Abstract
Vitamin D deficiency is currently a worldwide epidemic. Middle Eastern countries, including Saudi Arabia, have high vitamin D deficiency prevalence, most prominently among women, despite their plentiful year-round sunshine. Previous research investigating vitamin D status among Saudi women of reproductive age (15-49 years) is scarce, and no study has used a nationally representative sample, so this review quantified overall hypovitaminosis D prevalence among women in Saudi Arabia and explored the associated risk factors. The Web of Science, Scopus, and Medline databases were searched for prior studies in Saudi Arabia exploring vitamin D status among women of reproductive age, published between January 1, 2000 and May 25, 2017. Data were extracted from the identified studies, and a random effects model meta-analysis established the overall hypovitaminosis D prevalence. The initial search yielded 223 possibly relevant articles; 13 were confirmed as eligible, with samples totaling 2877 women aged between 15 and 49 years. Meta-analysis revealed a mean serum 25-hydroxyvitamin D, 25(OH)D, level of 13.1 ng/mL (95% confidence interval [CI]: 11.6-14.6) and an overall prevalence of hypovitaminosis D, defined as 25(OH)D < 30 ng/mL, of 77.4% (95% CI: 63.2-87.3), mostly due to insufficient sunlight exposure and low dietary vitamin D intake. There is therefore a need for a national strategy to raise vitamin D levels among women in Saudi Arabia by advising them on natural vitamin D sources, and recommending the timing and duration of sun exposure, while also defining a national approach to vitamin D fortification and supplementation.
Keywords: Hypovitaminosis D, meta-analysis, women of reproductive age, Saudi Arabia
Introduction
Over the past decade, vitamin D has attracted and maintained higher levels of interest than any other micronutrients among researchers in the health and biomedicine fields.1,2 There is consensus that it has a key role in bone mineralization, as well as in other human metabolic processes, including calcium (Ca) and phosphate homeostasis, and in skeletal growth.3 Furthermore, considerable recent epidemiological research has identified associations between low levels of vitamin D and various chronic non-skeletal diseases such as diabetes mellitus, cardiovascular diseases, autoimmune diseases, and cancers of the lung, breast, and colon.4 All these diseases are significant global public health problems.
Vitamin D is a fat-soluble prohormone which the body receives either via dietary sources or through synthesis in the skin prompted by exposure to ultraviolet B (UVB) radiation.5 The two key forms of vitamin D are vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol),6 both of which can be obtained in dietary form; however, only vitamin D3 can be synthesized in human skin after receiving UVB radiation from sunlight.7 The human body converts vitamin D into 25-hydroxy vitamin D, 25(OH)D, which is the main form of vitamin D in storage and circulation, and then into 1,25-dihydroxy vitamin D, the active form, via enzymes present in the liver and kidney.5
Vitamin D deficiency is globally widespread and is now thought to have reached epidemic level, affecting more than one billion people worldwide.8,9 In regions enjoying almost year-round sunshine, such as the Middle East, it might be anticipated that the vitamin D levels of most of the population would be sufficient.10 However, the high availability of sunlight in the Middle East apparently does not adequately protect the population against vitamin D deficiency, as endemic vitamin D deficiency has been found there,11 most prominently among women of varying age ranges.12 The population of the Kingdom of Saudi Arabia, which forms part of the Middle Eastern region, is thus subject to widespread vitamin D deficiency even though it enjoys year-round sunshine.1
The prior studies investigating vitamin D status among women of reproductive age (range: 15-49 years) in Saudi Arabia have been very limited, and to date, none of them have studied a sample which can be regarded as nationally or geographically representative. The objectives of the present paper are therefore to review the previous studies which have explored the prevalence of hypovitaminosis D among women in Saudi Arabia of reproductive age, and to combine their results to form an overall estimation of prevalence of hypovitaminosis D using meta-analysis techniques. This research also presents a discussion of the risk factors which have previously associated with hypovitaminosis D among women in Saudi Arabia of reproductive age.
Methods
The present review identified the prior research on the vitamin D status of women of reproductive age (aged between 15 and 49 years) in the context of Saudi Arabia by deploying a set protocol for its search, selection, and data extraction processes.
Search strategy and study selection
A search of the literature was performed in the Web of Science, Scopus, and Medline (via PubMed) databases, each of which were searched for the terms: “hypovitaminosis D or vitamin D or 25-hydroxyvitamin D” and “Saudi.” In instances where a study seemed to be potentially relevant because it contained data on vitamin D status in the context of Saudi Arabia, its full text was retrieved. The obtained articles’ reference lists were then checked to find further potentially relevant studies.
Studies were deemed eligible for inclusion in the present review if they met the following a priori criteria: (1) original research which aimed to examine hypovitaminosis D prevalence and/or associated factors, (2) a well-defined sample of female research subjects aged between 15 and 49 years, (3) only healthy, non-pregnant women were included, (4) data on serum concentrations of 25(OH)D, (5) published in English between January 1, 2000 and May 25, 2017 (the date of the final search), and (6) they were conducted in the Kingdom of Saudi Arabia.
Articles were excluded if they estimated vitamin D status (e.g. by using self-reported dietary intake data). They were also deemed ineligible if they did not recruit their sample from the general population (ie, if they focused on participants with conditions that may influence vitamin D metabolism, such as an obese population group or those with autoimmune diseases). Finally, studies which had previously only been published in abstract form were also excluded.
