Abstract
Despite long-standing public and scientific interest in the phenomenon of sleep, the current decade has shown tremendous growth in our understanding of the sleep of children who have medical or developmental conditions. To accommodate, promote, and guide that growth, Journal of Pediatric Psychology , Clinical Practice in Pediatric Psychology , and Journal of Developmental and Behavioral Pediatrics have published coordinated special issues, encompassing >30 relevant articles. This article introduces the special issue in Journal of Pediatric Psychology , highlighting papers that illustrate how sleep problems are not only commonly comorbid with childhood medical and developmental conditions; they are also likely caused by and contribute to these conditions. In doing so, these coordinated special issues guide clinical care and reveal opportunities for future research.
Keywords: developmental disabilities, health promotion and prevention, sleep
This special issue reflects the contribution of the Journal of Pediatric Psychology (JPP) to an unprecedented co-publication of related special issues on sleep at two other journals: Clinical Practice in Pediatric Psychology (CPPP) and Journal of Developmental and Behavioral Pediatrics (JDBP). The goal of coordinating these JPP/CPPP/JDBP special issues was to propel the field forward by highlighting new discoveries, inspiring investigators to consider sleep in their research programs, and providing guidance to clinicians who care for children with medical and developmental concerns. My counterparts at JDBP and CPPP, Drs Carolyn Ievers-Landis and Lisa Meltzer, share my appreciation for the tremendous work selected for publication, as well as my excitement for the future of the field.
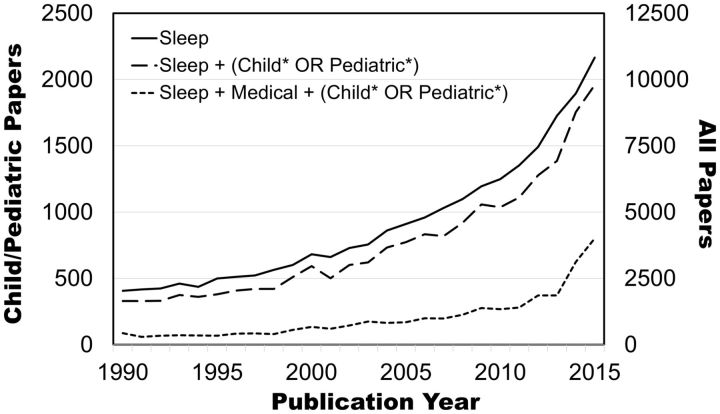
Given that sleep is a fundamental human process, it is not surprising that sleep advice and speculation date back thousands of years ( Thorpy, 1991 ). However, contemporary sleep science remains relatively new, coming into its own in the last half of the 20th century. Figure 1 illustrates the accelerating growth in Pubmed-indexed articles in the scientific literature over the past 25 years, showing parallel trajectories for the broader field of sleep and for sleep publications related to children. Publications on sleep in children with medical or developmental conditions have accelerated even more sharply and recently. While providing only a rough index of that phenomenon, Figure 1 shows the sudden spike in youth-related papers on sleep that integrate the term “medical” in their title, abstract, or keywords; more such papers were published in 2015 than during the entire decade of the 1990s ( Figure 1 ). Similarly, replacing the “medical” search term with autism or attention deficit/hyperactivity disorder (ADHD) shows that more relevant papers have been published since 2010 than were published in all of the indexed years before that date.
Figure 1.
Papers indexed in Pubmed over time that are broadly related to sleep (search term: “Sleep”), sleep in children (search term: “Sleep (child* OR pediatric*)” using * as a wildcard marker), and sleep in children with medical conditions (search terms: “Sleep Medical (child* OR pediatric*)”). The left vertical axis provides the count for child-oriented papers, while the right axis provides the count for all sleep papers.
Clearly, interest is mounting. The collection of papers in these JPP/CPPP/JDBP special issues show why. The field is rapidly learning about the degree to which sleep problems are comorbidities, contribute to, or are consequences of childhood medical or developmental issues. These “three C’s”—comorbidity, contribution, and consequence—are not mutually exclusive. Trying to settle on just one is like asking whether an apple is round versus red versus sweet. The “versus” is misplaced. Knowing one feature says little about the others, and even a comprehensive description of one variety of apple says little about another. This is why the papers in these special issues are so important; they highlight the breadth of comorbidity, illustrate the potential causal or contributing role of sleep issues in childhood medical and developmental disorders, and show that, even when sleep problems are a consequence of those disorders, they nevertheless are worth addressing.
