Abstract
Objective
Dog-bite injury posits a significant threat to children globally. This review evaluated efficacy of cognitive/behavioral interventions for improving children’s knowledge and behaviors around dogs.
Methods
Manuscripts published before January 3, 2014 evaluating cognitive/behavioral interventions for dog-bite prevention among children <18 years of age were eligible for inclusion. Among 2,270 abstracts screened, 123 full texts were retrieved. Twelve studies were included in the qualitative synthesis; nine were included in the meta-analysis. Risk of bias and quality of evidence were evaluated.
Results
Cognitive/behavioral interventions had a moderate effect in improving children’s knowledge and a larger effect in improving children’s behavior with dogs. The most effective intervention strategies were video for knowledge and instruction with live dogs for behaviors. Quality of evidence was poor.
Conclusions
Cognitive/behavioral interventions have potential to improve both children’s knowledge and behaviors around dogs. Future interventions should include multiple follow-ups on dog-bite rates from an international perspective using rigorous randomized controlled trials.
Keywords: children, dog-bite, injury, meta-analysis, prevention, review
Introduction
Dogs are often described as “man’s best friend.” As much companionship and comfort as dogs bring, however, dog-bite injuries present a serious risk to humans, and especially to children. The Centers for Disease Control and Prevention estimated >133,000 dog-bite injuries for children <18 years of age living in the United States in 2013, ranking dog bites among the top 10 nonfatal injuries for children aged 5–9 years (NCIPC, 2015). Internationally, dog-bite injury threatens children even more dramatically. This is especially true in developing regions, some of which report an estimated incidence rate about 100 times higher than that in developed countries (Georges & Adesiyun, 2008; Si et al., 2008).
Two primary factors lead to increased vulnerability of children to dog-bite injuries compared with adults, their physical size and their cognitive development. Smaller physical size increases both risk and severity of pediatric dog-bite injuries, as children’s short stature makes them more likely to suffer from dog bites in the head and neck region (Bernardo, Gardener, Rosenfield, Cohen, & Pitetti, 2002; Hon et al., 2007; Mcheik, Vergnes, & Bondonny, 2000). Children’s underdeveloped cognitive functioning, including their poor perception of vulnerability and their tendency to behave impulsively, also significantly increases dog-bite risk (Chouinard, 2007; Shen et al., 2013).
Despite substantial risk for pediatric dog-bite injuries globally, scientifically documented preventive efforts to reduce dog-bite injuries among children are few. Existing interventions can be categorized into two types: interventions targeting environmental factors such as dog management policies and cognitive/behavioral interventions teaching children to reduce their dog-bite risk. Examples of environmental interventions include fencing, castration efforts, and policy-making on dog management (Beaver, 2001; Hopkins, Schubert, & Hart, 1976; Klaassen, Buckley, & Esmail, 1996); they show mixed effect on reducing dog-bite injuries (Cleaveland, Kaare, Tiringa, Mlengeya, & Barrat, 2003; Klaassen et al., 1996; Overall & Love, 2001). This review focuses on the second category, interventions designed to change children’s cognition, knowledge, and/or behaviors around dogs. Interventions adopting this approach use a wide range of strategies that aim to improve children’s cognition and knowledge about how to engage with dogs, and ultimately to change their behavior so they are less likely to provoke dogs into biting. Intervention methodologies range widely and include traditional one-way (adult to child) educational programs (e.g., Beaver, 2001; Chapman, Cornwall, Righetti, & Sung, 2000; Shen, Pang, & Schwebel, 2015; Spiegel, 2000), interactive classroom-based lesson plans (e.g., Szecsi, Barbero, Del Campo, & Toledo, 2010; Wilson, Dwyer, & Bennett, 2003), and self-teaching lessons using animated computerized tasks (e.g., Meints & De Keuster, 2006, 2009; Schwebel, Morrongiello, Davis, Stewart, & Bell, 2012). Intervention strategies include education, cognitive restructuring, and behavior modification.
The present study was designed to systematically review existing evidence and inform further development and implementation of strategies to train children to be safer with dogs and reduce dog-bite risk. In particular, we sought to identify whether some intervention strategies may be more effective than others and whether outcomes might differ across children of different age-groups. Just one published systematic review has considered pediatric dog-bite injury interventions previously (Duperrex, Blackhall, Burri, & Jeannot, 2009). Framed as a systematic and quantitative review, it did not implement meta-analytic techniques owing to the low number of manuscripts (two) that met inclusion criteria. We updated results from Duperrex and colleagues (2009) by using more liberal inclusion criteria and incorporating all manuscripts on cognitive/behavioral interventions on dog-bite injury prevention published through March 2014.
Methods
Literature Search Strategy
The following databases were searched: MEDLINE (PubMed), PsycINFO, SafetyLit, CAB Abstract, Scopus, Dissertations & Theses, Worldcat, and Grey Literature in the Health Sciences. We used the following search term for all searches: “(dog OR dogs OR canine) AND (bite* OR scratch* OR injury OR injuries or safety) AND (child* or pediatric or paediatric).” In an effort to update the 2009 review by Duperrex et al. (2009), we searched all years (earliest date available in the database through March 2014) and languages available in each database without restriction. To supplement those searches, we also reviewed our personal libraries, posted inquiries on relevant scientific society listservs, and contacted prominent authors in the field to see whether they had or were aware of relevant unpublished materials. We also followed references in relevant articles and books. The review protocol is unregistered and available from the authors on request.
Inclusion/Exclusion Criteria
The review studied the efficacy of interventions for pediatric dog-bite injury prevention. Studies were included if they described empirical research with a focus on cognitive or behavioral interventions to prevent pediatric dog-bite injury for typically developing children anywhere in the range of ages 0–18 years. All types of research design were considered, including randomized controlled trials (RCTs), observational studies using case-control designs, and uncontrolled before–after designs. Studies were excluded if interventions did not include a cognitive or behavioral training component for children, or targeted only parents/caregivers. Also excluded were studies with <10 participants in any treatment arm and studies focused on general animal safety, environmental/policy changes, or dog management. Studies were included from all regions of the world.
