Abstract
Purpose
We examined the ambulatory health care visit utilization of spina bifida children, adults who transitioned to adult care, and adults who continued to seek care in a pediatric setting.
Methods
We evaluated utilization over a one-year period for SB patients who visited any outpatient medical clinic within an integrated health care system. Patients were categorized as pediatric (<18) or adult (≥ 18). Adults were divided into those who did not fully transition to adult care (DNT) and patients who fully transitioned (adult). Frequency and type of health care utilization were compared. Sub-analysis was performed for patients aged 18–25 to examine variables associated with successful complete transition to adult care.
Results
Over one year, 382 children, 88 DNT, and 293 adult SB patients had 4,931 clinic visits. Children had greater ambulatory care utilization (7.25 visits/year) compared to fully transitioned adults (5.33 visits/year, p=0.046). Children more commonly visited surgery clinics (52.3% of visits) and adults more commonly visited medical clinics (48.9%) (p<0.005). Adult transitioned patients were more likely to be female (p=0.004). Of patients 18–25 years old, those who did not transition to adult care had similar outpatient visit types but higher utilization of inpatient and emergency care than those who transitioned.
Conclusions
SB children utilized more ambulatory care than adults and were more likely to visit a surgical specialist. Adult SB patients who successfully transitioned to adult care were more likely to be female and patients who failed to transition were more likely to have more inpatient and emergency care.
Keywords: Transitional Care, Spina Bifida, Myelomeningocele, Ambulatory Care
Introduction
With improved medical and surgical care, 85% of patients with spina bifida (SB) are now living well into adulthood.1 For the first time, there are now more adults living with SB than children.1–4 These patients have complex health care needs requiring multi-subspecialty care coordination throughout their lives. Consistent care in the outpatient setting is thought to help these patients stay healthy and avoid potentially preventable adverse outcomes that require hospitalizations, surgeries, or emergency department visits.2–5 Age-appropriate care can also help patients achieve their fullest potential as adults.6 However, it is well-known that transitioning patients from the pediatric to adult setting can be problematic, with many patients never transitioning and others becoming lost to follow-up altogether.7,8 As such, there has been great effort to improve transitional care from many major medical organizations.6,9,10
A major limiting factor to implementing effective transitional care is our poor understanding of exactly what care these patients need. Their health care needs undoubtedly evolve and change over their lifetime. Since the aging SB patient is a relatively new phenomenon, these changes remain poorly defined. While there are reports on how patterns of inpatient admissions, emergency department visits, and surgical utilization of these patients change as they age,2,4,5,11,12 an understanding of their outpatient care utilization is lacking. Additionally, the utilization of patients who do not transition may be different from those who do, but these differences remain unclear. An improved understanding of both the ambulatory care utilization of SB patients across a life course and the utilization unique to the patients who do not transition can help providers better structure and facilitate patient-centered transitional care.
We sought to gain a better understanding of the ambulatory health care utilized by the following populations of people with SB: children, adults who fully transitioned to adult care, and adults who have not transitioned. There are two aims of this study. The primary aim is to compare the type and frequency of non-emergent outpatient health care utilization between those three groups: what providers do they see and how often? We hypothesize that the utilization remains consistent over time, with adults seeing the same types of providers with the same frequency as children. For our second aim, we performed a subset analysis on all young adult patients (ages 18–25) to examine utilization differences between patients who did and did not transition at a center that currently lacks a formal transition process. We hypothesize that those young adult patients who do not transition have significantly higher utilization of all types of care than those who have successfully transitioned. This knowledge will help determine what transitional care model may be most effective for patients with SB, both at our institution and beyond.
Materials and Methods
After approval from the Institutional Review Board at the University of Michigan, we used an international classification of diseases coding algorithm to identify all ambulatory care visits made by a patient with SB to any department within a single integrated health system over a one-year period between 2012–2013. This identified all visits made by a SB patient, whether or not the chief complaint or diagnosis code for the encounter was directly related to their SB status. A chart review was performed to confirm the diagnosis for all patients. Both the pediatric and adult hospitals are a part of the same institution and use the same electronic medical record, allowing us to track all visits across both hospitals.
