Abstract
Objective
A growing number of patients survive sepsis hospitalizations each year and are at high risk for readmission. However, little is known about temporal trends in hospital-based acute care (ED treat-and-release visits and hospital readmission) after sepsis. Our primary objective was to measure temporal trends in sepsis survivorship and hospital-based acute care use in sepsis survivors. In addition, because readmissions after pneumonia are subject to penalty under the national readmission reduction program, we examined whether readmission rates declined after sepsis hospitalizations related to pneumonia.
Design and Setting
Retrospective, observational cohort study conducted within an academic healthcare system from 2010 to 2015.
Patients
We used three validated, claims-based approaches to identify 17,256 sepsis or severe sepsis hospitalizations to examine trends in hospital-based acute care after sepsis.
Interventions
None
Measurements and Main Results
From 2010–2015, sepsis as a proportion of medical and surgical admissions increased from 3.9% to 9.4%, while in-hospital mortality rate for sepsis hospitalizations declined from 24.1% to 14.8%. As a result, the proportion of medical and surgical discharges at-risk for hospital readmission after sepsis increased from 2.7% to 7.8%. Over 6 years, 30-day hospital readmission rates declined modestly, from 26.4% in 2010 to 23.1% in 2015, driven largely by a decline in readmission rates amongst survivors of non-severe sepsis, and non-pneumonia sepsis specifically, as the readmission rate of severe sepsis survivors was stable. The modest decline in 30-day readmission rates was offset by an increase in ED treat-and-release visits, from 2.8% in 2010 to a peak of 5.4% in 2014.
Conclusions
Owing to increasing incidence and declining mortality, the number of sepsis survivors at risk for hospital readmission rose significantly between 2010 and 2015. The 30-day hospital readmission rates for sepsis declined modestly but were offset by a rise in ED treat-and-release visits.
Sepsis, an acute, life-threatening dysregulated response to infection, affects millions of patients within the United States annually and 30 million worldwide1,2. Studies indicate that the incidence of sepsis, known prior to 2016 as severe sepsis, is increasing at the national level3–5. At the same time, sepsis-related in-hospital mortality appears to be decreasing5–8.
Sepsis survivors frequently experience 30-day hospital readmissions9–19. The costs of hospital readmissions after sepsis have been estimated at 3 billion dollars19, reinforcing sepsis as the most expensive inpatient medical condition20. As part of the Affordable Care Act (ACA), passed in March of 2010, a Hospital Readmissions Reduction Program (HRRP) was developed. Starting in October 2012, financial penalties for hospitals with higher than expected 30-day readmission rates were implemented for targeted conditions (e.g., pneumonia). Despite being the most costly cause of readmission, sepsis is not a targeted condition of the HRRP.
Little is known about the relationship between sepsis incidence, in-hospital mortality, and post-discharge outcomes among sepsis survivors over time. Specific to sepsis survivorship, it is unclear whether the rate of hospital-based acute care use after sepsis, including 30-day hospital readmissions and Emergency Department (ED) treat-and-release visits, has changed over time. To examine these aspects of sepsis, which matter to patients and families21, we conducted a retrospective cohort study within an integrated academic medical center between 2010 and 2015. As a non-targeted condition of the HRRP, we hypothesized that the rate of hospital-based acute care use after sepsis, and 30-day readmission rate and ED treat-and-release visits specifically, would remain stable (i.e., readmission rates would not decrease over time), leading to a rising number of readmissions that follow a recent sepsis hospitalization. Further, we hypothesized that readmission rates after pneumonia – a diagnosis targeted by the HRPP – would decrease over time.
Methods
The University of Pennsylvania Institutional Review Board approved the study (Protocol # 818852) with an informed consent exemption.
Study Design
We conducted a multicenter retrospective cohort study within the University of Pennsylvania Health System (UPHS), an integrated academic health care system consisting of 3 acute care hospitals in Philadelphia, PA: The Hospital of the University of Pennsylvania, Penn Presbyterian and Pennsylvania Hospital.
We evaluated adult medical and surgical admissions to UPHS hospitals between July 1 2010 and June 30 2015. Given the outcomes of interest, and based on prior work9–10, 22, we excluded observation stays, admissions with a disposition of left against medical advice (AMA), transfer to another hospital, or when disposition was missing. In accord with the Agency for Healthcare Research and Quality approach to readmissions23, and prior work9–10, an admission could serve as an index admission and a hospital readmission. For analyses pertaining to re-hospitalization, we limited our analyses to patients discharged alive and not transitioned to hospice, hereafter known as discharges at-risk for hospital readmission. In accordance with our Institutional Review Board, admissions discharged to a correctional facility were excluded from our readmissions analyses.
