CONSPECTUS
The successful development of a noninvasive blood glucose sensor that can operate reliably over sustained periods of time has been a much sought after but elusive goal in diabetes management. Since diabetes has no well-established cure, control of elevated glucose levels is critical for avoiding severe secondary health complications in multiple organs including the retina, kidney and vasculature. While fingerstick testing continues to be the mainstay of blood glucose detection, advances in electrochemical sensing-based minimally invasive approaches have opened the door for alternate methods that would considerably improve the quality of life for people with diabetes. In the quest for better sensing approaches, optical technologies have surfaced as attractive candidates as researchers have sought to exploit the endogenous contrast of glucose, notably its absorption, scattering, and polarization properties. Vibrational spectroscopy, especially spontaneous Raman scattering, has exhibited substantial promise due to its exquisite molecular specificity and minimal interference of water in the spectral profiles acquired from the blood-tissue matrix. Yet, it has hitherto been challenging to leverage the Raman scattering signatures of glucose for prediction in all but the most basic studies and under the least demanding conditions.
In this Account, we discuss the newly developed array of methodologies that address the key challenges in measuring blood glucose accurately using Raman spectroscopy and unlock new prospects for translation to sustained noninvasive measurements in people with diabetes. Owing to the weak intensity of spontaneous Raman scattering, recent research has focused on enhancement of signals from the blood constituents by designing novel excitation-collection geometries and tissue modulation methods while our attempts have led to the incorporation of nonimaging optical elements. Additionally, invoking mass transfer modeling into chemometric algorithms has not only addressed the physiological lag between the actual blood glucose and the measured interstitial fluid glucose values but also offered a powerful tool for predictive measurements of hypoglycemia. This framework has recently been extended to provide longitudinal tracking of glucose concentration without necessitating extensive a priori concentration information. These findings are advanced by the results of recent glucose tolerance studies in human subjects, which also hint at the need for designing nonlinear calibration models that can account for subject-to-subject variations in skin heterogeneity and hematocrit levels. Together, the emerging evidence underscores the promise of a blood withdrawal-free optical platform—featuring a combination of high-throughput Raman spectroscopic instrumentation and data analysis of subtle variations in spectral expression—for diabetes screening in the clinic and, ultimately, for personalized monitoring.
Graphical abstract
1. INTRODUCTION
Nearly four decades after the commercialization of the first analyzer for blood glucose, noninvasive continuous measurement of this key metabolite persists as an outstanding challenge in the biomedical sciences. Given the lack of a well-established cure for chronic disorders of glucose homeostasis, careful management of blood glucose levels through frequent monitoring is critical to maintaining tight glycemic control and, consequently, avoiding serious health complications of diabetes such as higher risks of heart disease, kidney failure, or blindness. While the binding affinity of glucose to proteins in the bloodstream yields key long-term glycemic markers (e.g., glycated hemoglobin and glycated albumin),1 blood withdrawal-based glucose measurements remain the gold standard for diagnosis and therapeutic decision making in people with diabetes (PWD). The significance of glucose biosensors can be evidenced by the fact that they account for nearly 80% of all biosensors in the current world market.2 Although these tremendous opportunities have led to significant advances in electrochemical glucose biosensors, the promise of noninvasive personal glucose testing is still to be realized. A noninvasive sensor would eliminate the pain and inconvenience associated with fingerstick testing, thus making a transformative impact on the quality of life of PWD.
Numerous innovative designs to replace fingerstick testing have been put forth and tested with varying degrees of success. Broadly speaking, these proposals fall into two types of categories: (1) minimally invasive devices, which comprise the subcutaneous electrochemical sensors as well as optical contrast agent-based approaches; and (2) fully noninvasive prototypes. Minimally invasive blood glucose monitoring techniques entail the insertion of an indwelling sensor under the skin to measure the glucose concentration from interstitial fluid (ISF). They exploit a wide variety of mechanisms and exogenous labels to quantify glucose levels and include glucose oxidase and mediator-based amperometric sensors,3 glucose-responsive fluorescence protein, and functionalized carbon nanotube reporters,4 and microneedle-based glucose monitoring systems.5 While these constructs partially alleviate the pain of regular fingerstick testing and have resulted in a handful of United States Food and Drug Administration (FDA)-approved devices, several of the prototypes suffer from long-term stability concerns (and therefore require frequent recalibration) and susceptibility to biofouling. In principle, a shift toward fully noninvasive approaches would address all these limitations while also reducing the inconvenience of indwelling subcutaneous sensors. However, practical realization of these approaches in clinical settings has proven to be challenging and forms the focal point of ongoing research efforts.
Label-free photonic methods, in particular, have attracted considerable attention, due to the potential of nonperturbative measurements and simultaneous analysis of other blood constituents with minimal change in the diagnostic platform. Researchers have sought to directly exploit the endogenous optical attributes of glucose, such as absorption, optical rotation and inelastic scattering (see Figure 1).6 Combining the penetration depth of near-infrared (NIR) light and unique molecular fingerprinting capability, vibrational spectroscopy has offered the most promising results.7,8 Several laboratories, including our own, have focused on advancing Raman spectroscopy through investigations in test samples of progressively higher complexity.9,10 To determine glucose concentrations from subtle variances in spectral signatures, construction of multivariate calibration models, which can identify a subset of pixels sharing (un)known biochemical functions, has formed a cornerstone of the research efforts.
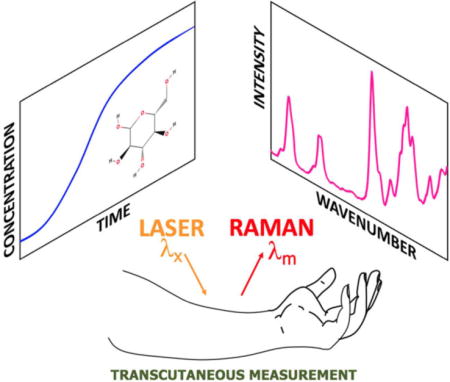
Figure 1.
Schematic of Raman spectroscopy-based transcutaneous blood glucose detection. Illustration of glucose molecules in bloodstream and interstitial fluid, and the generation of Raman spectrum from noninvasive interrogation of the fingertip.
