Abstract
Background
The use of iodine-based contrast agents entails the risk of contrast induced nephropathy (CIN). Radiocontrast agents elicit the third most common cause of nephropathy among hospitalized patients, accounting for 11–12% of cases. CIN is connected with clinically significant consequences, including increased morbidity, prolonged hospitalization, increased risk of complications, potential need for dialysis, and increased mortality rate. The number of in-hospital examinations using iodine-based contrast media has been significantly increasing over the last decade. In order to protect patients from possible complications of such examinations, new biomarkers are needed that are able to predict a risk of contrast-induced nephropathy. Urinary and plasma cyclic guanosine monophosphate (cGMP) concentrations are influenced by renal function. Urinary cGMP is primarily of renal cellular origin. Therefore, we assessed if urinary cGMP concentration may predict major adverse renal events (MARE) after contrast media exposure during coronary angiography.
Methods
Urine samples were prospectively collected from non-randomized consecutive patients with either diabetes or preexisting impaired kidney function receiving intra-arterial contrast medium (CM) for emergent or elective coronary angiography at the Charité Campus Mitte, University Hospital Berlin. Urinary cGMP concentration in spot urine was analyzed 24 hours after CM exposure. Patients were followed up over 90 days for occurrence of death, initiation of dialysis, doubling of plasma creatinine concentration or MARE.
Results
In total, 289 consecutive patients were included into the study. Urine cGMP/creatinine ratio 24 hours before CM exposure expressed as mean±SD was predictive for the need of dialysis (no dialysis: 89.77±92.85 μM/mM, n = 277; need for dialysis: 140.3±82.90 μM/mM, n = 12, p = 0.008), death (no death during follow-up: 90.60±92.50 μM/mM, n = 280; death during follow-up: 169.88±81.52 μM/mM, n = 9; p = 0.002), and the composite endpoint MARE (no MARE: 86.02±93.17 μM/mM, n = 271; MARE: 146.64±74.68 μM/mM, n = 18, p<0.001) during the follow-up of 90 days after contrast media application. cGMP/creatinine ratio stayed significantly increased at values exceeding 120 μM/mM in patients who developed MARE, required dialysis or died.
Conclusions
Urinary cGMP/creatinine ratio ≥ 120 μM/mM before CM exposure is a promising biomarker for the need of dialysis and all-cause mortality 90 days after CM exposure in patients with preexisting renal impairment or diabetes.
Introduction
Iodinated radiographic contrast media can cause kidney dysfunction, particularly in patients with preexisting renal impairment and/or diabetes. This dysfunction may lead to additional kidney injury, a so-called contrast induced acute kidney injury (AKI) defined as an acute impairment of renal function and manifested by an absolute increase of serum creatinine of at least 0.5 mg/dL or by a relative increase by at least 25% from baseline levels [1]. Peak creatinine typically occurs 3–5 days after contrast media administration and returned to baseline (or a new baseline) within 1–3 weeks [2]. Contrast-induced AKI is associated with an increase in both short- and long-term morbidity and mortality, increased hospital length of stay, and greater health care costs [3].
Diabetes and chronic renal dysfunction are independent factors for the development of coronary artery disease. Percutaneous coronary interventions (PCI) became a routine procedure, and they are performed more and more frequently in patients with significant co-morbidities such as chronic kidney disease (CKD) and/or diabetes. In addition, patients with CKD and/or diabetes have an increased mortality after PCI with or without stenting [4]. Therefore, there is a high need to identify biomarkers associated with subsequent life-threatening complications after CM application.
Mechanisms underlying contrast media nephrotoxicity are multifactorial, including renal ischemia, particularly in the renal medulla, the formation of reactive oxygen species (ROS), reduction of nitric oxide (NO) production, and tubular epithelial and vascular endothelial injury [5]. NO and atrial natriuretic peptide (ANP) induce vascular relaxation by increasing the production of cGMP, an important mediator of vascular tone. Although NO generation in the kidney is essential for preservation of renal perfusion and function, high levels of NO secondary to an increase in iNOS activity may inhibit eNOS activity, resulting in renal vasoconstriction and decreased GFR [6]. Fractional urine excretion of ANP [7] is increased in patients with chronic renal failure and is significantly correlated with creatinine clearance [8–13]. cGMP is produced by particulate (pGC) and soluble (sGC) guanylyl cyclases, as a result of natriuretic peptide and NO activation [14]. Although both sGC and pGC activation increase cGMP intracellular concentration, pGC activation (unlike sGC) results also in significant release of cGMP into the extracellular space and blood circulation [15–19]. Therefore, while both sGC and pGC increase cGMP within cells, the resulting biological actions are quite different. Due to in part different localizations of sGC and pGC receptors, and timing of their signaling in the kidney, the NP/pGC/cGMP pathway predominantly regulates GFR and sodium excretion whereas the NO/sGC/cGMP pathway mostly controls renal vascular tone[20, 21]. Urinary and plasma cGMP concentrations are influenced by renal function [19, 22]. Urinary cGMP is primarily of renal cellular origin [17]. A positive correlation between increased cGMP in plasma and cGMP in urine was shown previously [23], therefore it was suggested as biomarker candidate for kidney injury. Furthermore, in contrast to plasma cGMP, urinary cGMP is not related to the severity of heart failure as assessed clinically according to the NYHA classification[19]. Thus, the goal of our study was to evaluate the predictive value of urinary cGMP clearance 24 hrs prior to contrast medium application for the development of adverse events in patients at risk for contrast-induced kidney injury.