Data Collection
To examine the incidence, mortality and readmission rates associated with sepsis hospitalizations, we merged administrative and electronic health record datasets. The quality of the administrative dataset using this approach had been previously validated24 and subsequent quality assurance performed9–10. As in prior studies9–10, we collected information on socio-demographics, comorbid conditions, and hospitalizations in the prior year, in addition to hospitalization details.
We identified sepsis using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes, using previously validated approaches1,9–10, 24–25. As the study period pre-dated the 2016 definitions26, we used administrative codes that align with the categories of sepsis, severe sepsis, and septic shock in accord with the 2001 definitions27. We identified sepsis hospitalizations using three approaches: (a) explicit diagnosis codes for sepsis (ICD-9-CM code 995.91), referred to hereafter as explicit sepsis, (b) explicit diagnoses codes for severe sepsis and septic shock (995.92, 785.52), referred to hereafter as explicit severe sepsis, and (c) modified Angus approach of concurrent ICD-9-CM codes for infection (including codes for septicemia) and organ dysfunction1,24–25, referred to hereafter as implicit severe sepsis.
For comparison, we examined 30-day readmission rates after hospitalizations for acute myocardial infarction, congestive heart failure, and pneumonia (independent of sepsis status) over the study period using established ICD-9-CM codes.22 These conditions were selected as they are the high-risk conditions targeted by the HRRP at is inception. Because coding for pneumonia has varied over time28, and given our hypotheses, we also used the pneumonia and sepsis codes to identify three discrete admission categories: (a) pneumonia, non-sepsis admissions, (b) sepsis related to pneumonia admissions, and (c) non-pneumonia sepsis admissions.
Statistical Analyses
To understand temporal changes in sepsis survivorship, we focused on trends in sepsis hospitalizations, sepsis survivors at-risk for hospital readmission, and post-acute care use after sepsis. For post-acute care use, we examined 7- and 30-day all-cause hospital readmission and ED treat-and-release visits within 30 days9,29. We used a nonparametric test for trend across ordered groups (i.e., year) using the nptrend package in the Stata statistical software for the primary analysis.30 This method is an extension of the Wilcoxon rank-sum test but differs in that it examines the ranks for the variable of interest across ordered groups30.
First, we measured the incidence of sepsis hospitalizations and tested for changes over time. We completed this analysis separately for each sepsis coding strategy (explicit sepsis, explicit severe sepsis, and implicit severe sepsis). Next, we measured in-hospital sepsis-related mortality, and again tested for changes over time. Additionally, we evaluated the trends in a composite of in-hospital mortality and discharge to hospice to account for potential hospice discharge practice changes. We also measured whether the proportion of deaths related to sepsis changed over time. We then examined the characteristics of sepsis survivors at-risk for hospital readmission over time.
Next, we evaluated 7- and 30-day all-cause hospital readmissions among sepsis survivors over time. We examined 30-day hospital readmissions after sepsis, and by discrete sepsis coding strategy, by year, to determine whether changes in readmission rates were driven by explicit cases and/or illness severity.
To examine whether readmission rates differed over time according to pneumonia status, we examined readmission rates among the three, aforementioned subgroups: pneumonia, non-sepsis admissions, sepsis related to pneumonia admissions, and non-pneumonia sepsis admissions. As 2010 data began July 1, and 2015 data ended June 30th, annualized volume is presented for these years.
We present the temporal trends in incidence, in-hospital mortality, in-hospital mortality and discharge to hospice, and 30-day readmission, at the monthly level, using 95% confidence intervals in graphical format using a local polynomial smoothing function. For statistical analyses, we used Stata 13 (StataCorp, College Station, Texas). We defined significance as an alpha less than 0.05.
Results
After excluding 80,423 non-medical, non-surgical health system admissions (e.g., obstetrics), 2286 admissions where the patient left AMA, 1777 admissions transferred to an outside hospital, and 333 admissions missing a disposition status, there were 275,600 medical and surgical admissions over 5 years. Of these 275,600 hospitalizations, 17,256 were sepsis hospitalizations (6.3%, 95% confidence interval: 6.2, 6.4), including 7,603 explicit sepsis, 9,709 explicit severe sepsis, and 11,618 implicit severe sepsis.
