Abstract
Objectives
Depression, a chronic and disabling condition, frequently has its first onset during adolescence, underscoring the value of early effective treatment and prevention. Integrated medical-behavioral health care provides one strategy for improving treatment access for adolescents and young adults (AYA).
Methods
This study examined predictors of accessing treatment in a multisite randomized controlled trial evaluating an integrated collaborative care intervention aimed at improving access to evidence-based depression treatment through primary health care, compared with usual care.
Results
The integrated care intervention was able to overcome barriers to care associated with an initial reluctance to pursue active treatment and older age. Service use was low in both conditions among less acculturated/non-English-speaking families.
Conclusions
Results support the value of integrated medical-behavioral health care for improving rates of care. Findings highlight mechanisms by which integrated care may lead to improved rates of care and outcomes for AYA, an underserved and understudied group.
Keywords: adolescents, depression, primary care
Depression is prevalent among young people, estimated to affect between 15 and 20% of youths by age 18 (Lewinsohn, 2002). It has been recognized as a chronic, reoccurring condition that frequently first occurs during adolescence (Andrews, 2001). In naturalistic prospective studies of the course of depression, 10–20% of individuals who experience a major depressive episode go on to have chronic symptoms (Keller etal., 2013). A common course-related feature of chronic depression is age of onset. There appears to be an association between earlier age of onset and more lifetime depressive episodes, as well as other adverse outcomes such as greater long-term impairment, increased likelihood of psychiatric comorbidity, and disrupted transition into adulthood (Copeland, Wolke, Shanahan, & Costello, 2015). Despite the association of early-onset depression with a reoccurring and more pernicious trajectory of symptoms, roughly 40% of American youths with depressive disorders receive no treatment of any kind and 66% receive no mental health treatment or specific treatment for depression (Avenevoli, Swendsen, He, Burstein, & Merikangas, 2015).
In pediatric psychology, one approach to addressing health and behavioral health disparities, such as barriers to treatment engagement among young people with depression, is to improve access to mental health services through integration of mental health services within general primary care (Ader etal., 2015; Asarnow, Rozenman, Wiblin, & Zeltzer, 2015a; Asarnow, Kolko, Miranda, & Kazak, 2017; Kolko & Perrin, 2014; Stancin, Perrin, & Ramirez, 2009). This approach of improving access to behavioral health care through primary care has been emphasized in the current redesign of primary care as one strategy for achieving the triple aim of improving population health and patient experience of care while reducing costs (Ader etal., 2015). Integrated primary medical and behavioral health care, defined as the inclusion of behavioral health services as part of primary care using tightly integrated on-site teamwork (Heath, Wise, & Reynolds, 2013; McDaniel etal., 2014), represents an important opportunity to link young people to behavioral health care services (Asarnow, Kolko, Miranda, & Kazak, 2017; Asarnow etal., 2015a; Irwin, 2010; Kolko & Perrin, 2014; Stancin & Perrin, 2014; Weersing, 2010). Primary care is highly accessible in the United States, with approximately 90% of youth reporting contact with a primary care provider each year (Chevarley, 2003). However, most pediatricians do not feel comfortable assessing and providing treatment support for the majority of mental health conditions (Stein etal., 2008), highlighting the importance of improving access to mental health providers and/or consultation through primary care.
Given that the first onset of depression frequently occurs during adolescence, adolescence offers a critical period for intervention. As adolescents grow older and face new challenges and changes in how services are received (Callahan & Cooper, 2010; Fortuna, Robbins, & Halterman, 2009; Nicholson etal., 2009), promoting positive health behaviors such as fostering a sense of responsibility for one’s own care and establishing relationships with providers early on can meaningfully influence well-being and functioning during the transition to adulthood and beyond (Irwin, 2010).
Although data for pediatric and emerging adult populations are limited relative to data on adults, there is support for integrating primary medical and mental health care for adolescents and young adults (AYA). Findings from the field indicate higher rates of care for mental health problems when that care is integrated with and/or co-located within primary care services (Kolko & Perrin, 2014; Stancin & Perrin, 2014), and that integrated primary medical-behavioral health care leads to improved behavioral health outcomes for children and adolescents (for review, Asarnow etal., 2015a). Thus, integrated primary medical-behavioral care is a promising service delivery strategy for AYA with behavioral health problems, particularly racial/ethnic minority individuals who often face mental health disparities that hinder adequate treatment of depression symptoms (Elster etal., 2003), including difficulties engaging with needed services. For example, findings from epidemiological and other studies show that adults with limited English proficiency in the United States often do not seek out or obtain mental health services (Alegría etal., 2007; Sentell, Shumway, & Snowden, 2007; Weech-Maldonado etal., 2003), pointing to the importance of English-language comfort/dominance as a factor influencing service use. Further, Latino youth who are immigrants or are born to immigrant parents face difficulties that may contribute to having less access to care including higher rates of poverty (Fix, Zimmermann, & Passel, 2001; Hernandez, 2004), less likelihood of having insurance (Kaiser Commission on Medicaid and the Uninsured, 2000), and linguistic barriers to communication with service providers (Lessard & Ku, 2003). Integrated care interventions have been found to be effective in overcoming such barriers and are a potential mechanism for reducing mental health disparities (McGuire & Miranda, 2008; Miranda etal., 2003). However, within this service model, there remains a need to understand: (1) which barriers to treatment an integrated care model can effectively address, (2) what barriers to treatment require additional innovative approaches, and (3) the factors that facilitate and inhibit initiation of service use. The Youth Partners in Care (YPIC) trial (Asarnow etal., 2009; Asarnow etal., 2005) offers a unique opportunity to address these questions.
The YPIC trial was the first and largest randomized effectiveness trial to evaluate a quality improvement (QI) intervention that improved access to evidence-based depression care for AYA (ages 13–21 years) using a collaborative care model that integrated evidence-based depression care within primary care clinics (Asarnow etal., 2005). Collaborative care is an overarching term that refers to treatment guided by a treatment plan developed in collaboration with behavioral health and primary care clinicians, patients, and families (McDaniel etal., 2014). Recent data support the utility of the collaborative care model in addressing mental health problems among youth samples (for review, Asarnow etal., 2015a).
The QI intervention aimed to improve use of evidence-based treatments, reduce depression, and increase satisfaction with services. This was achieved by incorporating the following elements at each site: expert team leaders to adapt the intervention for the individual site; care managers who provided support for primary care physicians in assessment and management of participant’s depression; training in evidence-based depression treatment (primarily cognitive behavioral therapy [CBT] and antidepressant medications) for care managers; and allowing participants and clinicians to select their preferred treatment modality. Results from the YPIC study showed that the integrated care intervention compared with usual primary care enhanced by provider education about depression evaluation and treatment led to reduced depression, lower rates of severe depression, and improvements in quality of life and satisfaction with care (Asarnow etal. 2005; Asarnow etal., 2009). Moreover, rates of severe depression were significantly lower (10.9% vs. 45.2%, a 34% difference) among AYA receiving roughly guideline concordant care, defined as six or more psychotherapy visits or antidepressant medication use as determined by medication treatment algorithms (Wells, Tang, Carlson, & Asarnow, 2012). In particular, minority AYA appeared to benefit from enrollment in the QI condition. Black youth showed large reductions in depression symptoms and higher rates of continued service use at follow-up compared with other racial/ethnic groups of youth, and Latino youth reported greater satisfaction with care (Ngo etal., 2009).
