Abstract
Background
Restrictive blood transfusion practices in hospitalized patients with anemia have reduced use of transfusion. Consequently, hospitalized patients are more likely to have lower hemoglobin (Hb) concentrations. Lower Hb is associated with increased fatigue in ambulatory patients. However, it is not known whether anemia is associated with fatigue in hospitalized patients. It is also unclear how to best measure anemia in hospitalized patients, since Hb levels generally vary over a hospital stay.
Objective
To assess multiple Hb-based measures of anemia in hospitalized patients, and to test whether these are associated with fatigue.
Design
Prospective observational study.
Setting
Urban academic medical center.
Patients
Hospitalized general medicine patients, age ≥50, with any Hb <9g/dL.
Intervention
Patients’ anemia-related fatigue was measured during hospitalization.
Measurements
Measures of anemia were created for each patient based on the Hb values from their hospitalization (mean, median, minimum, maximum, admission, discharge). Fatigue was measured using the Functional Assessment of Chronic Illness Therapy Fatigue Subscale (FACIT).
Results
784 patients participated. Minimum Hb was strongly associated with fatigue. Patients with a minimum Hb <8g/dL had higher fatigue levels (Mean FACIT (SD) Hb<7g/dL: 25 (13), 7g/dL≤Hb<8g/dL: 25 (14) Hb≥8g/dL: 29 (14), p=<0.001) and were more likely to report high levels of fatigue (FACIT<27) (56% vs. 41%, p=0.002). Mean Hb had a less robust association with fatigue than minimum Hb, and no other measure of Hb was associated with patients’ fatigue levels.
Conclusion
Minimum Hb is associated with fatigue while hospitalized and may help identify patients for interventions to address anemia-related fatigue.
Keywords: Anemia, Fatigue, Red Blood Cell Transfusion, Symptoms of Anemia
INTRODUCTION
Fatigue is the most common clinical symptom of anemia, and is a significant concern to patients1,2. In ambulatory patients, lower hemoglobin (Hb) concentration is associated with increased fatigue2,3. Accordingly, therapies that treat anemia by increasing Hb concentration, such as erythropoiesis stimulating agents4–7, often use fatigue as an outcome measure.
In hospitalized patients, transfusion of red blood cell increases Hb concentration and is the primary treatment for anemia. However, the extent to which transfusion and changes in Hb concentration affect hospitalized patients’ fatigue levels is not well established. Guidelines support transfusing patients with symptoms of anemia, such as fatigue, on the assumption that the increased oxygen delivery will improve the symptoms of anemia. While transfusion studies in hospitalized patients have consistently reported that transfusion at lower or “restrictive” Hb concentrations is safe compared to transfusion at higher Hb concentrations8–10, these studies have mainly used cardiac events and mortality as outcomes, rather than patient symptoms like fatigue. Nevertheless, they have resulted in hospitals increasingly adopting restrictive transfusion policies that discourage transfusion at higher Hb levels11,12. Consequently, the rate of transfusion in hospitalized patients has decreased13, raising questions of whether some patients with lower Hb concentrations may experience increased fatigue as a result of restrictive transfusion policies. Fatigue among hospitalized patients is important not only because it is an adverse symptom but because it may result in decreased activity levels, deconditioning, and losses in functional status14,15.
While the effect of alternative transfusion policies on fatigue in hospitalized patients could be answered by a randomized clinical trial using fatigue and functional status as outcomes, an important first step is to assess whether the Hb concentration of hospitalized patients is associated with their fatigue level during hospitalization. Because hospitalized patients often have acute illness that itself can cause fatigue, it is possible that anemia is not associated with fatigue in hospitalized patients despite anemia’s association with fatigue in ambulatory patients. Additionally, Hb concentration varies during hospitalization16, raising the question of what measures of Hb during hospitalization might be most associated with anemia-related fatigue.
The objective of this study is to explore multiple Hb measures in hospitalized medical patients with anemia, and test whether any of these Hb measures are associated with patients’ fatigue level.
METHODS
Study Design
We performed a prospective observational study of hospitalized patients with anemia on the general medicine services at The University of Chicago Medical Center (UCMC). The institutional review board approved the study procedures and all study subjects provided informed consent.
Study Eligibility
Between April, 2014 and June, 2015, all general medicine inpatients were approached for written consent for The University of Chicago Hospitalist Project17, a research infrastructure at UCMC. Among patients consenting to participate in the Hospitalist Project, patients were eligible if they had a Hb <9g/dL at any point during their hospitalization and were age ≥50. A Hb concentration of <9g/dL was chosen to include the range of Hb values covered by most restrictive transfusion policies.8–10,18 Age ≥50 was an inclusion criteria since anemia is more strongly associated with poor outcomes, including functional impairment, among older patients compared to younger patients14,19–21. If patients were not eligible for inclusion at the time of consent for the Hospitalist Project, their Hb values were reviewed twice daily until hospital discharge to assess if their Hb was <9g/dL. Proxies were sought to answer questions for patients who failed the Short Portable Mental Status Questionnaire22.
