Abstract
Objective
Management of type 1 diabetes is a difficult self-regulatory process requiring continued attention to complex regimen tasks. The purpose of this study was to examine whether youths’ attention problems were associated with poorer adherence and HbA1c across time, and whether higher parental involvement reduced these associations.
Methods
Adolescents with type 1 diabetes (N = 199, M age = 12.43 years, SD = 1.50) and their mothers rated youths’ attention problems and adherence at three time points. Adolescents rated parents’ diabetes-specific monitoring and behavioral involvement. HbA1c was collected from medical records.
Results
Adolescents’ (but not mothers’) greater reports of attention problems compared with their average related to lower adherence across time. Adolescents' (but not mothers') reports of greater attention problems compared with their average related to lower adherence across time.
Conclusions
Youth attention problems may help us understand poor adherence, and interventions to promote parental involvement may buffer this risk.
Keywords: adolescents, attention problems, type 1 diabetes
Management of type 1 diabetes is a difficult self-regulatory process that involves adherence to a complex and demanding daily regimen. Regular illness management behaviors require attention to detail, such as remembering to check blood glucose levels, calculating consumed carbohydrates, and administering correct dosages of insulin based on blood glucose and carbohydrate counts (Hood, Peterson, Rohan, & Drotar, 2009). Forgetting or miscalculating these disease-specific tasks may engender poor metabolic control, which can subsequently lead to health complications (American Diabetes Association, 2011). Adolescents encounter unique developmental challenges and distractions that influence their ability to successfully manage the daily self-care demands of diabetes. Hormonal changes during puberty may reduce adolescents’ insulin sensitivity (relating to more labile blood glucose levels) and thus require additional focus and planning to maintain metabolic control (Amiel, Sherwin, Simonson, Lauritano, & Tamborlane, 1986; Tfayli & Arslanian, 2007). Additionally, some youth may become wholly responsible for their diabetes care before they are developmentally equipped to manage their illness independently (Greening, Stoppelbein, & Reeves, 2006; Iannotti & Bush, 1993; Wysocki, Greco, & Buckloh, 2003).
Youth with attention problems are likely to struggle with the complex self-regulatory tasks involved in diabetes management (Pelham, Fabiano, & Massetti, 2005; Sanchez, Chronis, & Hunter, 2006). Faculties in attention allow an individual to assess the environment, maintain focus on a task, and shift that focus to other competing demands when necessary, all of which are crucial processes for success on complicated self-regulatory tasks (Compas & Boyer, 2001; Cooley & Morris, 1990). Attentional regulation is often conceptualized as a foundational skill required for higher order executive function (EF) abilities (Diamond, 2013). Research on EF capabilities and diabetes management has demonstrated that lower EF capabilities are related to lower levels of adherence (Alioto & Janusz, 2004; Duke & Harris, 2014; Suchy et al., 2016), with adherence mediating the associations between EF and poorer metabolic control (McNally, Rohan, Pendley, Delamater, & Drotar, 2010). To the extent that attention skills underlie EF, these results support the idea that even small and temporary fluctuations in attention may influence adolescents’ capacities to use EF faculties in the service of diabetes management. Adults with nonclinical impairments in attention experience increases or decreases in attention within nonclinical levels of attention across days (Stawski, Sliwinski, & Hofer, 2013). Adolescents may also experience such fluctuations, with poorer attention related to events such as forgetting diabetes supplies at home, or getting distracted and overlooking necessary blood glucose checks or insulin injections (Compas & Boyer, 2001; Diamond, 2013).
Attention problems per se have been relatively unexplored in the pediatric diabetes literature. First, it is currently unknown whether attention problems are related to challenges for both adherence and metabolic control. In the two studies that explicitly examined the Attention Problems subscale of the Youth Self-Report (YSR; Achenbach, 1991), Leonard and colleagues (Leonard, Jang, Savik, & Plumbo, 2005; Leonard, Jang, Savik, Plumbo, & Christensen, 2002) found that higher attention problems related to worse metabolic control in a nonclinical sample of adolescents. Adolescents diagnosed with attention deficit/hyperactivity disorder (ADHD; per parent report or evaluation results available via medical records) have also demonstrated poorer metabolic control and higher rates of diabetic ketoacidosis compared with their counterparts without ADHD, even within a fairly well-controlled sample (Hilgard et al., 2017). These studies did not examine whether attention problems were related to diabetes adherence, the behavioral process associated with metabolic control.
Second, it is unclear whether the link between attention problems and diabetes outcomes holds for adolescent and parent report of youth attention problems. The Leonard et al. (2002; 2005) studies used child self-reported attention problems and did not include both youth and parent report, an approach that could provide a more complete picture of these processes in adolescence. On the one hand, research on reporter accuracy of ADHD symptoms has demonstrated that parent or teacher report of youth attention problems may be more reliable than adolescent self-report of the same symptoms (Hoza et al., 2004; Smith, Pelham, Gnagy, Molina, & Evans, 2000). On the other hand, research has suggested that older adolescents may possess unique information about their daily environment, management behaviors, and attention difficulties in everyday tasks unbeknownst to their parents (Ellis et al., 2012; Lehmkuhl et al., 2009). It may be clinically useful to assess whether adolescent or parent report of attention problems is more closely linked to diabetes outcomes over time to determine who is the better choice of report.
Third, the existing studies on attention problems have been cross-sectional in nature; no other known studies have examined the association of attention problems and diabetes outcomes across the period of adolescence. Previous studies have also not allowed for the examination of both between-subjects effects [such as work done by Leonard et al. (2002; 2005)], as well as within-subjects effects across time. The study of these corresponding processes across time is important because aspects of attention problems (Biederman, Mick, & Faraone, 2000) and adherence (King, Berg, Butner, Butler, & Wiebe, 2014) may change across time and therefore may covary together across time. It is possible that changes in parent and adolescent reports of attention problems are reflected in corresponding changes in reports of adherence and adolescent metabolic control. Thus, when adolescents experience more attention problems relative to their average, they may experience correspondingly lower levels of adherence and poorer metabolic control.
