Although cancer patients were satisfied with their physicians, treatment of cancer pain was still suboptimal. Guidelines should be revised to improve pain assessment and control in patients with cancer.
Keywords: cancer pain, guidelines, outpatient department, pain control, quality of life, satisfaction
Abstract
Background
We have limited knowledge about cancer patients’ pain control satisfaction in outpatient departments in Taiwan and doctors’ practice of adjusting analgesics according to their pain status. This survey examined pain management and satisfaction among cancer outpatients with pain and obtained information on their quality of life and treatment management for different pain intensities.
Methods
The Short version of the Brief Pain Inventory was used as the outcome questionnaire. Participants comprised 2075 patients with different cancers and disease statuses at 14 oncological outpatient departments, of which 1051 reported pain within the week prior to testing. The impact of pain management on physical and psychological functioning, and satisfaction with doctors were evaluated. Information about doctors’ prescriptions was collected. Logistic regression analyses were conducted to evaluate whether the interference scale performed identically in the different analgesic ladders.
Results
Pain was significantly linked to disease status and affected patients’ physical and psychiatric functioning. Almost 100% of patients were satisfied with their pain control, but more than 70% of doctors did not change analgesics based on patients’ current pain status. The results show that although patients were satisfied with their physicians, treatment of cancer pain was still suboptimal.
Conclusion
Pain assessment and treatment need to be more thorough and management guidelines should be revised to improve pain control in patients with cancer.
Introduction
Pain is one of the most common and distressing symptoms for cancer patients and a problem for caregivers. Poor control of pain and adverse effects of analgesics may have a great impact on physical functioning, psychological well-being, social activities, and quality of life (QoL).
Although etiologies of cancer pain vary, they can be generally managed with various pharmacological and non-pharmacological interventions (1). Although several guidelines for cancer pain control are available, including those published by the World Health Organization (2), National Comprehensive Cancer Network (3) and European Associations for Palliative Care (4), pain control may be ineffective and some patients still suffer from pain (5–7).
Recently, a pan-European survey of cancer-related pain prevalence found that among patients who had moderate-to-severe pain, 11% (67 of 573) were not receiving analgesia and the percentage was similar across gender (female patients: 11%; male patients: 12%). Consequently, 50% of patients believed that their healthcare professional did not consider their QoL as important, and 12% of them believed that their healthcare professional did not understand that pain was a problem (8).
Satisfaction with treatment and healthcare providers is important, as high satisfaction with care may influence the decision to seek care, change providers or medical plans, and treatment adherence (9). For patients with chronic diseases, particularly cancer, the patient–physician relationship is important for treatment adherence, and poor care for cancer pain may lead to poor satisfaction. Poor care for cancer pain may be linked to inadequate knowledge of pain treatment, inadequate pain assessment, inaccurate recognition of pain intensity, fear of adverse effects of strong opioids, and regulatory barriers to opioid prescription and dispensing. Moreover, dissatisfaction resulting from poor care may lead to poor patient–physician interactions, resulting in a stressful relationship.
Recently, Taiwanese healthcare organizations have sought to improve the quality of pain management. For example, the Health Promotion Administration developed guidelines for cancer pain management, including careful pain assessment and choice of appropriate therapeutic regimens.
The main objective of this survey was to explore pain management and satisfaction among patients with cancer pain at outpatient departments (OPDs) in various medical centers and regional hospitals to discover real-world satisfaction of pain management in Taiwan after the introduction of cancer-pain management guidelines. The secondary objectives were collecting information on patients’ QoL and prescriptions from physicians for management of pain at different intensities.
Materials and methods
Patient selection
Inclusion criteria were being at least 18 years of age, being diagnosed with cancer, having a prior OPD visit, and proving written informed consent. Exclusion criteria were having a diagnosed or suspected psychotic disorder and/or mental retardation and being unconscious. These inclusion and exclusion criteria have been described in detail in a previous study; the same population was used in the present study (10). After obtaining patients’ written informed consent at OPD, the questionnaire—on demographic data, current cancer status, pain control medication, characteristics and management of cancer pain, effect of pain on the physical and psychological functioning, pain intensity at the last visit, QoL, analgesic treatment compliance, and satisfaction with pain control, current treatment, and physician—was administered and guidance was provided to all patients. Disease status comprised ‘disease free’ for no evidence of disease recurrence after curative treatment; ‘relief’ to imply that the disease was stable involving partial or complete response to palliative treatments; and ‘deterioration’ to indicate disease progression. One visit was performed in this survey study.
