Abstract
Melanocytoma is rare pigmented tumor of the leptomeninges which arise from the neural crest. Intramedullary location of the tumor is extremely rare, and only a few case reports are available in the literature. We report a case of 35-year-old female with the entity who had a near total removal of the intramedullary tumor with good postoperative outcome. The available literature is reviewed.
Keywords: Cervicothoracic tumor, intramedullary tumor, melanocytoma
Introduction
Melanocytoma is a rare pigmented neoplasm of the leptomeninges first described in 1972 by Limas and Tio.[1] Melanocytoma is derived from scattered melanocytes that are present in the leptomeninges. They usually have an intracranial localization but also involve the spinal column, where they are most often detected as an intradural extramedullary lesion.[2,3,4] Intramedullary lesion of the spine is an extremely rare entity, and after searching PubMed database and Google search, we were able to find only 24 cases having this entity [Table 1]. We report a case of 35-year-old female with this entity and the available literature is reviewed.
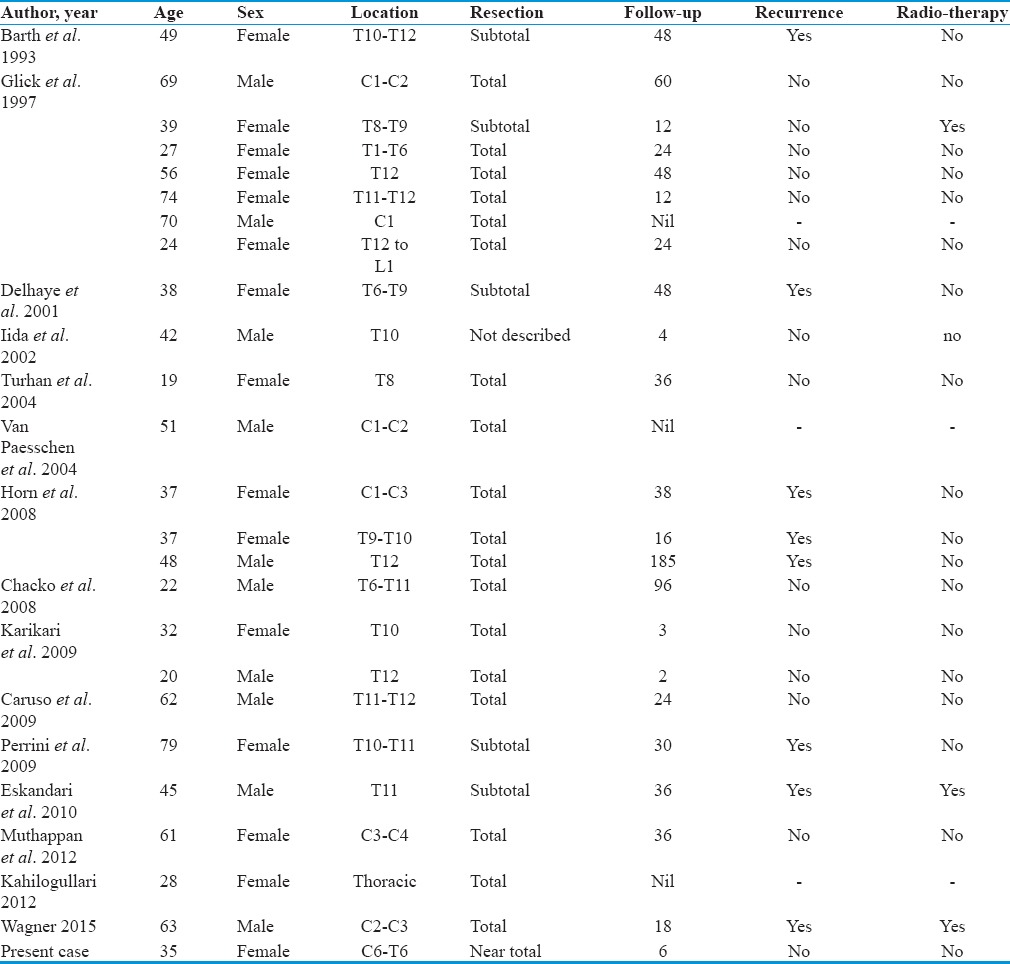
Table 1.
The comparison of previous case reports with present case
Case Report
A 35-year-old female presented with complaints of pain over lower cervical and upper thoracic region and progressive spastic paraparesis for the last 1½ years. On neurological examination, there was spastic paraparesis with power of grade 3/5 at bilateral hips and 1/5 at B/L ankle joints. There was no bladder or bowel involvement.