Methods
2.1 Study design
A prospective cohort of 289 consecutive patients underwent coronary angiography between January 2010 and December 2011 in the Department of Cardiology of the [13]Charité –Universitätsmedizin Berlin [24, 25]. This study was approved by the institutional review board and by the Ethics Commission of the Charité –Universitätsmedizin Berlin. Prior to enrollment into the study, each participant of the study has signed an informed consent form, which was approved by the Ethics Commission of the Charité –Universitätsmedizin Berlin. The study was conducted according to the Declaration of Helsinki, the European Guidelines on Good Clinical Practice and relevant national and regional authority requirements.
2.1.1 Inclusion criteria
Consecutive patients with plasma creatinine of at least 1.1 mg/dL or preexisting diabetes mellitus were considered as potential study participants.
Consecutive patients with a high risk of developing contrast induced renal failure, i.e. patients with plasma creatinine levels of at least 1.1 mg/dL but not requiring dialysis or patients with preexisting diabetes mellitus independently of plasma creatinine levels, were enrolled into the study. Inclusion criteria were based on Mehran contrast nephropathy risk score[26].
2.1.2 Exclusion criteria
Patients with end-stage renal disease as well as patients who were not able or refused to sign an informed consent were not included.
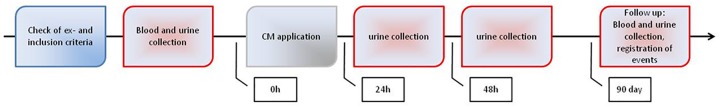
2.2 Course of the study (Fig 1)
Fig 1. Flow chart for sample collection.
All study participants underwent blood and urine sampling 24 hrs prior to coronary angiography with water-soluble, non-ionic, monomeric, low-osmolar, iodine-based contrast agent Iobitridol at a concentration of 350 mg Iod/mL (XENETIX® 350, Guerbet GmbH, Sulzbach/Taunus, Germany). Further, blood and urine samples were obtained 24 and 48 hrs after contrast agent application and 90 days after angiography [24].
2.3 Sample handling and biomarker measurement
Blood samples were centrifuged for 5 min at 3.000 rpm and the resulting plasma was immediately frozen at -80°C. Creatinine was measured according to the Jaffé method. Glomerular filtration rate (GFR) was estimated according to the modification of diet in renal disease (MDRD) formula (eGFR = 175 x (SCr)-1.154 x (age)-0.203 x 0.742 [if female])[27]. cGMP concentrations were measured using a commercially available radioimmunoassay kit (IBL, Hamburg, Germany) as previously described [28].
2.4 Study endpoints (Table 1)
Table 1. Overview of study endpoints.
| Endpoints | N | % |
|---|---|---|
| Death | 9 | 3.1 |
| Dialysis | 12 | 4.1 |
| Doubling of serum creatinine | 1 | 0.3 |
| MARE | 18 | 6.2 |
N—number of patients, %—percentage of the patients in total study cohort, MARE—major adverse renal event
Study endpoints included death, initiation of dialysis, doubling of plasma creatinine concentration during the 90 days follow-up or major adverse renal events (MARE). MARE was defined as an occurrence of death, initiation of dialysis or doubling of the creatinine concentration within 90 days after the procedure. A predictive value for the risk to develop one of the endpoints was assessed based on urinary cGMP/creatinine ratios 24 hrs prior to contrast medium application. Additionally, urinary cGMP/creatinine ratios were calculated for 24 and 48 hrs after CM exposure. According to National Kidney Foundation–Kidney Disease Outcomes Quality Initiative (NKF-KDOQI) guideline, the definition of chronic kidney disease is a GFR below 60 ml/min/1,73 m2 for three months or more or a GFR above 60 ml/min/1,73 m2 with kidney damage marked by high levels of albumin in urine[29].
2.5 Statistical analysis
The statistical analysis was performed using SPSS 20 (IBM® SPSS® Statistics IBM Cooperation, Armonk, USA). Shapiro–Wilk test was used evaluate the distribution of the data. The predictive value of urinary cGMP/creatinine ratios as a biomarker of death or MARE was assessed by receiver operating characteristic (ROC) analysis.
Mean levels of urinary cGMP/creatinine ratios at different time points were compared using t-tests. Cumulative MARE rates were compared using a χ2 tests with risk ratios (with 95% confidence intervals). For all analyzes a two-sided t-test was used. P of less than 0.05 was considered statistically significant.
Results
3.1 Patients characteristics
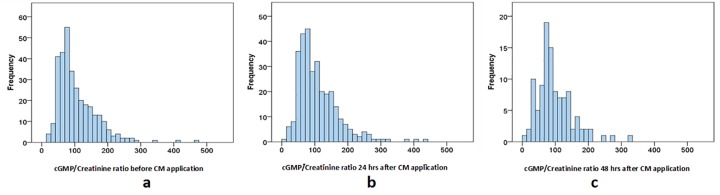
The study cohort included 289 consecutive patients who underwent coronary angiography (254 (77.0%) male and 76 (23.0%) female) with mean age of 68.91 ± 9.75 years and a body mass index (BMI) of 28.99 ± 5.57 kg/m2. Baseline creatinine was 1.24 ± 0.46 mg/dL, which corresponded to baseline GFR of 64.77 ± 21.73 ml/min/1.73m2. 156 patients (54.0%) patients were previously diagnosed with diabetes mellitus, 76 (26.3%) suffered from congestive heart failure and 74 (25.6%) had anemia. Anemia was diagnosed according to the definition of the World Health Organization: baseline hematocrit value <39% for men and <36% for women[30]. Most of the patients were treated with angiotensin-converting-enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs), in combination with diuretics and/or statins. ACE inhibitors, ARBs and diuretics are known for causing an acute kidney injury (AKI) in CKD patients, therefor they were stopped in patients that developed AKI. None of the patients from our cohort used of nitroglycerin or natriuretic peptides in order to avoid possible effect of these agents on urinary cGMP excretion. Mean volume of injected contrast medium was 113.35 ± 55.02 mL (Table 2). Urinary cGMP/creatinine ratios in our patient cohort were normally distributed at each follow-up time point (Fig 2).