Manuscript Inclusion
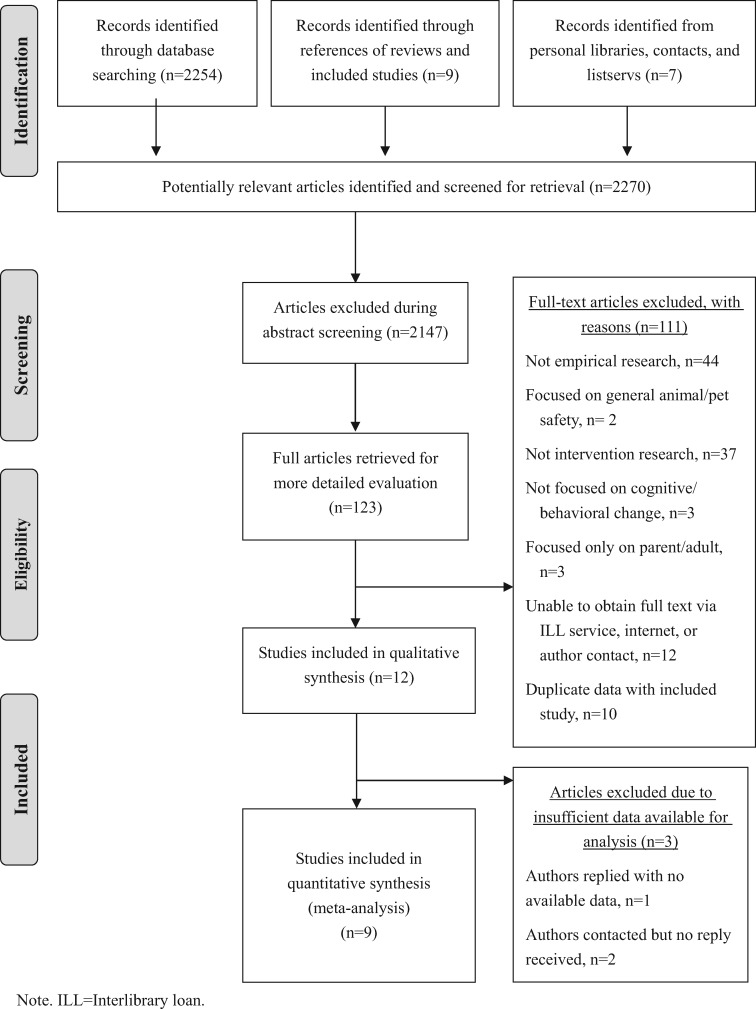
Figure 1 summarizes the steps for manuscript inclusion. First, two authors independently screened 2,270 manuscript abstracts applying the inclusion/exclusion criteria described above. Based on this review, 2,147 manuscripts were excluded. Inter-rater reliability was strong (k > .90) and manuscripts were retained if either reviewer judged that it should be included in the review or if abstracts were determined to provide insufficient information for exclusion. The remaining 123 manuscripts were included for full-text retrieval. Using the same review procedure as used for abstract screening, 12 articles met inclusion criteria for data extraction (see Figure 1 for exclusion reasons of the other 111 articles).
Figure 1.
PRISMA flow diagram of included studies. Note. ILL = interlibrary loan.
Data Extraction and Processing
Data extraction was conducted on the 12 included studies by two researchers using a standardized form, which included data on bibliographic information, country where the study was conducted, demographic information on the sample, description of the intervention, and statistical results for each outcome at each time point and/or each group when applicable. Disagreements were rare and were resolved by discussion between both researchers and a third researcher to reach consensus.
Three of the 12 studies eligible for inclusion lacked sufficient published data required to compute effect sizes of the intervention (Bernardo, Gardner, O’Dair, & Cohen, 2001; Szecsi et al., 2010; Wilson et al., 2003). We communicated with authors of one study (Bernardo et al., 2001), but they did not have data available to share for reanalysis owing to the long period since the study was conducted. The other authors were contacted but were unresponsive. The nine remaining studies were included in the quantitative meta-analysis of intervention effects. Data were entered into Comprehensive Meta-Analysis 3.0 (Biostat, Englewood, NJ) for analysis.
Type of Intervention
The current review included all cognitive/behavioral interventions for preventing pediatric dog-bite injuries. Two researchers reviewed the nine included studies and concurred that the following types of interventions were used: classroom-based in-person instruction with live dogs (Chapman et al., 2000; Coleman, Hall, & Hay, 2008), classroom-based video training (Shen et al., 2015; Spiegel, 2000), a combination of the former two methods (Mello, Getz, Lapidus, Moss, & Soulos, 2006, Study 1), lab-based video training (Lakestani, 2007, Study 4), lab-based computerized program (Meints & de Keuster, 2006, 2009; Morrongiello et al., 2013; Schwebel et al, 2012), and hospital-based video training (Dixon, Pomerantz, Hart, Lindsell, & Mahabee-Gittens, 2013). We reasoned that video interventions are rather unlikely to be highly influenced by the environment in which the video is viewed, so we merged the video interventions into a single category, “video-based intervention,” which was considered along with the other three intervention categories: instruction with live dogs, video plus live dogs, and computer-based intervention.
Types of Outcome Measures
Two researchers systematically reviewed primary outcomes in the 12 studies included in the qualitative synthesis to categorize them. The most common outcome, measured by eight of the nine studies, was children’s knowledge about safety around dogs (Coleman et al., 2008; Dixon et al., 2013; Lakestani, 2007 (Study 4); Meints & de Keuster, 2006, 2009; Mello et al., 2006 (Study 1); Morrongiello et al., 2013; Schwebel et al., 2012; Shen et al., 2015; Spiegel, 2000). Behavioral outcomes emerged as a second commonly used measure of intervention effects. Three studies (Coleman et al., 2008; Schwebel et al., 2012; Shen et al., 2015) measured children’s interactive behaviors with dogs in simulated situations and two (Chapman et al., 2000; Schwebel et al., 2012) measured children’s behaviors with live dogs. Personal consultation with the authors of the study that included both simulated- and live-dog behavioral outcomes (Schwebel et al., 2012) suggested the simulated measure was considered the more valid measure of the study outcomes in terms of construct validity, so it was used in subsequent analysis. Because both simulated and live behaviors with dogs assess similar behavioral constructs, they were merged into a category of “behavioral outcomes.”
Assessment of Risk of Bias
Two levels of bias were considered. Bias at the meta-analysis level was minimized by locating and including all possible studies, both published and unpublished. This was accomplished by searching thesis/dissertation databases and contacting experts in this field to obtain unpublished studies. Biases at the level of individual study were assessed using guidelines provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins & Green, 2011). Given Cochrane guidelines, only controlled studies were included in the assessment of risk of bias (Chapman et al., 2000; Coleman et al., 2008; Lakestani, 2007; Schwebel et al., 2012; Shen et al., 2015); the other studies have indisputable bias by failing to include control groups. Each of the included studies with controls was rated on the following five domains:
Random sequence generation (selection bias): Biased allocation to interventions owing to inadequate generation of a randomized sequence.
Allocation concealment (selection bias): Biased allocation to interventions owing to inadequate concealment of allocations before assignment.
