Abstract
Objectives
The understanding of how stress influences health behavior can provide insights into developing healthy lifestyle interventions. This understanding is traditionally attained through observational studies that examine associations at a population level. This nomothetic approach, however, is fundamentally limited by the fact that the environment-person milieu that constitutes stress exposure and experience can vary substantially between individuals, and the modifiable elements of these exposures and experiences are individual-specific. With recent advances in smartphone and sensing technologies, it is now possible to conduct idiographic assessment in users’ own environment, leveraging the full-range observations of actions and experiences that result in differential response to naturally occurring events. The aim of this paper is to explore the hypothesis that an ideographic N-of-1 model can better capture an individual’s stress-behavior pathway (or the lack thereof) and provide useful person-specific predictors of exercise behavior.
Methods
This paper used the data collected in an observational study in 79 participants who were followed for up to a 1-year period, wherein their physical activity was continuously and objectively monitored by actigraphy and their stress experience was recorded via ecological momentary assessment on a mobile app. In addition, our analyses considered exogenous and environmental variables retrieved from public archive such as day in a week, daylight time, temperature and precipitation. Leveraging the multiple data sources, we developed prediction algorithms for exercise behavior using random forest and classification tree techniques using a nomothetic approach and an N-of-1 approach. The two approaches were compared based on classification errors in predicting personalized exercise behavior.
Results
Eight factors were selected by random forest for the nomothetic decision model, which was used to predict whether a participant would exercise on a particular day. The predictors included previous exercise behavior, emotional factors (e.g., midday stress), external factors such as weather (e.g., temperature), and self-determination factors (e.g., expectation of exercise). The nomothetic model yielded an average classification error of 36%. The ideographic N-of-1 models used on average about two predictors for each individual, and had an average classification error of 25%, which represented an improvement of 11 percentage points.
Conclusions
Compared to the traditional one-size-fits-all, nomothetic model that generalizes population-evidence for individuals, the proposed N-of-1 model can better capture the individual difference in their stress-behavior pathways. In this paper, we demonstrate it is feasible to perform personalized exercise behavior prediction, mainly made possible by mobile health technology and machine learning analytics.
Keywords: ecological momentary assessment, exercise behavior, machine learning, stress-behavior pathway, personal informatics, self-quantification
1. INTRODUCTION
Behavioral factors including physical inactivity bear great responsibility for cardiovascular disease risk, accounting for approximately 41% of the global cardiovascular disease burden [1,2]. Improving health behaviors could reduce cardiovascular disease risk [3] and also reduce the associated public health burden up to 38% [4]. Exercise in particular is an appealing option because it is relatively low cost compared to pharmacologic treatment, does not generally interfere with medications, and is potentially modifiable. The importance of a healthy lifestyle, defined in part by regular exercise, is largely understood by epidemiologists, medical scientists, practitioners, and indeed, the general public. Despite all these, broad public adoption and maintenance of a healthy lifestyle remains elusive [5]. While the clinical trial data demonstrate that anyone can be taught to implement a regular program of exercise, these data are also notable for consistently demonstrating study participants’ failure to maintain this critical health practice over prolonged periods [6]. Indeed, the literature abounds with randomized clinical trials devoted to exercise maintenance, and while important features of a maintenance program have been identified, the implementation of these additional practices appears to be just one more health behavior that cannot be transformed into a habit. A key public health imperative is therefore to identify – and then intervene on - the factors that serve as obstacles to the adoption of sustained healthy exercise behavior [7].
A Stress-Behavior Mechanistic Pathway
There are long held beliefs that psychological stress contributes to cardiovascular disease, in part, through its adverse impact on health behaviors [8,9]. It is therefore no surprise that emerging research demonstrates that demanding features of daily life can promote psychological stress and can serve as a barrier to good health practices, thereby perpetuating poor health behavior [10]. Most definitions of stress share three assumptions reviewed in [11], summarized as follows: First, stress is a process that occurs when environmental demands exceed the adaptive capacity of the individual [11]. Second, this process results in psychological and biologic changes that may have detrimental consequences on health [12]. Third, individual interpretations of the environmental demands and adaptive capacity (“appraisals”) are important in determining psychological, behavioral, and physiological responses to stress [13]. These assumptions suggest a stress pathway to exercise behavior that is characterized by (i) the intra-personal appraisal process for experiencing a given environmental demand as stressful, and (ii) temporal feedback from the previously measured stress perception. Thus, if we can examine daily processes within subjects (as compared to the conventional between-subjects approach), we may increase our potential to discover new and possibly potent yet idiographic influences that stress has on the behavior of a particular individual.
In fact, psychologists and behavioral scientists have developed a variety of ideographic analytical approaches for single-case experimental designs [14,15,16]. To extend this novel experimental design to clinical care, researchers have further developed N-of-1 trials to determine optimal interventions based on individual data-driven criteria to help patients make health decisions that are informed by highly relevant, evidence-based, and personalized information [17,18,19]. In the field of personalized health, researchers have proposed the use of mobile technology and developed a user-centered self-experimentation framework to guide users through the process [19].
