The high rates of breast cancer mortality reported in low‐ and middle‐income countries are mainly due to diagnosis at an advanced stage of disease and barriers to accessing standard treatment. In Mexico, breast cancer is the most common cause of cancer‐related mortality among women. This study explores the factors associated with delays in the patient and diagnosis intervals of care, shedding light on the tailored interventions that could lead to earlier diagnosis and improve mortality rates.
Keywords: Delays, Intervals of care, Breast cancer, Early diagnosis, Barriers
Abstract
Background.
Most breast cancer patients in low‐ and middle‐income settings are diagnosed at advanced stages due to lengthy intervals of care. This study aimed to understand the mechanisms through which delays occur in the patient interval and diagnosis interval of care.
Materials and Methods.
We conducted a cross‐sectional survey including 886 patients referred to four major public cancer hospitals in Mexico City. Based in a conceptual model of help‐seeking behavior, a path analysis strategy was used to identify the relationships between explanatory factors of patient delay and diagnosis delay.
Results.
The patient and the diagnosis intervals were greater than 3 months in 20% and 65% of participants, respectively. We present explanatory models for each interval and the interrelationship between the associated factors. The patient interval was longer among women who were single, interpreted their symptoms as not worrisome, concealed symptoms, and perceived a lack of financial resources and the difficulty of missing a day of work as barriers to seek care. These barriers were more commonly perceived among patients who were younger, had lower socioeconomic status, and lived outside of Mexico City. The diagnosis interval was longer among those who used several different health services prior to the cancer hospital and perceived medical errors in these services. More health services were used among those who perceived errors and long waiting times for appointments, and who first consulted private services.
Conclusion.
Our findings support the relevance of strengthening early cancer diagnosis strategies, especially the improvement of quality of primary care and expedited referral routes to cancer services.
Implications for Practice.
This study's findings suggest that policy in low‐ and middle‐income countries (LMICs) should be directed toward reducing delays in diagnosis, before the implementation of mammography screening programs. The results suggest several factors susceptible to early diagnosis interventions. To reduce patient delays, the usually proposed intervention of awareness promotion could better work in LMIC contexts if the message goes beyond the advertising of screening mammography to encourage the recognition of potential cancer symptoms and sharing of symptoms with significant others. To reduce diagnosis delay, efforts should focus on strengthening the quality of public primary care services and improving referral routes to cancer care centers.
Introduction
The high rates of breast cancer (BC) mortality reported in low‐ and middle‐income countries (LMICs) are mainly due to diagnosis at advanced stages of disease and barriers to accessing standard treatment [1]. Advanced disease stage and low survival rates have been shown to be associated with lengthy intervals of care [2], [3], [4].
The total interval of care, defined as the time between symptom discovery and the beginning of cancer treatment, has been divided into several more specific intervals [5]. The patient interval starts with symptom discovery and ends with the first medical consultation. The health system interval begins with the first medical visit and concludes with the beginning of cancer treatment. This interval has been further classified into the diagnosis interval, defined as the time between the first medical consultation and the histopathologic confirmation of cancer, and the treatment interval, defined as the time between diagnosis confirmation and the beginning of oncologic treatment.
In Mexico, BC is the most common cause of cancer‐related mortality among women [6]. Although data on the clinical stages of breast cancer are scarce and are not nationally representative, existing studies have reported that 45%–48% of cases are diagnosed in stages III and IV, and only between 10% and 20% in stages 0 and I [7], [8]. In a previous study, both patient delay and health system delay were found to be independently associated with increased probability of advanced BC among Mexican women [9]. The present study aimed to explore the mechanisms through which patient characteristics and health system barriers influence patient delay and diagnosis delay among Mexican patients seeking care for breast symptoms.
The only factors that have been found to be strongly related with patient delay in a 1999 meta‐analysis are the patient's single marital status and advanced age [10]. Subsequent studies have shown contradictory findings regarding the association between patient delays and low education, residence in rural areas, low socioeconomic level, lack of health insurance, lack of cancer knowledge, previous experiences with family members or friends who had cancer, fear, denial, low cancer risk perception, breast symptoms other than a lump, and not talking to anyone about symptoms [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29]. As for diagnosis delay, the only strong predictors in the 1999 meta‐analysis were the patient's young age and presentation with symptoms other than a lump. Although in recent years there has been more interest in understanding diagnosis delay, it has been much less studied than patient delay. Few studies have shown an association with diagnosis delay of low socioeconomic status, rural residence, lack of social support, lack of screening participation, patients’ mistrust in health services, breast symptoms other than a lump, and medical errors [21], [23], [29], [30]. Most studies have been done in high‐income countries and focused on finding associations between sociodemographic factors and lengthy time intervals.
In contrast to previous studies that only describe factors associated individually with the delay intervals, we present two separate explanatory models that, in addition to the relation between each analyzed factor and the time interval, include the interrelationship between the different factors associated to patient delay and diagnosis delay. Our findings show the pathways through which these factors influence each type of delay, thus providing more insight into the kind of tailored interventions that could be more effective in reducing time intervals and, consequently, improving stages at diagnosis and mortality rates.
Materials and Methods
Design
Details of the study design have been reported in a previous publication [9]. We conducted a cross‐sectional study including patients who were newly referred with probable BC to four of the largest public cancer hospitals in Mexico City (MC): the Mexican National Cancer Institute (INCAN), General Hospital of Mexico (HGM), Mexican Social Security Institute (IMSS) National Hospital of Oncology, and IMSS Hospital of Gynecology and Obstetrics number four. The study protocol was approved by the research and ethics review boards of the participating hospitals, and informed consent was obtained from all participants.
Setting
The INCAN and HGM fall under the purview of the Ministry of Health (MoH) and offer BC services without cost to uninsured patients and those covered by Seguro Popular, which is a federal program that permits its affiliates to benefit from an explicit list of health interventions. The IMSS Oncology and Gynecology Hospitals offer medical services to BC patients covered by social security health insurance. According to the most recently conducted National Survey of Health and Nutrition (2016), 43.5% of the Mexican population is covered by Seguro Popular, 32.9% is covered by IMSS, and 13.4% of the population remains uninsured. The rest of the population (10.3%) is privately insured (0.6%) or insured through public schemes offered by other entities [31].
Participants
Overall, 1,497 patients first sought care at the breast tumor departments of the participating hospitals during the study period. We excluded those who exhibited the following characteristics: (a) had a personal history of cancer (43/1,497, 2.9%); (b) had a benign breast condition under medical surveillance (151/1,497, 10.1%); (c) began cancer treatment before arrival to the institution (234/1,497, 15.6%); (d) were not willing to participate (60/1,069, 5.6%); (e) had intellectual or hearing impairments, or did not speak Spanish (46/1,069, 4.3%); (f) could not recall the dates necessary for estimation of the examined intervals (5/963, 0.5%); or (g) were outliers, which was defined as having a total interval of care greater than 50 months (72/963, 7.5%).