Despite these promising results, a disappointment in the YPIC trial was that even with enhanced resources for integrated primary medical-behavioral health care, rates of treatment received were low (32% in the intervention group vs. 17% in controls). These findings underscore the necessity of better understanding the needs of AYA experiencing depression, as well as differential patterns of service use for depression across subgroups of AYA. Given that unfavorable health-related habits established at a young age (such as poor health care utilization) can persist into adulthood and diminish outcomes (Wysocki, Hough, Ward, & Green, 1992), facilitating early linkage to appropriate care serves the ultimate goal of mitigating long-term risk.
According to the Behavioral Model of Health Service Use (Anderson, 1995), factors that inhibit and/or promote service use are varied and can be categorized as predisposing (e.g., demographic characteristics and attitudes), enabling (e.g., logistical and structural variables such as income, insurance, childcare, transportation, resource availability), and need factors (e.g., severity level, impairment). In the literature, lower treatment rates have been found among ethnic minority populations (Avenevoli etal., 2015) and in less acculturated families (Brach, Fraser, & Paez, 2005; Weech-Maldonado etal., 2003). We also see this pattern for patients with lower need, as evidenced by fewer depressive symptoms (Avenevoli etal., 2015), fewer comorbid mental health conditions (Sourander, Helstela, Ristkari, Helenius, & Phia, 2001), and absence of a comorbid physical disorder (Richardson, Russo, Lozano, McCauley, & Katon, 2008). Systematic reviews of the literature concerning service use among a variety of populations, including primary care patients and individuals with depression, support these findings (Clement etal., 2015).
While we expect to see similar patterns of association in the present investigation as seen in the literature, analyses within the YPIC sample provide unique opportunities to address some understudied issues. First, comparisons across the QI and usual care (UC) conditions allow examination of the degree to which the QI intervention is able to overcome barriers to accessing care. Second, the sample includes AYA, an understudied age-group that experiences unique developmental changes and challenges and demonstrates low rates of care (Lansing & Berg, 2014; Park, Scott, Adams, Brindis, & Irwin, 2014). Third, the YPIC sample includes a relatively large number of racial/ethnic minority participants, predominately composed of Latino AYA, providing an opportunity to evaluate predictors of service use in a sample with a large proportion of minority AYA.
In regards to development, we hypothesize that younger age (corresponding with greater parental involvement/responsibility for care; Wysocki etal., 2009) and satisfaction with health care (which can be influenced by changes in availability of resources and provider relationships that might occur in response to “aging out” of certain programs; Nicholson etal., 2009) will predict a greater likelihood of service use. In regards to culture, having a parent who is an immigrant, speaking a language other than English at home, and viewing depression as stigmatizing (which has been shown to be culturally influenced; Turner, Jensen-Doss, & Heffer, 2015) are hypothesized to predict less service use. Research supports that the mechanisms by which the QI intervention facilitates care improves treatment uptake among underserved AYA (Lieberman, Adalist-Estrin, Erinle, & Sloan, 2006). Thus, we expect barriers that are pertinent to AYA and racial/ethnic minority individuals to be mitigated by the QI intervention, as evidenced by statistical interaction between predictor variables and intervention condition.
Method
This study involves secondary analyses of data from the YPIC trial. Patient assent and parent consent were required for participants aged <18 years, and patient consent was required for those >18 years. Institutional review boards of all participating organizations approved the study. As detailed descriptions of methods are available elsewhere, we provide an overview here emphasizing methods relevant to the aims of this study (for additional information, see Asarnow etal., 2005, 2009).
Participants
Participants were drawn from patients attending six primary health care sites affiliated with five diverse health care organizations purposely selected to include managed care, public sector, and academic medical centers. Study eligibility was determined by in-clinic screenings using brief questionnaires completed by consecutive patients during primary care visits. AYA were eligible for inclusion if: (1) the participant endorsed screening items assessing presence of major depression or dysthymia in the past month from the 12-month Composite International Diagnostic Interview (CIDI-12) (World Health Organization, 1997) modified slightly to conform to diagnostic criteria for adolescents, in addition to a total Center for Epidemiological Studies-Depression Scale (CES-D) (Radloff, 1977) score ≥ 16, or (2) CES-D score ≥ 24. Exclusion criteria were minimal and designed to include most clinic patients. They included: (1) medical provider not in study, (2) sibling already enrolled in study, (3) youth not English speaking, and (4) parent not English or Spanish speaking. Approximately 36% of the AYA approached for screening were found to be ineligible, 4.4% of which were excluded owing to the youth’s lack of English language proficiency. Other primary reasons that AYA were found to be ineligible for screening were that: (1) youth had already been screened (n = 696), (2) primary care provider not in study (n = 652), (3) youth was outside the eligible age range (n = 588), and (4) a sibling was enrolled in the study (n = 25).
The YPIC sample included 418 AYA who completed baseline (i.e., pretreatment) assessments and were subsequently randomly assigned to the QI intervention or enhanced UC. Randomization was implemented using a computerized random number generator, stratified by site and by provider within site, with assignments concealed from assessment staff. Because the primary focus of this study was on whether youths initiated treatment during the intervention period, outcomes for the present study were assessed at 6 months postintervention time point. This visit was completed by 344 AYA (82%) with no significant difference in completion by intervention condition.
The sample was predominately female (78%), with 87% reporting belonging to a racial/ethnic minority group (see Table I). Over half of the sample spoke a language other than English at home (64.3%), of which 89.6% were Spanish speakers.
Table I.
Demographic Characteristics of the Study Sample
| Characteristic | No. (%) |
||
|---|---|---|---|
| Total (N=418) | Quality improvement (n=211) | Usual care (n=207) | |
| Female | 326 (78.0) | 166 (78.7) | 160 (77.3) |
| Age, mean (SD) | 17.2 (2.1) | 17.3 (2.1) | 17.1 (2.1) |
| Race/ethnicity | |||
| Black | 56 (13.4) | 29 (13.7) | 27 (13.0) |
| Hispanic/Latino | 234 (56.0) | 121 (57.4) | 113 (54.6) |
| Mixed | 57 (13.6) | 27 (12.8) | 30 (14.5) |
| White | 53 (12.7) | 23 (10.9) | 30 (14.5) |
| Other | 13 (3.1) | 7 (3.3) | 6 (2.9) |
| At least 1 parent employed | 370 (88.5) | 186 (88.2) | 184 (88.9) |
| Language other than English spoken at home | 269 (64.3) | 141 (66.8) | 128 (61.8) |
Intervention Conditions
Enhanced UC
UC was enhanced by providing all primary care clinicians with training and educational materials on depression evaluation and treatment, as well as delivery of culturally competent care tailored to the cultural context of each AYA and their family. Treatment was available in English or Spanish depending on patient and family language preference. The training reviewed medication management based on the Texas Medication Algorithms for Major Depressive Disorder, emphasizing certain selective serotonin reuptake inhibitors as the first choice (Hughes etal., 1999). Providers had usual access to treatments for all patients, but study-trained care managers were available only to patients randomized to QI. UC generally involved referral for specialty mental health care and could include primary care management with medication and primary care counseling.