While the idiographic analytical approach is not a new concept, its practice has been limited by the inability to collect reliable intensive within-person data necessary for such a task. There has been no shortage of efforts to identify barriers to healthy lifestyle—primarily in the form of population-based studies that are designed to establish associations using cross-sectional data or limited longitudinal data. These studies generally identify demographic factors and co-morbidities that are associated with exercise and healthy behaviors, and are useful for public health policy-making and implementation science [20]. This nomothetic approach however offers little insight into overcoming individual obstacles in a counseling setting, partly because it ignores the fact that the “toxic” elements of stress exposure and the modifiable aspects of the environment-person milieu are highly varied among individuals.
mHealth and Ecological Momentary Assessment (EMA)
Idiographic assessment of stress-behavior relationships has become possible by using ecological momentary assessment (EMA) [21,22] in light of the recent advances in mobile health information and sensing technologies (mHealth) [23] and the broad use of mobile devices. For example, wearable activity trackers permit us to track physical activity of an individual remotely for extended periods of time. Recently, the collection of self-quantification data has been shown to exhibit population-based patterns through big data techniques [24], and new health informatics programs have been developed to generate scientific evidence [25].
In addition, by coupling EMA with smartphone use, we can repeatedly collect exposure data of psychosocial stressors in ecologically valid settings such as home and work, and in real time. Miniaturization has improved our ability to collect information with relatively little bias, in contrast to paper-and-pencil dairies. Assessments can focus on the immediate context (when an individual is prompted), thereby substantially reducing recall bias [26, 27].
2. OBJECTIVES
In this article, we explore the hypothesis that an N-of-1 model of stress-exercise behavior relationship and exogenous factors can provide useful person-specific predictors and improve accuracy for predicting daily exercise bouts in comparison to the conventional nomothetic approach that builds population-based prediction algorithms. This is made possible by using continuously available information collected through wearable devices and EMA, coupled with environmental factors over an extended period of time.
3. METHODS
From Jan 2014 to July 2015, we enrolled 79 healthy adults who were residents of northern Manhattan. The inclusion criteria are: (i) age 18 years or older; (ii) fluent in English or Spanish; (iii) primary care provider clearance to engage in at least 30 minutes of daily exercise; (iv) self-report of having exercised at least 6 times at moderate or higher intensity during the last month. Exclusion criteria include: (i) unable to complete the run-in assessment; (ii) deemed unable to comply with the protocol; (iii) active psychosis, bipolar disorder, or any overt personality disorder; (iv) prisoner; (v) unavailable for follow-up (including those with a terminal non-cardiovascular illness and those who indicate they are about to leave the U.S.); (vi) a score of <10 on the Charlson comorbidity index; (vii) a serious medical comorbidity that would compromise their ability to engage in regular exercise; (viii) occupational work demands that require regular exercise or would make responding to the EMA dangerous. At baseline, demographic characteristics were collected from each participant, including age, gender, race, ethnicity, education, partner status, and living situations. Each participant was then followed for up to a 1-year period. The study was approved by the Columbia Institutional Review Board. Details of enrollments, sample characteristics, and description of stress and stressors can be found in [28].
Physical Activity and Exercise
Physical activity was monitored continuously for up to 12 months using a wrist-worn Fitbit activity monitor (Fitbit Flex; http://www.fitbit.com). Data collected from the device were automatically uploaded to the Fitbit website whenever the device was within 15 feet of the base station, which was plugged into the participant’s own desktop computer. The monitor was worn on the non-dominant wrist of participants, who were instructed to sync and charge their device at least every 5–7 days to ensure no loss of activity data. The Fitbit data provided objectively measured daily physical activity patterns of each participant, and were used to ascertain the occurrence of cumulative 30-minute periods of moderate or high intensity physical activity in each 24-hour period. In this analysis, we defined “exercise” as any consecutive 30-minute period within which 24 or more minutes were classified as moderate or vigorous intensity. We followed the recommendations of Ward et al. [29] regarding best practices for the use of accelerometer data in research on physical activity. Specifically, physical activity guidelines recommend exercise in bouts of 10 minutes or more for at least 30 minutes a day while accommodating interruptions [30]. Thus, when analyzing accelerometer data, the conventional approach is to quantify exercise in bouts of 10 minutes with allowances for 2 minutes of interruption (e.g., 8 out of 10 minutes). Extrapolating the definition based on 10 to 30 minutes, this yielded 24 out of 30 minutes. Software was written to determine, for each day, whether there was any 30-minute period within which at least 24 minutes were classified as moderate or vigorous activity; this was our objectively assessed measure of a 30-minute period of exercise.