Patient Demographic Data Collection
Research assistants abstracted patient age and sex from the electronic health record (EHR), and asked patients to self-identify their race. The individual comorbidities included as part of the Charlson Comorbidity index were identified using International Classification of Disease 9 codes from hospital administrative data for each encounter and included specifically: myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatic disease, peptic ulcer disease, liver disease, diabetes, hemiplegia/paraplegia, renal disease, cancer, AIDS/HIV23. We also used Health Care Utilization Project (www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp) diagnosis categories to identify whether patients had sickle cell anemia (SC), gastrointestinal bleeding (GIB), or a depressive disorder (DD) because these conditions are associated with anemia (SC, GIB) and fatigue (DD)24.
Measuring Anemia
Hb measures were available only when hospital providers ordered them as part of routine practice. The first Hb concentration <9g/dL during a patient’s hospitalization, making them eligible for study participation, was obtained through manual review of the EHR. All additional Hb values during the patient’s hospitalization were obtained from the hospital’s administrative data mart. All Hb values collected for each patient during the hospitalization were used to calculate summary measures of Hb during the hospitalization, including the mean Hb, median Hb, minimum Hb, maximum Hb, admission (first recorded) Hb, and the discharge (last recorded) Hb. Hb measures were analyzed both as a continuous variable and as a categorical variable created by dividing the continuous Hb measures into integer ranges of 3 groups of approximately the same size.
Measuring Fatigue
Our primary outcome was patients’ level of fatigue reported during hospitalization, measured using the Functional Assessment of Chronic Illness Therapy Anemia (FACIT-An) questionnaire. Fatigue was measured using a 13 question fatigue subscale1,2,25, which measures fatigue within the past 7 days. Scores on the fatigue subscale range from 0-52, with lower scores reflecting greater levels of fatigue. As soon as patients met the eligibility criteria for study participation during their hospitalization (age≥50, Hb<9 g/dL), they were approached to answer the FACIT questions. Values for missing data in the fatigue subscale for individual subjects were filled in using a prorated score from their answered questions, as long as more than 50% of the items in the fatigue subscale were answered, in accordance with recommendations for addressing missing data in the FACIT26. Fatigue was analyzed as a continuous variable and as a dichotomous variable created by dividing the sample into high (FACIT <27) and low (FACIT ≥27) levels of fatigue based on the median FACIT score of the population. Previous literature has shown a FACIT fatigue score between 23-26 to be associated with an ECOG27 Performance Status Rating of 2-33, compared to scores ≥27.
Statistical Analysis
Statistical analysis was performed using Stata statistical software, StataCorp, College Station, TX. Descriptive statistics were used to characterize patient demographics. Analysis of variance was used to test for differences in the mean fatigue levels across Hb measures. Chi-squared tests were performed to test for associations between high fatigue levels and the Hb measures. Multivariable analysis including both linear and logistic regression models were used to test the association of Hb concentration and fatigue. P-values <0.05 using a two-tailed test were deemed statistically significant.
RESULTS
Patient Characteristics
8,559 patients were admitted to the general medicine service during the study period. 5,073 (59%) patients consented for participation in the Hospitalist Project, and 3,670 (72%) patients completed the Hospitalist Project inpatient interview. 1,292 (35%) of these patients had a Hb <9g/dL, and 784 (61%) of these patients were age 50 or older and completed the FACIT questionnaire.
Table 1 reports the demographic characteristics and comorbidities for the sample, the mean (SD) for the six Hb measures, and mean (SD) and median FACIT scores.
Table 1.
