Abstract
Building a culture of health in hospitals means more than participating in community partnerships. It also requires an enhanced capacity to recognize and respond to disparities in utilization patterns across populations. We identified all pediatric hospitalizations at Cincinnati Children’s Hospital Medical Center, in the period 2011–16. Each hospitalized child’s address was geocoded, allowing us to calculate inpatient bed-day rates for each census tract in Hamilton County, Ohio, across all causes and for specific conditions and pediatric subspecialties. We then divided the census tracts into quintiles based on their underlying rates of child poverty and calculated bed-day rates per quintile. Poorer communities disproportionately bore the burden of pediatric hospital days. If children from all of the county’s census tracts spent the same amount of time in the hospital each year as those from the most affluent tracts, approximately twenty-two child-years of hospitalization time would be prevented. Of particular note were “hot spots” in high-poverty census tracts neighboring the hospital, where bed-day rates were more than double the county average. Hospitals that address disparities would benefit from a more comprehensive understanding of the culture of health—a culture that is more cohesive inside the hospital and builds bridges into the community.
Health varies considerably between and within communities. Across Greater Cincinnati, life expectancy differs by more than twenty years.1 Similar disparities exist around the country for many acute and chronic pediatric conditions.2–5 Certain patients and populations are more likely to experience morbidity as well as the social and financial disruptions it can cause. Hospitals often view hospitalizations with a narrow lens, focusing attention on people as they enter care without fully addressing those disruptions. This can lead to missed opportunities to identify larger patterns in how and why certain patients and populations experience excess morbidity.6,7
The Robert Wood Johnson Foundation recently formulated a vision for a “Culture of Health,”8 defined as a “national movement toward better health where individuals, communities, and organizations take action to improve health.”9 For key stakeholders, including health systems, to support this movement, disparities in health outcomes must be better understood. This would allow for the more appropriate deployment of targeted interventions in inpatient, outpatient, and community settings.8 It would also help a broader array of stakeholders understand root causes more fully and develop coordinated action steps to address them.10–12
At Cincinnati Children’s Hospital Medical Center, we recently developed a measure, the community or census tract inpatient bed-day rate, to enumerate disparities and guide ourcommunity-based improvement efforts. The rate is calculated by dividing the number of days children from a given community spend in the hospital by the number of children living within that community. This rate likely reflects the variety of underlying medical and social factors that influence child morbidity. We initially set out to use this measure to illuminate all-cause disparities within our region. We hypothesized that disparities in the rate would extend across both specific conditions and pediatric subspecialties. We also saw such data as relevant to local action. Thus, we focused additional attention on the area encircling our hospital, considering the degree to which we and our partners could promote targeted, multidisciplinary, disparity-reducing improvements inside and outside the hospital.
Study Data And Methods
We examined all hospitalizations at Cincinnati Children’s Hospital Medical Center in the period January 1, 2011–December 31, 2016, for children younger than age eighteen from Hamilton County, Ohio. Cincinnati Children’s is a 628-bed urban pediatric academic center that cares for more than 90 percent of all Hamilton County children who require hospitalization. Hamilton County, which includes Cincinnati, has approximately 190,000 children spread across 222 urban, suburban, and rural census tracts. The median child poverty rate for those tracts, according to 2011–15 data from the Census Bureau’s American Community Survey, was 23.5 percent (inter-quartile range: 9.1 percent, 44.8 percent).13
During the study period, 46,076 hospitalizations were identified, contributed by 27,770 unique children. Each child’s home address extracted from the electronic health record (EHR) was geocoded using custom software based on 2015 census TIGER/Line address range files and assigned to an associated census tract.14 We excluded hospitalizations that were connected to addresses outside Hamilton County; could not be geocoded; or matched the address of the hospital, the local Ronald McDonald House, or the local foster care system. This left a final sample of 40,482 hospitalizations contributed by 24,428 unique children.
This study was approved by the Institutional Review Board of Cincinnati Children’s Hospital Medical Center.
MEASURES
Our outcome was the inpatient bed-day rate within each census tract in Hamilton County. We defined the rate as the annual number of bed-days per 1,000 children younger than eighteen years. The numerator was derived from the number of days children from a given tract spent in the hospital; the population denominator (that is, the number of children per tract) was obtained from data for 2011–15 from the American Community Survey.13 We normalized this value by 1,000 children to make the rate easier to interpret.
We used the child poverty rate measure, chosen a priori and also available from the American Community Survey, to approximate the underlying socioeconomic makeup of a given tract.15 This measure is created by dividing the number of children (people younger than age eighteen) within a household with an aggregate income below the federal poverty level during the previous twelve months by the number of children for whom poverty status has been determined.13 We categorized tracts into quintiles according to poverty rates (low, low-medium, medium, high-medium, and high poverty). We used this categorical measure in our subsequent analyses.
These analyses included a look at inpatient bed-day rates across all conditions and across a subset of conditions, defined using International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10), codes. We drew on previous work that cited asthma, gastroenteritis, seizure or epilepsy, and appendicitis or appendectomy as common reasons for pediatric hospitalization.16 To broaden our scope, we also included, a priori, respiratory infections (bronchiolitis and pneumonia), diabetic ketoacidosis, and injury. We saw these seven conditions collectively as broadly representative of the variety of acute and chronic medical-surgical conditions present on a typical inpatient pediatric unit. Still, these conditions accounted for just 28.4 percent of all included bed-days at Cincinnati Children’s Hospital Medical Center during the study period. The remaining bed-days were linked to more than a hundred other conditions. To begin to capture additional disparities across this breadth of conditions, and to simultaneously determine whether disparities extended across pediatric subspecialties, we next identified the subspecialty team or service that managed the patient during the inpatient stay (such as hospital medicine or hospitalist service, neurology, and surgery).