Ecological Momentary Assessments
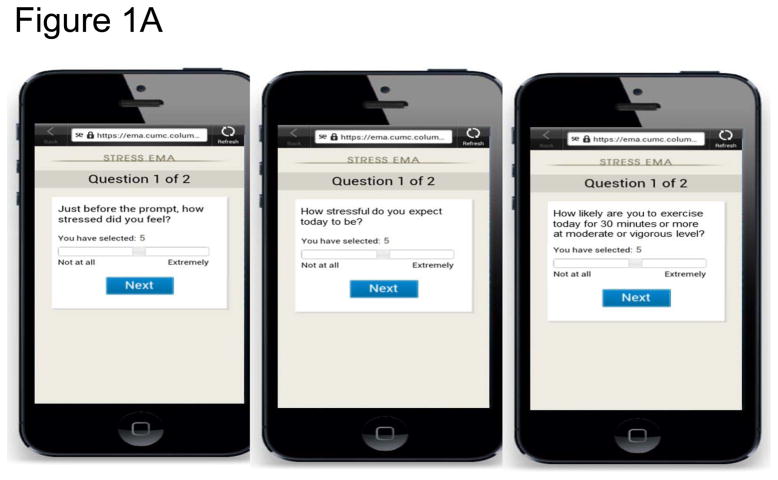
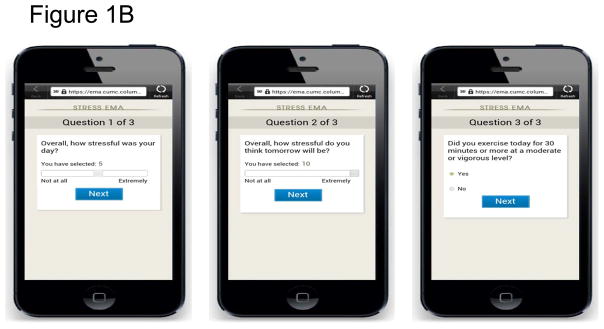
An electronic diary that used the participant’s own smartphone was used to capture momentary and summary aspects of the stress experience, and was programmed to prompt the participant to answer questions regarding their perception, appraisal, and sources of psychological stress, at different times of the day during a 15-hour awake time window. These actual stress experiences were elicited via midday EMA of the following question “Just before the prompt, how stressed did you feel?”; see Figure 1A. In addition to the actual stress experience, each morning upon rising, participants were prompted to rate their expected stress for the day and their plan for doing 30 minutes of cumulative exercise that day. Specifically, for the morning EMA, each participant was asked “How stressful do you expect today to be?” for expected stress, and “How likely are you to exercise today for 30 minutes or more at moderate or vigorous level?” for expected exercise; see Figure 1A. Self-reported exercise and expectation of stress the next day were also recorded at the end of each day via the electronic diaries with the question “Overall, how stressful do you think tomorrow will be?”; see Figure 1B. The range of answer for all the above questions was 0 (“not at all”) to 10 (“extremely likely”). These assessment instruments have been used extensively in the literature for capturing momentary and daily diaries before the era of smartphone or even electronic diaries, and have been used with smartphone for EMA in recent studies [31,32,33].
Figure 1.
Figure 1A. EMA screenshots (morning and midday)
Figure 1B. EMA screenshots (evening)
External and Environmental Variables
External and environmental variables, including temperature (high, low, average, range), daylight time, precipitation, and day of week, were retrieved from the meteorological station in Central Park, New York, NY which are made publically available by the National Oceanic and Atmospheric Administration’s National Center For Environmental Information (http://www.ncdc.noaa.gov/qclcd/QCLCD?prior=N).
Statistical Analyses
The objective of the analyses was to predict whether a participant would exercise on a given day using the EMA data on stress and expected exercise (5 measurements a day), the external and environmental factors (7 variables), and the actual exercise on previous days, tracked up to three past days. Thus, each measurement/variable might contribute up to 4 predictors in the models, except for day of week and actual exercise, which might contribute to 1 and up to 3 predictors respectively.
We considered two analytical approaches. First, we considered the N-of-1 approach whereby we built a classification decision tree for each of the 79 participants. Specifically, for each individual, we applied random forest [34] to yield a ranking of variable importance measured by the average decrease in classification accuracy after permuting the variables in all trees in the forest. Then we selected variables that would lead to a standardized average decrease in classification accuracy by at least 3 standard deviations from the mean average decrease over all variables; the threshold of 3 standard deviations was chosen to minimize the average cross-validation error based on ten-fold cross validation. Finally, we built a classification tree for exercise prediction using the selected variables [34]. The result of this N-of-1 approach was 79 decision trees, one for each participant.
Second, following the conventional method, we considered a nomothetic approach that used data from all 79 participants to build a single model for exercise prediction using the same analytical steps: we ranked the variables using the random forest approach, selected variables based on the same cross-validation threshold as in the N-of-1 method (i.e. 3 standard deviations from the mean decrease of accuracy), and built a classification tree using the variables selected as predictors in the model. The main difference is that the nomothetic method used data from all participants as inputs in building random forest and classification tree. The result of this nomothetic approach was a single tree that is applied to make predictions in all participants.
To compare the performance across the two approaches on the task of exercise prediction, the classification error of either method (N-of-1 or nomothetic) for each participant was calculated as the proportion of days that the model made a wrong prediction over the evaluation window. The evaluation window was a 177-day period in which the decision tree model was used to predict exercise between day 4 and day 180 of an individual. Statistical analyses were performed in R (version 3.3.2). The random forests and classification trees were built by binary recursive partitioning [34] using functions in the R packages randomForest and rpart.
RESULTS
The Nomothetic Model
In our sample, the average age was 32 years with a standard deviation of 10 years and a range from 20 to 58 years; 57% (n=45) were women; 42% (n=33) were of White race and 58% of other races including 19% Asian and 14% African American; 28% of participants were of Hispanic ethnicity. Details of the characteristics are provided in [28]. Out of 79 participants, sixty-six had a complete follow-up of all 180 days, with a mean of 171-day follow-up.