Patient Characteristics
| Total N=784 | N (%) |
|---|---|
|
| |
| Female | 447 (57) |
|
| |
| Age-Mean ± SD (years) | 66 ± 11 |
|
| |
| Race | |
| American Indian or Alaskan Native | 3 (<1) |
| Asian | 12 (2) |
| Black or African American | 507 (65) |
| White | 212 (27) |
| Multiple Reported Races | 8 (1) |
| Don’t Know/Refused | 42 (5) |
| Ethnicity | |
| Hispanic or Latino | 46 (6) |
| Not Hispanic or Latino | 711 (91) |
| Don’t Know/Refused | 27 (3) |
|
| |
| Admission Comorbidities | |
| Myocardial Infarction | 59 (8) |
| Congestive Heart Failure | 251 (32) |
| Peripheral Vascular Disease | 71 (9) |
| Cerebrovascular Disease | 25 (3) |
| Dementia | 0 (0) |
| Chronic Pulmonary Disease | 211 (27) |
| Rheumatic Disease | 40 (5) |
| Peptic Ulcer Disease | 47 (6) |
| Liver Disease | 126 (16) |
| Diabetes | 344 (43) |
| Hemiplegia/Paraplegia | 10 (1) |
| Renal Disease | 165 (21) |
| Cancer | 134 (17) |
| AIDS/HIV | 10 (1) |
| Sickle Cell Anemia | 21 (3) |
| Gastrointestinal Bleeding | 98 (13) |
| Depressive disorder | 103 (13) |
|
| |
| Hemoglobin (Hb) Measures ± SD (g/dL) | |
| Mean Hb | 8.5 ± 0.8 |
| Median Hb | 8.4 ± 0.8 |
| Minimum Hb | 7.3 ± 1.1 |
| Maximum Hb | 9.8 ± 1.5 |
| Admission Hb | 8.9 ± 1.8 |
| Discharge Hb | 8.5 ± 0.9 |
|
| |
| Transfusion During Hospitalization | 289 (35) |
|
| |
| FACIT Fatigue Subscale Score (Range 0–52) | |
| Mean ± SD | 26 ± 14 |
| Median (IQR1–IQR3) | 27 (15–37) |
SD=Standard Deviation
Hb=Hemoglobin
FACIT=Functional Assessment of Chronic Illness Therapy
IQR=Interquartile Range
Bivariate Association of Fatigue and Hemoglobin
Categorizing patients into low, middle or high Hb for each of the 6 Hb measures, minimum Hb was strongly associated with fatigue, with a weaker association for mean Hb, and no statistically significant association for the other measures.
Minimum Hb
Patients with a minimum Hb <7g/dL and patients with a Hb 7-8g/dL had higher fatigue levels (FACIT=25 for each) than patients with a minimum Hb ≥8g/dL (FACIT=29) (p<0.001) (Table 2). When excluding patients with SC and/or GIB, because their average minimum Hb differed from the average minimum Hb of the full population (p<0.001), patients with a minimum Hb <7g/dL or between 7-8g/dL had even higher fatigue levels (FACIT=23 and FACIT=24, respectively), with no change in the fatigue level of patients with a minimum Hb ≥8g/dL (FACIT=29) (p<0.001) (Table 2). Lower minimum Hb continued to be associated with higher fatigue levels when analyzed in 0.5g/dL increments (Figure 1).
Table 2.
Bivariate Analysis of Fatigue and Hemoglobin Measures
| Hemoglobin Measure | Range | Full Population (N=784) | Excluding SC/GIB Patients (N=666) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Subjects (n=784) |
Mean Fatigue Score* (s.e) |
P** | % High Fatigue, FACIT<27 | P*** | Subjects (n=594) |
Mean Fatigue Score* (s.e) |
P** | % High Fatigue, FACIT<27 | P*** | ||
| Mean | Hb<8g/dL | 214 | 26 (1.0) | 0.07 | 47 | 0.05 | 147 | 25 (1.2) | 0.06 | 51 | 0.09 |
| 8g/dL≤Hb<9g/dL | 370 | 25 (0.7) | 53 | 283 | 25 (0.8) | 53 | |||||
| Hb≥9g/dL | 200 | 28 (1.0) | 43 | 164 | 28 (1.1) | 43 | |||||
|
| |||||||||||
| Median | Hb<8g/dL | 222 | 26 (1.0) | 0.47 | 48 | 0.65 | 157 | 24 (1.1) | 0.3 | 52 | 0.81 |
| 8g/dL≤Hb<9g/dL | 380 | 26 (0.7) | 50 | 291 | 26 (0.8) | 50 | |||||
| Hb≥9g/dL | 182 | 27 (1.0) | 46 | 146 | 27 (1.1) | 48 | |||||
|
| |||||||||||
| Minimum | Hb<7g/dL | 284 | 25 (0.8) | <0.001 | 50 | 0.002 | 180 | 23 (0.9) | <0.001 | 54 | <0.001 |
| 7g/dL≤Hb<8g/dL | 234 | 25 (0.9) | 56 | 181 | 24 (1.0) | 57 | |||||
| Hb≥8g/dL | 266 | 29 (0.9) | 41 | 233 | 29 (0.9) | 41 | |||||
|
| |||||||||||
| Maximum | Hb<9g/dL | 212 | 27 (1.0) | 0.27 | 44 | 0.17 | 159 | 26 (1.1) | 0.32 | 47 | 0.36 |
| 9g/dL≤Hb<10g/dL | 278 | 26 (0.8) | 49 | 203 | 26 (0.9) | 49 | |||||
| Hb≥10g/dL | 294 | 25 (0.8) | 52 | 232 | 25 (0.9) | 53 | |||||
|
| |||||||||||
| Admission | Hb<8g/dL | 196 | 26 (1.0) | 0.27 | 47 | 0.37 | 112 | 24(1.2) | 0.23 | 51 | 0.72 |
| 8g/dL≤Hb<10g/dL | 384 | 27 (0.7) | 53 | 309 | 26 (0.8) | 49 | |||||
| Hb≥10g/dL | 204 | 25 (1.0) | 49 | 173 | 25 (1.0) | 52 | |||||
|
| |||||||||||
| Discharge | Hb<8g/dL | 244 | 26 (0.9) | 0.83 | 49 | 0.86 | 160 | 25 (1.1) | 0.59 | 52 | 0.66 |
| 8g/dL≤Hb<9g/dL | 267 | 26 (0.8) | 50 | 292 | 26 (0.8) | 50 | |||||
| Hb≥9g/dL | 273 | 27 (0.9) | 47 | 142 | 26 (1.1) | 50 | |||||
Higher fatigue scores equate with lower or less amounts of fatigue
P-values for ANOVA
P-values for Chi-Squared
SC=Sickle Cell Anemia
GIB=Gastrointestinal Bleeding
Figure 1. Mean Fatigue Score by Minimum Hemoglobin Concentration.