Blinding of outcome assessment: Detection bias owing to knowledge of the allocated interventions by outcome assessors.
Incomplete outcome data: Attrition bias owing to amount, nature or handling of incomplete outcome data.
Selective reporting: Reporting bias owing to selective outcome reporting.
Risks of bias were assessed by the lead author, with two co-authors reviewing all assessment and resolving the discrepancies through discussion. Interrater reliability was high (k > .90).
Quality of Research Assessment
Quality of the included research was assessed using the guidelines proposed by the Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group (Guyatt et al., 2011). Ratings were downgraded based on poor methodological quality, indirect evidence of results, heterogeneity of results (tested with Cochran’s Q and I2), imprecision of results, and risk of publication bias. Cochran’s Q measures the presence of heterogeneity and was calculated as the weighted sum of squared differences between each study effects and the pooled effect across studies (Cochran, 1954). I2 measures the extent of heterogeneity and was calculated as the percentage of variation across studies owing to heterogeneity rather than chance (Higgins & Thompson, 2002). Quality of evidence was upgraded for special considerations such as large magnitude of effect sizes, as recommended by GRADE guidelines. Quality of research ratings were evaluated by the lead author, with two co-authors reviewing all assessments and discrepancies resolved through discussion. Interrater reliability was high (k > .99).
Data Analysis Plan
Data were analyzed in four steps. First, descriptive data from each included study were reviewed. Second, tests of the effect of the interventions were performed for both knowledge (eight studies) and behavioral (four studies) outcomes. The moderating effect of age was examined using meta-regression analysis for both these outcomes. For all outcomes, we computed and aggregated effect sizes using Hedges’s g. Similar to Cohen’s d, Hedges’s g can be interpreted using the following guidelines: small (0.20–0.49), medium (0.50–0.79), and large (≥0.80). An overall effect size was computed respectively for knowledge and behavioral outcomes. The choice of a fixed versus random model in the estimation was based on heterogeneity among the effect sizes of the included studies for each outcome, tested by Q-statistic and I2. If effect sizes were not heterogeneous (Q-statistic nonsignificant and I2 < 50%), a fixed effect model was used to interpret the aggregate effect size. Otherwise, a random effect model was used, and so, bias in estimating confidence intervals caused by errors at the study level could be reduced (Lipsey & Wilson, 2001). All studies were weighted according to sample size. Third, effect sizes for both knowledge and behavioral outcomes were computed by type of intervention. Last, we assessed each included study for risk of bias according to Cochrane guidelines (Higgins & Green, 2011) and for quality of research based on GRADE guidelines (Guyatt et al., 2011).
Results
Descriptive Characteristics of the Included Studies
Following application of inclusion and exclusion criteria, 12 studies were included in the qualitative synthesis, 9 of which were included in the quantitative meta-analysis (see Table I). As shown in Table I, data were collected in five countries (Australia, Canada, China, United Kingdom, United States) and a wide age range of children participated, with the majority either preschool aged (3–5 years) or in middle childhood (ages 7–9 years). Of the 12 included studies, two (17%) used case-control designs, five (42%) were RCTs, and five (42%) used uncontrolled pre–post designs. Two studies (17%) used live dog demonstrations as an intervention, while the rest used videos, software, role-playing, and/or written materials to convey the intervention. Two studies (17%) assessed only behavioral outcomes (e.g., emergency department visits, behaviors toward a live dog), whereas six studies (50%) only assessed knowledge-based outcomes (e.g., pencil and paper test of knowledge). Three studies (25%) assessed both behavioral and knowledge outcomes, and one study (8%) delivered an intervention but did not report outcome data.
Table I.
Descriptive Information on Studies in Qualitative Synthesis (N = 12)
| Author(s), year | Sample (N for full study, mean (SD) and range of age, % male) | Study design | Intervention description | Comparison group | Methodology and procedure | Outcomes | Country |
|---|---|---|---|---|---|---|---|
| Bernardo et al., 2001* | 1,196, 0–19 | Case-control | Pediatric Animal Awareness and Safety Program: Age-appropriate info packet distributed to each participating family | 87 children with dog-bite injuries but did not receive packets | Intervention packets mailed to families in high-risk areas of dog bites. ED visits for dog bites and number of times a dog safety Web site was accessed was assessed after dissemination of packets. | Behavioral: ED visits for dog bites | USA |
| Chapman et al., 2000a | 346, 7–8 | RCT | 30-min lesson by a dog handler with dog. Children practiced with dogs in class. Kit for teacher activities | No-contact control | No baseline data; postintervention behavior assessment after 7–10 days | Behavioral: Number children who patted unfamiliar live dog at school | Australia |
| Coleman et al., 2008a,b | 123, 5-6, 52% | Case-control | Responsible Pet Ownership Program (RPOP): one classroom-based 30-min session lead by RPOP trainer with dog. Facts and canine body language delivered by cartoons, role-play with imaginary/live dog | No-contact control | No baseline data; control group data compared with intervention group at 2 weeks, 2 months, and 4 months | Knowledge: RPOP knowledge scores for each group; behavioral: percentage of correct/incorrect approaches in the task of role play with owner present | Australia |
| Dixon et al., 2013b | 120, 7 (1), 5-9, 55% | Pre–post | 20-min educational video “Dogs, Cats & Kids” at ED, individual delivery | N/A | Convenience sample from ED; baseline knowledge assessment; posttest knowledge immediately following intervention | Knowledge: “Yes” or “no” to 14 scenarios | USA |
