Abstract
IN BRIEF Successful management of patients with diabetes requires individualizing A1C and treatment goals in conjunction with identifying and managing hypoglycemia risk. This article describes the Veterans Health Administration’s Choosing Wisely Hypoglycemia Safety Initiative (CW-HSI), a voluntary program that aims to reduce the occurrence of hypoglycemia through shared decision-making about deintensifying diabetes treatment in a dynamic cohort of patients identified as being at high risk for hypoglycemia and potentially overtreated. The CW-HSI incorporates education for patients and clinicians, as well as clinical decision support tools, and has shown decreases in the proportions of high-risk patients potentially overtreated and impacts on the frequency of reported hypoglycemia.
The clinical management of patients with diabetes requires individualization of A1C and other treatment goals that consider patient-specific characteristics and risks for hypoglycemia. The use of measures of glycemic control that do not consider the diversity of these characteristics in patients has resulted in unintended, although predictable, consequences of hypoglycemia and polypharmacy (1). This is reflected by findings such as high hospital admission rates for hypoglycemia that exceed those for hyperglycemia in older adults (2). Moreover, the ACCORD (Action to Control Cardio-vascular Risk in Diabetes), VADT (Veterans Affairs Diabetes Trial), and ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation) trials found that intensive glycemic control has limited microvascular and no macrovascular benefits in older patients with longer duration of diabetes (3–5).
Individualization of goals has been a key component of the Department of Veterans Affairs and Department of Defense (VA/DoD) clinical practice guidelines since 2000 (6). In 2012, the VA/DoD guidelines introduced a shared decision-making tool to assist in determining a safe and evidence-based A1C goal (7). Also in 2012, the American Board of Internal Medicine Foundation announced the Choosing Wisely initiative, which included a recommendation from the American Geriatrics Society (AGS) to “avoid using medications other than metformin to achieve hemoglobin A1C <7.5% in most older adults; moderate control is generally better” (8,9). The American Diabetes Association, the European Association for the Study of Diabetes, and the Canadian Diabetes Association have also recommended against intensive control in high-risk populations (10,11). The U.S. Department of Health and Human Services (DHHS) published its “National Action Plan for Adverse Drug Event Prevention” in 2014, which included among its targets diabetes agents and preventing episodes of serious hypoglycemia (12). All of this provides support for deintensification of therapy to reduce the likelihood of hypoglycemia in higher-risk populations who realize limited or no benefit from intensive glycemic control and/or have comorbid conditions that could result in harms from intensive glycemic control.
To promote a shared decision-making approach for determining safe and evidence-based diabetes treatment plans and provide supportive resources, the VA Great Lakes Health Care System (Veterans Integrated Service Network [VISN] 12) began a voluntary hypoglycemia safety initiative in mid-2012 across its then seven Veterans Health Administration (VHA) medical centers and their associated outpatient clinics. The electronic medical record (EMR) was used to identify patients with diabetes at high risk for hypoglycemia who might be candidates for deintensification of therapy. The program also provided means for standardized screening for hypoglycemia and documentation of the shared decision care plan to mitigate hypoglycemia risk. In late 2014, after receiving endorsement by VHA leadership (13), the associated EMR tools were made available nationally across VHA, coupled with a focus on education for patients and clinicians, and the initiative was retitled the VHA Choosing Wisely Hypoglycemia Safety Initiative (CW-HSI) (14). This article describes the development, implementation, and spread of the VHA CW-HSI quality improvement program.
Program Development and Components
Stakeholder Engagement and Workgroup Formation
Before initiation, the VISN 12 Health Systems Council, which included chiefs of staff and nurse executives from each medical center, approved the initiative. A multi-professional workgroup reporting to the VISN chief medical officer provided assistance for the rollout of the program across VISN 12, leveraging existing staff and technology. Each medical center identified a clinical point of contact to aid in implementation and communication. This program met criteria as a nonresearch operations activity and was deemed exempt from institutional review board review.