To further characterize our population, we also extracted patient-level information from the EHR, including the child’s age at the time of hospitalization, sex, race, ethnicity, insurance status, and a marker of medical complexity. Age was treated as a continuous variable. Race was defined as white/Caucasian, black/African American, or other. Ethnicity was non-Hispanic or Hispanic. Insurance was defined as Medicaid/ other public or private. Within our EHR, patient complexity is estimated using the Pediatric Medical Complexity Algorithm. The algorithm uses ICD-10 codes to define patients as M1 (low complexity), M2 (medium complexity), or M3 (high complexity).17 We pulled these data to characterize our population, not to adjust for outcome assessments, given our hypothesis that such complexity may be influenced by poverty.
ANALYSES
Descriptive statistics illustrated the distribution of inpatient bed-day rates. The bivariate relationship between our continuous inpatient bed-day and census tract child poverty rate measures was assessed using a Spearman correlation coefficient. Our analyses of the inpatient bed-day rates across all causes, specified conditions, and subspecialties used quintiles (defined by census tract child poverty rates). Our primary analyses looked at differences on an absolute scale. However, given that certain conditions and subspecialties contributed a disproportionate absolute number of bed-days, we also pursued supplementary analyses to illustrate relative disparities (see the online appendix).18
Although we originally considered using a test for trend to assess for significant differences across poverty quintiles, initial analyses showed that the relationship between inpatient bed-day and poverty rates was neither linear nor monotonic. Because of this more complex relationship, we used the Kruskal-Wallis test to simplify interpretation and align with our main hypothesis—that disparities are present in the hospital setting.
LOCAL AREA ANALYSIS
We then used geographic information systems to identify bed-day “hot spots” within a two-mile radius of Cincinnati Children’s Hospital Medical Center, employing the point density function within ArcGIS, version 10.5.1. We also mapped community assets (such as schools, health centers, and pharmacies) that could serve as important partners in attempts to “cool” the hot spots through our communitywide learning network, which already includes providers of inpatient and out-patient care, community leaders, and parents.12
LIMITATIONS
This study was not without limitations. First, we used data specific to children from Hamilton County who were hospitalized at Cincinnati Children’s Hospital Medical Center. These children may differ from patients living elsewhere. Moreover, the range, distribution, and severity of the conditions that contributed to our institution’s bed-days may differ from those seen at other hospitals or health care systems.
Second, although Cincinnati Children’s Hospital Medical Center accounts for the vast majority of pediatric hospitalizations in the county, it is possible that children were hospitalized elsewhere.
Third, certain patients may be disproportionately represented in our data set as a result of multiple or prolonged hospitalizations. This could have skewed results for certain census tracts. Grouping tracts into quintiles likely diminished the impact of this limitation. That said, grouping tracts into categories places limits on our ability to capture the breadth of distributions of inpatient bed-day or poverty rates within these groupings.
Fourth, our condition- and subspecialty-level analyses may have been limited by the relative rarity of certain associated events (for example, hospitalizations for diabetic ketoacidosis or to the endocrinology service are less common than hospitalizations for asthma or to hospital medicine).
Fifth, the Kruskal-Wallis test allowed us to identify whether a disparity exists, but it could not statistically depict whether there was a “dose-response” relationship between variables of interest.
Finally, our analyses were isolated to medical-surgical reasons for hospitalization. Psychiatric hospitalizations were not included and warrant further inquiry. Similarly, our focus here was on inpatient utilization. We did not have the ability within our data to assess for disparities in the delivery of outpatient preventive services, unanticipated utilization, or access challenges.
Study Results
In our six-year study period, there were 40,482 hospitalizations, contributed by 24,428 unique children, that collectively amounted to 146,163 bed-days (exhibit 1). Of these hospitalizations, 54.6 percent involved males, and 61.0 percent involved publicly insured children. The median child age at the time of hospitalization was 4.6 years; the median length-of-stay was 1.38 days (IQR: 0.92, 2.71) (data not shown). Among hospitalized children, 35.9 percent were classified as with high medical complexity (M3) (exhibit 1), and about 54 percent of all bed days were attributed to these patients (data not shown).
EXHIBIT 1.
