Abstract
Objectives
One of the main objectives of the Targeted Subsidies Law (TSL) in Iran was to improve equity in healthcare financing. This study aimed at measuring the effects of the TSL, which was implemented in Iran in 2010, on equity in healthcare financing.
Methods
Segmented regression analysis was applied to assess the effects of TSL implementation on the Gini and Kakwani indices of outcome variables in Iranian households. Data for the years 1977-2014 were retrieved from formal databases. Changes in the levels and trends of the outcome variables before and after TSL implementation were assessed using Stata version 13.
Results
In the 33 years before the implementation of the TSL, the Gini index decreased from 0.401 to 0.381. The Gini index and its intercept significantly decreased to 0.362 (p<0.001) 5 years after the implementation of the TSL. There was no statistically significant change in the gross domestic product or inflation rate after TSL implementation. The Kakwani index significantly increased from -0.020 to 0.007 (p<0.001) before the implementation of the TSL, while we observed no statistically significant change (p=0.81) in the Kakwani index after TSL implementation.
Conclusions
The TSL reform, which was introduced as part of an economic development plan in Iran in 2010, led to a significant reduction in households’ income inequality. However, the TSL did not significantly affect equity in healthcare financing. Hence, while measuring the long-term impact of TSL is paramount, healthcare decision-makers need to consider the efficacy of the TSL in order to develop plans for achieving the desired equity in healthcare financing.
Keywords: Equity, Healthcare financing, income inequality, Social justice, Targeted Subsidies Law, Segmented regression analysis
INTRODUCTION
Spiraling healthcare expenditures, due to expensive modern medical technologies and citizens’ ever-increasing expectations, may lead to challenges such as catastrophic health expenditures and inequality in access to healthcare [1]. Health systems have been attempting to improve and maintain population welfare through contextually appropriate models of healthcare financing. Nevertheless, financial shortages have consistently hampered the achievement of these objectives [2]. Ensuring equity in health financing is an important objective of healthcare systems [3]. Many studies in recent years in developing countries, including Iran, have emphasized the importance of equity in healthcare financing [4,5].
The main source of primary healthcare financing in Iran is the public sector. The private and public sectors simultaneously provide secondary and tertiary service delivery and financing [4]. Thus, healthcare financing in Iran is complex and multifaceted. Despite reforms to improve equity in healthcare financing, such as the implementation of a family physician program and, recently, the Health Transformation Plan [6], the proportion of out-of-pocket healthcare expenditures is still high [7,8]. Healthcare financing indicators, such as out-of-pocket and catastrophic health expenditures, did not show a clear trend or status, and were not at appropriate levels in Iran during the last decades [9,10]. For instance, approximately 58% of health expenditures were out-of-pocket in 2001, and 10 years later, in 2011, this figure decreased to 52% [8]. Moreover, several national-level studies have shown that the concentration index (CI) for capacity to pay and healthcare payments implied inequality [5,11] and that annually, healthcare expenditures caused almost 1.8% of the society’s population fall below the poverty line [12]. The fair financing contribution index in 2006 was approximately 0.854, and it dropped to 0.842 in 2011 [13]. In general, these measures indicate the complexity and multidimensionality of healthcare financing in Iran.
Recently, the Iranian government has focused attention on ensuring equitable healthcare financing by developing the Targeted Subsidies Law (TSL). The TSL was the most important economic reform in Iran after the Islamic Revolution in 1978, and made Iran the first major oil-exporting country to substantially reduce implicit energy subsidies [14]. The implementation of the TSL began in 2010, when the government eliminated energy subsidies (i.e., the subsidy for gas and oil) and replaced them with cash payments to eligible citizens. As a result of this reform, domestic energy and agricultural prices increased by up to 20 times [14]. In the first 12 months following TSL implementation (December 2011), approximately USD 30 billion in freely usable cash was distributed to Iranian households, and another USD 10-15 billion will have been advanced to enterprises to finance investment in restructuring aimed at reducing energy intensity. Additionally, during this time, the reform planned to raise only an estimated 200 trillion rials (USD 20 billion) in additional revenues to compensate for price increases [14,15].
One of the main purposes of the TSL was to reduce income inequality by decreasing the income gap across deciles, aiming to combat and reduce poverty [16]. Paragraph B of Article 7 of the TSL directly notes the government is bound to implement a comprehensive social security system for the targeted population, by taking measures such as: (1) providing and expanding social insurance and healthcare services, and ensuring and enhancing public health and medical coverage for special and difficult-to-cure diseases; (2) providing assistance for financing housing costs, enhancing resistance of buildings, and creating employment; and (3) empowering and implementing social support programs by allocating funds from rising prices for energy carriers to the health sector in order to ensure equity in healthcare financing [17].