Until recently, however, studies that directly address the nonanalyte specific variances in the calibration models have been lacking. The progress toward clinical translation has been halting with the inability to convert the promising results in controlled settings to sustained accurate measurements in PWD. Emerging reports have aimed to fill this missing gap by accounting for sample-to-sample variability in tissue absorption and elastic scattering11 as well as autofluorescence and photobleaching of endogenous chromophores.12 Physiological factors that lead to imprecision in glucose prediction, prominently differences between blood and ISF glucose levels13 and fluctuations in hydration, turgor and hematocrit, have also been examined. Importantly, the development of tissue modulation interfaces14 and incorporation of customized nonimaging optical elements15 have considerably boosted the collection efficiency of Raman photons from the blood analytes. The conception of nonlinear calibration models has further allowed modeling of curved effects in the spectra-concentration relationship16 and steps toward a calibration-free approach17 has opened the door for CGM without necessitating interventions at intermediate time points.
This Account presents and critically discusses the results of this recent activity in terms of instrumentation development and innovative algorithmic frameworks. Promising approaches to counter the persistent challenges that hamper adoption of the otherwise transformative noninvasive glucose sensing method and an outlook of its bench-to-bedside translation is also presented.
2. TOWARD NONINVASIVE GLUCOSE MONITORING
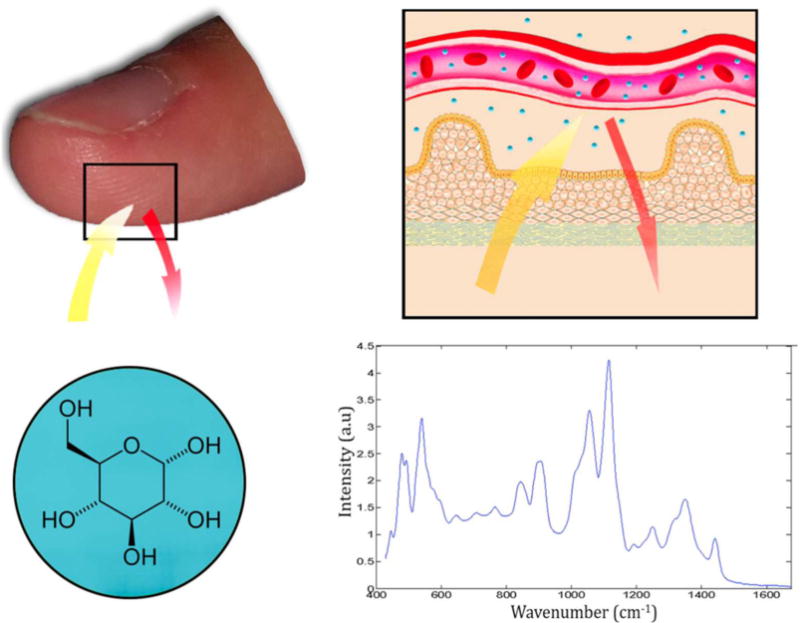
In the quest for less invasive methods for glucose detection, the first design embodiments employed the electrochemical sensing principles of lancet-based glucose meters—the evolution of which forms a separate intriguing story that has been detailed elsewhere.3,18 These subcutaneous sensors have reached a stable configuration consisting of a fine needle or flexible wire, with the active sensing element at or near the tip and implanted in the subcutaneous tissue. A radically different advancement was pioneered by Kost and co-workers19 based on ultrasound facilitation of the outward transport (and subsequent measurement) of ISF glucose. While initial results in preclinical studies were promising with minimal pain or damage to the skin being reported, the singular challenge of designing a reliable sensor for measuring small amounts of ISF glucose in a high ionic strength hydrogel environment (due to swamping of Donnan potential) has stymied significant progress. Searching for an optical solution to this pressing need, several approaches entailing the use of exogenous fluorescence labels have been espoused. The central idea is to implant fluorescence probe(s) beneath the skin and to interrogate it by using either an indwelling fiber optic component or an optical sensor from outside the body. For instance, Shibata et al. synthesized injectable polyacrylamide hydrogel microbeads based on fluorescent monomers featuring diboronic acid that enable reversible responsiveness to glucose and offer sufficient intensity to transdermally monitor glucose concentrations (Figure 2A).20 An intriguing advance has been the development of single-walled carbon nanotubes as fluorescence-emitting components of in vivo glucose sensors. Strano and co-workers have leveraged carbon nanotubes to construct an enzyme-based optical glucose sensor (Figure 2B) and also utilized protein competitive binding for a reversible glucose affinity sensor.21 Furthermore, implantable glucose sensors, harnessing surface enhanced Raman scattering (SERS)-active surfaces and the chemical functionalization of those surfaces with self-assembled monolayers (SAMs), have been proposed by the van Duyne group (Figure 2C–F).22,23 The ISF glucose measurements by this sensor and its recent derivative based on spatially offset SERS,24 which demonstrated continuous monitoring capability in rats for over 17 days after implantation, have been encouraging. Despite the promising results, additional investigations into the long-term safety profile and biocompatibility for these implantable sensor constructs are required prior to clinical translation.
Figure 2.
Toward noninvasive blood glucose monitoring. (A) Schematic of transdermal glucose monitoring using injectable glucose responsive fluorescent hydrogel microbeads. (Reprinted with permission from ref 20. Copyright 2010 National Academy of Sciences.) (B) Enzyme-based optical glucose sensor realized on a single-walled nanotube platform. Photograph shows a 200 μm × 1 cm capillary containing the SWNT solution. Corresponding fluorescence intensity map across capillary is shown alongside the reaction dynamics. (Adapted with permission from ref 21. Copyright 2005 Nature Publishing Group.) (C) Schematic of experimental setup used for SERS based in vivo glucose monitoring in a rat bearing surgically implanted sensor. (D) Fabrication of sensor by deposition of silver through a mask of self-assembled nanospheres and their functionalization by successive emersions in ethanolic solutions of decanethiol and mercaptohexanol. (E) Atomic force micrograph of the fabricated structure. (F) Position of localized surface plasmon resonance following functionalization. ((C–F) Reprinted with permission from ref 22. Copyright 2006 American Chemical Society.)
