Abstract
IN BRIEF Gestational diabetes mellitus (GDM) increases the risk for type 2 diabetes. This qualitative study aimed to evaluate health care providers’ perceptions of care responsibilities and resources related to reducing type 2 diabetes risk among women with previous GDM in Singapore. Health care providers acknowledged a shared responsibility. They felt that they had less understanding of compliance with long-term maintenance of lifestyle change, exacerbated further by fragmentation of follow-up care. The application of more integrated patient-centered care models, combined with greater health literacy, is urgently required in this area.
“Halt the rise in diabetes and obesity” is one of the nine voluntary global targets for prevention and control of noncommunicable diseases to be attained by 2025 (1). Asian countries currently contribute more than half of the total adult population with diabetes in the world, and patients of Asian ethnicity have an intrinsically higher risk for type 2 diabetes (2).
Singapore is a city-state in Asia and one of the few Asian countries with a high-income economy (3). Among Singapore’s population (composed primarily of Chinese, Indian, and Malay ethnicities), the prevalence of type 2 diabetes has increased from 8.2% in 2004 to 11.3% in 2010, and for women, the increase was from 7.6% in 2004 to 10.4% in 2010 (4). In 2016, the Ministry of Health announced the initiation of a nationwide program called “The Fight Against Diabetes” (5).
Gestational diabetes mellitus (GDM) increases the risk for type 2 diabetes sevenfold (6,7). Diagnosing abnormal insulin activity during pregnancy opportunistically identifies this high-risk population at a much earlier stage. In Singapore, GDM complicates up to 20% of pregnancies (8). Therefore, early behavior-change interventions, which have shown promising results, may potentially play a significant role in reducing the risk for type 2 diabetes during the first 5 years after pregnancy (9,10).
In the current qualitative study, we explored health care providers’ (HCPs’) perceptions of the roles and responsibilities of patients and providers, continuity of care, readiness of the existing health care system for primary prevention, and resources needed for women with a history of GDM in an Asian setting.
Study Method
This study was conducted with prenatal HCPs at KK Women’s and Children’s Hospital and National University Hospital and primary care providers (PCPs) from communities across Singapore to explore perceptions of continuity of care and responsibilities for reducing the risk of type 2 diabetes among mothers with a history of GDM. These are the two leading public hospitals providing obstetrical and gynecological services in Singapore and, collectively, providing care for 90% of child deliveries that happen in the public health care setting annually (11). PCPs were recruited randomly from private and public primary care clinics.
Participants were recruited using purposive sampling. Prenatal HCPs who were working in GDM clinics or directly engaged in treating GDM patients and from the departments of obstetrics and gynecology, endocrinology, dietetics, or nursing were regarded as eligible to participate in the study. Eligible participants were invited by the site principal investigators. One study member, S.S.H., provided brief information about the study to HCPs who were interested in participating. PCPs were recruited from private and public health care institutions using a snowball sampling method.
A semi-structured interview guide was developed using previously published research work and findings from the local context. Two widely accepted frameworks, namely the Andersen Behavior Framework and Wagner’s Chronic Care Model, were used as background for question design (12–14). The topic guide consisted of three main sections: providers’ perceptions of risk due to GDM and reducing future complications, their responsibility for postnatal care, and continuity of care and barriers. A field expert (J.Y.) verified the content.
The interview guide was pilot tested with two nurses, and the content was subsequently revised to increase clarity of the interview questions. Ethical approval was obtained from the National Healthcare Group Domain-Specific Review Board before data collection.