Questionnaires and measures
The outcome questionnaire was based on the Short version of the Brief Pain Inventory. Patients rated their current pain intensity and worst, lowest and average levels of pain over the 24 h prior to testing using a numeric scale from 0 to 10, to represent ‘no pain’ and ‘pain as bad as you can imagine’, respectively. For information on satisfaction about pain control, all participants were asked at OPD by research assistants to answer the following questions: (1) How satisfied are you with the way your doctor has treated your pain? (2) Are you satisfied with pain control? Responses were scored on a 5-point scale with anchors ‘very dissatisfied,’ ‘not satisfied,’ ‘fair,’ ‘satisfied,’ and ‘very satisfied,’ as previously described in detail (10).
Since this is a clinical survey, only descriptive data were presented, and no formal statistical considerations were employed in determining sample size.
Statistical analysis
This survey was designed as a non-intervention therapeutic strategy. Data of eligible participants were used for data analysis, as described in detail (10). The results were summarized using descriptive statistics. For continuous variables, case number, means and standard deviations were presented. For categorical variables, the number and percentages of subjects in each class were presented. Logistic regression analyses were performed to evaluate whether the interference scale performed identically in the different analgesic ladders. The dependent variables were satisfaction with physicians and treatments in separate analyses. The independent variables were characteristics such as sex, age, primary cancer, use of analgesics, pain intensity and pain interference.
Ethics approval
The institutional review board at each hospital in Taiwan—these hospitals are E-Da Hospital, Kaohsiung, Taiwan; Mackay Memorial Hospital, Taipei, Taiwan; Kaohsiung Medical University Chung-Ho Memorial Hospital, Kaohsiung, Taiwan; Kaohsiung Chang Gung Memorial Hospital, Kaohsiung, Taiwan; National Taiwan University Hospital, Taipei, Taiwan; Linko Chang Gung Memorial Hospital, Taoyuan, Taiwan; Wan Fang Hospital, Taipei, Taiwan; Changhua Show-Chwan Memorial Hospital, Changhua, Taiwan; Changhua Christian Hospital, Changhua, Taiwan; Taipei Medical University Hospital, Taipei, Taiwan; Taichung Veterans General Hospital, Taipei, Taiwan; Chia-Yi Christian Hospital, Chiayi, Taiwan; Chiayi Chang Gung Memorial Hospital, Chiayi, Taiwan; China Medical University Hospital, Taichung, Taiwan—granted their approval for aggregated anonymous data to be analyzed and published, and the ethics committee approved this study.
Results
Patient characteristics and dispositions
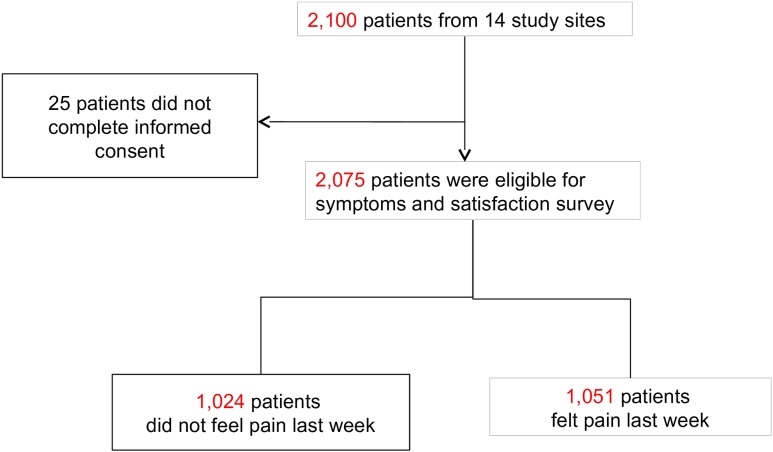
A total of 2075 patients were enrolled from 14 sites, of which 1051 reported pain within the week prior to the study. Sample derivation is shown in Fig. 1. Participants’ characteristics are presented in Table 1. Participants’ mean age was 57.47 ± 13.20 years. Breast, head and neck and gastrointestinal cancers—including colorectal cancer—were the most common cancers. More than 50% of subjects were relief from their illness at the time of evaluation.
Figure 1.
Flow diagram of patients included in this study.
Table 1.