Fully noninvasive optical approaches present a paradigmatic shift in the manner of application, as they exploit the intrinsic light-matter interactions within the blood-tissue matrix. Owing to its unique molecular fingerprinting capability, vibrational spectroscopy, namely, absorption in the mid- and near-infrared regions and spontaneous Raman scattering, has received the greatest attention. In spite of the sharp spectral features, NIR spectroscopy is severely limited by its penetration depth due to the high absorptivity of water in this wavelength range. While shifting to the NIR regime solves the issue of penetration depth, molecular specificity is significantly reduced by the presence of broader spectral features. Because the NIR absorption spectrum encodes information by probing the overtone and combination vibrational transitions of the molecules, spectral congestion among many overlapping features poses a serious hurdle. Nevertheless, several research groups have reported successful NIR absorption based blood glucose measurements.7,25 Yet, the validity of NIR glucose sensing studies has since been questioned, owing to the possibility of model development based on spurious spectral correlations.26
On the other hand, Raman scattering offers a complementary spectroscopic approach where the vibrational transitions alter the polarizability of the molecule and yields sharp spectral features in the recorded profile. Inspired by its unequivocal detection capability without issues of photostability and minimal interference from water, we and others have used Raman spectroscopy, in conjunction with chemometric analysis, to interrogate glucose levels.10,27–31 Using a wide range of study protocols ranging from glucose clamping in animal models to glucose tolerance tests in humans, we have demonstrated that, despite the lower intensity of glucose Raman-scattered signal, the developed models are more robust in relation to NIR absorption.29
3. NIR RAMAN SPECTROSCOPY BASED GLUCOSE SENSING
Raman spectroscopy exploits the inelastic scattering of photons to probe the structure and dynamics of molecules through their vibrational transitions. The shift in the initial and final vibrational states of the molecule is manifested in the form of characteristic spectral patterns, termed Raman fingerprints. Specifically, for the detection of blood glucose, a laser beam is subjected on the anatomical site under consideration and the Raman photons thus generated from the constituents of the blood tissue matrix are recorded (Figure 3A). Owing to the transcutaneous nature of measurement, selection of the excitation wavelength is critical to navigating the interplay of tissue autofluorescence and photodamage, Raman scattering cross section, and sample turbidity. NIR laser excitation is preferred, as it not only provides higher penetration depth in the “tissue-transparent” diagnostic window but also largely suppresses (but does not eliminate) the autofluorescence signal. Additionally, thermal and photochemical damage as well as potential mutagenic changes are minimized by the use of low energy NIR light. Efficient light detection, typically facilitated by deep depletion, back-illuminated charge coupled devices (CCD), also constitute a critical design aspect in order to alleviate the weak sensitivity of the Raman signal from glucose.
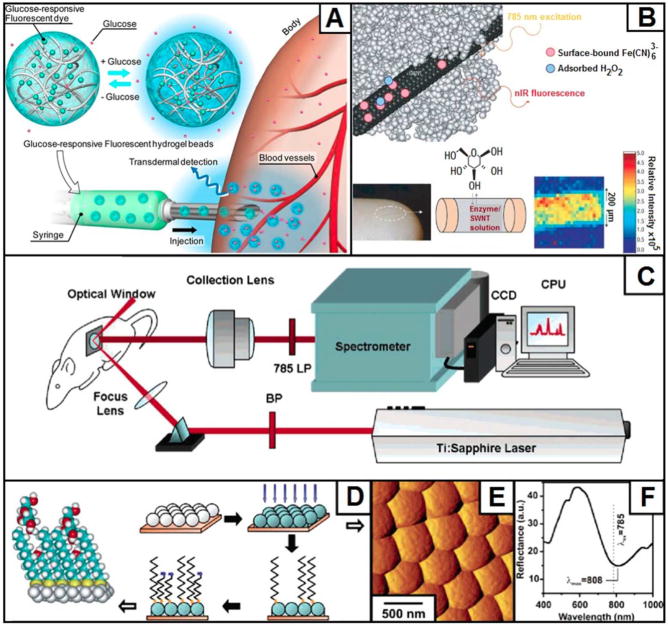
Figure 3.
Instrumentation for noninvasive near-infrared spectroscopic probing of human fingertip. (A) Fiber probe based portable Raman spectroscopic system developed for transcutaneous glucose monitoring in backscattering configuration. (B) Optical fiber probe showing arrangement of excitation and emission fibers relative to the other optical components. (C) Portable Raman system in transmission mode. (D) CHC used for enhancing light collection, as viewed from the output aperture. (E) Side view of the Raman spectroscopy setup in transmission configuration showing the position of CHC relative to excitation and collection fibers. (F) and (G) Active tissue modulation interface incorporated into measurement device. ((C–E) Reprinted with permission from ref 15. Copyright 2011 AIP Publishing LLC. (F, G) Reprinted with permission from ref 14. Copyright 2011 AIP Publishing LLC.)
Furthermore, due to the intrinsic advantages of system portability and ease of clinical translation, considerable efforts have been made to develop tailored optical fiber probes for delivery and collection of light to and from the tissue interface.32,33 The underlying idea for the probe design is to maximize signal collection while suppressing confounding signals generated in the fiber probe itself. One of the earliest, and most extensively used, design embodiments consists of a central excitation fiber surrounded by an annular ring of collection fibers (Figure 3B). The selection of the fiber parameters (i.e., dimension and numerical aperture) is based on optical design strategy focused on achieving maximum system etendué (AΩ product). The fiber probe tip also houses a specialized set of filters as well as a half-ball lens that serves to enhance collection efficiency. Recently, other prototypes featuring graded-index (GRIN) lens and hollow-core photonic crystal fibers have emerged for biomedical applications and can be adopted for glucose sensing.34
While most tissues are highly scattering and therefore emit photons at a wide angular range, traditional optical systems, both free-space and fiber probe-based, can collect scattered photons within a limited acceptance angle specified by their effective numerical apertures. In this milieu, a collection system that can redirect the light scattered at steep angles to be collimated within a limited range of conic half angles is highly desirable. To achieve this, the incorporation of nonimaging elements, such as gold-coated off-axis paraboloidal mirrors,35 sapphire ball lens,32 and compound parabolic concentrators (CPC),36 has been advocated by us and others. Although hollow gold-coated CPC offers very efficient light collection, the physical size makes it impractical for routine use in clinical diagnostic devices. On the other hand, compound hyperbolic concentrator (CHC) (Figure 3C), when coupled with a suitable focusing lens, offers equally efficient collection while maintaining practical physical dimensions and permitting integration with fiber probe-based portable systems (Figure 3D,E).15
Another challenge associated with Raman-based glucose sensing is the presence of highly idiosyncratic anatomical sites of measurement and the variability arising from motional artifacts that together necessitate a controlled mechanical interface. Chaiken and co-workers have elegantly addressed this by incorporating an active tissue modulation interface into the measurement device (Figure 3F,G).14 Tissue modulation involves spatiotemporally localized mechanical stimulus to manipulate the mobile components of tissue relative to the static components and use difference spectroscopy to isolate the spectra of the two. Blood (and its analytes) being the primary mobile component, this approach affords greater specificity in terms of selecting the signal of the blood constituent of interest while rejecting the extraneous features of the solid tissue matrix components.