Identification of Patients
The VISN 12 workgroup collaborated with VHA subject matter experts to identify criteria that would yield a manageable number of patients at high risk for hypoglycemia who may be overtreated. The criteria used have been described previously (15). In brief, patients eligible for inclusion in the high-risk patient cohort include those receiving insulin and/or sulfonylureas, which are frequently associated with serious hypoglycemia (12,16), who have limited life expectancy (<10–15 years) or other significant risk (i.e., impaired renal function [17] or dementia/cognitive impairment [18]).
A1C <7% was used as a measure of (potential) overtreatment based on the VA/DoD guidelines (19) and the AGS Choosing Wisely scientific review (8,9). In a study of VA patients with diabetes receiving insulin and/or sulfonylureas, about 32% had limited life expectancy or other significant risk as described here; 50% of these patients had an A1C <7% (15).
Of note, inclusion criteria were modified during the first 2 years of the VISN 12 implementation. Specifically, additional criteria were added (dementia/cognitive impairment and serum creatinine) and the timeframes for criteria were modified (e.g., from 12 to 18 months for A1C). All of the criteria described above have been included since May 2014 with the dynamic cohort composed of patients assigned to VHA Primary Care whose most recent A1C measured in the past 18 months was <7% with an active or expired (filled in the past 90 days) prescription for insulin and/or sulfonylurea and who are also ≥75 years of age, have dementia/cognitive impairment (based on the International Classification of Diseases, Ninth or Tenth Revision, Clinical Modification codes on outpatient encounters), or have a most recent serum creatinine in the past 18 months >150.3 µmol/l (1.7 mg/dL).
Tools
Clinical data to identify the dynamic patient cohort come from the VHA EMR. To support identification and management of patients, three informatics tools were developed for clinicians: a clinical alert, a template, and online panel reports. The clinical alert triggers in the EMR for patients who meet the cohort criteria in real time at the point of care (e.g., when patients come in for an appointment with their primary care provider), prompting assessment and management of hypoglycemia occurrence and risk. Completing the screening portion of the associated template resolves the clinical alert for 6 months. If a patient meets the cohort criteria and it has been at least 6 months since the last template completion, the clinical alert will re-trigger whenever the patient’s chart is next accessed.
The template includes a set of questions to screen for and assess the occurrence, frequency, and severity of hypoglycemia and captures the care plan subsequently decided on through shared decision-making. The template was designed to be brief and easy to complete within the EMR during conversation with patients. Question development was informed by diabetes questionnaires available in the public domain (20,21). The questions and available responses are included in Table 1. For each question, a negative response option of “None reported” or “No” is also available. Questions 2 and 4 are asked if there is a positive response to question 1; question 3 is asked if there is a positive response to question 2. The care plan options available for selection in the template are “‘No change in glycemic management at this time” or “Relax glycemic treatment.” Selection of “Relax glycemic treatment” indicates a decrease in dosage and/or frequency of administration or discontinuation of a medication being used to treat the patient’s diabetes (i.e., deintensification). Of note, the template can be used within the EMR for any patient regardless of cohort inclusion status, and there is no limit to the number of times it can be used for any individual patient.
TABLE 1.
Hypoglycemia Screening Template Findings (Seven Medical Centers, June 2012 Through March 2017)
| Template Component | Response | Template Uses (total n = 17,909) (n [%]) | Patients (total n = 8,495) (n [%]) |
|---|---|---|---|
| Question 1: In the past few months, how often did the patient/caregiver report that the patient had a low blood sugar? | Once 2–3 times per month Once a week Daily Any frequency |
1,952 (10.9) 1,683 (9.4) 578 (3.2) 67 (0.4) 4,280 (23.9) |
1,379 (16.2) 1,138 (13.4) 432 (5.1) 64 (0.8) 2,437 (28.7) |
| Question 2: In the past few months, how often did the patient/caregiver report that the patient had a low blood sugar serious enough that the patient felt they might pass out? | Once 2–3 times per month Once a week Daily Any frequency |
507 (2.8) 252 (1.4) 80 (0.4) 18 (0.1) 857 (4.8) |
478 (5.6) 243 (2.9) 80 (0.9) 18 (0.2) 780 (9.2) |
| Question 3: Did the patient/caregiver report that the patient passed out or fell because of a low blood sugar? | Yes | 126 (0.7) | 122 (1.4) |
| Question 4: Did the patient/caregiver report that the patient required a visit to a clinic/ED/hospital because of a low blood sugar? | Yes | 172 (1.0) | 166 (2.0) |
| Questions 2, 3, 4 | Any response indicating occurrence | 881 (4.9) | 802 (9.4) |
| Care plan | Relax (deintensification) No change Not available |
3,205 (17.9) 13,053 (72.9) 1,651 (9.2) |
2,224 (26.2) 5,680 (66.9) 591 (7.0) |
| Care plan in screenings reporting hypoglycemia* | Relax (deintensification) No change Not available |
2,139 (50.0) 1,915 (44.7) 226 (5.3) |
1,378 (56.5) 907 (37.2) 152 (6.2) |
Total template uses n = 4,280; total patients n = 2,437.