A qualitative study reported the challenges posed by the unpredictability of healthcare financing in Iran [18] to be one of the reasons for high out-of-pocket payments. The government of Iran introduced the TSL to ensure a more sustainable and equitable healthcare financing system, among other goals. Little evidence is available to demonstrate the impact of the TSL on equity in healthcare financing in Iran. This study aimed to measure the effects of TSL implementation on income inequality and equity in healthcare financing in Iran.
METHODS
Study Setting
Iran is a middle-income country of almost 80 million citizens that is located in west Asia. The gross national income per capita for Iran is about 15.410 purchasing power paritie dollars and total health expenditures account for approximately 6.9% of the gross domestic product (GDP). The total expenditure on health per capita (international $, 2014) is 1.082 [19].
Based on what is articulated in upstream documents, such as the Law of the Fourth Economic, Social, and Cultural Development Plan, improving equity in healthcare financing is one of the main goals of the Iranian health system [20]. The TSL, which was implemented in 2010, is considered to be one of the reforms that covered entire social sectors, such as the healthcare system, with the aim of ensuring equity.
Study Design
Segmented regression analysis, a powerful method of interrupted time series analysis [21], was conducted to estimate the effect of the TSL on income inequality and equity in healthcare financing. We used segmented regression analysis to assess the extent to which the TSL brought changes to these indicators immediately during the intervention period and over a longer time period (1977-2014). In this analysis, the time of the intervention was considered to be the changing point. We assumed that the TSL implementation had positive effects on equity in healthcare financing in Iran.
Variables
In this study, the Gini index (GI) and Kakwani index (KI) were the main outcome variables, while the GDP, inflation rate (InR), infant mortality rate (IMR), and the proportion of the population 60 years old (PoU60) and above were the control variables. The data for the years 1977 to 2014 were retrieved from the annual household income-expenditures survey reports of the National Statistics Center of Iran, the Ministry of Health and Medical Education, and the World Bank’s official website. The annual household income-expenditures survey data of the National Statistics Center of Iran are believed to be of the required quality. These data have also been used by other studies on healthcare equity and household expenditures on healthcare [4]. The data include detailed measures of household expenditures on goods and services such as healthcare, as well as household income. The healthcare expenditure data distinguish consumer co-payments from health insurance premiums, enabling us to calculate inequality measures for these 2 items separately, as well as together [4,12].
The GI was computed using the annual household income-expenditures survey reports and the annual aggregated number of households from 1977 to 2014. This was carried out as a preliminary analysis to determine the effect of the TSL on income inequality using segmented regression analysis. The GI can be mathematically expressed as follows:
| (1) |
Where the GI represents the aggregated GI; yi is the ith decile of household income, yi+1 is the (i+1)th decile of the next household income, χi is the number of households, and χi+1 is the number of the next households in the (i+1)th decile [22].
Furthermore, the KI, which shows the progressivity of healthcare financing, was calculated using the following formula.
Where CI is the concentration index and GI is the Gini index. The CI, which is a widely applied technique in health economic studies [23], was calculated to measure the inequality in total household expenditures on healthcare from 1988 to 2014. This period was used because household expenditures on healthcare data as deciles were available starting in 1988. This index corresponds to the area between the concentration curve and the perfect equality line (45°). A CI of 0 shows an absence of inequality between the rich and the poor; a positive value indicates that the concentration curve lies below the perfect equality line, implying a pro-rich inequality; and a negative value shows inequality in favor of the poor [24]. Overall, the CI can be represented mathematically as follows [25]:
| (2) |
Where P represents the cumulative percentage declines in population income and L household expenditures on healthcare, respectively.
The KI was calculated from the GI and CI models presented in equations 1 and 2, respectively, as a basis for the segmented regression analysis. The computed KI values range from -2 to 1. A value of -2 shows severely regressive healthcare financing and a value of 1 indicates strongly progressive healthcare financing [25]. Generally, the area between the concentration curve and the Lorenz curve represents the KI [25].
Control Variables
The GDP is one of many macroeconomic indicators, and it usually has an effect on other economic variables [24]. The InR is another independent variable that can affect other economic variables. The InR in Iran has been very high during the past 3 decades [26]. High inflation can occur when there is an imbalance between the availability of commodities in society and the amount of cash in circulation. It can also be affected by economic reforms. Hence, the annual GDP and 12-month average InR for the years 1977-2014 were used as control variables for the analysis.
Furthermore, the number of deaths among under-1-year-old children per 1000 live births (the IMR) for the years 1977-2014 and the proportion of people aged 60 years and above for the years 1988-2014 were included in our analysis as control variables related to health system outcome indicators.
Modeling the Segmented Regression Analysis
We used the backward approach to estimate the effect of the TSL on income inequality and equity in healthcare financing. Initially, the GI was calculated to estimate the effect of the TSL on total income inequality. This is mathematically presented as follows:
| (3) |
Where yGIt represents the GI at year t, tbefor is the GI trend before the intervention, ccafter is the change in the intercept changes of the GI after intervention, tcafter is the trend changes after the intervention, GDP represents the gross domestic product, InR is the inflation rate, and et is the random variability that is not explained by the model.