Given the challenges with diabetes management that youth with attention problems may experience, help from parents to successfully complete adherence behaviors may moderate the association between attention problems and diabetes outcomes. Sanchez, Chronis, and Hunter (2006) suggest that increased parental monitoring of and involvement with diabetes tasks may improve adolescent adherence behaviors and metabolic control among children with ADHD. Parental monitoring and reinforcement of children’s behavior at home (i.e., Behavioral Parent Training) can improve family functioning and the symptoms of ADHD (Pelham & Fabiano, 2008). The type 1 diabetes literature has also shown that adolescent diabetes management is most successful when it involves a collaborative process between parents and youth (Wiebe et al., 2005; Wysocki et al., 2009) and sustained parental monitoring (Ellis et al., 2007; King et al., 2012). Moreover, studies of Behavioral Family Systems Therapy for Diabetes demonstrate that increased collaboration and diabetes-specific parental involvement can benefit adolescents’ adherence and metabolic control (Wysocki et al., 2007). Parents’ involvement with diabetes may be especially important for early adolescents (as measured at Time 1 in the present study), as we know that responsibility for diabetes care shifts from parents to adolescents and monitoring declines across adolescence (King et al., 2014; Wiebe et al., 2014). Our previous work has demonstrated that adolescents’ perceptions of parental involvement were related to adherence and metabolic control, while parents’ reports of their own involvement were not (Author’s Citation). Thus, in the present study, we examined adolescents’ perceptions of parental involvement and whether adolescents’ levels of adherence would be better in the face of attention problems when adolescents perceived their parents as more involved in or as monitoring more of their diabetes management.
The purpose of the present study was to examine the role of attention problems (as reported by adolescents and mothers) as a predictor of diabetes adherence and metabolic control during adolescence, and whether parental involvement moderated these associations. The current study examined attention problems, adherence, and metabolic control across three time points within a sample of adolescents with type 1 diabetes. First, we explored how fluctuations in adolescents’ attention problems (compared with one’s average) related to type 1 diabetes adherence and metabolic control over three time points. We expected that higher levels of attention problems compared with one’s average would relate to poorer adherence and metabolic control. We also explored whether individual differences in attention problems at the first time point were associated with adherence and metabolic control. We expected that the associations of attention problems with diabetes adherence and metabolic control would be similar for youth and mother report. Second, we explored whether the association between adolescents’ perceptions of their own attention problems and diabetes outcomes in early adolescence (as measured at Time 1) would be reduced when they also saw their parents as more involved and as greater monitors of their own diabetes behavior. We predicted that this would be the case both for adolescents’ perceptions of parents’ behavioral involvement with diabetes and diabetes-specific monitoring (mothers’ and fathers’), and that this effect would be significant for adherence and metabolic control.
Method
Participants
The institutional review board approved the study. Participants included young adolescents (at Time 1, age range = 10–14 years; M age = 12.43 years, SD = 1.50, 54.2% females) diagnosed with type 1 diabetes mellitus and their mothers, recruited as part of a larger longitudinal study that included 252 adolescents and mothers followed every 6 months. Families were largely Caucasian (94%) and middle class. Sixty-six percent of qualifying individuals approached agreed to participate in the first wave of a 3-year longitudinal study. The most common reasons for declining to participate included the distance of commute (18%), being too busy (21%), not interested (30%), uncomfortable with being studied (14%), and time commitment (5%). Comparisons of eligible adolescents who participated versus those who did not indicated that participants were older (12.5 vs. 11.6 years, t (367) = 6.2, p < .01, η2 = .10), but did not differ on gender, pump status, Hba1c, or time since diagnosis compared with nonparticipants (p’s > .20). The measures included in the current study were administered at three time points, spaced at 1-year intervals. The current study only included dyads that had both mother and youth data at two or more time points to allow for comparison of the same sample (any combination of Times 1, 3, and 5; N = 199). At Time 1, participants in the current study had been diagnosed with type 1 diabetes for an average of 4.5 years (or 54 months; SD = 35.34 months) and 56.2% of the sample used an insulin pump. Dyads included did not differ from the overall sample on main study variables (e.g., adherence, metabolic control, attention problems, sex; p’s > .05), excepting the frequency of insulin pump use (participants included more often used an insulin pump, p = .007). This variable (along with time since T1D diagnosis) was used as a covariate in all analyses.
Materials and Procedure
Research staff recruited participants during their regular medical appointment at one of two participating clinics. Parents provided informed consent and adolescents assent. Adolescents and their caregivers reported on youth attention problems, and solely adolescents reported on parents’ involvement with diabetes (i.e., adolescents’ perceptions of parents’ behavioral involvement with diabetes and of mothers’ and fathers’ diabetes-specific monitoring) using take-home survey measures; participants were instructed to complete the measures individually. Dyads completed additional measures during a subsequent in-lab study visit, including a report of youth diabetes adherence. Levels of adherence behaviors, parental monitoring, and parental involvement were comparable with other samples of adolescents with type 1 diabetes (Anderson, Ho, Brackett, Finkelstein, & Laffel, 1997; Helgeson, Reynolds, Siminerio, Escobar, & Becker, 2008). We examined only adolescents’ reports of parental involvement because prior work with this sample has demonstrated that parental report of monitoring was not associated with adherence or HbA1c (Author’s Citation).
