Abstract
Background
Infants are thought to be protected against malaria during the first months of life mainly due to passage of maternal antibodies. However, in high transmission settings, malaria in early infancy is not uncommon and susceptibility to the infections varies between individuals. This study aimed to determine malaria morbidity and infection during early childhood in rural Burkina Faso.
Methods
Malariometric indices were determined over 1-year follow-up in a birth cohort of 734 infants living in Nanoro health district. Clinical malaria episodes were determined by passive case detection at peripheral health centres while asymptomatic malaria infections were identified during 4 cross-sectional surveys at 3, 6, 9 and 12 months of age. Plasmodium falciparum infections were detected by rapid diagnostic test and/or light microscopy (LM) and quantitative PCR (qPCR).
Results
In total, 717 clinical episodes were diagnosed by qPCR over 8335.18 person-months at risk. The overall malaria incidence was 1.03 per child-year and increased from 0.27 per child-year at 0–3 months of age to 1.92 per child-year at 9–12 months of age. Some 59% of children experienced at least one clinical episode with a median survival time estimated at 9.9 months, while 20% of infants experienced the first episode before 6 months of age. The majority of the clinical episodes were attributable to microscopic parasitaemia (84.2%), and there was a positive correlation between parasite density and age (Spearman’s rho = 0.30; P < 0.0001). Prevalence of asymptomatic infections was similar at 3, 6 and 9 months of age (17.7–20.1%) and nearly 1.6 times higher at 12 months (31.3%). Importantly, gametocyte prevalence among the LM-positive study population was 6.7%, but increased to 10% among asymptomatic infections. In addition, 46% of asymptomatic infections were only detected by qPCR suggesting that infants below 1 year are a potential reservoir for sustaining malaria transmission. Both symptomatic and asymptomatic infections showed marked seasonal distribution with the highest transmission period (July to December) accounting for about 89 and 77% of those infections, respectively.
Conclusions
These findings indicate high and marked age and seasonal-dependency of malaria infections and disease during the first year of life in Nanoro, calling for intensified efforts to control malaria in rural Burkina Faso.
Keywords: Malaria, Incidence, Prevalence, Infants, Burkina Faso
Background
Despite the scaling-up of malaria control measures in sub-Saharan Africa (sSA), malaria morbidity and mortality remains particularly high in some areas, especially among young children and pregnant women [1]. In 2015, an estimated 191 million cases of malaria occurred in Africa resulting in 394,000 deaths of which nearly 74% were among children under 5 years old [2].
Malaria burden among children under 5 years is well documented in sSA [2–8] with the majority of studies focusing on the prevalence of malaria in infants below 6 months (including congenital malaria) [9–18]. However, few epidemiological birth cohort studies have analysed malaria morbidity during the first year of life [19–21], and surveys screening asymptomatic infections (from which clinical episodes may derive) are scarce in infants. Importantly, the evaluation of currently recommended interventions such as intermittent preventive treatment in infancy with sulfadoxine–pyrimethamine (SP–IPTi) [22] requires baseline information on infection and diseases in infants below 1 year in order to evaluate its impact.
Although children in early infancy are thought to be protected from malaria by maternal antibodies acquired in utero [23–26] and fetal haemoglobin (HbF) [27, 28], increasing evidence shows that prevalence of disease is higher than previously thought. Studies in high transmission settings have shown that the prevalence of malaria (cases and/or infections) in neonates could reach 25–46% [9, 11, 13, 14], 20–36% in the first 6 months of life [15–17], and 52.1% during the first year of life [29]. In Benin and Cameroon, the proportion of infants who experienced at least one malaria episode of malaria in 12-months birth cohort studies was estimated at 35–44.5%, respectively [20, 21]. On the other hand, some infants may develop a resistant or a tolerant phenotype upon prenatal exposure to malaria parasites, which influences the development of malaria symptoms or the time to first infection/clinical episode leading to inter-individual variation in susceptibility to malaria in early childhood [30–33]. Due to the life-threatening risk of malaria during the first year of life, detailed up-to-date epidemiological information on the malaria burden in infants, including asymptomatic infections, are necessary to inform countries policy decisions.
In Burkina Faso, malaria in infants remains the first cause of attendance to health centres [2]. Epidemiological data on malaria available in the country rely mostly on reports from health facilities, which lack accuracy and do not account for asymptomatic parasite carriers. To the best of found knowledge, only one birth cohort study evaluating the long-term effects of insecticide-treated nets in newborns was conducted in Nouna (northwest of Burkina Faso) between 2000 and 2003. The study reported incidences of infections of 0.75 and 2.7 per child/year during the periods of 0–5 and 6–12 months, respectively [34]. Thus, there is limited epidemiological data on malariometric indices, age-dependency of parasite densities and seasonal variation of the infections occurring during the first 12 months of life.
The aim of the current study was to investigate malaria infections and morbidity during the first year of life and assess variability in susceptibility between individuals in the rural health district of Nanoro in Burkina Faso. Using a highly sensitive quantitative polymerase chain-reaction (qPCR), the incidence of clinical episodes in a longitudinal survey and the age-specific prevalences of asymptomatic infections through cross-sectional surveys were determined. In addition, these results were compared with parasite detection by expert light microscopy (LM) to determine the prevalence of sub-microscopic infections in both symptomatic and asymptomatic patients. Finally, differences in susceptibility to malaria between individuals in early childhood were characterized.
Methods
Study area
The study was conducted in Nanoro health district (NHD), a rural area in the central-west region of Burkina Faso at 85 km from Ouagadougou, the country’s capital (Fig. 1). NHD comprises 21 peripheral health centres and has approximately 166,683 inhabitants [35]. NHD is located in the Sudano-Sahelian area of the country with a rainy season lasting mostly from July to November with an average rainfall of 450–700 mm/year. Malaria transmission in the region is seasonal and hyperendemic. Almost all cases are caused by Plasmodium falciparum and the disease puts a significant burden on the population, especially in children under 5 years old and pregnant women. In 2016, health facilities in NHD reported 91,154 clinical malaria episodes, of which 9992 cases (11%) and 41,076 cases (45%) occurred among 0–1 year infants and 1–5 years children, respectively [35].
Fig. 1.