| Lakestani, 2007 (Study 4)b | 70, 4.4 | RCT | Two video-based training sessions. Videos included two clips for each of three states: fearful, defensive, and friendly (six clips in total). Instructors train children to correctly recognize dogs’ states in the videos. | Watched video on wild animals | Baseline 2–3 days before intervention; posttest 2–3 days after intervention, follow-up in 9–20 days (median: 14 days) | Knowledge: number of correct answers in recognition tests | UK |
| Meints & de Keuster, 2006, 2009b | N = 102: 3-year-olds: 24, 3.25, 3.17–3.50, 54%; 4-year-olds: 24, 4.17, 4.08–4.75, 46%; 5-year-olds: 24, 5.17, 5.08–5.67, 42%; 6-year-olds: 24, 6.42, 6.08–6.83, 58% | Pre–post | The Blue Dog CD, an interactive multimedia software program to teach safety with dogs; children used CD two to three times/week (half of sample used CD with parents) | N/A | Exposure to the Blue Dog CD and then assessment 1; bring software home and use for 2 weeks, then assessment two with eight items | Knowledge: Computer- based assessment of safety knowledge with animated dog in eight trials | UK |
| Mello et al., 2006 (Study 1)b | 51, 3rd grade | Pre–post | Injury Free of Providence, RI, three class sessions over 4–5 weeks: interaction with pet therapy dog, video on dog behaviors, essay writing | N/A | Baseline test, posttest at completion of training | Knowledge: Pictorial assessment on recognition of safe/unsafe situations | USA |
| Schwebel et al., 2012; Morrongiello et al., 2013a,b | 76, 4.80 (0.92), 3.5–6, 47%c | RCT | The Blue Dog CD (interactive computer software; see above) used at home for varying and unreported length of time | Software on fire safety (Great Escape) | Baseline assessment and posttest about 3 weeks later (M = 20.29 days, SD = 9.81) | Knowledge: Recognition of safe/unsafe dog pictures; behavioral: simulated behavior in a dollhouse | USA, Canada |
| Shen et al., 2015a,b | 280, 10.03 (0.83), 8–12, 49% | RCT | 36-min video of four testimonial stories on dog-bite prevention presented by actors portraying teachers, parents, and grandparents | Testimonial video on drowning risk | Baseline 1 week before intervention; posttest 1 week after intervention |
|
China |
| Spiegel, 2000b | 486, 8.05 (1.17), 5–12, 52% | Pre–post | The BARK (Be Aware, Responsible, and Kind) Dog Bite Prevention Program: written/video materials presented at school for 60 min, class discussion, and role play | N/A |
|
|
USA |
| Szecsi et al., 2010* | 19 kindergarteners | Pre–post | KIDS (Kids Interacting with Dogs Safely) Program: weekly 30-min lesson for 7 weeks; teaching with stuffed animal, role playing, etc. | N/A |
|
N/A | USA |
| Wilson et al., 2003* | 192, 4.68 (0.40), 4.0–5.9, 54.5% | RCT | 30-min class-based Delta DogSafe Program (photos, role-plays, and modeling) by animal management officer; parent package distributed |
|
|
|
Australia |
Note.RCT = randomized controlled trial.
*Not included in the meta-analysis owing to insufficient data in publication or from author contact to compute effect sizes; aIncluded to compute effect sizes of for behavioral outcomes; bIncluded to compute one effect size of intervention for knowledge outcomes; cMorrongiello et al. (2013) used a subset of the sample used in Schwebel et al. (2012), but the samples had comparable demographic traits.
Meta-Analysis Results: Omnibus Effect of Interventions on Outcomes
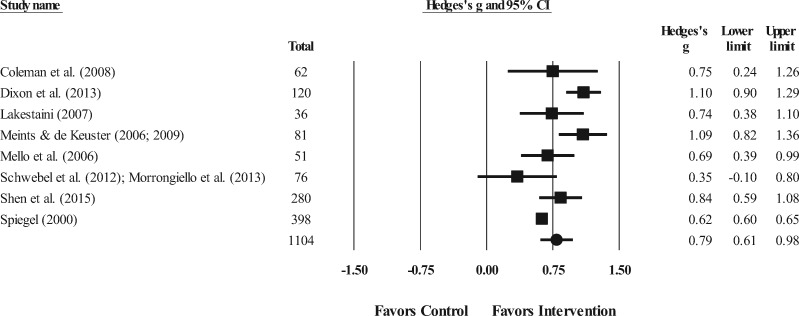
Figure 2 shows the results of meta-analysis on the effect of the cognitive/behavioral interventions on children’s safety knowledge around dogs. Significant heterogeneity existed among the effect sizes of the included studies (Q = 37.06, p < .001, df = 7, I2 = 81.11) so a random-effect model was used to compute the aggregate effect size of intervention on the knowledge outcomes. Measured with Hedges’s g, the results indicated a medium effect (g = 0.79, SE = 0.09, 95% CI = [0.61, 0.98], N = 1,104). This suggests that interventions can exert a significant and medium positive effect on children’s knowledge about safety around dogs. The moderating effect of age on knowledge outcome was not statistically significant, B = −.001, SE = 0.05, 95% CI = [−0.10, 0.09], z = −0.02, p > .05.
Figure 2.
Forest plot of effect sizes and their 95% CI of dog-bite prevention programs on children’s knowledge outcome. Note. The squares representing effect sizes of each study is proprortional to its weight in the meta-analysis. The circle at the bottom of the plot represents the overall effect size in a random-effect model. Participant sample size (“Total”) is less than that shown in Table I owing to data available for meta-analysis.
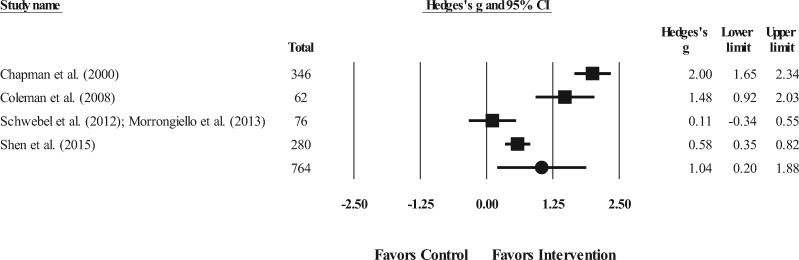
Figure 3 shows the meta-analysis results of the effect of cognitive/behavioral interventions on children’s interactive behaviors with live or simulated dogs. Similar to the cognitive outcome analysis, significant heterogeneity existed among the effect sizes of the four included studies (Q = 61.84, p < .001, df = 3, I2 = 95.15) so a random-effect model was used to compute the aggregate effect size of intervention on the behavioral outcomes. Measured with Hedges’s g, the results indicated a large effect (g = 1.04, SE = 0.43, 95% CI = [0.20, 1.88], N = 764), suggesting that the interventions exerted a significant and large positive effect on children behaviors with dogs in live/simulated environments. The moderating effect of age on behavior outcome was not statistically significant, B = .03, SE = 0.28, 95% CI = [−0.51, 0.57], z = 0.10, p > .05. Table II summarizes the meta-analysis of intervention effects on both outcomes.
Figure 3.
Forest plot of effect sizes and their 95% CI of dog-bite prevention programs on children’s behavioral outcome. Note. The squares representing effect sizes of each study is proprortional to its weight in the meta-analysis. The circle at the bottom of the plot represents the overall effect size in a random-effect model. Participant sample size (“Total”) is less than that shown in Table I owing to data available for meta-analysis.
Table II.