Characteristics of children involved in 40,482 hospitalizations in Hamilton County, Ohio, January 1, 2011–December 31, 2016, with data on the related inpatient bed-days and the county’s child population and inpatient bed-day rates
| No. or median | Percent or IQR | |
|---|---|---|
| CHILDREN | ||
|
| ||
| Male | 22,101 | 54.6 |
| Average age (years) | 4.6 | 1.3, 11.4 |
| Race | ||
| White or Caucasian | 19,218 | 47.5 |
| Black or African American | 17,709 | 43.7 |
| Other | 3,013 | 7.4 |
| Unknown or refused | 542 | 1.3 |
| Ethnicity | ||
| Non-Hispanic | 38,233 | 94.4 |
| Hispanic | 1,925 | 4.8 |
| Unknown or refused | 324 | 0.8 |
| Insurance | ||
| Medicaid/other public | 24,682 | 61.0 |
| Private | 15,800 | 39.0 |
| Medical complexity | ||
| Low | 13,929 | 34.4 |
| Medium | 7,847 | 19.4 |
| High | 14,534 | 35.9 |
| Missing | 4,172 | 10.3 |
|
| ||
| INPATIENT BED-DAYS | ||
|
| ||
| Total | 146,163 | 100.0 |
| By poverty quintile | ||
| Low | 19,628 | 13.4 |
| Low medium | 25,475 | 17.4 |
| Medium | 29,328 | 20.0 |
| High medium | 32,007 | 21.9 |
| High | 39,726 | 27.2 |
|
| ||
| COUNTY CHILD POPULATION | ||
|
| ||
| Total | 187,545 | 100.0 |
| By poverty quintile | ||
| Low | 37,322 | 19.9 |
| Low medium | 37,460 | 20.0 |
| Medium | 37,393 | 19.9 |
| High medium | 37,007 | 19.7 |
| High | 38,636 | 20.6 |
|
| ||
| COUNTY INPATIENT BED-DAY RATE (PER 1,000 CHILDREN PER YEAR) | ||
|
| ||
| All census tracts | 118.0 | 86.9, 165.0 |
| By poverty quintile | ||
| Low | 87.7 | —a |
| Low medium | 113.3 | —a |
| Medium | 130.7 | —a |
| High medium | 144.1 | —a |
| High | 171.4 | —a |
SOURCE Authors’ analysis. NOTES Medical complexity was determined using the Pediatric Medical Complexity Algorithm (see note 17 in text). The poverty rates for the quintiles are as follows: low, < 5 percent; low medium, 6–15 percent; medium, >15–27 percent; high medium, >27–45 percent; and high, >45 percent. IQR is interquartile range.
Not applicable.
The median inpatient bed-day rate across all 222 Hamilton County census tracts was 118.0 bed-days per 1,000 children per year. On a continuous scale, the rate was positively, albeit weakly, correlated with the census tract child poverty rate (r = 0.36; p < 0.001).
The all-cause inpatient bed-day rate within the low-poverty quintile of tracts was 87.7 per 1,000 children per year (exhibit 1). This rate increased across the other quintiles, to 113.3 in the low-medium, 130.7 in the medium, 144.1 in the high-medium, and 171.4 in the high-poverty quintile (p < 0.001). If all census tracts had had the same rate as the low-poverty quintile, there would have been 47,477 (32.5 percent) fewer bed days during the study period (annually, this would amount to 7,913 fewer days, or approximately 22 fewer child-years, of hospitalization time) (data not shown).