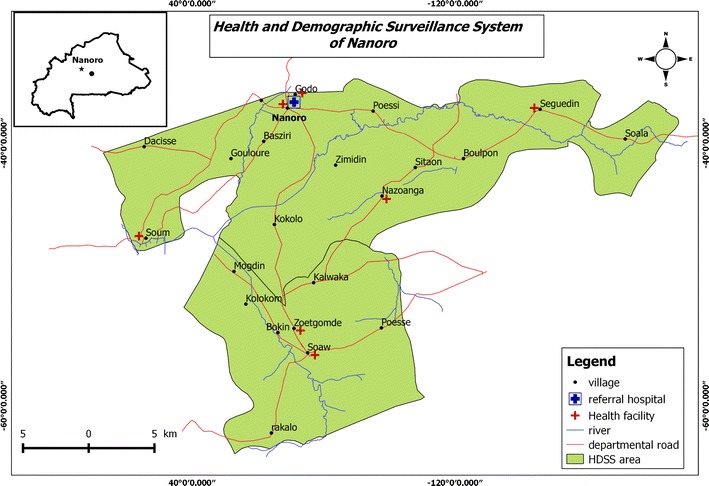
Map of the study area. Inset shows location of Nanoro Health District in Burkina Faso (black dot indicates location of capital Ouagadougou)
Study design and procedures
This study was designed as a prospective birth cohort study with a 12-month follow-up duration of each newborn. The study was nested within the COSMIC clinical trial (NCT01941264), a multicentre, cluster-randomized trial assessing the effectiveness of community-based, scheduled screening and treatment of pregnant women for malaria control in pregnancy in Burkina Faso, Benin and The Gambia [36]. Pregnant women participating into the main trial in Burkina Faso were invited to enrol their offspring in the present study during antenatal care visits prior to delivery. Prior written informed consent was obtained from the mothers before inclusion in the study. Exclusion criteria were presence of major congenital malformation, chronic disease or signs of cerebral asphyxia. In total, 761 healthy newborns were enrolled over 16-months recruitment period (June 2014 to October 2015).
Longitudinal follow-up
The longitudinal survey consisted of passive case detection of clinical episodes of malaria over 1 year. Mothers were encouraged to seek care any time their child felt sick at peripheral health centres where trained study nurses were appointed. At each visit, a clinical examination was performed and mothers reported previous health events. In the case of an axillary temperature ≥ 37.5 °C or history of fever within 24 h, a malaria rapid diagnostic test (RDT) was performed and positive infants were treated according to national guidelines (artemether–lumefantrine or artesunate–amodiaquine). Infants with severe malaria received either artesunate, artemether or quinine injection before being transferred to the Centre Médical avec Antenne Chirurgical Saint Camille, the referral hospital of NHD. From all febrile children, additional blood samples (blood smears and spots on Whatman 3MM filter papers) were collected from finger prick for retrospective analysis by LM and qPCR except for severe malaria cases for which LM results were made available. Infants with a negative RDT and those with no fever were further examined according to the national algorithm for the management of non-malaria illnesses in peripheral health centre. Free medications were provided for both malaria and non-malaria illnesses.
Cross-sectional surveys
All children enrolled in the longitudinal follow-up were visited at home at 3, 6, 9, and 12 months of age to detect asymptomatic infections. Thus, only asymptomatic infants (i.e. no fever or history of fever in the previous 24 h) by the time of the survey were included. Each cross-sectional survey consisted of the administration of a questionnaire to mothers to collect previous heath events of their offspring related to malaria by a field worker and, the collection of blood samples from finger prick for LM and qPCR examination. Infants with ongoing malaria treatment were excluded for the survey. Those with fever or history of fever in the previous 24 h were referred to the peripheral health centre for the longitudinal survey.
Detection of malaria infections
RDT
Malaria RDT was performed using SD-Bioline malaria antigen P.f® test (05FK50, Standard Diagnostics, Inc, Korea) detecting P. falciparum histidine-rich protein2, as recommended by the National Malaria Control Programme (NMCP) in Burkina Faso. RDTs were performed following manufacturer instructions.
Microscopy
Malaria parasite detection and quantification by LM was performed according to standard procedures [37]. Briefly, blood smears were stained with Giemsa and examined with 100× oil immersion lens. For positive slides, the number of parasite and leucocytes were counted until reaching 200 leucocytes and parasitaemia was expressed as the number of asexual parasites per microlitre of blood based on an assumed 8000 white blood cells per microlitre of blood. A slide was considered negative if no parasites were observed after examining 100 fields. The presence of gametocytes was examined in all positive blood smears. All slides were read by two independent, experienced microscopists and those with discrepant results were read by a third microscopist. An internal quality control was performed by a fourth experienced reader for 10% of slides.
Filter paper processing, DNA extraction and VarATS quantitative PCR
Filter paper samples were air dried in the field, put in sealable bags with silica and transported the same day to the laboratory at the Clinical Research Unit of Nanoro (CRUN, Burkina Faso). The dried blood spots on filter papers were kept at ambient temperature until shipment to the Institute of Tropical Medicine (ITM, Belgium) for processing. Genomic DNA was extracted from 3 punches of dried blood spots (5 mm in diameter) using QIAamp 96 DNA blood kit (Qiagen, Germany), following the manufacturer’s recommendations and a final elution in 150 µL of water (Lonza, AccuGENE). Five µL of DNA were used as template for qPCR analysis targeting P. falciparum var gene acidic terminal sequence (varATS, ≈59 copies per genome) as previously described [38]. Parasite densities were obtained by interpolating cycle thresholds (Ct) using a standard curve prepared with titrated samples containing known numbers of infected erythrocytes diluted in whole blood (100,000–0.01 parasites/μL). The limit of detection of the varATS-based qPCR was 0.1 parasite/μL. Samples with Ct value > 39.7 were considered negative. DNA extracted from P. falciparum obtained from reference 3D7 parasites cultures was used as positive control. The negative controls included human negative blood spots on filter paper and mastermix reagent used as no template control (NTC).
Case definitions
For the present analysis clinical malaria episode or symptomatic malaria infection was defined as the presence of P. falciparum of any density by qPCR and an axillary temperature ≥ 37.5 °C or history of fever within the past 24 h. Severe malaria was defined as a clinical episode with one or more danger signs of disease severity including impaired consciousness, respiratory distress, severe anaemia (haemoglobin concentration < 5 g/dL), incoercible vomiting and inability to drink or suckle [39]. Asymptomatic infections were defined as carriage of P. falciparum parasites detected by qPCR with no evidence of fever in the past 24 h. Sub-microscopic infections were defined as malaria infection or disease detected by qPCR but not by LM.
Statistical analysis
Data were analysed with STATA version 12.0 (StataCorp, USA). Descriptive statistics were used to summarize baseline data and to compute malariometric indices. Kaplan–Meir analysis of time from birth to first clinical episode was used to determine the survival rates over the 12-months follow-up. The association between clinical malaria episodes, malaria transmission seasons and qPCR-parasite density were determined [odds ratios with 95% confidence interval (CI)] using bivariate logistic regression models. Spearman correlation coefficient was used to estimate the correlation between parasite densities and age of occurrence of clinical episodes. The difference in median values (with interquartile ranges, IQR) of parasite densities between (i) symptomatic and asymptomatic infections and (ii) infections occurring at 0–6 and 6–12 months, was analysed using the non-parametric Wilcoxon matched-pairs test. P values < 0.05 were considered statistically significant.
Results
Characteristics of study participants
Out of the initial 761 infants (739 singletons and 11 pairs of twins) enrolled, 669 (87.9%; 649 singletons and 20 twins) completed 1-year follow-up. Among the 92 (12.1%) infants who did not complete the follow-up, 7 (5 singletons and 2 twins from different mothers) died within 4 weeks after birth and 6 other singletons died before 12 months. In addition, 41 were lost to follow-up and 38 withdrew their consent mainly due to relocation out of the study area. Infants that were excluded from the analysis were the 7 neonates who died before 4 weeks of age due to the short duration of the follow-up and the 20 live twins owing to the risk of mixed samples and data from twin pairs.