Table 2. Baseline characteristics of the cohort.
| Patients characteristics | |
|---|---|
| Female N (%)/Male N (%) | 76 (23.0)/254 (77.0) |
| Age, years (Median ± SD) | 68.91 ± 9.75 |
| Body mass index, kg/m2 (Median ± SD) | 28.99 ±5.57 |
| CM-volume, ml (Median ± SD) | 113.35 ± 55.02 |
| Baseline creatinine, mg/dl (Median ± SD) | 1.24 ± 0.46 |
| Baseline GFR, ml/min/1.73m2 (Median ± SD) | 64.77 ± 21.73 |
| Diabetes mellitus N (%) | 156 (54.0) |
| Congestive heart failure N (%) | 76 (26.3) |
| Anemia N (%) | 74 (25.6) |
| Hypertension N (%) | 257 (88.9) |
| Intake of N (%): | |
| - ACE inhibitors | 161 (55.7) |
| - ARB | 98 (33.9) |
| - Diuretics | 185 (64.0) |
| - Statins | 182 (63.0) |
N—number of patients, %—percentage of the patients in the study cohort, CM—contrast media, GFR—glomerular filtration rate according to the MDRD formula, SD—standard deviation; ACE—angiotensin converting enzyme, ARB—angiotensin II receptor blocker
Fig 2.
Histogram of cGMP/Creatinine ratio (μM/mM) (a) before, (b) 24h after and (c) 48h after CM application. cGMP: urinary cyclic guanosine monophosphate.
3.2 Correlation between cGMP and the study endpoints
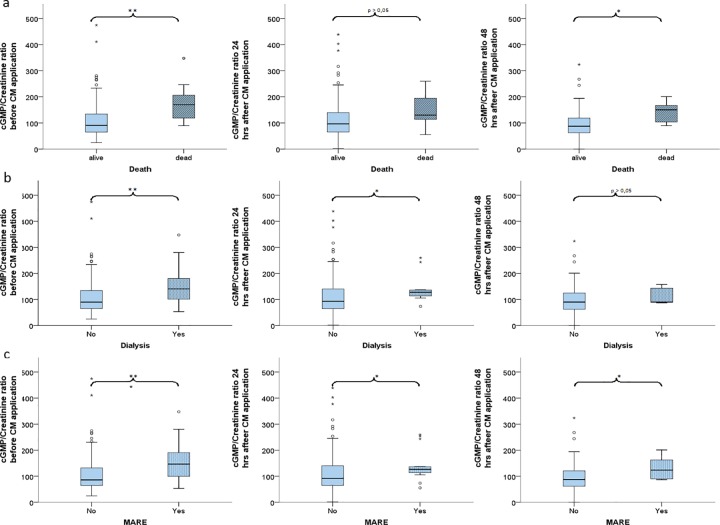
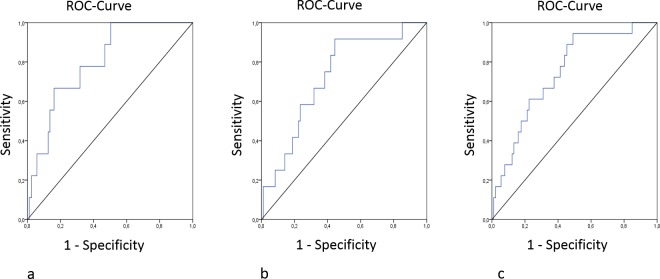
Nine patients died during the follow-up time of 90 days. The average death occurred at 74.5 days (95% CI 7–95) after study entry. Causes of death included cardiovascular diseases in 4 patients, infections in 2 patients, respiratory failure in 1 patient and unknown reasons in 2 patients. Urinary cGMP/creatinine ratios were significantly lower before CM injection in survivors (90.60±92.50 μM/mM) compared with deceased patients (169.88±81.52 μM/mM, n = 9; p = 0.002). This difference remained significant at 48 hours after CM application (87.44±54.23 vs.150.23±41.26 μM/mM, p = 0.014) (Table 3, Fig 3A). ROC analysis confirmed that increased urinary cGMP/creatinine ratiois a significant predictor of death during 90 days after CM application in patients with plasma creatinine of at least 1.1 mg/dl or preexisting diabetes mellitus (Fig 4A).