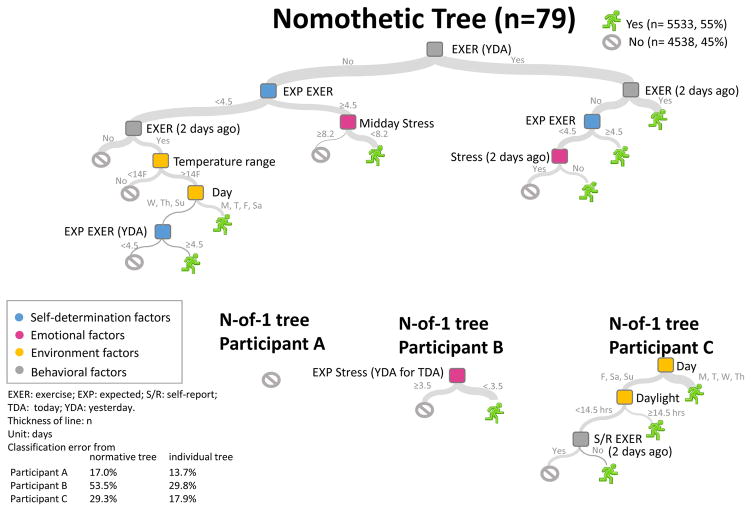
Using data in all 79 participants, the random forest identified 8 important variables of different nature, namely, stress experience (emotional), expectation of exercise (self-determination), day of the week (external), and exercise patterns in the previous days (behavioral); details are given in Table 1. Using these eight variables as input variables in classification algorithm, we obtained a nomothetic tree for exercise prediction shown in the top panel of Figure 2. The average classification error of this algorithm was 36% over the 79 participants. In other words, out of the 177 days, the model would have accurately predicted whether a participant exercised or not on about 113 days on average.
Table 1.
The eight variables selected for the nomothetic model using random forest
| Nature of variable | Variable | Source of data |
|---|---|---|
| Stress experience (emotional) | 1. Midday stress | EMA on the intra-personal appraisal of stress (on a scale of 0–10) prompted on user’s smartphone in the mid-point of a 15-hour awake time window |
| 2. Stress two days ago | EMA on self-reported perceived stress in the end of a 15-hour awake time window | |
| Exercise behavior (temporal feedback to stress perception) | 3. Exercise yesterday | The device-recorded occurrence of cumulative high intensity physical activity, measured with at least one 30-minutes in a 24-hours period (see definition under “Physical Activity and Exercise”) |
| 4. Exercise two days ago | ||
| Expected exercise (self-determination) | 5. Whether expected to exercise on the target day | EMA on the likelihood (on a scale of 0–10) to do at least 30 minutes of cumulative exercise that day |
| 6. Whether expected to exercise on the day before | ||
| Exogenous factor (environment/external) | 7. Temperature range | Measured in Fahrenheit (°F) |
| 8. Day of a week | Cyclic weekly pattern coded as M, T, W, Th, F, Sa, Su |
Figure 2.
Top: A nomothetic exercise prediction model based on all study participants. Bottom: Examples of “N-of-1” exercise prediction models in three study participants.
N-of-1 Models
The N-of-1 approach produced a prediction tree for each of the 79 participants. For illustration, the bottom panel of Figure 2 shows examples from three participants, for whom 0, 1, and 3 predictors were included in their models. The only exercise predictor of Participant B was the level of expected stress from the previous day. Specifically, the participant would exercise if he/she had experienced low stress level in the previous day. This provides direct evidence supporting the stress-behavior pathway we conjectured above—for one participant. N-of-1 models in other participants however revealed diversity in the predictors. The exercise pattern of Participant C was influenced by external factors including the day of the week and daylight duration and previous exercise behavior (self-reported); and stress was not an important predictor in this participant. Yet another case scenario was illustrated in Participant A, whom had a low exercise rate (14%) that was not predicted by any predictors used in our model and would be classified by a non-exerciser by the majority rule. This case might be classified as an unmotivated exerciser. Importantly, relying on the nomothetic model would have otherwise erroneously attributed a set of diverse predictors that were not relevant to exercise behavior in this participant.
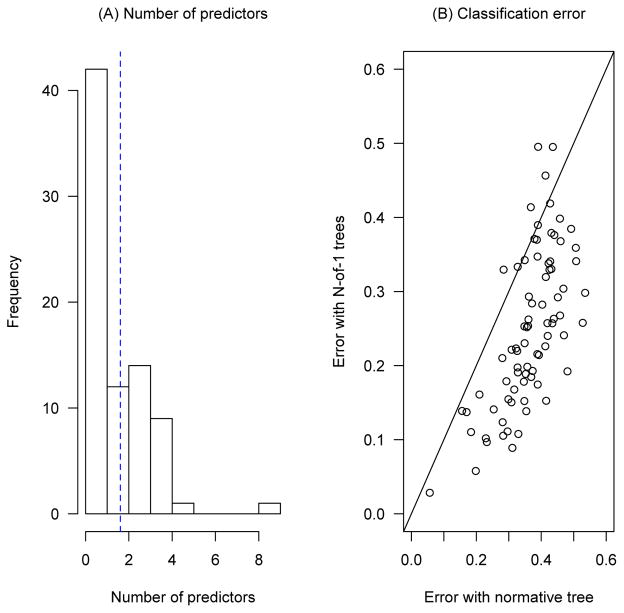
Analysis of common predictors across the 79 N-of-1 models further illustrates the diversity in the stress-behavior pathway: only 8 variables were used in predicting daily exercise for at least 5 participants; see Table 2. The most commonly included variable was the expectation of exercise, which was an important predictor in only 16 participants out of 79. Thus, there was no dominating predicting factor. It is also interesting to note that some of the most included variables such as day light duration and average temperature listed in Table 2 were not included in the nomothetic model. This suggests the population approach might have ignored factors that were important to individuals. Figure 3(A) gives the distribution of the number of predictors in the N-of-1 trees, and shows a range of 0–9 predictors and a mean of 1.6 predictors used in the N-of-1 trees. This demonstrates the varying degrees of complexity of decision making in different individuals.