Finally, 734 infants were included for the present analysis (Table 1). The mean age of their mothers was 26.4 ± 6.2 years and nearly two-thirds of them were multigravida (66.1%). More than half (62%) of pregnant women gave birth during malaria high-transmission season (from July to December); 48.5% of newborns were males and 51.5% females. The mean birth weight was 3012.7 ± 422.2 g. The proportions of asymptomatic infants enrolled into the cross-sectional surveys conducted at 3, 6, 9, and 12 months were 92.4% (678), 86% (631), 80% (587), and 86.9% (638), respectively. Out of the 649 singletons that completed the 12-months follow-up, 482 (74.3%) participated in the four cross-sectional surveys. Non-inclusion into the surveys was mainly attributable to ongoing malaria treatment, ongoing fever episode or the temporary absence from home. The highest number of infants excluded due to ongoing fever or history of fever in the previous 24 h was found at the cross-sectional survey performed at 9 months of age (2% [15/734]).
Table 1.
Characteristics of study participants
| Characteristics | Total study cohort (N = 734) |
|---|---|
| Maternal characteristics | |
| Age (years, mean ± SD) | 26.4 ± 6.2 |
| Gravidity [number (%)] | |
| Primigravida | 132 (18.0) |
| Secundigravida | 117 (15.9) |
| Multigravida | 485 (66.1) |
| Insecticide treated net use [number (%)] | 574 (78.2) |
| Infant characteristics | |
| Gender [number of females (%)] | 378 (51.5) |
| Birth weight (g, mean ± SD) | 3012.7 ± 422.2 |
| Low birth weight (< 2500) [number (%)] | 60 (8.2) |
| Birth season [number in malaria high-transmission season (%)] | 455 (62.0) |
SD Standard deviation, g gram
Clinical malaria episodes
In total, 717 clinical episodes of malaria were diagnosed by qPCR out of 1522 fever cases (47.11%) over 8335.18 person-months at risk, resulting in an incidence of malaria episodes during the first year of life of 1.03 per child-year. The proportion of clinical episodes increased from 7% (50/717) at 0–3 months to 43.8% (314/717) at 9–12 months (Fig. 2a and Table 2).
Fig. 2.
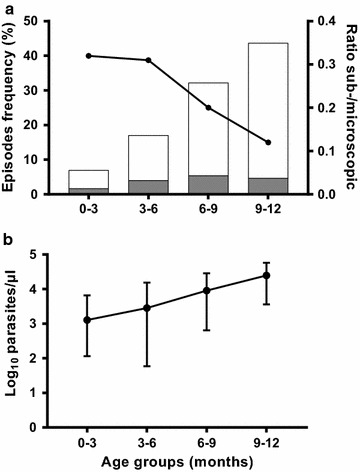
Clinical malaria episodes during the first year of life. a Frequency of clinical episodes by age group stratified by microscopic (white bars) and sub-microscopic (grey bars) malaria episodes. Black circles indicate the sub-microscopic:microscopic ratio. b Median parasite density (qPCR) on a log-scale by age group with interquartile ranges
Table 2.
Malariometric indices of clinical and asymptomatic infections during the first year of life
| Age groups | Total | ||||
|---|---|---|---|---|---|
| 0–3 months | 3–6 months | 6–9 months | 9–12 months | ||
| Longitudinal survey (N = 734) | |||||
| Clinical episodes by qPCR [number (% out of total cases)] | 50 (7) | 122 (17) | 231 (32.2) | 314 (43.8) | 717 (100) |
| Total time at risk (person-months) | 2197.07 | 2124.91 | 2056.62 | 1956.58 | 8335.18 |
| Incidence (per child-year) | 0.27 | 0.69 | 1.35 | 1.92 | 1.03 |
| Parasite density by qPCR [median (IQR)] | 1294 (116.5–6726) | 2848 (79.1–15,356) | 9044 (642–28,554) | 24,823 (3607–57,492) | 10,826.5 (876–38,021) |
| Sub-microscopic infections [number (% out of cases per age group)] | 12 (24) | 29 (23.8) | 39 (16.9) | 34 (10.8) | 114 (15.9) |
| Surveys timepoints | Total | ||||
|---|---|---|---|---|---|
| 3 months | 6 months | 9 months | 12 months | ||
| Cross-sectional surveys | |||||
| Total participants per survey | 678 | 631 | 587 | 638 | 2534a |
| Asymptomatic infections by qPCR [number (%)] | 120 (17.7) | 127 (20.1) | 108 (18.4) | 200 (31.3) | 555 (21.9)b |
| Parasite density by qPCR [median (IQR)] | 148 (4.2–1754) | 24.9 (1–954.7) | 454.9 (3.1–4524) | 1288 (2.6–13,998) | 347.8 (1.94–3534) |
| Sub-microscopic infections [number (% out of cases per survey)] | 58 (48.3) | 69 (54.3) | 49 (45.4) | 79 (39.5) | 255 (45.9) |
IQR interquartile range
a Total samples screened for asymptomatic infections
b Proportion of qPCR-positive samples out of total screened over the four cross-sectional surveys
A total of 433 children (59%) experienced at least one clinical episode, and 201 (27.4%) experienced more than one episode. The mean number of clinical episode was 1.6 (range 1–4) per child. Nearly two-thirds (65.6% [284/433]) of the first malaria episodes occurred during the period of 6–12 months of age as compared to one-third (34.4% [149/433]) during the period from birth to 6 months. The survival analysis shows that the 6-months survival rate was 80%, while half of the infants (50% [367/734]) experienced the first clinical episode by 9.9 months. Severe malaria episodes represented 1.5% of total clinical cases. The frequencies of danger signs of severe malaria were: incoercible vomiting (63.6% [7/11]), inability to drink or suckle (36.4% [4/11]), impaired consciousness (27.3% [3/11]), respiratory distress (18.2% [2/11]), and severe anaemia (18.2% [2/11]).
Overall, parasite densities by qPCR correlated with age (Spearman’s rho = 0.30; P < 0.001), with a median increasing from 1293.75 [IQR 127.00–7606.75] parasites/µL for 0–3 months to 24,822.50 [IQR 3624.00–57,650.25] parasites/µL for 9–12 months of age (Fig. 2b). Clinical episodes occurring from 6 to 12 months of age had 6.4 times higher parasite densities than those detected during the first 6 months of life (15,923.50 [IQR 1644.20–45,217.50] versus 2499.75 [IQR 85.00–14,230.50], P < 0.001).
The majority of clinical episodes presented with parasite densities detectable with LM (603/717, 84.1%). The distributions of sub-microscopic and microscopic parasitaemia according to age is presented in Fig. 2a. The proportion of sub-microscopic infections decreased with age as illustrated by the sub-microscopic:microscopic ratio, which decreased from 0.32 to 0.12 in infants from 0–3 to 9–12 months of age, respectively. The risk of having a sub-microscopic clinical episode was 1.8 times higher during the first 6 months of life (41/172, 23.8% sub-microscopic rate) than that during the period of 6–12 months of age (73/545, 13.4% sub-microscopic rate, risk ratio = 1.8; 95% CI = 1.28–2.54; P = 0.001).