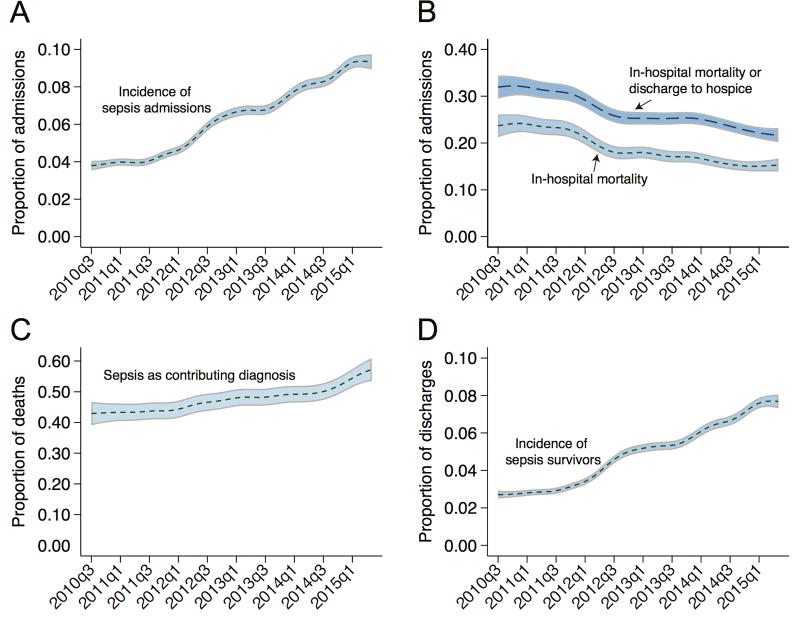
As shown in Table 1 and Figure 1, Panel A, from 2010 to 2015, the proportion of sepsis hospitalizations increased more than two-fold, from 3.9% to 9.4% (p<0.001); the absolute number increased from 2224 in 2010 to 4928 in 2015. Sepsis hospitalizations increased more than two-fold over time and independent of sepsis coding strategy (p<0.001 for explicit sepsis, explicit severe sepsis, and implicit severe sepsis).
Table 1.
Test for trends in sepsis as a proportion of hospital admissions, in-hospital mortality among sepsis admissions, and sepsis survivors as a proportion of discharges at-risk for hospital readmission.
| Year | Sepsis, % of Hospital Admissions * |
In-Hospital Mortality, % for Sepsis Hospitalizations * |
Sepsis Survivors, % of Discharges At- Risk for Hospital Readmission * |
|---|---|---|---|
| 2010 | 3.87 (1112/28740) | 24.10 (268/1112) | 2.72 (751/27608) |
| 2011 | 4.15 (2420/58310) | 23.10 (559/2420) | 2.99 (1669/55902) |
| 2012 | 5.63 (3152/55962) | 18.56 (585/3152) | 4.35 (2327/53498) |
| 2013 | 6.88 (3686/53541) | 17.55 (647/3686) | 5.38 (2743/51004) |
| 2014 | 8.37 (4422/52841) | 15.54 (687/4422) | 6.71 (3367/50216) |
| 2015 | 9.40 (2464/26206) | 14.77 (364/2464) | 7.80 (1950/24997) |
Significant test for trend, p<0.05.
Figure 1.
Temporal trends in sepsis from 2010 to 2015. Panel A depicts the proportion of sepsis hospitalizations among medical and surgical admissions. Panel B depicts in-hospital mortality and in-hospital mortality or transition to hospice at discharge amongst sepsis hospitalizations, respectively. Panel C depicts the proportion of deaths where sepsis contributed. Panel D depicts the proportion of medical and surgical admissions discharged alive and at-risk for hospital readmission over the same time interval. The temporal trends and the 95% confidence intervals were estimated using a local polynomial smoothing function with a bandwidth chosen as the plugin estimator of the asymptotically optimal constant bandwidth.
The in-hospital mortality rate for sepsis hospitalizations declined from 24.1% to 14.8% (p<0.001) (Figure 1, Panel B). Mortality declined over time for all sepsis definitions, p<0.001 (Supplemental Table 1). Despite the decline in sepsis case-fatality rate, given the increase in sepsis incidence, the total number of sepsis-related deaths increased from 536 to 728 from 2010 to 2015, and sepsis contributed to a higher percentage of in-hospital deaths over time (43.4% in 2010 to 55.4% in 2015, Figure 1, Panel C).
As a result of rising sepsis hospitalizations and declining in-hospital mortality, the proportion of medical and surgical discharges at-risk for hospital readmission after a sepsis hospitalization (i.e., sepsis survivors) increased 2.9-fold, from 2.7% in 2010 to 7.8% in 2015 (Figure 1, Panel D). The overall number of sepsis survivors at-risk for readmission increased from 1,502 in 2010 to 3,900 in 2015. The proportion of discharges at-risk for hospital readmission after a pneumonia hospitalization, regardless of sepsis status, began at a higher volume of cases, yet increased just 1.2-fold (2186 hospitalizations in 2010 to 2684 in 2015).