ED, emergency department.
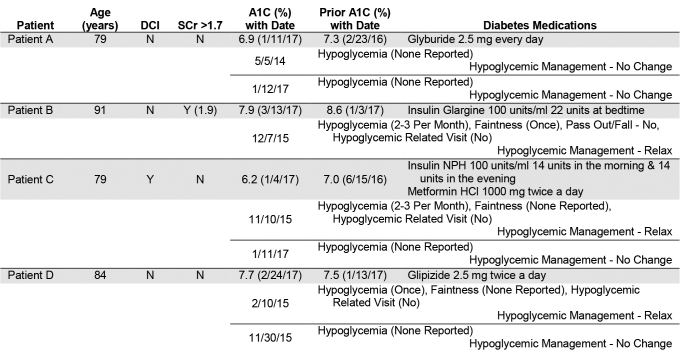
The online panel reports include patients currently in the cohort, as well as patients previously screened using the template. The display includes patient identifiers, cohort inclusion data, the two most recent A1C values within the past 3 years, prescribed diabetes medications, findings from previous screenings documented using the template, and future scheduled appointments (Figure 1). Information in these reports is updated daily and comes from the VHA Corporate Data Warehouse, a repository of data sourced from the VHA EMR (22). Web-based access to these reports is available on demand within the VA network, and the reports are flexible, allowing access by different sets of criteria (e.g., whole medical center, single primary care provider, cohort, and assessment status). These reports are accessed by care managers (e.g., clinical pharmacy specialists and certified diabetes educators) as needed for population health surveillance to identify and contact patients, often by modalities other than face-to-face visits such as telephone calls.
FIGURE 1.
CW-HSI online panel report. Future scheduled appointments are excluded in this sample report. DCI, dementia/cognitive impairment; N, no; SCr, serum creatinine (reported in mg/dL); Y, yes.
Education
For the VISN 12 implementation, clinicians were educated about the initiative during regularly scheduled meetings held within primary care, pharmacy, and nursing. Additionally, in-service training sessions and newsletters were provided at the discretion of each medical center. As the CW-HSI expanded across the VHA, education became the primary focus of efforts related to targeting glycemic overtreatment (see National Expansion section below).
National Expansion
In 2014, the VHA Office of the Deputy Undersecretary for Policy and Services chartered a CW-HSI workgroup consisting of representatives from medicine, nursing, pharmacy, nutrition, patient education services, and informatics to support a national rollout of the initiative. The workgroup’s focus complemented the AGS Choosing Wisely diabetes recommendation (8,9), targeting glycemic overtreatment with an emphasis on hypoglycemic safety, and the VISN 12 program served as its model.
In addition to making the clinical alert, template, and online panel reports available nationwide, the workgroup created educational resources for patients and clinicians on hypoglycemia risk, individualizing A1C targets, and other key elements of evidence-based diabetes care such as shared decision-making, health literacy, medication safety, and food insufficiency. These resources were made available on the CW-HSI website (23) and through the Veterans Health Library (24). In addition, an email distribution group was created for clinicians to disseminate information related to the CW-HSI and glycemic overtreatment and a patient information package containing a newsletter, patient case, and infographics was distributed to health education coordinators. Finally, virtual presentations were given about the CW-HSI and related topics during Community of Practice calls for medicine, pharmacy, nursing, and health education coordinators and during National Grand Rounds. In-progress work includes creating patient-facing videos to be used throughout VHA (e.g., in waiting rooms), as well as developing a continuing education program for clinicians.
