Abstract
Background
A general conclusion about the treatment of chronic, noncancer pain is that the results from traditional, passive modalities are disheartening. Perhaps this may be due to the propensity of patients to seek out passive versus active treatments. In pain management, active treatments should be the primary focus, with passive interventions as an adjunct.
Objective
The current study tested the hypotheses that Veterans would report a greater significant increase in active versus transitional and active versus passive complementary and integrative health (CIH) utilization after completing a formal pain education program.
Methods
The current study is a secondary analysis of existing data from an original study. The current study used a quasi-experimental, 1-group, pre-/posttest design. One hundred three Veterans completed a 12-week, “Pain Education School” program at a Midwestern VA Medical Center between November 4, 2011, and October 26, 2012. As part of the introduction and conclusion of the program, all Veterans completed a pre- and posteducation assessment which included an adaptation of the Complementary and Alternative Medicine Questionnaire©, SECTION A: Use of Alternative Health Care Providers measure.
Results
Significant differences were found between the pre- and posttest measures of use of active (P = .000) (p<.001), transitional (P = .011), and passive (P = .007) CIH modalities.
Conclusion
The current findings suggest that an educational intervention in conjunction with the availability of treatment options has the potential to increase the use of those treatments. The current pain education program also seems to be aligned with the goal of pain self-management, which is to utilize more active interventions as a primary therapy.
Keywords: complementary and integrative health, pain education, Veterans, active treatments, passive treatments
The overall treatment effectiveness for traditional modalities for chronic pain remains inconsistent and fairly poor; the best evidence averages around 30% in about half of treated patients.1 Perhaps this may be due to the propensity of patients to seek out passive treatments (such as medications, interventions, and surgery) versus active alternatives (such as self-hypnosis, relaxation techniques, and mindfulness practices).
In pain management, active treatments should be the primary focus, with passive interventions as an adjunct, not the other way around.2 Active, or activating, treatments can be available where and when the patient needs to manage the pain.3 However, they rely on the patient to actively participate in these techniques at home away from the clinic. It has been posed that the active approach offers the potential to change physical factors, such as pain, strength, and motor control, and psychological factors, such as self-efficacy and fear avoidance.4 Past research has shown that active movement and behavioral treatments for chronic low back pain are generally effective.5,6
Passive therapies tend to be discouraged as a primary focus because they have the potential of reinforcing feelings of powerlessness in the patient and put the onus of responsibility for pain management back in the hands of the provider.3 Passive treatments require the patient to be a submissive recipient of treatment. Passive treatment can help with immediate pain relief, but active treatment keeps the patient functional in the long term.7 For example, when a patient undergoes a surgery and fails to follow a proper rehabilitation program, he/she may still have pain long after recovering from his/her operation. Many passive interventions have shown positive effects for acute low back pain.8–10 In addition, passive interventions are the most commonly prescribed treatments for chronic low back pain despite the above observances.11 Interestingly, the interventions shown to be effective in acute low back pain appear less effective in chronic low back pain.5,11,12
It has been recommended that passive modalities not be employed except when necessary to facilitate participation in an active treatment program.2 Although passive treatments can be effective, it is critical to shift the patient into a model of active care. Active care can counter-stimulate the pain in the brain or teach the brain to move the relentless, persistent, and constant pain signaling to comfort and pleasure.13,14 Thus, it is recommended patients move from a passive “disempowering” stance to a more active “empowering” stance. It may be helpful to think of all of these treatments existing in a continuum, with passive treatments being on one end and active on the other. In the middle, one could envision treatments as being “transitional.” For example, a chiropractor may transition from using myofascial release to teaching the patient exercises to do at home to increase range of motion when offering spinal manipulation.15 Thus, the chiropractor would rely on the patient to actively participate in the techniques away from clinic. This is different from a massage therapist or acupuncturist who could teach someone else on how to perform the techniques but still would require the patient to continue being a submissive recipient of the treatment from another person.