Summary of Findings: Cognitive/Behavioral Interventions to Reduce Pediatric Dog-Bite Injury
| Outcomes | Illustrative probable outcomes (95% CI) |
Number of participantsa (studies) | Quality of the evidence (GRADE) | Notes | |
|---|---|---|---|---|---|
| Control | Intervention | ||||
| Safety knowledge | The mean knowledge change in the intervention groups was 0.79 SDs higher (0.61–0.98 higher) | 1,104 (8 studies) |
|
|
|
| Safe behavior | The mean behavioral change in the intervention groups was 1.04 SDs higher (0.20–1.88 higher) | 764 (4 studies) |
|
|
|
Note. GRADE Working Group grades of evidence:
High quality: Further research is very unlikely to change our confidence in the estimate of effect.
Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low quality: We are very uncertain about the estimate.
aParticipant sample size is less than that shown in Table I owing to data available for meta-analysis.
bQuality of the evidence was downgraded for study design, risk of bias, and indirectness.
cQuality of the evidence was downgraded for study design, risk of bias, and indirectness, and upgraded for large beneficial effect sizes.
Meta-Analysis Results: Intervention Effect by Type of Intervention for Each Outcome
Table III presents meta-analysis results organized by both outcomes and type of intervention. As shown in Table III, four types of interventions (video, instruction with live dogs, video plus live dogs, and computer program) were used to assess the knowledge outcome. Although video-based interventions emerged with the largest effect size (Hedges’s g = 0.82), the four intervention strategies demonstrated comparable medium effect sizes (Hedges’s g ranged from 0.69 to 0.82) in improving children’s safety knowledge around dogs.
Table III.
Summary of Meta-Analytic Results of Cognitive/Behavioral Interventions to Reduce Pediatric Dog-Bite Injury Risk, Separated by Type of Intervention and Outcome
| Type of intervention/outcome | k | Total Na | Hedges’s g | 95% CI | I2 |
|---|---|---|---|---|---|
| Knowledge outcome | |||||
| Video | 4 | 834 | 0.82 | 0.56, 1.08 | 88% |
| Instruction with live dogs | 1 | 62 | 0.75 | 0.24, 1.26 | NA |
| Video + live dogs | 1 | 51 | 0.69 | 0.39, 0.99 | NA |
| Computer program | 2 | 157 | 0.74 | 0.01, 1.47 | 87% |
| Behavioral outcome | |||||
| Video | 1 | 280 | 0.58 | 0.35, 0.82 | NA |
| Instruction with live dogs | 2 | 408 | 1.79 | 1.28, 2.29 | 59% |
| Computer program | 1 | 76 | 0.11 | −0.34, 0.55 | NA |
aParticipant sample size (“Total N”) is less than that shown in Table I owing to data available for meta-analysis.
In contrast, the three types of interventions evaluated with respect to children’s safe behaviors with dogs as an outcome (video, instruction with live dogs, and computer program) varied significantly in their effect sizes. Instruction with live dogs exerted the largest effect on children’s behavioral outcomes (Hedges’s g = 1.79), followed by video-based intervention (g = 0.58) and computer programs (g = 0.11).
Risk of Bias Assessment
Risk of bias for the five controlled studies was assessed (see Supplementary Table 1). One study (20%) demonstrated high risk for random sequence generation (selection bias) and two (40%) had insufficient information to achieve an objective rating. The majority (60%) of studies had insufficient data to be rated on allocation concealment (selection bias) and selective reporting (reporting bias). The highest risk was in the blinding of outcome assessment (detection bias) and incomplete outcome data (attrition bias), with two studies (40%) rated as high risk for each of those criterion.
Quality of Research Assessment
Quality of the research evidence was assessed according to GRADE guidelines (Guyatt et al., 2011) on the two outcomes of interest, safety knowledge and safe behaviors with dogs. As shown in Table II, the quality of evidence for safety knowledge was low, suggesting we must remain uncertain about the effect estimates for this outcome. The evidence for safety knowledge was downgraded owing to the use of non-RCT designs (e.g., uncontrolled pre–post design or case-control designs), potential risk of bias, and indirectness of the measures for pediatric dog-bite injuries. The quality of evidence for safe behaviors was rated as low, suggesting that further research is likely to have an impact on our confidence in the estimate of the effect and is likely to change the estimate. The evidence for safe behaviors was downgraded for the use of non-RCT designs, potential risk of bias, and indirectness of the measures for pediatric dog-bite injuries, but was upgraded for the overall large magnitude of beneficial effect sizes.
Discussion
This article conducted a systematic review and meta-analysis on the efficacy of cognitive/behavioral interventions to prevent pediatric dog-bite injuries. The results showed that cognitive/behavioral interventions were at least moderately effective in reducing dog-bite risk among children. Although this finding is consistent with the previous systematic review on pediatric dog-bite injury preventions (Duperrex et al., 2009), the quantitative analyses should be viewed as tentative rather than conclusive findings owing to the low quality of included studies.
A medium effect size was detected for cognitive/behavioral interventions to improve children’s safety knowledge around dogs. Assessment of children’s knowledge is an objective, accessible, and convenient method to evaluate the efficacy of a pediatric injury intervention program, and 9 of the 12 studies included in Table I incorporated a knowledge-based outcome into their research design. However, this finding should be interpreted with caution owing to the quality of evidence. As shown in Table II, the quality of the studies included in computing the aggregate effect size of safety knowledge was negatively affected by the use of non-RCT designs and by potential risk of bias (e.g., detection bias owing to the noncompliance of blinding outcome assessors). For the purpose of dog-bite injury reduction, the knowledge outcome also suffers from its indirect association to actual child–dog interactions or dog-bite rates (Schwebel et al., 2012).
We also examined children’s behavior with simulated or live dogs as an outcome. A relatively large effect size was detected for this outcome, suggesting the cognitive/behavioral interventions were successful in promoting children’s safe behaviors with dogs. Although none of the studies included in computing the aggregate effect size of behavioral outcome assessed actual dog-bite incidents in their sample (one study, Bernardo et al., 2001, included dog-bite incidents in their outcomes but lacked adequate data to be included in the quantitative analysis), interactive behaviors between children and live or simulated dogs provided researchers with direct insight into the potential efficacy of a dog-bite prevention program, and the results were promising.
The result that we had a larger effect size for behavioral outcomes than for knowledge-based outcomes is intriguing, and contrary to what is generally reported in the health behavior change literature (e.g., Schwebel et al., 2012). One explanation may relate to the quality of the evidence. Studies incorporating behavioral outcomes were generally more rigorous and therefore may have assessed outcomes with greater validity. They may also have tested higher-quality interventions if one assumes that more rigorous science is associated with higher-quality interventions. Another possible explanation is that knowledge about dogs is hard to teach young children, but that behavioral habits can be altered with appropriate behavior-based interventions. A third possibility is that behavioral outcomes tended to be evaluated on slightly older children than knowledge-based outcomes. However, the moderating effect of age was not significant for either the knowledge or the behavior outcome, suggesting that there are no statistically significant differences in the effect of the interventions on knowledge or behavior across different age-groups.