Asymptomatic infections
The prevalence of asymptomatic infections detected by qPCR were similar at 3, 6 and 9 months of age (120/678, 17.7%; 127/631, 20.1%; 108/587, 18.4%, respectively) but higher at 12 months (200/638, 31.3%) (Fig. 3a, Table 2). Among infants who completed the four surveys (N = 482), 156 (32.4%) experienced at least one asymptomatic infection, and 100 (20.7%) had at least two asymptomatic infections. The mean number of asymptomatic infections acquired per child was 1.5 (range 1–4). From all infants who completed the 12-months follow-up and did not develop any clinical malaria episode (N = 241), 104 (43.1%) had an asymptomatic infection at least in one survey.
Fig. 3.
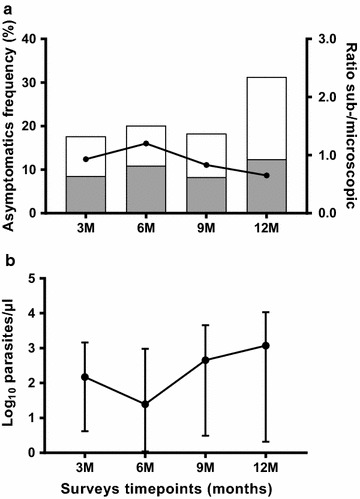
Asymptomatic malaria infections during the first year of life. a Prevalence of asymptomatic infections by age, stratified by microscopic (white bars) and sub-microscopic (grey bars). Black circles indicate the sub-microscopic:microscopic ratio. b Median parasite density (qPCR) on a log-scale by age with interquartile ranges
By qPCR, the overall median parasite density was 347.8 [IQR 1.94–3534] parasites/µL, which was significantly lower than that of clinical episodes (10,826.5 [IQR 876–38,021], P < 0.001). As shown in Fig. 3b, there was a tendency of increased parasite density in asymptomatic infections from 6 months of age. The median of cumulative parasite density at 3 and 6 months surveys was significantly lower than that observed at 9 and 12 months surveys: 87.5 [IQR 1.61–1262.5] parasites/µL versus 819.63 [IQR 2.2–7584] parasites/µL, P < 0.001.
In total, 46% (255/555) of asymptomatic infections were only detected by qPCR. The ratio of sub-microscopic:microscopic infections decreased from 0.9 to 1.2 at 3 and 6 months surveys to 0.6 at 12 months surveys (Fig. 3a).
Seasonality of Plasmodium falciparum infections
Both clinical episodes and asymptomatic infections showed a marked seasonal pattern (Fig. 4). The majority of clinical episodes (639/717, 89.1%) and asymptomatic infections (425/555, 76.6%) were diagnosed from July to December corresponding to the wet season with a peak in October. The odds ratio of having a clinical episode during the high-transmission versus the low-transmission season was 7.01 (95% CI 5.4–9.1; P < 0.001). The lowest frequencies of malaria episodes were observed in May and June (6/717, 0.8% and 2/717, 0.3%, respectively) (Fig. 4a). Infants born during malaria high-transmission season were at higher risk of experiencing a first clinical episode during the first 6 months of life whereas their counterparts born during malaria low-transmission season had a higher risk from 6 to 12 months of age (Fig. 5). Overall, the risk of having an asymptomatic infection was significantly higher when the cross-sectional survey occurred during the malaria high-transmission season from July to December (Table 3). The monthly distribution of asymptomatic infections showed that the beginning of the dry season (January to March) was characterized by a high number of asymptomatic infections (range 5.2–5.8%) compared to the period from April to June (range 1.8–3.1%) (Fig. 4b). The evolution of sub-microscopic:microscopic infections ratios by month highlighted a year-round higher ratios in asymptomatics [mean 0.9, range 0.7 (April)–2.4 (June)] than in clinical episodes [mean 0.2, range 0.1 (August)–1 (April)]. The ratios in asymptomatics compared to symptomatic infections, were 3.2 times higher during malaria low-transmission season (1.13 versus 0.35, respectively) and nearly 5 times higher during malaria high-transmission season (0.84 versus 0.17, respectively) (Fig. 4).
Fig. 4.
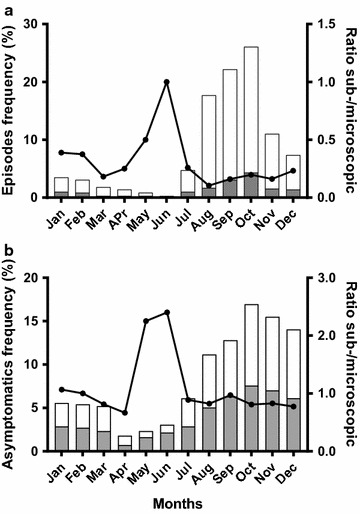
Monthly distribution of malaria infections during the first year of life. a Clinical episodes; b asymptomatic infections, stratified by microscopic (white bars) and sub-microscopic (grey bars) infection. Black circles indicate the sub-microscopic:microscopic ratio
Fig. 5.
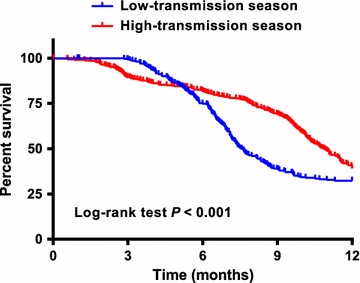
Risk of clinical malaria episode during the first year of life according to birth season. Kaplan–Meier survival curves stratified by infants born during malaria high-transmission season (July–December, red line) and low-transmission season (January–June, blue line)
Table 3.
Age-specific risk of asymptomatic infections in the context of seasonal risk of infection in Burkina Faso
| Month of birth | Surveys timepoints | |||||||
|---|---|---|---|---|---|---|---|---|
| 3 months | 6 months | 9 months | 12 months | |||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | OR (95%CI) | P | |
| Q1 (January–March) | Ref | Ref | Ref | Ref | ||||
| Q2 (April–June) | 22.05 (2.90–167.78) | 0.003 | 2.30 (1.27–4.15) | 0.005 | 0.72 (0.39–1.33) | 0.298 | 0.70 (0.36–1.37) | 0.298 |
| Q3 (July–September) | 88.96 (12.27–645.15) | < 0.001 | 1.22 (0.71–2.11) | 0.464 | 0.14 (0.07–0.30) | < 0.001 | 2.13 (1.25–3.61) | 0.005 |
| Q4 (October–December) | 7.47 (0.96–58.30) | 0.055 | 0.15 (0.06–0.37) | < 0.001 | 0.64 (0.38–1.10) | 0.105 | 3.66 (2.15–6.22) | < 0.001 |
Q quarter, OR odds ratio, CI confidence interval, Ref reference, OR (95% CI) with P values (P) < 0.05 are shown in italic
Gametocyte carriage
The proportion of clinical episodes carrying gametocytes among LM-positive samples was 3.6% (22/603), with the 22 cases occurring in different individuals. Out of the 300 LM-positive asymptomatic infections, P. falciparum gametocytes were detected in 29 blood smears from 28 individuals (9.7%). In total, 49 different gametocyte carriers were detected at both cross-sectional and longitudinal survey, resulting in an overall gametocyte prevalence of 6.7% (49/734) among the study population. The median gametocyte density was significantly higher in asymptomatic infections than in clinical episodes (128 [IQR 72–286] versus 48 [IQR 32–127] parasites/µL, P = 0.011).
