Abstract
Context:
The outcome of patients with depressed fracture varies and depends on multiple factors. There has been no previous study on the significance of these factors on the outcome of depressed fracture of the skull and hence this study. Aims: The primary aim of our study is to find the factors affecting the outcome in cases of depressed skull fracture (DSF). This will help us improve outcomes and give more accurate prediction of long-term outcomes.
Settings and Design:
Prospective observational study.
Subjects and Methods:
Institutional Ethics Committee approval was taken for doing this observational study. This was conducted in a tertiary care institute by collecting data of fifty cases of DSFs in 2 years, between January 2012 and December 2013. The study included patients who were diagnosed with DSFs admitted to our tertiary care public hospital. Patients with comorbidity involving injury to other organs or medical disorders and pediatric patients were excluded from our study.
Statistical Analysis Used:
Chi-square test and Fisher exact test. Results: There was a statistically significant impact on age, sex, Glasgow Coma Scale (GCS) score at presentation, type of DSF, and site of DSF in the long-term outcome of patients. The patients with GCS score of 13 or more fared well with good long-term outcome as against those with GCS score below it. Any additional brain injury in the form of hematomas, etc., has a significant negative impact on long-term outcome of the patient and warrant urgent surgical intervention. Complications such as dural tear, cerebral contusions, wound infections, and seizures have adverse effect on the recovery.
Conclusions:
Our observation suggests that patients brought to hospital with minimal delay, with GCS score between 13 and 15, with simple DSF and normal brain parenchyma without dural tear, have the best outcome.
Keywords: Depressed skull fracture, factors influencing outcome in skull fracture, outcome in depressed fracture of skull
Introduction
Head injury is one of the most important public health problems today. One of the varieties of serious head injuries is depressed skull fractures (DSFs).[1] A skull fracture is considered depressed when any portion of the outer table of the fracture line lies below the normal anatomical position of the inner table.[2] DSFs typically occur when objects with a large amount of kinetic energy (e.g., baseball bat, hammer, rock) make contact with the skull over a fairly small area.[3] This type of fracture carries a high risk of increasing pressure on the brain, crushing the delicate tissue. The outcome of patients with depressed fracture varies and depends on multiple factors. There has been no previous study on the significance of these factors on the outcome of depressed fracture of the skull and hence this study.
Subjects and Methods
Institutional Ethics Committee approval was taken for doing this observational study. This was conducted in a tertiary care institute by collecting data of fifty cases of DSFs over a period of 2 years, between January 2012 and December 2013. The study included patients who were diagnosed with DSFs admitted to our tertiary public hospital.
History and examination
On admission, a detailed history was taken, and thorough clinical examination of all patients was carried out. Assessment of pupillary size/reactivity and level of consciousness (as per Glasgow Coma Scale [GCS]) was carried out. The neurological reassessment was carried out frequently to identify any neurological deterioration. The local wound was inspected for external evidence of fracture and contamination.
Radiological examination
Computerized tomography (CT) scan was the imaging modality of choice. Plain CT scan brain with bone window cuts was taken. The benefit of getting a CT scan was the visualization of bone status in addition to diagnosing parenchymal injury.
Inclusion criteria
Age of 12 years or more
Patients with DSFs.
Exclusion criteria
Age <12 years
Patients with severe comorbid injuries involving other organs
Patients with severe comorbid medical disorders.
Standard preoperative steps
All the patients were given prophylactic antibiotics and anticonvulsants. The antibiotic given was cefotaxime 1 g 12 hourly in patients with clean wounds and 2 g 12 hourly in patients with gross contamination of the wound. Primary care such as hydration with intravenous (IV) fluids, cleaning and dressing of wound was carried out.
Investigations
Blood investigations
Routine biochemical investigations including hemoglobin, complete blood counts, serum electrolytes, liver function test, renal function test, random blood sugar, blood grouping, and cross match along with arterial blood gases were done.
Radiological investigations
X-ray skull, X-ray cervical spine, and X-ray chest posteroanterior view were done in all patients. In selected cases, relevant X-rays of abdomen, long bones, pelvis, and hips were done. Ultrasonography of abdomen and thorax were done whenever required.