QI Intervention
The QI intervention was modeled on the adult Partners in Care study (Wells etal., 2000). In addition to the training and resources described above for the UC condition, the QI intervention included: (1) expert practice leaders at each site who adapted and oversaw the implementation of the intervention at the site, and (2) care managers at the sites who provided manualized CBT for depression (Asarnow etal., 2005) and supported primary care clinicians with patient evaluation, education, treatment initiation and follow-up, and linkage to needed services. Care managers were psychotherapists with master’s or PhD level degrees in the fields of mental health (MSW, dual MSW and RN degree, MFT, MA in Psychology, or PhD in Psychology). All care managers were provided with training in the study CBT, treatment manuals, and ongoing consultation and supervision. The study CBT includes an overview session, three four-session modules focused on activities and social skills, cognition, and communication and problem-solving, and a final session on relapse prevention. If participants randomized to the QI condition were receiving other treatment when enrolled in the study, they continued to be followed by the care manager to ensure that treatment needs were being met, enhance coordination of primary care and specialty mental health care, and adjust services if youths were not responding to the care they received. This approach was viewed as consistent with a collaborative integrated care model with behavioral health care included as part of the primary care treatment plan. Care managers were available to follow patients for 6 months to coordinate care, assist with treatment, and provide CBT as needed. The study provided training, written manuals, and consultation to support model fidelity, including case consultation to care managers on CBT and other aspects of the care manager role. Treatment was delivered in either English or Spanish depending on the patient’s preference. The study paid for care managers’ time, which was available without co-pay.
Baseline Predictor Measures
Predisposing Factors
Demographics. Adolescents were asked to report basic demographic information including age, gender, race and ethnicity, languages spoken at home, estimated family income, insurance information, highest level of parental education, and parental immigration status during the baseline assessment.
Enabling Factors
Perceived Stigma of Depression. Five items adapted from the Partners in Care study (Wells etal., 2000) were used to assess participant’s views of depression as stigmatizing. Participants were asked to rate how much peer relationships would suffer (on a scale from one (“A Lot”) to four (“None”)) if friends thought that the participant was diagnosed with depression, asthma, HIV/AIDS, or received mental health services. A dichotomous variable was then derived to represent if the participant rated depression (coded one) or another condition/receiving mental health services (coded zero) as most stigmatizing (Jaycox etal., 2006). Treatment Preferences. Treatment preferences were assessed using an item adapted from the Partners in Care Study (Dwight-Johnson, Sherbourne, Liao, & Wells, 2000). This question presented the recovery rates for each treatment modality and asked participants to indicate preference for one of three treatment options for depression. From these choices, treatment preference variables were derived for watchful waiting, medication, and psychotherapy. Prior Mental Health Treatment. Patient response on the Service Assessment for Children and Adolescents (SACA; Stiffman etal., 2000), adapted slightly for our primary care population (Asarnow etal., 2005), was used to dichotomously code the presence versus absence of any mental health treatment during the previous 6 months. This measure has shown strong reliability of parent and youth reports on presence versus absence of mental health treatment, psychotherapy, and medication (κ= .72–.93; Asarnow etal., 2011) and test–retest reliability (κ=.86 for any treatment in the past 12 months; Horwitz etal., 2001).
Need Factors
Major Depression and dysthymia symptoms and diagnoses were obtained using the Mood Disorders module of the CIDI-12, a well-established diagnostic tool with good psychometric properties (World Health Organization, 1997). The Anxiety subscale of the Brief Symptom Inventory was used to assess anxiety symptoms. Each of the six items that comprise the subscale are rated on a 5-point Likert scale and totaled for a dimensional score. The subscale has been shown to have high internal consistency (α =.81) and retest reliability (r =.79) (Derogatis & Melisaratos 1983; Derogatis & Savitz, 2000), and showed strong internal consistency in the study sample (α= 0.80). Posttraumatic Stress Disorder (PTSD) was assessed using the four-item Primary Care PTSD Screen (Prins etal., 2004), a measure that compared with structured diagnostic interviews shows excellent sensitivity (.91) and specificity (.84) for classifying PTSD status (Kimerling, Trafton, & Nguyen, 2006). Attention problems were assessed via the Attention Problems subscale score derived from participant self-report on the parallel Youth Self-Report (Achenbach, 1991; Achenbach & Rescorla, 2001) and Young Adult Self-Report (Achenbach & Rescorla, 2001) for youths ages 13–17 and 18–21, respectively. There is extensive support for the psychometric adequacy of these measures (Achenbach, 1991; Achenbach & Rescorla, 2001). Mental health-related functioning was assessed using the Short Form Health Survey (SF-12; Ware, Kosinski, & Keller, 1994) which includes subscales assessing role limitations owing to emotional problems and a mental health summary scale. The SF-12 has strong psychometric support (Ware etal., 1994) and showed fair internal consistency in the present sample (α= .76).
Outcome
Mental Health Treatment. Our outcome variable was receipt of mental health services in the past 6 months, derived from patient response on the SACA (Stiffman etal., 2000). Participants were asked to indicate if they had received services from a mental health specialist in the past 6 months, including visits to a psychologist, psychiatrist, social worker, or counselor. Responses were dichotomously coded yes/no. Reliability, as indexed by cross-informant agreement, is good for this measure (κ = .72–.93) (Asarnow etal., 2011).
Statistical Analyses
Statistical analyses were run using SPSS 24, and plots of significant interactions were generated using Stata 14. Our data analytic plan proceeded as follows. First, we screened for possible interactions of unmodifiable demographic variables (i.e., age, gender, race/ethnicity) with intervention condition; specifically, for each of the possible independent variables, we ran an individual logistic regression with mental health treatment received (yes/no) as the outcome including the variable, intervention condition, and the interaction of the variable and intervention condition, controlling for site. If the interaction was not significant (p < .05), we removed the interaction and examined the main effect of the covariate. Next, we ran a parallel set of logistic regression models to test for possible interactions of predisposing, enabling, and need factors with intervention condition, controlling for the main effects and interactions with the unmodifiable demographic variables identified in the first phase. Finally, we used a best subsets algorithm to identify the subset of variables that best predicted mental health service use. In line with other research in the field, we adopted the convention of including all interactions and main effects that are associated with the outcome at a p-value of ≤.10. In determining which variables to include in the best subsets procedure, we opted to take a data-driven and conservative approach. However, in an attempt to not be overly stringent (and thus reducing the generalizability of our findings), we included predictors that showed trend level of association with service use. We evaluated model fit using several criteria including the Akaike Information Criterion (AIC; Akaike, 1973) and Mallows’ Cp (Mallows, 1973). The best fitting model was defined as the model demonstrating the lowest AIC value and Mallow’s Cp most similar to the number of predictors in the model, while accounting for the most amount of variance.
Nonresponse weights were constructed and applied in analyses to increase the likelihood that the results represented unbiased estimates for the original YPIC sample (Asarnow etal., 2005). Weighted and unweighted analyses yielded similar results; exceptions to this are noted in the results.