As shown in Supplemental Table 2, the age of sepsis survivors did not differ significantly over time. Clinically important differences, over time, include: a shift in demographics (e.g., more female survivors), a shift in comorbid conditions (e.g., less malignancy amongst survivors), lower illness severity during the hospitalization (e.g., less ICU admission, shock, use of mechanical ventilation, procedures, and shorter hospital length of stay), and survivors were more likely to be discharged to home health services (26.9% to 33.5% over 6 years) and less likely to be discharged to skilled care or long-term acute care facilities.
Over 6 years, the 7- and 30-day hospital readmission rate of sepsis survivors declined modestly, from 8.9% to 8.3% and 26.4% to 23.1%, respectively (Table 2). As a contrast, the 30-day hospital readmission rates were 10.8%, 18.2%, and 21.1% after acute myocardial infarction, heart failure, and pneumonia hospitalizations, respectively, and rates did not decline for any of these conditions between 2010 and 2015 (p=0.67, p=0.14, and p=0.84 for trend).
Table 2.
Trends in 7- and 30-day hospital readmissions and 30-day emergency department (ED) treat-and-release visits after sepsis.
| Year | 7-Day Hospital Readmission, % * |
30-Day ED Treat-and- Release Visit, % * |
30-Day Hospital Readmission, % * |
|---|---|---|---|
| 2010 | 8.92 (67/751) | 2.80 (21/751) | 26.36 (198/751) |
| 2011 | 9.89 (165/1669) | 3.36 (56/1669) | 26.30 (439/1669) |
| 2012 | 8.59 (200/2327) | 4.51 (105/2327) | 26.56 (618/2327) |
| 2013 | 9.15 (251/2743) | 5.21 (143/2743) | 25.96 (712/2743) |
| 2014 | 7.45 (251/3367) | 5.41 (182/3367) | 24.98 (841/3367) |
| 2015 | 8.31 (162/1950) | 4.67 (91/1950) | 23.08 (450/1950) |
Significant test for trend, p<0.05.
The decline in 30-day all-cause hospital readmission after sepsis was offset by an increase in the rate of ED treat-and-release visits (from 2.8% in 2010 to a peak of 5.4% in 2014, p=0.001). Additionally, despite the modest decline in readmission rates after sepsis, the total number of 7- and 30-day hospital readmissions of sepsis survivors increased nearly three-fold, from 134 to 324, and 396 to 900, respectively.
The modest decline in 30-day all-cause hospital readmission after sepsis was present amongst explicit sepsis cases (p=0.005), but not among explicit or implicit severe sepsis cases (p=0.49 and p=0.77, respectively) (Table 3). After combining explicit and implicit severe sepsis coding strategies, 30-day hospital readmission rates declined from 27.6% in 2010 to 22.9% in 2015 after sepsis (p=0.005), but not after severe sepsis (26.4% in 2010 to 24.4% in 2015, p=0.58) (Supplemental Table 3). Contrary to our hypothesis, the declining readmission rate after sepsis was not explained by pneumonia admissions. Rather, there was a modest reduction in readmission rates after non-pneumonia sepsis admissions (p=0.01).
Table 3.
Trends in 30-day hospital readmission rates after sepsis admissions identified using explicit codes and severe sepsis identified using explicit and implicit codes and by pneumonia status.
| Readmission Rates by Explicit and Implicit Codes | |||
| Year | 30-Day Hospital Readmission Rates After Explicit Sepsis, % * | 30-Day Hospital Readmission Rates After Explicit Severe Sepsis, % | 30-Day Hospital Readmission Rates After Implicit Severe Sepsis, % |
| 2010 | 27.61 (103/373) | 25.41 (94/370) | 26.69 (126/472) |
| 2011 | 27.15 (227/836) | 25.58 (210/821) | 25.64 (270/1053) |
| 2012 | 25.95 (288/1110) | 27.19 (332/1221) | 27.06 (390/1441) |
| 2013 | 23.63 (337/1426) | 28.50 (375/1316) | 28.05 (451/1608) |
| 2014 | 23.93 (457/1910) | 26.36 (387/1468) | 26.85 (504/1877) |
| 2015 | 22.89 (263/1149) | 23.40 (190/812) | 24.95 (261/1046) |
| Readmission Rates by Pneumonia and Sepsis Status | |||
| Year | 30-Day Hospital Readmission After Pneumonia, Non-Sepsis Admissions, % | 30-Day Hospital Readmission After Sepsis Related to Pneumonia Admissions, % | 30-Day Hospital Readmission After Non-Pneumonia Sepsis Admissions, % * |
| 2010 | 18.32 (174/950) | 23.78 (34/143) | 26.97 (164/608) |
| 2011 | 20.11 (418/2079) | 23.23 (95/409) | 27.30 (344/1260) |
| 2012 | 21.82 (384/1760) | 25.42 (135/531) | 26.89 (483/1796) |
| 2013 | 20.75 (344/1658) | 26.27 (166/632) | 25.86 (546/2111) |
| 2014 | 18.48 (287/1553) | 25.09 (199/793) | 24.94 (642/2574) |
| 2015 | 19.51 (168/861) | 20.37 (98/481) | 23.96 (352/1469) |
Significant test for trend, p<0.05.