Thirty-two in-depth interviews were conducted between August 2016 and August 2017 with eight obstetrician/gynecologists (OB/GYNs), five endocrinologists, six dietitians, eight nurses, and five PCPs. S.S.H., who has qualitative research training and experience, scheduled the interviews based on the availability and convenience of the participants and conducted all interviews in English. On average, interviews lasted ∼30 minutes. Most of the interviews were conducted at the health care facility in a private space conducive for participants sharing their thoughts effectively. Before the interviews, participants were asked to provide informed consent. All interviews were audio-recorded with consent. Interviews were continued until no new themes appeared. Ninety-five percent of the prenatal HCPs invited agreed to participate in the study. PCPs were recruited randomly from one public primary care clinic and four private clinics from the West, South, and East regions of Singapore. Among PCPs who were invited, 50% participated in the interviews. The most common reason given for nonparticipation was insufficient experience in treating women with a history of GDM.
Audio recordings were transcribed verbatim. Data analysis was carried out using a framework analysis approach (15). After listening to the audio recordings, verifying the transcripts for accuracy, and removing any identifying information, two coders (S.S.H. and S.R.S.) independently coded the transcripts using Atlas Ti Software (QSR International, Berlin, Germany) and Microsoft Excel (Microsoft, Redman, Wash.). The coders identified the majority of the codes in advance and added new codes as derived during the coding process. They had several meetings to reach a consensus on final themes and create final domains.
Results
There was a general recognition of the importance of continuity of care and attention to reducing the risk for type 2 diabetes among women with a history of GDM. Themes emerged under three domains: 1) gap between engagement and perception of future type 2 diabetes risk, 2) responsibilities for ordering and following up on postpartum oral glucose tolerance tests (OGTTs), and 3) roles for proactive care management to reduce type 2 diabetes risk. Key themes and supporting participant responses are presented in Table 1.
TABLE 1.
Key Themes of Domains and Participants’ Responses
| Themes | Participant Responses |
|---|---|
| Domain 1. Gap between engagement and perception of future type 2 diabetes risk | |
| Difficult to reduce type 2 diabetes risk with poor patient compliance | “I guess it is more difficult to assess their compliance postpartum. A lot of the focus is on them when they are pregnant until the point of delivery. And after they have delivered, the stress and pressure have gone down quite a lot. It is not that we demand a lot from them after they deliver as well . . . . If they are less diligent with their monitoring, we don’t want [to] chase after them.” (Endocrinologist) |
| Shared responsibility | “I think I have a responsibility, but mainly on an educational aspect. I think it is very important. But, I don’t have the resources to enforce and to check up on their lifestyle. I would—of course, if they are obese or get any other underlying IGT [impaired glucose tolerance test]—then I definitely will refer them to an endocrinologist or a primary care physician to follow-up with them. Because they are better able to keep track of them.” (OB/GYN) |
| Message framing | “During the pregnancy when they are having GDM, because it is going to be a big thing, and it will hit them. It is a life-changing event. I do think that it is the real starting point, where you can do the most changes . . . convince the patient the most.” (OB/GYN) |
| “. . . if they are anxious like Singaporeans and [who] have ‘kiasu’ [afraid to lose out] kind of personalities . . . . Some of them [are] like ‘oh’ and [are] motivated to push then: ‘Oh, my gosh, I need to do something about it.’ But, they actually get frightened—so frightened that they will go into a denial phase. So that is also difficult.” (Endocrinologist) | |
| “Because I guess the doctors always have a greater authority than us in terms of asking them, you know, ‘You need to lose some weight,’ for example.” (Dietitian) | |
| Competing priorities | “I think in family practice, family medicine, preventive care is our goal. It is not just treatment of the disease.” (PCP) |
| “One [highest level] will be most important. I think one. It is most important to prevent diabetes, post-delivery.” (Dietitian) | |
| “Maybe seven [lower level]. I mean for O and G [obstetrics and gynecology] being a very sub-specialized specialty, unfortunately, [it is] not very highly screened for type 2 diabetes in our practice.” (OB/GYN) | |
| Domain 2. Immediate postnatal period: responsibilities for postpartum OGTT ordering and follow-up | |