Table 2.
Variables that were important in at least 5 participants
| Variable | Frequency |
|---|---|
| Expected exercise today | 16 |
| Day of week | 13 |
| Day light duration | 11 |
| Average temperature | 10 |
| Range of temperature | 5 |
| Precipitation | 5 |
| Expected exercise yesterday | 5 |
| Expected today stress | 5 |
Figure 3.
Properties of the prediction models. (A) The number of predictors used in the N-of-1 trees (blue dotted line indicates the mean value, 1.6). (B) Classification errors of N-of-1 models vs that of nomothetic model.
The average classification error of the N-of-1 approach was 25%. Thus, it was favorable in comparison to the nomothetic approach (36%) by 11 percentage points. Figure 3(B) plots the error rates by the two approaches in the 79 participants: the nomothetic approach yielded error rate that was better than or the same as the N-of-1 trees in only 7 participants (9% of all participants). A close examination of the N-of-1 trees for these 7 participants revealed that they were all “null” trees where no predictive factor was identified (cf. Participant A). While the nomothetic algorithm provided better prediction in these 7 participants (by an average of 4 percentage points) than the null tree, the complicated process may induce a feasibility difficulty in the context of behavior counseling.
5. DISCUSSION
In this article, we have presented the results of two analytical approaches for building prediction algorithms for daily exercise behaviors in 79 participants enrolled in an observational study [28]. In order to achieve person-specific prediction, we included additional external and environmental variables in our analyses, and examined how these variables would increase the accurate prediction of daily exercise bouts. Our analyses above showed that the N-of-1 modeling approach revealed the diversity and heterogeneity in the predictive pathway to exercise across individuals; cf. Figures 2 and 3(A) and Table 2. As a result, approaches to remove obstacles to regular exercise in these participants may focus on completely different behavioral or environmental re-design strategies—as such models may identify prior-day high levels of work stress as the barrier to exercise for one participant (Participant B), and the weather as the barrier for another (Participant C). Clearly different interventions would need to be implemented to respond successfully to these different predictors.
Our analyses also served as an empirical validation for accounting for the idiosyncratic nature of some relationships, such as that of predictors of intermittent exercise by improving the classification rate by 11% on average. Importantly, such improvement was achieved with simpler prediction algorithms (i.e., fewer number of predictors in the N-of-1 models than in the nomothetic model), and hence a lower “developmental cost”. Building a nomothetic model will require using all data in all participants in the model fitting process. Our sample consists of a small number of individuals, each contributing 2,160 EMA measurements and external variables, in addition to the daily exercise status, over a 180-day period. If we implement a nomothetic approach in the broad population over a longer period, the computational cost will increase rapidly. In contrast, fitting a N-of-1 model will only require data from a single person. Thus, the requirement on computational capacity will be much less demanding with the idiographic modeling approach.
Compared to the one-size-fit-all, nomothetic modeling approach that is commonly applied to generate generalizable results from population data, N-of-1 modeling is motivated by patient-oriented implementation research where the goal is to provide quality improvement in specific settings (e.g., participants, clinics), instead of producing generalized results [35]. As illustrated in the abovementioned specific instances, the predictors of daily exercise do not apply to everyone and are not generalizable in this sense. Rather than training a nomothetic model to produce generalized knowledge, this study thus aims to come up with individualized decision rules that can benefit the population one individual at a time.
The types of data that can be collected are only limited by the possibilities offered by the monitoring and sensing technologies. In this paper, we considered psychosocial stressor information collected by EMA and environmental data that is publically available. While this calls for careful study and validation of the instruments used to measure stress and exercise behavior, we emphasize here the new opportunities made possible by technological advances, which allow us to take measurements in real time. Because of the recent advance in real-time tracking technologies, we can also objectively measure factors that correspond to the EMA, such as weather variables considered in this paper. Other possibilities include using global positioning systems to determine the immediate physical environment (indoor/outdoor) and real-time monitoring of biological measurements (ambulatory blood pressure, heart rate). Furthermore, with constant updates in the design and wearability of devices, it is possible to monitor individuals for a long or even indefinite period of time, thus providing streams of data to improve prediction (e.g., by incorporating seasonal data).
An advantage of using EMA and wearable trackers is that data are collected in one’s natural environment in the immediate context with minimal interruption. However, it is not sufficient to simply rely on unmasked data from EMA and wearable trackers to improve an outcome, as demonstrated in the recent evidence from large-scale studies such as the IDEA Trial for weight control [36] and the Scripps Health study for healthcare cost and utilization control [37]. A variety of personal factors, e.g., motivation, preference, stage of change, will need to be accounted for in a behavioral framework for personalized informatics and engagement [38,39]. The TRIMM trial has demonstrated that accommodating personal factors in the delivery of data-driven insights through text messaging can help users to achieve better outcome in weight control [40]. As natural observation records are often lengthy, it is important to develop ideographic approaches that can provide highly relevant, person-specific insights.