Results
Moderator Analyses: Interactions With Intervention Condition
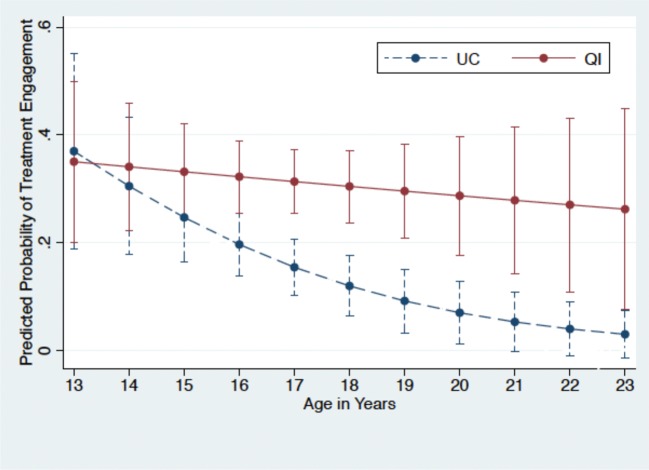
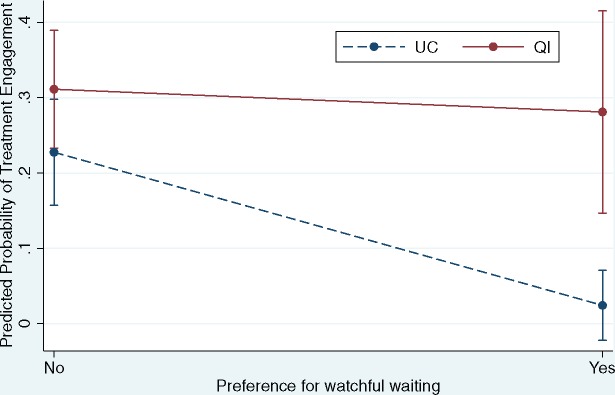
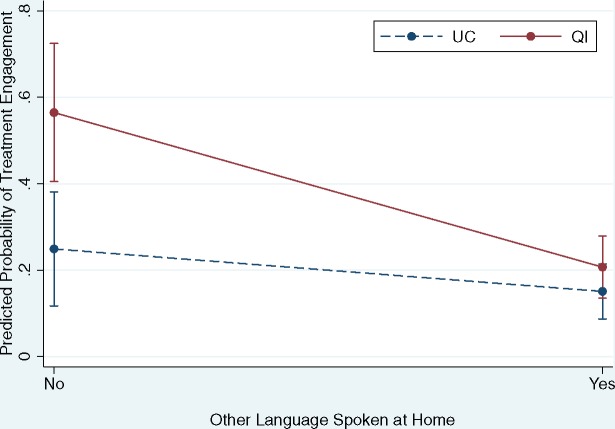
As predicted and reported previously (Asarnow etal., 2005), there was a significantly increased treatment rate among AYA in the QI condition compared with the UC condition. In the individual logistic regression models of each variable and its interaction with intervention condition, significant moderators emerged as follows: (1) older age (within the 13–21 age range) was associated with lower treatment rates in the UC but not the QI condition (p < .0001) (Figure 1); (2) a preference for watchful waiting over active treatment was associated with lower treatment rates in the UC but not the QI condition (p=.019) (Figure 2); (3) when English was the primary language spoken at home, treatment rates were higher in the QI condition but when another language was spoken at home, treatment rates were similar across conditions (p =.023) (Figure 3). This effect escaped statistical significance in the unweighted analyses (p =.06). All other findings were the same in weighted and unweighted analyses.
Figure 1.
Predicted probability of service use across the age range by intervention condition.
Figure 2.
Predicted probability of service use for adolescents and young adults who endorse a preference for watchful waiting versus active treatment by intervention condition.
Figure 3.
Predicted probability of service use for adolescents and young adults who speak a language other than English at home versus only English by intervention condition.
Predictors of Mental Health Treatment Use: Bivariate Predictors
Table II presents all significant associations between treatment use and predictor variables that did not significantly interact with intervention status, controlling for nonmodifiable demographic variables (i.e., study site, gender, race/ethnicity, and age). Because age significantly interacted with treatment condition, we also included this interaction as a covariate. Treatment was significantly more likely among AYA with low levels of perceived depression-related stigma, previous mental health treatment, and higher levels of need as indicated by higher rates of depression diagnoses (Major Depressive Disorder or dysthymia), suicidality, positive PTSD screens, higher levels of anxiety and attention problems, and lower self-reported mental health (Mental Health Index-5) and mental health-related functioning (SF-12). There were no other discrepancies between weighted and unweighted bivariate analyses. The following variables were tested but were not significantly associated with the outcome (all p-values > .20): study site, ethnicity, gender, parental education level, parent immigration status, satisfaction with mental health care, insurance status, substance use, externalizing problems, and eating disorders symptoms. Results were similar in weighted and unweighted analyses, with the exception that speaking English at home (vs. another language) was significantly associated with increased treatment rates in the unweighted analyses (odds ratio = 0.298, p=.002).
Table II.
Significant Results of Weighted Logistic Regression Predicting Service Use From Predisposing, Enabling, and Need Factors, Controlling for Unmodifiable Demographic Variables (i.e., Intervention Condition, Study Site, Gender, Race/Ethnicity, Age, and Age by Intervention Condition Interaction)
| Variable | Odds ratio | p-value | Odds ratio 95% CI |
|
|---|---|---|---|---|
| Lower | Upper | |||
| Predisposing factors | ||||
| View of depression as most stigmatizing problem | 0.597 | .045 | 0.361 | 0.988 |
| Enabling factors | ||||
| Previous treatment for mental health problems | 5.00 | <.0001 | 2.83 | 8.81 |
| Need factors | ||||
| CIDI MDD or dysthymia diagnosis | 2.68 | <.0001 | 1.64 | 4.40 |
| Suicidality | 1.41 | .005 | 1.11 | 1.80 |
| Positive PTSD screen | 1.94 | .01 | 1.17 | 3.21 |
| BSI anxiety subscale total score | 1.06 | .022 | 1.01 | 1.12 |
| Attention problems | 1.10 | .005 | 1.03 | 1.18 |
| SF-12 Mental Health Summary Score | 0.947 | <.0001 | 0.926 | 0.969 |
| MHI-5 Score | 0.935 | .01 | 0.888 | 0.984 |
Note: CI = confidence interval; CIDI= Composite International Diagnostic Interview; MDD = Major Depressive Disorder; PTSD = Posttraumatic Stress Disorder; BSI= Brief Symptom Inventory; SF-12 = Short Form Health Survey; MHI = Mental Health Index.
Joint Model: Best Subsets Procedure
We used a best subsets algorithm (which accounts for multiple comparisons) to identify the set of variables that best predicted service use in our sample. All significant interactions and predictors associated with the outcome at a p-value <.10 were included in the algorithm. Our final model (adjusted R2 = 0.208) included the following variables: interaction of intervention condition with age; interaction of intervention condition with preference for active treatment versus not; interaction of intervention and language use; conditional effects of age, preference for active treatment, and language use; and main effects of view of depression as stigmatizing, overall mental health, functioning problems/low mental health-related quality of life (SF-12), and history of previous mental health treatment. This model represents the best fitting and most unbiased model that accounted for the greatest amount of variance. The mean Variance Inflation Factor (VIF) of all predictors entered into the model was equal to 1.54 and individual VIF values ranged from 1.02 to 3.15, indicating no significant multicollinearity between predictors. Weighted and unweighted models did not differ meaningfully.
Discussion
This study examined predictors of mental health treatment in the largest extant trial to evaluate an integrated model for improving access to evidence-based depression care in adolescent and emerging adult primary care patients (Asarnow etal., 2009; Asarnow etal., 2005), a critical issue given the high morbidity and mortality and low treatment rates for AYA with depression. Integrating mental health care within primary care provides one strategy for increasing treatment rates and has been increasingly incentivized in the U.S. health care system owing to recognition of the potential of integrated medical-behavioral primary health care for defragmenting care and achieving the triple aim of improving health, the quality and experience of care, and reducing costs (Asarnow etal., 2015b; Miller, 2015).