| Responsibility for postpartum OGTTs | “I think so. Because, those who are still positive [with positive OGTT results] we will normally channel them to an endocrinologist . . . sort of like we close the loop . . . . Otherwise, they are still positive [have not resolved GDM after their delivery], and if they don’t do the test, they would not know.”(Nurse) |
| Inconsistent processes for follow-up | “. . . what we are doing now is [postpartum OGTT] is just a one-off thing. So, the monitoring, the screening, the annual screening, that is also still important. But, I don’t think that is being routinely done.” (Dietitian) |
| Patient barriers | “I guess that I am not sure. Maybe more of the patients are forgetting over time that they had this problem [GDM] before because there are other things in [their] life to worry over. And if it is a once a year thing [annual screening for type 2 diabetes], then [it’s] very easy to forget.” (Endocrinologist) |
| Domain 3. Follow-up care after postpartum period: roles for proactive care management to prevent type 2 diabetes | |
| Handing over care to PCPs |
“At least in primary care, they will have the same doctor [who] always sees the patient, knows everything about the patient. So that is some sort of ownership.” (Endocrinologist) “We usually do an OGTT and subsequently, we might do another OGTT or venous fasting depending on the patient’s preference. Again, there is no real guideline on whether we should do it subsequently.” (PCP) |
| Health care system readiness | “Because, the involvement of primary care, which is the polyclinics . . . that is much poorer here [Singapore] compared to everywhere else. I mean, the only example I know is the U.K., because we always learn their guidelines . . . . yearly follow-up with their [U.K.] primary care. . . . So, I guess that is something that we could work in partnership with the primary care [general practitioners], as well [as] the polyclinics, who have regular follow-up with these women. Because we already know that they are at risk.” (OB/GYN) |
| “It is untagged. Everybody is floating around freely. Once they have their 6 weeks [OGTT] they are let loose. So, we have no chance to get them back. So, if there is a tagging system in the hospital, because that is where they get diagnosed with GDM in the first place . . . ” (PCP) | |
| Community influences | “The Diabetes Prevention Program in the U.S. . . . . They started as a study, [and] they have managed to implement it [in] real life, and it is run as a community partnership, such as [with] the YMCA [Young Men’s Christian Association]. That is particularly effective because they utilize peer support . . . . There is a link to primary care, but, the program doesn’t rest completely on the physician to deliver everything.” (Endocrinologist) |
| Stakeholders in proactive care | “If we want to reduce all these various public health problems, you have to hit the root of the matter, isn’t it? When it comes to healthy eating and healthy lifestyle, who else is better than the government and the community?” (Nurse) |
1. Gap Between Engagement and Perception of Future Type 2 Diabetes Risk
Difficult to Reduce Type 2 Diabetes Risk With Poor Patient Compliance
Participants identified type 2 diabetes risk as the most serious long-term risk after GDM. The majority said that women might be able to prevent developing type 2 diabetes, whereas a few providers said that it could only be delayed. Providers said healthy lifestyle and regular screening would help to minimize type 2 diabetes risk. A few prenatal HCPs believed that women are given the appropriate knowledge about how to control GDM, and the same content can be applied to their lifestyle to lower type 2 diabetes risk. They also felt that these women were at an advantage compared to other high-risk groups because they had such knowledge.
However, most thought that women’s compliance to a healthy lifestyle tended to be lower after pregnancy because of other factors affecting patient compliance such as increased responsibility with the newborn baby, lack of insistence by HCPs, inadequately perceived risk of diabetes, and poor motivation with regard to their own health. Some could not comment because there is no follow-up system after childbirth.
Shared Responsibility
The majority of the providers acknowledged some responsibility for reducing type 2 diabetes risk among women with previous GDM, which they thought of as a shared contribution between care providers. However, they believed that the women should have the greatest responsibility for their own health and also pointed to the need for multidisciplinary involvement with a proper follow-up system. In extremis, a few believed that, ideally, there is no need for HCPs’ involvement and that patients should take sole responsibility for looking after their health.