In this paper, we thus focused on developing “simple” N-of-1 models to capture the personal-specific insights, e.g., individualized stress-behavior pathways, from observational data collected in user’s natural environment. However, it is conceivable that the response to EMA and even the awareness of being monitored modifies the experience through reactive arrangements. It points to the utilization of behavioral intervention technologies, which harness mobile and web technologies to support health behaviors [41,42], as tools to adapt intervention based on behavior prediction. For example, with apps that allow individuals to set goals (e.g., 60% exercise rate), the apps can be tailored to intervene by increasing the “dose” of motivational messages and exercise reminders when a predicted risk factor is detected. Dose optimization methods have been extensively studied as a nomothetic approach [43], but could in theory be tailored to the specific predictors and barriers of a single participant, to determine the minimally effective dose or change needed to help each individual exercise regularly. To a broader extent, machine learning, statistical techniques and the concepts of artificial intelligence for N-of-1 modeling have recently been brought up to scale for the development and evaluation of adaptive behavioral intervention technologies (and behavioral intervention programs in general) [44,45].
Despite these methodological advances, the role of human insights could remain central in predicting behavior that can be intervened on. Choosing the factors to intervene on is a personal endeavor. Elements that can be easily modified in one individual may pose an insurmountable challenge for another. In addition, the success of an intervention is likely to be affected by the number of elements that one should intervene upon. In the 79 participants, the N-of-1 models on average consisted of 2 predictor variables. Even for the infrequent exercisers (Participant A) who did not have apparent conditions that could change the likelihood of exercising, a “null” model would suggest looking for additional predictors and perhaps for other variables to monitor, to determine if they are predictive of future exercise bouts. In this light, the smallness of a model has merits in personalized behavior prediction and intervention, regardless of how much data is available.
In the era of precision medicine and wellness, it has been conjectured that person-centric comparative effectiveness studies would be an important alternative of Randomized Control Trials. To achieve this, previous review has established the need to further develop N-of-1 approaches against an incoming stream of observational data [17,18,19]. However, before clinical integration, a number of considerations need to be addressed. First, as discussed, we need to start developing methods to construct simple N-of-1 models. Second, in scenarios wherein the confidence level of a N-of-1 model is too low for the direct consumption of insights, the proposed apps need to interactively learn more about the target individual [46]. Third, to link user’s internal motivators with sense-making support [47,48], the proposed apps should adopt positive psychology and help the target users to focus on their own reason for goal attainment. Finally, the proposed apps can guide users to explore the different intervention options through a self-experimentation framework, wherein the associations between the attempted intervention and target proxy outcomes are visualized to facilitate shared decision-making.
There are several limitations in this study. First, we used the commercial Fitbit Flex instead of a clinically validated actigraphy sensor, which had a considerably higher cost. Having said that, we and others have demonstrated that the Fitbit Flex is an accurate and reliable device for measuring physical activity [49,50]. Second, our study consists of a moderate-small cohort of healthy adults who resided in northern Manhattan, and one might think the results are not generalizable to the general population. As discussed above, the goal of N-of-1 study is not to produce generalizable results to the general population, but rather to benefit a particular individual. It is useful to remind oneself that an N-of-1 study aims to produce knowledge that is beneficial to the universe of 1. From another angle, the analytical methods (N-of-1 trees) examined in this paper are generalizable at a population level and aim to bring about a new paradigm of how we build personalized prediction models.
6. CONCLUSIONS
In this paper, we describe analyses using data from a longitudinal study to build personalized prediction of exercise behavior with input variables of different nature, including stress experience (emotional), expectation of exercise (self-determination), exercise patterns in the previous days (behavioral), and other external and environmental factors such as day of the week, temperature, precipitation, and daylight time. By constructing simple N-of-1 models, we identified individual differences in stress-behavior pathways. In addition, we verified the hypothesis that an ideographic N-of-1 model could better capture individual stress-behavior pathways, compared to the traditional one-size-fits-all nomothetic model.
In summary, we illustrate the plausibility of stress-behavior pathway modulation made possible by mobile health technology, as well as the potential to adapt optimal behavioral interventions in practice with objective data-driven criteria. Moreover, we discuss possible solutions to integrate person-centric insights in a counseling setting with N-of-1 models. Our study offers optimism and preliminary evidence that small idiographic models digest the data as well as, or better than, a large nomothetic alternative.
