Abstract
Introduction:
Electronic cigarette (ECIG) use has grown rapidly in popularity within a short period of time. As ECIG products continue to evolve and more individuals begin using ECIGs, it is important to understand the potential adverse effects that are associated with ECIG use. The purpose of this study was to examine and describe the acute adverse effects associated with ECIG use.
Methods:
This study used an integrated, mixed-method participatory approach called concept mapping (CM). Experienced ECIG users ( n = 85) provided statements that answered the focus prompt “A specific negative or unpleasant effect (ie, physical or psychological) that I have experienced either during or immediately after using an electronic cigarette device is…” in an online program. Participants sorted these statements into piles of common themes and rated each statement. Using multidimensional scaling and hierarchical cluster analysis, a concept map of the adverse effects statements was created.
Results:
Participants generated 79 statements that completed the focus prompt and were retained by researchers. Analysis generated a map containing five clusters that characterized perceived adverse effects of ECIG use: Stigma, Worry/Guilt, Addiction Signs, Physical Effects, and Device/Vapor Problems.
Conclusions:
ECIG use is associated with adverse effects that should be monitored as ECIGs continue to grow in popularity. If ECIGs are to be regulated, policies should be created that minimize the likelihood of user identified adverse effects.
Implications:
This article provides a list of adverse effects reported by experienced ECIG users. This article organizes these effects into a conceptual model that may be useful for better understanding the adverse outcomes associated with ECIG use. These identified adverse effects may be useful for health professionals and policy makers. Health professionals should be aware of potential negative health effects that may be associated with ECIG use and policy makers could design ECIG regulations that minimize the risk of the adverse effects reported by ECIG users in this study.
Introduction
During a time when cigarette smoking in the United States is at an all-time low, 1 the use of electronic cigarettes (ECIGs) has begun to rise rapidly. ECIGs are a class of products/devices that use an electrically-powered heating element to heat a liquid solution so that an aerosol is produced for the user to inhale. The popularity of these products has increased dramatically since approximately 2009. 2 This increasing trend has occurred in all age groups including the general adult population, 3–6 young adults, 7–10 and adolescents. 11–15 Obtaining accurate and up-to-date ECIG use prevalence estimates presents many challenges given the increasing rate of adoption of ECIGs and the wide variety of ECIG products that are available. These difficulties aside, recent studies examining ECIG prevalence have reported 8.5% ever use and 6.8% current use (use within the past 30 days) among the general adult population, 5 29.9% ever use and 14.9% current use among the young adult population, 9 and 13.4% current use among high school students. 15 While those who use other tobacco products are significantly more likely to report ECIG use, 4 , 6 , 7 , 13 , 14 , 16 there are a substantial number of ECIG users who have never used any other tobacco product. 6 , 7 , 11 , 17 , 18 Though there is still much debate on what type of impact ECIG use may have on public health, it is clear that the increasing rates of ECIG use will broaden this impact, whatever it may be.
Though research detailing the long term effects of ECIG use does not currently exist, many ECIG users report perceptions of reduced harm associated with ECIG use compared to other forms of tobacco use. Many use this belief as a reason for initiating ECIG use. 8 , 19–21 Because ECIG use involves inhalation of chemicals such as flavorants, propylene glycol, vegetable glycerine, and the addictive chemical nicotine, there are likely adverse effects associated with ECIG use. However, partly due to the recent growth in popularity of ECIGs and constantly changing ECIG market, little is known about the adverse effects associated with ECIG use. Studies that identify these adverse effects could inform regulatory policies, such as requiring manufacturers to report known adverse effects experienced by ECIG users or setting product standards that minimize or eliminate the risk of commonly reported adverse outcomes. Understanding the long term adverse effects associated with ECIG use will require more time. However, well designed studies can empirically identify and examine the acute adverse effects of ECIG use now including psychological and physiological adverse effects.
Public health experts should develop and employ evaluation approaches that allow for the systematic reporting and surveillance of negative and positive events associated with novel tobacco product use. There are many methods that can be used to evaluate the harm potential and adverse effects of novel tobacco products. For instance, researchers have used laboratory methods to examine mainstream waterpipe tobacco smoke 22–27 and subjective effects of waterpipe tobacco smoking. 28–31 These laboratory methods are useful in that they can provide data on potential adverse effects of novel tobacco product use in a controlled setting and can also be extended to evaluate ECIGs, however, they almost certainly fail to capture the full breadth of outcomes associated with real-world use. In many cases, capturing all of the adverse outcomes associated with novel tobacco product use requires an approach that uses multiple methods that allows novel tobacco product users to provide their own “expert” accounts of their experiences. One such approach is concept mapping (CM), a participatory innovative and integrated method that combines the strengths of qualitative and quantitative research that has been applied previously to other health issues. 32–34 The purpose of this study was to use CM to identify and describe the adverse effects associated with ECIG use.
Methods
Overview
We used CM, an integrative mixed method participatory approach that incorporates group-level processes and multivariate analyses to identify latent constructs, to examine adverse effects associated ECIG use. This approach involved multiple steps to generate individual statements related to the adverse effects associated with ECIG use. These statements were then sorted, rated, and empirically analyzed to create an interpretable “map” representation of concepts in a broad conceptual framework. These steps included preparation, idea generation, sorting, rating, representation, and interpretation/utilization.