4. QUANTITATIVE SPECTRAL ANALYSIS
The wealth of intrinsic molecular information in the Raman spectra allows the deduction of molecular structure and concentration of myriad blood-tissue matrix constituents. Yet, the presence of the spectral interferents, stemming from other endogenous Raman-active constituents and fluorophores, represents a significant challenge in quantifying the glucose content. Given the millimolar detection limit of spontaneous Raman scattering and the 4–10 mM physiological concentration of glucose, the need for a robust and accurate concentration prediction algorithm is paramount. To address this and related problems of biomedical interest, chemometric algorithms have been developed and implemented.37 A particularly important aspect is to overcome the influence of the tissue autofluorescence background. Additionally, we have shown that the presence of photobleaching induced variations in the spectra may lead to spurious correlations that need to be addressed via experimental or computational methods to eliminate the adverse impact.38
4.1. Multivariate Calibration (MVC)
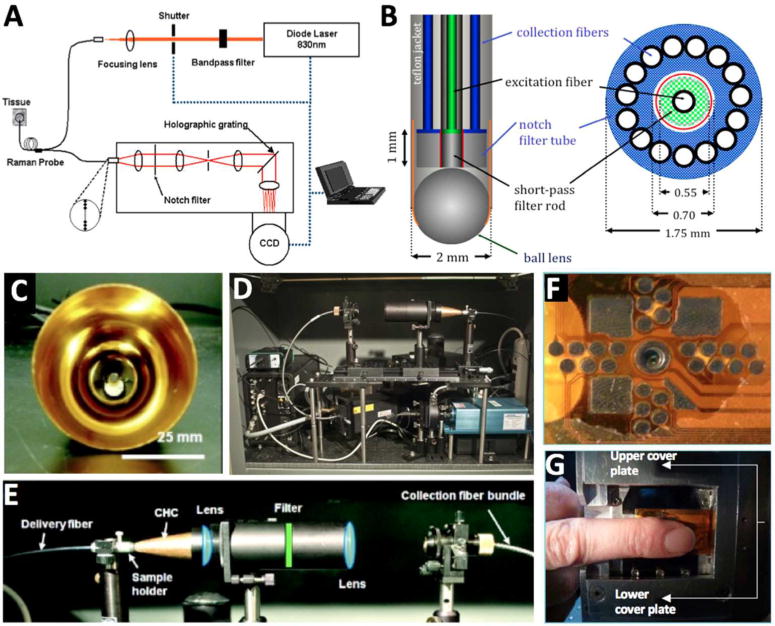
Given the small Raman scattering signal of glucose, the use of a single peak for concentration prediction is not feasible. One must resort to the application of MVC schemes that are able to exploit the multichannel nature of the spectroscopic data sets in order to determine concentration information. The two most commonly used methods to build a multivariate calibration model are principal component regression (PCR) and partial least-squares (PLS).37 The underlying assumption in these methods is that the measured Raman spectrum is a weighted linear combination of the constituent component spectra with the weights proportional to the corresponding concentrations. The overall goal of the developed calibration model is to predict the glucose concentration, c, of a prospective sample by taking the scalar product of the regression vector b with the spectrum recorded from the sample, s (Figure 4A,B).
Figure 4.
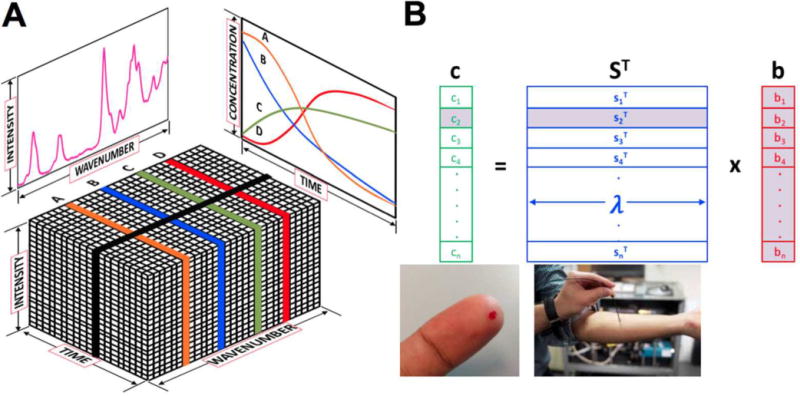
Multivariate data analysis. (A) Illustration of Raman spectral data set (intensity, wavelength) acquired as a function of time. The hyperspectral stack is analyzed to reveal the compositional contributors and their temporal changes. (B) The central idea of implicit calibration is to obtain the regression vector (b) from the recorded spectra (S) and glucose concentrations (c) in the calibration samples. The regression vector can then be used prospectively to predict glucose concentration using only the acquired spectrum from a test sample.