Like many meta-analytic reviews on pediatric psychology topics (e.g., Birnie et al., 2014; Eccleston et al., 2014; Lukens & Silverman, 2014; Palermo, Eccleston, Lewandowski, Williams, & Morley, 2010; Robinson, Kaizar, Catroppa, Godfrey, & Yeates, 2014), we discovered low quality of evidence in the field of pediatric dog-bite injury prevention. The fact that this level of quality of evidence spans much of the field may reflect the comparatively young status of the field of pediatric psychology, and reinforces the need for continued effort to use rigorous scientific design to study translational interventions in the field of child dog-bite prevention in particular, and the domains of child injury prevention and pediatric psychology more generally.
Effect by Type of Intervention and Implications for Practice
Effective interventions for pediatric dog-bite prevention are likely to be multifaceted. Animal behavior training and animal control strategies could probably reduce dog bite incidents in many regions of the world (Clarke & Fraser, 2013; Hou, Jin, & Ruan, 2012). Environment modifications are also needed (Raghavan, Martens, Chateau, & Burchill, 2013; World Health Organization, 2013), and may occur both at the household level (e.g., proper dog fencing/restriction; use of baby gates to separate toddlers from animals) and the community level (e.g., policy-making and enforcement of leash laws, spay/neuter policies). But environmental modifications are unlikely to be universally successful and must be combined with behavioral interventions targeting both children and the adults who supervise them to achieve optimal levels of dog-bite injury prevention. Our present focus, on interventions to improve children’s behavior near dogs, suggests cognitive/behavioral interventions can improve children’s safety near dogs.
One type of intervention we evaluated was videos. Videos offer tremendous capability to condense and deliver large amount of information in an engaging manner to large groups of children simultaneously. However, the present study found that video education was most effective in improving children’s knowledge about dog-bite risk and prevention (g = 0.82), not their behavior with dogs (g = 0.58). This may be partially because most educational videos used to teach children about dog-bite prevention focus primarily on imparting safety facts and rules. They do not include components that health behavior change theory might suggest would lead to behavior change. The Health Belief Model (Janz & Becker, 1984), for example, suggests behavior change may occur if children’s perceived vulnerability to dog bites is altered through emotional immersion into potential risk. Videos that deliver such messages, for example, through persuasive and emotional-arousing content, may result in the desired behavior change (Shen et al., 2015).
An alternative strategy that did prove more successful across studies was to use creative classroom-based curriculum programming such as educational lessons with live dogs (g = 1.79 in the present review; Chapman et al., 2000; Coleman et al., 2008). Live interaction and experience has been demonstrated effective in other domains of health interventions (e.g., nutrition; Faccio et al., 2013). Of course, a challenge to broad dissemination of behavior change strategies such as instruction with live dogs is the cost to implement it. Computerized immersion simulations such as virtual reality offer a promising direction for future intervention development and have been demonstrated to be successful in other domains of child injury prevention (e.g., Schwebel, McClure, & Severson, 2014) and health (e.g., Jeffs et al., 2014).
Pediatric Dog-Bite Prevention: An Understudied Global Challenge
Of the 12 studies included in our qualitative synthesis, 11 were conducted in developed countries (Australia, Canada, United States, United Kingdom) over the past 15 years and just one study was conducted in the middle- and low-income regions of the world (China) where risk of pediatric dog-bite injury is significantly higher owing to the differences in dog management laws and systems (Georges & Adesiyun, 2008; Shen et al., 2013; Si et al., 2008). Heightened risk of pediatric dog-bite injury in developing regions arises from a variety of cultural and environmental factors, including the prevalence of stray dogs, lack of rabies vaccines, and inadequate adult supervision (Duan, 2008; Shen, Li, Xiang, Lu, & Schwebel, 2014; Totton et al., 2010).
Future research should consider what aspects of dog bite prevention in Western countries can be adapted to developing country cultures, and what aspects require modification or reinvention to promote safe behaviors and reduce dog-bite injury among children living in lower-income nations. As an example, children across all countries and cultures share similar psychosocial and cognitive developmental trajectories in information processing and behavioral modeling. Thus, it is logical to translate intervention strategies developed in Western countries that rely on training grounded in those developmental trajectories (e.g., age-appropriate video education to teach knowledge about basic rules for safety; use of education with live dogs to model appropriate behavior and promote behavior change) in lower-income nations. However, content of many interventions may need modification or reinvention because interventions developed in Western countries focus primarily on the prevention of dog-bite injuries from pet dogs in the home. In low- and middle-income countries, the environmental context is different. Dog-bite risk is often not from pet dogs, but rather from stray or loose dogs in the community. Interventions and their components that work in high-income countries may need adaptation or reinvention for use with children in the context of lower-income countries.
Limitations
The present study has limitations. First, our focus as pediatric psychologists was on cognitive/behavioral interventions. We excluded potentially effective interventions aiming to change environmental factors such as laws and policies regarding dog management (e.g., Klaassen et al., 1996). In doing so, we recognize that in some contexts, environmental changes might be more efficient in reducing dog-bite injuries than child education. For example, in developing countries where stray dogs are prevalent, a good dog management system that eliminates stray dogs in public places might exert more direct and immediate effect in the reduction of child dog-bite injuries than any cognitive/behavioral program. Also excluded from our analysis were interventions deisgned only for rabies reduction (e.g., Lapiz et al., 2012) or general animal/pet safety (e.g., Muris, Bodden, Merckelbach, Ollendick, & King, 2003). Thus, our analysis should not be viewed as comprehenisve but rather one focused on cognitive/behavioral programs targeting children and dog-bite prevention.
Second, owing to the limited number of available studies in the literature, only two outcomes (knowledge and behavior) were analyzed and we did not distinguish between interactive behavior with live dogs versus simulated dogs. Third, we were unable to include interventions known to be implemented but not reported adequately (or at all) in the literature. We excluded a few published articles, as well as interventions documented on the Internet to be in practice but not studied empirically. Within the included interventions, the quality of methodology varied across studies and therefore caution is required in interpreting the quantitative results. Fourth, to provide a comprehensive picture of pediatric dog-bite prevention programs, we aggregated effects from a variety of study designs including both RCT and non-RCT (pre–post, case control). Future interventionists should adopt RCT designs so intervention efficacy can be evaluated more rigorously. Finally, because few studies incorporated multiple or long-term follow-up evaluations, we were unable to evaluate the long-term effect of cognitive/behavioral interventions.