Measures
Attention Problems
Youth attention problems were measured via adolescents’ and mothers’ reports on the YSR (Achenbach, 1991) and Child Behavior Checklist (CBC-L; Achenbach, 1991), respectively. For all items, respondents rated whether the behavior was not true (0), somewhat or sometimes true (1), or very true or often true (2) over the prior 6 months. The Attention Problems scale included items that assessed inattentiveness, impulsivity, and hyperactivity, the core components of ADHD. Adolescents’ alphas ranged from .80 to .83; adolescents’ reports were significantly correlated across time points (correlations ranged from r = .48, p ≤ .001 to r = .69, p ≤ .001). Mothers’ alphas ranged from .85 to .88 and correlations ranged from r = .73, p ≤ .001, to r = .75, p ≤ .001 across the three time points. We used raw scores1 for the Attention Problems scale in the final analyses as suggested by Drotar, Stein, and Perrin (1995). Raw scores were summed to create a total score for each reporter at each time point. At Time 1, 6.5% of the mothers and 3.5% of the adolescents reported clinically significant attention problems (≥71, per T-scores). At Time 3, 3.8% of the mothers and 3.3% of the adolescents reported clinically significant attention problems, and at Time 5, 3.4% of the mothers and 1.2% of the adolescents reported clinically significant attention problems.
Parental Monitoring
Adolescents’ perceptions of how much parents “really” knew about their diabetes management were used as an estimate of parental monitoring, as has been done in prior studies (Berg et al., 2008). Adolescents rated their mothers and fathers separately on five items regarding their diabetes care (Berg et al., 2008). Responses on this subscale ranged from 1 (doesn’t know) to 5 (knows everything). An average score was calculated for adolescents’ reports of each parent. This measure demonstrated excellent reliability in the current sample (alphas ranging from .80 to .91 for adolescents’ reports of mothers and fathers across time points).
Parental Involvement
Adolescents rated who was responsible for 23 diabetes management tasks (e.g., “Who determines the insulin dose?”) on a 1 to 5 scale (1 = Child does it alone, 3 = Child and parent share equally, 5= Parent does it alone) using a modified Diabetes Responsibility Scale (Rubin, Young-Hyman, & Peyrot, 1989; Wiebe et al., 2014). The original measure was updated to include items related to current insulin regimens with the help of a certified diabetes educator. Both the initial (Rubin et al., 1989) and modified versions of this scale demonstrate high reliability (α= .92 in this study).
Adherence
Adolescents and mothers completed a 16-item modification of the Self-Care Inventory (adapted from Lewin et al., 2009) to assess adolescent adherence to the diabetes regimen over the preceding month (1 = never did this, to 5 = always did this as recommended without fail). Items reflected contemporary standards for diabetes management related to insulin administration, blood glucose checking, diet, and exercise. Scores on this scale have good internal consistency (alpha= .86 at all time points) in our sample, and correlate well with other more time-intensive interview methods for measuring adherence (Lewin et al., 2009).
Metabolic Control
Metabolic control was obtained via glycosylated hemoglobin percentages (HbA1c) recorded in participants’ medical records. HbA1c is a measure of average blood glucose over the preceding 2- to 3-month period, and lower values indicate better metabolic control (American Diabetes Association, 2013). At Time 1, the average HbA1c for this sample was 8.20% (SD = 1.46).
Data Analysis Plan
Separate hierarchical linear models were conducted for adolescent and mother data using Hierarchical Linear and Nonlinear Modeling (HLM) 7 (Raudenbush, Bryk, Cheong, Congdon, & du Toit, 2011). To assess within-subjects relationships, time-varying covariate models were used at Level 1 to examine the association of adherence and metabolic control with attention problems across the three time points (Aim 1, see equations below). Attention problems were group centered so that the time-varying relationship between diabetes outcomes and attention problems (γ10) represented how fluctuations from a person’s own average level of attention problems predicted fluctuations in adherence. Time was coded 0, 1, and 2 so that the zero value was the first time point.
Additionally, we simultaneously analyzed the relation between attention problems and diabetes outcomes at Time 1, thereby capturing the between-subjects effect during early adolescence. We did this by entering attention problems at Time 1 (centered at the grand mean) as a variable at Level 2, predicting the Level 1 intercept (γ03) and the Level 1 time effect (γ21). The prediction of the Level 1 time effect (γ21) generated an interaction, which made it so that the main effect of attention problems (γ03) was the effect of attention problems at Time 1 on diabetes (either adherence or HbA1c) at Time 1. Therefore, the effect of attention problems at Time 1 (γ03) predicted diabetes outcomes at Time 1 only (the between-subjects effect). Without the inclusion of (γ21), the effect of attention problems at Time 1 (γ03) would represent the effect of attention problems at Time 1 on the average level of adherence across the three time points.
In all models, we did not allow for random effects on attention problems to avoid having an overspecified model. Finally, at Level 2, pump status (0 = multiple daily injections, 1 = using a pump) and time since diabetes diagnosis (in number of months) were included as covariates, as such variables frequently relate to both metabolic control and adherence.
Level-1 Model
Level-2 Model
To address Aim 2, we ran six (adolescent-reported attention problems × adolescent report of three types of parents’ diabetes involvement × two diabetes outcomes) separate multilevel models to test for the moderating effects of adolescents’ perceptions of parenting on their reports of attention problems in predicting their reports of adherence and HbA1c. We restricted this analysis to solely adolescents’ reports of attention problems, adherence, and parental involvement, as our previous work (Author’s Citation) indicated that only adolescents’ reports of parental involvement were associated with diabetes outcomes. At Level 1, adolescent-reported attention problems and time point were entered as predictors of adherence and metabolic control. To capture whether parental involvement at Time 1 moderated the effect of attention problems on adherence, we created interactions in SPSS between grand mean centered Time 1 attention problems × grand mean centered Time 1 parental diabetes involvement scores (separate interactions were created for behavioral involvement, maternal monitoring, and paternal monitoring). We selected Time 1 parental involvement as an examination of parental involvement because the examination of parental involvement across time could not be conducted with the time point variable included and only three time points (i.e., owing to the limited number of parameters available to be estimated). The selection of Time 1 also allowed us to examine the compensatory effect of parental involvement at a time when parents are most involved (as shown in our previous work with this sample; Author’s Citation) and attention problems may exert their greatest effect on adherence and metabolic control. Then in six separate analyses, we entered the interaction (and the main effects) on the intercept at Level 2 as moderators of the attention problems/adherence (attention problems/metabolic control) relationship. Consistent with our previous analyses, we also entered the interaction and main effect terms on the time variable (β2i), so that the coefficient of the interaction on the Level 2 intercept (γ04) was conditional on the time variable, and therefore represented how the Time 1 attention problems × Time 1 parental involvement interaction was associated with Time 1 adherence (and metabolic control; see model provided below). Recall that because Time 1 was centered at zero, this makes it so the effect is between subjects at Time 1. Adolescent age was tested as a moderator to account for differences in participant age at Time 1, but was not significant, and thus was dropped from the subsequent analyses.