| (1) |
The aforementioned approaches differ in the specific mathematical transformations used to arrive at the regression vector, b (eq 1), from the spectra acquired from calibration samples and corresponding concentration measurements. PCR utilizes the principal components obtained by subjecting the spectral data set to principal component analysis where the data is transformed into a set of abstract orthogonal coordinate axes that best capture the variance in the spectral data set. On the other hand, in PLS application, both the spectral matrix S and reference concentration vector c of the calibration samples are transformed by projecting them into a new space such that the covariance between the two score matrices obtained is maximized. Here, the error terms in spectroscopic measurements are assumed to be independent and identically distributed random normal variables. The limit of glucose detection of the Raman system can be determined via the Cramér–Rao lower bound on estimator covariance and is based on the measurement noise, signal strength, and spectral overlap.39
4.2. Recent Advances in MVC Application
The assumption of linearity in PLS, PCR and related class of implicit calibration models may often fail owing to fluctuations in process and system variables, such as changes in temperature and sampling volume. It is worth noting that weak nonlinearities are modeled by the linear methods by retaining larger number of factors than is required by the chemical rank of the system. This, however, may incorporate irrelevant sources of variance and noise leading to apparently functional models that cannot be used for prospective prediction. In our human volunteer studies, while PLS-based subject-specific calibration provided reasonable results, the accuracy of global calibration models built across a cohort of subjects showed poor predictive power. To address this drawback, we proposed to model the curved effects by nonlinear calibration methods, prominently support vector machines (SVM).16 SVM is adept at handling ill-posed problems, such as those encountered in spectroscopy-based glucose sensing, and offers unique global models.40 The central idea in SVM is to minimize the cost function that regularizes the coefficients and penalizes the net regression error. While minimization of large coefficients reduces the potential for overfitting to irrelevant variables, penalization of the regression error directly impacts the accuracy of the model. In SVM, this constrained optimization problem is solved with the help of Lagrange multipliers, which results in the following function:
| (2.1) |
where xi, x, and b, respectively, represent the calibration data, prediction spectrum, and the bias; and αi, represent the Lagrange multipliers for the inequality constraints used in the formulation; and K(xi,x) is the kernel function utilized for nonlinear transformation.
Nonlinear regression is handled using nonlinear kernels such as the radial basis function (with width of σ) (eq 2.2) and polynomials of degree d (eq 2.3). However, adequate caution should be exercised while using nonlinear calibration methods, as they are more prone to overfitting and sensitive to the choice of parameters compared to their linear counterparts.
| (2.2) |
| (2.3) |
In human subject studies, accounting for nonlinearity via SVM enhanced the glucose prediction performance by ca. 30% when compared to PLS-derived results.16 The key question that arises is what is the basis for this improvement, i.e., what are the contributing factors to the nonlinearity in the spectra-concentration relationship? We reasoned that one particularly important source is the variations in tissue turbidity (further detailed in the ensuing section). Integration of feature selection in SVM regression models has also been shown to further boost the prediction performance,41 and remains an area of ongoing research.
Another critical, yet underexplored, question is whether spectroscopy-based concentration tracking can be performed without requiring substantive calibration concentration measurements. Ozaki and co-workers proposed an analytical framework that empowers spectroscopy-based longitudinal tracking of chemical concentration with minimal a priori concentration information.42 Leveraging these ideas, we have employed concentration space transformation from the spectral information and used these estimates in conjunction with the concentration profiles generated from a system kinetic model.17 Use of this method has recently exhibited considerable reduction in prediction error over standard PLS regression when applied to a glucose tolerance test data set acquired from healthy volunteers.10,17
5. EMERGING SOLUTIONS TO RECALCITRANT ISSUES IN BLOOD GLUCOSE MEASUREMENTS
5.1. Turbidity in Biological Raman Spectroscopy
Turbidity-induced variations in sampling volume (Figure 5A) introduce substantive nonglucose specific variance in the recorded spectra, making accurate calibration extremely challenging. In fact, turbidity-induced alterations in the spectral intensity and peak widths may add nonlinearity to the spectra-concentration relationship, particularly when the absorption in the media is non-negligible. Over the past decade, three approaches have surfaced as attractive candidates for turbidity compensation in Raman spectroscopy. Temporal approaches depend on the differential time spent in the turbid sample by photons from the deeper layers as opposed to those generated at or close to the surface. Spatial approaches, on the other hand, rely on the deeper layer Raman signal being spread over a wider area than those emanating from shallower layers and therefore use spatially offset excitation and collection probes. While promising, these methods have not been extensively used for blood glucose sensing. The third approach blends measurements from an additional broadband source with an analytical formulation based on photon migration theory. The underlying hypothesis here is that the effects of turbidity are similarly manifested in both the diffuse reflectance and Raman measurements and thus, the former can be used to correct for the absorption and multiple scattering based distortions in the Raman spectra. Using Monte Carlo simulations, the relationship between Raman and diffuse reflectance has been elucidated for semi-infinite samples and samples of finite dimension (Figure 5B).43 Application of turbidity-corrected Raman spectroscopy,44 has shown near-perfect coalescence of Raman spectra acquired from a broad range of turbid media and, importantly, resulted in marked improvement in glucose concentration prediction.
Figure 5.
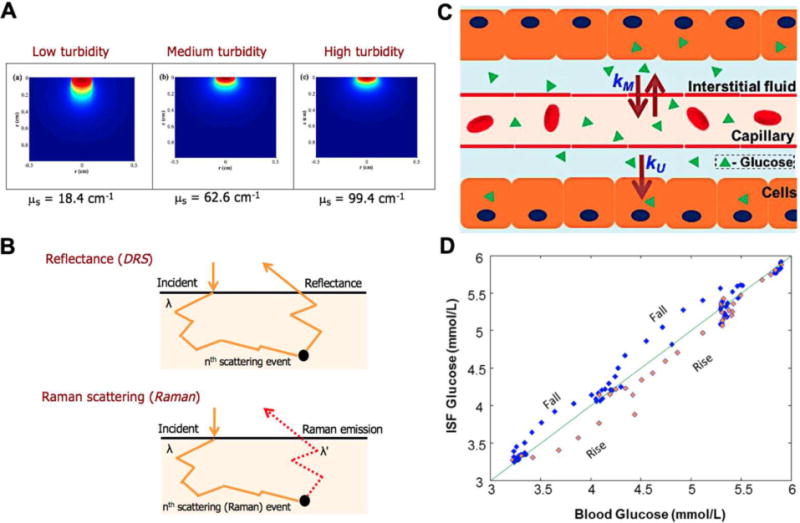
(A) Effects of turbidity on sampling volume as observed from simulations with tissue of different scattering coefficients. (B) Representation of the similar photon-tissue interactions for diffusely reflected and Raman scattered photons of the same wavelength. (C) Illustration of glucose diffusion between the blood and ISF compartments (mass transfer coefficient: kM) with a smaller amount of cellular uptake (kU). (D) Physiological lag between the glucose in the two compartments leads to a lack of one-to-one correspondence during rapid changes (rise/fall) in glucose concentrations.