An ambulatory care visit was defined as any visit in which the patient was cared for by a therapist, advanced practitioner, or physician. Visits for ancillary diagnostic studies such as lab draws, imaging studies, and other clinic procedures were excluded. Similarly, emergency room visits, surgical procedures, and inpatient admissions were excluded from the ambulatory care visit definition and were recorded separately. The visits were categorized into surgical, medical, and therapy visits based on the type of provider seen. A child was defined as a patient younger than age 18; a patient who did not transition (DNT) was defined as a patient 18 or older (no upper age limit) who was still seen in at least one pediatric clinic; an adult was defined as a patient 18 or older seen exclusively in adult clinics. The age of 18 was chosen due to an institutional policy that all patients 18 and older must be seen in the adult emergency department. Currently, there is no formal process or target age for transition of our SB patients. Instead, each individual physician determines the timing of transition for each patient.
For our primary analysis, we compared the number of visits and type of clinics visited between the pediatric, DNT, and adult patients. For our secondary analysis, we looked at all patients ages 18–25 years, which is the time when transition often occurs. We excluded both DNT and adult patients older than 25. After identifying within this cohort those patients who had transitioned and those who had not, we compared the number of non-emergent ambulatory care visits over the one-year period. We then evaluated for ongoing issues that could impact transition readiness in this group of 18–25 year olds. Specifically, we determined the number of hospital admissions, emergency department visits, and surgeries these patients had over a two-year period between 2011–2013. We compared the results between those who had or had not yet transitioned. We also evaluated possible sociodemographic factors that could impact transition readiness such as proximity to the hospital and insurance status.
Analysis was performed using parametric and non-parametric bivariate analysis including chi square, t-test, Wilcoxon Rank Sum, and Kruskal-Wallis Test. All analysis was performed using STATA® version 14.
Results
There were 4931 ambulatory care visits to 76 different clinics among 763 patients with SB over a one-year period. Patient demographics for the entire cohort are detailed in Table 1. Adult, fully transitioned patients were more likely to be female compared to both the DNT and the pediatric patients (69% vs 55% vs 57%, p=0.004). The most commonly visited clinics for each group of patients are listed in Table 2.
Table 1.
Demographics of all spina bifida patients. DNT, patients who did not transition.
| Children | DNT | Adults | P-value | ||
|---|---|---|---|---|---|
| Number of Patients | 382 | 88 | 293 | ||
| Total Number of Visits | 2769 | 599 | 1563 | ||
|
Mean age, years (SD) Range Median |
7.65 (SD 5.24) Range 1–17 4 |
24.10 (SD 7.20) Range 18–54 21.5 |
40.63 (SD 13.16) Range 18–81 39 |
||
| Gender | Male | 163 (42.7%) | 40 (45.5%) | 92 (31.4%) | P=0.004 |
| Female | 219 (57.3%) | 48 (54.5%) | 201 (68.6%) | ||
| Race | White | 339 (88.7%) | 72 (81.8%) | 244 (83.3%) | P=0.036 |
| Black | 14 (3.7%) | 10 (11.4%) | 28 (9.6%) | ||
| Hispanic | 11 (2.9%) | 4 (4.6%) | 5 (1.7%) | ||
| Other | 12 (3.1%) | 1 (1.1%) | 12 (4.1%) | ||
| Unknown | 6 (1.6%) | 1 (1.1%) | 4 (1.4%) | ||
|
Mean number of visits per person (SD) Range Median |
7.25 (SD 7.95) Range 1–50 4 |
6.80 (SD 7.97) Range 1–42 4 |
5.33 (SD 5.71) Range 1–37 3 |
P=0.046 |
Table 2.
Most common clinics visited by group.
| Pediatric (n=2769) | DNT (n=599) | Adult (n=1563) |
|---|---|---|
|
| ||
| Neurosurgery (21.16%) | Therapy (13.36%) | Primary Care (15.29%) |
| Orthopedics (14.95%) | Urology (12.35%) | Therapy (11.39%) |
| Urology (8.85%) | Neurosurgery (8.68%) | Urology (10.36%) |
| Therapy (7.44%) | Orthopedics (7.51%) | Neurosurgery (8.45%) |
| Prosthetics (7.37%) | Primary care (7.51%) | Ob-gyn (4.67%) |
| Primary Care (6.86%) | Ob-gyn (6.68%) | Neurology (4.29%) |
| PM&R (4.66%) | PM&R (6.34%) | Prosthetics (4.29%) |
| Preop Clinic (3.29%) | Psychiatry/Psychology (4.51%) | PM&R (4.09%) |
| Ophthalmology (2.75%) | Preop Clinic (4.01%) | Psychiatry/Psychology (3.90%) |
| Psychiatry/Psychology (2.20%) | Wheelchair Clinic (3.84%) | Pain Clinic (3.71%) |
| Plastic Surgery (2.20%) | ||
Therapy includes physical, occupational, and speech therapy.