Discussion
In this multicenter observational study within an academic health system, we examined trends in hospital-based acute care use after sepsis, including 30-day hospital readmissions and Emergency Department treat-and-release visits, over a six-year period. Consistent with previous reports using national data1,3–5,31–34, we found a rising volume of sepsis hospitalizations and declining in-hospital mortality rate. As a result, sepsis survivors at-risk for hospital readmission increased nearly three-fold over time, suggesting that the growing number of sepsis survivors is not limited to Medicare beneficiaries35. Given the long-term consequences of sepsis, which include recurrent infections and cognitive and physical impairment10–11,36–37, this is a significant public health threat.
We found that the characteristics of sepsis survivors changed over time (e.g., more female survivors, lesser illness severity). For example, in 2010, 57% of sepsis survivors required ICU admission, compared to 35% in 2015. These observations reinforce the Stage Migration Effect (i.e., with increased awareness comes increased identification, often of cases with milder stages of disease).38 These temporal shifts also highlight the importance of raising awareness of sepsis survivorship across ICUs and wards, both for evaluating the past medical history of newly admitted patients (i.e., is this patient a sepsis survivor?) and for discharge planning and anticipatory guidance, as 42% of hospital-based care encounters after sepsis may be preventable with effective out-patient management.15
Between 2010 and 2015, the rate of 7- and 30-day hospital readmission after sepsis remained high, with rates higher than the HRRP targeted conditions. While 30-day readmission rates declined, the improvements were modest, decreasing from 28% in 2010 to 23% in 2015 after explicit sepsis and from 26% in 2010 to 24% in 2015 after severe sepsis. We found that readmission rates were largely similar after sepsis and severe sepsis, and both exceeded nationally targeted conditions. These findings, which suggest that patients hospitalized with infection who exhibit a systemic inflammatory response without overt organ dysfunction (i.e., sepsis in Sepsis-2) incur a readmission risk similar to those with organ dysfunction, require confirmation.
Further, the modest reduction in the 30-day hospital readmission rate was offset by an increase in the rate of ED treat-and-release visits. As a result, the rate of hospital-based acute care use after sepsis remained largely unchanged. Coupled with an expanding population of sepsis survivors, the total number of 30-day hospital readmissions after sepsis increased three-fold over 6 years.
Recent evaluations of the national impact of the HRRP demonstrated declines in hospital readmissions among targeted conditions and non-targeted conditions, with greater declines in the targeted conditions39. Contrary to our hypothesis, we did not observe a decline in readmission rates after pneumonia. Rather, we found that readmission rates declined modestly among non-pulmonary sources of sepsis (e.g., urinary tract infection) and, potentially related, among those with less severe cases (e.g., explicit sepsis). While there is no clear signal that readmission rates differ by source of infection at the time of the index admission10, additional studies examining the relationship between the index sepsis admission and infection-related readmission are needed.
Our findings support the growing recommendations that sepsis warrants national attention as a targeted condition for acute care and post-acute care performance metrics18,40–41. To date, there has been little evaluation of hospital discharge practices after sepsis. We previously reported a notable lack of timely post-discharge follow-up for septic shock survivors, as most survivors are readmitted within 14 days11, leaving many readmitted prior to their scheduled appointments. Even less attention is placed on what should happen during primary care follow-up visits after sepsis. Notably, nearly 70% of unplanned hospital readmissions after sepsis are due to infections--about half of which are relapse or recrudesce of the initial infection and half are new11,42. Such results suggest that sepsis survivors are particularly susceptible to reinfection and may benefit from careful monitoring for recrudescence of infections.