Major findings from this study are as follows. We identified three variables that differentially predicted service use across conditions, highlighting mechanisms through which integrated care interventions may lead to improved rates of care and health/behavioral health benefits. First, we found that while treatment rates declined with increasing age under the UC condition, this decline in treatment rates with age was slower and nonsignificant in the intervention condition. This finding points to the value of integrated care approaches for addressing low rates of care in older AYA (Furstenberg, 2006; Park etal., 2014; Paul etal., 2009). To our knowledge, this study is the first to report on the effect of an integrated care intervention for reducing the age-related decline in service utilization often seen in older AYA. This decline may be attributable to changes in parental involvement in an adolescent’s mental health care, with parents taking a less active role with older adolescents/young adults, in contrast to the active role parents often play in obtaining services for younger children (Pescosolido, Garner, & Lubell, 1998). The QI intervention, in which care was made to be more accessible, was able to mitigate the negative influence of age on rates of service use. It is possible that the intervention made it easier for older adolescents who face more academic demands and often have to navigate the health system with less support from their parents to access treatment services. It is also possible that the QI intervention overcame age-related individual characteristics that have been found to influence service use. For example, as adolescents grow older they exhibit a greater tendency to be secretive about their health behaviors (Main etal., 2015) and be more responsive to models of care that forefront shared decision making (Bejarano etal., 2015). Thus, the QI intervention, which emphasized integrated and collaborative medical-behavioral primary care, may have fostered a more open, empowering patient–provider relationship that promoted increased use of needed services.
Second, while AYA in the UC condition tended to be less likely to receive care when they expressed a preference for watchful waiting over active depression treatment, the QI intervention was associated with similar treatment rates for AYA with initial preferences for both watchful waiting and active treatment. Attitudes toward help-seeking have been found to be potent predictors of service utilization (McKay, Pennington, Lynn, & McCadam, 2001), and some studies suggest that attitudes may be influenced by race/ethnicity (Dwight-Johnson etal., 2000; Yeates etal., 2002). The success of the QI intervention in overcoming the barrier of initial reluctance for active treatment was likely owing to the emphasis on psychoeducation regarding depression, depression treatment options, and the emphasis on patient choice of preferred treatment options (e.g., psychotherapy, medication, watchful waiting/care manager follow-up). This psychoeducation aimed to present depressive symptoms as a frequent and “normal” response to stress and encouraged providers to collaborate with patients to consider an optimal treatment plan for alleviating their stress and symptoms. This was intended to decrease stigma associated with depression and increase the likelihood that AYA would seek treatment, while also increasing the accessibility of treatment through integrated, co-located, and coordinated services. The present data support the efficacy of this approach for reducing the deleterious impact of initial reluctance to pursue treatment.
Lastly, while the intervention was associated with significantly improved treatment rates among AYA who spoke English at home, the intervention had minimal effects on treatment uptake among families who spoke another language at home. The language use variable was strongly associated with parents being immigrants to the United States and can be viewed as an indicator of lower levels of acculturation. Most AYA who spoke another language at home endorsed Hispanic-Latino ethnicity and sensitivity analyses revealed that results held within the Hispanic-Latino subgroup. This low rate of service use among AYA with non-English-speaking parents or bilingual parents is consistent with findings from epidemiological, and other studies showing that adults with limited English proficiency in the United States often do not seek out or obtain mental health services (Alegría etal., 2007; Sentell etal., 2007; Weech-Maldonado etal., 2003). It is of note that the effect of language on service use is often attributed in part to the limited availability of bilingual clinicians (Bernal & Castro, 1994). However, Spanish-speaking clinicians were available in the YPIC study, extensive training on cultural factors aimed at enhancing clinician cultural sensitivity was provided, and telephone outreach was used when patients were unable to attend the clinics. Our findings, therefore, underscore the challenges and need for novel strategies to identify and address other factors that may be deterring service use among less acculturated families (Becker Herbst, Margolis, Millar, Muther, & Talmi, 2016).
Tests of main effects of variables that did not significantly interact with treatment condition revealed additional variables that significantly predicted service use, and the joint model identified the subset of variables that represented the most robust predictors. In line with findings in the field, AYA who did not access mental health treatment were likely to view depression as highly stigmatizing (predisposing factor), have no mental health treatment at baseline (enabling factor), demonstrate a lesser degree of need as reflected by lower rates of depressive disorders, suicidality, PTSD, general anxiety symptoms, attention problems, and mental health-related functioning/impairment (need factors). Of note, as seen in previous research (Jaycox etal., 2006; Wichstrom, Belsky, Jozefiak, Sourander, & Berg-Nielson, 2014), prior mental health treatment emerged as a significant enabling variable. It appeared to be associated with the greatest fold increase in likelihood of receiving services and was included in the joint model. One possibility is that this is attributable to increased familiarity with pathways to care (Moses, 2011) and continued treatment during the intervention period. Furthermore, systems-level analysis of service use has shown that positive experiences with treatment systems influence future orientations to treatment seeking (Pescosolido, 1992). The large majority of AYA in this sample who reported previous mental health care at baseline rated these services as satisfactory or highly satisfactory, perhaps increasing propensity to continue and/or seek additional care (Moses, 2011). These findings are also consistent with other work demonstrating that brief emergency interventions that provide suicidal adolescents with exposure to high-quality mental health care lead to improved linkage to mental health services (Asarnow etal., 2011; Ougrin, Tranah, Stahl, Moran, & Asarnow, 2015; Rotheram-Borus, Piacentini, Cantwell, Bellin, & Song, 2002; Spirito, Boergers, Donaldson, Bishop, & Lewander, 2002).
The present study should be viewed in the context of several limitations. First, this study aimed to evaluate predictors of receiving treatment under two different approaches to behavioral health service delivery: the QI integrated collaborative care approach compared with usual primary care, where medication treatment was available but AYA were generally referred to specialty care for psychotherapy. In line with this goal, we made several decisions regarding our data analytic approach including coding our outcome dichotomously and focusing on whether youths received treatment during the 6-month intervention period. Future research is needed to examine variables related to dosage, quality of treatment, and longer term treatment patterns under different care delivery approaches. Second, the YPIC care model may be challenging to implement and not feasible in some settings. Notably, similar to some Health Maintenance Organizations and Accountable Care Organizations, behavioral health care was offered with no additional charge, reducing financial barriers to care. Third, as data were initially collected, there have been several large-scale policy shifts, which may have affected barriers to care (e.g., ability of AYA to stay on parents’ insurance), although the QI intervention is consistent with the current emphasis on integrating behavioral health and primary care (Asarnow etal., 2015b; Asarnow etal., 2017). For instance, the health policy change that allows young adults to remain on their parents’ health insurance may help to address the low rate of care among older youths that was observed in this sample under the UC condition. Finally, from a demographic perspective, while our sample included a large number of ethnic minorities, most of these individuals endorsed Hispanic-Latino ethnicity. We are not able to determine whether these results are unique to Latinos or would generalize to other racial/ethnic groups. Finally, AYA who did not speak English were excluded from the study, potentially representing a less acculturated subsample. We are not certain if the impact of the QI intervention would be different if this subsample were included.
Clinical Implications and Future Directions
This study provides important information to guide service delivery for AYA. Specifically, study results clarify predictors of receiving treatment (a necessary precondition for receiving effective treatment) under two treatment approaches: (1) an integrated collaborative care approach that aimed to improve access to evidence-based depression care, or (2) usual primary care. Our results indicate that AYA with the highest levels of need for mental health services are most likely to link to needed care, an encouraging point from the perspective of population health. Moreover, the YPIC integrated primary medical-behavioral health care program was able to overcome barriers to care associated with predisposing factors such as an initial reluctance to obtain active treatment and older age, leading to some AYA receiving needed treatment who might otherwise choose to go without care. Consistent with the whole systems approach in pediatric psychology and current trends toward integrated care models, our results indicate that the YPIC integrated care model was able to overcome some barriers to accessing care such as older age and an initial preference not to pursue treatment. Favorable findings support the promise of integrated care models for increasing rates of needed mental health care. Other findings regarding language use, and by proxy, help-seeking behaviors of Latino families, indicate the need to address issues more specific to racial/ethnic minorities. This may constitute further study of engagement strategies, or better understanding the factors that contribute to lesser service use in these populations. The YPIC-integrated care model featured collaborative care with a care manager/clinician to address behavioral health needs, a shared mental/behavioral health-medical treatment plan, co-located medical and behavioral health services, telephone outreach, a registry, and mental health consultant (usually a psychologist) to support evidence-based care and decision making. While this study provided a needed demonstration project, alternative less extensive models may yield similar improvements (Asarnow etal., 2015b; Asarnow, Kolko, Miranda, & Kazak, 2017).