Measures of Time Intervals
The conceptual and operational definitions of the time intervals used in this study were in line with those of most previous studies on BC care delay and the recommendations of a consensus statement [5].
Patient interval: time between the identification of the condition and the first medical consultation.
Diagnosis interval: time from the first medical consultation to the first medical note reporting histopathologic confirmation of cancer.
Data Collection
A validated questionnaire was used to retrieve the dates of the identification of a health problem and first medical consultation; the manner in which patients first identified the breast condition (either through symptom discovery or screening); symptom interpretation; perceived barriers to seeking medical care; medical services use before arrival to the cancer hospital; perceived barriers to seeking timely care; sociodemographic information; and BC screening knowledge and practices [32]. The questionnaire was administered via face‐to‐face interviews at the participating hospitals. To minimize the probability of recall bias, study participants were asked to remember dates using the aid of a calendar. Information regarding each patient's final diagnosis and date of diagnostic confirmation was extracted from the patients’ hospital records.
Statistical Analysis
Descriptive statistics were estimated for all variables. Fisher's exact test was used to assess differences in descriptive variables by final diagnosis (cancer vs. benign breast condition). Kaplan‐Meier curves were generated to examine the association between an aggregated patient and diagnosis interval variable and final diagnosis. Diagnostic confirmation was defined as the censoring event, and a Cox regression model was built to identify significant differences in interval length between the two different groups.
A principal component analysis was performed to consolidate most of the available socioeconomic data into a single index variable. A detailed description of this process is available in supplemental online Appendix 1.
Finally, a path analysis (PA) was performed to identify explanatory factors for patient delay and diagnosis delay in a multivariate model. PA is helpful to learn how much of the relationship between two or more dependent variables is accounted for by intervening or mediating factors. It is a special case of Structural Equation Modeling (SEMs), where a complex system of equations involving a set of responses and controls is investigated with the objective of disentangling causal links [33], [34]. Unlike more general SEMs, path analysis only involves observed variables. Latent variables do not exist. Control and response variables may be correlated among each other but are uncorrelated with the error term. Moreover, error terms across equations are uncorrelated. This implies that a dependent variable in one equation may serve as control in another equation without statistically complicating matters. The method is akin to multivariate regression and variance decomposition analyses. Each equation can be estimated by taking into account the nature of the dependent variable: logit regression for binary responses, ordered probit for ordinal responses, and linear multivariate regressions for continuous responses. Path analysis accepts a graphic representation commonly known as Path Diagrams, where straight unidirectional arrows represent causal relationships.
We can clarify the dynamics of the path analysis with a short example. In this case, we are interested in identifying the main determinants of diagnosis delay (DD), so we run an equation in which DD is the dependent variable:
Number of health services consulted was one of the most important variables that explain DD. It now becomes the dependent variable that we try to explain with the following equation:
The analysis keeps going using the same logic, until all relevant variables and the relationships between them are explained. The inclusion and order of variables in our PA was based in a conceptual model proposed in a previous study of help‐seeking behavior of women with breast cancer [35]. Tables 2 and 3 present the results of the equations that explain the most relevant variables of our analyses. Figures 2 and 3 are the path diagrams derived from these analyses.
Results
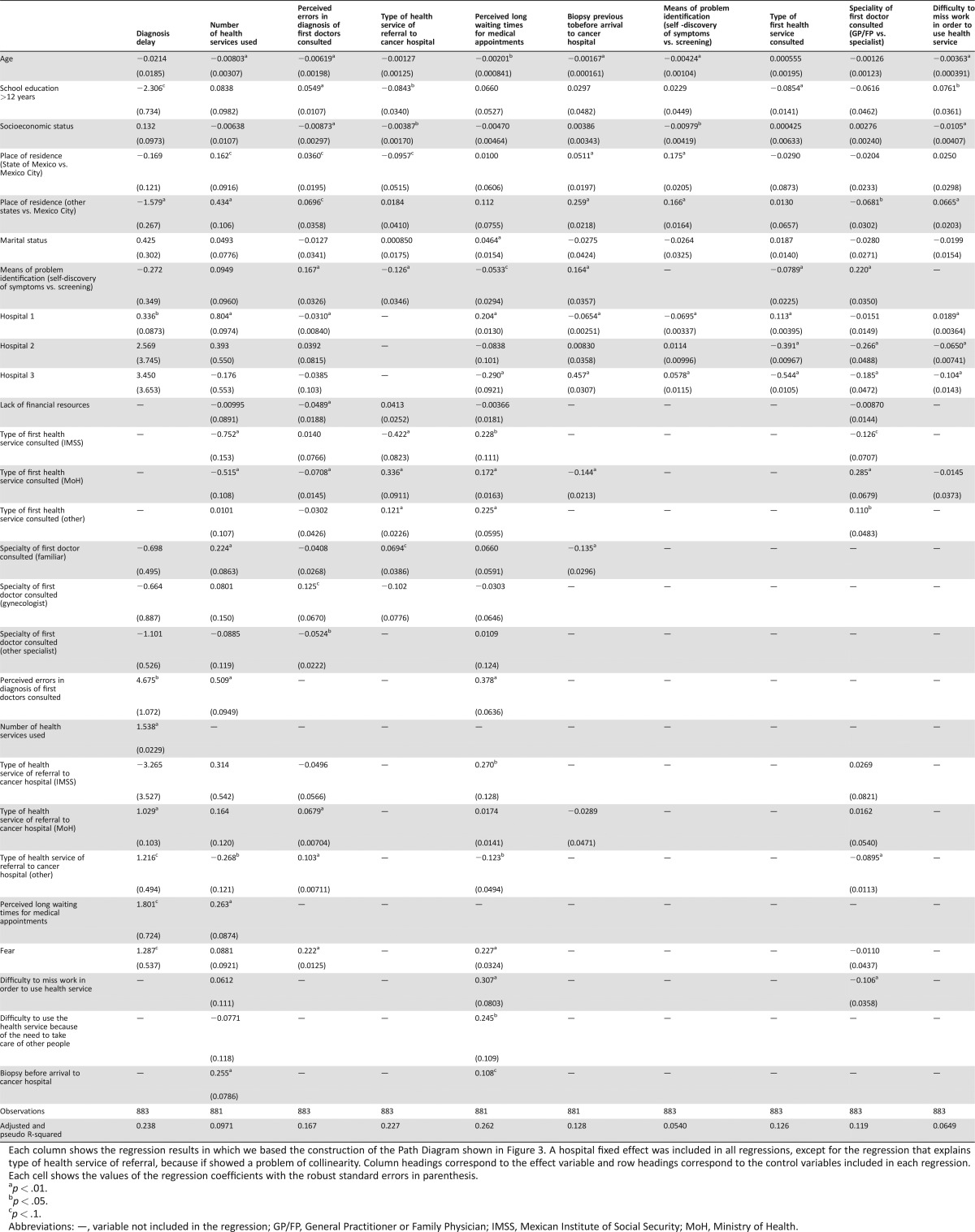
Table 1 compares some of the basic characteristics of the 886 participants. Their mean age was 50.9 years (standard deviation = 13.7). A diagnosis of a benign breast condition was ultimately confirmed in 289/886 (32.6%) patients. Almost 85% (504/597) of cancer patients discovered their condition through symptoms, whereas 43% (123/289) of patients with a benign diagnosis identified their condition through screening (Table 1). At diagnosis, only 32.75% of BC patients were in early stages (I and IIA).