Beginning with comorbidity, the >30 papers across the special issues show that sleep problems are common across a surprisingly wide range of conditions, including autism, ADHD, childhood cancers, type 1 diabetes (T1D), juvenile idiopathic arthritis, asthma, spina bifida, and obesity. As illustrated by Yuwen and colleagues ( 2016 , in this issue), these problems are generally more prevalent or severe than in healthy children, and can involve sleep duration, sleep quality, and sleep regularity. Further, these can persist well after a primary medical condition is cured or in long-term remission ( Crabtree et al., 2016 , in this issue; Zhou, Manley, Marcus, & Recklitis, 2016 , in this issue).
This comorbidity is concerning, even if one does not assume a causal relationship between a child’s sleep and other medical/developmental symptoms. Sleep problems have consequences—verified in experimental induction and clinical treatment trials—in healthy children, particularly affecting mood and attention regulation, learning, dietary behaviors, and overall quality of life ( Baum et al., 2014 ; Beebe, 2011 ; Beebe et al., 2013 ; Garetz et al., 2015 ; Marcus et al., 2013 ). Presumably these causal relationships also play out in the context of health and developmental conditions, in which sleep problems, daytime sleepiness, or fatigue are associated with poorer mood and diminished quality of life ( Crabtree et al., 2016 , in this issue; Quach, Mensah, & Hiscock, 2016 ). Broadening the scope even slightly shows the ripple effects on larger systems: parents of children with chronic health conditions are at high risk for poor sleep quality ( Meltzer & Booster, 2016 , in this issue), an effect even more prominent when those children have very poor quality sleep ( Yuwen et al., 2016 , in this issue).
Ethics considerations complicate studies of how child health might affect sleep. Even so, Daniel and colleagues ( Daniel, Schwartz, Mindell, Tucker, & Barakat, 2016 , in this issue) offer a conceptual model to understand the paths by which sleep problems might be caused by a child’s medical or developmental condition. These include biological processes (e.g., medication), environmental factors (e.g., hospitalizations), and psychosocial factors (e.g., coping). For example, craniopharyngiomas are brain tumors that tend to grow in or near the hypothalamus, which is heavily involved in sleep–wake regulation. Jacola and colleagues ( 2016 , in this issue) found that tumors with greater involvement of the hypothalamus were associated with notably greater daytime sleepiness in survivors. A similar effect was not evident at long-term follow-up with a different sample ( Zhou et al., 2016 , in this issue), but that paper focused on radiation to the hypothalamus, not direct tumor impingement.
The effects of a medical condition on a child’s sleep may differ over time and development. For example, Murray and colleagues ( 2016 , in this issue) found that, among children with spina bifida, having undergone more surgeries was associated with greater sleep problems in middle childhood, but not with subsequent trajectory of sleep problems through adolescence. In contrast, the trajectory of sleep problems across development was steeper among those who required shunting to prevent hydrocephalus. Others in this issue highlight the potential impact of treatment regimens on child or parent sleep ( Daniel et al., 2016 , in this issue; Meltzer & Booster, 2016 , in this issue). Even so, the effects of treatments for children’s medical or developmental conditions on their sleep has been surprisingly underresearched. One notable exception is the stimulant medication for ADHD, which has been shown to delay sleep onset in group studies, but which in some children seem to improve sleep ( Becker, Froehlich, & Epstein, 2016 ).
It is also ethically challenging to test the causal effects of sleep problems on a child’s medical or developmental condition. However, there is reason to suspect effects. Preliminary experimental trials suggest that modifying sleep may affect key health metrics in childhood asthma ( Meltzer et al., 2015 ) and T1D ( Perfect et al., 2016 ). Further, sleep restriction worsens attention in ADHD ( Gruber et al., 2011 ), and treatments for insomnia may ease daytime behavioral symptoms among children with autism ( Papadopoulos et al., 2015 ; Wright et al., 2011 ) or ADHD ( Corkum et al., 2016 , in this issue; Hiscock et al., 2015 ; Papadopoulos et al., 2015 ). The contribution of sleep is likely to be complex; there may be different effects for sleep duration and sleep quality, both overall and with respect to nightly variability, on T1D self-management and glucose levels ( Turner, Queen, Butner, Wiebe, & Berg, 2016 , in this issue) as well as waking activity levels and dietary behaviors among youth with obesity ( Ievers-Landis et al., 2016 , in this issue; Krietsch, Armstrong, McCrae, & Janicke, 2016 , in this issue).
Taken together, papers in these special issues highlight several important insights for clinical care. First, sleep should be routinely screened, given the high rates of sleep problems in children with medical and developmental concerns and the potential impact of those sleep problems on morbidity. Screening is important in both acutely ill children and long-term follow-up ( Crabtree et al., 2016 , in this issue; Zhou et al., 2016 , in this issue). Sleep screening can take several forms, but questionnaires and semi-structured interviews lend themselves well to general clinical settings ( Beebe, 2012 ).