Discussion
This study describes malaria infection and morbidity during the first year of life in NHD, a rural area of Burkina Faso where the seasonal malaria chemoprevention (SMC) in children and SP–IPTi were not implemented at the time the study was conducted, though adopted by NMCP in 2014 [39]. The findings showed a high burden of P. falciparum infections, which was characterized by an overall incidence of clinical malaria of 1.03 per child-year, an age-specific prevalence of asymptomatic infections ranging from 17.7 to 30.4% by cross-sectional survey, and a significant number of cases occurring during the first 6 months of life.
This high prevalence and incidence of infections and disease is in agreement with previous studies in the country [8, 34] and other reports from sSA [16, 18, 29, 40, 41], but contrasts with the previous perception of malaria as an uncommon infection/disease in early infancy in endemic settings [42–44].
The acquisition of maternal antibodies due to transplacental transfer and the presence of HbF in early infancy [23–28] are considered to provide a certain degree of protection against malaria to newborns during the first 6 months of life. Although there was a significant difference in both clinical and asymptomatic Plasmodium infections between 0–6 and 6–12 months, about 29% of infants experienced a clinical episode and/or asymptomatic infection during the first 6 months of life. On the other hand, the observed increase of malaria morbidity with age is in agreement with findings of a pooled analysis, which included data from different epidemiological settings in sSA [45].
The majority of clinical episodes had parasite densities detectable by LM (84%), while 46% of asymptomatic infections carried parasite densities only detectable by qPCR, indicating that parasite levels in peripheral blood are associated with clinical manifestations in infants. Moreover, in agreement with previous reports [29], parasite densities increased with age both in symptomatic and asymptomatic infections, with parasite densities from 0 to 6 months significantly lower than those from 6 to 12 months. That age-dependency of parasite load was further illustrated by a ratio of sub-microscopic: microscopic malaria infections decreasing after 6 months of age (Figs. 2 and 3). Altogether, these results indicate a gradual increase in malaria susceptibility during the first year of life as the passive immunity acquired from the mothers and levels of HbF progressively fade [28, 46–48]. Importantly, although gametocyte carriage could not be assessed here by reverse transcriptase (RT) qPCR, a prevalence of gametocyte of 6.7% was found among the study population, which increased to approximately 10% among LM-positive infants with asymptomatic infections. Therefore, the high rates of asymptomatics (and eventually sub-microscopic infections) found in the current study highlights the potential contribution of this age group as a reservoir for malaria transmission. Indeed, a previous study conducted in Burkina Faso has shown that sub-microscopic infections account for nearly 30% of human–mosquito transmission in the country, with a prominent contribution of children over adults to the infectious reservoir [49].
A marked seasonal distribution of malaria cases and infections was also observed, with the highest transmission period (coinciding with the wet season from July to December) accounting for 89 and 77% of all clinical episodes and asymptomatic infections respectively. In this regard, strategies such as SMC in children aged 3–59 months (from August to November) [39] can have an important impact in reducing the malaria burden during the rainy season. However, 23% of all asymptomatic infections (53% of which are also sub-microscopic) occur during the dry season, when SMC is not provided. In this context, SP–IPTi, which is administrated at 3, 4 and 9 months of age following the expanded programme for immunization schedule, can be a crucial strategy to clear asymptomatic infections irrespective of the transmission season, thus avoiding asymptomatic infections to further develop into clinical cases and/or to sustain transmission. Of note, 0.23 clinical malaria episodes per child-year occurred during the first 3 months of life and may be due to new infections or, during the first weeks of life, due to congenital transfer [13, 50–53] with potential life-threatening consequences for the infant at the long-term [53–55]. Currently, there is a lack of particular strategies to specifically target this age group, while the incidence and prevalence of cases and infections together with malaria deaths in this age group are urgently calling for new or improved preventive strategies as well as case management guidelines. In this sense, it could be that additional emphasis on vector control is merited, going for balance between improved drug-based and non-drug based strategies and, also addressing transmission reduction in addition to disease burden reduction.
In this study, 1.5% of infants developed severe malaria, which was lower than that estimated in peripheral health centres (4.2%) between 2014 and 2016 in the central-west region of the country [35, 56]. Although clinical episodes were passively detected in the present study, there was a close follow-up of infants through cross-sectional surveys and sensitization of the mothers for early health seeking for any health issue. Early diagnosis and treatment of clinical malaria episodes has probably contributed to the reduction of severe malaria cases and related-mortality among the study population [57, 58]. Owing to the recent implementation by the Burkina Faso government of medication free of charge for infectious diseases (including malaria) for children under 5 years, a reduction of malaria mortality among infants is expected in the future. The challenge will be to maintain the availability of RDTs and malaria treatments in health centres across the country, which has been intermittent in the past, and to increase the number of health facilities in areas with low coverage.
Overall, the number of malaria episodes and asymptomatic infections vary among the study population with some infants not developing a malaria episode despite carrying parasite infections (asymptomatic infections) at one or several time points during the follow-up, suggesting a potential control or tolerance of malaria infections by some infants [30, 31]. Unfortunately parasite population genotyping, which would have allowed investigation of whether asymptomatic infections detected at cross-sectional surveys were linked to any disease burden, was not performed in the present study.
Variation at individual level could be partially explained by differential benefit of the protective effect of maternal antibodies as their levels may vary from one newborn to another [19, 23, 24, 26, 41, 59]. However, factors that modulate malaria risk/protection in early childhood with regards to the transmission seasonality are not fully understood and further and complementary studies addressing the effect of pregnancy preventive treatments [20, 60], in utero exposure to malaria parasites and/or antigens and subsequent modification of fetal immunity [61–65] and host genetic polymorphisms in specific genes [66–68] are needed.
Conclusions
Despite substantial efforts made in malaria control during this current decade in Burkina Faso, this study showed a high burden of malaria infections, with marked age and seasonal-dependency, during the first year of life in Nanoro. The high rates of asymptomatic infections (with a gametocyte carriage of 10% among LM-positive cases) and of sub-microscopic infections suggest that infants under 1 year old are a potential reservoir for sustaining malaria transmission. Intensified efforts to control malaria in rural Burkina Faso are urgently needed in order to reduce the disease burden in susceptible populations.