Message Framing
PCPs felt the need to improve women’s perception of their own diabetes risk mainly during the pregnancy. While prenatal HCPs acknowledged the importance of providing comprehensive education to women to raise awareness of measures to prevent type 2 diabetes, opinions varied about how this discussion should be handled most effectively. Most providers believed that women needed to know about their risk of diabetes after childbirth, whereas a few believed that too much negative information about the future might hinder women’s motivation to control GDM successfully in the immediate period.
Participants believed that consistent messaging by prenatal HCPs would help emphasize early preventive care among women. However, nurses and dietitians shared that, in the local context, women consider prenatal care physicians to be more authoritative, and women tend to value information more when it is delivered by clinicians.
Competing Priorities
Providers had different specialty-specific views with respect to prioritizing reduction of type 2 diabetes risk. PCPs acknowledged that primary prevention is one of their main priorities. Similarly, the nurses and dietitians felt that this goal was a high priority for them. On the other hand, prenatal clinicians were less inclined to rate this as a high priority, stating instead that their main focus is to provide care for a successful pregnancy.
2. Immediate Postnatal Period: Responsibilities for Postpartum OGTT Ordering and Follow-Up
Responsibility for Postpartum OGTTs
Respondents agreed that postpartum OGTTs are useful to identify women with insulin impairment immediately after childbirth. They reported that informing women about the postpartum OGTT is a priority given less-than-desirable compliance. They acknowledged their responsibility to inform patients about the test and mentioned that patients should be reminded several times during pregnancy. Additionally, OB/GYNs and endocrinologists reported that they take responsibility for ordering the postpartum OGTT.
Inconsistent Processes for Follow-up
According to participants, health care institutions follow different protocols for postpartum OGTTs, but not all participants were clear on what routine care should be. When women are tested in the hospital setting, OB/GYNs and endocrinologists stated that they are responsible for following up with abnormal test results. If postpartum OGTTs are done in a primary care setting, however, providers assumed that patient follow-up would become the responsibility of the PCP. Similarly, PCPs identified their responsibility to perform postpartum OGTTs. A few contrasted the local system to the Australian health care system, in which follow-up care is systematically carried out using a national registry.
Despite the usefulness of OGTTs, a few providers had concerns about the inconsistency of medical recommendations based on postpartum OGTT results. They mentioned that women with poor test results are given immediate medical attention, and those with normal test results may be missed in follow-up, even though both groups are at elevated risk of type 2 diabetes. Almost all participants said that women with normal test results—the majority—do not get further medical advice and are thus likely to revert to their previous lifestyle practices.
Patient Barriers
Other than poor motivation, providers did not have a clear idea of what prevented women from getting an OGTT, although they described other potential factors involved in poor postpartum OGTT uptake, including lack of saliency, new responsibilities with a newborn, work commitments, cultural barriers, financial barriers, and lack of social support. Providers also suggested that awareness and prioritization of risk-reduction vary by socioeconomic and educational level, with more educated women reportedly being more compliant with preventive measures.
Some providers went as far as to suggest that having additional postpartum clinic visits to educate women about type 2 diabetes risk and care recommendations would be beneficial. However, providers mentioned that women are unlikely to even continue with the current recommended protocol of annual screening for diabetes in the primary care setting in the years after their immediate postpartum period.
3. Follow-Up Care After Postpartum Period: Roles for Proactive Care Management to Prevent Type 2 Diabetes
Handing Over Care to PCPs
Although prenatal HCPs generally felt that follow-up was crucial, they also clearly felt that their own role was limited in part by a lack of resources and time constraints. The majority of the prenatal HCPs believed that the primary care system should be responsible for following up with women with previous GDM after childbirth, whereas a few thought there should be a designated care provider such as a diabetes nurse educator.
Prenatal HCPs identified increased patient load, lack of time per patient, and insufficient technical expertise as possible barriers to expanding primary prevention in the primary health care setting. Moreover, PCPs were not clear about the guidelines or recommendations for follow-up in subsequent visits after the 6-week postpartum OGTT.