Data extraction and analysis
Following the search for relevant articles, data extraction was performed on the final sample of eligible published studies using a pre-set data extraction form to gather the following information: the reference (including the first author’s surname, the journal title, and the year of publication), the study’s context and data collection location, the study’s design and population, the sample selection method, the total number of participants, the outcome type, the statistical analysis method(s), the reported prevalence of hypovitaminosis D and the age group (in years) to which this result related, the factors found to be statistically significantly associated with hypovitaminosis D in the statistical model’s results, and the measure of those associations, and any other factors evaluated by the study which were not found to have a statistically significant association with hypovitaminosis D. To ensure consistency, all 25(OH)D values were presented as ng/mL using the conversion factor (1 ng/mL = 2.496 nmol/L) as necessary, and hypovitaminosis D (or vitamin D insufficiency) was defined as 25(OH)D levels below 30 ng/mL, a definition which has been widely used in related studies as the cut-off point for hypovitaminosis D.1
The present study presents the results of the data extraction in two tables (arranged alphabetically by the surname of the first author of each study), the first showing the research reporting hypovitaminosis D prevalence among women of reproductive age in the context of Saudi Arabia (Table 1), and the second showing the identified research investigating the factors influencing hypovitaminosis D among this population group (Table 2). A forest plot was generated using the Comprehensive Meta-Analysis (CMA) software version 3.0.
Table 1.
Studies reporting hypovitaminosis D prevalence among women of reproductive age in Saudi Arabia.
| Study | Design | Duration of recruitment | Setting/location | Age (years) |
Participants (n) | Serum 25(OH)D (ng/mL) |
Cut-off value (ng/mL) | Prevalence (%) |
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||||||
| Abdelkarem et al13 | Cross-sectional | November, 2013 to June, 2014 | Aljouf University, Sakaka | 20.71 (0.17) | 147 | Not mentioned | Insufficiency (20-29) | 27.3 |
| Deficiency (< 20) | 17.4 | |||||||
| Al Asoom14 | Cross-sectional | April to October, 2015 | University of Dammam, Dammam | 20.8 (2.4) | 87 | 15.2 (7.2) | Not mentioned | Not mentioned |
| Al-Daghri et al15 | Cross-sectional | Not mentioned | Primary health care centers, Riyadh | 32.2 (0.6) | 316 | 13.8 (0.5) | Insufficiency (10-20) | 23.6 |
| Deficiency (< 10) | 25.9 | |||||||
| Al-Daghri et al16 | Cross-sectional | February to October, 2013 | Multiple schools, Riyadh | 36.7 (0.37) | 462 | 15.9 (0.6) | Insufficiency (10-20) | 38.0 |
| Deficiency (< 10) | 36.8 | |||||||
| Al-Elq17 | Cross-sectional | Academic year, 2009-2010 | King Faisal University, Dammam | 19.4 (1.6) | 178 | 6.4 (3.3) | Insufficiency (20-30) | 4.7 |
| Deficiency (< 20) | 95.4 | |||||||
| Al-Mogbel18 | Cross-sectional | January to April, 2011 | Primary health care centers, Riyadh | 28.6 (6.6) | 465 | 7.3 (3.3) | Insufficiency (10-30) | 20.9 |
| Deficiency (< 10) | 79.1 | |||||||
| Al-Turki et al19 | Cross-sectional | February to May, 2008 | King Fahd University Hospital, Al-Kobar | 25-35a | 100 | Not mentioned | Insufficiency (21-29) | 19 |
| Deficiency (≤ 20) | 11 | |||||||
| Ali et al20 | Cross-sectional | September, 2011 to January, 2012 | University of Dammam, Dammam | 20.5 (1.9) | 96 | Not mentioned | Insufficiency (20-30) | 31 |
| Deficiency (< 20) | 28 | |||||||
| Alsuwaida et al21 | Cross-sectional | March to May, 2008 | 2 large commercial malls, Riyadh | ≥ 18 | 243 | 25.1 (12.6) | Insufficiency (20-30) | 24.7 |
| Deficiency (< 20) | 41.2 | |||||||
| Alzaheb and Al-Amer22 | Cross-sectional | May, 2016 | University of Tabuk, Tabuk | 19-25a | 180 | Not mentioned | Insufficiency (20-30) | 12.8 |
| Deficiency (< 20) | 16.1 | |||||||
| Severe deficiency (< 10) | 51.7 | |||||||
| Ardawi et al23 | Cross-sectional | June, 2008 to June, 2009 | Primary health care centers, Jeddah | 39.73 (7.8) | 501 | 17.2 (12.2) | Insufficiency (≥ 20-≤ 30) | 11.2 |
| Mild deficiency (≥ 10-< 20) | 34.1 | |||||||
| Moderate deficiency (5-10) | 38.3 | |||||||
| Severe deficiency (< 5) | 5.8 | |||||||
| Elsammak et al24 | Cross-sectional | December, 2008 to March, 2009 | King Fahd hospital, Dammam | 31.0 (7.2) | 52 | 9.9 (4.5) | Insufficiency (5-39) | Not mentioned |
| Deficiency (0-5) | ||||||||
| Elshafie et al25 | Cross-sectional | December, 2010 to January, 2011 | Primary health care centers, Riyadh | 30.6 (6.8) | 50 | 8.5 (3.9) | Deficiency (< 20) | 98.0 |
25(OH)D, 25-hydroxyvitamin D.
Range.
Table 2.