These gradients extended across multiple clinical conditions (exhibit 2). We found significant differences in numbers of bed-days between quintiles for multiple clinical conditions, including respiratory infections, asthma, and injury. Bed-days for epilepsy, gastroenteritis, appendicitis, and diabetic ketoacidosis did not differ significantly across quintiles, but ratios between the high-poverty and low-poverty tracts were always greater than 1.00. These ratios ranged from 1.30 for appendicitis to 6.77 for asthma. These relative differences are depicted in appendix exhibit 1, which shows comparisons on a transformed scale that is consistent across conditions.18 In appendix exhibit 1 the inpatient bed-day rate for each assessed condition in the high-poverty quintile was always above the mid-line (which represents the county mean), and the rate in the low-poverty quintile was always below the midline.
EXHIBIT 2. Inpatient bed-day rates for hospitalizations for selected conditions at Cincinnati Children’s Hospital Medical Center, by census tract poverty quintiles, 2011–16.
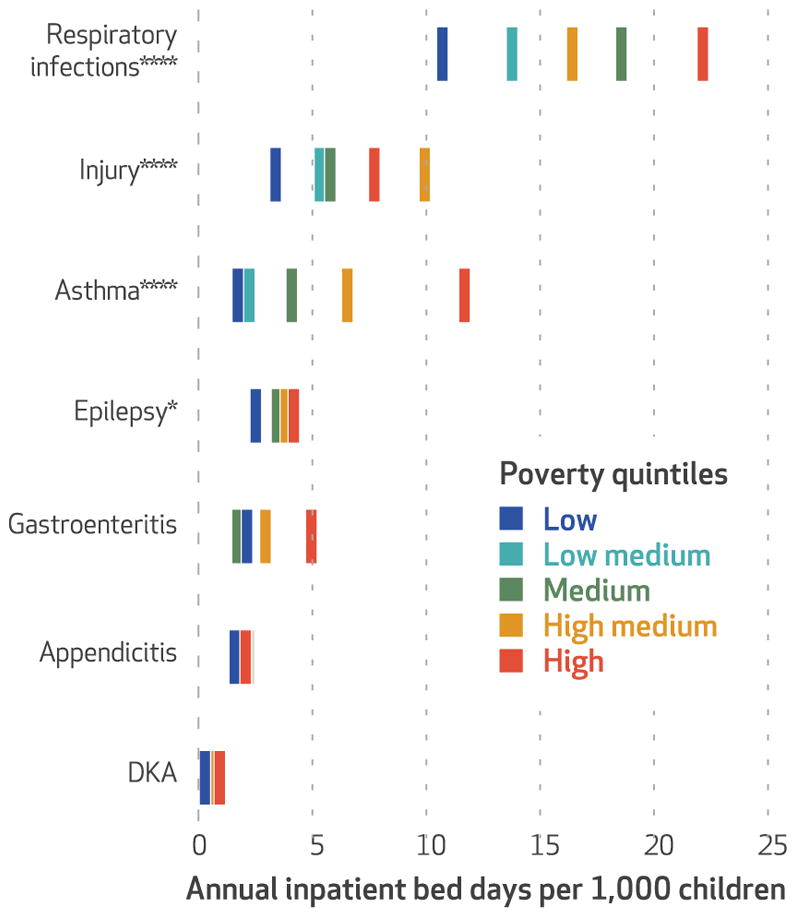
SOURCE Authors’ analysis. NOTES The quintiles are explained in the notes to exhibit 1. Significance was measured using the Kruskal-Wallis test. DKA is diabetic ketoacidosis. *p < 0.1 ****p < 0.001
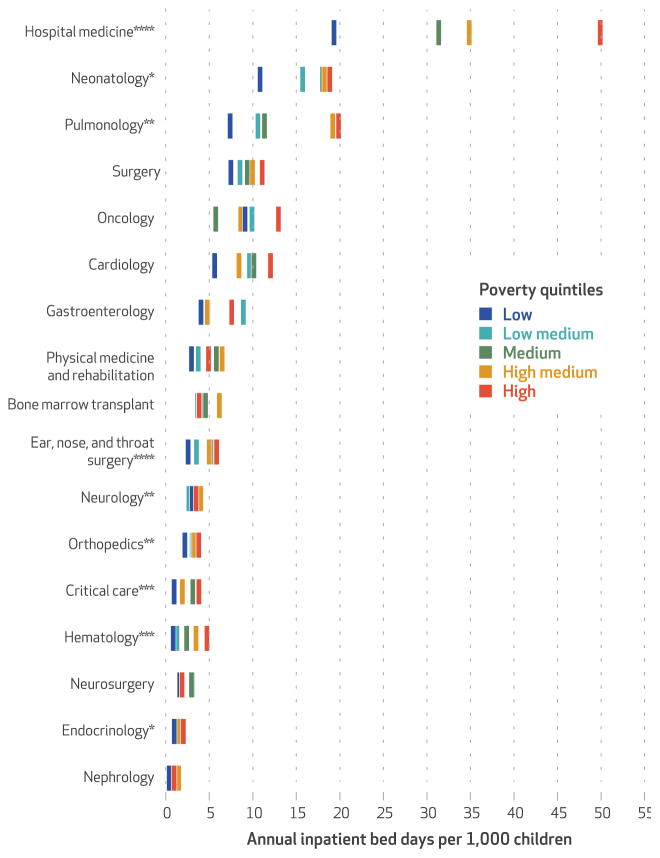
Exhibit 3 depicts similar relationships across hospital-based subspecialties. These relationships were found to be significant for hospital medicine; pulmonology; ear, nose, and throat surgery; neurology; orthopedics; critical care; and hematology. Each subspecialty except the bone marrow transplant service had a ratio greater than 1.00 when the total bed-days in the high-poverty quintile were divided by those in the low-poverty quintile (ranging from 0.97 for bone marrow transplant to 5.58 for hematology). Again, relative differences are depicted on a transformed scale in appendix exhibit 2.18 In appendix exhibit 2 the inpatient bed-day rate for each subspecialty in the high-poverty quintile was above the county mean except for bone marrow transplant and neurosurgery. Still, rates in the low-poverty quintile for each subspecialty were all below the county mean.
EXHIBIT 3. Inpatient bed-day rates for hospitalizations for selected subspecialties at Cincinnati Children’s Hospital Medical Center, by census tract poverty quintiles, 2011–16.