5.2. Narrowing the Physiological Lag
Another major challenge is the time lag between the glucose levels in the blood and ISF compartments. NIR Raman measurements sample an effective depth of <1 mm (e.g., at λex = 830 μm) for biological tissue,45 which means the greater part of the sampling volume resides in the avascular epidermis and the dermis (Figure 5C). Since the ISF compartment has nearly 9 times the volume of the capillary blood vessels, the acquired Raman spectra are largely indicative of the ISF glucose levels. Moreover, calibration models are typically built from measurements performed during glucose tolerance tests or glucose clamping studies. Both of these generate rapid changes in glucose levels, which leads to the lack of a one-to-one correspondence between blood and ISF glucose concentrations (Figure 5D). This creates an inconsistency in the model that manifests itself as systematic calibration errors, which in turn adversely impact long-term performance of minimally invasive and noninvasive sensors. Such systematic errors remain a leading reason for inaccurate prospective predictions of glucose concentrations, as they could otherwise lead to undesirable consequences.
To address this, we have introduced a mass transfer formulation into the spectroscopic calibration framework that connects blood glucose concentration [cBG] and ISF glucose concentration [cISF] using a first order linear differential equation (eq 3), where the lumped mass transfer parameter (α) (akin to a lag time constant) quantifies the physiological lag due to diffusion.
| (3) |
This dynamic concentration correction (DCC) method first transforms [cBG] in the calibration data set to their corresponding ISF values, which are used as the new inputs for the calibration model development ensuring a consistent regression vector based on [cISF]. Following the standard prediction step, the predicted ISF glucose concentrations are inverse-transformed to the corresponding blood glucose values. Analysis of human subject data using DCC is of significant value in various contexts. First, predictions based on DCC model are much better matched to the reference blood glucose values than those without the model; in a specific instance, a 16% reduction in leave-one-out cross-validation error was observed. in a cohort of healthy human subjects measured over a 2 h period.27 Notably, while this initial study observed relatively modest variation in the lag time (9.5 ± 1.6 min) in healthy volunteers, further characterization in a larger population is warranted to understand potential lag time differences induced by diabetes. Second, this affords the ability to predict impending hypoglycemia, a much-needed feature for the next generation of glucose sensors, on the basis of the rate of change in ISF glucose concentration.
6. FINAL REMARKS
The combination of advances in experimental methods and chemometric analysis has allowed the demonstration of causality and adequate sensitivity in biological systems of increasing complexity for Raman-spectroscopy based glucose sensing. While promising, its translational potential as a truly noninvasive approach is yet to be realized. Specifically, validation in larger cohorts of PWD in single sitting as well as in follow up studies forms a critical milestone in demonstrating its diagnostic value. Furthermore, given the need for self-monitoring of blood glucose, we anticipate that development of a miniaturized, yet sensitive, Raman device from its current portable version to a (hopefully) hand-held format will constitute a parallel and equally important research thrust. This approach is generalizable to noninvasive monitoring of other clinically relevant blood analytes, including the detection of creatinine and urea as well as bilirubin tracking in neonates. While the challenge remains substantial in seeking the “Holy Grail” of biophotonics, recent findings provide important insights into resolving some of the most intractable challenges thereby paving the way forward for this ambitious goal.
Acknowledgments
This research was supported by the National Institute of Biomedical Imaging and Bioengineering (9P41EB015871-26A1), JHU Startup Funding, Connecticut Children’s Innovation Center seed funding, and Samsung.
Biographies
Rishikesh Pandey is an Assistant Professor at University of Connecticut Health. His work centers on development of novel biophotonic technologies that interface and bridge spectroscopy, clinical diagnostics, and label-free imaging.
Santosh Kumar Paidi is a Ph.D. student at Johns Hopkins University. His research centers on spectroscopic data analysis and integration into diagnostic models for unified biochemical and morphological insights.
Tulio A. Valdez is a pediatric otolaryngologist at Connecticut Children’s Medical Center. His research interests lie in the development of multimodal optical devices to interrogate ear pathologies.
Chi Zhang is a Ph.D. student at Johns Hopkins University. His research focuses on employing nanofabrication technologies to architect plasmonic structures for cell sensing.
Nicolas Spegazzini, currently at University of Illinois at Urbana–Champaign, focuses on designing analytics models that identify spectral markers in tissue and in disease.
Ramachandra Rao Dasari is the Associate Director of Laser Biomedical Research Center, MIT. His recent efforts have been devoted in using an array of optical modalities, notably Raman spectroscopy, for different biomedical applications.
Ishan Barman is an Assistant Professor in Mechanical Engineering and Oncology at Johns Hopkins University, and his interests reside at the interface of optical spectroscopy, contrast agent development, and clinical diagnostics.
Footnotes
ORCID
Ishan Barman: 0000-0003-0800-0825
Notes
The authors declare no competing financial interest.