Factors associated by previous studies with hypovitaminosis D among women of reproductive age in Saudi Arabia.
| References | Factors |
|---|---|
| Al-Daghr et al15 | Frequency of consumption of dairy products. |
| Al-Mogbel18 | Younger women (< 29 years), single participants, working participants, higher levels of education, lower consumption of milk, and cod liver oil and multivitamin supplementation. |
| Alzaheb and Al-Amer22 | Urban residence, rare sun exposure, and insufficient vitamin D intake. |
Results
A total of 223 citations were retrieved following the initial search of databases, and finally, 13 of them had eligibility to be included in current review and meta-analysis (Figure 1).13–25
Figure 1.
Flow diagram of the selection process used in the review.
The 13 studies identified by the present review are outlined in Table 1.13–25 As the table shows, all 13 studies adopted a cross-sectional approach, and they provided data on a total of 2877 females of childbearing age (between 15 and 49 years old). The smallest study had a sample of 50 participants,25 while the largest used 501 participants.23 Five of the 13 research studies were performed in Riyadh (the Central Region, which includes the capital of Saudi Arabia),15,16,18,21 four were carried out in Dammam (the Eastern Region),14,17,20,24 and one study each was done in Al-Kobar (the Eastern Region),19 Jeddah (the Western Region),23 Tabuk (the North-Western Region),22 and Sakaka (the Northern Region).13
Prevalence of hypovitaminosis D
Table 1 summarizes the articles which were included in this review having reported on hypovitaminosis D prevalence in a sample of women of reproductive age in a Saudi Arabian context. However, it is important to note that none of them used a sample which could be considered to be nationally or geographically representative, nor did they use an agreed cut-off when defining hypovitaminosis D: eight of the studies defined hypovitaminosis D as 25(OH)D <30 ng/mL,13,17–23 two defined it as 25(OH)D ≤20 ng/mL,15,16 and the remaining study defined it as 25(OH)D <39 ng/mL.24
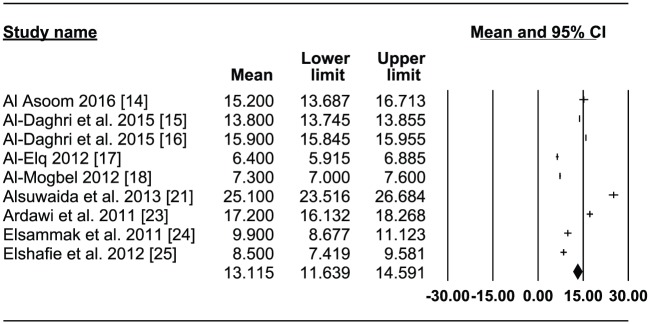
Nine of the 13 papers reported data on average vitamin D serum levels.14–18,21,23–25 These studies provided mean values in a range from 6.417to 25.1 ng/mL21 (Table 1). A forest plot was produced by this review which demonstrated that the 25(OH)D serum levels of the studies’ participants was 13.1 ng/mL (95% confidence interval [CI]: 11.6-14.6) using the random-effect model (Figure 2). This estimate was generated from the data in these nine studies,14–18,21,23–25 with a combined sample size of 2354 participants.
Figure 2.
Forest Plot of the average concentration of 25(OH)-vitamin D among women of reproductive age in Saudi Arabia.
Significant variations are evident across the prevalence of vitamin D insufficiency/deficiency reported by 11 of the 13 studies included in this review,13,15–23,25 ranging from a low of 30%19 to a peak of 100%17,18 (Table 1). The resulting forest plot shows an overall hypovitaminosis D prevalence across the samples of 77.4% (95% CI: 63.2-87.3) based on the random-effect model (Figure 3). This figure was calculated using the data reported by the eight studies that defined hypovitaminosis D as 25(OH)D < 30 ng/mL13,17–23; in total, their samples added up to 1910 participants.
Figure 3.
Forest Plot of hypovitaminosis D prevalence, defined as 25(OH)D < 30 ng/mL, among women of reproductive age in Saudi Arabia.
Risk factors for hypovitaminosis D
Only 3 of the 13 studies included in this review investigated the possible risk factors linked with hypovitaminosis D among women in their reproductive years in Saudi Arabia. These three studies employed different statistical methods to identify potentially statistically significant associations between their participants’ vitamin D levels and possible variables: the most recent study used a logistic regression analysis22; a previous study employed a Pearson correlation and linear regression analysis (adjusting for age and body mass index [BMI]),15 while the earliest of the three employed a chi-squared test.18
Table 2 displays the factors among this population group found to be associated with hypovitaminosis D by the three studies: the frequency of consumption of dairy products15; younger women (< 29 years), single participants, working participants, higher levels of education, low consumption of milk, and cod liver oil and multivitamin supplementation18; and urban residence, rare sun exposure, and insufficient vitamin D intake.22
Discussion
To the best of the author’s knowledge, this review is the first to have evaluated the hypovitaminosis D prevalence reported across previous studies’ samples of women of reproductive age in Saudi Arabia, and to fully explore all the risk factors associated with hypovitaminosis D among this population group. The review’s assessment of the prevalence of, and factors associated with, hypovitaminosis D was carried out to generate data which can be used to determine how best to promote healthy vitamin D levels among Saudi Arabian women in their reproductive years.
Prevalence of hypovitaminosis D
The present study’s first objectives were to review the prior research in Saudi Arabia investigating hypovitaminosis D prevalence among women aged between 15 and 49 years, and to combine the results of that review with an overall estimation of prevalence in the country using meta-analysis techniques. This was worthwhile because it allows a greater level of precision than was possible for the previous individual studies, since none of them employed a large, nationally representative sample of Saudi Arabian females aged between 15 and 49 years.