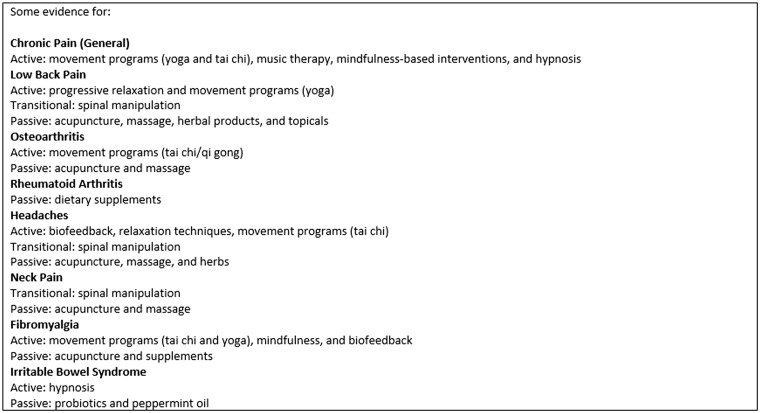
There is promising scientific evidence to support the use of complementary and integrative health (CIH) approaches for noncancer pain conditions, such as low back pain, arthritis, and headaches, and limited support for neck pain (see Figure 1).16 Clinical trials have also indicated the comparable efficacy of CIH modalities with traditional chronic pain treatments, such as acupuncture and behavioral therapy compared to exercise therapy and pharmacotherapy.17 Thus, the purpose of the current study was to determine whether a patient pain education program benefitted Veterans who suffer from chronic, noncancer pain by focusing more on active CIH treatments. Such an education-focused, professionally driven program assumes that if individuals are provided with adequate education, they will be empowered and self-manage chronic pain.18 The current study tested the hypotheses that Veterans would report a greater significant increase in (1) active versus transitional and (2) active versus passive CIH utilization after completing a formal pain education program in a Veterans Affairs medical center.
Figure 1.
Complementary and Integrative Health Findings.
Methods
Five hundred twenty-four Veterans were originally referred to the 12-week, “Pain Education School” program at a Midwestern VA Medical Center from several different clinics within the facility between November 4, 2011, and October 26, 2012. Potential candidates had several characteristics, including having failed medical/surgical treatment, exhibited an overreliance on medications/therapies, displayed pronounced inactivity, suffered from significant depression or anxiety related to his/her pain, demonstrated inadequate coping skills, and/or appeared receptive to adopting a self-management approach to pain management. The current study excluded Veterans diagnosed only with cancer pain. There were no other exclusion criteria. The referring provider submitted a consult in the computerized patient record system. Potential candidates were then added to the waiting list for the next available monthly mandatory introduction class. From this target population, a sample of almost half (N = 243) of the Veterans enrolled in the program and attended the introduction class. From this sample, 94% of the Veterans elected to complete the pre-education assessment. Each Veteran in this sample was subsequently scheduled for 11 weeks of 1-h classes. Participation in subsequent classes was voluntary. Veterans were encouraged to bring significant others when they attended classes. Veterans were given free parking validation/transportation reimbursement if they were in attendance and were qualified for such programs. Nearly half (N = 103) of the sample who completed the pre-education assessment also elected to complete the posteducation assessment, and their responses were included in the current study (see Figure 2). A recent VA Evidence-based Synthesis Program report (intranet communication, December 2012) indicated that group visits focusing on education for the management of chronic conditions in Veterans tend to suffer from high levels of attrition which was substantiated by the current study.
Figure 2.

Flowchart of Study Participants.
The current study is a secondary analysis of existing data from an original study.19 The purpose of the original study was to test the hypothesis that Veterans would report an increase in overall CIH utilization after completing a formal pain education program in a VA medical center. Using the research question approach, the current authors had a priori hypotheses in mind and utilized the existing data set to address the question and handled it appropriately. The current study protocol was reviewed and approved by the affiliated university’s Institutional Review Board and the VA’s Research and Development office. A waiver of informed consent was submitted because the current investigation is a secondary analysis of existing data from an original study.