The utilization of ambulatory care among patients with SB differed significantly by age groups. Children had the greatest ambulatory care utilization with an average of 7.25 visits per year compared to fully transitioned adults who had the lowest utilization with 5.33 visits per year (p=0.046 for this trend). The distribution of visit types changed with age. While the utilization of therapy services remained stable in all groups, children most commonly visited surgical clinics, but DNT and fully transitioned adults most commonly visited medical clinics (p<0.005 for trend) (Figure 1). Interestingly, while 21.16% of all pediatric clinic visits are to neurosurgery, this drops to only 8.45% of adult visits. Conversely, 8.85% of pediatric visits are to urologists, but this increases slightly to 10.36% of adult visits. The greatest increase in need over time is for primary care: 6.86% of pediatric visits are for primary care, but this increases to 15.29% of adult visits.
Figure 1. Type of clinic visited by patient group.
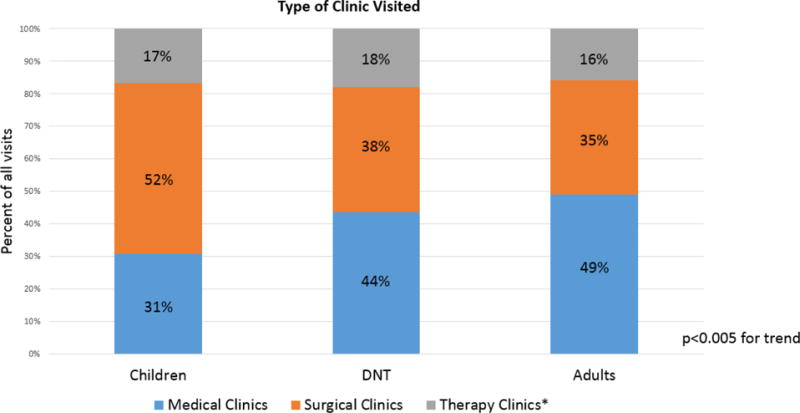
*Therapy Clinics include occupational, physical, and speech therapy, prosthetics clinic, wheelchair clinic, and wound/ostomy clinics.
Adult women had a higher average number of visits than adult men (5.91 SD 6.18 versus 4.07 SD 4.28, p<0.005). No differences in utilization by gender was appreciated for any other group. Although male and female adults utilized similar types of outpatient visit types in general, males were more likely to see a urologist [12.53% (47/375) of adult male visits versus 9.68% (115/1188) of adult female visits, p=0.085]. However, 6.14% (73/1188) of adult female visits were to an obstetrician-gynecologist.
The sociodemographic characteristics for the subset of patients who are the typical transitional age (18–25 years) are detailed in Table 3. There were 61 DNT patients this age (the remaining 27 DNT patients were older than 25) and 40 patients who had transitioned to adult care. Among this cohort, patients who had not transitioned were significantly younger than those who had transitioned (20.16 versus 22.5, p<0.001). There were no other significant demographic differences between the two groups.
Table 3.
Demographics of all spina bifida patients of typical transitional care age (18–25 years).
| Did not transition | Transitioned | P-value | ||
|---|---|---|---|---|
| Number of eligible Patients | 61 | 40 | ||
|
Mean age (years) Median |
20.16 (SD 2.18) 19 |
22.55 (SD 2.06) 24 |
<0.001 | |
| Gender | Male | 26 (42.6%) | 16 (40.0%) | 0.794 |
| Female | 35 (57.4%) | 24 (60.0%) | ||
| Race | White | 51 (83.6%) | 32 (80.0%) | 0.886 |
| Black | 7 (11.5%) | 5 (12.5%) | ||
| Hispanic | 1 (1.6%) | 0 (0%) | ||
| Other | 1 (1.6%) | 2 (5.0%) | ||
| Unknown | 1 (1.6%) | 1 (2.5%) | ||
| Insurance | Public | 18 (29.51%) | 17 (42.50%) | 0.331 |
| Private | 41 (67.21%) | 21 (52.50%) | ||
| None | 2 (3.28%) | 2 (5.00%) | ||
|
Mean distance from hospital (miles) Range Median |
70.27 (SD 63.80) Range 4.6–310 51.6 |
86.97 (SD 96.53) Range 11.8–459 53.5 |
0.550 | |
|
Mean number of visits Range Median |
6.92 (SD 8.51) Range 1–42 4 |
3.73 (SD 4.32) Range 1–19 2 |
0.031 | |
| Number of Visits | Medical Clinic | 166 (40.19%) | 62 (42.95%) | 0.593 |
| Surgical Clinic | 165 (39.95%) | 61 (40.94%) | ||
| Therapy Clinic | 82 (19.85%) | 2 (16.11%) |
There were several significant differences in total health care utilization among this subset of transitional-aged patients (Figure 2). Those who did not transition had a significantly higher utilization of outpatient and emergency care and tended to have more inpatient admissions and surgeries. There was no significant difference in the types of clinics they visited.