Participants and Procedures
For the CM preparation phase, we developed a focus prompt that would elicit responses from participants relevant to adverse effects associated with ECIG use. During this phase we pretested the initial prompt with the input of experienced ECIG users in a focus group session resulting in the finalized focus prompt of “A specific negative or unpleasant effect (ie, physical or psychological) that I have experienced either during or immediately after using an electronic cigarette device is….” This prompt was entered into The Concept System Global MAX, an internet-based CM program. Following the refinement of the focus prompt, we invited experienced adult ECIG users (≥18 years of age, past 30-day ECIG use) to participant in a CM study on adverse effects of ECIG use. ECIG users ( n = 85) were recruited through Craigslist, ECIG internet forums, “vape” conferences or conventions, and social media websites. These participants were instructed to complete a brainstorming task. For the brainstorming task, participants were instructed to provide five to eight brief statements that completed or answered the focus prompt and related to one thought (eg, no statements that described more than one negative or unpleasant effect). Participants received a $10 gift card for participation in the idea generation task.
In the generation phase of the study, participants answered demographic and tobacco use questions and then responded to the finalized focus prompt in an online brainstorming session. The majority of participants ( n = 85) in the generation phase heard about the study through social media (47.1%) followed by vape conventions or conferences (41.2%) and had an average age of 34.9 ( SD = 10.8). The majority were male (56.8%), non-Hispanic (87.6%) and White (91.4%). Most participants had been using ECIGs for 6 months or more (91.6%) and used ECIG all of the past 30 days (86.9%). Most participants reported using either tank systems (50.6%) or dripping systems (44.7%). Other demographic, ECIG use, and other tobacco use sample characteristics are displayed in Table 1 . Researchers reviewed continuously the participant-generated statements and closed the idea generation task module when content saturation had been reached. Of the 476 initial statements generated during the idea generation phase, 79 statements were retained after removing duplicate statements and inappropriate statements (eg, statements that did not relate to negative effects of ECIG use or statements that contained more than one thought). These statements were uploaded to The Concept System Global MAX for the sorting and rating phase.
Table 1.
Demographics
| Characteristic | N | % |
|---|---|---|
| Age ( M , SD ) | 34.9, 10.8 | |
| Sex | ||
| Female | 32 | 39.5 |
| Male | 46 | 56.8 |
| Ethnicity | ||
| Hispanic/Latino | 2 | 2.5 |
| Not Hispanic/Latino | 71 | 87.7 |
| Race | ||
| Asian | 1 | 1.2 |
| Native Hawaiian / Pacific Islander | 0 | 0 |
| Black / African American | 2 | 2.5 |
| White / European American | 74 | 91.4 |
| More than one race | 1 | 1.2 |
| Regular ECIG use duration | ||
| Less than a month | 0 | 0.0 |
| 1–5 months | 8 | 9.4 |
| 6–12 months | 30 | 35.3 |
| Between 1 and 2 years | 21 | 24.7 |
| More than 2 years | 26 | 30.6 |
| ECIG use in past 30 days | ||
| 1–5 days | 0 | 0 |
| 6–10 days | 2 | 2.4 |
| 11–20 days | 6 | 7.1 |
| 21–29 days | 3 | 3.6 |
| All 30 days | 73 | 86.9 |
| ECIG use times per day | ||
| Less than five times a day | 5 | 5.9 |
| Between 6 and 15 times a day | 30 | 35.3 |
| Between 16 and 25 times a day | 28 | 32.9 |
| More than 25 times a day | 22 | 25.9 |
| Nicotine concentration | ||
| Zero (0mg /0mL) | 5 | 5.9 |
| Low (less than 8mg/ 0.08mL) | 49 | 57.7 |
| Medium (between 8mg/ 0.08mL and 16mg / 1.6mL) | 17 | 20.0 |
| High (more than 16mg / 1.6mL) | 6 | 7.1 |
| Not sure | 8 | 9.4 |
| ECIG type | ||
| Prefilled | 3 | 3.5 |
| Drip feed from bottle | 38 | 44.7 |
| Tank feed | 43 | 50.6 |
| Lifetime cigarette use | ||
| No | 4 | 4.8 |
| Yes | 80 | 95.2 |
| Cigarette use past 30 days | ||
| None | 72 | 84.7 |
| 1–5 days | 9 | 10.6 |
| 6–10 days | 1 | 1.2 |
| 11–20 days | 1 | 1.2 |
| 21–29 days | 1 | 1.2 |
| All 30 days | 1 | 1.2 |
| Other tobacco use past 30 days | ||
| No | 78 | 91.8 |
| Yes | 7 | 8.2 |
ECIG = electronic cigarette. Regular use was left to the interpretation of participants given there is currently no standardized measure of ECIG use.