Authors’ contributions
HMN, ERV and ARU conceived and designed the study. HMN, MAS, SHZ, HS and MCT supervised data and samples collection in the field. HMN, MAS and SHZ supervised malaria diagnosis and management of malaria patient in peripheral health centers. HMN, PG and ERV performed the qPCR experiments. HMN, ERV and ARU analyzed the data. IV, PFM, HDFHS, HT, LK and ARU contributed for reagents/materials/analysis tools. HMN, ERV and ARU were the major contributors in writing the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We would like to express our sincere gratitude to infants participating in the study and their mothers. We acknowledge nurses, field workers, field supervisors, data managers and laboratory workers at the Clinical Research Unit of Nanoro (CRUN) in Burkina Faso, who played an important role for the successful completion of the study. We also thank the research team at the Malariology Unit at the Institute of Tropical Medicine (ITM), Belgium.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study protocols were reviewed and approved by institutional ethics committees at Centre Muraz, Bobo Dioulasso, Burkina Faso (006-2014/CE-CM), Institute of Tropical Medicine, Antwerp, Belgium (953/14) and University Hospital in Antwerp (UZA), Belgium (14/26/277). Written informed consent was obtained from all mothers.
Funding
The study was supported by the Belgium Directorate General for Development Cooperation (DGD) through the collaborative framework agreement 3 (FA3–DGD programme) between CRUN (Burkina Faso) and ITM (Belgium) and by European community’s Seventh Framework Programme under Grant Agreement No. 305662 (Project: Community-based scheduled screening and treatment of malaria in pregnancy for improved maternal and infant health: a cluster-randomized trial ‘COSMIC’). HMN holds a DGD PhD scholarship (Belgium).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bhatt S, Weiss DJ, Cameron E, Bisanzio D, Mappin B, Dalrymple U. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature. 2016;526:207–211. doi: 10.1038/nature15535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. World malaria report 2016. Geneva: World Health Organization. https://www.who.int/malaria/publications/world-malaria-report-2016/en/. Accessed 17 May 2017.
- 3.Roberts D, Matthews G. Risk factors of malaria in children under the age of five years old in Uganda. Malar J. 2016;15:246. doi: 10.1186/s12936-016-1290-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wanzira H, Katamba H, Okullo AE, Agaba B, Kasule M, Rubahika D. Factors associated with malaria parasitaemia among children under 5 years in Uganda: a secondary data analysis of the 2014 Malaria Indicator Survey dataset. Malar J. 2017;16:191. doi: 10.1186/s12936-017-1847-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zgambo M, Mbakaya BC, Kalembo FW. Prevalence and factors associated with malaria parasitaemia in children under the age of five years in Malawi: a comparison study of the 2012 and 2014 Malaria Indicator Surveys (MISs) PLoS ONE. 2017;12:e0175537. doi: 10.1371/journal.pone.0175537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nyarko SH, Cobblah A. sociodemographic determinants of malaria among under-five children in Ghana. Malar Res Treat. 2014;2014:304361. doi: 10.1155/2014/304361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tiono AB, Kangoye DT, Rehman AM, Kargougou DG, Kaboré Y, Diarra A, et al. Malaria incidence in children in South-West Burkina Faso: comparison of active and passive case detection methods. PLoS ONE. 2014;9:e86936. doi: 10.1371/journal.pone.0086936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ouédraogo A, Tiono AB, Diarra A, Sanon S, Yaro JB, Ouedraogo E, et al. Malaria morbidity in high and seasonal malaria transmission area of Burkina Faso. PLoS ONE. 2013;8:e50036. doi: 10.1371/journal.pone.0050036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Runsewe-Abiodun IT, Ogunfowora OB, Fetuga BM. Neonatal malaria in Nigeria: a 2 year review. BMC Pediatr. 2006;6:19. doi: 10.1186/1471-2431-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uneke CJ. Congenital Plasmodium falciparum malaria in sub-Saharan Africa: a rarity or frequent occurrence? Parasitol Res. 2007;101:835–842. doi: 10.1007/s00436-007-0577-9. [DOI] [PubMed] [Google Scholar]
- 11.Uneke CJ. Congenital malaria: an overview. Tanzan J Health Res. 2011;13:264–280. doi: 10.4314/thrb.v13i3.67615. [DOI] [Google Scholar]
- 12.Dicko-Traoré F, Sylla M, Djimdé AA, Diakité AA, Diawara M, Togo B, et al. Le paludisme congénital et néonatal en Afrique subsaharienne, un évènement rare? J Pediatr Pueric. 2011;24:57–61. [Google Scholar]
- 13.Nagalo K, Dao F, Minodier P, Sawadogo O, Sanon H, Tall FH, et al. Le paludisme congénital maladie à Plasmodium falciparum: aspects épidémiologiques, cliniques, biologiques, thérapeutiques et pronostiques à Ouagadougou, Burkina Faso. Pan Afr Med J. 2014;18:1–7. doi: 10.11604/pamj.2014.18.47.3614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Obiajunwa PO, Owa JA, Adeodu OO. Prevalence of congenital malaria in Ile-Ife, Nigeria. J Trop Pediatr. 2005;51:219–222. doi: 10.1093/tropej/fmi003. [DOI] [PubMed] [Google Scholar]
- 15.Ceesay SJ, Koivogui L, Nahum A, Taal MA, Okebe J, Affara M, et al. Malaria prevalence among young infants in different transmission settings, Africa. Emerg Infect Dis. 2015;21:1114–1121. doi: 10.3201/eid2107.142036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Afolabi BM, Salako LA, Mafe AG, Ovwigho UB, Rabiu KA, Sanyaolu NO, et al. Malaria in the first 6 months of life in urban African infants with anemia. Am J Trop Med Hyg. 2001;65:822–827. doi: 10.4269/ajtmh.2001.65.822. [DOI] [PubMed] [Google Scholar]
- 17.Mbonye MK, Burnett SM, Naikoba S, Colebunders R. Malaria care in infants aged under six months in Uganda: an area of unmet needs! PLoS ONE. 2015;10:e0123283. doi: 10.1371/journal.pone.0123283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Larru B, Molyneux E, Kuile FO, Taylor T, Molyneux M, Terlouw DJ. Malaria in infants below six months of age: retrospective surveillance of hospital admission records in Blantyre, Malawi. Malar J. 2009;8:310. doi: 10.1186/1475-2875-8-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wagner G, Koram K, McGuinness D, Bennett S, Nkrumah F, Riley E. High incidence of asymptomatic malaria infections in a birth cohort of children less than one year of age in Ghana, detected by multicopy gene polymerase chain reaction. Am J Trop Med Hyg. 1998;59:115–123. doi: 10.4269/ajtmh.1998.59.115. [DOI] [PubMed] [Google Scholar]
- 20.Apinjoh T, Anchang-Kimbi J, Mugri R, Njua-Yafi C, Tata R, Chi H, et al. Determinants of infant susceptibility to malaria during the first year of life in South Western Cameroon. Open Forum Infect Dis. 2015;2:ofv012. doi: 10.1093/ofid/ofv012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Le Port A, Watier L, Cottrell G, Ouédraogo S, Dechavanne C, Pierrat C, et al. Infections in infants during the first 12 months of life: role of placental malaria and environmental factors. PLoS ONE. 2011;6:e27516. doi: 10.1371/journal.pone.0027516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.WHO. Intermittent preventive treatment for infants using sulfadoxine- for malaria control in Africa (SP–IPTi) : implementation field guide. 2011. https://apps.who.int/iris/bitstream/10665/70736/1/WHO_IVB_11.07_eng.pdf. Accessed 29 May 2017.