SOURCE Authors’ analysis. NOTES The quintiles are explained in the notes to exhibit 1. In the hospital medicine subspecialty, the bars for the low and low-medium quintiles are in the same place. Significance was measured using the Kruskal-Wallis test. *p < 0.10 **p < 0.05 ***p < 0.01 ****p < 0.001
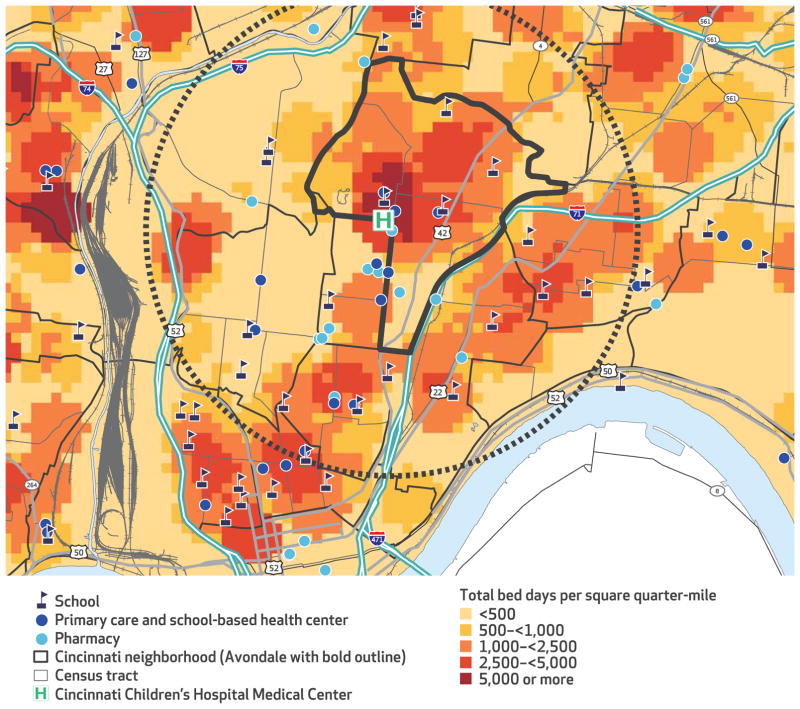
Finally, exhibit 4 shows the location of Cincinnati Children’s Hospital Medical Center and local disparities in inpatient bed-day rates. The circle represents the area within two miles of the center. “Hot spots” in the rates occur in close proximity to the hospital, within communities known to have high rates of both morbidity and poverty. In Avondale, the neighborhood bordering the hospital on three sides and outlined in bold, bed-day rates are more than double the county average. It is composed of four census tracts (three in the high-poverty quintile and one in the high-medium-poverty quintile). In the period 2011–16, the estimated 2,767 children residing in these four tracts13 accounted for 1,161 hospitalizations and 4,229 bed-days. This amounts to an inpatient bed-day rate of 254.7 days per 1,000 children per year, which is one of the highest rates in Hamilton County. Moreover, hospitalizations for Avondale children were managed by every subspecialty represented in exhibit 3. Thus, Avondale has become an early site for our population health improvement efforts, driving closer hospital-community partnerships. As the exhibit shows, within Avondale there are key assets (and partners), including schools, primary care and school-based health centers, and pharmacies. These are now coalescing around strategies aimed at cooling the hot spots and collectively building a culture of health.
EXHIBIT 4. Hot spots of inpatient bed-days for hospitalizations in Greater Cincinnati, 2011–16.
SOURCE Authors’ analysis of data from Cincinnati Children’s Hospital Medical Center and the Cincinnati Area Geographic Information System. NOTES Point density was determined using a radius of 1,320 feet or one-quarter mile. This density was split into quintiles using natural cut-points chosen a priori.
Discussion
Each year Hamilton County’s children collectively spend about 25,000 days, or roughly sixty-eight years, in the hospital. Children from communities with more poverty disproportionately bear this burden. We found clear relationships between the inpatient bed-day rate and that of child poverty across certain acute and chronic conditions managed by the range of clinical sub-specialties present in a large, academic pediatric facility. As a result, we argue that tackling disparities and narrowing associated equity gaps would benefit from a culture of health within hospitals. This may require an expanded focus on inpatient-to-outpatient transitions and community-connected work that gets to shared root causes affecting disparities across conditions and subspecialties. Such an approach may be more fruitful than attempting to tackle disparities condition by condition or hoping in vain that each subspecialty can close its own equity gap.
Historically, fee-for-service models provided hospitals with incentives to keep beds filled with patients. Evolving payment models are increasingly moving toward paying for value. As hospitals bear more financial risk, they will be driven toward prevention of hospitalizations. In this article we have identified ecological linkages between inpatient bed-day and child poverty rates. Perhaps these findings could, or should, push hospitals to more consistently and effectively identify and act on those factors that drive potentially preventable utilization (and disparities in that utilization).19–21 They may also inform how not-for-profit hospitals proceed with their needs assessments and community benefit programs in ways that aim to improve outcomes and narrow gaps.22
A key to making such improvements is ensuring that health equity is made a “shared value” within hospitals and health care systems.9 Data, presented systematically and transparently across an institution, could play a key role. Historically, information on condition- and subspecialty-specific disparities has not routinely reached front-line providers and clinical divisions in hospitals. Without these data in front of them, providers may find it difficult to foster equity-minded innovation and transform care delivery models.23 To expedite such innovation and transformation, the National Academy of Medicine explicitly highlights the benefit of “data acquisition, curation, and use for a continuously learning health system.”24 We suggest that relevant data, visible over time, should be easily accessible on institutional and divisional dashboards and to stakeholders from the top to the bottom of traditional health care hierarchies. We see this as critical to an effectively redesigned system—one that works for those patients and families who need that system the most.25
Establishing a culture of health, as articulated and envisioned by the Robert Wood Johnson Foundation, within health care settings will not be easy. Data availability and transparency must be supplemented by accessible, appropriately targeted interventions. Standard inpatient protocols tend to emphasize reactive medical management instead of more proactive risk assessments and upstream interventions. Prevention of acute conditions (such as respiratory infections) and enhanced management of chronic conditions (such as asthma) before, during, and after inpatient stays might facilitate a reduction in bed-days for those at highest risk of morbidity.26–28 We expect that such a reduction would occur more seamlessly if there were a greater focus on the root causes of the social determinants of health that are disproportionately present within the areas with the highest inpatient bed-day rates.29
Evidence clearly links disparities in certain conditions, such as asthma, to a range of such poverty-linked determinants (for example, substandard housing, limited access to pharmacy and primary care, and socioeconomic hardships).30–35 However, there is growing evidence that such links may extend to other pediatric conditions (such as epilepsy and diabetes mellitus), many of which are cared for in hospitals by subspecialists.36,37 We see the acknowledgment of disparate outcomes, and their potential linkage to competing social, economic, and environmental priorities, as relevant for clinical practice across the inpatient-to-outpatient, hospital-to-community continuum. Indeed, to enhance the likelihood that prescriptions for medications are filled and treatment plans are followed, clinicians (and hospital-based divisions) may need to focus attention on removing barriers for patients before their hospital discharge (for example, having needed medications and follow-up appointments made with transportation arranged), addressing social determinants (through connections to social workers, community health workers, or medical-legal partnerships), and fortifying communication between providers of inpatient and outpatient care.33,38–43 The layering of medical data (for example, inpatient bed-day rates) atop data on community-based social determinants may also have value by prompting collaborative interventions and pattern recognition.38,44,45 For example, a cluster of asthma admissions may be identified by community partners as an “outbreak” emanating from a problematic building complex. In turn, community organizers and legal advocates may join clinicians in seeking optimal outcomes.