Health Care System Readiness
The clinicians thought that established patient-provider relationships such as those in the United Kingdom would enhance care effectiveness and sustain follow-up care, whereas the lack of such features in the current system may lead to clinician behavior that exacerbates poor motivation and compliance among these women. The clinicians also voiced concern about the absence of a financing model based on health outcomes and quality care delivery. They noted that the absence of such incentives in Singapore’s health system might result in insufficient ownership and motivation among PCPs to support primary prevention. At the same time, some clinicians expressed doubt about whether the local health system is sufficiently ready to incorporate such incentives.
In addition to low patient motivation, the PCPs believed that there is no proper system to identify and retain patients in the current care model. They expressed the need for integrated and improved hospital electronic medical records, which can be easily accessed by PCPs. Moreover, they highlighted the importance of implementing effective communication channels between the hospital and primary care clinics to better assist in transitions from tertiary care to primary care settings.
Community Influences
Providers felt that, after childbirth, women leave the environment of prenatal care and rejoin the community, where understanding of type 2 diabetes risk is poor. Along with reduced insistence from care providers to maintain healthy behaviors, promoting healthy behavior among these women may be a challenge as women forget their individual risk and recalibrate their beliefs according to their peer or social groups. Furthermore, the providers felt that environmental influences negatively affect women’s motivation to maintain healthy behavior, mainly with respect to the prevalence of unhealthy food options. The providers suggested that strengthening the community with proper health promotion programs will assist in primary prevention, which will simultaneously benefit chronic disease prevention on a larger scale.
Stakeholders in Proactive Care
Participants felt that the government and families should be the main stakeholders to assist in the care process. Given the complexity of the disease, the providers felt that a national-level strategy with a multidisciplinary approach would be warranted. Many responders mentioned that, although the Singapore government has already initiated programs that have a primary focus on curbing diabetes at the national level, the current emphasis on high-risk groups, including women with a history of GDM, is inadequate. Other stakeholders such as industry and schools were mentioned, but to a lesser degree.
Discussion
In Singapore, prenatal HCPs and PCPs generally recognized the need for a systematic approach for follow-up screening and behavior improvements to reduce type 2 diabetes risk among women with a history of GDM. Prenatal HCPs acknowledged their responsibility to reduce the incidence of type 2 diabetes among women with GDM and felt that PCPs are responsible for follow-up care. Moreover, both prenatal HCPs and PCPs voiced their concern about the lack of a proper follow-up system. Such disintegration in the current health care system may act as a barrier to primary prevention efforts.
For most women with previous GDM, the condition resolves after childbirth; however, they remain at elevated risk for type 2 diabetes (16). Study data show that these women are at risk for two reasons. First, lack of adherence to primary prevention reduces the saliency of their future type 2 diabetes risk, leading to neglect of positive lifestyle behaviors, which is a key obstacle to care management (17,18). Second, having a negative OGTT result may increase the risk of being overlooked in primary prevention efforts because of limited follow-up. As a first step, gaining a proper understanding of patient factors—mainly risk perception, motivation to improve lifestyle habits, and follow-up with regular screenings, socioeconomic factors, and patient satisfaction—is vital in designing a successful patient-centered care model (19,20). Furthermore, empowering women in the postpartum period to modify their lifestyle using their GDM management knowledge is an opportunity worth exploring.
As suggested by a few participants, a registry for women with previous GDM could serve as a common resource for both specialists and PCPs. This practice has been adopted successfully in Australia, and there is an effort to implement it in New Zealand (21,22). Although such a registry does not exist in Singapore, a similar intervention would be a key resource for both the clinical practice and research communities, primarily to send patients reminders for annual diabetes screenings and information promoting a healthy lifestyle; track patients’ health care–seeking behaviors; and assess patients’ compliance with recommendations for reducing their risk of type 2 diabetes.