Intervention
The “Pain Education School” was developed in November 2009 at a Midwestern VA medical center using the Agency for Healthcare Research and Quality’s principles and the VA’s National Center for Health Promotion and Disease Prevention’s manual.20 The goals of the program were to share basic principles of pain relief and prevention and introduce services offering interventions for relief of chronic, noncancer pain including CIH modalities.21 A goal-based evaluation of the development and implementation of the program is available in the literature.22 The program consisted of an introduction class followed by twelve 1-h classes offered weekly that were led by guest speakers from over 20 different disciplines within the facility—13 of which are CIH modalities delineated below on the next page. The introduction class covered the ground rules, schedule of classes, and basic principles of the bio-psycho-social-spiritual approach to pain self-management. The menu of treatment modalities was then scheduled on a rotating basis regardless of the Veteran’s entry point—the providers from each discipline rotated on a schedule, not the Veterans. Since the schedule rotates, the later sessions are never the same for all the Veterans in the study which should decrease any position effect. Providers from each discipline shared information about chronic, noncancer pain from their perspective, what treatments were available in their service, and how to access their respective clinics. Lecturers just introduced the CIH modalities and did not provide any inducement for use. Veterans could ask questions and receive authoritative and useful answers from the providers themselves at the end of each class. Veterans also had access to each CIH modality immediately after it was presented in the program—patients did not have to wait till the completion of the program to begin seeking treatment. To account for differences in adult learning, audio, visual, and tactile methods were implemented during each class. Subsequent research studies have found that the Pain Education School program has shown to decrease pain intensity, improve pain knowledge and change beliefs about pain, make changes in subjective pain experiences, and create positive changes on depression measures.23,24
Outcome Measure
As part of the introduction and at the last session of the program, all Veterans completed a pre- and posteducation assessment. The assessment included questions which asked Veterans if they had ever been treated by specific CIH modalities. This questionnaire was adapted from the Complementary and Alternative Medicine (CAM) Questionnaire©, SECTION A: Use of Alternative Health Care Providers.25 Veterans responded either “no (0)” or “yes (1),” and if “yes” they were asked “then how long?” about their use of 13 different CIH modalities. These responses were then added up to calculate utilization. CIH modalities were then grouped for the analyses based on the type of CIH treatment, including the following active, transitional, or passive modalities:
Active: acceptance and commitment therapy/mindfulness, biofeedback/relaxation training, hypnosis, movement programs, music/art therapy, and spirituality/religion.
Transitional: chiropractic care and osteopathic manipulation.
Passive: acupuncture, aromatherapy, healing touch, massage therapy, and traditional healers.
The grouping of these modalities was then verified by the guest speakers from the different disciplines who led the classes from the intervention. Permission has been obtained to use an adaptation of the CAM Questionnaire in a publication and research trial from the California Health Interview Survey project.
Data Analyses
The current study is a secondary analysis of existing data from an original study.19 The current study used a quasi-experimental, 1-group, pre/posttest design. Chi-squares identified differences on demographic and outcome variables at baseline. The current study tested the hypotheses that Veterans would report a greater significant increase in (1) active versus transitional and (2) active versus passive CIH utilization after completing a formal pain education program using paired samples t tests to compare pre- and postassessment means of active, transitional, and passive CIH counts. Results will be reported using the following t test statistics:
Mdiff = The mean difference, or difference in means, measures the absolute difference between the mean value in 2 different groups.
SD = The standard deviation is a measure that is used to quantify the amount of variation or dispersion of a set of data values.
t = The t value measures the size of the difference relative to the variation in your sample data.
d = Cohen’s d is one of the most common ways to measure effect size. An effect size is how large an effect an intervention has on the intended variable.
Outcome analyses used an efficacy subset analysis strategy which selects the subset of the patients who received the intended programming and who did not drop out for any reason. A last-observation-carried-backward approach26 was used for missing data on the pre-education assessment, and a last-observation-carried-forward approach27 was used for missing data on the posteducation assessment. The Power and Sample Size Program28 was utilized to calculate sample size using an anticipated effect size (Cohen’s d) of 0.5, a desired statistical power level greater than or equal to 0.80, and a probability level less than or equal to 0.05. The minimum total sample size (pairs of subject scores) was N = 33. SPSS version 23 was used for all outcome analyses. The results are presented using Transparent Reporting of Evaluations with Nonrandomized Designs guidelines.
Results
Sample Characteristics
The responses from the 103 remaining Veterans were included in the outcome analyses in the current study. The Veteran sample had mixed idiopathic chronic, noncancer pain conditions, including back pain (75%), neck pain (13%), extremity pain (7%), head pain (3%), and fibromyalgia/soft tissue pain (2%). Most Veterans were African American (58%), but 36% were Caucasian, 5% identified as being Hispanic/Latino, and in 1% race was unknown. Most were males (82%), but there were also a large number of female Veterans (18%). The average “Pain Education School” Veteran attended 7 out of 12 classes, with Veterans most frequently (mode) attending 11 out of 12 classes. 13% (N = 31) of the Veteran sample only attended the introductory class. There were no significant differences found in Veterans utilization of active, passive, or transitional CIH modalities based on sex, racial/ethnic group, and/or completers/drop outs at the baseline (see Table 1). Most of the Veterans were 55 to 64 years (37%), and the youngest returning Veterans (17–24 years) were not represented in the current sample. The current findings specifically indicate that younger Veterans were more likely to seek passive CIH modalities than their older counterparts, F(5,97) = 3.84, P = .003. No other significant differences were found in active or transitional CIH use by age-group.