We expect that a more robust culture of health within our hospitals, one humbly shared with the broader community, will be necessary for closing equity gaps. In Cincinnati, we have invested in relationships between providers of inpatient and outpatient care; nonprofit organizations; public schools; the local health department; social service agencies; faith-based entities; businesses; and, importantly, parents and families. We have supported a growing learning network that aims to foster health and well-being for all of Cincinnati’s children, regardless of where they live, learn, and play.12 This collaborative strategy has been key to our early efforts to improve outcomes, particularly in neighborhoods such as Avondale that, despite being within steps of an internationally recognized children’s hospital, still experience unacceptable health outcomes. Although many at Cincinnati Children’s Hospital Medical Center, and across the Greater Cincinnati community, likely knew (and lived) this reality for years, a deep dive into our population-based epidemiological data has prompted new questions and a sharpened focus on a community-oriented strategic plan. This plan pushes ongoing population health improvement efforts, informs the allocation of community benefit dollars, and supports more equitable investment in social services within our hospitals, health care systems, and communities.46,47
Conclusion
If children from all of Hamilton County’s census tracts spent the same amount of time in the hospital as those from the most affluent tracts, roughly twenty-two child-years of hospitalization time would be prevented annually. Disparities such as this can be reduced, in part, by a strengthened culture of health within a hospital or health care system whose goals are aligned with those of the community it supports.
Supplementary Material
Acknowledgments
Support for this work was provided, in part, through the National Institutes of Health (Grant No. NIH 1K23AI112916) and the AcademyHealth Community Health Peer Learning Program, Communities for Connected Health (Office of the National Coordinator for Health Information Technology, Department of Health and Human Services, Grant No. 90CL0001.01-00, Subaward No. 375.90CL.006). Funders played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The authors thank Kate Rich for her assistance in acquiring the data central to this article’s analyses. The authors also thank all of the people who give of their time and energy to the All Children Thrive Learning Network.
Contributor Information
Andrew F. Beck, University of Cincinnati College of Medicine and Cincinnati Children’s Hospital Medical Center, in Ohio.
Carley L. Riley, University of Cincinnati College of Medicine and at Cincinnati Children’s Hospital Medical Center.
Stuart C. Taylor, James M. Anderson Center for Health Systems Excellence at Cincinnati Children’s Hospital Medical Center.
Cole Brokamp, University of Cincinnati College of Medicine and Cincinnati Children’s Hospital Medical Center.
Robert S. Kahn, University of Cincinnati College of Medicine and at Cincinnati Children’s Hospital Medical Center.
NOTES
- 1.Cincinnati Health Department. Neighborhood life expectancy data [Internet] Cincinnati (OH): The Department; c2018. [cited 2018 Feb 2]. Available from: http://www.cincinnati-oh.gov/health/community-health-data/neighborhood-life-expectancy-data/ [Google Scholar]
- 2.Gupta RS, Zhang X, Sharp LK, Shannon JJ, Weiss KB. Geographic variability in childhood asthma prevalence in Chicago. J Allergy Clin Immunol. 2008;121(3):639–645e1. doi: 10.1016/j.jaci.2007.11.036. [DOI] [PubMed] [Google Scholar]
- 3.Wright RJ, Subramanian SV. Advancing a multilevel framework for epidemiologic research on asthma disparities. Chest. 2007;132(5, Suppl):757S–69S. doi: 10.1378/chest.07-1904. [DOI] [PubMed] [Google Scholar]
- 4.Beck AF, Florin TA, Campanella S, Shah SS. Geographic variation in hospitalization for lower respiratory tract infections across one county. JAMA Pediatr. 2015;169(9):846–54. doi: 10.1001/jamapediatrics.2015.1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beck AF, Moncrief T, Huang B, Simmons JM, Sauers H, Chen C, et al. Inequalities in neighborhood child asthma admission rates and underlying community characteristics in one US county. J Pediatr. 2013;163(2):574–80. doi: 10.1016/j.jpeds.2013.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carroll-Scott A, Henson RM, Kolker J, Purtle J. The role of nonprofit hospitals in identifying and addressing health inequities in cities. Health Aff (Millwood) 2017;36(6):1102–9. doi: 10.1377/hlthaff.2017.0033. [DOI] [PubMed] [Google Scholar]
- 7.Cheng TL, Emmanuel MA, Levy DJ, Jenkins RR. Child health disparities: what can a clinician do? Pediatrics. 2015;136(5):961–8. doi: 10.1542/peds.2014-4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lavizzo-Mourey R. Why we need to build a culture of health in the United States. Acad Med. 2015;90(7):846–8. doi: 10.1097/ACM.0000000000000750. [DOI] [PubMed] [Google Scholar]