Second, when screening suggests a sleep problem, it is important to identify potential causes, so that interventions can be put into place. The primary interventions for most pediatric sleep problems are behavioral, not medical. Behavioral sleep interventions are effective ( Byars & Simon, 2014 ; Corkum et al., 2016 , in this issue; Loring, Johnston, Gray, Goldman, & Malow, 2016 ; Malow, MacDonald, Fawkes, Alder, & Katz, 2016 ; Meltzer & Mindell, 2014 ; Nelson, Van Dyk, McGinnis, Nguyen, & Long, 2016 ), lack the side-effects of medications (none of which is Food and Drug administration-approved for use in pediatric sleep), and are often preferred over medication by parents and health caregivers alike ( Daniel et al., 2016 , in this issue). Even when dealing with medical factors intrinsic to the child’s condition, Meltzer and Booster ( 2016 , in this issue) remind us that behavioral and environmental interventions can be put into place to mitigate their impact. However, the clinician must take care to balance the overall situation facing a family; there is no one-size-fits-all approach, especially in the face of a fluctuating medical condition ( Daniel et al., 2016 , in this issue).
Finally, even when sleep is not yet a problem, it is important to take sleep into consideration prophylactically. Certain groups are known to be at particularly high risk for sleep dysregulation (e.g., those with hypothalamic tumor involvement [ Jacola et al., 2016 , in this issue] or for developing unhealthy sleep patterns [ Bates et al., 2016 , in this issue]). Identifying high-risk youth offers the opportunity to prevent sleep problems or to minimize their impact quickly.
While the JPP/CPPP/JDBP special issues represent a leap forward, much work remains to be done. For some conditions, the field has done little more than show comorbidity; for others, it has not gotten even that far. Sleep should be considered from different angles, including duration, circadian timing, continuity, and perceived sleep quality. This necessitates multimodal assessments, as different sleep measures lend themselves best to different purposes. The field has much to learn about the shared and unique mechanisms for, and consequences of, poor sleep across childhood conditions. While being mindful of ethics concerns, creative research designs can answer important questions about cause and effect, including sleep manipulation trials ( Meltzer et al., 2015 ; Perfect et al., 2016 ), clinical sleep treatment trials ( Corkum et al., 2016 , in this issue; Loring et al., 2016 ; Malow et al., 2016 ; Nelson et al., 2016 ), and longitudinal studies with frequent measurement of outcomes, putative mechanisms, and potential confounding variables ( Murray et al., 2016 , in this issue; Schwichtenberg, Christ, Abel, & Poehlmann-Tynan, 2016 ; Williams & Sciberras, 2016 ). There is no shortage of research opportunities for both new and established investigators, and findings will have practical implications for the clinical management of children with medical and developmental conditions.
Funding
This work was funded by National Institutes of Health grant number R01 HL120879.
Conflicts of interest : None declared.
References
- Bates C., Bohnert A., Ward A., Burdette K., Kliethermes S., Welch S., Silton R. L., Dugas L. ( 2016. ). Sleep is in for summer: Patterns of sleep and physical activity in urban minority girls . Journal of Pediatric Psychology , 41 . doi: 10.1093/jpepsy/jsw009 [DOI] [PubMed] [Google Scholar]
- Baum K. T., Desai A., Field J., Miller L. E., Rausch J., Beebe D. W. ( 2014. ). Sleep restriction worsens mood and emotion regulation in adolescents . Journal of Child Psychology and Psychiatry , 55 , 180 – 190 . doi:10.1111/jcpp.12125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker S. P., Froehlich T. E., Epstein J. N. ( 2016. ). Effects of methylphenidate on sleep functioning in children with attention- deficit/hyperactivity disorder . Journal of Developmental and Behavioral Pediatrics , 37 . PMID: 27011002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beebe D. W. ( 2011. ). Cognitive, behavioral, and functional consequences of inadequate sleep in children and adolescents . Pediatric Clinics of North America , 58 , 649 – 665 . doi:10.1016/j.pcl.2011.03.002 S0031-3955(11)00018-6 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beebe D. W. ( 2012. ). A brief primer on sleep for pediatric and child clinical neuropsychologists . Child Neuropsychology , 18 , 313 – 338 . doi:10.1080/09297049.2011.602014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beebe D. W., Simon S., Summer S., Hemmer S., Strotman D., Dolan L. M. ( 2013. ). Dietary intake following experimentally restricted sleep in adolescents . Sleep , 36 , 827 – 834 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byars K., Simon S. ( 2014. ). Practice patterns and insomnia treatment outcomes from an evidence-based pediatric behavioral sleep medicine clinic . Clinical Practice in Pediatric Psychology , 2 , 337 – 349 . doi:10.1037/cpp0000068 [Google Scholar]