Table 3. Ratios of urinary cGMP and creatinine (in μM/mM) before, 24 hours after and 48h after contrast media application.
| cGMP/Cr before CM | cGMP/Cr 24 hours after CM | cGMP/Cr 48 hours after CM | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | M ± SD | p | N | M ± SD | p | N | M ± SD | p | ||
| MARE | No | 271 | 86.02 ± 93.17 | <0.001 | 250 | 92.01 ± 62.29 | 0.014 | 85 | 87.44 ± 54.86 | 0.039 |
| Yes | 18 | 146.64 ± 74.68 | 16 | 126.45 ± 59.67 | 8 | 123.37 ± 43.38 | ||||
| Dialysis | No | 277 | 89.77 ± 92.85 | 0.008 | 255 | 93.71 ± 62.48 | 0.028 | 88 | 89.88 ± 55.55 | 0.323 |
| Yes | 12 | 140.30 ± 82.90 | 11 | 127.50 ± 57.14 | 5 | 89.74 ± 34.22 | ||||
| Death | No | 280 | 90.60 ± 92.50 | 0.002 | 258 | 96.81 ± 62.00 | 0.069 | 87 | 87.44 ± 54.23 | 0.014 |
| Yes | 9 | 169.88 ± 81.52 | 8 | 129.91 ± 71.19 | 6 | 150.23 ± 41.26 | ||||
cGMP—urinary cyclic guanosine monophosphate, Cr—urinary creatinine, MARE—major adverse renal event; N—number of patients, M—median, SD—standard deviation, p—significance according to MANOVA, p<0.05 is statistically significant.
Fig 3.
Distribution of urinary cGMP/creatinine ratios (μM/mM) before 24 hours after and 48h after contrast media application detected in patients without (No) or with (Yes) following adverse events: death(a), dialysis (b) or MARE (c). cGMP: urinary cyclic guanosine monophosphate, MARE: major adverse renal event, *** p<0.001, ** p<0.01, * p<0.05.
Fig 4.
ROC-curves of the cGMP/Creatinine ratio before CM application for (a) death, (b) dialysis and (c) MARE.
12 patients in our cohort needed dialysis during the follow-up period. cGMP/creatinine ratios in urine 24 hrs before CM injection were significantly higher in those patients (140.3±82.90 vs. 89.77±92.85 μM/mM, p = 0.008). This difference remained significant 24 hrs after CM application (127.50±57.14 vs. 93.71±62.48 μM/mM, p = 0.028) (Table 3, Fig 3B). ROC analysis showed that increased urinary cGMP/creatinine ratios are predictive for dialysis following CM application in patients with creatinine concentration of at least 1.1 mg/dL or preexisting diabetes mellitus (Fig 4B).
MAREs were detected in 18 patients of our study population and were characterized by significantly higher levels of urinary cGMP/creatinine ratio 24 hrs prior to CM exposure (146.64±74.68 vs. 86.02±93.17 μM/mM, p<0.001). This difference remained significant at 24 hrs (126.45±59.67 vs. 92.01±62.29 μM/mM, p = 0.014) and 48 hrs after coronary angiography (123.37±43.38 vs. 87.44±54.86 μM/mM, p = 0.039) (Table 3, Fig 3C). ROC curve demonstrated that an increase in urine cGMP/creatinine ratio strongly predicted the risk of MARE following CM application in patients with creatinine of at least 1.1 mg/dL or preexisting diabetes mellitus (Fig 4C). Multivariate logistic regression analysis confirmed that urinary cGMP/creatinine ratios ≥ 120 μM/mM before CM application are a significant predictor of MARE (Table 4).
Table 4. Multivariate logistic regression analysis for predictors of MARE.
| Variables | B | S.E. | Wald | P | Exp(B) | 95% C.I. for EXP(B) | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Age | 0.014 | 0.030 | 0.218 | 0.640 | 1.014 | 0.957 | 1.075 |
| Diabetes mellitus | -0.508 | 0.591 | 0.740 | 0.390 | 0.602 | 0.189 | 1.915 |
| Chronic Kidney Disease | -1.250 | 0.961 | 1.692 | 0.193 | 0.286 | 0.044 | 1.884 |
| Anemia | 1.488 | 0.556 | 7.169 | 0.007 | 4.427 | 1.490 | 13.154 |
| Congestive heart failure | 0.939 | 0.549 | 2.923 | 0.087 | 2.557 | 0.872 | 7.499 |
| Contrast volume | -0.014 | 0.404 | 0.001 | 0.973 | 0.986 | 0.447 | 2.175 |
|
Urinary cGMP/creatinine ratio ≥ 120 μM/mM before CM application |
1.173 | 0.559 | 4.410 | 0.036 | 3.233 | 1.081 | 9.666 |
cGMP: urinary cyclic guanosine monophosphate, uCr: urinary creatinine, MARE: major adverse renal event, Exp(B): Odds Ratio, p<0.05 –is statistically significant.
In analogy to cGMP/Cr ration in Table 3, we calculated serum creatinine and GFR in each group divided by death, dialysis or MAREs, but did not see any statistically significant difference between the patients who developed MARE, needed dialysis or died during the follow up and those who did not (Table 5).