Participants who completed the brainstorming task were invited to sort and rate the final 79 statements. For sorting, participants accessed the list of statements in an online program and organized all of the statements into piles of statements, similar to the card game Solitaire. Using established methods, 35 , 36 participants were instructed to categorize the statements into piles according to their views of meaning or theme. Each pile was required to be made up of statements related to a single meaning or theme and could not be organized according to priority or value such as “Important,” “Hard to do,” “Random,” or “Other.” Within this rule, participants could sort the statements any way they deemed appropriate with the exception of putting all the statements into one category or having a miscellaneous pile. Participants created and assigned labels/names to each of the piles they created which completed the sorting task. Following completing the sorting activity, participants rated each statement in response to the question “I have experienced this negative or unpleasant effect either during or immediately after using my electronic cigarette device” with response options ranging from 1 (Definitely No) to 7 (Definitely Yes). The rating data allowed the research team to examine variations between participants for individual statements and clusters. A total of 50 participants completed the sorting task and 57 participants completed the rating task.
Analyses
A 79×79 matrix of similarities based on aggregated sort information from participants was generated with each cell representing the number of times statements were sorted together by participants. Multidimensional scaling was used to assign each statement a two-dimensional coordinate (x, y) that accounted for values from the similarity matrix. Using these coordinates, each statement was plotted to generate a point map that provided a visual representation of the similarity matrix. Points located nearer to one another represented statements that were more frequently grouped into the same categories in the sorting activity, while points that were further away from one another represented statements that were less frequently grouped together in the sorting activity. Using hierarchical clustering, statements were empirically grouped into clusters based on their two-dimensional space coordinates and participants’ average rating. Models with a range of clusters were examined until a final, best fitting model was achieved. The number of clusters in the final model was determined using interpretability and parsimony as indicators of best model fit.
Average ratings of statements within each cluster were compared using t tests to determine which clusters were most frequently reported by participants. Additional subgroup analyses were conducted to determine if participants’ ratings of statements within clusters differed based on ECIG user characteristics. Clusters were compared based on type of ECIG device used, ECIG use experience (ie, how long participants had used ECIGs), and liquid nicotine concentration used in ECIG.
Results
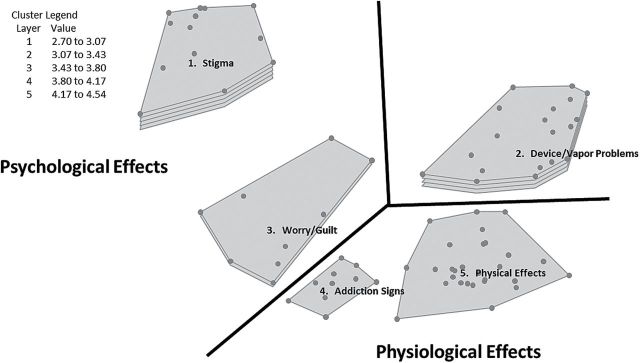
The final map generated from the sorting and rating tasks included five clusters of statements related to adverse effects associated with ECIG use as identified by experienced ECIG users ( Figure 1 ). These clusters fell under three broad constructs: psychological effects, physiological effects, and problems with ECIG devices. A summary of the clusters is provided below and a complete list of statements within each cluster is displayed in Table 2 .
Figure 1.
Combined cluster map and cluster rating map separated by adverse effects domains. Points within each cluster represent individual statements sorted by participants. Clusters with greater number of layers represent clusters with greater mean statement ratings regarding frequency of experiencing adverse effects within the cluster.
Table 2.
List of Clusters and Statements With Mean Ratings
| Cluster | Statement | Average rating |
|---|---|---|
| Psychological effects | ||
| 1. Stigma | 4.54 | |
| Others telling me it’s worse than cigarettes. | 5.47 | |
| Being still considered a “smoker” by certain people. | 5.40 | |
| Still being considered a smoker. | 5.30 | |
| People kicking me back outside with the smokers. | 5.19 | |
| Having to explain to people that I am not smoking anything. | 5.09 | |
| When people think my vaping will hurt them like cigarette smoke. | 4.98 | |
| Fear government regulations will push me back to smoking. | 4.39 | |
| Having to walk off property at work due to it being equated with smoking. | 4.35 | |
| Societal stigma of ECIG users being unintelligent, or otherwise unpleasant | 4.28 | |
| The lack of ability to vape in bars or restaurants even after owner’s permission. | 3.98 | |
| Friends or family asking when I am going to quit that nasty habit (vaping). | 3.70 | |
| Authorities profiling. | 3.58 | |
| Negative views from the vaping community in regards to purchasing cloned devices. | 3.25 | |
| 2. Worry/Guilt | 3.11 | |
| Smelling cigarettes after starting was unpleasant. | 4.68 | |
| Expensive trying flavors to keep you motivated. | 3.75 | |
