitli H, Saleh R, Shihadeh A. Direct measurement of toxicants inhaled by water pipe users in the natural environment using a real-time in situ sampling technique. Inhal Toxicol. 2010;22(13):1101–1109. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization. WHO Advisory Note: “Waterpipe Tobacco Smoking: Health Effects, Research Needs and Recommended Actions by Regulators”. Geneva, Switzerland: World Health Organization; 2005. [Google Scholar]
- 6. Zhou S, Behrooz L, Weitzman M, et al. Secondhand hookah smoke: an occupational hazard for hookah bar employees. Tob Control. 2016. doi:10.1136/tobaccocontrol-2015-052505. [DOI] [PubMed] [Google Scholar]
- 7. Zhou S, Weitzman M, Vilcassim R, et al. Air quality in New York City hookah bars. Tob Control. 2015;24(e3):e193–e198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kassem NOF, Daffa RM, Liles S, et al. Children’s exposure to secondhand and thirdhand smoke carcinogens and toxicants in homes of hookah smokers. Nicotine Tob Res. 2014;16(7):961–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ward KD, Vander Weg MW, Relyea G, Debon M, Klesges RC. Waterpipe smoking among American military recruits. Prev Med. 2006;43(2):92–97. [DOI] [PubMed] [Google Scholar]
- 10. Noonan D, Kulbok PA. New tobacco trends: waterpipe (hookah) smoking and implications for healthcare providers. J Am Acad Nurse Pract. 2009;21(5):258–260. [DOI] [PubMed] [Google Scholar]
- 11. Knishkowy B, Amitai Y. Water-pipe (narghile) smoking: an emerging health risk behavior. Pediatrics. 2005;116(1):e113–e119. [DOI] [PubMed] [Google Scholar]
- 12. Eissenberg T, Shihadeh A. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. Am J Prev Med. 2009;37(6):518–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cobb C, Ward KD, Maziak W, Shihadeh AL, Eissenberg T. Waterpipe tobacco smoking: an emerging health crisis in the United States. Am J Health Behav. 2010;34(3):275–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shihadeh A, Saleh R. Polycyclic aromatic hydrocarbons, carbon monoxide, “tar”, and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food Chem Toxicol. 2005;43(5):655–661. [DOI] [PubMed] [Google Scholar]
- 15. Koul PA, Hajni MR, Sheikh MA, et al. Hookah smoking and lung cancer in the Kashmir valley of the Indian subcontinent. Asian Pac J Cancer Prev. 2011;12(2):519–524. [PubMed] [Google Scholar]
- 16. Tamim H, Musharrafieh U, El Roueiheb Z, Yunis K, Almawi WY. Exposure of children to environmental tobacco smoke (ETS) and its association with respiratory ailments. J Asthma.. 2003;40(5):571–576. [DOI] [PubMed] [Google Scholar]
- 17. Nuwayhid IA, Yamout B, Azar G, Kambris MA. Narghile (hubble-bubble) smoking, low birth weight, and other pregnancy outcomes. Am J Epidemiol. 1998;148(4):375–383. [DOI] [PubMed] [Google Scholar]
- 18. American Lung Association. Hookah Smoking: A Growing Threat to Public Health. [Google Scholar]
- 19. Aljarrah K, Ababneh ZQ, Al-Delaimy WK. Perceptions of hookah smoking harmfulness: predictors and characteristics among current hookah users. Tob Induc Dis. 2009;5(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Martinasek MP, Gibson-Young L, Forrest J. Hookah smoking and harm perception among asthmatic adolescents: findings from the Florida youth tobacco survey. J Sch Health. 2014;84(5):334–341. [DOI] [PubMed] [Google Scholar]
- 21. Minaker LM, Shuh A, Burkhalter RJ, Manske SR. Hookah use prevalence, predictors, and perceptions among Canadian youth: findings from the 2012/2013 Youth Smoking Survey. Cancer Causes Control. 2015;26(6):831–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. World Health Organization. WHO Report on the Global Tobacco Epidemic, 2008: The MPOWER Package. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 23.The World Bank. Curbing the epidemic: governments and the economics of tobacco control. Tob Control. 1999;8(2):196–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. American Lung Association. Tobacco Policy Trend Alert: An Emerging Deadly Trend: Waterpipe Tobacco Use. 2007. [Google Scholar]