- 9.Trujillo MD, Plough A. Building a culture of health: a new framework and measures for health and health care in America. Soc Sci Med. 2016;165:206–13. doi: 10.1016/j.socscimed.2016.06.043. [DOI] [PubMed] [Google Scholar]
- 10.Woolf SH, Braveman P. Where health disparities begin: the role of social and economic determinants—and why current policies may make matters worse. Health Aff (Millwood) 2011;30(10):1852–9. doi: 10.1377/hlthaff.2011.0685. [DOI] [PubMed] [Google Scholar]
- 11.Woolf SH, Purnell JQ. The good life: working together to promote opportunity and improve population health and well-being. JAMA. 2016;315(16):1706–8. doi: 10.1001/jama.2016.4263. [DOI] [PubMed] [Google Scholar]
- 12.Kahn RS, Iyer SB, Kotagal UR. Development of a child health learning network to improve population health outcomes; presented in honor of Dr Robert Haggerty. Acad Pediatr. 2017;17(6):607–13. doi: 10.1016/j.acap.2017.04.024. [DOI] [PubMed] [Google Scholar]
- 13.Census Bureau. American FactFinder [Internet] Washington (DC): Census Bureau; [cited 2018 Feb 2]. Available [through database search] from: https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t. [Google Scholar]
- 14.Brokamp C, Wolfe C, Lingren T, Harley J, Ryan P. Decentralized and reproducible geocoding and characterization of community and environmental exposures for multisite studies. J Am Med Inform Assoc. 2017 doi: 10.1093/jamia/ocx128. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brokamp C, LeMasters GK, Ryan PH. Residential mobility impacts exposure assessment and community socioeconomic characteristics in longitudinal epidemiology studies. J Expo Sci Environ Epidemiol. 2016;26(4):428–34. doi: 10.1038/jes.2016.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morse RB, Hall M, Fieldston ES, Goodman DM, Berry JG, Gay JC, et al. Children’s hospitals with shorter lengths of stay do not have higher readmission rates. J Pediatr. 2013;163(4):1034–8e1. doi: 10.1016/j.jpeds.2013.03.083. [DOI] [PubMed] [Google Scholar]
- 17.Simon TD, Cawthon ML, Stanford S, Popalisky J, Lyons D, Woodcox P, et al. Pediatric Medical Complexity Algorithm: a new method to stratify children by medical complexity. Pediatrics. 2014;133(6):e1647–54. doi: 10.1542/peds.2013-3875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.To access the appendix, click on the Details tab of the article online.
- 19.Galloway I. Using pay-for-success to increase investment in the non-medical determinants of health. Health Aff (Millwood) 2014;33(11):1897–904. doi: 10.1377/hlthaff.2014.0741. [DOI] [PubMed] [Google Scholar]
- 20.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable Health Communities—addressing social needs through Medicare and Medicaid. N Engl J Med. 2016;374(1):8–11. doi: 10.1056/NEJMp1512532. [DOI] [PubMed] [Google Scholar]
- 21.Hughes LS, Peltz A, Conway PH. State innovation model initiative: a state-led approach to accelerating health care system transformation. JAMA. 2015;313(13):1317–8. doi: 10.1001/jama.2015.2017. [DOI] [PubMed] [Google Scholar]
- 22.Kindig D, Stoddart G. What is population health? Am J Public Health. 2003;93(3):380–3. doi: 10.2105/ajph.93.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Plough AL. Building a culture of health: a critical role for public health services and systems research. Am J Public Health. 2015;105(Suppl 2):S150–2. doi: 10.2105/AJPH.2014.302410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dzau VJ, McClellan MB, McGinnis JM, Burke SP, Coye MJ, Diaz A, et al. Vital directions for health and health care: priorities from a National Academy of Medicine initiative. JAMA. 2017;317(14):1464. doi: 10.1001/jama.2017.1964. [DOI] [PubMed] [Google Scholar]
- 25.Wong WF, LaVeist TA, Sharfstein JM. Achieving health equity by design. JAMA. 2015;313(14):1417–8. doi: 10.1001/jama.2015.2434. [DOI] [PubMed] [Google Scholar]
- 26.Bhaumik U, Sommer SJ, Giller-Leinwohl J, Norris K, Tsopelas L, Nethersole S, et al. Boston Children’s Hospital Community Asthma Initiative: five-year cost analyses of a home visiting program. J Asthma. 2017;54(2):134–42. doi: 10.1080/02770903.2016.1201837. [DOI] [PubMed] [Google Scholar]
- 27.Woods ER, Bhaumik U, Sommer SJ, Chan E, Tsopelas L, Fleegler EW, et al. Community Asthma Initiative to improve health outcomes and reduce disparities among children with asthma. MMWR Suppl. 2016;65(1):11–20. doi: 10.15585/mmwr.su6501a4. [DOI] [PubMed] [Google Scholar]
- 28.Grinberg C, Hawthorne M, LaNoue M, Brenner J, Mautner D. The core of care management: the role of authentic relationships in caring for patients with frequent hospitalizations. Popul Health Manag. 2016;19(4):248–56. doi: 10.1089/pop.2015.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Woolf SH. Progress in achieving health equity requires attention to root causes. Health Aff (Millwood) 2017;36(6):984–91. doi: 10.1377/hlthaff.2017.0197. [DOI] [PubMed] [Google Scholar]