Collectively, findings indicate that further research is needed to clarify: (1) whether similar findings would be obtained in other care settings or other service delivery models that have become increasingly common since the passage of health care reform legislation (e.g., Patient Centered Medical Homes), (2) the power of different intervention components for improving treatment rates, (3) further variables that may influence how AYA access and receive mental health care to better understand patterns of help-seeking and identify targets for interventions that might promote positive health behaviors (e.g., seeking depression treatment) that mitigate lifetime risk (Perrin, Anderson, & Van Cleave, 2014), and (4) innovative approaches to engaging AYA from less acculturated families in needed treatment. The present findings also highlight the need to examine cultural variables as they relate to treatment engagement. In particular, examining how the acculturative process (which includes dynamics such as language acquisition, experiences of discrimination, stigma, and intergenerational conflict) impacts the decisions racial/ethnic minority families make about mental health treatment is warranted.
Conclusions
Integrated medical-behavioral primary care offers one strategy for addressing the problem of unmet need for behavioral health care among AYA. Study results highlight the value of collaborative integrated care interventions for overcoming barriers to care associated with an initial reluctance to pursue active treatment and older age. Results point to the need for monitoring and outreach for AYA without prior mental health treatment, for including measures of functional impairment to be maximally effective in identifying AYA who may require services, and for promoting engagement efforts among less acculturated families (i.e., where English is not the primary language spoken at home), as these AYA are less likely to receive care under both integrated care and usual primary care conditions.
A major contribution of the present study is that findings help inform ways to improve access to and use of behavioral health care, which is particularly important given recent increased focus on integrated medical-behavioral primary care. Understanding the factors that contribute to service use during the critical period of the lifespan when adolescents begin to transition into adulthood may improve the field of pediatric psychology’s ability to promote healthy outcomes and reduce long-term morbidity owing to chronic mental health conditions.
Funding
This study was conducted without funding. The original Youth Partners in Care trial was funded by the Agency for Health Care Research and Quality (HS09908).
Conflict of interest: Amy M. Rapp declares that she has no conflict of interest. Denise A. Chavira declares that she has no conflict of interest. Catherine A. Sugar declares that she has no conflict of interest. Joan R. Asarnow receives research grant funding from the National Institute of Mental Health and American Foundation for Suicide Prevention. She has also consulted on quality improvement and interventions for depression and suicidal/self-harm behavior.
References
- Achenbach T. M. (1991). Manual for the youth self-report. Burlington, VT: Department of Psychiatry, University of Vermont. [Google Scholar]
- Achenbach T. M., Rescorla L. A. (2001). Manual for the ASEBA school-age forms & profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Ader J., Stille C., Keller D., Miller B. F., Barr M. S., Perrin J. M. (2015). The medical home and integrated behavioral health: Advancing the policy agenda. Pediatrics, 135, 1–9. [DOI] [PubMed] [Google Scholar]
- Akaike H. (1973). Information theory as an extension of the maximum likelihood principle In Petrov B. N., Csaki F. (Eds.), Second international symposium on information theory (pp. 267–281). Budapest: Akademiai Kiado. [Google Scholar]
- Alegría M., Mulvaney-Day N., Woo M., Torres M., Gao S., Oddo V. (2007). Correlates of past-year mental health service use among Latinos: Results from the National Latino and Asian American Study. American Journal of Public Health, 97, 76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson R. M. (1995). Revisiting the behavioral model and access to medical care; does it matter? Journal of Health and Social Behavior, 36, 1–10. [PubMed] [Google Scholar]
- Andrews G. (2001). Should depression be managed as a chronic disease? British Medical Journal, 322, 419.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow J. R., Baraff L., Berk M., Grob C., Devich-Navarro M., Suddath R., Piacentini J. C., Rotheram-Borus M. J., Cohen D., Tang L. (2011). Effects of an emergency department mental health intervention for linking pediatric suicidal patients to follow-up mental health treatment: A randomized controlled trial. Psychiatric Services, 62, 1303–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow J. R., Hoagwood K. E., Stancin T., Lochman J. E., Hughes J. L., Miranda J. M., Wysocki T., Portwood S. G., Piacentini J., Tynan D., Atkins M., Kazak A. E. (2015b). Psychological science and innovative strategies for informing health care redesign: A policy brief. Journal of Clinical Child and Adolescent Psychology, 44, 923–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow J. R., Jaycox L. H., Duan N., LaBorde A. P., Rea M. M., Tang L., Anderson M., Murray P., Landon C., Tang B., Huizar D. P., Wells K. B. (2005). Depression and role impairment among adolescents in primary care clinics. Journal of Adolescent Health, 37, 477–483. [DOI] [PubMed] [Google Scholar]
- Asarnow J. R., Jaycox L. H., Tang L., Duan N., LaBorde A. P., Zeledon L. R., Anderson M., Murray P. J., Landon C., Rea M. M., Wells K. B. (2009). Long-term benefits of short-term quality improvement interventions for depressed youths in primary care. American Journal of Psychiatry, 166, 1002–1010. [DOI] [PubMed] [Google Scholar]
- Asarnow J. R., Jaycox L., Duan N., LaBorde A. P., Rea M. M., Murray P., Anderson M., Landon C., Tang L., Wells K. B. (2005). Effectiveness of a Quality Improvement intervention for adolescent depression in primary care clinics. A randomized controlled trial. Journal of the American Medical Association, 293, 311–319. [DOI] [PubMed] [Google Scholar]
- Asarnow J. R., Kolko D. J., Miranda J., Kazak A. E. (2017). The pediatric patient-centered medical home: Innovative models for improving behavioral health. American Psychologist, 72, 13–27. [DOI] [PubMed] [Google Scholar]
- Asarnow J. R., Rozenman M., Wiblin J., Zeltzer J. (2015a). Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: A meta-analysis. JAMA Pediatrics, 169, 929–937. [DOI] [PubMed] [Google Scholar]
- Avenevoli S., Swendsen J., He J., Burstein M., Merikangas K. (2015). Major depression in the National Comorbidity Survey-Adolescent Supplement: Prevalence, correlates, and treatment. Journal of the American Academy of Child and Adolescent Psychiatry, 54, 37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker Herbst R., Margolis K. L., Millar A. M., Muther E. F., Talmi A. (2016). Lost in translation: Identifying behavioral health disparities in pediatric primary care. Journal of Pediatric Psychology, 41, 481–491. [DOI] [PubMed] [Google Scholar]
- Bejarano C., Fuzzell L., Clay C., Leonard S., Shirley E., Wysocki T. (2015). Shared decision making in pediatrics: A pilot and feasibility project. Clinical Practice in Pediatric Psychology, 3, 25–36. [Google Scholar]
