Abstract
Introduction:
Parinaud's Syndrome is an inability to move the eyes upwards which is caused by damage to the tectal plate of midbrain. Commonest causes implicated are the Pineal tumors in children, Multiple Sclerosis in adults and stroke in elderly patients. We present a rare case of Tectal plate tuberculoma leading to Parinaud's Syndrome.
Discussion:
Parinaud's syndrome is caused by damage to the tectal plate or posterior commissure of midbrain. Our patient presented with upward gaze paresis and was diagnosed to have tuberculoma involving the midbrain region. He was managed conservatively and responded to the treatment.
Conclusion:
Tectal plate tuberculoma though a rare possibility, warrants proper diagnostic workup in order to prevent unnecessary brainstem surgery.
Keywords: Hydrocephalus, parinaud's syndrome, tectal plate, tuberculoma
Introduction
Parinaud's Syndrome is an inability to move the eyes upward. It is caused by the compression of vertical gaze center at the rostral interstitial nucleus of medial longitudinal Fasciculus.[1] The most common causes implicated are the pineal tumors in children, multiple sclerosis in adults, and stroke in elderly patients.[2] However, an isolated tectal plate tuberculoma as a cause of Parinaud's syndrome is never reported. We present a case of an adult male who presented with restriction of upward gaze due to tectal plate tuberculoma. He was managed with ventriculoperitoneal shunt and antitubercular medical treatment.
Case Report
Forty-year-old male came to our outpatient department with complaints of headache, vomiting and blurring of vision since 15 days. He also narrated a history of increased somnolence, difficulty in looking upward and urinary incontinence. On admission, the patient was conscious and oriented with Glasgow Coma Scale 15/15. Clinically, he had upward gaze palsy and vertical diplopia with convergence retraction nystagmus on attempted upward gaze. Fundoscopy revealed bilateral pappilledema. He was investigated with computed tomography (CT) and magnetic resonance imaging (MRI) brain along with other routine preoperative workup.
MRI brain revealed two lesions in the Tectum of midbrain measuring 13 mm × 11 mm × 10 mm and 7 mm × 8 mm × 6 mm extending into the quadrigeminal cistern. These lesions were isointense on T1 and hypointense on T2 weighted images. Contrast study showed intense peripheral enhancement. Mass effect in the form of compression of aqueduct with dilatation of both lateral and third ventricles was evident.
CT brain revealed two conglomerated ring enhancing lesions in the median and left paramedian tectum of the midbrain. [Figure 1] Cerebrospinal fluid (CSF) study was suggestive of lymphocyte predominance with marginally elevated adenosine deaminase (ADA) levels and polymerase chain reaction was positive for Mycobacterium tuberculosis (MT). Erythrocyte sedimentation rate (ESR) was 48 mm at the end of 1 h. High-resolution CT chest and CT abdomen did not show any tuberculous involvement, and sputum examination for acid-fast bacilli was inconclusive [Figures 2 and 3].
Figure 1.
Postcontrast image showing peripherally enhancing lesion involving tectal plate
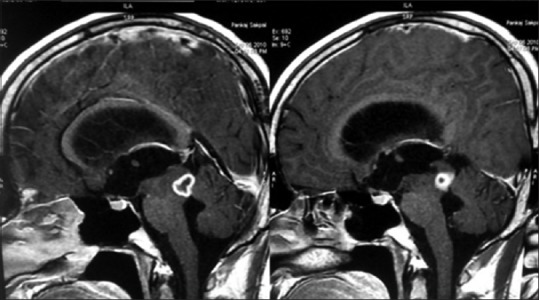
Figure 2.
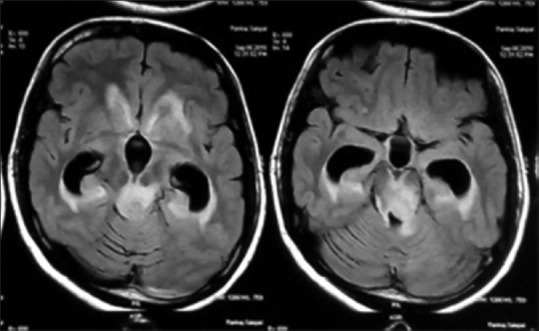
Tectal lesion with significant perilesional edema and hydrocephalus
Figure 3.