The required care coordination is specifically challenging among this patient population, as sepsis survivors are two times more likely to be discharged to skilled nursing facilities and ten times more likely to require long term acute care hospital placement compared to non-sepsis patients9. To improve post-discharge outcomes after sepsis, comprehensive, coordinated multidisciplinary approaches to caring for sepsis survivors are needed. Given the growth in home health services that we observed after sepsis, and evidence that early and intense home health visits can reduce hospital readmission43, novel interventions applied to home health services and focused on ambulatory care sensitive conditions15 for sepsis survivors are warranted. A successful program will likely include a number of facets, including continuity between inpatient, post-acute care services, and outpatient providers, antibiotic stewardship, management of sepsis specific impairments, and surveillance for new or recurrent infection. Provider education will be an essential component, but likely incomplete without engaging survivors and caregivers to facilitate self-care. Empowerment, potentially augmented by survivors supporting one another44, could expedite realization of readmission reductions45.
Our findings suggest a number of future directions. First, investigation is warranted to determine the role that readmissions, and infection-related readmissions in particular, play in the long-term mortality risk of sepsis survivors. Future studies should examine the timing and location of death and hospice use in the year after sepsis. Second, given the growth in ED treat-and-release visits, a greater understanding of the nature of treatment delivered during these encounters, and subsequent outcomes, are warranted. Third, post-discharge, novel surveillance strategies, leveraging mobile health technology, may prove useful to identify a new or recurrent infection. Last, while studies have examined risk factors associated with hospital readmission after sepsis, important questions (e.g., do outcomes differ between culture-positive and culture-negative sepsis cases) remain unanswered.
Limitations
There are important limitations to this study. This study is limited to three hospitals within a single academic center; confirmatory studies are justified. Although we included hospital transfers to increase our readmission captures, we acknowledge that the rate is likely an underestimate as we were unable to identify readmissions outside of UPHS. However, we are not aware of any systematic changes over the study period that would bias the measurements of trend. There is no perfect method for identifying sepsis hospitalizations in claims data and we acknowledge temporal trends in clinical documentation and coding practice. For this reason, we used multiple, validated methods to identify sepsis hospitalizations. As sepsis cohorts derived from administrative datasets tend to be more severely ill24, changes in documentation likely reflect a more accurate picture of the overall disease burden of sepsis and its outcomes, while admittedly overestimating the increase in sepsis incidence and the decline in sepsis-related mortality. Future studies should utilize objective clinical data based abstraction methods to confirm our findings related to hospital readmissions.
Conclusion
In a retrospective cohort study conducted within an academic center over 6 years, we observed a growing population of sepsis survivors who experienced a high rate of 7- and 30-day hospital readmissions. The modest decline in 30-day hospital readmission rates after sepsis was countered by a rise in ED treat-and-release visits, revealing a potential shift in hospital-based acute care after sepsis.
Supplementary Material
Acknowledgments
Drs. Prescott and Mikkelsen received support for article research from the National Institutes of Health (NIH). Dr. Prescott’s institution received funding from the NIH, and she disclosed government work. Dr. Bowles’s institution received funding from the National Institute of Nursing Research and the Agency for Healthcare Quality and Research, and she disclosed that she receives licensing royalties from the University of Pennsylvania not related to this topic.
Funding:
The study was supported in part by the National Institutes of Health, National Institute of Nursing Research (NIH NINR R01 NR016014 01) (KB, MEM). Dr. Prescott is supported in part by NIH/NIGMS K08 GM115859. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Copyright form disclosure: The remaining authors have disclosed that they do not have any potential conflicts of interest.
For each of the above authors, no financial or other potential conflicts of interest exist related to the work.