Table 1. Demographic and disease information.
Values are n (%).
p values were estimated with Fisher's exact test to assess differences between patients finally diagnosed with cancer and those with benign conditions.
The minimum wage in Mexico is approximately $5 USD per day.
First symptom is reported for the 670 patients who identified the problem through symptoms.
Abbreviations: CBE, clinical breast exam; IMSS, Mexican Institute of Social Security; USD, U.S. dollar.
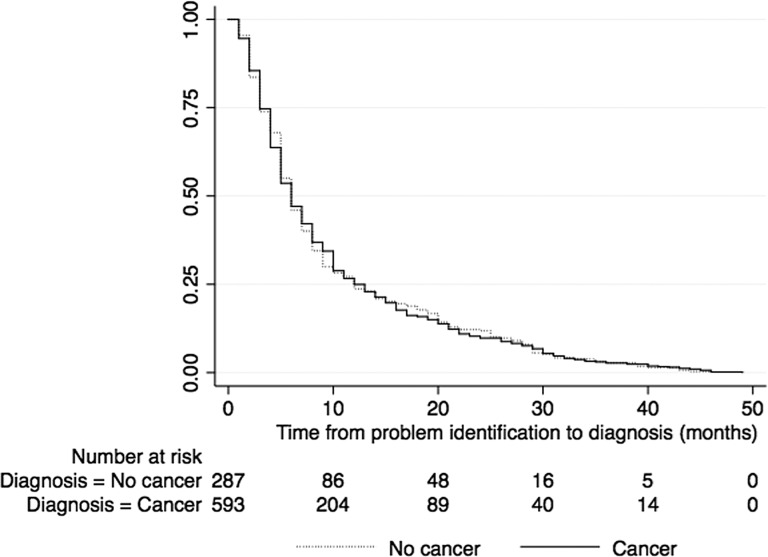
The entire patient sample was included in the multivariate analysis because no significant differences between cancer patients and those with benign conditions were identified in the interval from condition identification to diagnosis (hazard ratio = 0.99, p = .94; Fig. 1).
Figure 1.
Kaplan‐Meier curves of interval from problem identification to diagnosis stratified by final diagnosis.
The patient interval had a median duration of 10 days; 30% of the participants delayed seeking care for more than 1 month after symptom discovery and 20% did so for more than 3 months. The diagnosis interval had a median duration of 128 days (approximately 4 months); this interval was longer than 3 and 6 months in 65% and 36% of our participants, respectively.
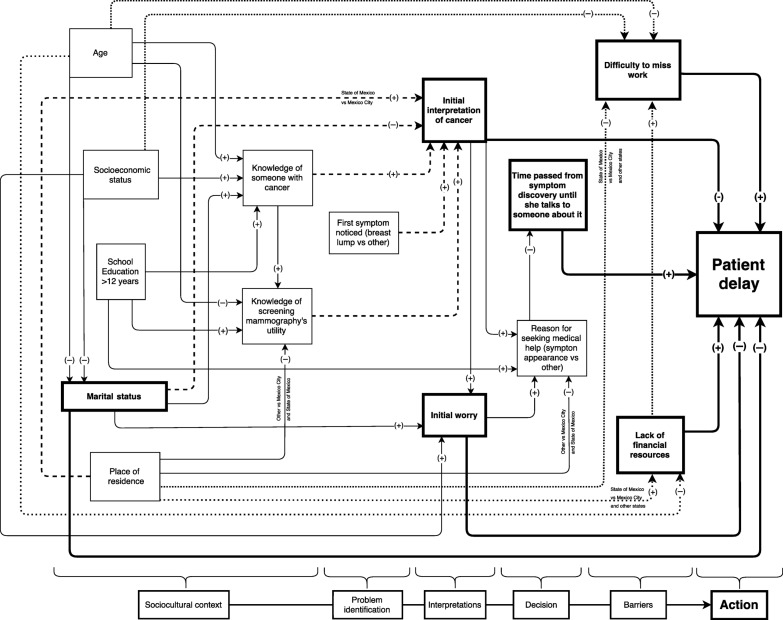
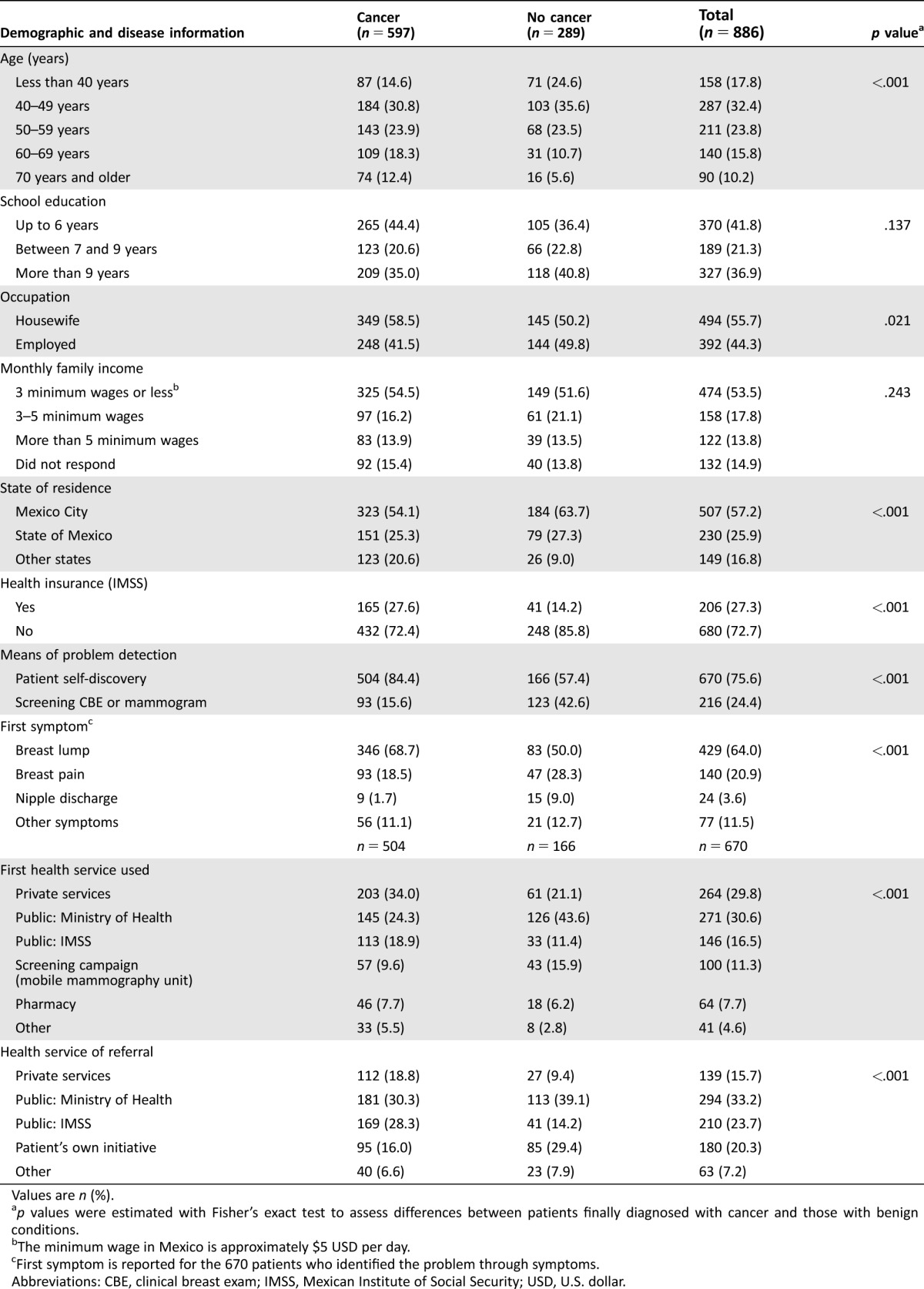
When controlling for other variables, the patient interval was significantly longer among women who were not in a relationship, did not initially interpret their symptoms as suggestive of cancer, did not initially think their symptoms were worrisome, and concealed their symptoms for an extended length of time; perceived barriers to seeking care included a lack of financial resources and the difficulty of missing a day of work (Fig. 2; Table 2).