The present study’s meta-analysis found that the average 25(OH)D serum level of the total of 2354 female subjects of the papers in the review was 13.1 ng/mL (95% CI: 11.6-14.6), an average significantly below the optimal level which is generally considered as between 20 and 100 ng/mL.26 Similarly, low 25(OH)D levels have also been found by researchers studying Middle Eastern and North African women, including in Saudi Arabia.11,27,28 For example, a recent literature review by Hwalla et al27 reported that low serum 25(OH)D levels are a common issue among women in their childbearing years in the Middle Eastern region. The authors found that Middle Eastern women of childbearing age had vitamin D levels far lower than those considered healthy; more specifically, the mean serum 25(OH)D reported among a sample of Emirati women aged 20.8 ± 4.0 years was 8.4 ± 6.0 ng/mL29; further, a level of 14.7 ± 5.9 was found among Egyptian women aged 30.5 ± 5.8 years30; and the highest level (which, however, was still inadequate) was found among a sample of Lebanese women aged 40.4 ± 11.0 years, with a mean of 15.8 ± 8.2.31
The meta-analysis performed on the data drawn from the included studies (the samples of which totaled 1910 participants) also revealed that the overall hypovitaminosis D prevalence among Saudi women in their childbearing years was 77.4% (95% CI: 63.2-87.3). This supports the results of another recent meta-analysis on the prevalence of vitamin D deficiency in Saudi Arabia, which examined different populations (ie, adults, children and adolescents, newborns and pregnant/lactating women), and which found an overall prevalence of 81.0% (95% CI: 68.0-90.0).1 In 1983, Sedrani et al32 were the first to present data on vitamin D deficiency in Saudi Arabia, among a sample of apparently healthy male students studying at King Saud University (KSU) in Riyadh, Saudi Arabia. Other research studies utilizing various healthy subpopulations have since been published, most of which have studied women of child-bearing age.1,33 The research carried out to date in Saudi Arabia has reported levels of vitamin D deficiency ranging from one in five Saudis to almost 100%.33 The widespread vitamin D deficiency reported in Saudi Arabia has also been observed in nearby Gulf countries and other Middle Eastern states.27,28,34 Indeed, it appears that despite the plentiful sunshine enjoyed by the region, Middle Eastern inhabitants generally have a high prevalence of hypovitaminosis D.28,34 For instance, a meta-analysis by Badawi et al35 concluded that 90.4% of the Qatari population have a low vitamin D status (95% CI: 90.1-91.0; range 83%-91%).
Risk factors for hypovitaminosis D
Fortunately, an individual’s vitamin D status can be improved, so accurate identification of the factors directly associated with vitamin D status is vital.36 The second objective of the present review was therefore to explore the factors potentially associated with low vitamin D levels among Saudi women of reproductive age.
The research to date in Saudi Arabia examining the vitamin D status of women in this age group has been very limited, and those studies which have done so have generally not attempted to identify the factors potentially contributing to the noticeably high prevalence of vitamin D deficiency and insufficiency among women in Saudi Arabia, which are likely to feature various socio-demographic and lifestyle factors including their dietary intakes. The high hypovitaminosis D prevalence observed among the samples of Saudi women by the present review is suggested to result mainly from the influence of two groups of factors: limited exposure to direct sunlight and insufficient vitamin D in dietary intakes.
It has been established that humans’ main vitamin D source is through exposure of the skin to sunlight,6 as vitamin D can be created in skin which has received direct sunlight.37 This means that ensuring that individuals receive sufficient exposure to sunlight is key to preventing vitamin D deficiency,38 and that any obstruction to the direct exposure of the skin to the sun will reduce a person’s level of vitamin D synthesis.39 Sunshine is plentiful in all Arab countries (including Saudi Arabia) throughout the year; however, women in Arab countries are reported to generally suffer from vitamin D deficiency, which can be explained by their insufficient levels of skin exposure to sunlight.40 The authors of one prior study in this review identified a positive association between the 25(OH)D concentration of individuals and their level of sunlight exposure.22 The results from this study are in line with those of previous research in Saudi Arabia,41–43 and in other countries in the Middle East44–47 in demonstrating that women whose skin rarely receives exposure to the sun had a significantly higher vitamin D deficiency prevalence than women whose skin was frequently exposed to the sun. A possible reason for this is that Middle Eastern women generally dress conservatively, covering up most of their skin while outside including their limbs, head, and often their face and hands.40,44,48 A few prior studies have investigated the influence of clothing style on vitamin D status.49–53 For example, a paper with a multinational sample of women of childbearing age living in the United Arab Emirates found variations in the mean serum 25(OH)D between different nationality groups: 8.6 ng/mL among Emiratis, 12.6 ng/mL among non-Gulf Arabs, and 64.3 ng/mL among Europeans, and identified the wearing of a veil an independent predictor of hypovitaminosis D.53 Aside from the conservative clothing generally worn in Arab countries, attitudes to sun exposure and sun protection may also contribute to the high prevalence of vitamin D deficiency among women living in these countries.48 As Saudi Arabia is a very hot and sunny country where temperatures can reach dangerous levels of over 50 °C,32 Saudi people often avoid being outdoors during the day, meaning that the evening is a better time for them to attempt to achieve sensible levels of sun exposure.41 It is therefore important that Saudi women are informed of why sun exposure is beneficial to their health, and advised on how this can be achieved while also minimizing the skin cancer risk connected to sun exposure.