Conclusions
The present study reviewed and analyzed the efficacy of cognitive/behavioral interventions to reduce pediatric dog-bite injury. The results showed that interventions have a moderate effect on improving children’s safety knowledge around dogs and a relatively large effect on promoting safe interactions between children and dogs. Video-based interventions were most effective in the improvement of safety knowledge, while instruction with live dogs was most effective in increasing children’s safe behaviors with dogs. Future interventions should include actual dog-bite rates as an outcome, incorporate long-term follow-up evaluations, and use rigorous RCTs to evaluate the intervention programs. They also should adopt an international perspective to reduce pediatric dog-bite risk globally, with particular attention to high-risk environments in low- and middle-income countries.
Supplementary Data
Supplementary data can be found at: http://www.jpepsy.oxfordjournals.org/.
Funding
This study was partially supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under Award Number R21HD075960. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Health.
Conflicts of interest: None declared.
Supplementary Material
References
- Beaver B. V. (2001). A community approach to dog bite prevention. Journal of the American Veterinary Medical Association , 218, 1732–1749. [DOI] [PubMed] [Google Scholar]
- Bernardo L. M., Gardner M. J., O'Dair J., Cohen B. (2001). The PAWS program: Pediatric animal awareness and safety. Journal of Emergency Nursing, 274, 387–390. [DOI] [PubMed] [Google Scholar]
- Bernardo L. M., Gardener M. J., Rosenfield R. L., Cohen B., Pitetti R. (2002). A comparison of dog bite injuries in younger and older children treated in a pediatric emergency department. Pediatric Emergency Care , 18, 247–249. [DOI] [PubMed] [Google Scholar]
- Birnie K. A., Noel M., Parker J. A., Chambers C. T., Uman L. S., Kisely S. R., McGrath P. J. (2014). Systematic review and meta-analysis of distraction and hypnosis for needle-related pain and distress in children and adolescents. Journal of Pediatric Psychology, 39, 783–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman S., Cornwall J., Righetti J., Sung L. (2000). Preventing dog bites in children: randomised controlled trial of an educational intervention. BMJ: British Medical Journal , 320, 1512–1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chouinard M. M. (2007). Children's questions about animals. Monographs of the Society for Research in Child Development , 72, 58–82. [DOI] [PubMed] [Google Scholar]
- Clarke N. M., Fraser D. (2013). Animal control measures and their relationship to the reported incidence of dog bites in urban Canadian municipalities. The Canadian Veterinary Journal, 54, 145–149. [PMC free article] [PubMed] [Google Scholar]
- Cleaveland S., Kaare M., Tiringa P., Mlengeya T., Barrat J. (2003). A dog rabies vaccination campaign in rural Africa: impact on the incidence of dog rabies and human dog-bite injuries. Vaccine , 21, 1965–1973. [DOI] [PubMed] [Google Scholar]
- Cochran W. G. (1954). The combination of estimates from different experiments. Biometrics , 10, 101–129. [Google Scholar]
- Coleman G. J., Hall M. J., Hay M. J. (2008). An evaluation of a pet ownership education program for school children. Anthrozoös, 21, 271–284. [Google Scholar]
- Dixon C. A., Pomerantz W. J., Hart K. W., Lindsell C. J., Mahabee-Gittens E. M. (2013). An evaluation of a dog bite prevention intervention in the pediatric emergency department. Journal of Trauma and Acute Care Surgery, 75, S308–S312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan B. (2008). Mo hu shi nong cun gou huan [Do not neglect the danger of dogs in rural areas] (in Chinese). Henan Science and Technology , 4, 44. [Google Scholar]
- Duperrex O., Blackhall K., Burri M., Jeannot E. (2009). Education of children and adolescents for the prevention of dog bite injuries. Cochrane Database Systematic Review , 2, CD004726. [DOI] [PubMed] [Google Scholar]
- Eccleston C., Palermo T. M., Williams A. C. D. C., Lewandowski Holley A., Morley S., Fisher E., Law E. (2014). Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database of Systematic Reviews, Issue 5. Art. No.: CD003968. doi: 10.1002/14651858.CD003968.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faccio E., Costa N., Losasso C., Cappa V., Mantovani C., Cibin V., Andrighetto I., Ricci A. (2013). What programs work to promote health for children? Exploring beliefs on microorganisms and on food safety control behavior in primary schools. Food Control, 33, 320–329. [Google Scholar]
- Georges K., Adesiyun A. (2008). An investigation into the prevalence of dog bites to primary school children in Trinidad. BMC Public Health , 81, 85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt G., Oxman A. D., Akl E. A., Kunz R., Vist G., Brozek J., Norris S., Falck-Ytter Y., Glasziou P., DeBeer H., Jaeschke R., Rind D., Meerpohl J., Dahm P., Schünemann H. J. (2011). GRADE guidelines: 1. Introduction – Grade evidence profiles and summary of findings tables . Journal of Clinical Epidemiology , 64, 383–394. [DOI] [PubMed] [Google Scholar]
- Higgins J. P. T., Green S. (Eds.) (2011). Cochrane handbook for systematic reviews of interventions, version 5.1.0. The Cochrane Collaboration. Retrieved from www.cochrane-handbook.org [Google Scholar]
- Higgins J. P. T., Thompson S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine , 21, 1539–1558. [DOI] [PubMed] [Google Scholar]
- Hon K. E., Fu C. A., Chor C., Tang P. H., Leung T., Man C. Y., Ng P. (2007). Issues associated with dog bite injuries in children and adolescents assessed at the emergency department. Pediatric Emergency Care , 23, 445–449. [DOI] [PubMed] [Google Scholar]
- Hopkins S., Schubert T., Hart B. (1976). Castration of adult male dogs: Effects on roaming, aggression, urine marking, and mounting. Journal of the American Veterinary Medical Association , 168, 1108. [PubMed] [Google Scholar]
- Hou Q., Jin Z., Ruan S. (2012). Dynamics of rabies epidemics and the impact of control efforts in Guangdong Province, China. Journal of Theoretical Biology, 300, 39–47. [DOI] [PubMed] [Google Scholar]
- Janz N. K., Becker M. H. (1984). The health belief model: A decade later. Health Education & Behavior, 111, 1–47. [DOI] [PubMed] [Google Scholar]
- Jeffs D., Dorman D., Brown S., Files A., Graves T., Kirk E., Meredith-Neve S., Sanders J., White B., Swearingen C. J. (2014). Effect of virtual reality on adolescent pain during burn wound care. Journal of Burn Care & Research, 35, 395–408. [DOI] [PubMed] [Google Scholar]