| Guilt over spending money on vapor devices. | 3.72 | |
| I feel like I’m trading one addiction for another. | 3.70 | |
| I feel bad that I can’t completely shake the social aspect of smoking. | 3.19 | |
| Feel guilty for still giving into my cravings. | 2.79 | |
| I’m afraid it’ll make my kids think it’s ok to do this instead of smoking. | 2.67 | |
| It will stain my fingers, clothes, etc. | 2.02 | |
| I’m worried that my girlfriend might continue with ECIGs if/when she becomes pregnant. | 1.44 | |
| Physiological effects | ||
| 3. Physical Effects | 2.70 | |
| “Vaper’s tongue” meaning if you stay on one flavor too long, you can’t taste it anymore. | 4.35 | |
| Dry mouth from vaping too much. | 4.23 | |
| Feeling slightly dehydrated. | 3.74 | |
| Constantly have to drink water. | 3.60 | |
| Chapped lips from not properly hydrating while vaping. | 3.32 | |
| Sharp cough from a scratchy throat. | 3.00 | |
| Itchy, dry throat. | 2.89 | |
| Nausea and headache from too much nicotine. | 2.88 | |
| I’ve felt dizzy after vaping too much. | 2.81 | |
| Post-nasal drip when vaping e-liquids with a high VG [vegetable glycerin] content. | 2.68 | |
| I’ve gained a bit of weight because I can actually taste food now. | 2.68 | |
| Some juices make me feel like I have extra mucus in my throat that I can’t quite swallow, almost like when you have a head cold draining mucus down the back of throat. | 2.67 | |
| Sometimes the vapor is too hot and I cough. | 2.67 | |
| Headaches from dropping nicotine levels too fast. | 2.65 | |
| A tingling sensation in the back of my throat that feels like the onset of a cough. | 2.65 | |
| Feeling jittery because of the nicotine. | 2.61 | |
| Metallic taste after using a metal drip tip. | 2.56 | |
| When the ECIG gets too hot it makes me choke. | 2.51 | |
| Sometimes the sweet flavors make me want to eat candy. | 2.42 | |
| Condensation on my mustache from exhale. | 2.42 | |
| Tired after too much nicotine. | 2.39 | |
| It makes my sinuses feel funny. | 2.26 | |
| Extremely hot vapor from dripper burns my lungs. | 2.23 | |
| Over the last few weeks, when I use my ECIG for the first time in the morning, I do feel a bit of heaviness in my breathing. | 2.21 | |
| Burned lip because I forgot the top cap. | 2.12 | |
| The nauseous feeling when I vape on an empty stomach. | 2.00 | |
| Immediate need for a bowel movement. | 1.56 | |
| Loose tooth from hitting it with my ECIG drip tip. | 1.46 | |
| 4. Addiction Signs | 2.72 | |
| Sometimes I vape too much under stress. | 4.56 | |
| It’s hard for me to put down. | 4.51 | |
| The buzz is not the same as regular cigarettes. | 3.11 | |
| There is a withdrawal when phasing out cigarettes due to the high level of nicotine in cigarettes and lower levels in vapor. | 2.54 | |
| A desire for more nicotine. | 2.42 | |
| Psychological affects make me want to smoke. | 2.21 | |
| Not getting real cigarette flavor. | 2.14 | |
| Disappointment from never getting a nicotine buzz like I got from cigarettes. | 2.12 | |
| It is hard to completely discontinue the use of cigarettes. | 1.82 | |
| A desire for real smoke. | 1.75 | |
| Problems with ECIG device | ||
| 5. Device/Vapor | 3.88 | |
| Problems | ||
| Disliking a flavor after purchase. | 5.53 | |
| Being disappointed with a flavor after the first few uses. | 4.88 | |
| Juice (e-liquid) on my devices. | 4.86 | |
| Having to charge batteries. | 4.67 | |
| “Gunked-up” coils causing a nasty hit. | 4.58 | |
| Occasionally burning my wicking material. | 4.56 | |
| Occasionally the e-liquid will leak from the mouthpiece and cause an unpleasant burning/tingling sensation. | 4.37 | |
| Flavors leaving bad aftertaste. | 4.30 | |
| Battery fails at inopportune times. | 4.11 | |
| Hits are sometimes inconsistent, even when using a fresh battery and cartridge. | 3.93 | |
| Taste of burning liquid. | 3.88 | |
| I have to carry my ECIG/vape gear with me because I can’t leave it in the car on a hot day, heats up the e-juice (e-liquid) and makes the tanks leak. | 3.86 | |
| Drip tip gets hot. | 3.75 | |
| Lingering flavor from using cinnamons, anises, or heavy menthols. | 3.12 | |
| Some juices (e-liquids) taste like alcohol. | 2.84 | |
| Sometimes the vapor smells bad. | 2.81 | |
| Burns from an atomizer when the mod has been auto-firing for a minute or more. | 2.75 | |
| Variable voltage battery adjusts to wrong voltage when put in pocket. | 2.72 | |
| Electronic devices are prone to failure and leads to smoking cigarettes during the repair or replacement. | 2.30 | |
ECIG = electronic cigarette.
Psychological Effects
Stigma
The statements in this cluster ( M = 4.54, SD = 0.73) described participants’ perception of being viewed negatively due to their ECIG use. In particular, many of the statements documented the frustration or resentment of ECIG users being categorized in the same groups as traditional combustible cigarette smokers. Common statements in this cluster described negative emotions as a result of being considered a “smoker,” being required to exit a building/use an ECIG outdoors despite not smoking a combustible cigarette, and being told that ECIG use is associated with similar harms compared to combustible cigarettes as adverse effects associated with ECIG use.