Level-1 Model
Level-2 Model
Results
Association of Attention Problems and Diabetes Outcomes Over Time
To examine whether adherence and HbA1c were associated with fluctuations in attention problems over time (Aim 1), we conducted separate HLM analyses predicting adherence and HbA1c from adolescent and mother report of attention problems, controlling for study time point, time since diagnosis, and pump status (see Table I). Adolescents’ fluctuations from their average reports of attention problems related to adherence across three time points β1i, such that when adolescents reported more attention problems compared with their average, they reported lower levels of adherence. When controlling for the Level 1 effect, the association between Time 1 attention problems and Time 1 adherence was not significant (γ03), but trended in the expected direction. Fluctuations in adolescents’ reports of attention problems over time (β1i) were not related to HbA1c over time. Conversely, adolescents’ reports of attention problems at Time 1 did predict metabolic control at Time 1 (γ03), such that more attention difficulties related to poorer (higher) HbA1c at the first time point.
Table I. Adherence and Metabolic Control Predicted From YSR/CBC-L Attention Problems
| Adolescent report |
Mother report |
|||||
|---|---|---|---|---|---|---|
| Variable | B | SE | t | B | SE | t |
| DV: Adherence | ||||||
| Intercept (β0i) | 3.98 | 0.04 | 107.96*** | 3.62 | 0.03 | 113.21*** |
| Pump status (γ01) | 0.16 | 0.06 | 2.53* | 0.16 | 0.06 | 2.68** |
| Time since diagnosis (γ02) | −0.001 | 0.001 | −1.62 | −0.003 | 0.001 | −3.98*** |
| T1 attention problems (γ03) | −0.02 | 0.01 | −1.81 | −0.04 | 0.01 | −4.78*** |
| Attention problems (β1i) | −0.03 | 0.01 | −3.08** | −0.01 | 0.01 | −1.11 |
| Time (β2i) | −0.06 | 0.01 | −4.16*** | −0.06 | 0.01 | −6.02*** |
| T1 attention problems (γ21) | −0.01 | 0.005 | −1.37 | 0.0001 | 0.003 | 0.06 |
| DV: Metabolic control | ||||||
| Intercept (β0i) | 8.33 | 0.10 | 87.38*** | 8.31 | 0.10 | 86.30*** |
| Pump status (γ01) | −0.93 | 0.18 | −5.11*** | −0.90 | 0.19 | −4.77*** |
| Time since diagnosis (γ02) | 0.01 | 0.003 | 1.96 | 0.01 | 0.003 | 1.65 |
| T1 attention problems (γ03) | 0.10 | 0.03 | 4.02*** | 0.07 | 0.03 | 2.40* |
| Attention problems (β1i) | −0.03 | 0.02 | −1.18 | 0.01 | 0.02 | 0.42 |
| Time (β2i) | 0.18 | 0.03 | 6.36*** | 0.18 | 0.03 | 6.49*** |
| T1 attention problems (γ21) | −0.02 | 0.01 | −1.72 | −0.002 | 0.01 | −0.27 |
p < .05; **p < .01; ***p < .001.
DV = Dependent Variable; YSR/CBC-L = Youth Self-Report/Child Behavior Checklist.
Fluctuations in mothers’ reports of adolescent attention problems over time were not related to their reports of adolescents’ adherence or to HbA1c (β1i). In contrast, mothers’ reports of attention problems at Time 1 were related to both their reports of adolescents’ adherence and to HbA1c at Time 1 (γ03), reflecting that more attention problems at Time 1 related to both poorer adherence (lower) and metabolic control (higher) at this time point.
Attention Problems Moderated by Parents’ Involvement With Diabetes
To assess whether parental involvement moderated attention problems over time to predict adherence and HbA1c, we examined adolescents’ reports of their attention problems as moderated by their reports of parents’ diabetes involvement and mothers’ and fathers’ diabetes monitoring. First, we input the adolescent Attention Problems scale (group centered) as a predictor at Level 1, along with time point. Next, we entered the Time 1 interaction term (grand mean centered in SPSS), its main effects, and covariates on the intercept at Level 2. The main effect and interaction terms were also entered on the time point variable at Level 2.
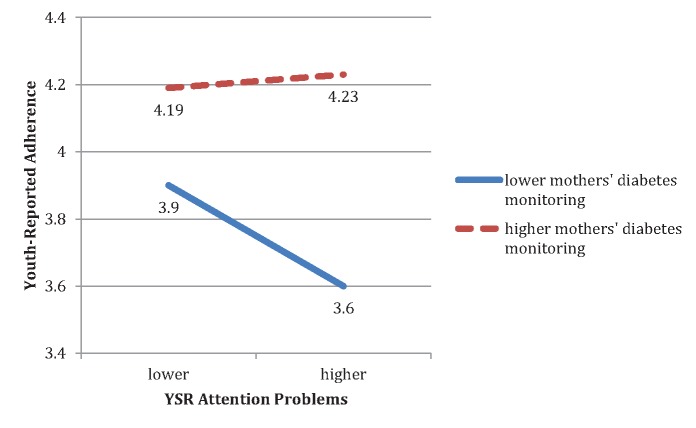
Greater adolescent-perceived mothers’ diabetes monitoring at Time 1 was significantly related to better Time 1 adherence (b = 0.29, SE = 0.05, t = 6.40, p ≤ .001), and also significantly moderated the association between self-reported attention problems and adherence at Time 1 (b = 0.03, SE = 0.01, t = 2.30, p = .022). Simple slope effects of this two-way interaction were tested at lower (−1 SD) and higher (+1 SD) levels of Time 1 mothers’ diabetes monitoring (corresponding to centered values of −0.79 and 0.79) using methods by Preacher, Curran, and Bauer (2006). Figure 1 illustrates simple slopes of the association between attention problems and adherence by mothers’ diabetes monitoring. As predicted, for adolescents who reported lower levels of mothers’ diabetes monitoring at Time 1, higher attention problems were associated with poorer adherence (b = −0.04, SE = 0.01, t = −3.68, p = .0003); however, when mothers’ monitoring was higher, attention problems were not associated with adherence (b = 0.005, SE = 0.01, t = 0.28, p = .78). Youth-reported mothers’ diabetes monitoring did not moderate the association between self-reported attention problems and metabolic control (b = −0.009, SE = 0.03, t = −0.29, p = .77). Fathers’ diabetes monitoring at Time 1 did not significantly moderate the association between Time 1 attention problems and adherence (b = −0.01, SE = 0.008, t = −1.52, p = .13) or metabolic control (b = −0.01, SE = 0.02, t = −0.47, p = .64).