References
- 1.Pandey R, Dingari NC, Spegazzini N, Dasari RR, Horowitz GL, Barman I. Emerging trends in optical sensing of glycemic markers for diabetes monitoring. TrAC, Trends Anal Chem. 2015;64:100–108. doi: 10.1016/j.trac.2014.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aggidis AGA, Newman JD, Aggidis GA. Investigating pipeline and state of the art blood glucose biosensors to formulate next steps. Biosens Bioelectron. 2015;74:243–262. doi: 10.1016/j.bios.2015.05.071. [DOI] [PubMed] [Google Scholar]
- 3.Heller A, Feldman B. Electrochemistry in Diabetes Management. Acc Chem Res. 2010;43:963–973. doi: 10.1021/ar9002015. [DOI] [PubMed] [Google Scholar]
- 4.Barone PW, Strano MS. Single Walled Carbon Nanotubes as Reporters for the Optical Detection of Glucose. J Diabetes Sci Technol. 2009;3:242–252. doi: 10.1177/193229680900300204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zimmermann S, Fienbork D, Stoeber B, Flounders AW, Liepmann D. A microneedle-based glucose monitor: fabricated on a wafer-level using in-device enzyme immobilization. TRANSDUCERS, Solid-State Sensors, Actuators and Microsystems, 12th International Conference on 2003. 1:99–102. [Google Scholar]
- 6.Khalil OS. Non-Invasive Glucose Measurement Technologies: An Update from 1999 to the Dawn of the New Millennium. Diabetes Technol Ther. 2004;6:660–697. doi: 10.1089/dia.2004.6.660. [DOI] [PubMed] [Google Scholar]
- 7.Olesberg JT, Liu L, Zee VV, Arnold MA. In Vivo Near-Infrared Spectroscopy of Rat Skin Tissue with Varying Blood Glucose Levels. Anal Chem. 2006;78:215–223. doi: 10.1021/ac051036i. [DOI] [PubMed] [Google Scholar]
- 8.Lambert JL, Pelletier CC, Borchert M. Glucose determination in human aqueous humor with Raman spectroscopy. J Biomed Opt. 2005;10:031110. doi: 10.1117/1.1914843. [DOI] [PubMed] [Google Scholar]
- 9.Rohleder D, Kiefer W, Petrich W. Quantitative analysis of serum and serum ultrafiltrate by means of Raman spectroscopy. Analyst. 2004;129:906–911. doi: 10.1039/b408927h. [DOI] [PubMed] [Google Scholar]
- 10.Enejder AMK, Scecina TG, Oh J, Hunter M, Shih W-C, Sasic S, Horowitz GL, Feld MS. Raman spectroscopy for noninvasive glucose measurements. J Biomed Opt. 2005;10:031114. doi: 10.1117/1.1920212. [DOI] [PubMed] [Google Scholar]
- 11.Aarnoutse PJ, Westerhuis JA. Quantitative Raman Reaction Monitoring Using the Solvent as Internal Standard. Anal Chem. 2005;77:1228–1236. doi: 10.1021/ac0401523. [DOI] [PubMed] [Google Scholar]
- 12.Zeng H, MacAulay C, McLean DI, Palcic B, Lui H. The Dynamics of Laser-Induced Changes in Human Skin Autofluorescence—Experimental Measurements and Theoretical Modeling. Photochem Photobiol. 1998;68:227–236. [PubMed] [Google Scholar]
- 13.Boyne MS, Silver DM, Kaplan J, Saudek CD. Timing of Changes in Interstitial and Venous Blood Glucose Measured With a Continuous Subcutaneous Glucose Sensor. Diabetes. 2003;52:2790–2794. doi: 10.2337/diabetes.52.11.2790. [DOI] [PubMed] [Google Scholar]
- 14.Chaiken J, Deng B, Bussjager RJ, Shaheen G, Rice D, Stehlik D, Fayos J. Instrument for near infrared emission spectroscopic probing of human fingertips in vivo. Rev Sci Instrum. 2010;81:034301. doi: 10.1063/1.3314290. [DOI] [PubMed] [Google Scholar]
- 15.Kong CR, Barman I, Dingari NC, Kang JW, Galindo L, Dasari RR, Feld MS. A novel non-imaging optics based Raman spectroscopy device for transdermal blood analyte measurement. AIP Adv. 2011;1:032175. doi: 10.1063/1.3646524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barman I, Kong C-R, Dingari NC, Dasari RR, Feld MS. Development of Robust Calibration Models Using Support Vector Machines for Spectroscopic Monitoring of Blood Glucose. Anal Chem. 2010;82:9719–9726. doi: 10.1021/ac101754n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spegazzini N, Barman I, Dingari NC, Pandey R, Soares JS, Ozaki Y, Dasari RR. Spectroscopic approach for dynamic bioanalyte tracking with minimal concentration information. Sci Rep. 2014;4:7013. doi: 10.1038/srep07013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vashist SK. Non-invasive glucose monitoring technology in diabetes management: A review. Anal Chim Acta. 2012;750:16–27. doi: 10.1016/j.aca.2012.03.043. [DOI] [PubMed] [Google Scholar]
- 19.Kost J, Mitragotri S, Gabbay RA, Pishko M, Langer R. Transdermal monitoring of glucose and other analytes using ultrasound. Nat Med. 2000;6:347–350. doi: 10.1038/73213. [DOI] [PubMed] [Google Scholar]
- 20.Shibata H, Heo YJ, Okitsu T, Matsunaga Y, Kawanishi T, Takeuchi S. Injectable hydrogel microbeads for fluorescence-based in vivo continuous glucose monitoring. Proc Natl Acad Sci U S A. 2010;107:17894–17898. doi: 10.1073/pnas.1006911107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barone PW, Baik S, Heller DA, Strano MS. Near-infrared optical sensors based on single-walled carbon nanotubes. Nat Mater. 2005;4:86–92. doi: 10.1038/nmat1276. [DOI] [PubMed] [Google Scholar]
- 22.Stuart DA, Yuen JM, Shah N, Lyandres O, Yonzon CR, Glucksberg MR, Walsh JT, Van Duyne RP. In Vivo Glucose Measurement by Surface-Enhanced Raman Spectroscopy. Anal Chem. 2006;78:7211–7215. doi: 10.1021/ac061238u. [DOI] [PubMed] [Google Scholar]
- 23.Sharma B, Bugga P, Madison LR, Henry A-I, Blaber MG, Greeneltch NG, Chiang N, Mrksich M, Schatz GC, Van Duyne RP. Bisboronic Acids for Selective, Physiologically Relevant Direct Glucose Sensing with Surface-Enhanced Raman Spectroscopy. J Am Chem Soc. 2016;138:13952–13959. doi: 10.1021/jacs.6b07331. [DOI] [PubMed] [Google Scholar]