Furthermore, the KI was calculated to determine the effect of the TSL on the equity in healthcare financing. This is presented in the equation below.
| (4) |
Where yKIt is the KIakwani index as an indicator of healthcare financing equity indicator at year t; IMR is the infant mortality rate, and PoU60 is the ratio of the population over the age of 60 years.
Furthermore, the absolute effect of the TSL intervention on income inequality (GI) (equation 8) was calculated by subtracting the value of equation 7 from the value of equation 6. This is mathematically presented as follows.
| (5) |
| (6) |
| (7) |
Statistical Analysis
A segmented regression analysis was carried out on the calculated values of the GI and KI to determine the effects of the TSL, which was implemented in 2010. The analysis was conducted to see whether there were changes in the level and trend of these variables during, before, and after the implementation of the TSL. The effect of the intervention was detected by comparing the value of the intercept and trend before and after the intervention [21]. To detect the effect of an intervention using segmented regression analysis, at least 3 time series observations before and 3 times series observations after are required [27]. Accordingly, this analysis applied 33 yearly GI observations before and 5 yearly GI observations after the intervention. Similarly, we used 22 yearly KI observations before and 5 yearly KI observations after the intervention (Table 1). The stepwise elimination method was used to exclude non-significant independent variable from the fitted model. Hence, the model from which all non-significant variables were removed could be considered parsimonious.
Table 1.
Trends of the Gini index, concentration index, Kakwani index, gross domestic product (GDP), inflation rate, infant mortality rate (IMR), and proportion of the population over 60 years, 1977-2014
| Year | 1977-1980 | 1980-1990 | 1990-2000 | 2000-2009 | 2010 | 2011 | 2012 | 2013 | 2014 |
|---|---|---|---|---|---|---|---|---|---|
| Gini index1 | 0.401 | 0.401 | 0.397 | 0.401 | 0.381 | 0.372 | 0.365 | 0.365 | 0.362 |
| GDP2 | 5273.70 | 14 710.80 | 210 864.50 | 2.10E+06 | 5.5E+06 | 5.80E+06 | 5.80E+06 | 5.30E+08 | 5.30E+08 |
| Inflation rate3 | 15.51 | 19.53 | 24.03 | 14.75 | 12.42 | 21.53 | 30.51 | 34.74 | 27.53 |
| IMR4 | 87.61 | 58.72 | 36.62 | 22.53 | 16.56 | 15.74 | 15.12 | 14.46 | 13.71 |
| 60 y4 | 3.04 | 2.99 | 3.71 | 4.77 | 5.16 | 5.20 | 5.24 | 5.28 | 5.29 |
| Concentration index5 | - | - | 0.371 | 0.381 | 0.388 | 0.368 | 0.389 | 0.388 | 0.370 |
| Kakwani index5 | - | - | 0.0256 | -0.0216 | 0.007 | -0.001 | 0.024 | 0.023 | 0.008 |
From Iran Statistical Center report, 2014.
From World Bank Report 2014.
From Central Bank of Iran.
From Deputy of Treatment of Ministry of Health Report 2014.
Calculated by authors.
Mean over 10 years.
The final fitted model was assessed for autocorrelation, co-integration of the variables, and any spurious regression. Thus, the Durbin-Watson statistic was estimated on the residuals of the fitted model. Results closer to 2 indicate the absence of autocorrelation [28]. This test yielded nonstationary results for almost all the variables (Tables 2 and 3). The Breusch-Pagan diagnostic test for heteroscedasticity was also done on the residuals. The null hypothesis (H0) of this test was that the variances of the variables were same, and the decision was made at p-values less than 0.05. Finally, the Shapiro-Wilk W test was performed to assess the normality of the residuals.
Table 2.