Participants’ characteristics
| Variable | n (%) |
|---|---|
| Age, years (mean ± SD) | 57.47 ± 13.20 |
| Gender | |
| Male | 992 (47.81) |
| Female | 1083 (52.19) |
| Primary cancer | |
| Head and neck | 309 (14.89) |
| Gastrointestinal and colon-rectum | 394 (18.99) |
| Hepatobiliary and pancreas | 120 (5.78) |
| Breast | 527(25.40) |
| Lung and mediastinum | 184 (8.87) |
| Blood/lymphoma | 314 (15.18) |
| Gynecological and genitourinary | 133 (6.41) |
| Others | 93 (4.48) |
| Disease status | |
| Disease free | 407 (19.61) |
| Relief | 1226 (59.08) |
| Deterioration | 442 (21.30) |
| Pain caused by cancer | |
| Yes | 906 (43.66) |
| No | 564 (27.18) |
| Undetermined | 605 (29.16) |
| Pain caused by anti-cancer therapy | |
| Yes | 285 (13.73) |
| No | 1790 (86.27) |
SD, standard deviation.
Patient compliance
When disease status deteriorated, the need for analgesics increased, and pain-related sleep interruptions rose. A total of 768 patients reported needing analgesics in the week prior to testing. Regardless of patients’ disease status, more than half needed analgesics before their following treatment session. Higher chances of pain and sleep interruption were reported for participants with deterioration than for other participants (P = 0.026; Table 2).
Table 2.
Compliance by disease status
| Item | Disease status | |||
|---|---|---|---|---|
| Disease free (N = 407) | Relief (N = 1226) | Deterioration (N = 442) | P value | |
| Received analgesics during last week | 68 (16.71%) | 426 (34.75%) | 274 (61.99%) | <0.001 |
| Suffered from pain until next treatmenta | 36 (52.94%) | 231 (54.23%) | 178 (64.96%) | 0.013 |
| Sleep intervention due to receiving analgesicsa | 14 (20.59%) | 86 (20.19%) | 79 (28.83%) | 0.026 |
aCalculated for subjects who received analgesics during the week prior to testing.
Impact of pain on physical and psychological functioning
Patients with severe pain reported impaired physical and psychological functioning. As patients’ level of pain increased, their activity levels decreased, and their moods, interpersonal relationships, sleep and enjoyment of life worsened (P < 0.0001; Table 3).
Table 3.
The association between pain severity scores and functional interference
| Items | Pain average score | P value | ||
|---|---|---|---|---|
| <4 Mean ± SD | 4–7 Mean ± SD | >7 Mean ± SD | ||
| Physical function | ||||
| General activity | 2.0 ± 2.40 | 4.6 ± 2.97 | 6.8 ± 3.04 | <0.0001 |
| Walking ability | 1.8 ± 2.54 | 3.9 ± 3.12 | 5.5 ± 3.54 | <0.0001 |
| Normal work | 2.1 ± 2.74 | 4.4 ± 3.29 | 6.1 ± 3.62 | <0.0001 |
| Psychological function | ||||
| Mood | 2.1 ± 2.38 | 4.5 ± 2.81 | 6.3 ± 2.79 | <0.0001 |
| Relations with people | 1.6 ± 2.44 | 3.3 ± 3.07 | 4.7 ± 3.64 | <0.0001 |
| Sleep | 2.2 ± 2.63 | 4.3 ± 3.11 | 6.7 ± 3.30 | <0.0001 |
| Enjoyment of life | 2.2 ± 2.75 | 4.4 ± 3.03 | 6.9 ± 2.85 | <0.0001 |
SD, standard deviation.
Patients’ satisfaction with physician and treatment
Among patients who were satisfied by their treatment, they were almost 100% satisfied with their physicians. When patients believed that their treatments were only fair or were unsatisfactory, they tended to rate their physicians as fair or unsatisfactory. However, regardless of whether patients who still suffered from pain or not, most were satisfied with their physicians. Disease free participants had a higher rate of satisfaction than participants with relieved or deteriorated disease. Other variables—gender, pain etiology and metastasis—led to small differences in satisfaction (Table 4). Interestingly, among patients who complained of pain, only 10 patients felt dissatisfied/very dissatisfied with their treatment; most patients, even those with a pain score over three were satisfied with their treatment (Table 5).
Table 4.