The initiative remains voluntary, with no mandated participation, specific funding, or associated performance measures. VHA centers that choose to participate are encouraged to use and implement the tools and resources in ways that are best suited for their patients and clinicians.
Results
Patient Cohort
As in any dynamic cohort, the patients identified as meeting the inclusion criteria fluctuate each time the data are generated (e.g., daily for the online panel reports). Based on data snapshots (cross-sections) taken on the first day of every month from June 2014 through March 2017, the number of VHA Primary Care patients in the cohort at seven VISN 12 medical centers averaged 9.0 ± 0.2 patients per Primary Care panel, with a range of 8.6–9.5. This number represents 1.75 ± 0.04% of the total panel (range 1.68–1.82%). When the CW-HSI was expanded nationally, similar proportions were found (data not shown).
VISN 12 Implementation
When the initiative first started in VISN 12 in June 2012, five of its seven medical centers chose to participate and began using the clinical alert, template, and online panel reports within primary care teams. By June 2013, primary care teams at all seven medical centers were participating. As of April 2017, >85% of primary care patients in the cohort at these medical centers have been screened using the template.
The template-related data reported here includes uses of the template in these seven VISN 12 medical centers and their outpatient clinics from June 2012 through March 2017. There were 17,909 uses of the template in 8,495 patients documenting the occurrence, frequency, and severity of hypoglycemia; 90.8% of these uses also documented a care plan (n = 16,258). Many patients were screened more than once during this time period, with screening occurring two, three, four, and five or more times in 1,850 (21.8%), 930 (10.9%), 387 (4.6%), and 560 (6.6%) patients, respectively.
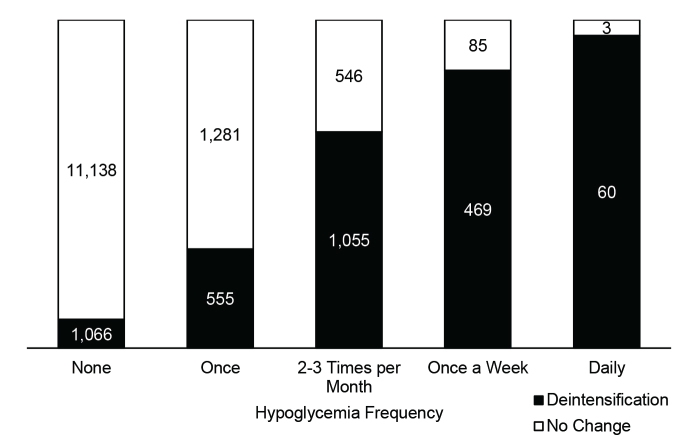
Recent episodes of hypoglycemia were reported during 4,280 screenings (23.9%) in 2,437 patients screened (28.7%). Moderate to severe hypoglycemia episodes such that patients felt they may pass out, did pass out, or required a visit to a clinic, emergency department, or hospital were reported by 802 patients screened (9.4%). Table 1 provides additional details about the frequency and severity of these reported episodes. Diabetes treatment was deintensified during at least one screening in 26.2% of all patients screened and 56.5% of patients reporting hypoglycemia (Table 1). As the frequency of reported hypoglycemia increased, the proportion of documented deintensification of treatment also increased (Figure 2).
FIGURE 2.
Uses of hypoglycemia screening template care plan by hypoglycemia frequency in seven medical centers, June 2012 through March 2017.
There were 782 patients whose first screening reported hypoglycemia who subsequently had a second screening. Occurrence scores were determined by assigning a numeric value of 0–4 to each hypoglycemia occurrence response (none reported = 0, once = 1, 2–3 times/month = 2, once/week = 3, and daily = 4). The average first and second occurrence scores in patients deintensifying glycemic treatment (n = 395) were 2.08 and 0.76, respectively (–1.32). In screenings documenting no change in treatment (n = 387), there was a decrease in average occurrence score from 1.43 to 0.72 (–0.71). Although both groups had a reduction in average occurrence score, the deintensification group experienced a more significant decrease than the no change group (P <0.001, two-way repeated measures analysis of variance).