Worry/Guilt
The statements in this cluster ( M = 3.11, SD = 0.94) generally described concerns and worry regarding outcomes associated with ECIG use. Some of the statements were more focused on the guilt associated with ECIG use effects on the ECIG user. For instance, some statements indicated feelings of guilt for spending too much money on ECIG paraphernalia while others described feelings of guilt associated with inability to abstain from an addictive behavior. Other statements in the category addressed worry due to the potential effect of ECIG use on loved ones. These statements included concern that children may think ECIG use is acceptable because of parental use or worry that a female romantic partner may continue to use an ECIG after becoming pregnant.
Physiological Effects
Physical Effects
The statements in this cluster ( M = 2.70, SD = 0.66) described adverse physical outcomes associated with ECIG use, much like side effects associated with drug use. This cluster contained the most statements of all clusters ( n = 28). Statements in this cluster described a wide variety of negative side effects associated with ECIG use of varying degrees of potential health concern. For instance, some statements appeared to be relatively minor in terms of health effects including statements describing the ECIG vapor flavors not tasting as strongly after prolonged ECIG use, having a dry mouth from continued use, or needing to drink water continuously as a result of ECIG use. Other statements described ECIG use being associated with stronger adverse effects including coughing due to hot vapor, feeling nauseated, burning one’s lip on the ECIG device, or having increased mucus in the throat or nose. Some statements also described the perception of a causal link between the nicotine in the ECIG liquid and some of the adverse effects. These events included feeling tired, feeling jittery, having headaches, and feeling nauseated due to too much or too little nicotine in ECIG liquid.
Addiction Signs
The statements in this cluster ( M = 2.72, SD = 0.98) described adverse effects of ECIG use that appeared to be related to addiction symptoms such as withdrawal and cravings. Many of the statements appeared to indicate signs of dependence. For instance, statements described the difficulty of putting down one’s ECIG device, vaping under stress, and the desire for higher amounts of nicotine. A larger subset of the statements in this cluster indicated the lack of satisfaction from ECIG use compared to combustible tobacco use. These statements described the desire for “real” smoke, not getting real cigarette flavor, not getting the same buzz as combustible cigarettes, and feelings of withdrawal when switching from cigarettes to ECIGs as adverse effects associated with ECIG use.
Problems With ECIG Device
Device/Vapor Problems
The statements in this cluster ( M = 3.88, SD = 0.88) described how problems with ECIG devices or device and user interactions could be associated with adverse effects. Compared to other clusters, the majority of statements in the Device/Vapor Problems cluster did not relate as strongly to direct psychological or physiological adverse effects from ECIG use, but rather described how certain issues with ECIG device components could result in negative ECIG use experiences. Some statements described adverse effects that may represent common annoyances associated with ECIG use such as batteries failing at inopportune times or being required to carry equipment necessary for ECIG use when away from the home. Other statements described events that appeared to represent disappointment or dissatisfaction with the device including being disappointed with vapor flavor, having a bad taste in one’s mouth after ECIG use, or perceiving the vapor to smell bad. Other statements, however, described potentially harmful adverse effects related to device problems such as feeling tingling sensations on parts of the body that directly contact the ECIG liquid or burning oneself on the ECIG device.
Cluster Ratings
On average, participants rated clusters between 2.70 and 4.54 (out of 7) for experiencing events described in the statements within each cluster. As displayed in the cluster rating map ( Figure 1 ), participants were more likely to report experiencing statements within certain clusters compared to others. Overall, participants reported the highest ratings for statements in the Stigma cluster ( M = 4.54) followed by the Device/Vapor Problems ( M = 3.88), Worry/Guilt ( M = 3.12), Addiction Signs ( M = 2.72), and Physical Effects ( M = 2.70) clusters. Statements in the Stigma cluster were rated on average significantly higher than statements in the Device/Vapor Problems ( t (30) = 2.29, P < .05), the Worry/Guilt ( t (20) = 3.84, P < .002), the Addiction Signs ( t (21) = 4.93, P < .001), and the Physical Effects ( t (39) = 7.76, P < .001) clusters. This indicated that participants were most likely to report experiencing statements from the Stigma cluster compared to statements from all other clusters.
While cluster ratings were not significantly associated with sex, ethnicity, or race, average cluster ratings were significantly associated with certain ECIG use characteristics. Participants who reported “dripping” their ECIG liquid rated the statements in the Physical Effects cluster higher ( M = 2.95) compared to participants who reported using ECIG devices with tank systems ( M = 2.44; t (54) = 2.67, P < .01). ECIG users with greater experience (greater than 2 years of ECIG use) rated statements in the Physical Effects cluster lower ( M = 2.28) compared to ECIG users who reported less than 2 years of ECIG use ( M = 2.29; t (54) = 3.73). Newer and more experienced users also differed on ratings of statements in the Worry/Guilt cluster. Participants who reported less than 1 year of ECIG use reported higher ratings of statements in the Worry/Guilt cluster ( M = 3.47) compared to ECIG users who reported more than 2 years of ECIG use ( M = 2.53; t (16) = 2.16, P < .05).