Patients’ satisfaction with physician and treatment
| Item | Satisfaction with physician | P value | |
|---|---|---|---|
| Satisfied, N (%) | Fair/dissatisfied, N (%) | ||
| Satisfaction with treatment | |||
| Satisfied | 1623 (99.39) | 10 (0.61) | <0.0001 |
| Fair/dissatisfied | 53 (11.99) | 389 (88.01) | |
| Pain status | |||
| Pain | 831 (79.07) | 220 (20.93) | 0.0461 |
| Pain free | 845 (82.52) | 179 (17.48) | 0.1395 |
| Sex | |||
| Male | 788 (79.44) | 204 (20.56) | 0.5894 |
| Female | 888 (81.99) | 195 (18.01) | 0.0004 |
| Age (years) | |||
| ≦50 | 487 (81.99) | 107 (18.01) | 0.8254 |
| 51–60 | 527 (79.49) | 136 (20.51) | 0.0240 |
| 61–70 | 367 (79.96) | 92 (20.04) | 0.7705 |
| >70 | 295 (82.17) | 64 (17.83) | |
| Disease status | |||
| Disease free | 353 (86.73) | 54 (13.27) | |
| Relief | 987 (80.51) | 239 (19.49) | |
| Deterioration | 336 (76.02) | 106 (23.98) | |
| Metastasis | |||
| No | 842 (80.96) | 198 (19.04) | |
| Yes | 834 (80.58) | 201 (19.42) | |
| Pain caused by cancer | |||
| No | 471 (83.51) | 93 (16.49) | |
| Yes | 737 (81.35) | 169 (18.65) | |
| Unknown | 468 (77.36) | 137 (22.64) | |
| Pain caused by anti-cancer therapy | |||
| No | 1444 (80.67) | 346 (19.33) | |
| Yes | 232 (81.40) | 53 (18.60) | |
| Total | 1676 (80.77) | 399 (19.23) | |
Table 5.
Average pain score and satisfaction with treatment
| Satisfaction with treatment | Average pain score | ||
|---|---|---|---|
| <4, n (%) | 4–7, n (%) | >7, n (%) | |
| Very good, n = 269 | 148 (28.57) | 99 (21.57) | 22 (29.73) |
| Good, n = 543 | 278 (53.67) | 236 (51.42) | 29 (39.19) |
| Fair, n = 229 | 92 (17.76) | 114 (24.84) | 23 (31.08) |
| Dissatisfied, n = 9 | 0 (0.00) | 9 (1.96) | 0 (0.00) |
| Very dissatisfied, n = 1 | 0 (0.00) | 1 (0.22) | 0 (0.00) |
| Total, N = 1051 | 518 (49.29) | 459 (43.67) | 74 (7.04) |
Change in analgesic treatment and patients’ pain score
In order to understand whether doctors listened to their patients and changed analgesics according to the patients’ perceptions, we checked previous analgesics ladders for patients who complained of pain (n = 1 051). Of these, 518 patients (49.28%) had pain scores of less than four, among whom, 223 patients (43.05%) did not receive any analgesics. Among patients whose pain score was equal to or more than four, 160 patients (15.2%) did not receive any analgesics, including 20 patients whose pain score was more than 7 (Table 6).
Table 6.
Previous analgesic ladders by average pain score
| Previous treatment ladder (N = case number) | Pain average score | % of all patients who reported pain | ||
|---|---|---|---|---|
| <4, N (%) | 4–7, N (%) | >7, N (%) | ||
| None (N = 383) | 223 (43.05) | 140 (30.50) | 20 (27.03) | 36.4 |
| Adjuvant agents only (N = 54) | 36 (6.95) | 16 (3.49) | 2 (2.70) | 5.1 |
| Ladder 1 (N = 167) | 83 (16.02) | 73 (15.90) | 11 (14.86) | 15.9 |
| Ladder 2 (N = 244) | 107 (20.66) | 119 (25.93) | 18 (24.32) | 23.2 |
| Ladder 3 (N = 203) | 69 (13.32) | 111 (24.18) | 23 (31.08) | 19.3 |
| Total N = 1051 | 518 (49.28) | 459 (43.67) | 74 (7.04) | 100 |
In order to determine whether oncologists in Taiwan altered analgesic treatments when their patients complained of poor control of pain, we assessed changes in analgesics at their last visit against patients’ average pain score, we found that more than 70% of doctors did not change previously prescribed analgesics based on patients’ current pain status (Table 7).
Table 7.