Figure 2.
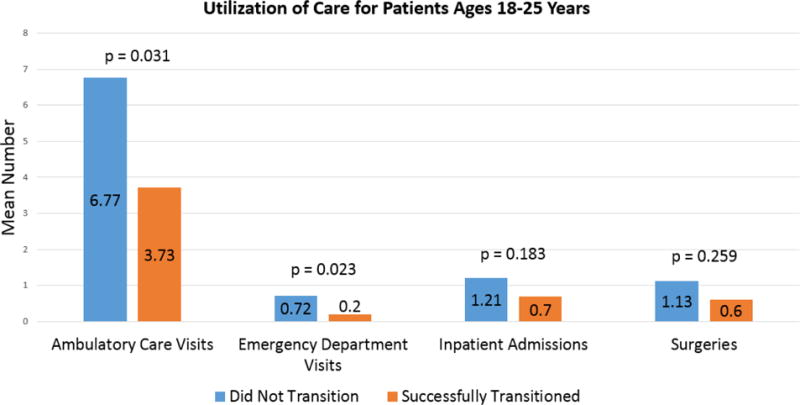
All health care utilization for transitional aged patients.
Discussion
In our institutional cohort, the ambulatory care utilization of patients with SB differed by age. Children required more frequent visits overall and most commonly to surgical providers. Conversely, adults required the fewest visits, but most visits were to medical providers. The need for urologic care remained consistently high while the need for neurosurgery and orthopedic surgery decreased. The need for primary care increased such that it was the most common adult outpatient visit. Patients ages 18–25 who did not transition had higher utilization of outpatient, inpatient, and emergency health care compared to patients that age who did transition. There was a significant change in the gender composition of the age groups over time, with an increase in the percentage of women in the adult group. Adult women also utilized ambulatory care significantly more often than adult men.
Children likely had higher utilization of outpatient surgically-based care for several reasons associated with growth and development. These children are monitored closely for evidence of tethered cord, changes in bladder dynamics and renal function, development of contractures, and evolving prosthetics and wheelchair needs during periods of linear growth. These findings parallel those of Bowles et al13 who reported that the health care costs of patients with SB are highest in childhood due to greater utilization during this time.
There could be many factors that explain why more adult women sought care and had higher utilization then men. Potentially they could have greater medical needs requiring more care such as gynecologic concerns including menstrual issues, pregnancy, or pelvic organ prolapse. Men may also be less likely than women to access health care.14 Other studies have also reported a higher proportion of females in adult SB clinics, although to a lesser degree than seen in this study.5,15,16 The greater difference seen in this cohort may be due to the lack of a transitional care process, which may disproportionally effect men. This could indicate a need to more intentionally keep men engaged in their medical care during the transitional process and in adulthood. Since adult men are high utilizers of urologic care, we are well positioned to help encourage them to seek regular preventative care.