As highlighted in interviews, an arrangement similar to the U.K. National Health Service would allow for systematic referrals from tertiary care to primary care settings (23). In Singapore, where mainly private practitioners deliver primary care services (24), such a universal system has not been established.
Participants shared that a lack of resources, increased patient loads, lack of proper reimbursement to PCPs based on the quality of care delivered, and inadequate technical training might hinder effective care by PCPs (17,23,25,26). A possible solution offered by respondents was to replace clinicians with other medical professionals such as diabetes nurse educators and dietitians. Similar interventions have reported successful results in disease management and patient satisfaction (27,28). However, the feasibility and acceptance of such interventions in the local context need to be explored before implementation. As stated by study participants, systematic incentives that encourage PCPs to deliver high-quality primary prevention merit exploring. Moreover, it is imperative to equip PCPs with updated guidelines and recommendations in a timely manner to ensure delivery of consistent care (29). Furthermore, providers looked toward an increased role for the government and the public health care sector, which they regard as key figures in funding programs, implementing public health policies to involve the community in behavior improvement, and reducing the burden on the health care system.
In general, qualitative study findings are context-specific; thus, generalizing to other settings can be limited. However, a few studies, including some conducted in significantly different health care settings, have drawn similar conclusions (30,31). Therefore, it may be possible to generalize our main study finding, which is that a lack of follow-up care and resources to reduce type 2 diabetes risk for women with previous GDM appears to be a common gap in diabetes preventive care.
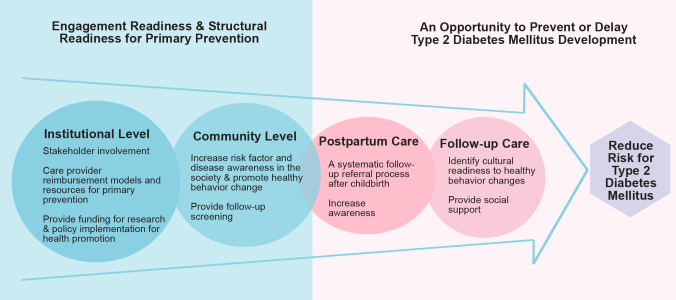
Based on our study findings, a possible action plan can be conceptualized for postpartum care management (Figure 1). It was noted that a strong link between institutions, mainly the government and the community, appears to be important in improving continuity of care for women after GDM. The action plan would involve:
At the institutional level: setting up a care provider reimbursement model and providing funding resources for preventive care, research, and implementation of health promotion policies
At the community level: increasing disease awareness, promoting healthy behavior changes, and providing follow-up screenings
FIGURE 1.
Action plan to reduce type 2 diabetes risk among women with a history of GDM.
Generally, having a robust, fundamental structure at both the institutional and community levels facilitates chronic disease prevention. Because early preventive measures are important to reduce type 2 diabetes risk, women with previous GDM ideally should be provided immediate and longer-term care within such a system, which would include:
Early postpartum care: having a systematic follow-up referral procedure from specialists to PCPs and improving awareness of type 2 diabetes risk among women
Follow-up care: identifying culturally appropriate interventions for lifestyle modification and providing social support
The current work provides an understanding of the perceptions of a wide variety of experts involved in treating women from their diagnosis of GDM to follow-up after childbirth. Data were collected from prenatal HCPs of the two leading public tertiary health care facilities that provide prenatal care and from PCPs representing different areas of the country. However, there are some limitations to this study. The study did not focus on the perceptions of other groups such as prenatal HCPs in private tertiary institutes, women with previous GDM, national agencies such as the Health Promotion Board, or policymakers. Separate studies are in progress to better understand patients’ barriers in the immediate postpartum period and throughout 5 years after having GDM.