Change of analgesics by average pain score
| Pain average score | Decreased ladder, N (%) | Unchanged, N (%) | Increased ladder, N (%) |
|---|---|---|---|
| ≤3 (N = 518) | 82 (15.83) | 389 (75.10) | 47 (9.07) |
| 4–7 (N = 459) | 56 (12.20) | 342 (74.51) | 61 (13.29) |
| >7 (N = 74) | 10 (13.51) | 52 (70.27) | 12 (16.22) |
| Total (N = 1051) | 148 (14.08) | 783 (74.50) | 120 (11.42) |
Discussion
The first published multi-center study on satisfaction with pain control among cancer patients in Taiwan reported that while 54% of patients from oncology OPDs reported pain, only 58% of these patients received analgesics. Nonetheless, most of the patients (64%) reported being satisfied or very satisfied with pain control (7). In the current prospective study, we attempted to investigate the status, characteristics and management of cancer pain after the introduction of guidelines, education and training programs.
As expected, before the week of study, patients with deteriorated status received more analgesics than patients who were at other disease status. However, more than one-third of patients who were at relief status still needed analgesics, and more than 50% experienced pain even if they had already received analgesics. Further, patients with deterioration reported more sleep interruptions (Table 2). This suggests that close monitoring, follow-ups and evaluations are important for patients receiving analgesics, especially those patients whose diseases are worsening. Even for disease-free or improving cases, disease- or treatment-related pain could lower QoL. Another issue is whether analgesic intake is regular or only when pain presents. Liang et al. found that adherence to prescribed opioids among Taiwanese oncology outpatients was 63.6% and 30.9% for around-the-clock and as-needed opioid analgesics, respectively (11). A better understanding of barriers to analgesic adherence and improvement efforts is needed.
Unexpectedly, although pain control was not good for most patients, a high percentage of patients experiencing pain still expressed satisfaction with their physicians (79.07%) compared with those who gave fair/dissatisfied ratings (20.93%, Table 4). Beck et al. have also reported the coexistence of high levels of satisfaction and pain: 22% of the advanced-cancer group reported severe pain frequently or constantly and 83% of the advanced-cancer group reported being very satisfied or satisfied with their pain management (12). In another study of 72 surgical patients, the mean severest pain score in the previous 24 h was 7.56. More than 70% reported a score of seven or greater, but more than 70% of the patients also reported that they were very satisfied (20%) or satisfied (51%) with their pain relief (13). Nonetheless, dissatisfied patients showed a significantly higher average pain level compared with satisfied patients (9). Breivik found that average or poor pain control may interfere with patients’ QoL (8). This paradox of high pain and high satisfaction could mislead physicians in their assessments, potentially leading to under-treatment of pain.
Regarding satisfaction with physicians, a high percentage of patients at different pain intensities were satisfied with their treatment, but the number of patients who were dissatisfied or rated their treatment as fair increased with increases in pain scores (Table 5).
Moreover, although there were 1051 patients in our study (50.65% of all patients) who reported pain within the past week, not all of them had good control of pain; 160 patients (15.2% of all patients) with a pain score of more than three did not receive analgesic or adjuvant treatment (Table 6). This is consistent with Breivik’s pan-European survey wherein 11% of all patients did not receive any analgesic medication for their pain. These similar results indicate that even after years of education and the introduction of guidelines in Taiwan, assessments are often not adequate and frequently result in suboptimal treatment and outcomes. Moreover, such treatment issues are rather universal (6,8,14,15), they occur more commonly for elderly patients (15) and minority (16). Moreover, 40% of all cancer patients lack the resources to effectively manage their pain (17). Thus, both patients and doctors should be considered responsible for inadequate treatment.
For example, patients may not report their pain regularly; may be afraid of side effects of analgesics, especially opioids, of addiction, and of distracting the physician from treating the underlying medical condition (18); or may believe that pain is an inevitable consequence of cancer (19). Thus, information given to doctors will be insufficient for making correct judgments.
On the other hand, doctors fail to appreciate the intensity of pain may lead to poor pain control. Doctors should be able to evaluate current disease status and the extent and severity of cancer-related pain. Communication is important for patient-centered care and addressing misconceptions, fears, or uncertainty. Doctors’ empathy, effective communication, responsiveness to patients’ opinions and perceptions, and inclusion of patients in treatment are associated with better treatment outcomes (20).