The higher utilization of all health care among patients who did not transition may indicate ongoing medical or surgical concerns that make transition difficult for both the patients and the providers. The patients may want a provider that knows them well and has given them consistent care during a difficult or uncertain time.8,17 Pediatric providers may be reluctant to refer their patients to adult providers when there are active issues that have not been optimized.8 These patients could have other factors that increase their complexity and complicate transition, such as a severe physical or intellectual disability. These patients would likely benefit from a more customized transitional process to ensure continuity of their care. Additionally, patients who did not transition were younger than those who did, which could suggest that 18 may not be a practical cut-off for transition. No matter what age is chosen for transition, pediatric providers need to identify adult provider colleagues who can manage complex issues, although such providers can be very difficult to find.11,18
This study suggests that the optimal clinic model for pediatric patients may not be as effective for adults. Multidisciplinary clinics, often with a urologist, neurosurgeon, orthopedic surgeon, and physical medicine and rehabilitation physician have proven effective in the pediatric setting.19 With high utilization of surgical care during childhood, this model is logical for young patients. However, with the decreasing need for surgical specialists and increasing need for primary care physicians in adulthood, a more effective transitional and adult model for these patients may be a primary care medical home. Some clinics have reported success with such a model run by medicine-pediatric physicians who specialize in care of patients with congenital anomalies.20 These physicians make referrals to sub-specialists as needed. Such clinics may be better equipped to provide the more holistic approach patients and families are accustomed to in the pediatric setting by addressing career goals, psychosocial changes, and social work needs.10,17,18,20 For patients with disabilities, a medical home can provide increased access to subspecialty care, less inpatient and emergency department utilization, fewer unmet medical and support service needs, and decreased family financial burden.18
Undoubtedly this model will not fit for all institutions. When designing a transitional care clinic, providers should seek to deliver the best care possible working within the strengths and restraints unique to their institution.21 Additionally, not all patients will have local access to resources. For some, it will be most practical to receive primary care from a local physician who communicates with specialists. In order to make this feasible, there needs to be more adult medical providers equipped to care for these patients. Currently, over 70% of adults with SB have difficulty accessing medical care.11 Many adult providers feel uncomfortable caring for these patients due to a lack of training.22 They may be least willing to care for SB patients out of all patients with chronic pediatric disorders.22 However, these adult providers have reported that good communication with subspecialists help them feel better equipped to provide quality care to these patients.23 As urologists, we consistently care for these patients throughout their lives. Therefore, we have the opportunity to provide such communication and education so adult primary care doctors may be more willing to care for SB patients.
There are several limitations to this study. This is a single-institution study at a tertiary referral center which serves as a referral center of excellence for SB care. Therefore, the utilization patterns are reflective of the referral patterns of this institution. Physicians in a community setting may not have as ready access to specialties and utilization may reflect this. Additionally, the study does not account for patients who do not get all their care at this institution and as a result may under-report ambulatory utilization. Anecdotally, most of our patients choose to receive care at our institution exclusively due to the complexity of their diagnosis. Finally, while this study does account for patients who did not follow-up with urologists but did get care from other providers, it does not account for those patients who fail to follow-up altogether.
Improved understanding of the changes in ambulatory care needs of SB patients can help providers model more patient-centered transitional care clinics. No matter the model used, urologists should be a leader in the process.
Conclusion
The ambulatory care utilization of patients with SB changes as they age, with a higher utilization of surgical subspecialty services during childhood and a shift to higher utilization of medical services during adulthood. Patients who do not transition have significantly higher utilization of all care compared to those who successfully transition. This knowledge can inform the model and process for patient-centered transitional care.
Sources