Although there is no doubt that sunlight is a key contributor to an individual’s vitamin D level, their dietary intake can also provide vitamin D, which is important when exposure to sunlight is limited for any reason.54,55 However, this can be problematic due to the small number of vitamin D food sources; only some oily fish, fish liver oils, and egg yolk contain vitamin D.55,56 A few prior research studies in Saudi Arabia have explored the influence of dietary intake on vitamin D status. One study included in this review found a significant association between the inadequate dietary intakes of vitamin D among a group of healthy female students aged between 19 and 25 years and their low mean vitamin D status.22 This finding supported those of prior studies in the contexts of Saudi Arabia25,43 and the wider Middle Eastern region.57–59 The dietary intake of vitamin D by women in Saudi Arabia was also discovered to be significantly lower than the recommended level.60 For instance, recent research carried out in Saudi Arabia by Al-Faris41 found that only 8.1% of pregnant women reported an adequate vitamin D intake. This was to be expected, since the limited number of foods naturally rich in vitamin D, such as fatty fish (salmon, sardines, and tuna) and their oils, are not very popular in Saudi Arabia18; a recent study by Al-Mogbel,18 in which the author employed a sample of 353 Saudi women aged between 19 and 40 years, confirmed that the majority of the participants (61%) rarely or never consumed seafood. Similarly, a study in Kuwait, one of Saudi Arabia’s neighbors, also found that most (in this case, 69%) of the young women in its sample ate fatty fish less than three times per week.61 Furthermore, research in Jordan (another Middle Eastern country) established that 75% of the sampled Jordanian women never ate fresh fish or sardines, or did so rarely.62
Furthermore, even when an individual follows a varied and balanced diet, it can be difficult for them to reach the recommended vitamin D levels, which is why the fortification of selected foods with vitamin D (eg, mainly milk and margarine) has become an acceptable strategy by which to boost the general population’s vitamin D status both in many European countries and in the USA.55,63 Vitamin D food fortification is not mandatory at present in Saudi Arabia, or in many other Middle Eastern countries.59 Sadat-Ali et al64 researched the fortification levels of some food products being sold at Saudi Arabian markets, and found that those most commonly consumed by the Saudi population, which claim to be fortified with vitamin D, were either not fortified at all, or contained small amounts of vitamin D which fell short of US market guidelines. Furthermore, previous research has linked inadequate food product fortification to low vitamin D status even in developed nations’ populations, although the estimation of the minimum vitamin D level required for healthy living (and, hence, the required level of fortification) is still at the active research stage.65 Considering the apparently high prevalence of vitamin D deficiency among the Saudi population, and their low vitamin D intake as documented by previous studies, there is a clear need for a national strategy to improve food fortification in order to combat the high prevalence of hypovitaminosis D in the country.64
The studies included in this review also examined other risk factors and groups which they associated with hypovitaminosis D: urban residence, younger women, women with higher levels of education, women in employment, unmarried women, and women who rarely used supplements. Among them, a recent article associated urban residence with a 6.5-fold increase in hypovitaminosis D risk among a sample of healthy female students aged between 19 and 25 years, because of the limited exposure of their skin to sunlight due to spending most of their time indoors.22 This finding agrees with those presented by prior studies in Saudi Arabia,43 as well as in other Middle Eastern countries,44,45,66 which also concluded that vitamin D levels are noticeably lower among samples of urban residents than among women who live rurally or in semi-urban areas. Another study included in the present review also found a significantly higher prevalence of vitamin D deficiency among women who were younger, more highly educated, and not in employment compared to their older, less educated, and employed peers.18 The author ventured the explanation that most women with higher levels of education work indoors, which means that they are likely to receive lower amounts of sun exposure and to have less healthy diets (eg, they consume more fast food) than housewives, who are likely to have more free time which will allow them to enjoy more sun exposure and healthier diets. Another Saudi study later supported these findings by reporting that younger and more educated women had a higher prevalence of vitamin D deficiency than older and less educated women.41 Furthermore, inadequate dietary vitamin D supplementation has been identified as an additional risk factor influencing low levels of vitamin D.18 The consumption of vitamin D supplements is not common among Saudi women,67 and no recommendations have been issued on vitamin D supplementation by the Saudi Ministry of Health (MOH), meaning that vitamin D supplementation has been left to individual health institutions, and therefore varies across them.68,69 Since dietary intake is not generally a rich source of vitamin D with the exceptions of the foods mentioned above, high-quality, cheap and more widely available vitamin D supplements are required for the benefit of the wider population.70
The findings of this review should be considered in the light of a few potential limitations. The first and primary one is the relatively small number of eligible studies which were included in the review. Second, the review combines data from prior research employing various definitions of hypovitaminosis D, and these variations may result in the over- or underestimation of hypovitaminosis D prevalence among women of reproductive age in Saudi Arabia. Third, 9 of the 13 papers reported data on average vitamin D serum levels, but the other four did not. Fourth, some of the studies included in the analysis deployed convenience sampling, which may mean that they contained potential bias because this method cannot guarantee that all individuals who are potentially eligible for the study within a population have an equal chance of being chosen for the sample. Fifth, the information validity of many of the reviewed studies may be questioned with regard to their reported variables because they display a high risk of measurement error and recall bias. Finally, all the studies included in this review had cross-sectional research designs, so no conclusions concerning causal relationships between hypovitaminosis D and the risk factors identified by the studies could be drawn.