Figure 2.
Path analysis of proposed mechanisms for patient delay. This diagram depicts the proposed causal mechanisms of patient delay. Each arrow reflects the presence of a statistically significant relationship between two variables after controlling for other confounders in multivariate analyses. The multivariate regression models selected for each explanatory variable in the diagram are presented in Table 2. The signs on the arrows reflect whether a positive (+) or negative (−) association was identified between the variables. Variables that were significant in the multivariate analysis of factors impacting patient delay are highlighted in boxes and arrows with thicker lines. At the bottom, a schematic of the conceptual model that guided the inclusion of variables and order of variable inclusion in the path analysis of patient delay is presented.
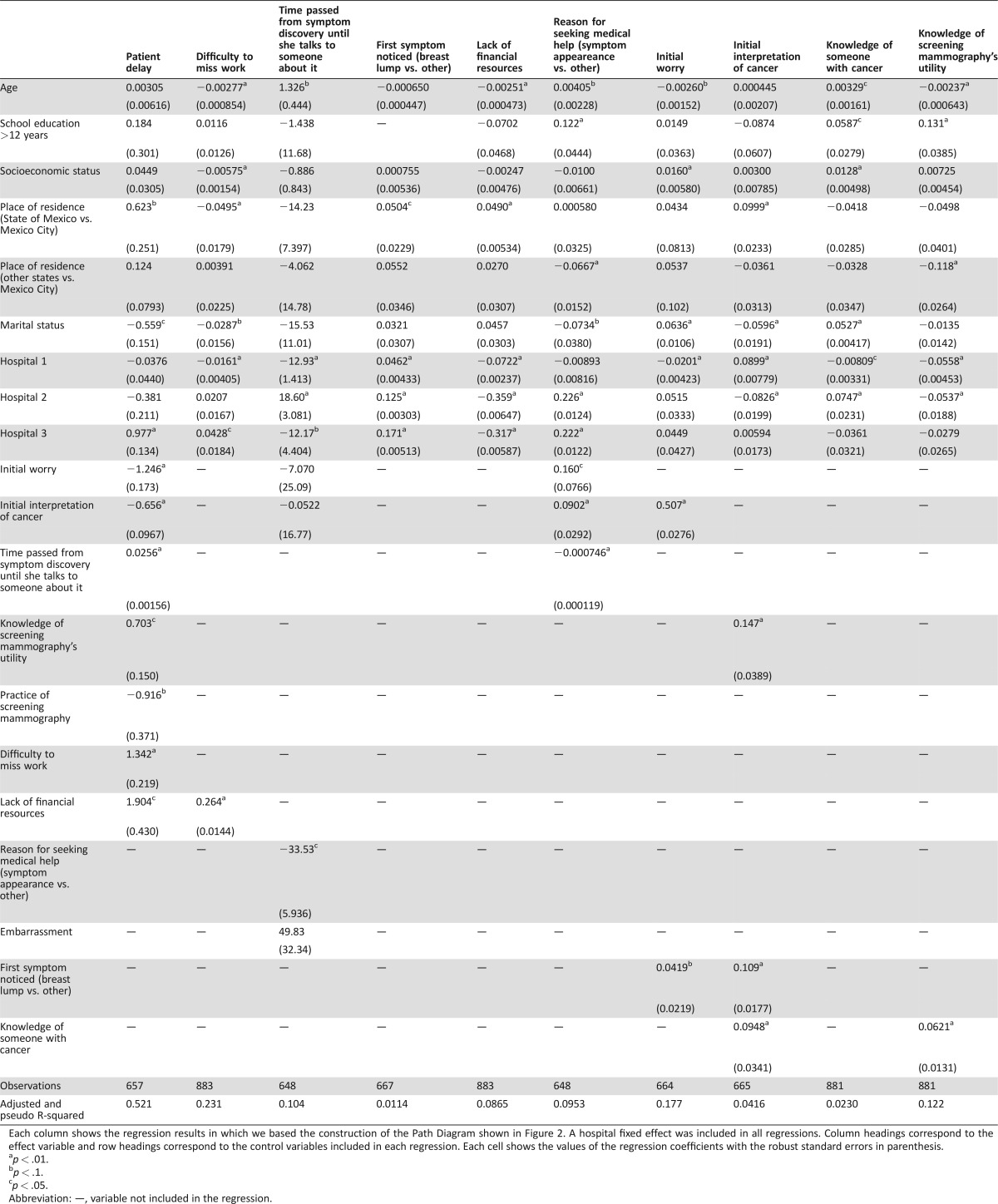
Table 2. Selected regressions for the path analysis of patient delay.
Each column shows the regression results in which we based the construction of the Path Diagram shown in Figure 2. A hospital fixed effect was included in all regressions. Column headings correspond to the effect variable and row headings correspond to the control variables included in each regression. Each cell shows the values of the regression coefficients with the robust standard errors in parenthesis.
p < .01.
p < .1.
p < .05.
Abbreviation: —, variable not included in the regression.