- 25. Maziak W, Hammal F, Rastam S, et al. Characteristics of cigarette smoking and quitting among university students in Syria. Prev Med. 2004;39(2):330–336. [DOI] [PubMed] [Google Scholar]
- 26. Khabour OF, Alzoubi KH, Eissenberg T, et al. Waterpipe tobacco and cigarette smoking among university students in Jordan. Int J Tuberc Lung Dis. 2012;16(7):986–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Baheiraei A, Shahbazi Sighaldeh S, Ebadi A, Kelishadi R, Majdzadeh R. The role of family on hookah smoking initiation in women: a qualitative study. Global J Health Sci. 2015;7(5):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McKelvey K, Attonito J, Madhivanan P, et al. Determinants of waterpipe smoking initiation among school children in Irbid, Jordan: a 4-year longitudinal analysis. Drug Alcohol Depend. 2014;142:307–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. U.S. Food and Drug Administration. Deeming Tobacco Products To Be Subject to the Federal Food, Drug, and Cosmetic Act, as Amended by the Family Smoking Prevention and Tobacco Control Act; Restrictions on the Sale and Distribution of Tobacco Products and Required Warning Statements for Tobacco Products, 21 CFR Parts 1100, 1140, and 1143. 2016. [PubMed] [Google Scholar]
- 30. Centers for Disease Control and Prevention. 2012–2013 National Adult Tobacco Survey Sample Design and Methodology Summary. Atlanta, Georgia: Center for Disease Control and Prevention; 2015. [Google Scholar]
- 31. Abedini S, MorowatiSharifabad M, Chaleshgar K, ordasiabi M, Ghanbarnejad A. Predictors of non- hookah smoking among high-school students based on prototype/willingness model. Health Promot Perspect. 2014;4(1):46–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Foster DW, Greene MR, Allan NP, Geldsetzer P. The influence of drinking motives on hookah use frequency among young multi-substance users. Int J Mental Health Addict. 2016:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Heinz AJ, Giedgowd GE, Crane NA, et al. A comprehensive examination of hookah smoking in college students: use patterns and contexts, social norms and attitudes, harm perception, psychological correlates and co-occurring substance use. Addict Behav. 2013;38(11):2751–2760. [DOI] [PubMed] [Google Scholar]
- 34. Agaku IT, King BA, Husten CG, et al. Tobacco product use among adults—United States, 2012–2013. MMWR Morb Mortal Wkly Rep. 2014;63(25):542–547. [PMC free article] [PubMed] [Google Scholar]
- 35. Hu SS, Neff L, Agaku IT, et al. Tobacco product use among adults—United States, 2013–2014. MMWR Morb Mortal Wkly Rep. 2016;65(27):685–691. [DOI] [PubMed] [Google Scholar]
- 36. Centers for Disease Control and Prevention. 2012–2013 National Adult Tobacco Survey Weighting Specifications. 2014. [Google Scholar]
- 37. Salloum RG, Thrasher JF, Kates FR, Maziak W. Water pipe tobacco smoking in the United States: findings from the National Adult Tobacco Survey. Prev Med. 2015;71:88–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Primack BA, Shensa A, Kim KH, et al. Waterpipe smoking among U.S. university students. Nicotine Tob Res. 2013;15(1):29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Villanti AC, Cobb CO, Cohn AM, Williams VF, Rath JM. Correlates of hookah use and predictors of hookah trial in U.S. young adults. Am J Prev Med. 2015;48(6):742–746. [DOI] [PubMed] [Google Scholar]
- 40. Linde BD, Ebbert JO, Pasker CK, et al. Prevalence and predictors of hookah use in US Air Force military recruits. Addict Behav. 2015;47:5–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Schoenborn CA. Marital status and health: United States, 1999–2002. Adv Data. 2004(351):1–32. [PubMed] [Google Scholar]