Conclusion
This review is the first to have explored hypovitaminosis D prevalence and its risk factors among women of reproductive age in Saudi Arabia. Although Saudi Arabia has a very hot climate with plentiful sunshine which should, theoretically, enable its inhabitants to enjoy year-round vitamin D synthesis, the present review has shown that the reality is that Saudi women of reproductive age have low mean levels of vitamin D and a high prevalence of hypovitaminosis D. Previous researchers in the country have largely explained these findings with reference to inadequate skin exposure to sunlight, and low levels of vitamin D in dietary intakes. It is therefore clear that a strategy is required to raise the vitamin D status of women in Saudi Arabia via education on how to boost their awareness of natural sources of vitamin D, and of the duration and recommended timing of the sun exposure they need. Furthermore, a national approach to encourage vitamin D fortification and supplementation across the country would also be beneficial.
Supplemental Material
Supplemental material, prisma_2009_checklist_ for The Prevalence of Hypovitaminosis D and Its Associated Risk Factors Among Women of Reproductive Age in Saudi Arabia: A Systematic Review and Meta-Analysis by Riyadh A Alzaheb in Clinical Medicine Insights: Women’s Health
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: RAA performed the literature search, and wrote and revised the manuscript.
References
- 1. Al-Daghri NM. Vitamin D in Saudi Arabia: prevalence, distribution and disease associations. J Steroid Biochem Mol Biol. 2018;175:102–107. [DOI] [PubMed] [Google Scholar]
- 2. Alkerwi A, Sauvageot N, Gilson G, Stranges S. Prevalence and correlates of vitamin D deficiency and insufficiency in Luxembourg adults: evidence from the observation of cardiovascular risk factors (ORISCAV-LUX) study. Nutrients. 2015;7:6780–6796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Palacios C. The role of nutrients in bone health, from A to Z. Crit Rev Food Sci Nutr. 2006;46:621–628. [DOI] [PubMed] [Google Scholar]
- 4. Rabenberg M, Scheidt-Nave C, Busch MA, Rieckmann N, Hintzpeter B, Mensink GB. Vitamin D status among adults in Germany—results from the German health interview and examination survey for adults (DEGS1). BMC Public Health. 2015;15:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Christakos S, Ajibade DV, Dhawan P, Fechner AJ, Mady LJ. Vitamin D: metabolism. Endocrinol Metab Clin North Am. 2010;39:243–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–281. [DOI] [PubMed] [Google Scholar]
- 7. Hart G, Furniss J, Laurie D, Durham SK. Measurement of vitamin D status: background, clinical use, and methodologies. Clin Lab. 2006;52:335–343. [PubMed] [Google Scholar]
- 8. Lehmann B, Meurer M. Vitamin D metabolism. Dermatol Ther. 2010;23:2–12. [DOI] [PubMed] [Google Scholar]
- 9. Holick MF, Chen TC. Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr. 2008;87:1080S–1086S. [DOI] [PubMed] [Google Scholar]
- 10. Al Turki YA. Vitamin D deficiency health population overview. Saudi J Sports Med. 2014;14:74–76. [Google Scholar]
- 11. Al-Mohaimeed A, Khan NZ, Naeem Z, Al-Mogbel E. Vitamin D status among women in Middle East. J Health Sci. 2012;2:49–56. [Google Scholar]
- 12. Maalouf G, Gannage-Yared MH, Ezzedine J, et al. Middle East and North Africa consensus on osteoporosis. J Musculoskelet Neuronal Interact. 2007;7:131–143. [PubMed] [Google Scholar]
- 13. Abdelkarem HM, El-Sherif MA, Gomaa SB. Vitamin D status and insulin resistance among young obese Saudi females. Saudi Med J. 2016;37:561–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Al Asoom LI. The association of adiposity indices and plasma vitamin D in young females in Saudi Arabia. Int J Endocrinol. 2016;2016:1215362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Al-Daghri NM, Aljohani N, Al-Attas OS, et al. Dairy products consumption and serum 25-hydroxyvitamin D level in Saudi children and adults. Int J Clin Exp Pathol. 2015;8:8480–8486. [PMC free article] [PubMed] [Google Scholar]
- 16. Al-Daghri NM, Al-Saleh Y, Aljohani N, et al. Vitamin D deficiency and cardiometabolic risks: a juxtaposition of Arab adolescents and adults. PLoS ONE. 2015;17: e0131315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Al-Elq AH. The status of vitamin D in medical students in the preclerkship years of a Saudi medical school. J Family Community Med. 2012;19:100–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Al-Mogbel ES. Vitamin D status among adult Saudi Females visiting primary health care clinics. Int J Health Sci. 2012;6:116–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Al-Turki H, Sadat-Ali M, Al-Elq A, Al-Mulhim FA, Al-Ali AK. 25-hydoxyvitamin D levels among healthy Saudi Arabian women. Saudi Med J. 2008;29:1765–1768. [PubMed] [Google Scholar]
- 20. Ali A, Amin L, Al-Ali A. Vitamin D level among female students in College of Nursing in Saudi Arabia and its relation to students’ symptoms. J Am Sci. 2012;8:132–138. [Google Scholar]
- 21. Alsuwaida AO, Farag YM, Al Sayyari AA, et al. Prevalence of vitamin D deficiency in Saudi adults. Saudi Med J. 2013;34:814–818. [PubMed] [Google Scholar]