Parameter estimates of segmented regression analysis models of the effects of TSL implementation on income inequality (Gini index) in Iran, 1977-2014 (year of intervention, 2010)
| Explanatory variables |
Goodness of fit |
Residual tests |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intercept | Tbefore | CCafter | TCafter | lGDP | InR | F | R-2 | RMST | DF | NO | DW | B-P | ||
| Models | A | 0.374 | -0.001 | -0.008 | -0.008 | 0.003 | 0.000 | 19.58 | 0.00717 | 0.0071 | -4.859 | 0.967 | 1.628 | 1.08 |
| p-value | <0.001 | 0.07 | 0.38 | 0.03 | 0.12 | 0.76 | <0.001 | 0.32 | 0.30 | |||||
| B | 0.373 | -0.001 | -0.008 | -0.008 | 0.004 | - | 25.15 | 0.00707 | 0.0070 | -4.793 | 0.964 | 1.604 | 1.06 | |
| p-value | <0.001 | 0.06 | 0.39 | 0.02 | 0.11 | - | <0.001 | 0.26 | 0.30 | |||||
| C | 0.405 | 0.000 | -0.017 | -0.003 | - | 0.000 | 22.83 | 0.00733 | 0.0073 | -4.613 | 0.965 | 1.510 | 1.43 | |
| p-value | <0.001 | 0.14 | 0.05 | 0.11 | - | 0.70 | <0.001 | 0.28 | 0.23 | |||||
| D | 0.404 | 0.000 | -0.016 | -0.004 | - | - | 31.17 | 0.00723 | 0.0072 | -4.513 | 0.964 | 1.473 | 1.34 | |
| p-value | <0.001 | 0.14 | 0.05 | 0.08 | - | - | <0.001 | 0.27 | 0.25 | |||||
| Most parsimonious model | 0.401 | - | -0.032 | - | - | - | 79.53 | 0.00761 | 0.0076 | -3.770 | 0.886 | 1.472 | 1.47 | |
| <0.001 | - | <0.001 | - | - | - | <0.001 | <0.001 | 0.24 | ||||||
TSL, Targeted Subsidies Law; Tbefore, time trend before intervention; CCafter, intercept changes after intervention; TCafter, trend changes after the intervention; lGDP, log gross domestic product; InR, inflation rate; RMST, restricted mean survival time; DF, stationary of residuals with the Dicky-Fuler test; NO, normality of residuals with the Shapiro-Wilk W test; DW, Durbin-Watson test for autocorrelation; B-P, Breusch-Pagan test for heteroscedasticity.
Table 3.
Parameter estimates of segmented regression analysis models of the effects of TSL implementation on inequality in healthcare financing (Kakwani index) in Iran, 1988-2014 (year of intervention, 2010)
| Models | Explanatory variables |
Goodness of fit |
Residual tests |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intercept | Tbefore | CCafter | TCafter | lGDP | IMR | PoU60 | InR | F | R-2 | RMST | ST | NO | DW | B-P | |
| A | -0.02 | 0.01 | 0.01 | -0.01 | 0.00 | 0.00 | -0.06 | 0.00 | 5.95 | 0.69 | 0.01 | -5.20 | 0.78 | 2.16 | 0.37 |
| p-value | 0.95 | 0.33 | 0.67 | 0.53 | 0.98 | 0.91 | 0.17 | 0.13 | <0.001 | <0.001 | 0.54 | ||||
| B | 0.02 | 0.01 | 0.01 | -0.01 | - | 0.000 | -0.06 | 0.00 | 7.31 | 0.59 | 0.01 | -5.20 | 0.78 | 2.16 | 0.38 |
| p-value | 0.94 | 0.32 | 0.62 | 0.37 | - | 0.91 | 0.16 | 0.12 | <0.001 | <0.001 | 0.54 | ||||
| C | 0.48 | 0.01 | 0.01 | -0.01 | - | - | -0.06 | 0.00 | 9.20 | 0.61 | 0.01 | -5.19 | 0.78 | 2.15 | 0.34 |
| p-value | 0.57 | 0.06 | 0.55 | 0.27 | - | - | 0.14 | 0.11 | <0.001 | <0.001 | 0.52 | ||||
| D | -0.07 | 0.00 | 0.01 | 0.00 | - | - | - | 0.00 | 31.17 | 0.73 | 0.01 | -4.77 | 0.81 | 1.97 | 0.56 |
| p-value | <0.001 | <0.001 | 0.36 | 0.70 | - | - | - | 0.05 | <0.001 | <0.001 | 0.45 | ||||
| E | -0.05 | 0.00 | 0.01 | 0.00 | - | - | - | - | 11.68 | 0.55 | 0.01 | -3.37 | 0.84 | 1.62 | 0.33 |
| p-value | <0.001 | <0.001 | 0.41 | 0.81 | - | - | - | - | <0.001 | <0.001 | 0.56 | ||||
TSL, Targeted Subsidies Law; Tbefore, time trend before intervention; CCafter, intercept changes after intervention; TCafter, trend changes after the intervention; lGDP, log gross domestic product; IMR, infant mortality rate; PoU60, proportion of the population 60 years old; InR, inflation rate; RMST, restricted mean survival time; DF, stationary of residuals with the Dicky-Fuler test; NO, normality of residuals with the Shapiro-Wilk W test; DW, Durbin-Watson test for autocorrelation; B-P, Breusch-Pagan test for heteroscedasticity.
The findings are presented as numeric, percentage, and mean values and are presented graphically and in tables. All analyses were performed using Stata version 13 (StataCorp., College Station, TX, USA).
Ethics Statement
The Research and Ethics Committee of Tehran University of Medical Sciences approved the protocol of this study on August 12, 2014 (no. 9021557003).