Table 5. GFR (in ml/min/1.73m2) before, 24 hours after and 48h after contrast media application.
| GFR before CM | GFR 24hrs after CM | GFR 48hrs after CM | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | M ± SD | p | N | M ± SD | p | N | M ± SD | p | ||
| MARE | No | 271 | 68.07 ± 30.96 | 0.14 | 250 | 72.19 ± 32.23 | 0.12 | 85 | 71.09 ± 30.03 | 0.001 |
| Yes | 18 | 62.12 ± 40.38 | 16 | 61.91 ± 50.59 | 8 | 14.04 ± 23.20 | ||||
| Dialysis | No | 277 | 68.80 ±31.72 | 0.06 | 255 | 71.35 ± 32.77 | 0.03 | 88 | 72.18 ± 30.69 | 0.003 |
| Yes | 12 | 55.85± 31.90 | 11 | 17.51 ± 39.14 | 5 | 11.27 ± 3.94 | ||||
| Death | No | 280 | 68.43 ± 32.57 | 0.09 | 258 | 71.51 ± 33.47 | 0.06 | 87 | 71.09 ± 32.29 | 0.002 |
| Yes | 9 | 63.11 ± 29.9 | 8 | 59.69 ± 46.97 | 6 | 24.04 ± 23.21 | ||||
GFR—glomerular filtration rate according to the MDRD formula, MARE—major adverse renal event; N—number of patients, M—median, SD—standard deviation, p—significance according to MANOVA, p<0.05 is statistically significant.
Discussion
To our knowledge, this is the first study demonstrating that urinary cGMP/creatinine ratio ≥ 120 μM/mM is predictive for death, the need of emergent dialysis or MARE during 90 days of follow-up in patients with high risk of developing contrast-induced renal failure after CM application for coronary angiography.
We chose 90 days follow-up because this timeframe was previously reported as critical for development of adverse events among patients with AKI [31–33]. Our results are consistent with data on increase of urinary cGMP in patients with diabetes. Comparable with our study, the authors did not find any correlation between creatinine clearance and clearance of cGMP [34].
Hypoxia is an early sign and trigger of progression of diabetic nephropathy [35]. Recent clinical data reported decreased renal oxygenation in patients with CKD. Indeed, decline in renal oxygenation precedes matrix accumulation in vivo suggesting that hypoxia may influence both initiation and promotion of fibrosis and that chronic hypoxia is a final common condition of end-stage renal disease [36]http://www.ncbi.nlm.nih.gov/pubmed/?term=Chronic+hypoxia+as+a+mechanism+of+progression+of+chronic+kidney+diseases%3A+from+hypothesis+to+novel+therapeutics. Neylon et al. showed that hypoxia increases urinary cGMP without changes in GFR and absolute sodium excretion [37]. In addition, it was previously reported that the selective activation of soluble guanylate cyclase (sGC) with subsequent rise in cGMP concentration causes potent systemic and renal vasodilating effects, unloads the heart, increases cardiac output, and preserves GFR and sodium and water excretion in experimental chronic heart failure [38].
In contrast to this data, some studies report significantly lower cGMP concentrations in urine in patients with CKD [19]. Additionally, a correlation between decline of urinary cGMP and decrease in diuresis, renal blood flow, glomerular filtration rate and fractional sodium excretion has been reported [39]. In line with our results, it was recently reported that CIN was a significant predictor of subsequent renal events after cardiac catheterization and CIN and anemia were associated with increased risk for worse long-term clinical outcome, especially when both were present [40].
Experimental inhibition and stimulation of renal cGMP was studied in a rodent model of acute and chronic renal failure. Pretreatment of animals with cGMP-specific phosphodiesterase inhibitor accelerated renal recovery after ischemia due to stimulation of regional renal blood flow [41]. Enhancement of renal cGMP levels by administration of sGC stimulator BAY 41–2272 to animals with a progressive renal fibrosis at one week after induction of anti-Thy-1-induced chronic glomerulosclerosis, significantly limited tubulointerstitial fibrosis and preserved renal function [42]. In addition, sildenafil treatment significantly increased urinary cGMP excretion in OLETF diabetic rats and attenuated diabetic nephropathy by decreasing albuminuria, attenuating glomerular hyperfiltration, decreasing glomerular hypertrophy and reducing the glomerulosclerosis score [43, 44]. Furthermore, daily administration of sildenafil initiated immediately after renal ablation resulted in stabilization of creatinine levels, prevention of hypertension, reduction in proteinuria and increase of urinary cGMP excretion in 5/6 nephrectomized rats [45].
Reports on the origin of urinary cGMP are controversial. In clearance studies in rats, urinary cGMP was primarily of renal cellular origin [46]. cGMP clearance in healthy pregnant women is increased in the setting of decreased plasma cGMP levels, indicating increased nephrogenic cGMP production [47]. Studies on 3H-labeled cGMP in dogs showed that a significant amount of urinary cGMP is derived from plasma by tubular secretion [48]. A study on renal clearances of plasma cGMP in humans using tritium-labeled cyclic nucleotides showed that plasma was the source of virtually all of the cGMP excreted with urine [49]. Jakob et al. reported that there was no significant correlation between urinary concentrations of cGMP and creatinine [19].
An increased death rate of patients with higher urinary cGMP/creatinine ratios may be at least partially explained by the fact the patients in our cohort had symptoms of coronary heart disease as an indication for coronary angiography. In patients with heart failure, cGMP concentrations in urine were significantly higher than in healthy volunteers [50]. However, according to New York Heart Association there is no relationship between cGMP concentrations in urine and severity of heart failure functional classes. In plasma, by contrast, there was a significant direct correlation between cGMP concentrations and the severity of heart failure [19]. In addition, ROC analysis showed no significant correlation between plasma cGMP and cumulative (24-month) all-cause mortality in patients with myocardial infarction [51].