- 23.Branch OH, Udhayakumar V, Hightower AW, Oloo AJ, Hawley WA, Nahlen BL, et al. A longitudinal investigation of IgG and IgM antibody responses to the merozoite surface protein-1 19-kiloDalton domain of Plasmodium falciparum in pregnant women and infants: associations with febrile illness, parasitemia, and anemia. Am J Trop Med Hyg. 1998;58:211–219. doi: 10.4269/ajtmh.1998.58.211. [DOI] [PubMed] [Google Scholar]
- 24.Hogh B, Marbiah NT, Burghaus PA, Andersen PK. Relationship between maternally derived anti-Plasmodium falciparum antibodies and risk of infection and disease in infants living in an area of Liberia, West Africa, in which malaria is highly endemic. Infect Immun. 1995;63:4034–4038. doi: 10.1128/iai.63.10.4034-4038.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khattab A, Chia Y, May J, Le Hasran J, Deleron P, Klinkert M. The impact of IgG antibodies to recombinant Plasmodium falciparum 732var CIDR-1alpha domain in mothers and their newborn babies. Parasitol Res. 2007;101:767–774. doi: 10.1007/s00436-007-0548-1. [DOI] [PubMed] [Google Scholar]
- 26.Deloron P, Dubois B, Le Hesran JY, Riche D, Fievet N, Cornet M, et al. Isotypic analysis of maternally transmitted Plasmodium falciparum-specific antibodies in Cameroon, and relationship with risk of P. falciparum infection. Clin Exp Immunol. 1997;110:212–218. doi: 10.1111/j.1365-2249.1997.tb08319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Amaratunga C, Lopera-Mesa TM, Brittain NJ, Cholera R, Arie T, Fujioka H, et al. A role for fetal hemoglobin and maternal immune IgG in infant resistance to Plasmodium falciparum malaria. PLoS ONE. 2011;6:e14798. doi: 10.1371/journal.pone.0014798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kangoye DT, Nebie I, Yaro JB, Debe S, Traore S, Ouedraogo O, et al. Plasmodium falciparum malaria in children aged 0–2 years: the role of foetal haemoglobin and maternal antibodies to two asexual malaria vaccine candidates (MSP3 and GLURP) PLoS ONE. 2014;9:e107965. doi: 10.1371/journal.pone.0107965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kitua AY, Smith T, Alonso PL, Masanja H, Urassa H, Menendez C, et al. Plasmodium falciparum malaria in the first year of life in an area of intense and perennial transmission. Trop Med Int Health. 1996;1:475–484. doi: 10.1046/j.1365-3156.1996.d01-89.x. [DOI] [PubMed] [Google Scholar]
- 30.Vounatsou P, Smith T, Kitua AY, Alonso PL, Tanner M. Apparent tolerance of Plasmodium falciparum in infants in a highly endemic area. Parasitology. 2000;120:1–9. doi: 10.1017/S0031182099005211. [DOI] [PubMed] [Google Scholar]
- 31.Nash SD, Prevots DR, Kabyemela E, Khasa YP, Lee K-L, Fried M, et al. A Malaria-resistant phenotype with immunological correlates in a Tanzanian birth cohort exposed to intense malaria transmission. Am J Trop Med Hyg. 2017;96:1190–1196. doi: 10.4269/ajtmh.16-0554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Malhotra I, Dent A, Mungai P, Wamachi A, Ouma JH, Narum DL, et al. Can prenatal malaria exposure produce an immune tolerant phenotype? A prospective birth cohort study in Kenya. PLoS Med. 2009;6:e1000116. doi: 10.1371/journal.pmed.1000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Le Hesran JY, Cot M, Personne P, Fievet N, Dubois B, Beyemé M, et al. Maternal placental infection with Plasmodium falciparum and malaria morbidity during the first 2 years of life. Am J Epidemiol. 1997;146:826–831. doi: 10.1093/oxfordjournals.aje.a009200. [DOI] [PubMed] [Google Scholar]
- 34.Wehner S, Stieglbauer G, Traoré C, Sie A, Becher H, Muller O. Malaria incidence during early childhood in rural Burkina Faso: analysis of a birth cohort protected with insecticide-treated mosquito nets. Acta Trop. 2017;175:78–83. doi: 10.1016/j.actatropica.2017.03.017. [DOI] [PubMed] [Google Scholar]
- 35.Burkina Faso: Ministère de la santé. Annuaire statistique 2016. http://www.sante.gov.bf. Accessed 10 May 2017.
- 36.Scott S, Mens PF, Tinto H, Nahum A, Ruizendaal E, Pagnoni F, et al. Community-based scheduled screening and treatment of malaria in pregnancy for improved maternal and infant health in The Gambia, Burkina Faso and Benin: study protocol for a randomized controlled trial. Trials. 2014;15:340. doi: 10.1186/1745-6215-15-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.WHO. Basic malaria microscopy: part I. Learner’s guide. 2nd ed. Geneva: World Health Organization; 2010. http://apps.who.int/iris/bitstream/10665/44208/1/9789241547826_eng.pdf. Accessed 10 Oct 2017.
- 38.Hofmann N, Mwingira F, Shekalaghe S, Robinson LJ, Mueller I, Felger I. Ultra-sensitive detection of Plasmodium falciparum by amplification of multi-copy subtelomeric targets. PLoS Med. 2015;12:e1001788. doi: 10.1371/journal.pmed.1001788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Burkina Faso: Ministère de la santé. Directives nationales pour la prise en charge du paludisme dans les formations sanitaires du Burkina Faso. 2014. http://www.sante.gov.bf. Accessed 28 June 2017.