Figure 1.
Simple slopes as a function of youth-reported mothers’ diabetes monitoring.
Note: Lower and higher values of youth-reported mothers’ diabetes monitoring are defined as ± 1 SD about the mean (centered values of −.79 and .79). The simple slope of association between youth-reported attention problems and adherence at Time 1 is not significantly different from zero for those with higher mothers’ diabetes monitoring; the simple slope for lower mothers’ diabetes monitoring is significantly different from zero (see text for simple slope estimates and results of significance tests).
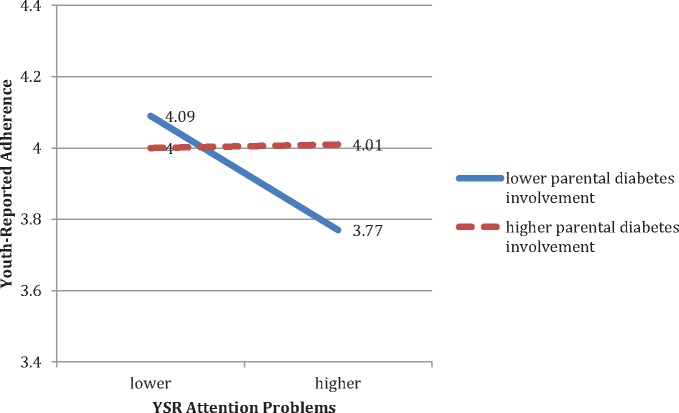
The association between adolescents’ attention problems and adherence at Time 1 was also significantly moderated by youth reports of parents’ behavioral involvement (b = 0.03, SE = 0.01, t = 2.57, p = .011) at Time 1. Contrary to the results previously presented for Aim 1, in this model, youth-reported attention problems at Time 1 were significantly associated with Time 1 adherence (b = −0.02, SE = 0.01, t = −2.0, p = .047). We tested simple slope effects of the two-way interaction at lower (−1 SD) and higher (+1 SD) levels of Time 1 parental involvement (centered values of −0.62 and 0.62, respectively) again using methods by Preacher et al. (2006). Figure 2 illustrates simple slopes of the association between attention problems and adherence by parents’ diabetes involvement. At Time 1, when adolescents perceived parents as less involved with diabetes, adolescents’ attention problems were associated with lower adherence (b = −0.05, SE = 0.01, t = −3.39, p = .0008); however, when adolescents perceived parents as more involved, attention problems were not associated with adherence (b = 0.002, SE = 0.02, t = 0.11, p = .91). These findings support the idea that parental involvement moderated the relation between attention problems and adherence2.
Figure 2.
Simple slopes as a function of youth-reported parents’ diabetes involvement.
Note: Lower and higher values of parents’ diabetes involvement are defined as ± 1 SD about the mean (centered values of −.62 and .62). The simple slope of association between youth-reported attention problems and adherence at Time 1 is not significantly different from zero for those with higher parental diabetes involvement; the simple slope for lower parents’ diabetes involvement is significantly different from zero (see text for simple slope estimates and results of significance tests).
Discussion
Overall, results indicated that adolescents’ attention problems as measured by the CBC-L/YSR Attention Problems subscale related to both diabetes outcomes at Time 1 and to adherence across time. Specifically, fluctuations in adolescents’ self-reported attention problems were associated with self-reported adherence over a 2-year period. In addition, adolescents’ reports of attention problems at Time 1 were associated with their metabolic control at Time 1, indicating that youth who reported higher attention problems during early adolescence were less able to manage their diabetes at that time. Fluctuations in mothers’ reports of youth attention problems on the CBC-L were not related to their reports of adolescents’ adherence or to HbA1c over time in time-varying covariate models. However, mothers’ reports of adolescents’ attention problems at Time 1 were significantly associated with their reports of Time 1 adherence and metabolic control. It is somewhat surprising that while mothers’ reports of attention problems were associated with adherence at Time 1, their reports of attention problems over time did not covary with adherence (i.e., did not emerge in multilevel models across time). Mothers’ perceptions of adolescents’ attention problems may be more stable over time and reflect less within-subjects variability, evidenced by larger correlations between their reports at each time point when compared with adolescents’ reports. The within-subjects relation between adolescents’ reports of adherence and attention problems may reflect adolescents’ greater sensitivity to changes across time. This relation may also reflect superior knowledge of their daily management abilities across adolescence, and potentially a greater understanding (compared with parents’) of how their continual management (i.e., their daily adherence) is influenced by lapses in attention (Berg et al., 2014).
The lack of associations between fluctuations in adolescents’ reports of attention problems and HbA1c and between mothers’ reports and adherence/HbA1c across time could be owing to the specific measure of attention problems used in this study, which may not fully capture domains of impaired functioning. Results may have differed had we used a symptom-specific measure expressly designed to diagnose attention problems. In support of this idea, Berg et al. (2014) found that in a sample of older adolescents, the Conners’ scales for ADHD were associated with both mother- and adolescent-reported global adherence. Moreover, objective measures of attention problems such as the Conners’ Continuous Performance Task (CPT 3; Conners, 2014) may also more effectively capture clinically significant attention problems, making it easier to detect associations with diabetes management.