On magnetic resonance imaging (MRI), there was an intramedullary mass present from C7 to D6 level. It was heterogeneously hyperintense on T1-weighted image and hypointense on T2-weighted image. There were syrinx formation and edema of cord both cranial and caudal to the lesion. MRI contrast images showed heterogeneous enhancement of the lesion [Figure 1].
Figure 1.

(a) Preoperative T1-weighted magnetic resonance imaging, (b) preoperative magnetic resonance imaging T1 with gadolinium, (c) preoperative magnetic resonance imaging T2-weighted image
A C6 to D7 laminectomy was performed. Dura opened in the midline and tented laterally. Arachnoid opened. A standard midline myelotomy was performed through the posterior median septum. Intraoperatively, a dark black intramedullary mass was found having intratumoral tangle of vessels. Part of the tumor was demarcated from surrounding spinal cord tissue, but the tumor was infiltrating anteriorly to the spinal cord tissue at some places. A near total excision was performed. Histopathological examination [Figure 2] revealed heavy brown pigment in the cell cytoplasm which was consistent with melanocytoma. Postoperatively, patient's condition gradually improved. There was improvement in the power of lower limbs. After 6 months, the power in bilateral lower limb was of grade 4/5, and she was able to stand and walk without support.
Figure 2.
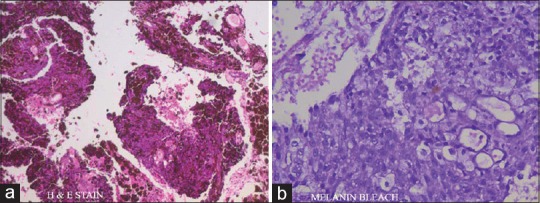
(a) H and E stain, (b) melanin bleach stain
Six months follow-up MRI contrast showed postoperative changes from C6 to D7 level with a small area of minimal contrast uptake suggestive of near total excision [Figure 3].
Figure 3.
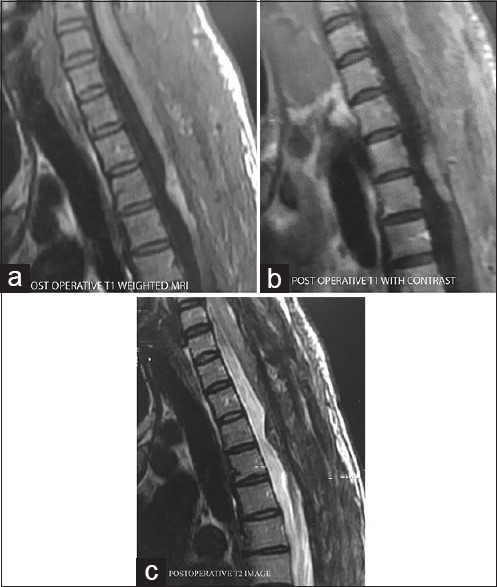
(a) Postoperative magnetic resonance imaging T1-weighted image, (b) Postoperative magnetic resonance imaging T1 with gadolinium, (c) postoperative magnetic resonance imaging T2-weighted image
Table 1 shows the comparison of previous case reports with the present case.[5]
Discussion
Primary melanocytic tumors of the spine are part of a spectrum of rare neoplasm derived from scattered melanocytes located in the leptomeninges. The World Health Organization has classified melanocytic lesions of the central nervous system (CNS) into[1] diffuse melanocytosis and melanomatosis,[2] melanocytoma, and[3] malignant melanoma. The melanocytic lesions of CNS have been classified as low, intermediate, and high grades by Brat et al.[2] These melanocytes are most frequently encountered at the posterior fossa and upper part of the cervical spinal cord.[1,6]
These tumors were first described as meningeal melanocytoma by Limas and Tio in 1972.[1] Melanocytoma is commonly solitary, low-grade neoplasms that do not invade surrounding structures. In the spine, they usually present as intradural extramedullary lesions.[2,3,4] In cases with intraparenchymal localization, the melanocytes most probably originate from the Virchow–Robin spaces.[5,6] Intramedullary melanocytoma is extremely rare and very little data exist to guide the clinicians about the management of the patients with this entity.
MRI with gadolinium is the preferred imaging modality for the diagnosis of melanocytoma. Intramedullary melanocytoma lacks characteristic imaging features. Typical MRI findings are that of an intramedullary lesion iso- to hyper-intense on T1-weighted sequences, hypointense on T2-weighted sequences, and with homogeneous enhancement.[5,7] In our case, mass was hyperintense on T1-weighted images and hypointense on T2-weighted images, and it showed heterogeneous enhancement. These signal features are biased by variable degrees of tumor melanization that affects the signal characteristics on MRI.[5] Diagnosis on the basis of MRI findings is still challenging as individual appearances may vary widely.