- Klaassen B., Buckley J. R., Esmail A. (1996). Does the dangerous dogs act protect against animal attacks: a prospective study of mammalian bites in the accident and emergency department. Injury, 27, 89–91. [DOI] [PubMed] [Google Scholar]
- Lakestani N. N. (2007). A study of dog bites and their prevention (Unpublished doctoral dissertation). University of Edinburgh, United Kingdom. [Google Scholar]
- Lapiz S. M. D., Miranda M. E. G., Garcia R. G., Daguro L. I., Paman M. D., Madrinan F. P., Rances P. A., Briggs D. J. (2012). Implementation of an intersectoral program to eliminate human and canine rabies: The Bohol Rabies Prevention and Elimination Project. PLoS Neglected Tropical Diseases, 6, e1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsey M. W., Wilson D. B. (2001). Practical metaanalysis. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Lukens C. T., Silverman A. H (2014). Systematic review of psychological interventions for pediatric feeding problems. Journal of Pediatric Psychology, 39, 903–917. [DOI] [PubMed] [Google Scholar]
- Mcheik J. N., Vergnes P., Bondonny J. M. (2000). Treatment of facial dog bite injuries in children: A retrospective study. Journal of Pediatric Surgery , 35, 580–583. [DOI] [PubMed] [Google Scholar]
- Meints K., De Keuster T. (2006). Test Yourself–A First Assessment of the Dog Bite Prevention Project” Blue Dog". Part I: Education–The” Blue Dog” is Born; Part II: The” Blue Dog"–Do Children Really Get the Message? Retreived from http://www.vin.com/apputil/content/defaultadv1.aspx?meta=Generic&pId=11223&id=3859304 [Google Scholar]
- Meints K., De Keuster T. (2009). Don’t kiss a sleeping dog: The first assessment of “the blue dog” bite prevention program. Journal of Pediatric Psychology , 34, 1084–1090. [DOI] [PubMed] [Google Scholar]
- Mello M. J., Getz M. A., Lapidus G., Moss J., Soulos P. (2006). Innovations in injury prevention education. Journal of Trauma and Acute Care Surgery, 63, S7–S9. [DOI] [PubMed] [Google Scholar]
- Morrongiello B. A., Schwebel D. C., Stewart J., Bell M., Davis A. L., Corbett M. R. (2013). Examining parents’ behaviors and supervision of their children in the presence of an unfamiliar dog: Does The Blue Dog intervention improve parent practices?. Accident Analysis and Prevention, 54, 108–113. [DOI] [PubMed] [Google Scholar]
- Muris P., Bodden D., Merckelbach H., Ollendick T. H., King N. (2003). Fear of the beast: A prospective study on the effects of negative information on childhood fear. Behaviour Research and Therapy, 41, 195–208. [DOI] [PubMed] [Google Scholar]
- National Center for Injury Prevention and Control. (2015). WISQARSTM (Web-based Injury Statistics Query and Reporting System). Retrieved from http://www.cdc.gov/injury/wisqars/. Retrieved 7 July 2015. [Google Scholar]
- Overall K. L., Love M. (2001). Dog bites to humans-demography, epidemiology, injury, and risk. Journal of the American Veterinary Medical Association , 218, 1923–1934. [DOI] [PubMed] [Google Scholar]
- Palermo T. M., Eccleston C., Lewandowski A. S., Williams A. C. D. C., Morley S. (2010). Randomized controlled trials of psychological therapies for management of chronic pain in children and adolescents: An updated meta-analytic review. PAIN, 148, 387–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raghavan M., Martens P. J., Chateau D., Burchill C. (2013). Effectiveness of breed-specific legislation in decreasing the incidence of dog-bite injury hospitalisations in people in the Canadian province of Manitoba. Injury Prevention, 19, 177–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson K. E., Kaizar E., Catroppa C., Godfrey C., Yeates K. O. (2014). Systematic review and meta-analysis of cognitive interventions for children with central nervous system disorders and neurodevelopmental disorders. Journal of Pediatric Psychology, 398, 846–865. [DOI] [PubMed] [Google Scholar]
- Schwebel D. C., McClure L. A., Severson J. (2014). Teaching children to cross streets safely: A randomized, controlled trial. Health Psychology, 337, 628–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwebel D. C., Morrongiello B. A., Davis A. L., Stewart J., Bell M. (2012). The Blue Dog: Evaluation of an interactive software program to teach young children how to interact safely with dogs. Journal of Pediatric Psychology , 373, 272–281. [DOI] [PubMed] [Google Scholar]
- Shen J., Li S., Xiang H., Lu S., Schwebel D. C. (2014). Antecedents and consequences of pediatric dog-bite injuries and their developmental trends: 101 cases in rural China. Accident Analysis and Prevention, 63, 22–29. [DOI] [PubMed] [Google Scholar]
- Shen J., Li S., Xiang H., Pang S., Xu G., Schwebel D. C. (2013). A Multi-Site Study on Knowledge, Attitudes, Beliefs and Practice of Child-Dog Interactions in Rural China. International Journal of Environmental Research and Public Health , 103, 950–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen J., Pang S., Schwebel D. C. (2015). A randomized trial evaluating child dog-bite prevention in rural China through video-based testimonials Health Psychology. Online first publication. doi: 10.1037/hea0000273, http://www.ncbi.nlm.nih.gov/pubmed/26523353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Si H., Guo Z., Hao Y., Liu Y., Zhang D., Rao S., Lu J. (2008). Rabies trend in China (1990–2007) and post-exposure prophylaxis in the Guangdong province. BMC Infectious Diseases , 8, 113–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel I. B. (2000). A pilot study to evaluate an elementary school-based dog bite prevention program. Anthrozoös, 13, 164–173. [Google Scholar]
- Szecsi T., Barbero M., Del Campo A., Toledo M. (2010). Teaching strategies: Teaching respect, responsibility, and kindness through dog safety lessons. Childhood Education, 87, 125–128. [Google Scholar]
- Totton S. C., Wandeler A. I., Zinsstag J., Bauch C. T., Ribble C. S., Rosatte R. C., McEwen S. A. (2010). Stray dog population demographics in Jodhpur, India following a population control/rabies vaccination program. Preventive Veterinary Medicine , 97, 51–57. [DOI] [PubMed] [Google Scholar]
- Wilson F., Dwyer F., Bennett P. C. (2003). Prevention of dog bites: Evaluation of a brief educational intervention program for preschool children. Journal of Community Psychology , 31, 75–86. [Google Scholar]
- World Health Organization. (2013). WHO expert consultation on rabies. Second report. World Health Organization Technical Report Series , 982, 1–139. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.