- 22. Alzaheb RA, Al-Amer O. Prevalence and predictors of hypovitaminosis d among female university students in Tabuk, Saudi Arabia. Clin Med Insights Womens Health. 2017;10:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ardawi MS, Qari MH, Rouzi AA, Maimani AA, Raddadi RM. Vitamin D status in relation to obesity, bone mineral density, bone turnover markers and vitamin D receptor genotypes in healthy Saudi pre- and postmenopausal women. Osteoporos Int. 2011;22:463–475. [DOI] [PubMed] [Google Scholar]
- 24. Elsammak MY, Al-Wossaibi AA, Al-Howeish A, Alsaeed J. High prevalence of vitamin D deficiency in the sunny Eastern region of Saudi Arabia: a hospital-based study. East Mediterr Health J. 2011;17:317–322. [PubMed] [Google Scholar]
- 25. Elshafie DE, Al-Khashan HI, Mishriky AM. Comparison of vitamin D deficiency in Saudi married couples. Eur J Clin Nutr. 2012;66:742–745. [DOI] [PubMed] [Google Scholar]
- 26. Yüksel RN, Altunsoy N, Tikir B, et al. Correlation between total vitamin D levels and psychotic psychopathology in patients with schizophrenia: therapeutic implications for add-on vitamin D augmentation. Ther Adv Psychopharmacol. 2014;4:268–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hwalla N, Al Dhaheri AS, Radwan H, et al. The prevalence of micronutrient deficiencies and inadequacies in the Middle East and approaches to interventions. Nutrients. 2017;9: E229.28273802 [Google Scholar]
- 28. Bassil D, Rahme M, Hoteit M, Fuleihan Gel-H. Hypovitaminosis D in the Middle East and North Africa: prevalence, risk factors and impact on outcomes. Dermatoendocrinol. 2013;5:274–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Al Anouti F, Thomas J, Abdel-Wareth L, Rajah J, Grant WB, Haq A. Vitamin D deficiency and sun avoidance among university students at Abu Dhabi, United Arab Emirates. Dermatoendocrinol. 2011;3:235–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. El-Sagheer GM, Soliman E, Abdulla AM, et al. Vitamin D deficiency and pseudofractures in child-bearing Egyptian women: successful medical treatment helps to avoid fractures and surgical interference. Open J Endocr Metab Dis. 2016;6:183–191. [Google Scholar]
- 31. Gannage-Yared MH, Helou E, Zaraket V, et al. Serum 25 hydroxyvitamin D in employees of a Middle Eastern university hospital. J Endocrinol Invest. 2014;37:541–546. [DOI] [PubMed] [Google Scholar]
- 32. Sedrani SH, Elidrissy AW, El Arabi KM. Sunlight and vitamin D status in normal Saudi subjects. Am J Clin Nutr. 1983;38:129–132. [DOI] [PubMed] [Google Scholar]
- 33. Alshahrani F, Aljohani N. Vitamin D: deficiency, sufficiency and toxicity. Nutrients. 2013;5:3605–3616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Arabi A, El Rassi R, El-Hajj Fuleihan G. Hypovitaminosis D in developing countries-prevalence, risk factors and outcomes. Nat Rev Endocrinol. 2010;6:550–561. [DOI] [PubMed] [Google Scholar]
- 35. Badawi A, Arora P, Sadoun E, et al. Prevalence of vitamin D insufficiency in Qatar: a systematic review. J Public Health Res. 2012;1:229–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Dawodu A, Akinbi H. Vitamin D nutrition in pregnancy: current opinion. Int J Womens Health. 2013;5:333–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Nair R, Maseeh A. Vitamin D: the “sunshine” vitamin. J Pharmacol Pharmacother. 2012;3:118–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Song SJ, Zhou L, Si S, et al. The high prevalence of vitamin D deficiency and its related maternal factors in pregnant women in Beijing. PLoS ONE. 2013;8: e85081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Levy MA, McKinnon T, Barker T, et al. Predictors of vitamin D status in subjects that consume a vitamin D supplement. Eur J Clin Nutr. 2015;69:84–89. [DOI] [PubMed] [Google Scholar]
- 40. Muhairi SJ, Mehairi AE, Khouri AA, et al. Vitamin D deficiency among healthy adolescents in Al Ain, United Arab Emirates. BMC Public Health. 2013;13:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Al-Faris NA. High prevalence of vitamin D deficiency among pregnant Saudi women. Nutrients. 2016;8:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ardawi MS, Sibiany AM, Bakhsh TM, Qari MH, Maimani AA. High prevalence of vitamin D deficiency among healthy Saudi Arabian men: relationship to bone mineral density, parathyroid hormone, bone turnover markers, and lifestyle factors. Osteoporos Int. 2012;23:675–686. [DOI] [PubMed] [Google Scholar]
- 43. Naeem Z, AlMohaimeed A, Sharaf FK, Ismail H, Shaukat F, Bazmi Inam SN. Vitamin D status among population of Qassim Region, Saudi Arabia. Int J Health Sci (Qassim). 2011;5:116–124. [PMC free article] [PubMed] [Google Scholar]
- 44. Nichols EK, Khatib IM, Aburto NJ, et al. Vitamin D status and determinants of deficiency among non-pregnant Jordanian women of reproductive age. Eur J Clin Nutr. 2012;66:751–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Batieha A, Khader Y, Jaddou H, et al. Vitamin D status in Jordan: dress style and gender discrepancies. Ann Nutr Metab. 2011;58:10–18. [DOI] [PubMed] [Google Scholar]
- 46. Bener A, Al-Ali M, Hoffmann GF. Vitamin D deficiency in healthy children in a sunny country: associated factors. Int J Food Sci Nutr. 2009;60:60–70. [DOI] [PubMed] [Google Scholar]
- 47. El-Hajj Fuleihan G, Nabulsi M, Choucair M, et al. Hypovitaminosis D in healthy schoolchildren. Pediatrics. 2001;107: E53. [DOI] [PubMed] [Google Scholar]