The PA revealed the potential relevance of other variables as mediators in the aforementioned relationships. For example, the initial symptom interpretation as a possible cancer was more common among patients who presented with a breast lump (vs. other symptoms), knew a person who had cancer, and knew the purpose of screening mammograms. Moderate‐to‐high levels of initial worry (vs. none or low) were more commonly identified among patients with higher socioeconomic status (SES), those who were in a relationship, and those who initially interpreted their symptoms as a possible cancer.
Lacking the financial resources necessary for health‐service utilization was more commonly perceived as a barrier to seeking care by younger patients and those who live in other states versus MC and State of Mexico (SoM). Perceived difficulty in missing work was also associated with a perceived lack of financial resources, young age, low SES, and residence in states outside of MC.
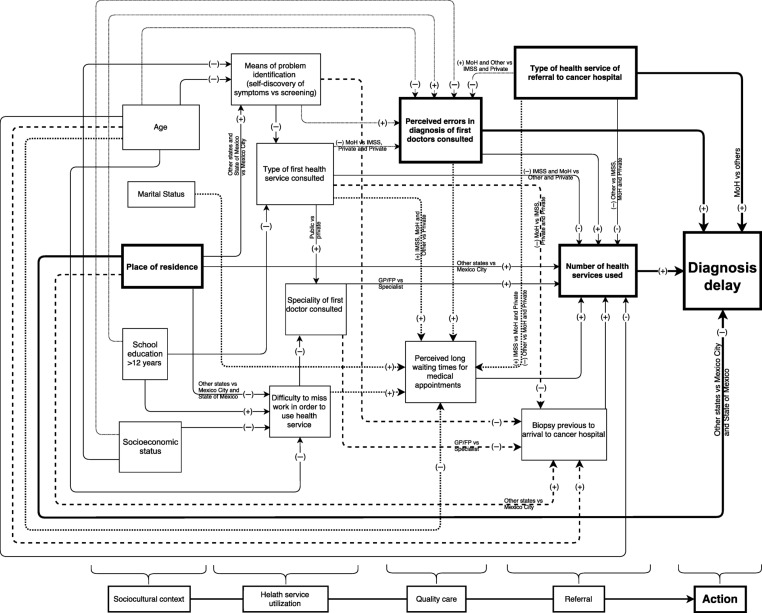
The median number of different health services used by the patients prior to their arrival to the cancer hospital was three (interquartile range = 2–3). The diagnosis interval was significantly longer among women who used more different types of health services prior to cancer institution arrival, perceived medical errors to have occurred in these services, were referred to the cancer institution by a health service dependant of the MoH (vs. IMSS and private services), and resided in states other than MC and SoM (Fig. 3; Table 3).
Figure 3.
Path analysis of proposed mechanisms for diagnosis delay. This diagram depicts the proposed causal mechanisms of diagnosis delay. Each arrow reflects the presence of a statistically significant relationship between two variables after controlling for other confounders in multivariate analyses. The multivariate regression models selected for each explanatory variable in the diagram are presented in Table 3. The signs on the arrows reflect whether a positive (+) or negative (−) association was identified between the variables. Variables that were significant in the multivariate analysis of factors impacting diagnosis delay are highlighted in boxes and arrows with thicker lines. At the bottom, a schematic of the conceptual model that guided the inclusion of variables and order of variable inclusion in the path analysis of patient delay is presented.
Abbreviations: GP/FP, General practitioner or Family physician; IMSS, Mexican Social Security Institute; MoH, Ministry of Health.
Table 3. Selected regressions for the path analysis of diagnosis delay.
Each column shows the regression results in which we based the construction of the Path Diagram shown in Figure 3. A hospital fixed effect was included in all regressions, except for the regression that explains type of health service of referral, because if showed a problem of collinearity. Column headings correspond to the effect variable and row headings correspond to the control variables included in each regression. Each cell shows the values of the regression coefficients with the robust standard errors in parenthesis.
p < .01.
p < .05.
p < .1.
Abbreviations: —, variable not included in the regression; GP/FP, General Practitioner or Family Physician; IMSS, Mexican Institute of Social Security; MoH, Ministry of Health.
Moreover, the number of health services used was directly associated with perceived errors in diagnosis, the perception of long waiting times for medical appointments, first consulting a primary care doctor (vs. a specialist), living in a state other than MC or SoM, and having had a biopsy taken before arrival to the cancer institution (Fig. 3).
Perceiving diagnostic errors to have occurred was more common among women who were younger, had higher education, identified the problem through symptoms (vs. screening), and first used private services. It is not possible to determine with certainty whether these perceived errors were in fact medical errors, as data were collected through patient interviews. However, we compared each patient's final diagnosis (obtained from patient medical files) with their response to another questionnaire item: the diagnosis that patients understood after the first medical consultation. We have these data for only 701/886 (79.1%) patients, as the remaining 20.9% stated that the first doctor did not explain anything or that they did not understand the doctor's explanation. Overall, 199/482 (41.2%) cancer patients reported that the first doctor they consulted had given them a benign diagnosis (Table 4).
Table 4. Final diagnosis in comparison with initial diagnostic impression.
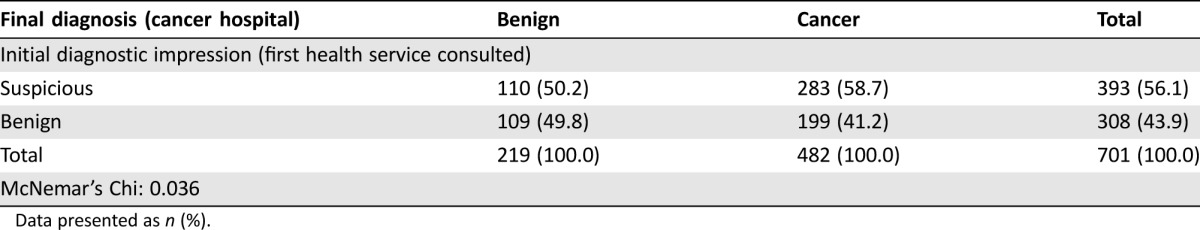
Data presented as n (%).
Discussion
Our findings show the pathways through which different factors influence delay, thus providing more insight into the kind of tailored interventions that could be more effective in reducing time intervals and, consequently, improving stages at diagnosis and mortality rates of breast cancer in our country. The most relevant factors that determine the patient interval (i.e., the time a patient takes to seek medical care) are related with BC awareness, her social network, and financial difficulties in seeking care. Regarding the diagnosis interval, the most relevant factors that resulted from our analyses have to do with access and quality of care. We will now discuss these findings in comparison with previous findings reported in the literature and in the Mexican context.
The known relevance of breast cancer awareness in the patients’ medical‐seeking behavior is confirmed in our findings. The association identified between the patients’ initial interpretations of breast symptoms as “not cancer” and “not worrisome” and postponement of seeking care has been described in previous studies [21], [22], [26], [30]. The results of the PA reveal that these initial interpretations are associated with higher cancer awareness indicators like knowing someone who had cancer, knowledge of mammography, and knowledge of BC symptoms.