In the recent systematic review and meta-analysis, Klein et al. identified the most promising biomarkers of risk for renal replacement therapy among patients with acute kidney injury. Altogether, nine urinary biomarkers were eligible for meta-analysis: NGAL, urinary interleukin 18 (IL18), Kidney injury molecule-1 (KIM-1), urinary N-acetyl-beta-d-glucosaminidase (NAG), Tissue inhibitor of metalloproteinases 2 (TIMP-2), insulin-like growth factor-binding protein-7 (IGFBP7), the fractional excretion of sodium (FeNa) T, urinary cystatin C and urinary output [52]. The authors underlined the moderate quality of the studies, small sample sizes and luck of standardization with risk of bias and confounding suggesting a need for further research in this area.
Conclusion
Urinary cGMP/creatinine ratios of more than 120 μM/mM could be a promising biomarker for prediction of death, dialysis or MARE during 90 days of follow-up in patients with impaired but remnant kidney function or diabetes after coronary angiography.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by Bayer Pharma AG, Wuppertal, Germany provided measurements of cGMP as well as salary for authors[MP, PS, AK, JPS], but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Maliborski A, Zukowski P, Nowicki G, Boguslawska R. Contrast-induced nephropathy—a review of current literature and guidelines. Med Sci Monit. 2011;17(9):RA199–204. PubMed Central PMCID: PMCPMC3560518. doi: 10.12659/MSM.881923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Malyszko J, Bachorzewska-Gajewska H, Poniatowski B, Malyszko JS, Dobrzycki S. Urinary and serum biomarkers after cardiac catheterization in diabetic patients with stable angina and without severe chronic kidney disease. Ren Fail. 2009;31(10):910–9. doi: 10.3109/08860220903216113 [DOI] [PubMed] [Google Scholar]
- 3.Au TH, Bruckner A, Mohiuddin SM, Hilleman DE. The Prevention of Contrast-Induced Nephropathy. Ann Pharmacother. 48(10):1332–42. doi: 10.1177/1060028014541996 [DOI] [PubMed] [Google Scholar]
- 4.Gami AS, Garovic VD. Contrast nephropathy after coronary angiography. Mayo Clin Proc. 2004;79(2):211–9. doi: 10.4065/79.2.211 [DOI] [PubMed] [Google Scholar]
- 5.Andreucci M, Faga T, Pisani A, Sabbatini M, Michael A. Acute Kidney Injury by Radiographic Contrast Media: Pathogenesis and Prevention. Biomed Res Int. 2014:362725 doi: 10.1155/2014/362725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bae EH, Kim IJ, Ma SK, Lee JU, Kim SW. Altered Regulation of Renal Nitric Oxide and Atrial Natriuretic Peptide Systems in Lipopolysaccharide-induced Kidney Injury. Korean J Physiol Pharmacol. 15(5):273–7. doi: 10.4196/kjpp.2011.15.5.273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ando K, Umetani N, Kurosawa T, Takeda S, Katoh Y, Marumo F. Atrial natriuretic peptide in human urine. Klin Wochenschr. 1988;66(17):768–72. [DOI] [PubMed] [Google Scholar]
- 8.Marumo F, Sakamoto H, Ando K, Ishigami T. Concentrations of atrial natriuretic peptide in plasma and urine of kidney disease patients. Clin Chem. 1990;36(9):1650–3. [PubMed] [Google Scholar]
- 9.Cannone V, Huntley BK, Olson TM, Heublein DM, Scott CG, Bailey KR, et al. Atrial natriuretic peptide genetic variant rs5065 and risk for cardiovascular disease in the general community: a 9-year follow-up study. Hypertension. 62(5):860–5. doi: 10.1161/HYPERTENSIONAHA.113.01344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glode A, Naumann J, Gnad T, Cannone V, Kilic A, Burnett JC Jr. et al. Divergent effects of a designer natriuretic peptide CD-NP in the regulation of adipose tissue and metabolism. Mol Metab. 6(3):276–87. doi: 10.1016/j.molmet.2016.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jarocka IT, Bachorzewska-Gajewska H, Kobus G, Czaban S, Malyszko J, Dobrzycki S. Renal function after percutaneous coronary interventions depending on the type of hydration. Adv Med Sci. 2013;58(2):369–75. doi: 10.2478/ams-2013-0006 [DOI] [PubMed] [Google Scholar]
- 12.Andreucci M, Faga T, Pisani A, Sabbatini M, Michael A. Acute kidney injury by radiographic contrast media: pathogenesis and prevention. Biomed Res Int. 2014;2014:362725 doi: 10.1155/2014/362725 PubMed Central PMCID: PMCPMC4150431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bae EH, Kim IJ, Ma SK, Lee JU, Kim SW. Altered Regulation of Renal Nitric Oxide and Atrial Natriuretic Peptide Systems in Lipopolysaccharide-induced Kidney Injury. Korean J Physiol Pharmacol. 2011;15(5):273–7. doi: 10.4196/kjpp.2011.15.5.273 PubMed Central PMCID: PMCPMC3222796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsai EJ, Kass DA. Cyclic GMP signaling in cardiovascular pathophysiology and therapeutics. Pharmacol Ther. 2009;122(3):216–38. doi: 10.1016/j.pharmthera.2009.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsutamoto T, Kinoshita M, Ohbayashi Y, Wada A, Maeda Y, Adachi T. Plasma arteriovenous cGMP difference as a useful indicator of nitrate tolerance in patients with heart failure. Circulation. 1994;90(2):823–9. [DOI] [PubMed] [Google Scholar]