Operative procedure
Standard surgical procedures done were as follows:
Elevation of depressed bone fragment
Removal of in-driven bone fragment with thorough washes
Repair of dural tear if any
Evacuation of hematoma if any
Hemostasis
Debridement of wound margin and primary repair.
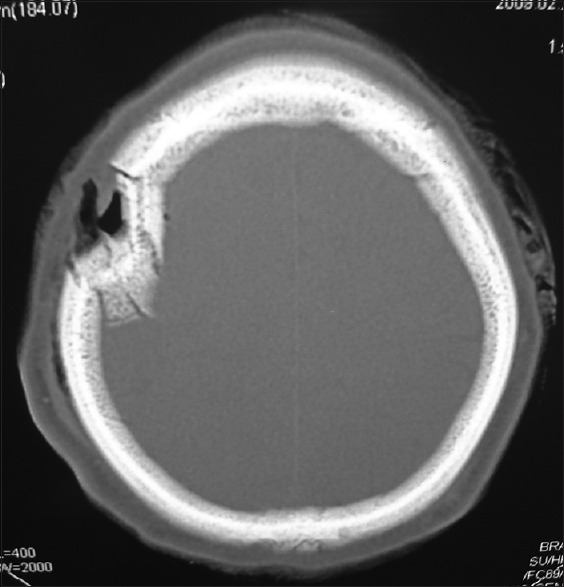
Figure 1 shows intraoperative picture of a depressed fracture.
Figure 1.

Intraoperative picture of a depressed fracture near the midline. Burr holes have been placed near the depressed segment to elevate it
Postoperative management
In postoperative management of head injury trauma, the airway was maintained using either mouth airway tube, intubation or tracheostomy. Ventilatory support was provided if required. The patient was given propped up position to reduce raised intracerebral pressure. IV fluids were started to maintain electrolyte and metabolic balance. IV antibiotics were given to prevent meningitis. Anticonvulsants - injection phenytoin and injection phenobarbitone - were given to prevent posttraumatic seizures. IV 20% mannitol 100 ml 8 hourly was given to reduce cerebral edema in the case of raised Intracranial Tension (ICT).
Follow-up
Patients were asked to follow-up over a period of 6 months after discharge to assess long-term outcome and complications. Postmortem was done in all cases of mortality.
The outcome was measured by GCS [Table 1] as good when a course inward postoperatively was uneventful and poor when the patient developed some residual focal neurological deficit, posttraumatic seizure disorder, vegetative state, or death in hospital in due course of treatment.[4]
Table 1.
Glasgow outcome scale

Study of outcome with respect to following variables
Age and sex
Mode of injury
GCS score on admission
Prehospitalization delay
Site of fracture
Additional component of head injury
Type of depressed fracture (simple or compound)
Complications of DSFs.
Results
The study group consisted of fifty patients. All these patients were analyzed according to:
Symptoms
Mode of management
Final outcome and analysis of factors affecting it
Complications of depressed fracture and their relation to outcome.
Symptoms
The symptoms with which our patients presented are as shown in Table 2.
Table 2.
Distribution of symptoms in our study population

Mode of management
Out of fifty patients in study group, 24 (48%) were operated, and 26 were managed conservatively. The criteria for surgical management included:
Break in continuity of skin with gross contamination of wound
Brain matter pouting through the wound
Grossly depressed segment of bone
Cerebrospinal fluid (CSF) leak
Seizures
Associated CT findings showing operable indication
Neurological deficit
Meningitis.
In the absence of these criteria, we have managed the patient conservatively [Figure 2].
Figure 2.

Graphical representation on mode of management of patients in our series
Illustrative cases
A 34-year-old male with depressed fracture in the right frontal bone with external break in skin integrity with no significant contamination or neurological deficit. CT showed a depressed fracture in the right frontal bone with no underlying parenchymal injury [Figure 3]. This patient was managed conservatively and had a good outcome
A 26-year-old male with depressed fracture in the left posterior parietal bone presented to us with overlying contused lacerated wound and contamination of the wound. GCS was 14/15 and with disoriented speech. CT revealed underlying contusion in the left posterior parietal region [Figure 4]. The patient was operated, and the depressed segment was excised (due to contamination) with the dural repair. Postoperative CT showed resolution of contusion with postoperative bony defect [Figure 5].