In summary, the prenatal HCPs and PCPs who participated in this study recognized the need to take actions to reduce type 2 diabetes risk in women with previous GDM. The key barriers identified were poor patient motivation, lack of ownership, and health care system barriers. The providers noted that having a registry to remind women about their regular screenings for diabetes may help to increase OGTT uptake and identify new diabetes cases without delay. There is a clear need to include this high-risk group in the current national diabetes prevention program and to increase the perception of diabetes risk among women with a history of GDM and the larger community. In addition to published postnatal care recommendations (32), identified gaps in follow-up care at both the patient and health care system levels require attention. Information about such gaps is crucial to designing a systematic care process initiated at the prenatal level, followed by postpartum care, and linked to continual follow-up care to reduce the incidence of type 2 diabetes and related complications among women with a history of GDM.
Acknowledgments
The authors thank the providers who participated in this study. They also thank Peck Hoon Ong, Suan Ong, and Samuel Gunter for their assistance in reviewing the manuscript.
Funding
This research was supported by the National University of Singapore (NUS) Global-Asia Institute NUS Initiative to Improve Health in Asia Research Grant (Grant No. NIHA-2013-1-002).
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
S.S.H. conceptualized and designed the study, obtained necessary ethics approval, collected data, performed the analyses, assisted in drafting the manuscript, and finalized the draft based on comments from other authors’ feedback. S.R.S. assisted in study design and in the analyses. C.C., J.K.Y.C., T.W.Y., and W.M.H. assisted in participant recruitment and critical review of the manuscript. J.Y. assisted in the study design and critically reviewed the manuscript. All authors approved the final manuscript as submitted. S.S.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation
Parts of this study were presented in abstract form as an oral presentation at the Lifestyle Medicine conference in Melbourne, Australia, 4–6 November 2016.
References
- 1.World Health Organization Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva, Switzerland, World Health Organization, 2013 [Google Scholar]
- 2.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 2016;387:1513–1530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Bank. Singapore: overview. Available from http://beta.worldbank.org/en/country/singapore/overview. Accessed 18 January 2017.
- 4.Health Promotion Board of Singapore. Information paper on diabetes in Singapore, November 14, 2011. Available from https://www.nrdo.gov.sg/docs/librariesprovider3/Publications---Kidney-Failure/info_paper_diabetes_2011nov.pdf. Accessed 22 January 2017.
- 5.Ministry of Health Singapore The fight against diabetes: a nationwide effort. Available from https://www.moh.gov.sg/content/moh_web/home/pressRoom/highlights/2016/Budget2016/the-fight-against-diabetes.html. Accessed 17 January 2017
- 6.Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373:1773–1779 [DOI] [PubMed] [Google Scholar]
- 7.Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care 2002;25:1862–1868 [DOI] [PubMed] [Google Scholar]
- 8.Chong Y-S, Cai S, Lin H, et al. Ethnic differences translate to inadequacy of high-risk screening for gestational diabetes mellitus in an Asian population: a cohort study. BMC Pregnancy Childbirth 2014;14:345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gilinsky A, Kirk A, Hughes A, Lindsay R. Lifestyle interventions for type 2 diabetes prevention in women with prior gestational diabetes: a systematic review and meta-analysis of behavioural, anthropometric and metabolic outcomes. Prev Med Rep 2015;2:448–461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gæde P, Lund-Andersen H, Parving H-H, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 2008;358:580–591 [DOI] [PubMed] [Google Scholar]
- 11.Ministry of Health Singapore Delivery (normal). Available from https://www.moh.gov.sg/content/moh_web/home/costs_and_financing/hospital-charges/Total-Hospital-Bills-By-condition-procedure/delivery_normal.html. Accessed 12 October 2017