- 24.Ma K, Yuen JM, Shah NC, Walsh JT, Glucksberg MR, Van Duyne RP. In Vivo, Transcutaneous Glucose Sensing Using Surface-Enhanced Spatially Offset Raman Spectroscopy: Multiple Rats, Improved Hypoglycemic Accuracy, Low Incident Power, and Continuous Monitoring for Greater than 17 Days. Anal Chem. 2011;83:9146–9152. doi: 10.1021/ac202343e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heise HM, Marbach R, Koschinsky T, Gries FA. Noninvasive Blood Glucose Sensors Based on Near-Infrared Spectroscopy. Artif Organs. 1994;18:439–447. doi: 10.1111/j.1525-1594.1994.tb02230.x. [DOI] [PubMed] [Google Scholar]
- 26.Arnold MA, Burmeister JJ, Small GW. Phantom Glucose Calibration Models from Simulated Noninvasive Human Near-Infrared Spectra. Anal Chem. 1998;70:1773–1781. doi: 10.1021/ac9710801. [DOI] [PubMed] [Google Scholar]
- 27.Barman I, Kong CR, Singh GP, Dasari RR, Feld MS. Accurate spectroscopic calibration for noninvasive glucose monitoring by modeling the physiological glucose dynamics. Anal Chem. 2010;82:6104–6114. doi: 10.1021/ac100810e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berger AJ, Koo T-W, Itzkan I, Horowitz G, Feld MS. Multicomponent blood analysis by near-infrared Raman spectroscopy. Appl Opt. 1999;38:2916–2926. doi: 10.1364/ao.38.002916. [DOI] [PubMed] [Google Scholar]
- 29.Dingari NC, Barman I, Singh GP, Kang JW, Dasari RR, Feld MS. Investigation of the specificity of Raman spectroscopy in non-invasive blood glucose measurements. Anal Bioanal Chem. 2011;400:2871–2880. doi: 10.1007/s00216-011-5004-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shao J, Lin M, Li Y, Li X, Liu J, Liang J, Yao H. In Vivo Blood Glucose Quantification Using Raman Spectroscopy. PLoS One. 2012;7:e48127. doi: 10.1371/journal.pone.0048127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Barman I, Dingari NC, Singh GP, Soares JS, Dasari RR, Smulko JM. Investigation of Noise-Induced Instabilities in Quantitative Biological Spectroscopy and Its Implications for Non-invasive Glucose Monitoring. Anal Chem. 2012;84:8149–8156. doi: 10.1021/ac301200n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Motz JT, Hunter M, Galindo LH, Gardecki JA, Kramer JR, Dasari RR, Feld MS. Optical Fiber Probe for Biomedical Raman Spectroscopy. Appl Opt. 2004;43:542–554. doi: 10.1364/ao.43.000542. [DOI] [PubMed] [Google Scholar]
- 33.Mahadevan-Jansen A, Mitchell MF, Ramanujam N, Utzinger U, Richards-Kortum R. Development of a Fiber Optic Probe to Measure NIR Raman Spectra of Cervical Tissue In Vivo. Photochem Photobiol. 1998;68:427–431. [PubMed] [Google Scholar]
- 34.Ghenuche P, Rammler S, Joly NY, Scharrer M, Frosz M, Wenger J, Russell PSJ, Rigneault H. Kagome hollow-core photonic crystal fiber probe for Raman spectroscopy. Opt Lett. 2012;37:4371–4373. doi: 10.1364/OL.37.004371. [DOI] [PubMed] [Google Scholar]
- 35.Enejder AMK, Koo T-W, Oh J, Hunter M, Sasic S, Feld MS, Horowitz GL. Blood analysis by Raman spectroscopy. Opt Lett. 2002;27:2004–2006. doi: 10.1364/ol.27.002004. [DOI] [PubMed] [Google Scholar]
- 36.Tanaka K, Pacheco MTT, Brennan JF, Itzkan I, Berger AJ, Dasari RR, Feld MS. Compound parabolic concentrator probe for efficient light collection in spectroscopy of biological tissue. Appl Opt. 1996;35:758–763. doi: 10.1364/AO.35.000758. [DOI] [PubMed] [Google Scholar]
- 37.Reddy RK, Bhargava R. Chemometric Methods for Biomedical Raman Spectroscopy and Imaging. In: Matousek P, Morris DM, editors. Emerging Raman Applications and Techniques in Biomedical and Pharmaceutical Fields. Springer; Berlin, Heidelberg: 2010. pp. 179–213. [Google Scholar]
- 38.Barman I, Kong C-R, Singh GP, Dasari RR. Effect of photobleaching on calibration model development in biological Raman spectroscopy. J Biomed Opt. 2011;16:011004. doi: 10.1117/1.3520131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Šćepanović OR, Bechtel KL, Haka AS, Shih W-C, Koo T-W, Berger AJ, Feld MS. Determination of uncertainty in parameters extracted from single spectroscopic measurements. J Biomed Opt. 2007;12:064012. doi: 10.1117/1.2815692. [DOI] [PubMed] [Google Scholar]
- 40.Cortes C, Vapnik V. Support-vector networks. Mach Learn. 1995;20:273–297. [Google Scholar]
- 41.Dingari NC, Barman I, Kang JW, Kong C-R, Dasari RR, Feld MS. Wavelength selection-based nonlinear calibration for transcutaneous blood glucose sensing using Raman spectroscopy. J Biomed Opt. 2011;16:087009. doi: 10.1117/1.3611006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Spegazzini N, Siesler HW, Ozaki Y. Sequential Identification of Model Parameters by Derivative Double Two-Dimensional Correlation Spectroscopy and Calibration-Free Approach for Chemical Reaction Systems. Anal Chem. 2012;84:8330–8339. doi: 10.1021/ac301867u. [DOI] [PubMed] [Google Scholar]
- 43.Shih W-C, Bechtel KL, Feld MS. Intrinsic Raman spectroscopy for quantitative biological spectroscopy Part I: Theory and simulations. Opt Express. 2008;16:12726–12736. doi: 10.1364/oe.16.012726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barman I, Singh GP, Dasari RR, Feld MS. Turbidity-Corrected Raman Spectroscopy for Blood Analyte Detection. Anal Chem. 2009;81:4233–4240. doi: 10.1021/ac8025509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Šćepanović OR, Fitzmaurice M, Gardecki JA, Angheloiu GO, Awasthi S, Motz JT, Kramer JR, Dasari RR, Feld MS. Detection of morphological markers of vulnerable atherosclerotic plaque using multimodal spectroscopy. J Biomed Opt. 2006;11:021007. doi: 10.1117/1.2187943. [DOI] [PubMed] [Google Scholar]