Figure 3.
Computerized tomography scan bone window showing depressed fracture or right frontal bone
Figure 4.

Axial plain computerized tomography image showing postoperative changes with resolution of contusion
Figure 5.

Axial plain computerized tomography image showing depressed fracture in left posterior parietal bone with underlying contusion
Final outcome and analysis of factors affecting it
The graphical [Figure 6] and tabular presentation [Table 3] of final outcome of patients in our series.
Figure 6.

Three-dimensional bar chart showing graphical representation of outcome in our series
Table 3.
Long-term outcome in our series

Tabular representation of variable factors and outcomes in our series are as shown in Table 4.
Table 4.
Factors influencing outcome in our series
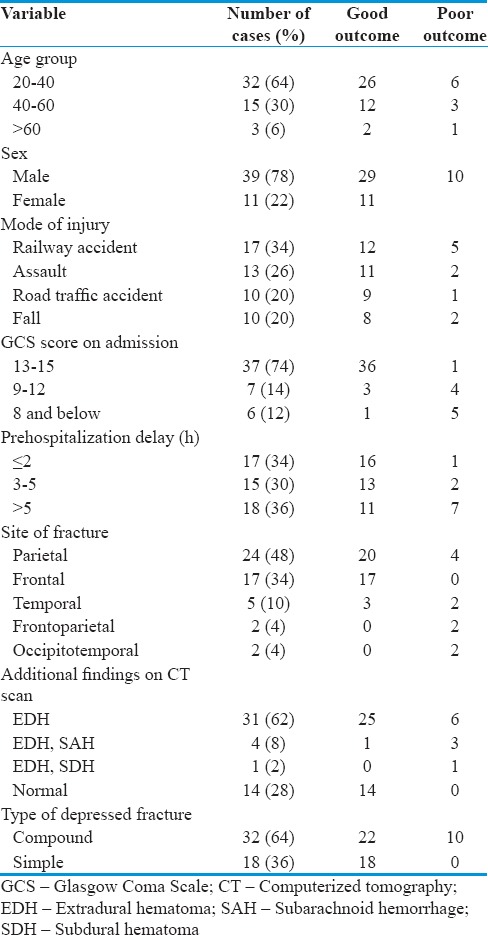
Age distribution and their correlation with outcome
Most of the patients were in the 20–40 age group and this correlates well with the fact that trauma is a disease affecting the young. The mean age was 37.6 ± 12.8 years. We found in our study group that as age increased, outcome worsened. Age group of 20–40 years had the most number of patients with good outcome (81.3%).
Sex distribution and their correlation with outcome
An overwhelming majority of patients were males (78%), and they also had poorer outcomes as compared to females. This can be explained by their involvement in more severe trauma.
Mode of injury and their correlation with outcome
Railway accidents were the most common mode of injury in our series. Analysis of data using Chi-square test revealed a P = 0.62 indicating no significant correlation of mode of injury with the outcome.
Glasgow Coma Scale score at admission and their correlation with outcome
It was observed that as the GCS score at presentation decreased, the morbidity and mortality among patients increased. Nearly 97.3% patients who presented with GCS between 13 and 15 had good outcome as against 16.7% patients who had GCS of 8 or below. We found significant statistical correlation between GCS at presentation and final outcome of patient (P < 0.01).
Prehospital delay and their correlation with outcome
There was no significant statistical relationship between prehospital delay and outcome (P < 0.38), but we observed that as the time to reach hospital increased, morbidity and mortality increased among study groups.
Site of fracture and their correlation with outcome
Most common site for DSF in our study group was parietal region (48%). Patients with frontal bone fractures had the best outcome (100% good) and worst in those involving more than two bones (100% poor). Statistically significant association was found between site of fracture and outcome (P < 0.01). This can probably be explained by the fact that when two or more bones are involved in fracture, the amount of trauma will be more.