- 48. Golbahar J, Al-Saffar N, Altayab DD, Al-Othman S, Darwish A, Al-Kafaji G. Predictors of vitamin D deficiency and insufficiency in adult Bahrainis: a cross-sectional study. Public Health Nutr. 2013;7:732–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hatun S, Islam O, Cizmecioglu F, et al. Subclinical vitamin D deficiency is increased in adolescent girls who wear concealing clothing. J Nutr. 2005;135:218–222. [DOI] [PubMed] [Google Scholar]
- 50. Hashemipour S, Larijani B, Adibi H, et al. Vitamin D deficiency and causative factors in the population of Tehran. BMC Public Health. 2004;4:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Guzel R, Kozanoglu E, Guler-Uysal F, Soyupak S, Sarpel T. Vitamin D status and bone mineral density of veiled and unveiled Turkish women. J Womens Health Gend Based Med. 2001;10:765–770. [DOI] [PubMed] [Google Scholar]
- 52. ElSonbaty R, Abdul-Ghaffar NU. Vitamin D deficiency in veiled Kuwaiti women. Eur J Clin Nutr. 1996;50:315–318. [PubMed] [Google Scholar]
- 53. Dawodu A, Absood G, Patel M, et al. Biosocial factors affecting vitamin D status of women of childbearing age in the United Arab Emirates. J Biosoc Sci. 1998;30:431–437. [DOI] [PubMed] [Google Scholar]
- 54. Desai NS, Tukvadze N, Frediani JK, et al. Effects of sunlight and diet on vitamin D status of pulmonary tuberculosis patients in Tbilisi, Georgia. Nutrition. 2012;28:362–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Spiro A, Buttriss JL. Vitamin D: an overview of vitamin D status and intake in Europe. Nutr Bull. 2014;39:322–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Yoo K, Cho J, Ly S. Vitamin D intake and serum 25-hydroxyvitamin D levels in Korean adults: analysis of the 2009 Korea National Health and Nutrition Examination Survey (KNHANES IV-3) using a newly established vitamin D database. Nutrients. 2016;8: E610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Allali F, El Aichaoui S, Khazani H, et al. High prevalence of hypovitaminosis D in Morocco: relationship to lifestyle, physical performance, bone markers, and bone mineral density. Semin Arthritis Rheum. 2009;38:444–451. [DOI] [PubMed] [Google Scholar]
- 58. Dawodu A, Kochiyil J, Altaye N. Pilot study of sunlight exposure and vitamin D status in Arab women of childbearing age. East Mediterr Health J. 2011;17:570–574. [PubMed] [Google Scholar]
- 59. Saadi HF, Nagelkerke N, Benedict S, et al. Predictors and relationships of serum 25 hydroxyvitamin D concentration with bone turnover markers, bone mineral density, and vitamin D receptor genotype in Emirati women. Bone. 2006;39:1136–1143. [DOI] [PubMed] [Google Scholar]
- 60. Ross AC, Manson JE, Abrams SA, et al. The 2011 report on dietary reference intakes for calcium and vitamin d from the institute of medicine: what clinicians need to know. J Clin Endocrinol Metab. 2011;96:53–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Alyahya K, Lee WT, Al Mazidi Z, Morgan J, Lanham-New S. Risk factors of low vitamin D status in adolescent females in Kuwait: implications for high peak bone mass attainment. Arch Osteoporos. 2014;9:178. [DOI] [PubMed] [Google Scholar]
- 62. Gharaibeh MA, Stoecker BJ. Assessment of serum 25(OH)D concentration in women of childbearing age and their preschool children in Northern Jordan during summer. Eur J Clin Nutr. 2009;63:1320–1326. [DOI] [PubMed] [Google Scholar]
- 63. Jäpelt RB, Jakobsen J. Vitamin D in plants: a review of occurrence, analysis, and biosynthesis. Front Plant Sci. 2013;4:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Sadat-Ali M, Al Elq A, Al Farhan M, Sadat NA. Fortification with vitamin D: comparative study in the Saudi Arabian and US markets. J Family Community Med. 2013;20:49–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. de Lourdes Samaniego-Vaesken M, Alonso-Aperte E, Varela-Moreiras G. Vitamin food fortification today. Food Nutr Res. 2012;56:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Maddah M, Sharami SH, Neyestani TR. Vitamin D insufficiency among postmenopausal women in urban and rural areas in Guilan, Northern Iran. J Nutr Elder. 2009;28:386–393. [DOI] [PubMed] [Google Scholar]
- 67. Tuffaha M, El Bcheraoui C, Daoud F, et al. Deficiencies under plenty of sun: vitamin D status among adults in the kingdom of Saudi Arabia, 2013. N Am J Med Sci. 2015;7:467–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Alfaleh KM, Al-Manie AM, Al-Mahmoud HF, et al. Prevalence of vitamin D deficiency in Saudi newborns at a tertiary care center. Saudi Med J. 2014;35:178–182. [PubMed] [Google Scholar]
- 69. Babli AI, AlDawood KM, Khamis AH. Knowledge, attitude, and practice of general practitioners in Dammam, Saudi Arabia towards Vitamin D supplementation to infants. J Family Community Med. 2015;22:135–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Haq A, Wimalawansa SJ, Pludowski P, Anouti FA. Clinical practice guidelines for vitamin D in the United Arab Emirates. J Steroid Biochem Mol Biol. 2018;175:4–11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, prisma_2009_checklist_ for The Prevalence of Hypovitaminosis D and Its Associated Risk Factors Among Women of Reproductive Age in Saudi Arabia: A Systematic Review and Meta-Analysis by Riyadh A Alzaheb in Clinical Medicine Insights: Women’s Health