Why doctors cannot well adjust analgesics according to the patient’s experience of pain? It might also be because of a lack of familiarity with analgesics, fewer choices of analgesics, lack of empathy, fear of addiction or dependence, and regulatory barriers to opioid prescription and dispensing. Thus, the barriers to pain control can also stem from physicians.
The poor improvement in the control of cancer pain might also come from high pain intensity, high comorbidity, and low treatment motivation. The consequences of inappropriate pain assessments and poor communication between patients and physicians may explain why 70% of the physicians in our study did not change analgesics for patients whose previous pain score was greater than three, and why more than 10% of doctors reduced analgesic treatment strength for patients who still had severe pain (Table 7). Unfortunately, most physicians in Taiwan who prescribe pain medications are overworked at OPD and do not have enough time to administer lengthy assessment tools to determine their patients’ adherence to analgesics. Physicians need to assign time to discuss cancer pain with their patients, individualize pain management medications, and improve each patient’s perception of control, thereby improving self-efficacy in health and pain management (21).
High satisfaction with care may influence decisions to seek care, change providers or medical plans, and adhere to prescribe treatment plans. Several factors may influence patients’ satisfaction with pain control, such as the stage of cancer, communication between patients and healthcare providers, management of side effects, efficacy of medications, and support from family and society (12). In Sherwood et al.’s study on 241 in-hospital patients, including those with postoperative pain and cancer, four distinct themes affecting patient satisfaction were identified: pain experience, view of providers, pain management experiences, and pain management outcomes. High satisfaction was directly linked to the doctor’s or nurse’s ability to identify pain management as an important goal and to decreases in pain over the previous year (22).
In our study, we confirmed that pain could influence patients’ QoL, as poor pain control was linked to poor sleep quality and poorer daily functioning. Although we found that most cancer patients at OPDs were satisfied with their physicians, this did not mean that patients had good control of pain. On the contrary, despite the years of education on cancer pain management, more than 50% of patients still did not have adequate control of their pain, and most physicians did not change or increase analgesics for pain alleviation, suggesting that educational efforts should involve both healthcare providers and patients, and the content should include the nature and management of cancer pain; the side effects from different types of management—especially analgesics—and ways to handle them; and development of empathy, interaction, and communication skills through palliative care training (23). Thus, physicians must listen to patients’ descriptions to better investigate the causes of pain and provide effective treatments.
In our study, 20% of cancer survivors reported pain at oncological OPDs. They require different supports because of their long lifespans, implying that pain control is critical for their QoL.
Conclusion
Although more than 75% of the OPD patients with cancer pain in this study reported satisfaction with their physician and pain management, most physicians did not change the prescribed analgesics according to patients’ current pain status. In order to achieve good control over cancer pain and consequently, satisfaction, strategies to ensure adequate reporting, good doctor–patient communication, thorough assessments of disease status, and familiarity with analgesics are essential. Further, cancer pain control evaluations should be conducted regularly.
Acknowledgments
We would like to thank Johnson & Johnson, Taiwan for providing a grant to support this study.
Authors’ contributions
K.M.R. undertook data collection, data analysis and drafted the manuscript. J.S.C., H.B.W. and S.F.L. undertook data analysis and interpretation. J.M.C., M.L.H., C.J.W., C.J.T., W.L.H., Y.C.L. and C.H.C. undertook data collection, data interpretation and edited the manuscript. R.K.H. contributed to study conception and design, data interpretation and edited the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by a program grant from Johnson and Johnson.
Conflict of interest statement
The authors declare that there are no competing interests.