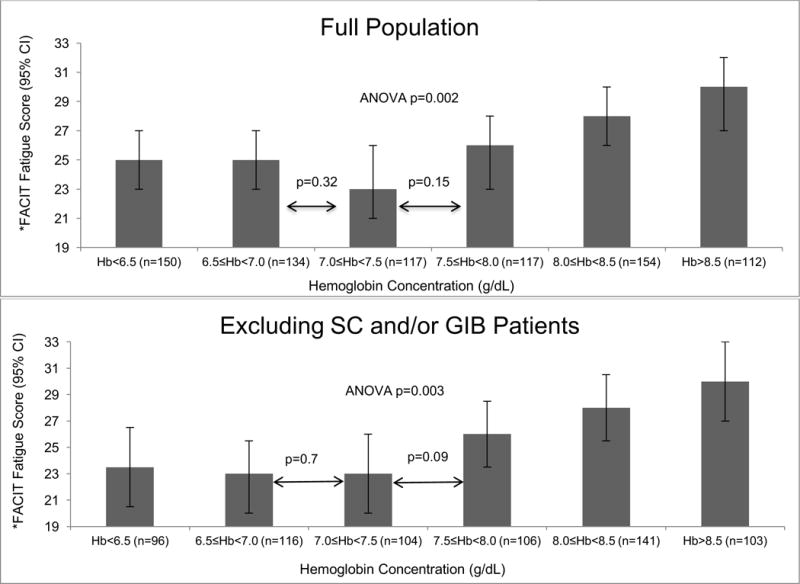
*Higher FACIT fatigue scores equate with lower fatigue
ANOVA=Analysis of Variance
Hb=Hemoglobin
SC=Sickle Cell Disease
GIB=Gastrointestinal Bleeding
Lower values of minimum Hb were also associated with patients reporting high fatigue levels (FACIT<27). Fatigue levels were high for 50% of patients with a minimum Hb <7g/dL and 56% of patients with a minimum Hb between 7-8g/dL compared to only 41% of patients with a minimum Hb ≥8g/dL (p<0.002). Excluding patients with SC and/or GIB, fatigue levels were high for 54% of patients with a minimum Hb <7g/dL and 57% of patients with a minimum Hb between 7-8g/dL, compared to 41% of patients with a minimum Hb ≥8g/dL (p<0.001) (Table 2).
Mean Hb and other measures
Fatigue levels were high for 47% of patients with a mean Hb <8g/dL, and 53% of patients with a mean Hb between 8-9g/dL, compared to 43% of patients with a mean Hb ≥9g/dL (p=0.05). However, the association between high fatigue and mean Hb was not statistically significant when patients with SC and/or GIB were excluded (Table 2). None of the other four Hb measures was significantly associated with fatigue.