- Bernal M. E., Castro F. G. (1994). Are clinical psychologists prepared for service and research with ethnic minorities? Report of a decade of progress. American Psychologist, 49, 797–805. [DOI] [PubMed] [Google Scholar]
- Brach C., Fraser I., Paez K. (2005). Crossing the language chasm. Health Affairs, 24, 424–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callahan S. T., Cooper W. O. (2010). Changes in ambulatory health care use during the transition to young adulthood. Journal of Adolescent Health, 46, 407–413. [DOI] [PubMed] [Google Scholar]
- Chevarley F. (2003). Children's access to necessary health care, fall 2001 In Medical expenditure panel survey. Rockville, MD: Agency for Healthcare Research and Quality. [Google Scholar]
- Clement S., Schauman O., Graham T., Maggioni F., Evans-Lacko S., Bezborodovs N., Morgan C., Rüsch N., Brown J. S., Thornicroft G. (2015). What is the impact of mental-health related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychological Medicine, 45, 11–27. [DOI] [PubMed] [Google Scholar]
- Copeland W. E., Wolke D., Shanahan L., Costello E. J. (2015). Adult functional outcomes of common childhood psychiatric problems: A prospective longitudinal study. JAMA Psychiatry, 72, 892–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis L. R., Savitz K. L. (2000). The SCL-90- and Brief Symptom Inventory (BSI) in primary care In Maurish M. E. (Ed.), The handbook of psychological assessment in primary care settings (pp. 297–329). Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Derogatis L. R., Melisaratos N. (1983). The brief symptom inventory: An introductory report. Psychological Medicine, 13, 595–605. [PubMed] [Google Scholar]
- Dwight-Johnson M., Sherbourne C. D., Liao D., Wells K. B. (2000). Treatment preferences among depressed primary care patients. Journal of General Internal Medicine, 15, 527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elster A., Jarosik J., VanGeest J., Fleming M. (2003). Racial and ethnic disparities in health care for adolescents: A systematic review of the literature. Archives of Pediatric and Adolescent Medicine, 157, 867–874. [DOI] [PubMed] [Google Scholar]
- Fix M., Zimmermann W., Passel J. (2001). The integration of immigrant families in the United States. Washington, DC: Urban Institute. [Google Scholar]
- Fortuna R. J., Robbins B. W., Halterman J. S. (2009). Ambulatory care in the United States. Annals of Internal Medicine, 51 (379–385. [DOI] [PubMed] [Google Scholar]
- Furstenberg F. F. (2006). Growing up healthy: Are adolescents the right target group? Journal of Adolescent Health, 29 (303–304. [DOI] [PubMed] [Google Scholar]
- Heath B., Wise R. P., Reynolds K. (2013). A standard framework for levels of integrated healthcare. Washington, DC: SAMHSA-HRSA Center for Integrated Health Solutions. [Google Scholar]
- Hernandez D. J. (2004). Demographic change and the life circumstances of immigrant families. Future Child, 14, 17–45. [Google Scholar]
- Horwitz S. M., Hoagwood K., Stiffman A. R., Summerfeld T., Weisz J. R., Costello E. J., Rost K., Bean D. L., Cottler L., Leaf P. J., Roper M., Norquist G. (2001). Reliability of the services assessment for children and adolescents. Psychiatric Services, 52, 1088–1094. [DOI] [PubMed] [Google Scholar]
- Hughes C., Graham E., Crismon M., Wagner K., Birmaher B., Geller B., Pliszka S. R., Ryan N. D., Strober M., Trivedi M. H., Toprac M. G., Sedillo A., Llana M. E., Lopez M., Rush A. (1999). The Texas Children's Medication Algorithm Project: Report of the Texas Consensus Conference Panel on medication treatment of childhood Major Depressive Disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 38, 1442–1454. [DOI] [PubMed] [Google Scholar]
- Irwin C. E. (2010). Young adults are worse off than adolescents. Journal of Adolescent Health, 46, 405–406. [DOI] [PubMed] [Google Scholar]
- Jaycox L., Asarnow J., Sherbourne C., Rea M., LaBorde A., Wells K. (2006). Adolescent primary care patients’ preferences for depression treatment. Administration and Policy in Mental Health and Mental Health Services Research, 33, 198–207. [DOI] [PubMed] [Google Scholar]
- Keller M. B., Boland R., Leon A., Solomon D., Endicott J., Li C. (2013). Clinical course and outcome of unipolar major depression In Keller M. B., Coryell W. H., Endicott J., Maser J. D., Schettler P. J. (Eds.), Clinical guide to depression and bipolar disorder (pp. 155–173). Washington, DC: American Psychiatric Press. [Google Scholar]
- Kimerling R., Trafton J. A., Nguyen B. (2006). Validation of a brief screen for post-traumatic stress disorder with substance use disorder patients. Addictive Behaviors, 31 (2074–2079. [DOI] [PubMed] [Google Scholar]
- Kolko D. J., Perrin E. J. (2014). The integration of behavioral health services in pediatric primary care: Services, science, and suggestions. Journal of Clinical Child and Adolescent Psychology, 43, 216–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansing A. H., Berg C. A. (2014). Topical review: Adolescent self-regulation as a foundation for chronic illness self-management. Journal of Pediatric Psychology, 39, 1091–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lessard G., Ku L. (2003). Gaps in coverage for children in immigrant families. Future Child, 13, 101–115. [PubMed] [Google Scholar]
- Lewinsohn P. (2002). Depression in adolescents In Gotlib I. H., Hammen C. L. (Eds.), Handbook of depression. New York, NY: Guilford Press. [Google Scholar]
- Lieberman A., Adalist-Estrin A., Erinle O., Sloan N. (2006). On-site mental health care: a route to improving access to mental health services in an inner-city, adolescent medicine clinic. Child: Care, Health & Development, 32, 407–413. [DOI] [PubMed] [Google Scholar]
- Main A., Wiebe D. J., Van Bogart K., Turner S. L., Tucker C., Butner J. E., Berg C. A. (2015). Secrecy from parents and Type 1 diabetes management in late adolescence. Journal of Pediatric Psychology, 40, 1075–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallows C. L. (1973). Some comments on Cp. Technometrics, 15, 661–675. [Google Scholar]
- McDaniel S. H., Grus C. L., Cubic B. A., Hunter C. L., Kearney L. K., Schuman C. C., Karel M. J., Kessler R. S., Larkin K. T., McCutcheon S., Miller B. F., Nash J., Qualls S. H., Connolly K. S., Stancin T., Stanton A. L., Sturm L. A., Johnson S. B. (2014). Competencies for psychology practice in primary care. American Psychologist, 69, 409–429. [DOI] [PubMed] [Google Scholar]
- McGuire T. G., Miranda J. (2008). Racial and ethnic disparities in mental health care: Evidence and policy implications. Health Affairs (Project Hope), 27, 393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay M. M., Pennington J., Lynn C. J., McCadam K. (2001). Understanding urban child mental health l service use: Two studies of child, family, and environmental correlates. The Journal of Behavioral Health Services & Research, 28, 475–483. [DOI] [PubMed] [Google Scholar]
- Miller B. F. (2015). When frontline practice innovations are ahead of the health policy community: The example of behavioral health and primary care integration. Journal of the American Board of Family Medicine, 28(Suppl 1), S98–S101. [DOI] [PubMed] [Google Scholar]
- Miranda J., Duan N., Sherbourne C., Schoenbaum M., Lagomasino I., Jackson-Triche M., Wells K. B. (2003). Improving care for minorities: Can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health Services Research, 38, 613–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moses J. (2011). Individual psychological assessment: You pay for what you get. Industrial and Organizational Psychology, 4, 334–337. [Google Scholar]