Discussion
As ECIGs continue to grow in popularity, public health professionals need be informed of the potential adverse effects associated with ECIG use. This study used CM to identify five broad clusters of adverse effects associated with ECIG use as described by experienced ECIG users. These statements identified by participants indicated that the adverse effects of ECIG use appear to relate to psychological, physiological, and device problems. Participant were most likely to identify feeling stigmatized for their ECIG use as an adverse event, however, ratings for frequency of all of the adverse effects of ECIG use clusters were relatively low. ECIG use characteristics including ECIG device type used and level of ECIG experience/time since initiating ECIG use were associated with greater levels of some of the adverse effect clusters. Newer ECIG users and “drippers” were more likely to experience negative physical effects of ECIG use and newer users were also more likely to experience adverse effects related to worry/guilt.
The implications for the findings of this study are difficult to determine, however, several discussion points can be raised. First, the adverse effects in the Physical Effects cluster should be investigated further. Though the outcomes identified in this cluster vary in severity of harm to the ECIG user, some of these adverse effects could be indicators or greater harm or potential future negative health effects (eg, post nasal drip after ECIG use or feeling like one’s lungs are burning). In addition to monitoring these types of effects, regulatory bodies may consider requiring manufacturers to disclose reported adverse effects that could be indicative of harm. Second, given that many ECIG users report using ECIGs to quit other forms of tobacco use, the Addiction Signs cluster represents cause for concern. The statements in this cluster describe levels of dissatisfaction with ECIG products and desires for using traditional cigarettes. While there is still debate on whether switching from combustible cigarettes to ECIGs represents a harm reduction strategy, the statements in this cluster suggest some ECIG users may be at risk for either dual use of ECIGs and combustible cigarettes or returning to combustible cigarette use.
While statements in the Stigma, Worry/Guilt, and Device/Vapor Problems clusters may not represent the same concerns for acute adverse health effects or signs of addiction that are important to health professionals, statements from these clusters may warrant further investigation. Given that ECIGs are still a relatively new class of products, especially compared to combustible cigarettes, ECIG users’ perceptions of the statements from the Stigma and Worry/Guilt clusters may change as ECIG continue to grow in popularity and normalcy in the United States. Perhaps ECIG users who experience more events from the perceived Stigma and Worry/Guilt clusters may be less likely to continue ECIG use. Similarly, ECIG users who report more problems with their devices may lose interest in ECIG use. Future work examining how reported adverse effects such as those identified in the Stigma, Worry/Guilt, and Device/Vapor Problems clusters impact ECIG use as well as use of other tobacco products over time would be useful for regulatory bodies and health professionals.
There are several points to consider when interpreting the results of this study. Though participants were asked to identify adverse effects that were specifically attributed to their ECIG use, the connection between participant reported effects and ECIG use is based on participant interpretation. That is, some of the reported adverse effects could have been caused by other factors (eg, coughing due to allergies or a cold as opposed to ECIG use). Conversely, participants may have failed to report adverse effects not perceived to be connected to their ECIG use when in fact these effects were caused by their ECIG use. Participants in this study were experienced ECIG users, meaning they were regular users who were well past the ECIG experimentation and initiation stage. Just as trying alcohol or cigarettes for the first time is often somewhat aversive, the initial ECIG uses may be associated with more acute adverse effects than ECIG use after one is experienced. Therefore, someone trying an ECIG for the first time may experience other adverse effects than those described in this study or possibly the same adverse effects with varying intensities. Finally, some individuals who try ECIGs may experience adverse effects that are significant enough to prevent further experimentation and continued use. As a result, the findings from this study are likely most generalizeable to experienced ECIG users. A study examining adverse effects of ECIG use among those who tried ECIGs but did not progress to regular use may reveal more adverse effects associated with ECIG, possibly some that are more unpleasant than those identified in this study.
An intriguing finding of this study was that more experienced users rated the Worry/Guilt and Physical Effects statements lower than new ECIG users. This study cannot determine whether the actual occurrence of these adverse effects decrease as ECIG user experience increases or users modify their perceptions of what constitutes an adverse effect, but future studies could investigate if these changes in adverse effects perceptions represent actual changes or psychological processes such as efforts to reduce cognitive dissonance. Research should examine how perceptions of adverse effects of ECIG use change as individuals gain more experience with ECIGs.
As ECIGs continue to grow in popularity and devices continue to evolve, new adverse effects associated with ECIG use will likely emerge, however, these adverse effects are almost impossible to predict. For instance, when tank systems and nicotine-containing liquid became available for purchase, a new risk of poisoning arose. 37 Similarly, other ECIG innovations may result in unforeseeable ECIG-associated adverse effects. These known and potential adverse effects will need to be considered when determining the appropriate ways to regulate or not regulate ECIG devices including product characteristics, marketing, and policies regarding where and how ECIGs can be used.
Funding
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number P50DA036105 and the Center for Tobacco Products of the US Food and Drug Administration. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Food and Drug Administration.
Declaration of Interests
SR is a senior consultant at Concept Systems Incorporated. SR provides consultations on concept mapping methods and concept mapping software.
Acknowledgments
We would like to thank Ms Mckayla Stokes and Ms Mckenzie Stokes for their contributions to this study.