RESULTS
The GI during the time series period (1977 to 2014) had a negative trend (Table 1). The mean GI decreased from 0.401 in the 1980s to 0.381 in 2010, and then to 0.362 in 2014. The maximum level of the GI was 0.401 in the 1980s and the minimum level was 0.362 in 2014. The GDP increased over time between 1977 and 2014. The average InR increased from 15.51% in 1977-1980 to 24.03% in 1990-2000, and then decreased to 12.42% during 2000-2010. The maximum and minimum InR were 24.03 and 12.42%, respectively. The IMR decreased over time, while the proportion of PoU60 increased, from 3.04% in 1977 to 5.29% in 2014.
Furthermore, the CI showed that inequality in healthcare expenditures decreased from 1988 to 2014. However, the trend of the CI showed considerable oscillation. The highest CI was in 2012 and the lowest was in 2011. The KI also showed fluctuating findings, although improvements in the indices were noted after 2012. The average KI of healthcare financing during the first 10 years (1990-2000) was more equitable (K=0.025) than was observed in the last 10 years before the implementation of the TSL (2000-2009, K=-0.021). We found no statistically significant effect on equity in healthcare financing after the implementation of the TSL. Nevertheless, the general trend of the KI during the TSL implementation period showed an increase, from -0.050 to 0.001.
The segmented regression analysis estimated the GI of the different models, as shown in Table 2. The most parsimonious model showing the effect of the TSL on income inequality was model D. The F statistic value (31.17) and adjusted coefficient of determination (R2=73.3%) in this model were higher than in the other models. There was a statistically significant (p<0.001) decrease in the slope of the mean GI before the intervention (1977 to 2010). Immediately after the intervention of the TSL, the level of the mean GI dropped by -0.032, showing a statistically significant (p<0.001) immediate reduction in income inequality, although there was no significant change in the slope of the mean GI during the period after the intervention (2010 to 2014, p=0.08) (Table 2). Thus, the TSL implementation led to a reduction of the GI by 0.08, but the effect of the TSL on reducing income inequality was very small (Figure 1).
Figure. 1.
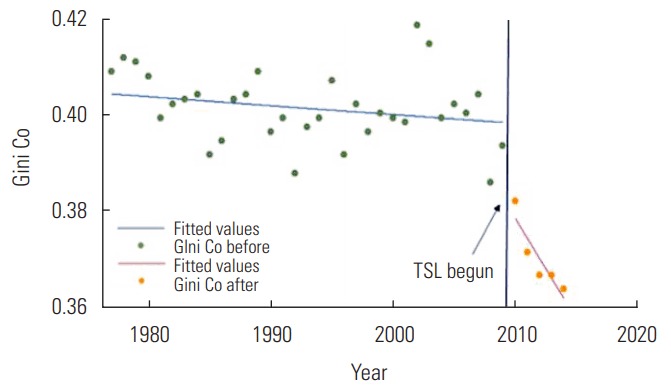
The distribution of Gini Index during the study time (1977–2014). Co, coefficient; TSL, Targeted Subsidies Law.
Effect of the Targeted Subsidies Law on Equity in Healthcare Financing
The segmented regression analysis revealed that the TSL did not have any statistically significant effect on the level or trend of the KI in either of the models (Table 3). The F statistic of the KI model D showed it to be a well-fitted model (F=31.17, p< 0.001) and the index before the intervention was decreasing to a significant extent (p<0.001), by 0.07 annually. Our study revealed no statistically significant change in the trend of KI after the implementation of the TSL (Figure 2). Over time, there was a negligible but statistically significant (p<0.001) positive effect of the InR on the KI.
Figure. 2.
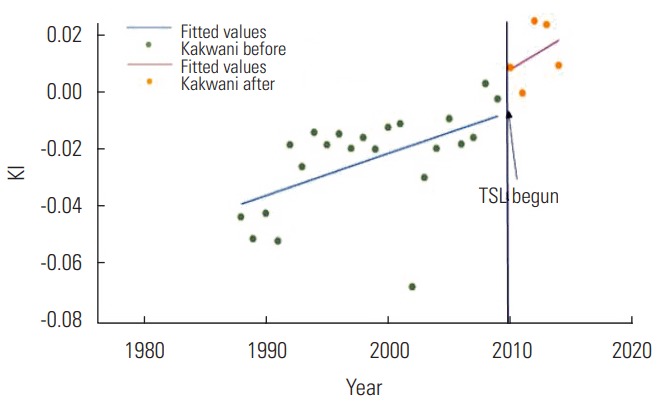
The distribution of Kakwani index (KI) during the study time (1988-2014), 22 years before and 5 years after TSL, Targeted Subsidies Law (TSL) implementation (2010).