In addition to BC awareness, the role of the patient's social network is very relevant in the decision of seeking care. Our study found that the longer a patient concealed her symptoms from others, the longer she delayed seeking medical care. This has also been reported in a few other studies [10], [36]. Speaking about symptoms to significant others helps affected individuals to face and make sense of the problem and decide what courses of action to take [37].
Finally, financial circumstances are very important in the patient's decision and action of seeking care. Previous studies have also reported financial difficulties and low SES to be barriers to the seeking of timely medical care [19], [22], [27]. Our results show that difficulty to miss work was more common among younger women and those of low socioeconomic status. These problems are inherent to people without health insurance (13.5% of the Mexican population) and those covered by Seguro Popular (43.5% of the population), as they cannot justify taking medical leave from their jobs (usually located in the informal sector). Furthermore, patients seen at public facilities are expected to be full‐time available to receive medical care, as they face long transportation times prior to arriving at the closest hospital (mean of 1 hour) and long times in waiting rooms prior to being seen by a physician [38]. The opportunity cost of IMSS ambulatory service utilization has been estimated to be equivalent to more than half the standard minimum wage [39]. For the informally employed, the loss of their daily wage is an additional cost.
Furthermore, the fact that having a perceived lack of financial resources may serve as a barrier to the use of medical services reflects the high use of private services. Patients often seek care from private physicians because these practitioners may be found in many neighborhoods, can provide timely care to patients by avoiding the bureaucratic maze of public sector medicine, and are often perceived as being higher quality, even though this perception is not necessarily true [40]. As for the factors associated with longer diagnosis delays, the high number of different health services used before arrival to the cancer center reflect the difficulties that patients have in accessing the needed care. According to our analyses, there are different mechanisms that explain a high use of several health services. (a) The patients may be referred from one health service to another, especially if they first consult a local primary care service run by a general practitioner or family physician. (b) The patients themselves insist in seeking care in different places when they perceive that there were medical errors in the first services consulted, or when they face long waiting times for the next appointments. (c) The first health service used is private, and the patients start their diagnostic workup there, until they run out of money and are now forced to seek care in the public system.
Finally, the perception of medical errors in diagnostic impressions of the first doctors consulted was associated with longer diagnosis intervals. Previous studies have reported medical errors and a lack of patient trust in health services to be barriers that favor diagnosis delay [21], [23]. Forty‐one percent of the patients in whom a cancer diagnosis was finally confirmed in our study reported having been diagnosed with a “benign” condition during their first medical consultation. Additionally, a recent study among a national sample of primary care physicians of Mexico revealed a BC basic knowledge score of only 38% [41]. Therefore, it seems possible that our participants’ perceptions of medical errors are correct.
It is interesting to note that medical errors were more commonly perceived to have occurred by younger patients. This could be because health‐care providers may be less likely to suspect a cancer diagnosis in young patients. It could also be that younger patients have higher health literacy and are more critical of the health‐care system. This idea is supported by the fact that younger patients had higher levels of education than their older counterparts (data not shown). Medical errors were also more commonly reported among those that first used private services, which might be due to the great heterogeneity in the quality of private services that the poor can access.
A last group of results that are worth discussing are those related with the high proportion of breast benign diagnosis. Approximately 30% of our participants ultimately were diagnosed with a benign breast condition. Time to diagnosis did not differ between cancer patients and those with benign conditions. Furthermore, 42% of patients with final benign diagnoses first identified a health problem via mammography screening. Benign breast conditions and false‐positive screening mammograms are not being adequately diagnosed in breast early detection units, or in the primary and secondary levels of care, thereby further saturating the already overwhelmed public cancer service system to the detriment of timely cancer patient care. This is an unintended consequence of the promotion of screening mammography in a setting where quality of screening cannot be warranted, and access to cancer diagnostic services outside a cancer referral center is scarce.
Study Limitations
One study limitation was that causality could not be established due to the study's cross‐sectional design. Another potential limitation is that recall bias could have affected the precision of the measurement of intervals and other variables. Nevertheless, the instrument utilized in this study demonstrated good reliability for the estimation of intervals of care in a previous validation process [32], and memory bias was minimized by doing the interviews as early in the diagnostic process as possible. Additionally, there is a source of delay that is not measurable: time to symptom recognition, that is, the interval between appearance of potentially detectable symptoms and their discovery. The recognition of bodily sensations as symptoms of potential illness that require professional care requires interpreting the body in the social and cultural context [42].
Implications
The focus of health policy directed toward the reduction of BC mortality in many LMICs, including Mexico, has been the promotion of population‐based mammography screening, even if they lack the infrastructure and the human and financial resources to implement these programs successfully. Despite these efforts, the national screening coverage remains at a low 20% [43]. Our results showed that 84% of BC patients presented with symptoms, a rate that is similar to what has been previously estimated in high‐income countries with well‐established mammography screening programs [44]. Great delays to diagnosis confirmation impacted even those whose condition was detected by screening. Continuing to focus on increasing screening coverage without the guarantee of quality and expedited referral routes will most likely not have an impact on BC mortality.
The World Health Organization and the Breast Health Global Initiative Guidelines recommend that population‐based mammography programs should not be implemented until access to the basic cancer diagnosis and treatment resources is guaranteed. Rather, they recommend early diagnosis (or downstaging) approaches for LMICs [45], [46], [47] A successful example of an effective downstaging program took place in Malaysia. The program consisted of training first‐line health personnel in hospitals and rural clinics to improve their skills in early detection, and of raising public awareness through sensitization by trained health personnel. After 4 years of program implementation, late‐stage (III and IV) BC cases were reduced by half [48].
Our study findings suggest the presence of several factors susceptible to early diagnosis interventions that could better work in our context. To reduce the patient interval, awareness campaigns need to go beyond the advertising of screening mammography and promotion of pink ribbon use to the design of more effective tailored campaigns directed to enhance the recognition of potential cancer symptoms, prompt seeking of medical attention after symptom discovery, give information in regard to the specific health services that patients are entitled to use, and improve the patients’ perceptions of access and quality of these services. Additionally, these campaigns could include messages that encourage patients to share their symptoms with significant others. However, more research is needed to identify the most cost‐effective ways to promote the recognition of early warning signs without making patients unnecessarily anxious and without overburdening health‐care providers with the provision of consultations to the “worried well.” [49].
To reduce diagnosis delay, efforts should focus on facilitating access to and strengthening the quality of public primary care services as well as imaging and pathology services necessary for the diagnosis, and the improvement of referral routes and coordination between primary, secondary, and tertiary levels of care. In several countries, such as the U.K., Denmark, Spain, and Australia, urgent referral pathways have been developed to facilitate the assessment of symptomatic patients [50].