References
- 1. U. S. Department of Health and Human Services . The Health Consequences of Smoking – 50 Years of Progress: A Report of the Surgeon General . Atlanta, GA: : U. S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; ; 2014. . [Google Scholar]
- 2. Hajek P, Etter JF, Benowitz N, Eissenberg T, McRobbie H . Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit . Addiction . 2014. ; 109 ( 11 ): 1801 – 1810 . doi: 10.1111/add.12659 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Regan AK, Promoff G, Dube SR, Arrazola R . Electronic nicotine delivery systems: adult use and awareness of the ‘e-cigarette’ in the USA . Tob Control . 2013. ; 22 ( 1 ): 19 – 23 . doi: 10.1136/tobaccocontrol-2011-050044 . [DOI] [PubMed] [Google Scholar]
- 4. McMillen R, Maduka J, Winickoff J . Use of emerging tobacco products in the United States . J Environ Public Health . 2012. ; 2012 : 989474 . doi: 10.1155/2012/989474 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. King BA, Patel R, Nguyen KH, Dube SR . Trends in awareness and use of electronic cigarettes among US adults, 2010-2013 . Nicotine Tob Res . 2015. ; 17 ( 2 ): 219 – 227 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McMillen RC, Gottlieb MA, Shaefer RM, et al. Trends in electronic cigarette use among U. S. adults: use is increasing in both smokers and nonsmokers [published online ahead of print November 6, 2014]. Nicotine Tob Res . doi: 10.1093/ntr/ntu213 . [DOI] [PubMed] [Google Scholar]
- 7. Sutfin EL, McCoy TP, Morrell HE, Hoeppner BB, Wolfson M . Electronic cigarette use by college students . Drug Alcohol Depend . 2013. ; 131 ( 3 ): 214 – 221 . doi: 10.1016/j.drugalcdep.2013.05.001 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Choi K, Forster JL . Beliefs and experimentation with electronic cigarettes: a prospective analysis among young adults . Am J Prev Med . 2014. ; 46 ( 2 ): 175 – 178 . doi: 10.1016/j.amepre.2013.10.007 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Saddleson ML, Kozlowski LT, Giovino GA, et al. . Risky behaviors, e-cigarette use and susceptibility of use among college students . Drug Alcohol Depend . 2015. ; 149 : 25 – 30 . doi: 10.1016/j.drugalcdep.2015.01.001 . [DOI] [PubMed] [Google Scholar]
- 10. Berg CJ, Stratton E, Schauer GL, et al. Perceived harm, addictiveness, and social acceptability of tobacco products and marijuana among young adults: marijuana, hookah and electronic cigarettes win . Subst Use Misuse . 2015. ; 50 ( 1 ): 79 – 89 . doi: 10.3109/10826084.2014.958857 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Camenga DR, Kong G, Cavallo DA, et al. Alternate tobacco product and drug use among adolescents who use electronic cigarettes, cigarettes only, and never smokers . J Adolesc Health . 2014. ; 55 ( 4 ): 588 – 591 . doi: 10.1016/j.jadohealth.2014.06.016 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention . Tobacco product use among middle and high school students – United States, 2011 and 2012 . MMWR Morb Mortal Wkly Rep . 2013. ; 62 ( 45 ): 893 – 897 . [PMC free article] [PubMed] [Google Scholar]
- 13. Barnett TE, Soule EK, Forrest JR, et al. Adolescent electronic cigarette use: associations with conventional cigarette and hookah smoking . Am J Prev Med . 2015. ; 49 ( 2 ): 199 – 206 . doi: 10.1016/j.amepre.2015.02.013 . [DOI] [PubMed] [Google Scholar]
- 14. Krishnan-Sarin S, Morean ME, Camenga DR, Cavallo DA, Kong G . E-cigarette use among high school and middle school adolescents in Connecticut . Nicotine Tob Res . 2015. ; 17 ( 7 ): 810 – 818 . doi: 10.1093/ntr/ntu243 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Centers for Disease Control and Prevention . Tobacco use among middle and high school students – United States, 2011–2014 . MMWR Morb Martal Wkly Rep . 2015. ; 64 ( 14 ): 381 – 385 . [PMC free article] [PubMed] [Google Scholar]
- 16. Li J, Newcombe R, Walton D . The prevalence, correlates and reasons for using electronic cigarettes among New Zealand adults . Addict Behav . 2015. ; 45 : 245 – 251 . doi: 10.1016/j.addbeh.2015.02.006 . [DOI] [PubMed] [Google Scholar]