Table 1.
Baseline CIH Utilization by Patient Characteristics (N = 243).
| CIH Modality | Completers |
|
|---|---|---|
| X 2 | P | |
| Active | ||
| ACT/mindfulness | 0.000 | .607 |
| Biofeedback/relaxation | 0.301 | .359 |
| Hypnosis | 1.561 | .458 |
| Movement (eg, yoga) | 2.153 | .341 |
| Music/art therapy | 1.167 | .193 |
| Spirituality/religion | 0.099 | .443 |
| Transitional | ||
| chiropractor | 0.007 | .527 |
| Osteopathic manipulation | 1.831 | .400 |
| Passive | ||
| acupuncture | 0.065 | .473 |
| Aromatherapy | 0.174 | .473 |
| Healing touch | 0.079 | .510 |
| Massage therapy | 2.107 | .097 |
| Traditional healer | 0.223 | .407 |
indicates p-value is significant at p<.05
indicates p-value is significant at p<.01
Nearly 44% (N = 45) of Veterans reported not using any type of CIH at the baseline. The remaining 56% of Veterans utilized different combinations of CIH at the baseline, including active (30%), passive (41%), and transitional (36%) CIH modalities. Pre- and postcounts of CIH users by type was also delineated at the baseline. Approximately 16% of Veterans reported not using any type of CIH after completing the Pain Education School program; which is more than a 25% difference from the baseline. The remaining 84% of Veterans reported increases in different combinations of CIH after completing the patient education program, including active (24%), passive (12%), and transitional (14%) CIH modalities. A diagram of the pre- and postcount percentages of CIH users by type illustrated an overall increase in utilization and a shift away from passive to transitional and active CIH modalities (see Figure 3).
Figure 3.

Pre- and Postpercentage of (CIH) Users.
Program Outcome
Significant differences were found between the pre- and posttest measures (Mdiff = −0.54, SD = 1.29) of use of active CIH modalities—t(102) = −4.28, p<.001, d =−0.45; the pre- and posttest measures (Mdiff = −0.19, SD = 0.71) of use of transitional CIH modalities—t(102) = −2.76, P = .011, d = −0.28; and the pre- and posttest measures (Mdiff = −0.23, SD = 0.91) of use of passive CIH modalities—t(102) = −2.60, P = .007, d = −0.22. The mean numbers are the total counts of modalities.
Discussion
People who suffer from chronic pain tend to go for short-term relief at a long-term cost. Perhaps the reason why patients gravitate to passive treatments is because medical providers have reinforced the belief that these treatments are the standard of care for chronic pain management which has led to their participation. Scholars in pain medicine have recommended that providers focus more on offering active treatments and utilize passive interventions as an adjunct to chronic pain management. Active techniques have a synergistic rather than a mere additive effect when combined with other interventions. Active treatments have the added benefit of reinforcing the self-management approach to pain management, as opposed to passive interventions which have been shown to put the responsibility back in the providers’ hands. Past research has also indicated that the implementation of pain education programming can increase Veteran utilization of CIH.19 However, research investigating differences in utilization among active, transitional, and passive CIH modalities among Veterans is lacking. The primary purpose of the current study was to investigate whether completion of a formal patient pain education program would increase utilization of active versus transitional and active versus passive CIH among Veterans.
Findings from the current study indicate that participants overall increased their utilization of active, transitional, and passive CIH modalities upon completion of the Pain Education School. This finding is consistent with past research which has found that providing adequate self-management education will increase practice of the cultivated tools.18 The use of CIH has grown in the VA over the past decade. According to a 2011 report commissioned by the VA Field Advisory Committee on CIH, about 9 in 10 (89 ± 2%) VA facilities provide CIH therapies or refer patients to licensed practitioners.29 Primary findings also provided effect sizes which suggest the Pain Education School program had small to moderate effects in increasing active, transitional, and passive CIH utilization.