References
- 1.Garcia MC, Bastian B, Rossen LM, et al. Potentially preventable deaths among the five leading causes of death—United States, 2010 and 2014. MMWR Morb Mortal Wkly Rep. 2016;65:1245–1255. doi: 10.15585/mmwr.mm6545a1. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Global health risks: Mortality and burden of disease attributable to selected major risks. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
- 3.Cheung YK, Moon YP, Kulick ER, et al. Leisure-time physical activity and cardiovascular mortality in an elderly population in northern Manhattan: a prospective cohort study. J Gen Intern Med. 2017;32:168–174. doi: 10.1007/s11606-016-3884-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Després J-P, Fullerton HJ, Howard VJ, Huffman MD, Isasi CR, Jiménez MC, Judd SE, Kissela BM, Lichtman JH, Lisabeth LD, Liu S, Mackey RH, Magid DJ, McGuire DK, Mohler ER, III, Moy CS, Muntner P, Mussolino ME, Nasir K, Neumar RW, Nichol G, Palaniappan L, Pandey DK, Reeves MJ, Rodriguez CJ, Rosamond W, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Woo D, Yeh RW, Turner MB on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2016 Update: a report from the American Heart Association. Circulation. 2016;133:447–454. doi: 10.1161/CIR.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 5.Marcus BH, Forsyth LH, Stone EJ, Dubbert PM, McKenzie TL, Dunn AL, Blair SN. Physical activity behavior change: Issues in adoption and maintenance. Health Psychology. 2000;19:32–41. doi: 10.1037/0278-6133.19.suppl1.32. [DOI] [PubMed] [Google Scholar]
- 6.Linke SE, Gallo LC, Norman GJ. Attrition and adherence rates of sustained vs. intermittent exercise interventions. Ann Behav Med. 2011;42:197–209. doi: 10.1007/s12160-011-9279-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pratt M, Epping J, Dietz W. Putting physical activity into public health: A historical perspective from the CDC. Preventive Medicine. 2009;49(4):301–302. doi: 10.1016/j.ypmed.2009.06.011. [DOI] [PubMed] [Google Scholar]
- 8.Graboys TB, Lown B. Coffee, arrhythmias, and common sense. N Engl J Med. 1983;308:835–837. doi: 10.1056/NEJM198304073081409. [DOI] [PubMed] [Google Scholar]
- 9.Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exericise. Sports Med. 2014;44:81–121. doi: 10.1007/s40279-013-0090-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oman RF, King AC. The effect of life events and exercise program format on the adoption and maintenance of exercise behavior. Health Psychol. 2000;19:605–612. doi: 10.1037//0278-6133.19.6.605. [DOI] [PubMed] [Google Scholar]
- 11.Holmes SD, Krantz DS, Rogers H, Gottdiener J, Contrada RJ. Mental stress and coronary artery disease: A multidisciplinary guide. Prog Cardiovasc Dis. 2006;49:106–122. doi: 10.1016/j.pcad.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 12.Selye H. The Stress of Life. New York: McGraw-Hill; 1956. [Google Scholar]
- 13.Lazarus R. Psychological stress and the coping process. New York: McGraw-Hill; 1996. [Google Scholar]
- 14.Barlow DH, Hersen M, Hartmann DP, Kazdin AE. Single case experimental designs: strategies for studying behavior change. Allyn and Bacon; 1984. [Google Scholar]
- 15.Barlow DH, Nock M, Hersen M. Single case experimental designs: strategies for studying behavior for change. Pearson/Allyn and Bacon; 2009. [Google Scholar]
- 16.Smith JD. Single-case experimental designs: a systematic review of published research and current standards. Psychological Methods. 2012;17(4):510–50. doi: 10.1037/a0029312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lillie EO, Patay B, Diamant J, Issell B, Topol EJ, Schork NJ. The n-of-1 clinical trial: the ultimate strategy for individualizing medicine? Personalized Medicine. 2011;8(2):161–173. doi: 10.2217/pme.11.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kravitz RL, Duan N, editors. and the DEcIDE Methods Center N-of-1 Guidance Panel. Design and Implementation of N-of-1 Trials: A User’s Guide. 14. Vol. 13. Rockville, MD: Agency for Healthcare Research and Quality; 2014. AHRQ Publication. [Google Scholar]
- 19.Shaffer JA, Falzon L, Cheung K, Davidson KW, Gabler N, Duan N, Bennett D. N-of-1 randomized trials for psychological and health behavior outcomes: a systematic review protocol. Systematic Reviews. 2015;4(1):87. doi: 10.1186/s13643-015-0071-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheung YK, Chakraborty B, Davidson KW. Sequential multiple assignment randomized trial (SMART) with adaptive randomization for quality improvement in depression treatment program. Biometrics. 2015;71:450–459. doi: 10.1111/biom.12258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bolger N, Davis A, Rafaeli E. Diary methods: capturing life as it is lived. Ann Rev Psychol. 2003;54:579–616. doi: 10.1146/annurev.psych.54.101601.145030. [DOI] [PubMed] [Google Scholar]
- 22.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 23.Kumar S, Nilsen WJ, Abernethy A, Atienza A, Patrick K, Pavel M, Riley WT, Shar A, Spring B, Spruijt-Metz D, Hedeker D, Honavar V, Kravitz R, Lefebvre D, Mohr DC, Murphy SA, Quinn C, Shusterman V, Swendeman D. Mobile health technology evaluation. Am J Prev Med. 2013;45:228–236. doi: 10.1016/j.amepre.2013.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Swan M. The Quantified Self: Fundamental Disruption in Big Data Science and Biological Discovery. Big Data. 2013;1(2):85–99. doi: 10.1089/big.2012.0002. [DOI] [PubMed] [Google Scholar]
- 25.Gray K, Martin-Sanchez FJ, Lopez-Campos GH, Almalki M, Merolli M. Person-generated Data in Self-quantification. Methods of Information in Medicine. 2016;55(6) doi: 10.3414/ME15-02-0006. [DOI] [PubMed] [Google Scholar]
- 26.Rosenberg M. Society and the adolescent self-image. Princeton, New Jersey: Princeton University Publishers; 1965. [Google Scholar]