- 12.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 1995:36;1–10 [PubMed] [Google Scholar]
- 13.McDonald KM, Sundaram V, Bravata DM, et al. Closing the Quality Gap: A Critical Analysis of Quality Improvement Strategies. (Vol. 7: Care Coordination; Report No.: 04(07)-0051-7). Rockville, Md, Agency for Healthcare Research and Quality, 2007 [PubMed] [Google Scholar]
- 14.Wagner E. Care of older people with Chronic illness. In New Ways to Care for Older People: Building Systems Based on Evidence. New York, Springer Publishing Company, 1999, p.39–64 [Google Scholar]
- 15.Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London, Sage, 2013 [Google Scholar]
- 16.Winhofer Y, Tura A, Thomas A, et al. Hidden metabolic disturbances in women with normal glucose tolerance five years after gestational diabetes. Int J Endocrinol 2015;2015:342938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Geense WW, van de Glind IM, Visscher TL, van Achterberg T. Barriers, facilitators and attitudes influencing health promotion activities in general practice: an explorative pilot study. BMC Fam Pract 2013;14:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jallinoja P, Absetz P, Kuronen R, et al. The dilemma of patient responsibility for lifestyle change: perceptions among primary care physicians and nurses. Scand J Prim Health Care 2007;25:244–249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dwamena F, Holmes-Rovner M, Gaulden CM, et al. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev. 2012;12:CD003267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baker MK, Simpson K, Lloyd B, Bauman AE, Singh MAF. Behavioral strategies in diabetes prevention programs: a systematic review of randomized controlled trials. Diabetes Res Clin Pract 2011;91:1–12 [DOI] [PubMed] [Google Scholar]
- 21.Atalag K, Zivaljevic A, Eagleton C, Pickering K. A standards-based approach to development of clinical registries: initial lessons learnt from the Gestational Diabetes Registry. In: HiNZ; 2014. [Google Scholar]
- 22.National Diabetes Services Scheme National gestational diabetes register. Available from http://gd.ndss.com.au/en/Diabetes-Register. Accessed 20 January 2017
- 23.Van Ryswyk E, Middleton P, Hague W, Crowther C. Clinician views and knowledge regarding healthcare provision in the postpartum period for women with recent gestational diabetes: a systematic review of qualitative/survey studies. Diabetes Res Clin Pract 2014;106:401–411 [DOI] [PubMed] [Google Scholar]
- 24.Ministry of Health Singapore Healthcare institution statistics. Available from https://www.moh.gov.sg/content/moh_web/home/statistics/healthcare_institutionstatistics.html. Accessed 17 January 2017
- 25.Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med 1995;24:546–552 [DOI] [PubMed] [Google Scholar]
- 26.Cornuz J, Ghali WA, Di Carlantonio D, Pecoud A, Paccaud F. Physicians’ attitudes towards prevention: importance of intervention-specific barriers and physicians’ health habits. Fam Pract 2000;17:535–540 [DOI] [PubMed] [Google Scholar]
- 27.Emina S. Barriers to Providing Nutrition Counseling by Primary Care Physicians: Opportunities for Registered Dietitians., Columbus, Ohio, Ohio State University, 2012 [Google Scholar]
- 28.Laurant M, Reeves D, Hermens R, Braspenning J, Grol R, Sibbald B. Substitution of doctors by nurses in primary care. Cochrane Database Syst Rev 2005;2:CD001271. [DOI] [PubMed] [Google Scholar]
- 29.Goh SY, Ang SB, Bee YM, et al. Ministry of Health clinical practice guidelines: diabetes mellitus. Singapore Med J 2014;55:334–347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bernstein JA, McCloskey L, Gebel CM, Iverson RE, Lee-Parritz A. Lost opportunities to prevent early onset type 2 diabetes mellitus after a pregnancy complicated by gestational diabetes. BMJ Open Diabetes Res Care 2016;4:e000250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pennington AV, O’Reilly SL, Young D, Dunbar JA. Improving follow-up care for women with a history of gestational diabetes: perspectives of GPs and patients. Aust J Prim Health 2017;23:66–74 [DOI] [PubMed] [Google Scholar]
- 32.Gabbe SG, Landon M, Warren-Boulton E, Fradkin J. Promoting health after gestational diabetes: a National Diabetes Education Program call to action. Obstet Gynecol 2012;119:171–176 [DOI] [PMC free article] [PubMed] [Google Scholar]