References
- 1.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Reinhart K, Daniels R, Kissoon N, et al. Recognizing sepsis as a global health priority – a WHO resolution. N Engl J Med. 2017 doi: 10.1056/NEJMp1707170. [DOI] [PubMed] [Google Scholar]
- 3.Gaieski DF, Edwards JM, Kallans MJ, et al. Benchmarking the incidence and mortality of severe sepsis in the United States. Crit Care Med. 2013;41:1167–74. doi: 10.1097/CCM.0b013e31827c09f8. [DOI] [PubMed] [Google Scholar]
- 4.Rhee C, Murphy MV, Li L, Platt R, Klompas M, Centers for Disease Control and Prevention Epicenters Program Comparison of trends in sepsis incidence and coding using administrative claims vs. objective clinical data. Clin Infect Dis. 2015;60(1):88–95. doi: 10.1093/cid/ciu750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kadri SS, Rhee C, Strich JR, et al. Estimating ten-year trends in septic shock incidence and mortality in United States academic medical centers using clinical data. Chest. 2017;151:278–285. doi: 10.1016/j.chest.2016.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaukonen KM, Bailey M, Suzuki S, et al. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000–2012. JAMA. 2014;311(13):1308–16. doi: 10.1001/jama.2014.2637. [DOI] [PubMed] [Google Scholar]
- 7.Stevenson EK, Rubenstein AR, Radin GT, Wiener RS, Walkey AJ. Two decades of mortality trends among patients with severe sepsis: a comparative meta-analysis. Crit Care Med. 2014;42(3):625–631. doi: 10.1097/CCM.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prescott HC, Kepreos KM, Wiitala WL, Iwashyna TJ. Temporal changes in the influence of hospitals and regional healthcare networks on severe sepsis mortality. Crit Care Med. 2015;43(7):1368–1374. doi: 10.1097/CCM.0000000000000970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones TK, Fuchs BD, Small DS, et al. Post-acute care use and hospital readmission after sepsis. Ann Am Thorac Soc. 2015;12(6):904–13. doi: 10.1513/AnnalsATS.201411-504OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sun A, Netzer G, Small DS, et al. Association between index hospitalization and hospital readmission in sepsis survivors. Crit Care Med. 2016;44:478–87. doi: 10.1097/CCM.0000000000001464. [DOI] [PubMed] [Google Scholar]
- 11.Ortego A, Gaieski DF, Fuchs BD, et al. Hospital- based acute care use in survivors of septic shock. Crit Care Med. 2015;43:729–37. doi: 10.1097/CCM.0000000000000693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donnelly JP, Hohmann SF, Wang HE. Unplanned readmissions after hospitalization for severe sepsis at academic medical center-affiliated hospitals. Crit Care Med. 2015;43(9):1916–27. doi: 10.1097/CCM.0000000000001147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elixhauser A, Steiner C. HCUP statistical brief #161. Rockville (MD): Agency for Healthcare Research and Quality; 2013. Readmissions to U.S. hospital by diagnosis, 2010. Available at: www.hcup-us.ahrq.gov/reports/statbriefs/sb153.pdf. [PubMed] [Google Scholar]
- 14.Prescott HC, Langa KM, Liu V, et al. Increased one- year health care utilization in survivors of severe sepsis. Am J Respir Crit Care Med. 2014;190(1):62–9. doi: 10.1164/rccm.201403-0471OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prescott HC, Langa KM, Iwashyna TJ. Readmission diagnoses after hospitalization for severe sepsis and other acute medical conditions. JAMA. 2015;313(10):1055–7. doi: 10.1001/jama.2015.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Norman BC, Cooke CR, Ely EW, et al. Sepsis-associated 30-day risk-standardized readmissions: analysis of a nationwide medicare sample. Crit Care Med. 2017;45(7):1130–1137. doi: 10.1097/CCM.0000000000002476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Prescott HC. Variation in postsepsis readmission patterns: a cohort study of veterans affairs beneficiaries. Ann Am Thorac Soc. 2017;14(2):230–237. doi: 10.1513/AnnalsATS.201605-398OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mayr FB, Talisa VB, Balakumar V, et al. Proportion and cost of unplanned 30-day readmissions after sepsis compared with other medical conditions. JAMA. 2017;317(5):530–531. doi: 10.1001/jama.2016.20468. [DOI] [PubMed] [Google Scholar]
- 19.Goodwin AJ, Rice DA, Simpson KN, et al. Frequency, cost, and risk factors of readmissions among severe sepsis survivors. Crit Care Med. 2015;43:738–46. doi: 10.1097/CCM.0000000000000859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Torio C, Andrews R. National inpatient hospital costs: the most expensive conditions by payer, 2011. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb204-Most-Expensive-Hospital-Conditions.pdf. [PubMed]
- 21.Groff AC, Colla CH, Lee TH. Days spent at home – a patient-centered goal and outcome. N Engl J Med. 2016;375:1610–1612. doi: 10.1056/NEJMp1607206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, Barreto-Filho JA, Kim N, Bernheim SM, Suter LG, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013;309:355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barrett M, Raetzman S, Andrews R. HCUP Methods Series Report #2012-04. U.S. Agency for Healthcare Research and Quality; Overview of key readmission measures and methods. 2012. ONLINE December 20, 2012. Available at: http://www.hcupus.ahrq.gov/reports/emthods/methods.jsp. [Google Scholar]