- 42. Stringhini S, Rousson V, Viswanathan B, Gedeon J, Paccaud F, Bovet P. Association of socioeconomic status with overall and cause specific mortality in the Republic of Seychelles: results from a cohort study in the African region. PLoS One. 2014;9(7):e102858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Palamar JJ, Zhou S, Sherman S, Weitzman M. Hookah use among U.S. high school seniors. Pediatrics. 2014;134(2):227–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Haddad L, El-Shahawy O, Ghadban R, Barnett TE, Johnson E. Waterpipe smoking and regulation in the United States: a comprehensive review of the literature. Int J Environ Res Public Health. 2015;12(6):6115–6135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Arrazola RA, Neff LJ, Kennedy SM, et al. Tobacco use among middle and high school students—United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63(45):1021–1026. [PMC free article] [PubMed] [Google Scholar]
- 46. Barnett TE, Smith T, He Y, et al. Evidence of emerging hookah use among university students: a cross-sectional comparison between hookah and cigarette use. BMC Public Health. 2013;13:302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Berg CJ, Stratton E, Schauer GL, et al. Perceived harm, addictiveness, and social acceptability of tobacco products and marijuana among young adults: marijuana, hookah, and electronic cigarettes win. Subst Use Misuse. 2015;50(1):79–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Montgomery SB, De Borba-Silva M, Singh P, Dos Santos H, Job JS, Brink TL. Exploring Demographic and substance use correlates of hookah use in a sample of Southern California community college students. Calif J Health Promot. 2015;13(1):26–37. [PMC free article] [PubMed] [Google Scholar]
- 49. Noonan D, Patrick ME. Factors associated with perceptions of hookah addictiveness and harmfulness among young adults. Subst Abus. 2013;34(1):83–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sidani JE, Shensa A, Barnett TE, Cook RL, Primack BA. Knowledge, attitudes, and normative beliefs as predictors of hookah smoking initiation: a longitudinal study of university students. Nicotine Tob Res. 2014;16(6):647–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Link AR, Cawkwell PB, Shelley DR, Sherman SE. An exploration of online behaviors and social media use among hookah and electronic-cigarette users. Addict Behav Rep. 2015;2:37–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Carroll MV, Shensa A, Primack BA. A comparison of cigarette- and hookah-related videos on YouTube. Tob Control. 2013;22(5):319–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Krauss MJ, Sowles SJ, Moreno M, et al. Hookah-related Twitter chatter: a content analysis. Prev Chronic Dis. 2015;12:E121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Berg CJ, Schauer GL, Asfour OA, Thomas AN, Ahluwalia JS. Psychosocial factors and health-risk behaviors associated with hookah use among college students. J Addict Res Ther. 2011;Suppl 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Primack BA, Mah J, Shensa A, Rosen D, Yonas MA, Fine MJ. Associations between race, ethnicity, religion, and waterpipe tobacco smoking. J Ethn Subst Abuse. 2014;13(1):58–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bruice ME. Smoke Signals: An Analysis of Policies to Reduce Hookah Use Among Adolescents in Washington State. Seattle, WA: University of Washington; 2014. [Google Scholar]
- 57. Bahelah R. Waterpipe tobacco labeling and packaging and World Health Organization Framework Convention on Tobacco Control (WHO FCTC): a call for action. Addiction. 2014;109(2):333. [DOI] [PubMed] [Google Scholar]
- 58. Mannocci A, Colamesta V, Mipatrini D, et al. From directive to practice: are pictorial warnings and plain packaging effective to reduce the tobacco addiction? Public Health. 2015;129(12): 1563–1570. [DOI] [PubMed] [Google Scholar]