- Corkum P., Lingley-Pottie P., Davidson F., McGrath P. J., Chambers C., Mullane J., Laredo S., Woodford K., Weiss S. ( 2016. , in this issue ). Better nights/better days - distance intervention for insomnia in school-aged children with/without ADHD: A Randomized Controlled Trial . Journal of Pediatric Psychology , 41 . [DOI] [PubMed] [Google Scholar]
- Crabtree V., Graef D., Phipps S., Parris K., Martin-Elbahesh K., Huang L., Zhang H. ( 2016. , in this issue ). Sleepiness, fatigue, behavioral functioning, and quality of life in survivors of childhood hematopoietic stem cell transplant . Journal of Pediatric Psychology , 41 . doi: 10.1093/jpepsy/jsw011 [DOI] [PubMed] [Google Scholar]
- Daniel L., Schwartz L., Mindell J., Tucker C., Barakat L. ( 2016. , in this issue ). Initial validation of the sleep disturbances in pediatric cancer model . Journal of Pediatric Psychology , 41 . doi: 10.1093/jpepsy/jsw008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garetz S. L., Mitchell R. B., Parker P. D., Moore R. H., Rosen C. L., Giordani B., Muzumdar H., Paruthi S., Elden L., Willging P., Beebe D. W., Marcus C. L., Chervin R. D., Redline S. ( 2015. ). Quality of life and obstructive sleep apnea symptoms after pediatric adenotonsillectomy . Pediatrics , 135 , e477 – e486 . doi:10.1542/peds.2014-0620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber R., Wiebe S., Montecalvo L., Brunetti B., Amsel R., Carrier J. ( 2011. ). Impact of sleep restriction on neurobehavioral functioning of children with attention deficit hyperactivity disorder . Sleep , 34 , 315 – 323 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiscock H., Sciberras E., Mensah F., Gerner B., Efron D., Khano S., Oberklaid F. ( 2015. ). Impact of a behavioural sleep intervention on symptoms and sleep in children with attention deficit hyperactivity disorder, and parental mental health: Randomised Controlled Trial . BMJ , 350 , h68 . doi:10.1136/bmj.h68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ievers-Landis C., Kneifel A., Giesel J., Rahman F., Narasimhan S., Uli N., O'Riordan M. ( 2016. , in this issue ). Dietary intake and eating-related cognitions related to sleep among adolescents who are overweight or obes . Journal of Pediatric Psychology , 41 . [DOI] [PubMed] [Google Scholar]
- Jacola L. M., Conklin H., Scoggins M. A., Ashford J., Merchant T. E., Mandrell B. N., …, Crabtree V. ( 2016. , in this issue ). Investigating the role of hypothalamic tumor involvement in sleep and cognitive outcomes among children treated for craniopharyngioma . Journal of Pediatric Psychology , 41 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krietsch K., Armstrong B., McCrae C., Janicke D. ( 2016. , in this issue ). Temporal associations between sleep and physical activity among overweight/obese youth . Journal of Pediatric Psychology , 41 . doi:10.1093/jpepsy/jsv167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loring W. A., Johnston R., Gray L., Goldman S., Malow B. ( 2016. ). A brief behavioral intervention for insomnia in adolescents with autism spectrum disorders . Clinical Practice in Pediatric Psychology , 4 . [Google Scholar]
- Malow B. A., MacDonald L., Fawkes D. B., Alder M. L., Katz T. ( 2016. ). Teaching children with autism spectrum disorder how to sleep better: A pilot educational program for parents . Clinical Practice in Pediatric Psychology , 4 . [Google Scholar]