The current study has some limitations. This study used a quasi-experimental, 1-group, pre/posttest design rather than a randomized control trial with a control group. Quasi-experimental designs are viable alternatives when innovative interventions are developed, and preliminary testing is appropriate prior to further financial investment in a more definitive trial. The current study also explores the benefits of programming when based on patient self-selection which is aligned with the spirit of autonomy expected from self-management. All Veterans were referred to the program by their VA providers which neither account for a provider effect nor consider whether Veterans had engaged in other types of pain education. Changes on the outcome measure may have been impacted by these outside resources and not the programming delineated in this study. An important limitation is the use, definition, and classification of chiropractic and osteopathic manipulation as a transitional treatment. There may be differences in opinion about how these modalities were categorized separately from other CIH modalities (eg, acupuncture) on the active–transitional–passive spectrum. The current study only looked at self-reported use before and upon completion of the pain education program. Thus, the study only investigates the time period in-between these 2 time points. Future studies may want to explore additional follow-up points. The CIH preferences of all Veterans with chronic, noncancer pain may differ as the current sample was predominately African American, had a large sample of females, and did not include a sample of the 17 to 24 years of age-group when compared to the typical U.S. Veteran profile.30
Conclusion
The results of the current study substantiate past research findings which indicate increased use of CIH modalities when additional education is provided about their availability.28 The current study further confirmed that there was a shift away from passive to more transitional and active CIH modalities upon completion of the pain education program. Thus, the program was found to be more aligned with the goal of pain management—that patients engage in more self-management. These findings should be considered when making decisions about resource allocations in the VA toward CIH. It may also be astute to consider different messages and interventions when dealing with Veterans of differing age-groups.
Acknowledgments
The authors thank all the Veterans and providers who made this research possible. The authors would also like to thank the Anesthesiology/Pain Clinic Department, Jesse Brown VA Medical Center, for their vision and ongoing support of the “Pain Education School” program.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Turk D, Wilson H, Cahana A. Treatment of chronic non-cancer pain. Lancet. 2011;377: 2226–2235. [DOI] [PubMed] [Google Scholar]
- 2.Loranger L. Good practice: active vs. passive treatments. Physiotherapy Alberta News. https://www.physiotherapyalberta.ca/physiotherapists/news/good_practice_active_vs._passive_treatments?page=12. Published 2015. Accessed November 4, 2015.
- 3.Arnstein P. Clinical Coach for Effective Pain Management. Philadelphia, PA: F. A. Davis Company, 2010. [Google Scholar]
- 4.Anderson B. Randomized clinical trial comparing active versus passive approaches to the treatment of recurrent and chronic low back pain [Dissertation]. Coral Gables, FL: University of Miami, 2005. [Google Scholar]
- 5.Mannion A, Muntener M, Taimela S, Dvorak J. A randomized clinical trial of three active therapies for chronic low back pain. Spine. 1999;24:2435–2448. [DOI] [PubMed] [Google Scholar]
- 6.van Tulder M, Ostelo R, Vlaeyen J, Linton S, Morley S, Assendelft W. Behavioral treatment for chronic low back pain: a systematic review within the framework of the Cochrane Back Review Group. Spine. 2000;25:2688–2699. [DOI] [PubMed] [Google Scholar]
- 7.Aktivortho. Solutions-Passive vs. Active Therapy. http://www.aktivortho.com/solution-passive-active-therapy.asp. Accessed November 4, 2015.
- 8.van Tulder M, Koes B, Bouter L. Conservative treatment of acute and chronic nonspecific low back pain: a systematic review of randomized controlled trials of the most common interventions. Spine. 1997;22:2128–2156. [DOI] [PubMed] [Google Scholar]
- 9.Aure O, Nilsen J, Vasseljen O. Manual therapy and exercise therapy in patients with chronic low back pain: a randomized, controlled trial with 1-year follow-up. Spine. 2003;28:525–531. [DOI] [PubMed] [Google Scholar]
- 10.Haas M, Groupp E, Kraemer D. Dose-response for chiropractic care of chronic low back pain. Spine. 2004;4:574–583. [DOI] [PubMed] [Google Scholar]
- 11.Accident Compensation Corporation. The New Zealand Acute Low Back Pain Guide and Assessing Yellow Flags in Acute Low Back Pain: Risk Factors for Long-term Disability and Work Loss. Wellington, New Zealand: New Zealand Guideline Group, 2003. [Google Scholar]
- 12.Reitman C, Esses S. Conservative options in the management of spinal disorders, Part I. Bed rest, mechanical, and energy-transfer therapies. Am J Orthop. 1995;24:109–116. [PubMed] [Google Scholar]
- 13.Moskowitz M, Golden M. Neuroplastix: change the brain; relieve the pain; transform the person. http://www.neuroplastix.com/styled-6/styled-7/introduction.html. Published 2015. Accessed November 4, 2015.