Linear Regression of Fatigue on Hemoglobin
In linear regression models, minimum Hb consistently predicted patient fatigue, mean Hb had a less robust association with fatigue, and the other Hb measures were not associated with patient fatigue. Increases in minimum Hb, analyzed as a continuous variable, were associated with reduced fatigue (higher FACIT fatigue score) (β=1.4, p=0.005). In models in which minimum Hb was a categorical variable, patients with a minimum Hb of <7g/dL or between 7-8g/dL had greater fatigue (lower FACIT fatigue score) than patients whose minimum Hb was ≥8g/dL (Hb<7g/dL: β=-4.2, p=<0.001; Hb 7-8g/dl: β=-4.1, p<0.001). These results control for patients’ age, sex, individual comorbidities, and whether their minimum Hb occurred before or after the measurement of fatigue during hospitalization (Model 1), and the results are unchanged when also controlling for the number of Hb laboratory draws a patient had during their hospitalization (Model 2) (Table 1). In a stratified analysis excluding patients with either SC and/or GIB, changes in minimum Hb were associated with larger changes in patient fatigue levels (Supplemental Table 1). We also stratified our analysis to include only patients whose minimum Hb occurred before the measurement of their fatigue level during hospitalization, to avoid a spurious association of fatigue with minimum Hb occurring after fatigue was measured. In both model 1 and 2, minimum Hb remained a predictor of patients’ fatigue levels with similar effect sizes, although in model 2 the results did not quite reach a statistically significant level, in part due to larger confidence intervals from the smaller sample size of this stratified analysis (Supplemental Table 2a). We further stratified this analysis to include only patients whose transfusion, if they received one, occurred after their minimum Hb and the measurement of their fatigue level, to account for the possibility that a transfusion could affect the fatigue level patients report. In this analysis, most of the estimates of the effect of minimum Hb on fatigue were larger than those seen when only analyzing patients whose minimum Hb occurred before the measurement of their fatigue level, although again, the smaller sample size of this additional stratified analysis does produce larger confidence intervals for these estimates (Supplemental Table 2b).
Analyzed as a categorical variable, a mean Hb <8g/dL or between 8-9g/dL was also associated with higher levels of fatigue compared to patients whose mean Hb ≥9g/dL in both model 1 and 2, although the results were only statistically significant for patients with a mean Hb between 8-9g/dL (β=-2.5, p<0.04) (Table 3). There were no statistically significant associations between mean Hb and fatigue when excluding SC and/or GIB patients (Supplemental Table 3).
Table 3.
Minimum and Mean Hemoglobin Effect on Patient Fatigue (N=784)
| Model | Hb Concentration | Inpatient Fatigue Level | High Fatigue (FACIT<27) | |||||
|---|---|---|---|---|---|---|---|---|
| β | 95% CI | p | OR | 95% CI | p | |||
|
|
||||||||
| Minimum Hemoglobin | 1 | Minimum Hb (continuous) | 1.4 | (0.4, 2.3) | 0.005 | 0.9 | (0.8, 1.0) | 0.09 |
|
| ||||||||
| 7g/dL≤Hb<8g/dL* | −4.1 | (−6.6, −1.7) | <0.001 | 1.9 | (1.3, 2.8) | <0.001 | ||
| Hb<7g/dL* | −4.2 | (−6.6, −1.6) | <0.001 | 1.5 | (1.1, 2.2) | 0.03 | ||
|
| ||||||||
| 2 | Minimum Hb (continuous) | 1.0 | (−0.1, 2.0) | 0.05 | 0.9 | (0.8, 1.1) | 0.41 | |
|
| ||||||||
| 7g/dL≤Hb<8g/dL* | −3.9 | (−6.3, −1.4) | 0.02 | 1.9 | (1.3, 2.7) | 0.001 | ||
| Hb<7g/dL* | −3.2 | (−5.7, −0.6) | 0.02 | 1.3 | (0.9, 1.9) | 0.21 | ||
|
| ||||||||
| Model | Hb Concentration | Inpatient Fatigue Level | High Fatigue (FACIT<27) | |||||
| β | 95% CI | p | OR | 95% CI | p | |||
|
|
||||||||
| Mean Hemoglobin | 1 | Mean Hb (continuous) | 0.22 | (−1.0, 1.5) | 0.71 | 1.0 | (0.9, 1.2) | 0.67 |
|
| ||||||||
| 8g/dL≤Hb<9g/dL# | −2.5 | (−4.9, −0.1) | 0.04 | 1.5 | (1.0, 2.1) | 0.03 | ||
| Hb<8g/dL# | −2.4 | (−5.1, 0.4) | 0.09 | 1.2 | (0.8, 1.9) | 0.3 | ||
|
| ||||||||
| 2 | Mean Hb (continuous) | 0.4 | (−0.9, 1.6) | 0.6 | 1.0 | (0.9, 1.2) | 0.3 | |
|
| ||||||||
| 8g/dL≤Hb<9g/dL# | −2.5 | (−4.9, −0.2) | 0.04 | 1.5 | (1.1, 2.2) | 0.03 | ||
| Hb<8g/dL# | −2.4 | (−5.1, 0.3) | 0.08 | 1.3 | (0.8, 1.9) | 0.27 | ||
Hb≥8g/dL referent group
Hb≥9g/dL referent group
Linear/Logistic Regression Model 1: Adjusted for age, sex, time of minimum Hb relative to measurement of fatigue, comorbidities
Linear/Logistic Regression Model 2: Adjusted for age, sex, time of minimum Hb relative to measurement of fatigue, # of cbc’s drawn during hospitalization, comorbidities
Comorbidities: myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, rheumatic disease, peptic ulcer disease, liver disease, diabetes, hemiplegia/paraplegia, renal disease, cancer, sickle cell anemia, gastrointestinal bleeding, depressive disorder
No Hb measure other than minimum or mean had significant association with patient fatigue levels in linear regression models.