The numbers of VISN 12 patients in the high-risk cohort based on data snapshots taken in March 2012 and March 2017 were 4,185 and 4,085, respectively. The proportions of these patients with A1C <7%, <6.5%, and <6% (measures of possible overtreatment) decreased from 35.7 to 28.4% (–20.4%), from 17.2 to 13.7% (–20.3%), and from 5.5 to 4.5% (–18.2%), respectively.
National Expansion
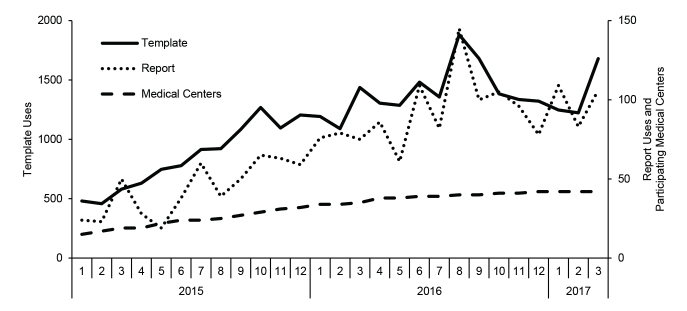
In early 2014, the CW-HSI was implemented in VISN 1, a group of eight VHA medical centers in the Northeast region of the United States; their implementation leveraged the clinical alert and template for point-of-care identification (25). Since making the tools available for all VHA medical centers in January 2015, the online panel reports have been accessed 1,908 times by 481 VHA staff, and the template has been used 31,063 times for 20,051 VHA patients through March 2017. As of March 2017, 44 VHA medical centers have shown participation in the CW-HSI as measured by regular use of the template and/or the online panel reports; regular use was defined as at least 6 consecutive months with use. This includes 15 VISN 1 and VISN 12 medical centers and an additional 29 medical centers across the VHA, 18 showing both template and online panel reports use, 5 showing only template use, and 6 showing only online panel reports use (of which 4 had sustained use into 2017). The number of template uses and online panel report uses, along with the cumulative number of VHA medical centers showing participation by month, are provided in Figure 3. In addition, nine national webinars to educate on CW-HSI key focus areas have been provided, and staff from >80 VHA medical centers have joined the CW-HSI email distribution group (187 members as of April 2017).
FIGURE 3.
VHA CW-HSI adoption by month.
Discussion
Our data demonstrate the feasibility of identifying a specific, manageable patient cohort using electronic methods to support a national initiative, the CW-HSI. The electronic identification of patients allows providers to focus time on the shared decision-making process with patients to make treatment decisions. Integrating the program into the EMR and providing on-demand electronic panel management reports have promoted participation within existing health care workflows. Moreover, the presence of a single systemwide EMR facilitates the scale-up and spread of the initiative, with use of the CW-HSI tools occurring in nearly one-third of VHA medical centers nationwide, based on administrative data. We note that the impact of CW-HSI educational resources and efforts are not entirely captured solely by measuring the use of the EMR tools or online reports.
A goal during risk criteria selection was to identify a low-volume, high-risk group of patients who would benefit greatly from hypoglycemia risk screening and management of possible overtreatment. The CW-HSI patient cohort criteria were met by only nine patients per primary care panel on average. Identification of a small, manageable number of patients may have facilitated the actions of clinicians. With the hypoglycemia screening template, the CW-HSI has been able to demonstrate and measure screening of hypoglycemia occurrence and management of hypoglycemia risk. Within VISN 12, hypoglycemia was found to be frequently reported in the population assessed, with >25% of patients reporting at least one recent episode of hypoglycemia and >5% reporting hypoglycemia at least once per week. Nearly 10% of patients assessed reported at least one recent moderate to severe hypoglycemia episode. These findings validate the criteria applied as being indicative of high risk for hypoglycemia and emphasize the importance of additional patient education and management. Template use analysis showed reductions in the rate of hypoglycemia in all patients after an initial screening. These findings demonstrate the positive impact of treatment deintensification, when performed, as well as the positive impact of a conversation about hypoglycemia occurrence and other measures that may have occurred (e.g., diet adjustments) even without treatment deintensification.