Enough clinical evidence exists, based on multiple small case reports and series, to show that gross total resection is the initial treatment of choice for the management of these tumors; however, the question remains about the best possible follow-up method for postsurgical patients and how residual tumor or recurrences should be managed. Local control rates have been shown to be four times higher if complete resection is achieved and morbidity and mortality rates for incomplete resection now mandate the use of adjuvant radiation therapy.[3,8,9,10,11,12] Although they are considered to be a benign tumor, melanocytomas have been reported to recur even after gross total resection.[11] Rades and Schild[10,11] have proposed high-dose local radiation, even in cases of complete tumor resection, to prevent local recurrence. More aggressive approaches have also been advocated including re-resection of recurring tumor and reservation of adjuvant radiotherapy for those lesions that cannot be completely resected.[8]
Close postoperative monitoring and diligent follow-up, even in the case of gross total resection, is extremely important. Although these tumors are histopathologically benign, they do have an aggressive clinical course secondary to their location and the mass effect they impose within the spinal cord. It is therefore crucial that recurrences should be caught early as this allows for early adjuvant therapy or re-resection. Hopefully, more reports and longer follow-up periods after surgical resection, recurrence, and subsequent treatment will enable clinicians to render more accurate information as to the best treatment for melanocytomas.
Conclusion
Melanocytoma is an extremely rare entity. The lack of distinctive imaging characteristics increases the challenge during preoperative diagnosis. Complete surgical excision should be advocated as optimal treatment. The question remains whether more aggressive early adjuvant therapy should play a role in treating patients with these benign, yet locally aggressive intramedullary tumors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Limas C, Tio FO. Meningeal melanocytoma (“melanotic meningioma”). Its melanocytic origin as revealed by electron microscopy. Cancer. 1972;30:1286–94. doi: 10.1002/1097-0142(197211)30:5<1286::aid-cncr2820300522>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 2.Brat DJ, Giannini C, Scheithauer BW, Burger PC. Primary melanocytic neoplasms of the central nervous systems. Am J Surg Pathol. 1999;23:745–54. doi: 10.1097/00000478-199907000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Horn EM, Nakaji P, Coons SW, Dickman CA. Surgical treatment for intramedullary spinal cord melanocytomas. J Neurosurg Spine. 2008;9:48–54. doi: 10.3171/SPI/2008/9/7/048. [DOI] [PubMed] [Google Scholar]
- 4.Turhan T, Oner K, Yurtseven T, Akalin T, Ovul I. Spinal meningeal melanocytoma. Report of two cases and review of the literature. J Neurosurg. 2004;100(3 Suppl):287–90. [PubMed] [Google Scholar]
- 5.Wagner F, Berezowska S, Wiest R, Gralla J, Beck J, Verma RK, et al. Primary intramedullary melanocytoma in the cervical spinal cord: Case report and literature review. Radiol Case Rep (Online) 2015;10:1010. doi: 10.2484/rcr.v10i1.1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glick R, Baker C, Husain S, Hays A, Hibshoosh H. Primary melanocytomas of the spinal cord: A report of seven cases. Clin Neuropathol. 1997;16:127–32. [PubMed] [Google Scholar]
- 7.Karikari IO, Powers CJ, Bagley CA, Cummings TJ, Radhakrishnan S, Friedman AH. Primary intramedullary melanocytoma of the spinal cord: Case report. Neurosurgery. 2009;64:E777–8. doi: 10.1227/01.NEU.0000341516.22126.AA. [DOI] [PubMed] [Google Scholar]
- 8.Eskandari R, Schmidt MH. Intramedullary spinal melanocytoma. Rare Tumors. 2010;2:e24. doi: 10.4081/rt.2010.e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rades D, Heidenreich F, Tatagiba M, Brandis A, Karstens JH. Therapeutic options for meningeal melanocytoma. Case report. J Neurosurg. 2001;95(2 Suppl):225–31. doi: 10.3171/spi.2001.95.2.0225. [DOI] [PubMed] [Google Scholar]
- 10.Rades D, Schild SE. Dose-response relationship for fractionated irradiation in the treatment of spinal meningeal melanocytomas: A review of the literature. J Neurooncol. 2006;77:311–4. doi: 10.1007/s11060-005-9048-2. [DOI] [PubMed] [Google Scholar]
- 11.Rades D, Schild SE, Tatagiba M, Molina HA, Alberti W. Therapy of meningeal melanocytomas. Cancer. 2004;100:2442–7. doi: 10.1002/cncr.20296. [DOI] [PubMed] [Google Scholar]
- 12.Rades D, Tatagiba M, Brandis A, Dubben HH, Karstens JH. The value of radiotherapy in treatment of meningeal melanocytoma. Strahlenther Onkol. 2002;178:336–42. doi: 10.1007/s00066-002-0930-y. [DOI] [PubMed] [Google Scholar]