Logistic Regression of High Fatigue Level on Hemoglobin
Using logistic regression, minimum Hb analyzed as a categorical variable predicted increased odds of a high fatigue level. Patients with a minimum Hb <7g/dL were 50% (OR=1.5, p=0.03) more likely and patients with a minimum Hb between 7-8g/dL were 90% (OR=1.9, p<0.001) more likely to have high fatigue compared to patients with a minimum Hb ≥8g/dL in Model 1. These results were similar in Model 2, although the effect was only statistically significant in the 7-8g/dL Hb group (Table 3). When excluding SC and/or GIB patients, the odds of having high fatigue as minimum Hb decreased were the same or higher for both models compared to the full population of patients. However, again, in Model 2 the effect was only statistically significant in the 7-8g/dL Hb group (Supplemental Table 1).
Patients with a mean Hb <8g/dL were 20%–30% more likely and patients with mean Hb between 8-9g/dL were 50% more likely to have high amounts of fatigue compared to patients with a mean Hb ≥9g/dL, but the effects were only statistically significant for patients with a mean Hb between 8-9g/dL in both model 1 and 2 (Table 3). These results were similar when excluding patients with SC and/or GIB, but they were only significant for patients with mean Hb between 8-9g/dL in the model 1 and patients with a mean Hb <8g/dL in the model 2 (Supplemental Table 3).
DISCUSSION
These results demonstrate that minimum Hb during hospitalization is associated with fatigue in hospitalized patients age ≥50 years, and the association is stronger among patients without either SC and/or GIB as comorbidities. The analysis of Hb as a continuous and categorical variable and the use of both linear and logistic regression models support the robustness of these associations and illuminate their clinical significance. For example, in linear regression with minimum Hb a continuous variable, the coefficient of 1.4 suggests that an increase of 2g/dL in Hb, as might be expected from transfusion of 2 units of red blood cells, would be associated with about a 3-point improvement in fatigue. Additionally, as a categorical variable, a minimum Hb ≥8g/dL compared to a minimum Hb<7g/dL or between 7-8g/dL is associated with 3-4 points less fatigue. Previous literature suggests that a difference of 3 in the FACIT fatigue score is the minimum clinically important difference in fatigue3, and changes in minimum Hb in either model predicts changes in fatigue that are in the range of potential clinical significance.
The clinical significance of the findings is also reflected in the results of the logistic regressions, which may be mapped to potential effects on functional status. Specifically, the odds of having a high fatigue level (FACIT<27) increase 90% for persons with a minimum Hb between 7-8g/dL, compared to persons with a minimum Hb ≥8g/dL. For persons with a minimum Hb <7g/dL, point estimates suggest a smaller (50%) increase in the odds of high fatigue, but the 95% confidence interval overlaps heavily with the estimate of patients whose minimum Hb is between 7-8g/dL. While it might be expected that patients with a minimum Hb <7g/dL have greater levels of high fatigue compared to patients with a minimum Hb between 7-8g/dL, we did not observe such a pattern. One reason may be that the confidence intervals on our estimated effects are wide enough that we cannot exclude such a pattern. Another possible explanation is that in both groups the fatigue levels are sufficiently severe, such that the difference in their fatigue levels may not be clinically meaningful. For example, a FACIT score of 23-26 has been shown to be associated with an ECOG performance status of 2-3, requiring bedrest for at least part of the day3. Therefore, patients with a minimum Hb between 7-8g/dL (mean FACIT score=24, Table 2) or a minimum Hb of <7g/dL (mean FACIT score=23, Table 2) are already functionally limited to the point of being partially bed bound, such that further decreases in their Hb may not produce additional fatigue in part because they reduce their activity sufficiently to prevent an increase in fatigue. In such cases, the potential benefits of increased Hb may be better assessed by measuring fatigue in response to a specific and provoked activity level, a concept known as fatigability20.
That minimum Hb is more strongly associated with fatigue than any other measure of Hb during hospitalization may not be surprising. Mean, median, maximum and discharge Hb may all be affected by transfusion during hospitalization that could affect fatigue. Admission Hb may not reflect true oxygen carrying capacity because of hemo-concentration.