- Marcus C. L., Moore R. H., Rosen C. L., Giordani B., Garetz S. L., Taylor H. G., Mitchell R. B., Amin R., Katz E. S., Arens R., Paruthi S., Muzumdar H., Gozal D., Thomas N. H., Ware J., Beebe D., Snyder K., Elden L., Sprecher R. C., Willging P., Jones D., Bent J. P., Hoban T., Chervin R. D., Ellenberg S. S., Redline S. for the Childhood Adenotonsillectomy, T. ( 2013. ). A randomized trial of adenotonsillectomy for childhood sleep apnea . New England Journal of Medicine , 368 , 2366 – 2376 . doi:10.1056/NEJMoa1215881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer L. J., Booster G. ( 2016. , in this issue ). Sleep disturbance in caregivers of children with chronic illness . Journal of Pediatric Psychology , 41 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer L. J., Faino A., Szefler S. J., Strand M., Gelfand E. W., Beebe D. W. ( 2015. ). Experimentally manipulated sleep duration in adolescents with asthma: Feasibility and preliminary findings . Pediatric Pulmonology , 50 , 1360 – 1367 . doi:10.1002/ppul.23179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer L. J., Mindell J. A. ( 2014. ). Systematic review and meta-analysis of behavioral interventions for pediatric insomnia . Journal of Pediatric Psychology , 39 , 932 – 948 . doi:10.1093/jpepsy/jsu041 [DOI] [PubMed] [Google Scholar]
- Murray C., Kirsch A., Palermo T., Holmbeck G., Kolbuck V., Psihogios A., Pigott T. ( 2016. , in this issue ). Developmental course and determinants of sleep disturbances in adolescents with Spina Bifida . Journal of Pediatric Psychology , 41 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson T. D., Van Dyk T. R., McGinnis J. C., Nguyen A. V., Long S. K. ( 2016. ). Brief sleep intervention to enhance behavioral parent training for noncompliance: Preliminary findings from a practice-based study . Clinical Practice in Pediatric Psychology , 4 . [Google Scholar]
- Papadopoulos N., Sciberras E., Hiscock H., Mulraney M., McGillivray J., Rinehart N. ( 2015. ). The efficacy of a brief behavioral sleep intervention in school-aged children with ADHD and comorbid autism spectrum disorder . Journal of Attention Disorders . doi:10.1177/1087054714568565 [DOI] [PubMed] [Google Scholar]
- Perfect M. M., Beebe D. W., Levine-Donnerstein D., Frye S. S., Bluez G. P., Quan S. F. ( 2016. ). Feasibility of a clinically-relevant sleep modification protocol for youth with type 1 diabetes . Clinical Practice in Pediatric Psychology , 4 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quach J., Mensah F., Hiscock H. ( 2016. ). Differential outcomes of sleep problems in children with and without special health care needs: Australian population study . Journal of Developmental and Behavioral Pediatrics , 37 . PMID: 26982245 [DOI] [PubMed] [Google Scholar]
- Schwichtenberg A. J., Christ S., Abel E., Poehlmann-Tynan J. A. ( 2016. ). Circadian sleep patterns in toddlers born preterm: Longitudinal associations with developmental and health concerns . Journal of Developmental and Behavioral Pediatrics , 37 . PMID: 27011003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpy M. J. ( 1991. ). History of sleep and man . In Thorpy M. J., Yager J. (Eds.), The encylopedia of sleep and sleep disorders (pp. xvii – xxxviii ). New York, NY: : Facts on File, Inc; . [Google Scholar]
- Turner S., Queen T., Butner J., Wiebe D., Berg C. ( 2016. , in this issue ). Variations in daily sleep quality and type 1 diabetes management in late adolescents . Journal of Pediatric Psychology , 41 . doi: 10.1093/jpepsy/jsw010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams K. E., Sciberras E. ( 2016. ). Sleep and self-regulation from birth to 7 years: A retrospective study of children with and without ADHD at 8-9 years . Journal of Developmental and Behavioral Pediatrics , 37 . PMID: 26982247 [DOI] [PubMed] [Google Scholar]
- Wright B., Sims D., Smart S., Alwazeer A., Alderson-Day B., Allgar V., Whitton C., Tomlinson H., Bennett S., Jardine J., McCaffrey N., Leyland C., Jakeman C., Miles J. ( 2011. ). Melatonin versus placebo in children with autism spectrum conditions and severe sleep problems not amenable to behaviour management strategies: A randomised controlled crossover trial . Journal of Autism and Developmental Disorders , 41 , 175 – 184 . doi:10.1007/s10803-010-1036-5 [DOI] [PubMed] [Google Scholar]
- Yuwen W., Chen M. L., Cain K., Ringold S., Wallace C., Ward T. ( 2016. , in this issue ). Daily sleep patterns, sleep quality and sleep hygiene among parent-child dyads of young children newly diagnosed with juvenile idiopathic arthritis and typically developing children . Journal of Pediatric Psychology , 41 . doi: 10.1093/jpepsy/jsw007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou E., Manley P., Marcus K., Recklitis C. ( 2016. , in this issue ). Medical and psychosocial correlates of insomnia symptoms in adult survivors of pediatric brain tumors . Journal of Pediatric Psychology , 41 . doi: 10.1093/jpepsy/jsv071 [DOI] [PubMed] [Google Scholar]