Additional computerized tomography scan findings and their correlation to outcome
The most common additional CT scan finding was found to be extradural hematoma (EDH) (62%). Statistically significant association was found between outcome and additional CT findings like intracranial bleed (P < 0.01).
Type of depressed skull fracture
Statistically significant correlation was found between type of DSF and outcome. Patients with simple DSF had better outcome (100% good) as compared to those with compound DSF (68.8% good).
Complications of depressed skull fractures
Tabular [Table 5] and graphical representation [Figure 7] of complications associated with DSF in our series.
Table 5.
Complications seen in our series patients

Figure 7.
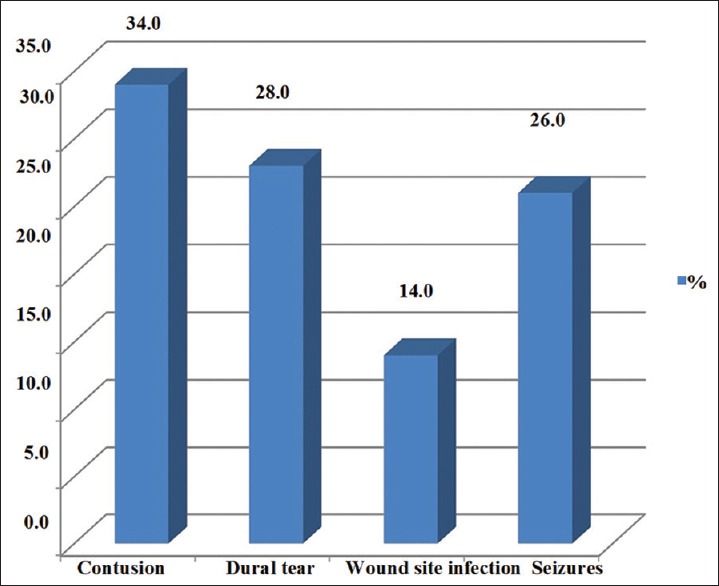
Graphical representation of complications seen in our series
There was significant correlation between outcome and brain contusions (P < 0.01). The patients with contusions showed poor outcome (47.1%) as against those without it (97%). Similarly, there was a significant association between dural tear and long-term outcome of patients in our study (P < 0.01). Nearly 97.2% patients of those without dural tear had good outcome as against 35.7% of those having a dural tear. Patients with wound infection had greater morbidity and mortality (71.4%) than those without it. Statistically significant relation was found between long-term outcome and wound infection (P < 0.01). There was significant correlation between the presence of seizures and poor outcome (P < 0.01).
Discussion
Trauma is a huge problem in both developing and developed countries. Head injury largely contributes to the mortality and morbidity of trauma patients. The incidence of head injuries is steadily increasing, which has led to increased concerns on management and to improve outcome.
In DSF, the outer table of one or more of the fracture edges lies below the normal anatomical level of the inner table as determined by the surrounding intact skull.[1,2]
Patients with DSFs present with a history of trauma, depression over the skull, neurological signs, seizure, CSF leak, or brain matter coming through the wound.[3]
Plain X-ray skull will demonstrate the fracture, type, location, and degree of depression. CT scan is helpful in the diagnosis of skull fracture and associated intracranial lesion. DSF is a common variety in traumatic head injury, and with the advent of better imaging modalities such as CT scan, their detection has increased. In general, CT is more useful in demonstrating depressed fractures except when they are at the vertex.[5]
Both conservative and surgical methods can be adopted for the management of these patients depending on cosmetic and functional outcomes.
Comparing the general factors in our fifty patients with other studies, we noted few factors affecting the outcome in these patients. These were age, sex, GCS on presentation, site of DSF, type of DSF, associated CT findings, the presence of contusions in brain, dural tear, infection, seizures at presentation or postoperatively, and treatment given.