Results of the parental involvement moderation analyses supported our hypotheses of parental buffering on attention problems. Specifically, Time 1 mothers’ diabetes monitoring and parents’ behavioral involvement with diabetes each significantly moderated the Time 1 YSR attention problems/adherence association; in both cases, lower levels of parents’ involvement (i.e., simple slopes) were significant, such that lower involvement at Time 1 appeared especially detrimental for adolescents with higher attention problems. These results support the idea that parental involvement can support adolescents who concurrently experience attention problems and lower levels of adherence. However, we recommend caution when interpreting these findings, as a more comprehensive assessment of parental involvement is needed that assesses changes in involvement across time. In the present study, we were unable to test the interaction between attention problems and parental involvement across time with study time point included in the model because we only had three time points at our disposal, limiting the number of parameters available to be estimated.
The results of the present study must be interpreted in the context of some limitations. First, this sample of adolescents was reflective of the clinic population at endocrinology clinics in one western U.S. city, where the population was mostly Caucasian from middle to high socioeconomic backgrounds. Although those who participated did not differ on race/ethnicity compared with those who did not participate, results of the current study should be replicated in a more diverse sample. Second, we are interpreting the association among attention problems and diabetes outcomes in the context of a nonclinical sample. It is possible that the association between attention problems and diabetes management would be heightened in a sample of adolescents with clinically significant attention problems. Relatedly, we did not have available data as to whether adolescents were receiving treatment for clinically significant attention problems, which is important data to further understand the range of attention problems. Third, the analyses examined how attention problems covaried with adherence and metabolic control, and thus, causal directions cannot be made. Multiple studies have argued that poor metabolic control leads to cognitive difficulties, such as attention problems and executive dysfunction (Naguib, Kulinskaya, Lomax, & Garralda, 2009; Rovet & Alvarez, 1997). The fact that our results held when controlling for time since diagnosis addresses this concern to some extent. Finally, we used subjective reports of youth attention problems and adherence rather than behavioral measures of these constructs, making it possible that the association between adolescent-reported attention problems and adherence reflects common method variance. More objective measures of diabetes adherence that are likely influenced by attention difficulties (e.g., glucometer and insulin pump downloads for frequency of blood glucose monitoring and insulin administration) could be used in future studies. Further research is needed to ascertain whether the link between attention problems and adherence over time results in clinically significant metabolic outcomes.
This study is important in evaluating the associations between adolescents’ and mothers’ reports of attention problems and adherence across time. Examining these associations is essential, as we know that adherence, metabolic control, and parental involvement typically decline across adolescence, with deteriorations in parental involvement predicting subsequent poorer diabetes outcomes for youth (King et al., 2012; King et al., 2014). Our results demonstrated a relation between higher attention problems and poorer adherence in a nonclinical sample (i.e., most scores fell within the normative range of attention problems); even larger associations may occur among patients with clinically elevated levels of attention problems. Therefore, the results suggest that the consideration of adolescent attention problems within the context of type 1 diabetes is important in clinical practice, as it has implications for disease management. First, evaluation of attention problems even within a nonclinical sample may help to identify youth who may also demonstrate difficulty managing the complex tasks of the diabetes regimen. Additionally, assessing attention problems may alert physicians and families alike to the need for additional parental support with diabetes management. Although different kinds of interventions might be needed for those adolescents experiencing attention problems within a nonclinical range, our results suggest that some parental support is helpful for adherence. In summary, the intersection of attention problems and type 1 diabetes management represents an important area for future study, with possible implications for intervention with youth and their families.
Funding
This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health (Grant Number R01 DK063044).
Conflicts of interest: None declared.
Acknowledgment
The authors thank the physicians and staff at the Utah Diabetes Center, Mountain Vista Medicine, and the parents and adolescents who participated in this study.
Footnotes
1 T-scores were also tested in analyses without significant change in results.
2 Additional models were run without time point included as a Level 1 predictor: the attention problems × parental involvement (diabetes involvement and monitoring) interactions and their main effect terms were entered at Level 1 (group centered by hand in SPSS) and covariates were entered at Level 2. Parental involvement significantly moderated the effect of attention problems, both on adherence (b = 0.14, SE = 0.05, t = 3.08, p = .002) and metabolic control (b = −0.22, SE = 0.11, t = −1.97, p = .05), such that when adolescents perceived their parents as less involved with diabetes, adolescents’ attention problems were associated with lower adherence and higher metabolic control across time points. Adolescents’ reports of mothers’ and fathers’ diabetes monitoring did not moderate the effect of attention problems on adherence or metabolic control (p’s > .4).
References
- Achenbach T. M. (1991). Manual for the child behavior checklist. Burlington, VT: University of Vermont. [Google Scholar]
- Alioto A., Janusz J. A. (2004). The role of executive functioning in adolescents’ self-management of type 1 diabetes. Poster session presented at the Child Health Conference, Charleston, SC.