The association between Hb and fatigue in hospitalized patients is important because increased fatigue could contribute to slower clinical recovery in hospitalized patients. Additionally, increased fatigue during hospitalization and at hospital discharge could exacerbate the known deleterious consequences of fatigue on patients and their health outcomes14,15 after hospital discharge. Although one previous study, the FOCUS8 trial, did not report differences in patients fatigue levels at 30 and 60 days post-discharge when transfused at a restrictive (8g/dL) compared to liberal (10g/dL) Hb thresholds, confidence in the validity of this finding is reduced by the fact that over half of the patients were lost to follow up at the 30 and 60 day time points. Further, patients in the restrictive transfusion arm of FOCUS were transfused to maintain Hb levels at or above 8g/dL. This transfusion threshold of 8g/dL may have mitigated the high levels of fatigue that are seen in our study when patients’ Hb drops below 8g/dL, and maintaining a Hb level of 7g/dL is now the standard of care in stable hospitalized patients. Lastly, FOCUS was limited to post-operative hip fracture patients, and the generalizability of FOCUS to hospitalized medicine patients with anemia is limited.
Therefore, our results support guideline suggestions that practitioners incorporate the presence of patient symptoms like fatigue into transfusion decisions, particularly if patients’ Hb<8g/dL18. Though reasonable, the suggestion to incorporate symptoms like fatigue into transfusion decisions have not to date been strongly supported by evidence, and may often be neglected in practice. Definitive evidence to support such recommendations would benefit from study through an “optimal trial”18 that incorporated symptoms into decision making. Our findings add support for a study of transfusion strategies that incorporates patients’ fatigue level in addition to their Hb concentration.
This study has several limitations. Although our sample size is large and includes patients with a range of comorbidities that we believe is representative of hospitalized general medicine patients, as a single center observational study our results may not be generalizable to other centers. Additionally, although these data support a reliable association between hospitalized patients’ minimum Hb and their fatigue level, the observational design of this study cannot prove that this relationship is causal. Also, patients’ Hb values were measured at the discretion of their clinician, and therefore the measures of Hb were not uniformly measured for participating patients. In addition, fatigue was only measured at one time point during a patient’s hospitalization, and it is possible that patients’ fatigue levels change during a hospitalization in relation to variables we did not consider. Finally, our study was not designed to assess the association of Hb with longer-term functional outcomes, which may be of greater concern than fatigue.
CONCLUSION
In hospitalized patients ≥50 years old, minimum Hb is reliably associated with patients’ fatigue level. Patients whose minimum Hb is <8g/dL experience higher fatigue levels compared to patients whose minimum Hb is ≥8g/dL. Additional studies are warranted to understand if patients may benefit from improved fatigue levels by correcting their anemia through a transfusion.
Supplementary Material
Acknowledgments
None
Dr. Prochaska is supported by an Agency for Healthcare Research and Quality K12 Patient Centered Outcomes Research Award. (AHRQ/PCORI 1K12HS023007-01, Meltzer, PI)
Dr. Meltzer is supported by an National Institutes of Health Clinical and Translational Science Award (NIH/NCATS 2UL1TR000430-06, Solway PI) and by a grant from the Patient Centered Outcomes Research Network in support of the Chicago Patient Centered Outcomes Research Network.
Footnotes
Conflicts of Interest: None
References
- 1.Yellen SB, Cella DF, Webster K, Blendowski C, Kaplan E. Measuring fatigue and other anemia-related symptoms with the Functional Assessment of Cancer Therapy (FACT) measurement system. J Pain Symptom Manage. 1997;13(2):63–74. doi: 10.1016/s0885-3924(96)00274-6. [DOI] [PubMed] [Google Scholar]
- 2.Cella D, Lai J-S, Chang C-H, Peterman A, Slavin M. Fatigue in cancer patients compared with fatigue in the general United States population. Cancer. 2002;94(2):528–538. doi: 10.1002/cncr.10245. [DOI] [PubMed] [Google Scholar]
- 3.Cella D, Eton DT, Lai J-S, Peterman AH, Merkel DE. Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. J Pain Symptom Manage. 2002;24(6):547–561. doi: 10.1016/s0885-3924(02)00529-8. [DOI] [PubMed] [Google Scholar]