In our study, the mean age of presentation was 37.6 years. Maximum number of patients (64%) belonged to the working population in age group of 20–30 years who were at special risk of road traffic and railway accidents while commuting. Assault was also common in the same age group. The outcome became worse with increase in age from 18.8% in age group of 20–40 years to 33.3% in group of >60 years. These findings are similar to multiple studies done earlier.[6]
In the present study, 39 (78%) cases out of 50 were males and 11 (22%) were females. Among admitted patients male:female ratio was 3.5:1. All the females had good outcome (100%) as compared to males (74.4%). In a similar study done by Mumtaz et al., 35.71% cases were females and 64.28% were males.[3]
The most common mode of injury was railway accident (34%). Morbidity and mortality (29.4%) was more common in railway accidents. Jaggar et al. evaluating compound depressed fractures found that the road traffic accident was the most frequent mechanism of injury.[6,7] In the series by Swann et al., assault was the principle mode of injury.[8] Heary et al. suggested that injuries were roughly equal between assault and road traffic accidents.[9] A similar study done by Al-Derazi et al. shows that an accidental heavy object fall on the head was the cause of injury in 36 (30%) of patients, which occurred mainly during industrial work or building constructions.[10] Fall from height was the cause in 19 patients (24%) and road traffic accident in 24 patients (20%). Depressed fractures as a cause of assault were documented in 22 patients (19.8%), sports injury in 13 patients (10%), and suicide attempt in two patients (1.53%).[10] The predominance of a particular type of mode of injury can be due to selection bias in a hospital which caters to a particular subsection of society such as construction workers or trauma center on a highway.
The patients with GCS score of 13 or more (74%) fared well with better long-term outcome as against those with GCS score below it. Patients with preoperative GCS in the range of 13–15 were 37 (74%), in the range of 9–12 were 7 (14%), and those below 8 were 6 (12%). In a similar study by Hossain et al., patients with preoperative GCS in the range of 13–15 were 50%, 9–12 were 31%, and those who presented with GCS of 8 or lower were 19%.[11]
In our study groups, 52% patients were managed conservatively as against 70% by Al-Derazi et al.[10] The primary question facing the neurosurgeon with regard to DSF is whether or not to operate. Heary et al. reported a group of patients with compound DSFs in which nonsurgical therapy was used for a subgroup of 26 patients without clinical or radiographic evidence of dural violation or significant underlying brain injury.[9] Similarly, van den Heever and van der Merwe reported an equally low incidence of infection in a group of nonoperatively treated patients which included 139 compound depressed fractures.[12]
The most common site for DSF in our study group was parietal region (48%), followed by frontal (34%) and temporal (10%). Those involving more than one area were 2% each in frontoparietal and occipitotemporal. The patients with involvement of two or more scalp bones or extensive neuroparenchymal damage had more morbidity and mortality. In a study by Al-Derazi et al., the sites for DSF were frontal (32%), parietal (44%), temporal (18%), and occipital (6%) which matches those of our study group.[10]
Compound DSF was seen in 32 patients (64%) while 18 had simple or closed DSF. Patients with simple DSF had better outcome (100% good) as compared to those with compound DSF (68.8% good). In a study by Al-Derazi et al., compound DSF was present in 86 (72%) patients and simple in 34 (28%) patients.[10]
Additional CT findings in our study group were EDH (62%), cerebral contusions (34%), and dural tear (14%). In the study by Hossain et al., findings were EDH (22%), brain contusions (31%), dural tear (25%), and in-driven bone fragment (13%).[11]
Of all the patients treated, seven developed infectious complications, for whom morbidity and mortality was found to be higher than those without infection. Those with meningitis were given antibiotics based on CSF culture and sensitivity. Debridement of osteomyelitic bone was done in one patient with osteomyelitis of fractured bone fragment. In a patient with cerebral abscess, surgical drainage was done along with antibiotic therapy.