Treatment affordability is now guaranteed in Mexico, thanks to the inclusion of breast cancer in the Fund of Protection for Catastrophic Health Expenses. The challenge is to diagnose patients in earlier stages of the disease in order to reduce mortality, improve the quality of life of survivors and provide more cost‐effective treatments. Adequate funding of public health services is essential in LMICs like Mexico to achieve the structural changes required to improve access, quality of care and coordination between the different levels of care, and therefore reduce cancer care delays [51]. Additionally, better regulation of the private sector is imperative to ensure quality of care and protect uninsured patients from catastrophic health expenses [52].
Conclusion
This study reveals very long diagnosis intervals and barriers of care faced by cancer patients in the context of an LMIC with a fragmented health‐care system. Our results suggest that policy in these settings should be directed toward the reduction of diagnosis delays, before the implementation of population‐based mammography screening programs, by focusing on early diagnosis strategies. Our findings suggest the presence of several factors susceptible to early diagnosis interventions that might be more successful in the context of an LMIC with a fragmented health‐care system. To reduce patient delays, the usually proposed intervention of awareness promotion could better work in our context if the message goes beyond the advertising of screening mammography to encourage the recognition of potential cancer symptoms and sharing of symptoms with significant others and to provide specific information regarding the available health services where patients should seek care. To reduce diagnosis delay, efforts should focus on strengthening the quality of care of public primary care services and improving referral routes to cancer care services.
See http://www.TheOncologist.com for supplemental material available online.
Supplementary Material
Acknowledgments
This study was supported by a National Council of Science and Technology Grant (CONACYT/SSA/IMSS/ISSSTE SALUD‐2007‐C01–69439). The funding institution had no role in the study design, data collection, analysis or interpretation of the data, writing of the manuscript, and decision to submit it for publication. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication. The views and conclusions expressed in this publication are those of the authors and not necessarily those of the Mexican National Cancer Institute, Banco de Mexico, Centro de Investigación y Docencia Económicas (CIDE), or Consejo Nacional de Ciencia y Tecnología (CONACYT).
Author Contributions
Conception/design: Karla Unger‐Saldaña
Collection and/or assembly of data: Karla Unger‐Saldaña
Data analysis and interpretation: Karla Unger‐Saldaña, Daniel Ventosa‐Santaulària, Alfonso Miranda, Guillermo Verduzco‐Bustos
Manuscript writing: Karla Unger‐Saldaña
Final approval of manuscript: Karla Unger‐Saldaña, Daniel Ventosa‐Santaulària, Alfonso Miranda, Guillermo Verduzco‐Bustos
Disclosures
The authors indicated no financial relationships.
References
- 1. Anderson BO, Cazap E, El Saghir NS et al. Optimisation of breast cancer management in low‐resource and middle‐resource countries: Executive summary of the Breast Health Global Initiative consensus, 2010. Lancet Oncol 2011;12:387–398. [DOI] [PubMed] [Google Scholar]
- 2. Richards MA, Westcombe AM, Love SB et al. Influence of delay on survival in patients with breast cancer: A systematic review. Lancet 1999;353:1119–1126. [DOI] [PubMed] [Google Scholar]
- 3. Neal RD, Tharmanathan P, France B et al. Is increased time to diagnosis and treatment in symptomatic cancer associated with poorer outcomes? Systematic review. Br J Cancer 2015;112(suppl 1):S92–S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Torring ML, Frydenberg M, Hansen RP et al. Evidence of increasing mortality with longer diagnostic intervals for five common cancers: A cohort study in primary care. Eur J Cancer 2013;49:2187–2198. [DOI] [PubMed] [Google Scholar]
- 5. Weller D, Vedsted P, Rubin G et al. The Aarhus statement: Improving design and reporting of studies on early cancer diagnosis. Br J Cancer 2012;106:1262–1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.International Agency for Research on Cancer. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide. IARC Cancer Base No. 11 (2013). Available at http://globocan.iarc.fr. Accessed December 28, 2013.
- 7. Angeles‐Llerenas A, Torres‐Mejia G, Lazcano‐Ponce E et al. Effect of care‐delivery delay on the survival of Mexican women with breast cancer. Salud Publica Mex 2016;58:237–250 [DOI] [PubMed] [Google Scholar]
- 8. Mohar A, Reynoso N, Villarreal‐Garza C et al. Cáncer de mama en el Instituto Nacional de Cancerología. Experiencia del Seguro Popular 2007–2013. Rev Mex Mastol 2015;5:6–11. [Google Scholar]
- 9. Unger‐Saldaña K, Miranda A, Zarco‐Espinoza G et al. Health system delay and its effect on clinical stage of breast cancer: Multicenter study. Cancer 2015;121:2198–2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ramirez AJ, Westcombe AM, Burgess CC et al. Factors predicting delayed presentation of symptomatic breast cancer: A systematic review. Lancet 1999;353:1127–1131. [DOI] [PubMed] [Google Scholar]
- 11. Nosarti C, Crayford T, Roberts JV et al. Delay in presentation of symptomatic referrals to a breast clinic: Patient and system factors. Br J Cancer 2000;82:742–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Montella M, Crispo A, D'Aiuto G et al. Determinant factors for diagnostic delay in operable breast cancer patients. Eur J Cancer Prev 2001;10:53–59. [DOI] [PubMed] [Google Scholar]
- 13. Montazeri A, Ebrahimi M, Mehrdad N et al. Delayed presentation in breast cancer: A study in Iranian women. BMC Womens Health 2003;3:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tjemsland L, Soreide JA. Operable breast cancer patients with diagnostic delay–Oncological and emotional characteristics. Eur J Surg Oncol 2004;30:721–727. [DOI] [PubMed] [Google Scholar]
- 15. Harirchi I, Ghaemmaghami F, Karbakhsh M et al. Patient delay in women presenting with advanced breast cancer: An Iranian study. Public Health 2005;119:885–891. [DOI] [PubMed] [Google Scholar]
- 16. Allgar VL, Neal RD. Delays in the diagnosis of six cancers: Analysis of data from the National Survey of NHS Patients: Cancer. Br J Cancer 2005;92:1959–1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Friedman LC, Kalidas M, Elledge R et al. Medical and psychosocial predictors of delay in seeking medical consultation for breast symptoms in women in a public sector setting. J Behav Med 2006;29:327–334. [DOI] [PubMed] [Google Scholar]
- 18. Wiesner C. Determinantes psicológicos, clínicos y sociales del diagnóstico temprano del cáncer de mama en Bogotá, Colombia. Rev Colomb Cancerol 2007;11:13–22. [Google Scholar]