- Ngo V., Asarnow J., Lange J., Jaycox L., Rea M., Landon C., Tang L., Miranda J. (2009). Outcomes for youths from racial-ethnic minority groups in a quality improvement intervention for depression treatment. Psychiatric Services, 60, 1357–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson J. L., Collins S. R., Mahato B., Gould E., Schoen C., Rustgi S. D. (2009). Rite of passage? Why young adults become uninsured and how new policies can help In The commonwealth fund issue brief. New York, NY: The Commonwealth Fund. [PubMed] [Google Scholar]
- Ougrin D., Tranah T., Stahl D., Moran P., Asarnow J. R. (2015). Therapeutic interventions for suicide attempts and self-harm in adolescents: Systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry, 54, 97–107. [DOI] [PubMed] [Google Scholar]
- Park M. J., Scott J. T., Adams S. H., Brindis C. D., Irwin C. E. Jr (2014). Adolescent and young adult health in the United States in the past decade: Little improvement and young adults remain worse off than adolescents. Journal of Adolescent Health, 55, 3–16. [DOI] [PubMed] [Google Scholar]
- Paul T., Park M. J., Adams S. H., Irwin C. E. Jr, Brindis C. D. (2009). Adolescent/young adult health in the US: Trends and implications. Journal of Adolescent Health, 45, 8–24. [DOI] [PubMed] [Google Scholar]
- Perrin J. M., Anderson L. E., Van Cleave J. (2014). The rise in chronic conditions among infants, children, and youth can be met with continued health system innovations. Health Affairs, 33, 2099–2105. [DOI] [PubMed] [Google Scholar]
- Pescosolido B., Garner C., Lubell K. (1998). How people get into mental health services: Stories of choice, coercion, and "muddling through" from "first timers". Social Science and Medicine, 46, 275–286. [DOI] [PubMed] [Google Scholar]
- Pescosolido B. A. (1992). Beyond rational choice: The social dynamics of how people seek help. American Journal of Sociology, 97, 1096–1138. [Google Scholar]
- Prins A., Ouimette P., Kimerling R., Camerond R. P., Hugelshofer D. S., Shaw-Hegwer J. (2004). The primary care PTSD screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry, 9, 9–14. [Google Scholar]
- Radloff L. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. [Google Scholar]
- Richardson L. P., Russo J. E., Lozano P., McCauley E., Katon W. (2008). The effect of comorbid anxiety and depressive disorders on health care utilization and costs among adolescents with asthma. General Hospital Psychiatry, 30, 398–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus M. J., Piacentini J., Cantwell C., Bellin T. R., Song J. (2002). The 18-month impact of an emergency room intervention for adolescent female suicide attempters. Journal of Consulting and Clinical Psychology, 68, 1081–1093. [DOI] [PubMed] [Google Scholar]
- Sentell T., Shumway M., Snowden L. (2007). Access to mental health treatment by English language proficiency and race/ethnicity. Journal of General Internal Medicine, 22(Suppl 2), 289–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sourander A., Helstela L., Ristkari K., Helenius H., Phia J. (2001). Child and adolescent mental health service use in Finland. Social Psychiatry and Psychiatric Epidemiology, 36, 294–298. [DOI] [PubMed] [Google Scholar]
- Spirito A., Boergers J., Donaldson D., Bishop D., Lewander W. (2002). An intervention trial to improve adherence to community treatment by adolescents following a suicide attempt. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 435–442. [DOI] [PubMed] [Google Scholar]
- Stancin T., Perrin E. C. (2014). Psychologists and pediatricians: Opportunities for collaboration in primary care. American Psychologist, 69, 332–343. [DOI] [PubMed] [Google Scholar]
- Stancin T., Perrin E. C., Ramirez L. (2009). Pediatric psychology and primary care In Roberts M. C., Steele R. G. (Eds.), Handbook of pediatric psychology (4th ed., pp. 630–646). New York, NY: Guilford Press. [Google Scholar]
- Stein R. E. K., Horwitz S. M., Storfer-Isser A., Heneghan A., Olson L., Hoagwood K. (2008). Do pediatricians think they are responsible for identification and management of child mental health problems? Results of the APP Periodic Survey. Ambulatory Pediatrics, 8, 11–17. [DOI] [PubMed] [Google Scholar]
- Stiffman A. R., Horwitz S. M., Hoagwood K., Compton W., Cottler L., Bean M. S., Narrow W. E., Weisz J. (2000). Adult and child reports of mental health services in the Service Assessment for Children and Adolescents (SACA). Journal of the Academy of Child and Adolescent Psychiatry, 39, 1032–1039. [DOI] [PubMed] [Google Scholar]
- Turner E. A., Jensen-Doss A., Heffer R. W. (2015). Ethnicity as a moderator of how parents’ attitudes and perceived stigma influence intentions to seek child mental health services. Cultural Diversity and Ethnic Minority Psychology, 21, 613–618. [DOI] [PubMed] [Google Scholar]
- Kaiser Commission on Medicaid and the Uninsured. (2000). Immigrant’s health care: Coverage and access. Washington, DC: The Henry J. Kaiser Family Foundation. [Google Scholar]
- Ware J. E. J., Kosinski M., Keller S. D. (1994). SF36: Physical and mental summary scales: A user’s manual. Boston, MA: The Health Institute, New England Medical Center. [Google Scholar]
- Weech-Maldonado R., Morales L. S., Elliott M., Spritzer K., Marshall G., Hays R. D. (2003). Race/ethnicity, language and patients’ assessments of care in Medicaid managed care. Health Services Research, 38, 789–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weersing V. R. (2010). Samples and systems: Finding the fit to improve care for adolescent depression. Administration and Policy in Mental Health and Mental Health Services Research, 37, 197–200. [DOI] [PubMed] [Google Scholar]
- Wells K. B., Sherbourne C., Schoenbaum M., Duan N., Meredith L., Unützer J., Miranda J., Carney M. F., Rubenstein L. V. (2000). Impact of disseminating quality improvement programs for depression in managed primary care. A Randomized Controlled Trial. JAMA, 283, 212–220. [DOI] [PubMed] [Google Scholar]
- Wells K. B., Tang L., Carlson G. A., Asarnow J. R. (2012). Treatment of youth depression in primary care under usual practice conditions: observational findings from Youth Partners in Care. Journal of Child and Adolescent Psychopharmacoly, 22, 80–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichstrom L., Belsky J., Jozefiak T., Sourander A., Berg-Nielson T. S. (2014). Predicting service use for mental health problems among young children. Pediatrics, 133, 1054–1060. [DOI] [PubMed] [Google Scholar]
- World Health Organization (1997). Composite International Diagnostic Interview (CIDI) core version 2.1 interviewer’s manual. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Wysocki T., Hough B. S., Ward K. M., Green L. B. (1992). Diabetes mellitus in the transition to adulthood: Adjustment, self-care, and health status. Developmental and Behavioral Pediatrics, 13, 194-201.. [PubMed] [Google Scholar]
- Wysocki T., Nansel T. R., Holmbeck G. N., Chen R., Laffel L., Anderson B. J., Weissberg-Benchell J. (2009). Cooperative involvement of primary and secondary caregivers: Associations with youths’ diabetes outcomes. Journal of Pediatric Psychology, 34, 869–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeates K. O., Taylor G., Woodrome S. E., Wade S. L., Stancin T., Drotar D. (2002). Race as a moderator of parent and family outcomes following pediatric traumatic brain injury. Journal of Pediatric Psychology, 27, 292–403. [DOI] [PubMed] [Google Scholar]