- 4.Tonelli M, Hemmelgarn B, Reiman T, et al. Benefits and harms of erythropoiesis-stimulating agents for anemia related to cancer: a meta-analysis. CMAJ Can Med Assoc J J Assoc Medicale Can. 2009;180(11):E62–71. doi: 10.1503/cmaj.090470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Foley RN, Curtis BM, Parfrey PS. Erythropoietin Therapy, Hemoglobin Targets, and Quality of Life in Healthy Hemodialysis Patients: A Randomized Trial. Clin J Am Soc Nephrol. 2009;4(4):726–733. doi: 10.2215/CJN.04950908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keown PA, Churchill DN, Poulin-Costello M, et al. Dialysis patients treated with Epoetin alfa show improved anemia symptoms: A new analysis of the Canadian Erythropoietin Study Group trial. Hemodial Int Int Symp Home Hemodial. 2010;14(2):168–173. doi: 10.1111/j.1542-4758.2009.00422.x. [DOI] [PubMed] [Google Scholar]
- 7.Palmer SC, Saglimbene V, Mavridis D, et al. Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd; 2014. Erythropoiesis-stimulating agents for anaemia in adults with chronic kidney disease: a network meta-analysis. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD010590.pub2/abstract. Accessed June 15, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carson JL, Terrin ML, Noveck H, et al. Liberal or Restrictive Transfusion in High-Risk Patients after Hip Surgery. N Engl J Med. 2011;365(26):2453–2462. doi: 10.1056/NEJMoa1012452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holst LB, Haase N, Wetterslev J, et al. Transfusion requirements in septic shock (TRISS) trial - comparing the effects and safety of liberal versus restrictive red blood cell transfusion in septic shock patients in the ICU: protocol for a randomised controlled trial. Trials. 2013;14:150. doi: 10.1186/1745-6215-14-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hébert PC, Wells G, Blajchman MA, et al. A Multicenter, Randomized, Controlled Clinical Trial of Transfusion Requirements in Critical Care. N Engl J Med. 1999;340(6):409–417. doi: 10.1056/NEJM199902113400601. [DOI] [PubMed] [Google Scholar]
- 11.Corwin HL, Theus JW, Cargile CS, Lang NP. Red blood cell transfusion: Impact of an education program and a clinical guideline on transfusion practice. J Hosp Med. 2014;9(12):745–749. doi: 10.1002/jhm.2237. [DOI] [PubMed] [Google Scholar]
- 12.The Transfusion Committee. Putting Patient Safety First. 2nd. Bethesda, Maryland: American Association of Blood Banks; 2013. [Google Scholar]
- 13.The 2011 National Blood Collection and Utilization Report. http://www.hhs.gov/ash/bloodsafety/2011-nbcus.pdf.
- 14.Vestergaard S, Nayfield SG, Patel KV, et al. Fatigue in a Representative Population of Older Persons and Its Association With Functional Impairment, Functional Limitation, and Disability. J Gerontol A Biol Sci Med Sci. 2009;64A(1):76–82. doi: 10.1093/gerona/gln017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001;135(5):313–321. doi: 10.7326/0003-4819-135-5-200109040-00007. [DOI] [PubMed] [Google Scholar]
- 16.Koch CG, Li L, Sun Z, et al. Hospital-acquired anemia: Prevalence, outcomes, and healthcare implications. J Hosp Med. 2013;8(9):506–512. doi: 10.1002/jhm.2061. [DOI] [PubMed] [Google Scholar]
- 17.Meltzer D, Manning WG, Morrison J, et al. Effects of Physician Experience on Costs and Outcomes on an Academic General Medicine Service: Results of a Trial of Hospitalists. Ann Intern Med. 2002;137(11):866–874. doi: 10.7326/0003-4819-137-11-200212030-00007. [DOI] [PubMed] [Google Scholar]
- 18.Carson JL, Grossman BJ, Kleinman S, et al. Red Blood Cell Transfusion: A Clinical Practice Guideline From the AABB*. Ann Intern Med. 2012;157(1):49–58. doi: 10.7326/0003-4819-157-1-201206190-00429. [DOI] [PubMed] [Google Scholar]
- 19.Moreh E, Jacobs JM, Stessman J. Fatigue, function, and mortality in older adults. J Gerontol A Biol Sci Med Sci. 2010;65(8):887–895. doi: 10.1093/gerona/glq064. [DOI] [PubMed] [Google Scholar]
- 20.Eldadah BA. Fatigue and Fatigability in Older Adults. PM&R. 2010;2(5):406–413. doi: 10.1016/j.pmrj.2010.03.022. [DOI] [PubMed] [Google Scholar]
- 21.Hardy SE, Studenski SA. Fatigue Predicts Mortality among Older Adults. J Am Geriatr Soc. 2008;56(10):1910–1914. doi: 10.1111/j.1532-5415.2008.01957.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 23.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 24.HCUP Clinical Classifications Software (CCS) for ICD-9-CM. Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: 2006–2009. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed November 22, 2016. [PubMed] [Google Scholar]
- 25.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol Off J Am Soc Clin Oncol. 1993;11(3):570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 26.Webster K, Cella D, Yost K. The Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System: properties, applications, and interpretation. Health Qual Life Outcomes. 2003;1:79. doi: 10.1186/1477-7525-1-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oken MMMD, Creech RHMD, Tormey DCMD, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. J Clin Oncol. 1982;5(6):649–656. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