- American Diabetes Association. (2011). Living with diabetes: Complications. Retrieved from http://www.diabetes.org/living-with-diabetes/complications/?loc=DropDownLWD-complications
- American Diabetes Association. (2013). A1c. Retrieved from http://www.diabetes.org/living-with-diabetes/treatment-and-care/blood-glucose-control/a1c/
- Amiel S. A., Sherwin R. S., Simonson D. C., Lauritano A. A., Tamborlane W. V. (1986). Impaired insulin action in puberty: A contributing factor to poor glycemic control in adolescents with diabetes. The New England Journal of Medicine, 315, 215–219. [DOI] [PubMed] [Google Scholar]
- Anderson B., Ho J., Brackett J., Finkelstein D., Laffel L. (1997). Parental involvement in diabetes management tasks: Relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes mellitus. The Journal of Pediatrics, 130, 257–265. [DOI] [PubMed] [Google Scholar]
- Berg C. A., Butler J. M., Osborn P., King G., Palmer D. L., Butner J., Murray M., Lindsay R., Donaldson D., Foster C., Swinyard M., Wiebe D. J. (2008). Role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 diabetes. Diabetes Care, 31, 678–683. doi:10.2337/dc07-1678 [DOI] [PubMed] [Google Scholar]
- Berg C. A., Wiebe D. J., Suchy Y., Hughes A. E., Anderson J. H., Godbey E. I., Butner J., Tucker C., Franchow E. I., Pihlaskari A. K., King P. S., Murray M. A., White P. C. (2014). Individual differences and day-to-day fluctuations in perceived self-regulation associated with daily adherence in late adolescents with type 1 diabetes. Journal of Pediatric Psychology, 39, 1038–1048. doi:10.1093/jpepsy/jsu05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J., Mick E., Faraone S. V. (2000). Age-dependent decline of symptoms of attention deficit hyperactivity disorder: Impact of remission definition and symptom type. American Journal of Psychiatry, 157, 816–818. [DOI] [PubMed] [Google Scholar]
- Compas B. E., Boyer M. C. (2001). Coping and attention: Implications for child health and pediatric conditions. Developmental and Behavioral Pediatrics, 22, 323–333. [DOI] [PubMed] [Google Scholar]
- Conners C. K. (2014). Continuous performance test III. Toronto: Pearson. [Google Scholar]
- Cooley E. L., Morris R. D. (1990). Attention in children: A neuropsychologically based model for assessment. Developmental Neuropsychology, 6, 239–274. [Google Scholar]
- Diamond A. (2013). Executive functions. Annual Review of Psychology, 64, 135–168. Doi: 10.1146/annurev-psych-113011-143750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drotar D., Stein R. E. K., Perrin E. C. (1995). Methodological issues in using the child behavior checklist and its related instruments in clinical child psychology research. Journal of Clinical Child Psychology, 24, 184–192. [Google Scholar]
- Duke D. C., Harris M. A. (2014). Executive function, adherence, and glycemic control in adolescents with type 1 diabetes: A literature review. Current Diabetes Reports, 14, 532–541. DOI: 10.1007/s11892-014-0532-y. [DOI] [PubMed] [Google Scholar]
- Ellis D. A., Podolski C. L., Frey M., Naar-King S., Wang B., Moltz K. (2007). The role of parental monitoring in adolescent health outcomes: Impact on regimen adherence in youth with type 1 diabetes. Journal of Pediatric Psychology, 32, 907–917. doi:10.1093/jpepsy/jsm009 [DOI] [PubMed] [Google Scholar]
- Ellis D. A., Templin T. N., Moltz K., Naar-King S., Dekelbab B., Carcone A. I. (2012). Psychometric properties of the revised parental monitoring of diabetes care questionnaire in adolescents with type 1 diabetes. Journal of Adolescent Health, 50, 289–295. doi:10.1016/j.jadohealth.2011.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greening L., Stoppelbein L., Reeves C. B. (2006). A model for promoting adolescents’ adherence to treatment for type 1 diabetes mellitus. Children’s Health Care, 35, 247–267. [Google Scholar]
- Helgeson V. S., Reynolds K. A., Siminerio L., Escobar O., Becker D. (2008). Parent and adolescent distribution of responsibility for diabetes self-care: Links to health outcomes. Journal of Pediatric Psychology, 33, 497–508. doi:10.1093/jpepsy/jsm081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilgard D., Konrad K., Meusers M., Bartus B., Otto K. P., Lepler R., Schober E., Bollow E., Holl R. W (2016). Comorbidity of attention deficit hyperactivity disorder and type 1 diabetes in children and adolescents: Analysis based on the multicentre DPV registry. Pediatric Diabetes, 1-8. Advance online publication. DOI 10.1111/pedi.12431. [DOI] [PubMed] [Google Scholar]
- Hood K. K., Peterson C. M., Rohan J. M., Drotar D. (2009). Association between adherence and glycemic control in pediatric type 1 diabetes: A meta-analysis. Pediatrics, 124, e1171–e1179. doi:10.1542/peds.2009-0207 [DOI] [PubMed] [Google Scholar]
- Hoza B., Gerdes A. C., Hinshaw S. P., Arnold L. E., Pelham W. E., Molina B. S., Abikoff H. B., Epstein J. N., Greenhill L. L., Hechtman L., Odbert C., Swanson J. M., Wigal T. (2004). Self-perceptions of competence in children with ADHD and comparison children. Journal of Consulting and Clinical Psychology, 72, 382–391. doi: 10.1037/0022-006X.72.3.382 [DOI] [PubMed] [Google Scholar]
- Iannotti R. J., Bush P. J. (1993). Toward a developmental theory of compliance In Krasnegor N. A., Epstein L., Johnson S. B., Yaffe S. (Eds.), Developmental aspects of health compliance behavior (pp. 59–76). Hillsdale, NJ: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- King P. S., Berg C. A., Butner J., Butler J. M., Wiebe D. J. (2014). Longitudinal trajectories of parental involvement in type 1 diabetes and adolescents' adherence. Health Psychology, 33, 424–432. doi: 10.1037/a0032804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King P. S., Berg C. A., Butner J., Drew L. M., Foster C., Donaldson D., Murray M., Swinyard M., Wiebe D. J. (2012). Longitudinal trajectories of metabolic control across adolescence: Associations with parental involvement, adolescents’ psychosocial maturity, and health care utilization. Journal of Adolescent Health, 50, 491–496. doi:10.1016/j.jadohealth.2011.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmkuhl H. D., Cammarata C., Meyer K., Duke D., Lewin A., Williams L., Storch E. A., Nichols R., Silverstein J., Geffken G. R. (2009). Psychometric properties of a self-report measure of adherence to the diabetes regimen. Children’s Health Care, 38, 76–90. doi: 10.1080/02739610802615914 [Google Scholar]