- 14.Flor H, Braun C, Elbert T, Birbaumer N. Extensive reorganization of primary somatosensory cortex in chronic back pain patients. Neurosci Lett. 1997;224:5–8. [DOI] [PubMed] [Google Scholar]
- 15.Bode G. Chiropractic … Active vs. passive care it makes all the difference in the world. http://bodechiropractic.blogspot.com/2010/11/chiropractic-active-vs-passive-care-it.html. Published 2010. Accessed November 4, 2015.
- 16.National Center for Complementary and Integrative Health. Chronic pain: in depth. https://nccih.nih.gov/health/pain/chronic.htm#hed. Published 2018. Accessed February 14, 2018.
- 17.Keller A, Hayden J, Bombardier C, van Tulder M. Effect sizes of non-surgical treatments of non-specific low-back pain. Eur Spine J. 2007;16:1776–1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kralik D, Koch T, Price K, Howard N. Chronic illness self-management: taking action to create order. J Clin Nurs. 2004;13:259–267. [DOI] [PubMed] [Google Scholar]
- 19.Cosio D, Lin E. Using patient pain education to increase complementary & alternative treatment utilization in U.S. Veterans with chronic, non-cancer pain. Complement Ther Med. 2015;23:413–422. [DOI] [PubMed] [Google Scholar]
- 20.Kinsinger L, Lewis S, Strickland R. VA National Center for Health Promotion and Disease Prevention. Put prevention into VA practice: a step-by-step guide to successful program implementation. http://www.prevention.va.gov/PreventionLeaderResources/StepByStepManual.pdf. Published 2004. Accessed January 23, 2012.
- 21.Ferrell B, Rhiner M, Ferrell B. Development and implementation of a pain education program. Cancer. 1993;72:3426–3432. [DOI] [PubMed] [Google Scholar]
- 22.Cosio D, Hugo E, Roberts S, Schaefer D. A pain education school for Veterans with chronic non-cancer pain: putting prevention into VA practice. Fed Pract. 2012;29:23–29. [Google Scholar]
- 23.Cosio D, Lin E. Effects of a pain education program for Veterans with chronic, non-cancer pain: a pilot study. J Pain Palliat Care Pharmacother. 2013;27:340–349. [DOI] [PubMed] [Google Scholar]
- 24.Simmons E, Cosio D, Lin E. Using audience response systems to enhance chronic, non-cancer pain knowledge acquisition among Veterans. Telemed e-Health. 2015;21:557–563. [DOI] [PubMed] [Google Scholar]
- 25.California Health Interview Survey.. Complementary and Alternative Medicine Questionnaire: A CHIS 2001 Follow-back Study. Oakland, CA: The Regents of the University of California, 2003. [Google Scholar]
- 26.Blankers M, Koeter M, Schippers G. Missing data approaches in eHealth research: simulation study and a tutorial for non-mathematically inclined researchers. J Med Internet Res. 2010;12:e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Streiner D, Geddes J. Intention to treat analysis in clinical trials when there are missing data. Evid Based Mental Health. 2001;4:70–71. [DOI] [PubMed] [Google Scholar]
- 28.Dupont W, Plummer W. PS: Power and sample size calculation version 3.0. http://biostat.mc.vanderbilt.edu/wiki/Main/PowerSampleSize. Published 2009. Accessed March 12, 2013.
- 29.VHA Complementary and Integrative Health Services (formerly CIH). Healthcare Analysis & Information Group (HAIG). Washington, DC. http://vaww.va.gov/HAIG/haig_pubs3_CIH.asp. Published 2015. Accessed May 3, 2016.
- 30.American Community Survey: Profile of Veterans. Data from the American Community Survey. National Center for Veterans Analysis and Statistics. http://www.va.gov/vetdata/docs/SpecialReports/ProfileofVeterans2009FINAL.pdf. Published 2009. Accessed February 23, 2012.