- 27.Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. J Health Soc Behav. 1981;22:337–356. [PubMed] [Google Scholar]
- 28.Burg MM, Schwartz JE, Kronish IM, et al. Does stress result in you exercising less? Or does exercising result in you being less stressed? Or is it both? Testing the bi-directional stress-exercise association at the group and person (n of 1) level. Ann Behav Med. 2017 doi: 10.1007/s12160-017-9902-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ward DS, Evenson KR, Vaughn A, Rodgers AB, Troiano RP. Accelerometer use in physical activity: best practices and research recommendations. Med Sci Sports Exerc. 2005;37:S582–588. doi: 10.1249/01.mss.0000185292.71933.91. [DOI] [PubMed] [Google Scholar]
- 30.Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand. Quanity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 31.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 32.Smyth JM, Wonderlich SA, Sliwinski MJ, Crosby RD, Engel SG, Mitchell JE, Calogero RM. Ecological momentary assessment of affect, stress, and binge-purge behaviors: day of week and time of day effects in the natural environment. Int J Eat Disord. 2009;42(5):429–436. doi: 10.1002/eat.20623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moore RC, Depp CA, Wetherell JL, Lene EJ. Ecolgoical momentary assessment versus standard assessment instruments for measuring mindfulness, depressed mood, and anxiety among older adults. J Psychiatr Res. 2016;75:116–123. doi: 10.1016/j.jpsychires.2016.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Breiman L. Random forests. Machine Learning. 2001;45(1):5–32. [Google Scholar]
- 35.Cheung K, Duan N. Design of implementation studies for quality improvement programs: an effectiveness-cost-effectiveness framework. Am J Public Health. 2014;104(1):e23–e30. doi: 10.2105/AJPH.2013.301579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jakicic JM, Davis KK, Rogers RJ, King WC, Marcus MD, Helsel D, Belle SH. Effect of Wearable Technology Combined With a Lifestyle Intervention on Long-term Weight Loss. JAMA. 2016;316(11):1161–71. doi: 10.1001/jama.2016.12858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bloss CS, Wineinger NE, Peters M, Boeldt DL, Ariniello L, Kim JY, Topol EJ. A prospective randomized trial examining health care utilization in individuals using multiple smartphone-enabled biosensors. PeerJ. 2016;4:e1554. doi: 10.7717/peerj.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.King AC, Sallis JF. Why and how to improve physical activity promotion: Lessons from behavioral science and related fields. Preventive Medicine. 2009;49(4):286–8. doi: 10.1016/j.ypmed.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hsueh PS, Chang H, Ramakrishnan S. Next Generation Wellness: A Technology Model for Personalizing Healthcare. In: Weaver CA, Ball M, Kim G, Kiel JM, editors. Healthcare information Management Systems. 4. Springer International Publishing; 2016. pp. 356–74. [Google Scholar]
- 40.Lin M, Mahmooth Z, Dedhia N, Frutchey R, Mercado CE, Epstein DH, O’Brien MS. Tailored, interactive text messages for enhancing weight loss among African American adults: the TRIMM randomized controlled trial. The American Journal of Medicine. 2015;128(8):896–904. doi: 10.1016/j.amjmed.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 41.Mohr DC, Burns MN, Schueller SM, Clarke G, Klinkman M. Behavioral intervention technologies: evidence review and recommendations for future research in mental health. Gen Hosp Psychiatry. 2013;35(4):332–338. doi: 10.1016/j.genhosppsych.2013.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mohr DC, Cheung K, Schueller SM, Brown CH, Duan N. Continuous evaluation of evolving behavioral intervention technologies. Am J Prev Med. 2013;45(4):517–523. doi: 10.1016/j.amepre.2013.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cheung YK. Dose Finding by the Continual Reassessment Method. Chapman Hall/CRC Press; 2012. [Google Scholar]
- 44.Cheung YK, Yu G, Wall MM, Sacco RL, Elkind MSV, Willey JZ. Patterns of leisure-time physical activity using multivariate finite mixture modeling and cardiovascular risk factors in the Northern Manhattan Study. Annals of Epidemiology. 25:469–474. doi: 10.1016/j.annepidem.2015.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hsueh PS, Zhu X, Deng V, Ramarishnan S, Ball M. Dynamic and accretive composition of patient engagement instruments for personalized plan generation. Studies in Health Technology and Informatics. 2014 [PubMed] [Google Scholar]
- 46.Mamykina L, Smaldone AM, Bakken SR. Adopting the sensemaking perspective for chronic disease self-management. Journal of Biomedical Informatics. 2015;56:406–417. doi: 10.1016/j.jbi.2015.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McGillicuddy JW, Gregoski MJ, Weiland AK, Rock RA, Brunner-Jackson BM, Patel SK, Treiber FA. Mobile Health Medication Adherence and Blood Pressure Control in Renal Transplant Recipients: A Proof-of-Concept Randomized Controlled Trial. JMIR Research Protocols. 2013;2(2):e32. doi: 10.2196/resprot.2633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Karkar R, Zia J, Vilardaga R, Mishra SR, Fogarty J, Munson SA, Kientz JA. A framework for self-experimentation in personalized health. Journal of the American Medical Informatics Association. doi: 10.1093/jamia/ocv150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Diaz KM, Krupka DJ, Chang MJ, Peacock J, Ma Y, Goldsmith J, Schwartz JE, Davidson KW. Fitbit®: An accurate and reliable device for wireless physical activity tracking. Int J Cardiol. 2015;185:138–140. doi: 10.1016/j.ijcard.2015.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Evenson KR, Goto MM, Furberg RD. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int J Behav Nutr Phys Act. 2015;12:159. doi: 10.1186/s12966-015-0314-1. [DOI] [PMC free article] [PubMed] [Google Scholar]