- 19. Hansen RP, Olesen F, Sorensen HT et al. Socioeconomic patient characteristics predict delay in cancer diagnosis: A Danish cohort study. BMC Health Serv Res 2008;8:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ermiah E, Abdalla F, Buhmeida A et al. Diagnosis delay in Libyan female breast cancer. BMC Res Notes 2012;5:452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jassem J, Ozmen V, Bacanu F et al. Delays in diagnosis and treatment of breast cancer: A multinational analysis. Eur J Public Health 2014;24:761–767. [DOI] [PubMed] [Google Scholar]
- 22. Forbes LJ, Warburton F, Richards MA et al. Risk factors for delay in symptomatic presentation: A survey of cancer patients. Br J Cancer 2014;111:581–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ozmen V, Boylu S, Ok E et al. Factors affecting breast cancer treatment delay in Turkey: A study from Turkish Federation of Breast Diseases Societies. Eur J Public Health 2015;25:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Huo Q, Cai C, Zhang Y et al. Delay in diagnosis and treatment of symptomatic breast cancer in China. Ann Surg Oncol 2015;22:883–888. [DOI] [PubMed] [Google Scholar]
- 25. Thakur NA, Humne AY, Godale LB. Delay in presentation to the hospital and factors affecting it in breast cancer patients attending tertiary care center in Central India. Indian J Cancer 2015;52:102–105. [DOI] [PubMed] [Google Scholar]
- 26. Odongo J, Makumbi T, Kalungi S et al. Patient delay factors in women presenting with breast cancer in a low income country. BMC Res Notes 2015;8:467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Khan MA, Shafique S, Khan MT et al. Presentation delay in breast cancer patients, identifying the barriers in North Pakistan. Asian Pac J Cancer Prev 2015;16:377–380. [DOI] [PubMed] [Google Scholar]
- 28. Abu‐Helalah AM, Alshraideh HA, Al‐Hanaqtah M et al. Delay in presentation, diagnosis, and treatment for breast cancer patients in Jordan. Breast J 2016;22:213–217. [DOI] [PubMed] [Google Scholar]
- 29. Dianatinasab M, Fararouei M, Mohammadianpanah M et al. Impact of social and clinical factors on diagnostic delay of breast cancer: A cross‐sectional study. Medicine (Baltimore) 2016;95:e4704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Maghous A, Rais F, Ahid S et al. Factors influencing diagnosis delay of advanced breast cancer in Moroccan women. BMC Cancer 2016;16:356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hernández‐Ávila M, Rivera Dommarco J, Shamah Levy T et al. Encuesta Nacional de Salud y Nutrición de Medio Camino 2016. Instituto Nacional de Salud Pública, México. [DOI] [PubMed]
- 32. Unger‐Saldana K, Pelaez‐Ballestas I, Infante‐Castaneda C. Development and validation of a questionnaire to assess delay in treatment for breast cancer. BMC Cancer 2012;12:626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bollen KA, Noble MD. Structural equation models and the quantification of behavior. Proc Natl Acad Sci U S A 2011;108(suppl 3):15639–15646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Skrondal A, Rabe‐Hesketh S. Generalized latent variable modeling: Multilevel, longitudial and structural equation models. Boca Raton, FL: Chapman & Hall/CRC, 2004.
- 35. Unger‐Saldana K, Infante‐Castaneda CB. Breast cancer delay: A grounded model of help‐seeking behaviour. Soc Sci Med 2011;72:1096–1104. [DOI] [PubMed] [Google Scholar]
- 36. Leydon GM, Bynoe‐Sutherland J, Coleman MP. The journey towards a cancer diagnosis: The experiences of people with cancer, their family and carers. Eur J Cancer Care (Engl) 2003;12:317–326. [DOI] [PubMed] [Google Scholar]
- 37. Pescosolido BA. Beyond rational choice: The social dynamics of how people seek help. Am J Sociol 1992;97:1096–1138. [Google Scholar]
- 38.Consejo Nacional de Evaluación de la Política de Desarrollo Social. Indicadores de acceso y uso efectivo de los servicios de salud de afiliados al Seguro Popular. México, D.F: CONEVAL, 2014.
- 39. Martínez Carranza EO, Villarreal Ríos E, Vargas Daza ER et al. Costo de oportunidad en hombres que acuden a las unidades de medicina familiar en la ciudad de Querétaro, México. Revista Panamericana de Salud Publica 2010;28:456–462. [DOI] [PubMed] [Google Scholar]
- 40. Finkler K. Biomedicine globalized and localized: Western medical practices in an outpatient clinic of a Mexican hospital. Soc Sci Med 2004;59:2037–2051. [DOI] [PubMed] [Google Scholar]
- 41. Ortega‐Olvera C, Torres‐Mejia G, Sanchez‐Zamorano LM et al. Knowledge and recommendations regarding breast cancer early screening in an upper middle income country: Primary and secondary health care professionals. Prev Med 2016;86:147–152. [DOI] [PubMed] [Google Scholar]
- 42. Andersen RS, Paarup B, Vedsted P et al. 'Containment' as an analytical framework for understanding patient delay: A qualitative study of cancer patients' symptom interpretation processes. Soc Sci Med 2010;71:378–385. [DOI] [PubMed] [Google Scholar]
- 43. Torres‐Mejia G, Ortega‐Olvera C, Angeles‐Llerenas A et al. Utilization patterns of prevention and early diagnosis for cancer in women [in Spanish]. Salud Publica Mex 2013;55(suppl 2):S241–S248. [PubMed] [Google Scholar]
- 44. Emery JD, Shaw K, Williams B et al. The role of primary care in early detection and follow‐up of cancer. Nat Rev Clin Oncol 2014;11:38–48. [DOI] [PubMed] [Google Scholar]
- 45.World Health Organization . WHO position paper on mammography screening. Geneva: World Health Organization, 2014. [PubMed] [Google Scholar]
- 46.World Health Organization . Guide to cancer early diagnosis. Geneva: World Health Organization, 2017. Licence: CC BY‐NC‐SA 3.0 IGO. [Google Scholar]
- 47. Anderson BO, Yip CH, Smith RA et al. Guideline implementation for breast healthcare in low‐income and middle‐income countries: Overview of the Breast Health Global Initiative Global Summit 2007. Cancer 2008;113(suppl 8):2221–2243. [DOI] [PubMed] [Google Scholar]
- 48. Devi BC, Tang TS, Corbex M. Reducing by half the percentage of late‐stage presentation for breast and cervix cancer over 4 years: A pilot study of clinical downstaging in Sarawak, Malaysia. Ann Oncol 2007;18:1172–1176. [DOI] [PubMed] [Google Scholar]
- 49. Quaife SL, Forbes LJ, Ramirez AJ et al. Recognition of cancer warning signs and anticipated delay in help‐seeking in a population sample of adults in the UK. Br J Cancer 2014;110:12–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rubin G, Berendsen A, Crawford SM et al. The expanding role of primary care in cancer control. Lancet Oncol 2015;16:1231–1272. [DOI] [PubMed] [Google Scholar]
- 51. Cazap E, Magrath I, Kingham TP et al. Structural barriers to diagnosis and treatment of cancer in low‐ and middle‐income countries: The urgent need for scaling up. J Clin Oncol 2016;34:14–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Schwellnus C. Achieving higher performance: Enhancing spending efficiency in healthcare and education in Mexico. Paris: Organisation for Economic Cooperation and Development (OECD), 2009. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.