- 30.Beck AF, Simmons JM, Huang B, Kahn RS. Geomedicine: area-based socioeconomic measures for assessing risk of hospital reutilization among children admitted for asthma. Am J Public Health. 2012;102(12):2308–14. doi: 10.2105/AJPH.2012.300806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beck AF, Huang B, Simmons JM, Moncrief T, Sauers HS, Chen C, et al. Role of financial and social hardships in asthma racial disparities. Pediatrics. 2014;133(3):431–9. doi: 10.1542/peds.2013-2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Auger KA, Kahn RS, Davis MM, Beck AF, Simmons JM. Medical home quality and readmission risk for children hospitalized with asthma exacerbations. Pediatrics. 2013;131(1):64–70. doi: 10.1542/peds.2012-1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kattan M, Mitchell H, Eggleston P, Gergen P, Crain E, Redline S, et al. Characteristics of inner-city children with asthma: the National Cooperative Inner-City Asthma Study. Pediatr Pulmonol. 1997;24(4):253–62. doi: 10.1002/(sici)1099-0496(199710)24:4<253::aid-ppul4>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 34.Rosenfeld L, Rudd R, Chew GL, Emmons K, Acevedo-García D. Are neighborhood-level characteristics associated with indoor allergens in the household? J Asthma. 2010;47(1):66–75. doi: 10.3109/02770900903362676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sandel M, Wright RJ. When home is where the stress is: expanding the dimensions of housing that influence asthma morbidity. Arch Dis Child. 2006;91(11):942–8. doi: 10.1136/adc.2006.098376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O’Malley JA, Klett BM, Klein MD, Inman N, Beck AF. Revealing the prevalence and consequences of food insecurity in children with epilepsy. J Community Health. 2017;42(6):1213–9. doi: 10.1007/s10900-017-0372-1. [DOI] [PubMed] [Google Scholar]
- 37.Valenzuela JM, Seid M, Waitzfelder B, Anderson AM, Beavers DP, Dabelea DM, et al. Prevalence of and disparities in barriers to care experienced by youth with type 1 diabetes. J Pediatr. 2014;164(6):1369–75e1. doi: 10.1016/j.jpeds.2014.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Beck AF, Sandel MT, Ryan PH, Kahn RS. Mapping neighborhood health geomarkers to clinical care decisions to promote equity in child health. Health Aff (Millwood) 2017;36(6):999–1005. doi: 10.1377/hlthaff.2016.1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Klein MD, Beck AF, Henize AW, Parrish DS, Fink EE, Kahn RS. Doctors and lawyers collaborating to HeLP children—outcomes from a successful partnership between professions. J Health Care Poor Under-served. 2013;24(3):1063–73. doi: 10.1353/hpu.2013.0147. [DOI] [PubMed] [Google Scholar]
- 40.Kercsmar CM, Beck AF, Sauers-Ford H, Simmons J, Wiener B, Crosby L, et al. Association of an asthma improvement collaborative with health care utilization in Medicaid-insured pediatric patients in an urban community. JAMA Pediatr. 2017;171(11):1072–80. doi: 10.1001/jamapediatrics.2017.2600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Crocker DD, Kinyota S, Dumitru GG, Ligon CB, Herman EJ, Ferdinands JM, et al. Effectiveness of home-based, multi-trigger, multicomponent interventions with an environmental focus for reducing asthma morbidity: a community guide systematic review. Am J Prev Med. 2011;41(2, Suppl 1):S5–32. doi: 10.1016/j.amepre.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 42.Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: how interventions that address the social determinants of health can improve health and reduce disparities. J Public Health Manag Pract. 2008;14(Suppl):S8–17. doi: 10.1097/01.PHH.0000338382.36695.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thornton RL, Glover CM, Cené CW, Glik DC, Henderson JA, Williams DR. Evaluating strategies for reducing health disparities by addressing the social determinants of health. Health Aff (Millwood) 2016;35(8):1416–23. doi: 10.1377/hlthaff.2015.1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hardt NS, Muhamed S, Das R, Estrella R, Roth J. Neighborhood-level hot spot maps to inform delivery of primary care and allocation of social resources. Perm J. 2013;17(1):4–9. doi: 10.7812/TPP/12-090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Beck AF, Huang B, Chundur R, Kahn RS. Housing code violation density associated with emergency department and hospital use by children with asthma. Health Aff (Millwood) 2014;33(11):1993–2002. doi: 10.1377/hlthaff.2014.0496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bradley EH, Canavan M, Rogan E, Talbert-Slagle K, Ndumele C, Taylor L, et al. Variation in health outcomes: the role of spending on social services, public health, and health care, 2000–09. Health Aff (Millwood) 2016;35(5):760–8. doi: 10.1377/hlthaff.2015.0814. [DOI] [PubMed] [Google Scholar]
- 47.Baum FE, Bégin M, Houweling TA, Taylor S. Changes not for the faint-hearted: reorienting health care systems toward health equity through action on the social determinants of health. Am J Public Health. 2009;99(11):1967–74. doi: 10.2105/AJPH.2008.154856. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.