- 24.Whittaker SA, Mikkelsen ME, Gaieski DF, Koshy S, Kean C, Fuchs BD. Severe sepsis cohorts derived from claims-based strategies appear to be biased toward a more severely ill patient population. Crit Care Med. 2013;41:945–953. doi: 10.1097/CCM.0b013e31827466f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Iwashyna TJ, Odden A, Rohde J, et al. Identifying patients with severe sepsis using administrative claims: patient-level validation of the Angus implementation of the international consensus conference definition of severe sepsis. Med Care. 2014;52:e39–e43. doi: 10.1097/MLR.0b013e318268ac86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31(4):1250–1256. doi: 10.1097/01.CCM.0000050454.01978.3B. [DOI] [PubMed] [Google Scholar]
- 28.Lindenauer PK, Lagu T, Shieh MS, Pekow PS, Rothberg MB. Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA. 2012;307:1405–1413. doi: 10.1001/jama.2012.384. [DOI] [PubMed] [Google Scholar]
- 29.Vashi AA, Fox JP, Carr BG, et al. Use of hospital-based acute care among patients recently discharged from the hospital. JAMA. 2013;309:364–371. doi: 10.1001/jama.2012.216219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cuzick J. A Wilcoxon-type test for trend. Stat Med. 1985;4:87–90. doi: 10.1002/sim.4780040112. [DOI] [PubMed] [Google Scholar]
- 31.Bouza C, Lopez-Cuadrado T, Amate-Blanco JM. Use of explicit ICD9-CM codes to identify adult severe sepsis: impacts on epidemiological estimates. Crit Care. 2016;20(1):313. doi: 10.1186/s13054-016-1497-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rhee C, Murphy MV, Li L, Platt R, Klompas M, Centers for Disease Control and Prevention Epicenters Program Comparison of trends in sepsis incidence and coding using administrative claims vs. objective clinical data. Clin Infect Dis. 2015;60(1):88–95. doi: 10.1093/cid/ciu750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rhee C, Kadri S, Huang SS, Murphy MV, Li L, Platt R, Klompas M. Objective sepsis surveillance using electronic clinical data. Infect Control Hosp Epidemiol. 2016;37(2):163–71. doi: 10.1017/ice.2015.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kadri SS, Rhee C, Strich JR, et al. Estimating ten-year trends in septic shock incidence and mortality in United States academic medical centers using clinical data. Chest. 2017;151:278–285. doi: 10.1016/j.chest.2016.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Iwashyna TJ, Cooke CR, Wunsch H, Kahn JM. The population burden of long-term survivorship after severe sepsis among older Americans. J Am Geriatr Soc. 2012;60(6):1070–1077. doi: 10.1111/j.1532-5415.2012.03989.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Maley JH, Mikkelsen ME. Short-term gains with long-term consequences: the evolving story of sepsis survivorship. Clin Chest Med. 2016;37(2):367–380. doi: 10.1016/j.ccm.2016.01.017. [DOI] [PubMed] [Google Scholar]
- 37.Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304:1787–1794. doi: 10.1001/jama.2010.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Iwashyna TJ, Angus DC. Declining case fatality rates for severe sepsis: good data bring good news with ambiguous implications. JAMA. 2014;311(13):1295–1297. doi: 10.1001/jama.2014.2639. [DOI] [PubMed] [Google Scholar]
- 39.Zuckerman RB, Sheingold SH, Orav EJ, et al. Readmissions, observation, and the hospital readmissions reduction program. N Engl J Med. 2016;374:1543. doi: 10.1056/NEJMsa1513024. [DOI] [PubMed] [Google Scholar]
- 40.Cooke CR, Iwashyna TJ. Sepsis mandates: improving inpatient care while advancing quality improvement. JAMA. 2014;312:1397–1398. doi: 10.1001/jama.2014.11350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chang DW, Tseng CH, Shapiro MF. Rehospitalizations following sepsis: common and costly. Crit Care Med. 2015;43(10):2085–93. doi: 10.1097/CCM.0000000000001159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.DeMerle KM, Royer SC, Mikkelsen ME, Prescott HC. Readmissions for recurrent sepsis: new or relapsed infection? Crit Care Med. 2017 doi: 10.1097/CCM.0000000000002626. ePub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Murtaugh CM, Deb P, Zhu C, et al. Reducing readmissions among heart failure patients discharged to home health care: effectiveness of early and intensive nursing services and early physician follow-up. Health Serv Res. 2016 doi: 10.1111/1475-6773.12537. ePub ahead of print July 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mikkelsen ME, Jackson JC, Hopkins RO, et al. Peer support as a novel strategy to mitigate post-intensive care syndrome. AACN Adv Crit Care. 2016;27(2):221–229. doi: 10.4037/aacnacc2016667. [DOI] [PubMed] [Google Scholar]
- 45.Leppin AL, Gionfriddo MR, Kessler M, et al. Preventing 30-day hospital readmissions: a systematic review and meta-analysis of randomized trials. JAMA Intern Med. 2014;174(7):1095–1107. doi: 10.1001/jamainternmed.2014.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.