DISCUSSION
The TSL was a recent reform that was implemented in Iran in 2010 [29]. This reform was part of the economic development plan of the country, the fundamental aim of which was to reduce income inequality among Iranian households and to improve equity in healthcare financing by implementing comprehensive social security [14]. The GI, InR, and GDP are indicators that are strongly influenced by economic conditions [30].
The findings of this study revealed that TSL implementation had a positive effect on the GI in Iran. The GI showed a negative trend in income inequality before the implementation of the TSL, which may indicate a gradual decline in income inequality over time. However, this was not statistically significant. Income inequality decreased immediately after the implementation of the TSL. Evidence has been found of a correlation between income inequality and healthcare outcomes [31]. Another study likewise reported a relationship between income inequality and increased stroke mortality [32].
Our study found no statistically significant relationships between the GI and the InR and GDP after the implementation of the TSL. Although previous studies have found an increasing InR and a decreasing trend in the GDP [33], some have reported a positive association between InR and income inequality [34]. However, the reduction in income inequality may be due to at least 2 reasons: the effects of the recently introduced TSL reform and the lag of the effect of the InR on income inequality. The reduction in income inequality after the implementation of the TSL indicates the conformity of the reform with its planned objectives of redistributing wealth and reducing income inequality among citizens. Several other studies have reported that subsidies and reducing taxation resulted in equitable income distributions [23].
Equity in healthcare financing is one of the main indicators of sound healthcare system performance [25]. Our study revealed a progressive healthcare financing trend over time, which is consistent with progressive healthcare insurance payments (positive slope of the KI) [4,35]. Furthermore, a positive KI, indicating improvements in health expenditures, was also reported [3,36]. In contrast, studies in Iran and other developing countries have reported regressive healthcare financing, indicating that low-income households pay more for healthcare than others [35,37].
The segmented regression analysis in our study did not show a significant effect of TSL on equity in healthcare financing (KI). However, this study revealed a positive trend in the KI before the introduction of the TSL. This may have been due to other health sector-related reforms introduced before the TSL implementation, as well as the lack of proper implementation of the TSL and insufficient funds paid to the health system [18]. Another study reported that equity-based healthcare reform significantly reduced income-related inequality [38]. Moreover, studies have shown positive effects of economic or health system reforms on equity in healthcare financing [39]. Hu et al. [39], in a study of employment practices, taxation, and workers’ health/welfare benefit coverage in China that evaluated the effects of the enterprise reform on workers’ healthcare benefits and their financial burden due to medical expenses, concluded that the reform reduced workers’ out-of-pocket expenditures [39]. These variations could be related to the focus of our study on the effects of general economic reforms on healthcare financing, whereas other studies assessed the effects of reforms that were primarily focused on the health sector.
This study was based on survey data from a large sample (31 000-36 000 households annually) retrieved from the reports of the Statistical Center of Iran and other national and international reports for the years 1977-2014. Hence, the findings can be generalized to the entire population of Iran. The KI was used in this study, as it is a commonly used indicator for assessing equity in healthcare financing [4]. Using segmented regression analysis was a strength of this study, as it is a powerful method of interrupted time series analysis [21]. Segmented regression analysis requires multiple observations before and after a single intervention [27]. However, the presence of fewer observations after the TSL implementation might have limited the detection of the real effect of the TSL on income inequality and equity in healthcare financing. Additionally, several additional control variables could have been included in this study, but due to the lack of access to data on control variables or their incompleteness in the time frame of the present study (1977-2014), only the InR and GDP were used as control variables for examining the effect of the TSL on the Gini coefficient, and the IMR and the PoU60 were used as control variables for examining the effect of the TSL on the KI.
The study investigated the effects of the TSL on equity in healthcare financing and on income inequality since 2010 in Iran. The segmented regression analysis revealed that the TSL did not show a significant effect on equity in healthcare financing, although income inequality decreased after the implementation of the TSL. The KI showed that the equity in healthcare financing has improved over time. This finding suggests that economic reforms, such as the TSL, may have a progressive effect on equity in healthcare financing. Thus, considering the long-term effects of the TSL on equity in healthcare financing and other related health system indicators is of paramount importance for healthcare decision-makers.
Acknowledgments
The authors acknowledge all of the academic and administrative entities that helped them in the design of the study and provided comments useful for finalizing the manuscript. This manuscript was fully sponsored by Tehran University of Medical Sciences (TUMS) (grant no. 9021557003).
Footnotes
CONFLICT OF INTEREST
The authors have no conflicts of interest associated with the material presented in this paper.