- 16.Vorderwinkler KP, Artner-Dworzak E, Jakob G, Mair J, Diensti F, Pichler M, et al. Release of cyclic guanosine monophosphate evaluated as a diagnostic tool in cardiac diseases. Clin Chem. 1991;37(2):186–90. [PubMed] [Google Scholar]
- 17.Heim JM, Gottmann K, Weil J, Schiffl H, Lauster F, Loeschke K, et al. Effects of a small bolus dose of ANF in healthy volunteers and in patients with volume retaining disorders. Klin Wochenschr. 1990;68(14):709–17. [DOI] [PubMed] [Google Scholar]
- 18.Jakob G, Mair J, Puschendorf B. On the relation of atrial natriuretic peptide and cyclic guanosine 3',5'-monophosphate plasma concentrations during ergometric exercise in healthy individuals. Horm Metab Res. 1994;26(2):121–2. doi: 10.1055/s-2007-1000788 [DOI] [PubMed] [Google Scholar]
- 19.Jakob G, Mair J, Vorderwinkler KP, Judmaier G, Konig P, Zwierzina H, et al. Clinical significance of urinary cyclic guanosine monophosphate in diagnosis of heart failure. Clin Chem. 1994;40(1):96–100. [PubMed] [Google Scholar]
- 20.Burnett J. Modulating cGMP in heart failure. BMC Pharmacology. 2007;Volume 7(Number Suppl 1):Page S14. [Google Scholar]
- 21.Krawutschke C, Koesling D, Russwurm M. Cyclic GMP in Vascular Relaxation: Export Is of Similar Importance as Degradation. Arterioscler Thromb Vasc Biol. 35(9):2011–9. doi: 10.1161/ATVBAHA.115.306133 [DOI] [PubMed] [Google Scholar]
- 22.Mair J, Puschendorf B. Is measurement of cyclic guanosine monophosphate in plasma or urine suitable for assessing in vivo nitric oxide production? Circulation. 1998;97(12):1209–10. [DOI] [PubMed] [Google Scholar]
- 23.Heim JM, Gottmann K, Weil J, Haufe MC, Gerzer R. Is cyclic GMP a clinically useful marker for ANF action? Z Kardiol. 1988;77 Suppl 2:41–6. [PubMed] [Google Scholar]
- 24.Chaykovska L, Heunisch F, von Einem G, Alter ML, Hocher CF, Tsuprykov O, et al. Urinary Vitamin D Binding Protein and KIM-1 Are Potent New Biomarkers of Major Adverse Renal Events in Patients Undergoing Coronary Angiography. PLoS One. 11(1):e0145723 doi: 10.1371/journal.pone.0145723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heunisch F, Chaykovska L, von Einem G, Alter M, Dschietzig T, Kretschmer A, et al. ADMA predicts major adverse renal events in patients with mild renal impairment and/or diabetes mellitus undergoing coronary angiography. Medicine (Baltimore). 96(6):e6065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004;44(7):1393–9. doi: 10.1016/j.jacc.2004.06.068 [DOI] [PubMed] [Google Scholar]
- 27.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461–70. [DOI] [PubMed] [Google Scholar]
- 28.Stasch JP, Dembowsky K, Perzborn E, Stahl E, Schramm M. Cardiovascular actions of a novel NO-independent guanylyl cyclase stimulator, BAY 41–8543: in vivo studies. Br J Pharmacol. 2002;135(2):344–55. doi: 10.1038/sj.bjp.0704483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chapter 1: Definition and classification of CKD. Kidney Int Suppl (2011). 2013;3(1):19–62. doi: 10.1038/kisup.2012.64 PubMed Central PMCID: PMCPMC4089693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nutritional anaemias. Report of a WHO scientific group. World Health Organ Tech Rep Ser. 1968;405:5–37. Epub 1968/01/01. [PubMed] [Google Scholar]
- 31.Harel Z, Wald R, Bargman JM, Mamdani M, Etchells E, Garg AX, et al. Nephrologist follow-up improves all-cause mortality of severe acute kidney injury survivors. Kidney Int. 83(5):901–8. doi: 10.1038/ki.2012.451 [DOI] [PubMed] [Google Scholar]
- 32.Wald R, Shariff SZ, Adhikari NK, Bagshaw SM, Burns KE, Friedrich JO, et al. The association between renal replacement therapy modality and long-term outcomes among critically ill adults with acute kidney injury: a retrospective cohort study*. Crit Care Med. 42(4):868–77. doi: 10.1097/CCM.0000000000000042 [DOI] [PubMed] [Google Scholar]
- 33.Go AS, Parikh CR, Ikizler TA, Coca S, Siew ED, Chinchilli VM, et al. The assessment, serial evaluation, and subsequent sequelae of acute kidney injury (ASSESS-AKI) study: design and methods. BMC Nephrol. 11:22 doi: 10.1186/1471-2369-11-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Matata BM, Galinanes M. Effect of diabetes on nitric oxide metabolism during cardiac surgery. Diabetes. 2001;50(11):2603–10. [DOI] [PubMed] [Google Scholar]