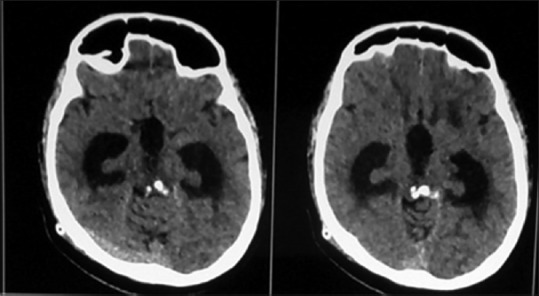
Computed tomography brain – calcified tectal lesion causing hydrocephalus
Considering the obstructive hydrocephalus patient undergone ventriculoperitoneal shunt. CSF opening pressure was high. Postoperatively, the patient improved symptomatically after surgery. Headache relieved immediately. Urinary incontinence and visual blurring improved gradually over 3–4 days but vertical gaze paresis persisted. He was given Anti Kochs for 12 months.
Regular follow-up was done. MRI brain after 6 months and 1 year demonstrated reduction in the size of the lesion and perilesional edema. Gradually, the lesion got calcified. Clinically, the patient improved except persistent features of Parinaud's syndrome.
Discussion
Parinaud's syndrome is a group of abnormalities of eye movement and pupillary dysfunction. It is caused by damage to the tectal plate or posterior commissure of midbrain. It is named after Henry Parinaud, a French ophthalmologist (1844–1905). The syndrome consists of upward gaze paresis, Pseudo-Argyll Robertson pupils, Convergence-Retraction nystagmus, Eyelid retraction, and Conjugate down gaze in the primary position (setting-sun sign).[1]
It is commonly caused by pineal gland tumors or midbrain infraction. Other causes are arteriovenous malformations, demyelinating disorders, obstructive hydrocephalus, etc.[3,4]
Central nervous system (CNS) tuberculosis (TB) is a serious form of TB, due to hematogenous spread of MT. Intracranial tuberculomas are the least common presentation of CNS TB, found in 1% of these patients. Tuberculomas develop in the brain when the initial “Rich focus” does not rupture into the meninges but expands locally within the brain parenchyma.[3]
CNS TB is very rampened in India but isolated involvement of tectal plate with tuberculomas was rarely seen; hence, the initial diagnosis was tectal plate glioma or metastatic lesion. However, CSF examination did not reveal any malignant cells and elevated ADA levels pointed toward possible primary CNS TB [Figure 4].
Figure 4.
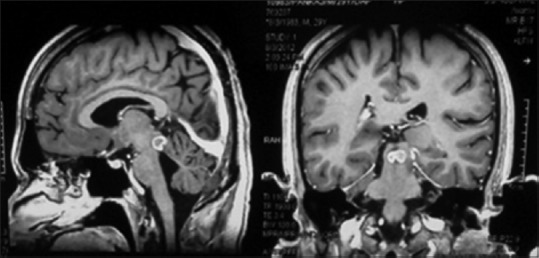
Follow-up image 6 months after shunt procedure and medical management showing decrease in size of the lesion with resolved hydrocephalus
In our case, tectal plate and posterior commissure were involved causing secondary aqueductal stenosis and hydrocephalus. Shunt procedure took care of the hydrocephalus. Gradually, the patient responded to anti-Koch's treatment also. However, damage of posterior commissure fibers resulted in persistence of features of Parinaud's syndrome. Now the patient is referred to ophthalmologist for correction of gaze paresis.
Conclusion
While dealing cases with Parinaud's syndrome Tectal tuberculomas should also be considered as a possibility as correct and timely diagnosis can prevent unindicated surgery for biopsy or excision of the lesion.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Wilkins RH, Brody IA. Neurological classics. XLI. Parinaud's syndrome. Arch Neurol. 1972;26:91–3. doi: 10.1001/archneur.1972.00490070109014. [DOI] [PubMed] [Google Scholar]
- 2.Quint DJ, Cornblath WT, Trobe JD. Multiple sclerosis presenting as Parinaud syndrome. AJNR Am J Neuroradiol. 1993;14:1200–2. [PMC free article] [PubMed] [Google Scholar]
- 3.Pimentel ML, Alves SM, Novis SA, Brandão RZ, Belo Neto E. Intracranial tuberculomas developing during treatment of pulmonary tuberculosis: Case report. Arq Neuropsiquiatr. 2000;58:572–7. doi: 10.1590/s0004-282x2000000300028. [DOI] [PubMed] [Google Scholar]
- 4.Keane JR. The pretectal syndrome: 206 patients. Neurology. 1990;40:684–90. doi: 10.1212/wnl.40.4.684. [DOI] [PubMed] [Google Scholar]