REFERENCES
- 1.Gerstl S, Sauter J, Kasanda J, Kinzelbach A. Who can afford health care? Evaluating the socio-economic conditions and the ability to contribute to health care in a post-conflict area in DR Congo. PLoS One. 2013;8(10):e77382. doi: 10.1371/journal.pone.0077382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Evans DB, Etienne C. Health systems financing and the path to universal coverage. Bull World Health Organ. 2010;88(6):402. doi: 10.2471/BLT.10.078741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khan JA, Ahmed S, Evans TG. Catastrophic healthcare expenditure and poverty related to out-of-pocket payments for healthcare in Bangladesh-an estimation of financial risk protection of universal health coverage. Health Policy Plan. 2017;32(8):1102–1110. doi: 10.1093/heapol/czx048. [DOI] [PubMed] [Google Scholar]
- 4.Hajizadeh M, Connelly LB. Equity of health care financing in Iran: the effect of extending health insurance to the uninsured. Oxf Dev Stud. 2010;38(4):461–476. [Google Scholar]
- 5.Mehrolhassani M, Najafi B, Yazdi Feyzabadi V, Haghdoost AA, Abolhallaje M, Ansari M, et al. Total health expenditures and proportion of out-of-pocket payments in Iranian provinces; 2008-2014. Iran J Epidemiol. 2017;12(5):1–12. (Persian) [Google Scholar]
- 6.Takian A, Rashidian A, Doshmangir L. The experience of purchaser-provider split in the implementation of family physician and rural health insurance in Iran: an institutional approach. Health Policy Plan. 2015;30(10):1261–1271. doi: 10.1093/heapol/czu135. [DOI] [PubMed] [Google Scholar]
- 7.Hajizadeh M, Nghiem HS. Out-of-pocket expenditures for hospital care in Iran: who is at risk of incurring catastrophic payments? Int J Health Care Finance Econ. 2011;11(4):267–285. doi: 10.1007/s10754-011-9099-1. [DOI] [PubMed] [Google Scholar]
- 8.Yazdi Feyzabadi V, Mehrolhassani MH, Haghdoost AA, Bahrampour M. The trend of impoverishing effects of out-of-pocket health expenditure in Iranian provinces in 2008-2014. Iran J Epidemiol. 2017;12(5):20–31. (Persian) [Google Scholar]
- 9.Mostafavi H, Aghlmand S, Zandiyan H, Alipoori Sakha M, Bayati M, Mostafavi S. Inequitable distribution of specialists and hospital beds in west Azerbaijan province. J Allied Med Sch Tehran Univ Med Sci. 2015;9(1):55–66. (Persian) [Google Scholar]
- 10.Zandiyan H, Ghiasvand H, Nasimi DR. Measuring inequality of distribution of health resources: a case study. Payesh. 2012;11(6):799–805. (Persian) [Google Scholar]
- 11.Yazdi Feyzabadi V, Bahrampour M, Rashidian A, Haghdoost AA, Abolhallaje M, Najafi B, et al. Incidence and intensity of catastrophic health expenditures in Iranian provinces; 2008-2014. Iran J Epidemiol. 2017;12(5):40–54. (Persian) [Google Scholar]
- 12.Davari M, Haycox A, Walley T. Health care financing in iran; is privatization a good solution? Iran J Public Health. 2012;41(7):14–23. [PMC free article] [PubMed] [Google Scholar]
- 13.Kavosi Z, Rashidian A, Pourreza A, Majdzadeh R, Pourmalek F, Hosseinpour AR, et al. Inequality in household catastrophic health care expenditure in a low-income society of Iran. Health Policy Plan. 2012;27(7):613–623. doi: 10.1093/heapol/czs001. [DOI] [PubMed] [Google Scholar]
- 14.Guillaume D, Zytek R, Farzin MR. Iran–the chronicles of the subsidy reform. 2011 [cited 2018 Mar 7]. Available from: http://www.greenfiscalpolicy.org/wp-content/uploads/2013/08/Iran-The-Chronicles-of-the-Subsidy-Reform1.pdf.