References
- 1. Bruera E, Kim HN. Cancer pain. JAMA 2003;290:2476–9. [DOI] [PubMed] [Google Scholar]
- 2. Zech DF, Grond S, Lynch J, Hertel D, Lehmann KA. Validation of World Health Organization Guidelines for cancer pain relief: a 10-year prospective study. Pain 1995;63:65–76. [DOI] [PubMed] [Google Scholar]
- 3. Janjan N. Improving cancer pain control with NCCN guideline-based analgesic administration: a patient-centered outcome. J Natnl Compr Canc Netw 2014;12:1243–9. [DOI] [PubMed] [Google Scholar]
- 4. Caraceni A, Hanks G, Kaasa S, et al. . Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC. Lancet Oncol 2012;13:e58–68. [DOI] [PubMed] [Google Scholar]
- 5. Von Roenn JH, Cleeland CS, Gonin R, Hatfield AK, Pandya KJ. Physician attitudes and practice in cancer pain management: a survey from the Eastern Cooperative Oncology Group. Ann Intern Med 1993;119:121–6. [DOI] [PubMed] [Google Scholar]
- 6. Pargeon KL, Hailey BJ. Barriers to effective cancer pain management: a review of the literature. J Pain Symptom Manage 1999;18:358–68. [DOI] [PubMed] [Google Scholar]
- 7. Hsieh RK. Pain control in Taiwanese patients with cancer: a multicenter, patient-oriented survey. J Formosan Medical Assoc [Taiwan yi zhi] 2005;104:913–9. [PubMed] [Google Scholar]
- 8. Breivik H, Cherny N, Collett B, et al. . Cancer-related pain: a pan-European survey of prevalence, treatment, and patient attitudes. Ann Oncol 2009;20:1420–33. [DOI] [PubMed] [Google Scholar]
- 9. McNeill JA, Sherwood GD, Starck PL, Thompson CJ. Assessing clinical outcomes: patient satisfaction with pain management. J Pain Symptom Manage 1998;16:29–40. [DOI] [PubMed] [Google Scholar]
- 10. Rau KM, Chen JS, Wu HB, et al. . The impact of pain control on physical and psychiatric functions of cancer patients: a nation-wide survey in Taiwan. Jpn J Clin Oncol 2015;45:1042–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liang SY, Wu SF, Tsay SL, Wang TJ, Tung HH. Prescribed opioids adherence among Taiwanese oncology outpatients. Pain Manag Nurs 2013;14:155–60. [DOI] [PubMed] [Google Scholar]
- 12. Beck SL, Towsley GL, Berry PH, Lindau K, Field RB, Jensen S. Core aspects of satisfaction with pain management: cancer patients’ perspectives. J Pain Symptom Manage 2010;39:100–15. [DOI] [PubMed] [Google Scholar]
- 13. Miaskowski C, Nichols R, Brody R, Synold T. Assessment of patient satisfaction utilizing the American Pain Society’s Quality Assurance Standards on acute and cancer-related pain. J Pain Symptom Manage 1994;9:5–11. [DOI] [PubMed] [Google Scholar]
- 14. Cleeland CS, Gonin R, Hatfield AK, et al. . Pain and its treatment in outpatients with metastatic cancer. New Engl J Med 1994;330:592–6. [DOI] [PubMed] [Google Scholar]
- 15. Cleeland CS. Undertreatment of cancer pain in elderly patients. JAMA 1998;279:1914–5. [DOI] [PubMed] [Google Scholar]
- 16. Cleeland CS, Gonin R, Baez L, Loehrer P, Pandya KJ. Pain and treatment of pain in minority patients with cancer. The Eastern Cooperative Oncology Group minority outpatient pain study. Ann Int Med 1997;127:813–6. [DOI] [PubMed] [Google Scholar]
- 17. Koller A, Miaskowski C, De Geest S, Opitz O, Spichiger E. Results of a randomized controlled pilot study of a self-management intervention for cancer pain. Eur J Oncol Nurs 2013;17:284–91. [DOI] [PubMed] [Google Scholar]
- 18. Narayan MC. Culture’s effects on pain assessment and management. Am J Nurs 2010;110:38–47. quiz 48-39. [DOI] [PubMed] [Google Scholar]
- 19. Ward SE, Goldberg N, Miller-McCauley V, et al. . Patient-related barriers to management of cancer pain. Pain 1993;52:319–24. [DOI] [PubMed] [Google Scholar]
- 20. Farin E, Gramm L, Schmidt E. The patient-physician relationship in patients with chronic low back pain as a predictor of outcomes after rehabilitation. J Behav Med 2013;36:246–58. [DOI] [PubMed] [Google Scholar]
- 21. Baker TA, O’Connor ML, Krok JL. Experience and knowledge of pain management in patients receiving outpatient cancer treatment: what do older adults really know about their cancer pain? Pain Med 2014;15:52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sherwood G, Adams-McNeill J, Starck PL, Nieto B, Thompson CJ. Qualitative assessment of hospitalized patients’ satisfaction with pain management. Res Nurs Health 2000;23:486–95. [DOI] [PubMed] [Google Scholar]
- 23. Silvoniemi M, Vasankari T, Vahlberg T, Vuorinen E, Clemens KE, Salminen E. Physicians’ self-assessment of cancer pain treatment skills: more training required. Support Care Canc 2012;20:2747–53. [DOI] [PubMed] [Google Scholar]