- 1.Shin M, Kucik JE, Siffel C, et al. Improved survival among children with spina bifida in the United States. The Journal of pediatrics. 2012;161:1132–7. doi: 10.1016/j.jpeds.2012.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kinsman SL, Doehring MC. The cost of preventable conditions in adults with spina bifida. European journal of pediatric surgery: official journal of Austrian Association of Pediatric Surgery [et al] = Zeitschrift fur Kinderchirurgie. 1996;6(Suppl 1):17–20. doi: 10.1055/s-2008-1071031. [DOI] [PubMed] [Google Scholar]
- 3.Wilson R, Lewis SA, Dicianno BE. Targeted preventive care may be needed for adults with congenital spine anomalies. PM & R: the journal of injury, function, and rehabilitation. 2011;3:730–8. doi: 10.1016/j.pmrj.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 4.Young NL, Steele C, Fehlings D, Jutai J, Olmsted N, Williams JI. Use of health care among adults with chronic and complex physical disabilities of childhood. Disability and rehabilitation. 2005;27:1455–60. doi: 10.1080/00222930500218946. [DOI] [PubMed] [Google Scholar]
- 5.Liu JS, Greiman A, Casey JT, Mukherjee S, Kielb SJ. A snapshot of the adult spina bifida patient - high incidence of urologic procedures. Central European journal of urology. 2016;69:72–7. doi: 10.5173/ceju.2016.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110:1304–6. [PubMed] [Google Scholar]
- 7.Grimsby GM, Burgess R, Culver S, Schlomer BJ, Jacobs MA. Barriers to transition in young adults with neurogenic bladder. Journal of pediatric urology. 2016;12:258.e1–5. doi: 10.1016/j.jpurol.2016.04.015. [DOI] [PubMed] [Google Scholar]
- 8.Binks JA, Barden WS, Burke TA, Young NL. What do we really know about the transition to adult-centered health care? A focus on cerebral palsy and spina bifida. Archives of physical medicine and rehabilitation. 2007;88:1064–73. doi: 10.1016/j.apmr.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 9.Healthy People. National Center for Health Statistics, Centers for Disease Control and Prevention; 2010. [Google Scholar]
- 10.Rosen DS, Blum RW, Britto M, Sawyer SM, Siegel DM. Transition to adult health care for adolescents and young adults with chronic conditions: position paper of the Society for Adolescent Medicine. The Journal of adolescent health: official publication of the Society for Adolescent Medicine. 2003;33:309–11. doi: 10.1016/s1054-139x(03)00208-8. [DOI] [PubMed] [Google Scholar]
- 11.Liptak GS, Robinson LM, Davidson PW, et al. Life course health and healthcare utilization among adults with spina bifida. Developmental medicine and child neurology. 2016;58:714–20. doi: 10.1111/dmcn.12952. [DOI] [PubMed] [Google Scholar]
- 12.Mann JR, Royer JA, Turk MA, et al. Inpatient and emergency room visits for adolescents and young adults with spina bifida living in South Carolina. PM & R: the journal of injury, function, and rehabilitation. 2015;7:499–511. doi: 10.1016/j.pmrj.2014.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bowles D, Wasiak R, Kissner M, et al. Economic burden of neural tube defects in Germany. Public health. 2014;128:274–81. doi: 10.1016/j.puhe.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 14.Smith JA, Braunack-Mayer A, Wittert G. What do we know about men’s help-seeking and health service use? The Medical journal of Australia. 2006;184:81–3. doi: 10.5694/j.1326-5377.2006.tb00124.x. [DOI] [PubMed] [Google Scholar]
- 15.Duplisea JJ, Romao RL, MacLellan DL, Cox AR, Anderson PA. Urological Follow-up in Adult Spina Bifida Patients: Is There an Ideal Interval? Urology. 2016;97:269–72. doi: 10.1016/j.urology.2016.06.025. [DOI] [PubMed] [Google Scholar]
- 16.Hopson B. Spina bifida transition to adulthood-the genesis of a program. Third World Congress on Spina Bifida Research & Care. 2017 [Google Scholar]
- 17.Woodhouse CR, Neild GH, Yu RN, Bauer S. Adult care of children from pediatric urology. The Journal of urology. 2012;187:1164–71. doi: 10.1016/j.juro.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 18.Murphy NA, Carbone PS. Parent-provider-community partnerships: optimizing outcomes for children with disabilities. Pediatrics. 2011;128:795–802. doi: 10.1542/peds.2011-1467. [DOI] [PubMed] [Google Scholar]
- 19.Kaufman BA, Terbrock A, Winters N, Ito J, Klosterman A, Park TS. Disbanding a multidisciplinary clinic: effects on the health care of myelomeningocele patients. Pediatric neurosurgery. 1994;21:36–44. doi: 10.1159/000120812. [DOI] [PubMed] [Google Scholar]
- 20.Berens JC, Peacock C. Implementation of an academic adult primary care clinic for adolescents and young adults with complex, chronic childhood conditions. Journal of pediatric rehabilitation medicine. 2015;8:3–12. doi: 10.3233/PRM-150313. [DOI] [PubMed] [Google Scholar]
- 21.Joseph D. Transitioning Care in Spina Bifida, Panel Discussion: Urologic Congenitalism: Successful transition from childhood to adulthood. SPU/AUA Annual Meeting San Diego. 2016 [Google Scholar]
- 22.Patel MS, O’Hare K. Residency training in transition of youth with childhood-onset chronic disease. Pediatrics. 2010;126(Suppl 3):S190–3. doi: 10.1542/peds.2010-1466P. [DOI] [PubMed] [Google Scholar]
- 23.Okumura MJ, Kerr EA, Cabana MD, Davis MM, Demonner S, Heisler M. Physician views on barriers to primary care for young adults with childhood-onset chronic disease. Pediatrics. 2010;125:e748–54. doi: 10.1542/peds.2008-3451. [DOI] [PubMed] [Google Scholar]