- 15.Salehi-Isfahani D, Wilson Stucki B, Deutschmann J. The reform of energy subsidies in Iran: the role of cash transfers. Emerg Mark Financ Trade. 2015;51(6):1144–1162. [Google Scholar]
- 16.Abbasian E, Asadbaygi Z. Targeted communication of energy subsidies and social welfare through economic growth. Soc Welf. 2012;12(44):143–173. (Persian) [Google Scholar]
- 17.Zamanzadeh H. Targeted subsidies: achievements, challenges and costs. Tazehaye Egtesad. 2011;9(133):108–116. (Persian) [Google Scholar]
- 18.Zandian H, Olyaeemanesh A, Takian A, Hosseini M. Contribution of targeted subsidies law to the equity in healthcare financing in Iran: exploring the challenges of policy process. Electron Physician. 2016;8(2):1892–1903. doi: 10.19082/1892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pourasghari H, Jafari M, Bakhtiari M, Keliddar I, Irani A, Afshari M. Analysis of equality in Iranian household healthcare payments during Iran’s fourth development program. Electron Physician. 2016;8(7):2645–2649. doi: 10.19082/2645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Doshmangir L, Doshmangir P, Abolhassani N, Moshiri E, Jafari M. Effects of targeted subsidies policy on health behavior in Iranian Households: a qualitative study. Iran J Public Health. 2015;44(4):570–579. [PMC free article] [PubMed] [Google Scholar]
- 21.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 22.Giles DE. Calculating a standard error for the Gini coefficient: some further results. Oxf Bull Econ Stat. 2004;66(3):425–433. [Google Scholar]
- 23.Yusuf AA, Resosudarmo BP. Is reducing subsidies on vehicle fuel equitable? A lesson from Indonesian reform experience. In: Sterner T, editor. Fuel taxes and the poor: the distributional effects of gasoline taxation and their implications for climate policy. New York: RFF Press; 2012. pp. 171–180. [Google Scholar]
- 24.O’Donnell O, van Doorslaer E, Wagstaff A, Lindelow M. Analyzing health equity using household survey data a guide to techniques and their implementation. 2007 [cited 2018 Mar 8]. Available from: http://siteresources.worldbank.org/INTPAH/Resources/Publications/459843-1195594469249/HealthEquityFINAL.pdf.
- 25.O’Donnell OA, Wagstaff A. Analyzing health equity using household survey data: a guide to techniques and their implementation. Washington, DC: World Bank; 2008. pp. 1–165. [Google Scholar]
- 26.Paya A, Raghfar H, Abdi A, Poor DM, Fadavi-Ardekani M. Social, economic, political, and intellectual changes in Iran since 1960s. In: Tiliouine H, Estes RJ, editors. The state of social progress of Islamic societies: social, economic, political, and ideological challenges. Switzerland: Springer; 2016. pp. 211–235. [Google Scholar]
- 27.Ramsay CR, Matowe L, Grilli R, Grimshaw JM, Thomas RE. Interrupted time series designs in health technology assessment: lessons from two systematic reviews of behavior change strategies. Int J Technol Assess Health Care. 2003;19(4):613–623. doi: 10.1017/s0266462303000576. [DOI] [PubMed] [Google Scholar]
- 28.Hamilton JD. Time series analysis. Princeton: Princeton University Press; 1994. p. 571. [Google Scholar]
- 29.Hassanzadeh E. Recent developments in Iran’s energy subsidy reforms. 2012 [cited 2018 Mar 10]. Available from: https://www.iisd.org/gsi/sites/default/files/pb14_iran.pdf.
- 30.Graeff P, Mehlkop G. The impact of economic freedom on corruption: different patterns for rich and poor countries. Eur J Polit Econ. 2003;19(3):605–620. [Google Scholar]
- 31.Heshmati A. The world distribution of income and income inequality: a review of the economics literature. J World-Syst Res. 2006;12(1):61–107. [Google Scholar]
- 32.Vincens N, Stafström M. Income inequality, economic growth and stroke mortality in Brazil: longitudinal and regional analysis 2002-2009. PLoS One. 2015;10(9):e0137332. doi: 10.1371/journal.pone.0137332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Farzanegan MR, Markwardt G. The effects of oil price shocks on the Iranian economy. Energy Econ. 2009;31(1):134–151. [Google Scholar]
- 34.Monnin P. Inflation and income inequality in developed economies. 2014 [cited 2018 Mar 10]. Available from: https://www.cepweb.org/wp-content/uploads/2014/05/CEP_WP_Inflation_and_Income_Inequality.pdf.
- 35.Hajizadeh M, Connelly LB. Equity of health care financing in Iran. 2009 [cited 2018 Mar 10]. Available from: https://mpra.ub.uni-muenchen.de/14672/1/MPRA_paper_14672.pdf.
- 36.Rezaei S, Fallah R, Kazemi Karyani A, Daroudi R, Zandiyan H, Hajizadeh M. Determinants of healthcare expenditures in Iran: evidence from a time series analysis. Med J Islam Repub Iran. 2016;30:313. [PMC free article] [PubMed] [Google Scholar]
- 37.Munge K, Briggs AH. The progressivity of health-care financing in Kenya. Health Policy Plan. 2014;29(7):912–920. doi: 10.1093/heapol/czt073. [DOI] [PubMed] [Google Scholar]
- 38.Cabieses B, Cookson R, Espinoza M, Santorelli G, Delgado I. Did socioeconomic inequality in self-reported health in Chile fall after the equity-based healthcare reform of 2005? A concentration index decomposition analysis. PLoS One. 2015;10(9):e0138227. doi: 10.1371/journal.pone.0138227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hu TW, Ong M, Lin ZH, Li E. The effects of economic reform on health insurance and the financial burden for urban workers in China. Health Econ. 1999;8(4):309–321. doi: 10.1002/(sici)1099-1050(199906)8:4<309::aid-hec440>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]