- 40.Guinovart C, Bassat Q, Sigaúque B, Aide P, Sacarlal J, Nhampossa T, et al. Malaria in rural Mozambique. Part I: children attending the outpatient clinic. Malar J. 2008;7:36. doi: 10.1186/1475-2875-7-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dobbs KR, Dent AE. Plasmodium malaria and antimalarial antibodies in the first year of life. Parasitology. 2016;143:129–138. doi: 10.1017/S0031182015001626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brabin B. An analysis of malaria parasite rates in infants: 40 years after Macdonald. Trop Dis Bull. 1990;87:1–21. [PubMed] [Google Scholar]
- 43.Biggar R, Collins WE, Campbell C. The serological response to primary malaria infection in urban Ghanaian infants. Am J Trop Med Hyg. 1980;29:720–724. doi: 10.4269/ajtmh.1980.29.720. [DOI] [PubMed] [Google Scholar]
- 44.Mwaniki MK, Talbert AW, Mturi FN, Berkley JA, Kager P, Marsh K, et al. Congenital and neonatal malaria in a rural Kenyan district hospital: an eight-year analysis. Malar J. 2010;9:313. doi: 10.1186/1475-2875-9-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Carneiro I, Roca-feltrer A, Griffin JT, Smith L, Tanner M, Schellenberg A, et al. Age-patterns of malaria vary with severity, transmission intensity and seasonality in sub-Saharan Africa: a systematic review and pooled analysis. PLoS ONE. 2010;5:e8988. doi: 10.1371/journal.pone.0008988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Achidi EA, Perlmann H, Salimonu LS, Perlmann P, Walker O, Asuzu MC. A longitudinal study of seroreactivities to Plasmodium falciparum antigens in Nigerian infants during their first year of life. Acta Trop. 1995;59:173–183. doi: 10.1016/0001-706X(95)00076-Q. [DOI] [PubMed] [Google Scholar]
- 47.Riley EM, Wagner GE, Ofori MF, Wheeler JG, Tetteh K, Mcguinness D, et al. Lack of association between maternal antibody and protection of African infants from malaria infection lack of association between maternal antibody and protection of African infants from malaria infection. Infect Immun. 2000;68:5856–5863. doi: 10.1128/IAI.68.10.5856-5863.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Duah NO, Miles DJC, Whittle HC, Conway DJ. Acquisition of antibody isotypes against Plasmodium falciparum blood stage antigens in a birth cohort. Parasite Immunol. 2010;32:125–134. doi: 10.1111/j.1365-3024.2009.01165.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ouédraogo AL, Gonçalves BP, Gnémé A, Wenger EA, Guelbeogo MW, Ouédraogo A, et al. Dynamics of the human infectious reservoir for malaria determined by mosquito feeding assays and ultrasensitive malaria diagnosis in Burkina Faso. J Infect Dis. 2016;213:90–99. doi: 10.1093/infdis/jiv370. [DOI] [PubMed] [Google Scholar]
- 50.Natama HM, Ouedraogo DF, Sorgho H, Rovira-Vallbona E, Serra-casas E, Somé MA, et al. Diagnosing congenital malaria in a high-transmission setting: clinical relevance and usefulness of P. falciparum HRP2-based testing. Sci Rep. 2017;7:2080. doi: 10.1038/s41598-017-02173-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Douamba Z, Dao NGL, Zohoncon TM, Bisseye C, Compaoré TR, Kafando JG, et al. Mother-to-children Plasmodium falciparum asymptomatic malaria transmission at Saint Camille Medical Centre in Ouagadougou, Burkina Faso. Malar Res Treat. 2014;2014:390513. doi: 10.1155/2014/390513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Larkin GL, Thuma PE. Congenital malaria in a hyperendemic area. Am J Trop Med Hyg. 1991;45:587–592. doi: 10.4269/ajtmh.1991.45.587. [DOI] [PubMed] [Google Scholar]
- 53.Ekanem AD, Anah MU, Udo JJ. The prevalence of congenital malaria among neonates with suspected sepsis in Calabar, Nigeria. Trop Doct. 2008;38:73–76. doi: 10.1258/td.2007.005274. [DOI] [PubMed] [Google Scholar]
- 54.Poespoprodjo JR, Hasanuddin A, Fobia W, Sugiarto P, Kenangalem E, Lampah DA, et al. Case report: severe congenital malaria acquired in utero. Am J Trop Med Hyg. 2010;82:563–565. doi: 10.4269/ajtmh.2010.09-0744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Opare DA. Congenital malaria in newborn twins. Ghana Med J. 2010;44:76–78. doi: 10.4314/gmj.v44i2.68888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Burkina Faso: Ministère de la santé. Annuaire statistique 2014. http://www.sante.gov.bf. Accessed 10 May 2017.
- 57.Sirima SB, Konate A, Tiono AB, Convelbo N, Cousens S, Pagnoni F. Early treatment of childhood fevers with pre-packaged antimalarial drugs in the home reduces severe malaria morbidity in Burkina Faso. Trop Med Int Health. 2003;8:133–139. doi: 10.1046/j.1365-3156.2003.00997.x. [DOI] [PubMed] [Google Scholar]
- 58.Gomes MF, Warsame M, Nasemba N, Singlovic J, Kapinga A, Mwankuyse S, et al. Gaining time: early treatment of severe pediatric malaria in Tanzania. Drug Dev Res. 2010;71:92–98. [Google Scholar]
- 59.Akanmori BD, Afari EA, Sakatoku H. A longitudinal study of malaria infection, morbidity and antibody titres in infants of a rural community in Ghana. Trans R Soc Trop Med Hyg. 1995;89:560–561. doi: 10.1016/0035-9203(95)90107-8. [DOI] [PubMed] [Google Scholar]
- 60.Moya-alvarez V, Abellana R, Cot M. Pregnancy-associated malaria and malaria in infants: an old problem with present consequences. Malar J. 2014;13:271. doi: 10.1186/1475-2875-13-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Engelmann I, Santamaria A, Kremsner PG, Luty AJF. Activation status of cord blood gamma delta T cells reflects in utero exposure to Plasmodium falciparum antigen. J Infect Dis. 2005;191:1612–1622. doi: 10.1086/429336. [DOI] [PubMed] [Google Scholar]
- 62.Prahl M, Jagannathan P, McIntyre TI, Auma A, Farrington L, Wamala S, et al. Timing of in utero malaria exposure influences fetal CD4 T cell regulatory versus effector differentiation. Malar J. 2016;15:497. doi: 10.1186/s12936-016-1545-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Flanagan KL, Halliday A, Burl S, Landgraf K, Jagne YJ, Noho-Konteh F, et al. The effect of placental malaria infection on cord blood and maternal immunoregulatory responses at birth. Eur J Immunol. 2010;40:1062–1072. doi: 10.1002/eji.200939638. [DOI] [PubMed] [Google Scholar]
- 64.Adegnika AA, Köhler C, Agnandji ST, Chai SK, Labuda L, Breitling LP, et al. Pregnancy-associated malaria affects toll-like receptor ligand-induced cytokine responses in cord blood. J Infect Dis. 2008;198:928–936. doi: 10.1086/591057. [DOI] [PubMed] [Google Scholar]
- 65.Gbédandé K, Varani S, Ibitokou S, Houngbegnon P, Borgella S, Nouatin O, et al. Malaria modifies neonatal and early-life toll-like receptor cytokine responses. Infect Immun. 2013;81:2686–2696. doi: 10.1128/IAI.00237-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Driss A, Hibbert JM, Wilson NO, Iqbal SA, Adamkiewicz TV, Stiles JK. Genetic polymorphisms linked to susceptibility to malaria. Malar J. 2011;10:271. doi: 10.1186/1475-2875-10-271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hill AV. The immunogenetics of resistance to malaria. Proc Assoc Am Physicians. 1999;111:272–277. doi: 10.1046/j.1525-1381.1999.99234.x. [DOI] [PubMed] [Google Scholar]
- 68.Chapman SJ, Hill AVS. Human genetic susceptibility to infectious disease. Nat Rev Genet. 2012;13:175–188. doi: 10.1038/nrg3114. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.