Haines concluded that it is unclear whether all patients with compound DSFs required antibiotic treatment.[13] The controlled study for all types of neurosurgical craniotomies of van Ek et al. showed a statistically significant reduction in the infection rate in the group given antibiotics.[14] A study from South Africa by van den Heever and van der Merwe and that of Heary et al. from the USA presented a detailed description of a nonsurgical management plan.[9,12]
Conclusion
Our study could find a few significant factors which influence the outcome of depressed fractures. Those who were young (20–40 years) had more chances of having uncomplicated course of treatment and uneventful recovery. There was a statistically significant impact of GCS score at presentation, type of DSF, and site of DSF in the long-term outcome of patients. The patients with GCS score of 13 or more fared well with better long-term outcome as against those with GCS score below it. Any additional brain injury in the form of hematomas, etc., has a significant negative impact on long-term outcome of the patient and warrant urgent surgical intervention. Complications such as dural tear, cerebral contusions, wound infections, and seizures have adverse effect on the recovery of patient. This usually leads to increased stay in hospital, increased morbidity and mortality.
Thus, our observation suggests that patients brought to hospital with minimal delay, with GCS score between 13 and 15, with simple DSFs and normal brain parenchyma without dural tear, have the best outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cooper PR, editor. 3rd ed. Baltimore: Williams and Wilkins; 1993. Skull fracture and traumatic cerebrospinal fluid fistulas. In: Head Injury; pp. 115–36. [Google Scholar]
- 2.Vollmer DG, Dacey RG, Jane JA. Cranio-cerebral-trauma. In: Joynt RJ, editor. Clinical Neurology. Vol. 3. Philadelphia: Lippincott; 1991. pp. 1–79. [Google Scholar]
- 3.Mumtaz A, Ali L, Roghani IS. Surgical management of depressed skull fracture. J Postgraduate Med Inst. 2003;17:46–8. [Google Scholar]
- 4.Jennett B, Snoek J, Bond MR, Brooks N. Disability after severe head injury: Observations on the use of the Glasgow Outcome Scale. J Neurol Neurosurg Psychiatry. 1981;44:285–93. doi: 10.1136/jnnp.44.4.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cowan BF, Segall HD, Zee CS. Neuroradiological Assesment of Depressed Skull Fracture: Axial Versus Skull Roentgenography. Western Neuroradiological Society Annual Meeting. 1980 Oct [Google Scholar]
- 6.Jaggar J, Levin JI, Jane JA. Epidemiologic features of head injury in a predominant rural population. J Trauma. 1984;24:40–4. doi: 10.1097/00005373-198401000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Jamieson KG, Yelland JD. Depressed skull fractures in Australia. J Neurosurg. 1972;37:150–5. doi: 10.3171/jns.1972.37.2.0150. [DOI] [PubMed] [Google Scholar]
- 8.Swann IJ, MacMillan R, Strong I. Head injuries at an inner city accident and emergency department. Injury. 1981;12:274–8. doi: 10.1016/0020-1383(81)90200-x. [DOI] [PubMed] [Google Scholar]
- 9.Heary RF, Hunt CD, Krieger AJ, Schulder M, Vaid C. Nonsurgical treatment of compound depressed skull fractures. J Trauma. 1993;35:441–7. doi: 10.1097/00005373-199309000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Al-Derazi T, Das K, Gupta PK, Thajudeen BA, Ravindra J. Management strategy of depressed skull fractures. Pan Arab J Neurosurg. 2008;12:80–5. [Google Scholar]
- 11.Hossain MZ, Mondle MS, Monzurul Hoque M. J Teach Assoc. 2008;21:140–6. [Google Scholar]
- 12.van den Heever CM1, van der Merwe DJ. Management of depressed skull fractures.Selective conservative management of nonmissile injuries. J Neurosurg. 1989;71:186–90. doi: 10.3171/jns.1989.71.2.0186. [DOI] [PubMed] [Google Scholar]
- 13.Haines SJ. Systemic antibiotic prophylaxis in neurological surgery. Neurosurgery. 1980;6:355–61. [PubMed] [Google Scholar]
- 14.van Ek B, Dijkmans BA, van Dulken H, van Furth R. Antibiotic prophylaxis in craniotomy: A prospective double-blind placebo-controlled study. Scand J Infect Dis. 1988;20:633–9. doi: 10.3109/00365548809035664. [DOI] [PubMed] [Google Scholar]