- Leonard B. J., Jang Y. P., Savik K., Plumbo P. M. (2005). Adolescents with type 1 diabetes: Family functioning and metabolic control. Journal of Family Nursing, 11, 102–121. doi:10.1177/1074840705275152 [DOI] [PubMed] [Google Scholar]
- Leonard B. J., Jang Y. P., Savik K., Plumbo P. M., Christensen R. (2002). Psychosocial factors associated with levels of metabolic control in youth with type 1 diabetes. Journal of Pediatric Nursing, 17, 28–37. doi:10.1053/jpdn.2002.30931 [DOI] [PubMed] [Google Scholar]
- Lewin A. B., La Greca A. M., Geffken G. R., Williams L. B., Duke D. C., Storch E. A., Silverstein J. H. (2009). Validity and reliability of an adolescent and parent rating scale of type 1 diabetes adherence behaviors: The self-care inventory (SCI). Journal of Pediatric Psychology, 34, 999–1007. doi:10.1093/jpepsy/jsp032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally K., Rohan J., Pendley J. S., Delamater A., Drotar D. (2010). Executive functioning, treatment adherence, and glycemic control in children with type 1 diabetes. Diabetes Care, 33, 1159–1162. DOI: 10.2337/dc09-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naguib J. M., Kulinskaya E., Lomax C. L., Garralda M. E. (2009). Neuro-cognitive performance in children with type 1 diabetes—A meta-analysis. Journal of Pediatric Psychology, 34, 271–282. doi:10.1093/jpepsy/jsn074 [DOI] [PubMed] [Google Scholar]
- Pelham W. E., Fabiano G. A. (2008). Evidence-based psychosocial treatments for attention-deficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology, 37, 184–214. doi:10.1080/15374410701818681 [DOI] [PubMed] [Google Scholar]
- Pelham W. E., Fabiano G. A., Massetti G. M. (2005). Evidence-based assessment of attention deficit hyperactivity disorder in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34, 449–476. doi:10.1207/s15374424jccp3403_5 [DOI] [PubMed] [Google Scholar]
- Preacher K. J., Curran P. J., Bauer D. J. (2006). Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31, 437–448. [Google Scholar]
- Raudenbush S. W., Bryk A. S., Cheong Y. F., Congdon R. T., Du Toit M. (2011). HLM 7: Hierarchical linear and nonlinear modeling. Lincolnwood, IL: SSI. [Google Scholar]
- Rovet J., Alvarez M. (1997). Attentional functioning in children and adolescents with IDDM. Diabetes Care, 20, 803–810. [DOI] [PubMed] [Google Scholar]
- Rubin R. R., Young-Hyman D., Peyrot M. (1989). Parent– child responsibility and conflict in diabetes care. Diabetes Care, 38, 28A. [Google Scholar]
- Sanchez L. M., Chronis A. M., Hunter S. J. (2006). Improving compliance with diabetes management in young adolescents with Attention-Deficit/Hyperactivity disorder using behavior therapy. Cognitive and Behavioral Practice, 13, 134–145. [Google Scholar]
- Smith B. H., Pelham W. E., Gnagy E., Molina B., Evans S. (2000). The reliability, validity, and unique contributions of self-report by adolescents receiving treatment for attention deficit/hyperactivity disorder. Journal of Consulting and Clinical Psychology, 68, 489–499. doi:10.1037//0022-006X.68.3.489 [DOI] [PubMed] [Google Scholar]
- Stawski R. S., Sliwinski M. J., Hofer S. M. (2013). Between-person and within-person associations among processing speed, attention switching, and working memory in younger and older adults. Experimental Aging Research, 39, 194–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchy Y., Turner S. L., Queen T. L., Duraccio K., Wiebe D. J., Butner J., Franchow E. I., White P. C., Murray M. A., Swinyard M., Berg C. A. (2016). The relation of questionnaire and performance-based measures of executive functioning with type 1 diabetes outcomes among late adolescents. Health Psychology, 35, 661–669. http://dx.doi.org/10.1037/hea0000326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tfayli H., Arslanian S. (2007). The challenge of adolescence: Hormonal changes and sensitivity to insulin. Diabetes Voice, 52, 28–30. [Google Scholar]
- Wiebe D. J., Berg C. A., Korbel C., Palmer D. L., Beveridge R. M., Upchurch R., Lindsay R., Swinyard M. T., Donaldson D. L. (2005). Children’s appraisals of maternal involvement in coping with diabetes: Enhancing our understanding of adherence, metabolic control, and quality of life across adolescence. Journal of Pediatric Psychology, 30, 167–178. doi:10.1093/jpepsy/jsi004 [DOI] [PubMed] [Google Scholar]
- Wiebe D. J., Chow C. M., Palmer D. L., Butner J., Butler J. M., Osborn P., Berg C. A. (2014). Developmental factors associated with longitudinal declines in parental responsibility and adherence to type 1 diabetes management across adolescence. Journal of Pediatric Psychology, 39, 532–541. doi: 10.1093/jpepsy/jsu006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wysocki T., Greco P., Buckloh L. M. (2003). Childhood diabetes in psychological context In Roberts M. C. (Ed.), Handbook of pediatric psychology (3rd ed., pp. 304–320). New York, NY: Guilford. [Google Scholar]
- Wysocki T., Harris M. A., Buckloh L. M., Mertlich D., Lochrie A. S., Mauras N., White N. H. (2007). Randomized trial of behavioral family systems therapy for diabetes maintenance of effects on diabetes outcomes in adolescents. Diabetes Care, 30, 555–560. [DOI] [PubMed] [Google Scholar]
- Wysocki T., Nansel T. R., Holmbeck G. N., Chen R., Laffel L., Anderson B. J., Weissberg-Benchell J. (2009). Collaborative involvement of primary and secondary caregivers: associations with youth’s diabetes outcomes. Journal of Pediatric Psychology, 34, 869–881. doi:10.1093/jpepsy/jsn136. [DOI] [PMC free article] [PubMed] [Google Scholar]