- 17. Bunnell RE, Agaku IT, Arrazola RA, et al. . Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011–2013 . Nicotine Tob Res . 2015. ; 17 ( 2 ): 228 – 235 . doi: 10.1093/ntr/ntu166 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Moore GF, Littlecott HJ, Moore L, et al. . E-cigarette use and intentions to smoke among 10-11-year-old never-smokers in Wales [published online ahead of print December 22, 2014]. Tob Control . doi: 10.1136/tobaccocontrol-2014-052011 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ambrose BK, Rostron BL, Johnson SE, et al. Perceptions of the relative harm of cigarettes and e-cigarettes among U.S. youth . Am J Prev Med . 2014. ; 47 ( 2S1 ): S53 – S60 . doi: 10.1016/j.amepre.2014.04.016 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kong G, Morean ME, Cavallo DA, Camenga DR, Krishnan-Sarin S . Reasons for electronic cigarette experimentation and discontinuation among adolescents and young adults . Nicotine Tob Res . 2015. ; 17 ( 7 ): 847 – 854 . doi: 10.1093/ntr/ntu257 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tan ASL, Bigman CA . E-cigarette awareness and perceived harmfulness: prevalence and associations with smoking-cessation outcomes . Am J Prev Med . 2014. ; 47 ( 2 ): 141 – 149 . doi: 10.1016/j.amepre.2014.02.011 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shihadeh A, Saleh R . Polycyclic aromatic hydrocarbons, carbon monoxide, “tar”, and nicotine in the mainstream smoke aerosol of the narghile water pipe . Food Chem Toxicol . 2005. ; 43 ( 5 ): 655 – 661 . [DOI] [PubMed] [Google Scholar]
- 23. Eissenberg T, Shihadeh A . Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure . Am J Prev Med . 2009. ; 37 ( 6 ): 518 – 523 . doi: 10.1016/j.amepre.2009.07.014 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Monzer B, Sepetdjian E, Saliba N, Shihadeh A . Charcoal emissions as a source of CO and carcinogenic PAH in mainstream narghile waterpipe smoke . Food Chem Toxicol . 2008. ; 46 ( 9 ): 2991 – 2995 . doi: 10.1016/j.fct.2008.05.031 . [DOI] [PubMed] [Google Scholar]
- 25. Nguyen T, Hlangothi D, Martinez RA, III, et al. . Charcoal burning as a source of polyaromatic hydrocarbons in waterpipe smoking . J Environ Sci Health B . 2013. ; 48 ( 12 ): 1097 – 1102 . doi: 10.1080/03601234.2013.824300 . [DOI] [PubMed] [Google Scholar]
- 26. Al Rashidi M, Shihadeh A, Saliba NA . Volatile aldehydes in the mainstream smoke of the narghile waterpipe . Food Chem Toxicol . 2008. ; 46 ( 11 ): 3546 – 3549 . doi: 10.1016/j.fct.2008.09.007 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Schubert J, Bewersdorff J, Luch A, Schulz TG . Waterpipe smoke: a considerable source of human exposure against furanic compounds . Anal Chim Acta . 2012. ; 709 : 105 – 112 . doi: 10.1016/j.aca.2011.10.012 . [DOI] [PubMed] [Google Scholar]
- 28. Cobb CO, Shihadeh A, Weaver MF, Eissenberg T . Waterpipe tobacco smoking and cigarette smoking: a direct comparison of toxicant exposure and subjective effects . Nicotine Tob Res . 2011. ; 13 ( 2 ): 78 – 87 . doi: 10.1093/ntr/ntq212 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shishani K, Howell D, McPherson S, Roll J . Young adult waterpipe smokers: Smoking behaviors and associated subjective and physiological effects . Addict Behav . 2014. ; 39 ( 6 ): 1113 – 1119 . doi: 10.1016/j.addbeh.2014.03.010 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Blank MD, Cobb CO, Kilgalen B, et al. Acute effects of waterpipe tobacco smoking: a double-blind, placebo-control study . Drug Alcohol Depend . 2011. ; 116 ( 1–3 ): 102 – 109 . doi: 10.1016/j.drugalcdep.2010.11.026 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Maziak W, Rastam S, Ibrahim I, Ward KD, Shihadeh A, Eissenberg T . CO exposure, puff topography, and subjective effects in waterpipe tobacco smokers . Nicotine Tob Res . 2009. ; 11 ( 7 ): 806 – 811 . doi: 10.1093/ntr/ntp066 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. DeRidder D, Depla M, Severens P, Malsch M . Beliefs on coping with illness: a consumer’s perspective . Soc Sci Med . 1997. ; 44 ( 5 ): 553 – 559 . [DOI] [PubMed] [Google Scholar]
- 33. Trochim W, Milstein B, Wood B, Jackson S, Pressler V . Setting objectives for community and systems change: an application of concept mapping for planning a statewide health improvement initiative . Health Promot Pract . 2004. ; 5 ( 1 ): 8 – 19 . [DOI] [PubMed] [Google Scholar]
- 34. Stillman FA, Schmitt CL, Rosas SR . Opportunity for collaboration: a conceptual model of success in tobacco control and cancer prevention . Prev Chronic Dis . 2012. ; 9 : E02 . [PMC free article] [PubMed] [Google Scholar]
- 35. Rosenberg S, Kim MP . The method of sorting as a data gathering procedure in multivariate research . Multivar Behav Res . 1975. ; 10 ( 4 ): 489 – 502 . doi: 10.1207/s15327906mbr1004_7 . [DOI] [PubMed] [Google Scholar]
- 36. Weller SC, Romney AK . Systematic Data Collection . Newbury Park, CA: : Sage; ; 1988. . [Google Scholar]
- 37. Centers for Disease Control and Prevention . Calls to poison control centers for exposures to electronic cigarettes – United States, September 2010-February 2014 . MMWR Morb Martal Wkly Rep . 2015. ; 63 ( 13 ): 292 – 293 . [PMC free article] [PubMed] [Google Scholar]