- 35.Takiyama Y, Haneda M. Hypoxia in diabetic kidneys. Biomed Res Int. 2014:837421 doi: 10.1155/2014/837421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fine LG, Norman JT. Chronic hypoxia as a mechanism of progression of chronic kidney diseases: from hypothesis to novel therapeutics. Kidney Int. 2008;74(7):867–72. doi: 10.1038/ki.2008.350 [DOI] [PubMed] [Google Scholar]
- 37.Neylon M, Marshall JM, Johns EJ. The effects of chronic hypoxia on renal function in the rat. J Physiol. 1997;501(Pt 1):243–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boerrigter G, Costello-Boerrigter LC, Cataliotti A, Lapp H, Stasch JP, Burnett JC Jr. Targeting heme-oxidized soluble guanylate cyclase in experimental heart failure. Hypertension. 2007;49(5):1128–33. doi: 10.1161/HYPERTENSIONAHA.106.083832 [DOI] [PubMed] [Google Scholar]
- 39.Siragy HM, Johns RA, Peach MJ, Carey RM. Nitric oxide alters renal function and guanosine 3',5'-cyclic monophosphate. Hypertension. 1992;19(6 Pt 2):775–9. [DOI] [PubMed] [Google Scholar]
- 40.Sato A, Aonuma K, Watanabe M, Hirayama A, Tamaki N, Tsutsui H, et al. Association of contrast-induced nephropathy with risk of adverse clinical outcomes in patients with cardiac catheterization: From the CINC-J study. Int J Cardiol. 2017;227:424–9. Epub 2016/11/14. doi: 10.1016/j.ijcard.2016.11.019 [DOI] [PubMed] [Google Scholar]
- 41.Guan Z, Miller SB, Greenwald JE. Zaprinast accelerates recovery from established acute renal failure in the rat. Kidney Int. 1995;47(6):1569–75. [DOI] [PubMed] [Google Scholar]
- 42.Wang Y, Kramer S, Loof T, Martini S, Kron S, Kawachi H, et al. Enhancing cGMP in experimental progressive renal fibrosis: soluble guanylate cyclase stimulation vs. phosphodiesterase inhibition. Am J Physiol Renal Physiol. 2006;290(1):F167–76. doi: 10.1152/ajprenal.00197.2005 [DOI] [PubMed] [Google Scholar]
- 43.Kuno Y, Iyoda M, Shibata T, Hirai Y, Akizawa T. Sildenafil, a phosphodiesterase type 5 inhibitor, attenuates diabetic nephropathy in non-insulin-dependent Otsuka Long-Evans Tokushima Fatty rats. Br J Pharmacol. 162(6):1389–400. doi: 10.1111/j.1476-5381.2010.01149.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stasch JP, Schlossmann J, Hocher B. Renal effects of soluble guanylate cyclase stimulators and activators: a review of the preclinical evidence. Curr Opin Pharmacol. 21:95–104. doi: 10.1016/j.coph.2014.12.014 [DOI] [PubMed] [Google Scholar]
- 45.Rodriguez-Iturbe B, Ferrebuz A, Vanegas V, Quiroz Y, Espinoza F, Pons H, et al. Early treatment with cGMP phosphodiesterase inhibitor ameliorates progression of renal damage. Kidney Int. 2005;68(5):2131–42. doi: 10.1111/j.1523-1755.2005.00669.x [DOI] [PubMed] [Google Scholar]
- 46.Wong KR, Xie MH, Shi LB, Liu FY, Huang CL, Gardner DG, et al. Urinary cGMP as biological marker of the renal activity of atrial natriuretic factor. Am J Physiol. 1988;255(6 Pt 2):F1220–4. [DOI] [PubMed] [Google Scholar]
- 47.Chapman AB, Abraham WT, Zamudio S, Coffin C, Merouani A, Young D, et al. Temporal relationships between hormonal and hemodynamic changes in early human pregnancy. Kidney Int. 1998;54(6):2056–63. doi: 10.1046/j.1523-1755.1998.00217.x [DOI] [PubMed] [Google Scholar]
- 48.Blonde L, Wehmann RE, Steiner AL. Plasma clearance rates and renal clearance of 3H-labeled cyclic AMP and 3H-labeled cyclic GMP in the dog. J Clin Invest. 1974;53(1):163–72. doi: 10.1172/JCI107534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Broadus AE, Kaminsky NI, Hardman JG, Sutherland EW, Liddle GW. Kinetic parameters and renal clearances of plasma adenosine 3',5'-monophosphate and guanosine 3',5'-monophosphate in man. J Clin Invest. 1970;49(12):2222–36. doi: 10.1172/JCI106441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Greene SJ, Gheorghiade M, Borlaug BA, Pieske B, Vaduganathan M, Burnett JC Jr., et al. The cGMP signaling pathway as a therapeutic target in heart failure with preserved ejection fraction. J Am Heart Assoc. 2(6):e000536 doi: 10.1161/JAHA.113.000536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Richards AM, Nicholls MG, Yandle TG, Frampton C, Espiner EA, Turner JG, et al. Plasma N-terminal pro-brain natriuretic peptide and adrenomedullin: new neurohormonal predictors of left ventricular function and prognosis after myocardial infarction. Circulation. 1998;97(19):1921–9. [DOI] [PubMed] [Google Scholar]
- 52.Klein SJ, Brandtner AK, Lehner GF, Ulmer H, Bagshaw SM, Wiedermann CJ, et al. Biomarkers for prediction of renal replacement therapy in acute kidney injury: a systematic review and meta-analysis. Intensive Care Med. 2018;44(3):323–36. doi: 10.1007/s00134-018-5126-8 PubMed Central PMCID: PMCPMC5861176. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.