We recognize that the CW-HSI high-risk cohort did not include all potential risk factors for serious hypoglycemia, such as major neurological disorders, cardiovascular disease, major depression, and alcohol/substance abuse (15). Additionally, social determinants of health such as diminished health literacy (26), food insufficiency (27), or quality of life (28) were not considered because of the current inability to identify these in the EMR. Finally, we recognize that many episodes of serious hypoglycemia occur in patients with an A1C >7% (29). Nevertheless, the number of patients identified by our criteria is substantial.
The VISN 12 implementation resulted in a 20% relative reduction from baseline in the percentage of high-risk patients with A1C <7% after 5 years of the program. Although this is a dynamic cohort, this change suggests that the frequency of overtreatment has decreased. The VISN 1 implementation also resulted in reductions in the number of potentially overtreated patients (25). Treatment deintensification occurred in 57% of patients reporting hypoglycemia and 26% of all patients screened in VISN 12. Although the emphasis of the CW-HSI is on individualized assessments rather than an expectation of deintensification of treatment in all patients identified, these findings indicate that many patients and providers are willing to deintensify treatment in response to overtreatment. We note that deintensification occurred more often as the frequency of reported hypoglycemia increased. In addition, deintensification rates were higher in the VISN 12 implementation than the VISN 1 implementation (25); one difference between these two programs was the data timeframe (nearly 5 years in VISN 12 vs. 1 year in VISN 1). This difference may indicate the need in some cases for multiple conversations about glycemic overtreatment and hypo-glycemia risk over time before deintensification occurs. Future work is needed to determine specific provider and patient factors that influence the decision to deintensify treatment.
The diffusion and scale-up of this initiative beyond two early adopters has been modest. The CW-HSI is not immune to well-known challenges in changing provider behavior (in this case, to consider treatment deintensification in appropriate patients with diabetes) and scaling up (30–32). “Unlearning” an outmoded practice (e.g., tight control for all patients with diabetes), especially one that has been well established and highly promoted, may be particularly difficult (30,31). This was found in a recent study that surveyed 594 VHA primary care providers (33). In that study, 39% of respondents thought that a 77-year-old patient with an A1C of 6.5% who was at high risk for hypoglycemia and would not be a can-didate for intensive glycemic control would benefit if his A1C were maintained to <7%, and 45% of respon-dents reported that they would not worry about potential harm from tight control. In addition, 42% worried that deintensification would lead to an A1C outside of what they erroneously believed was a performance measure target of <7%, and 24% worried that deintensification could leave them vulnerable to malpractice claims. Because behavior is diffi-cult to change, interventions to pro-mote practice change typically involve multiple levels of the health care system down to individual clinicians and patients, which the CW-HSI has considered and found to be consistent with a conceptual model of provider behavior change (34). Given the challenges of changing practice, the design of this program as a major initiative is even more important to affect behavior.
The ways in which recommendations for A1C targets are presented can also influence practice. Although organizations that provide diabetes treat-ment recommendations recognize the need to individualize A1C targets based on patient-specific factors, these targets are presented in some instances as upper bound limits only (e.g., <8%) as opposed to a range that also includes a lower bound (e.g., 7–8%). A range presentation emphasizes that there are risks associated with low A1C and that diabetes management should consider both under- and overtreatment.
Future objectives of the VHA CW-HSI workgroup, in collaboration with other VHA programs and federal partners, include promoting EMR documentation of social determinants of health (e.g., food insufficiency) and individualized A1C target ranges rather than dichotomous A1C levels. However, we believe that EMR use alone is insufficient and that informed patients are the foundation of successful shared decision-making. Ultimately, proactive patient engagement and a coordinated national public health effort that includes professional societies and patient advocacy groups will be essential. This effort should be designed to support the recommendations from the multiple guidelines and the DHHS National Action Plan for Adverse Drug Event Prevention (8–12,19,35).
In summary, we share the sentiments of VHA leadership in announcing the CW-HSI in late 2014: “Our objective is to change how diabetes is managed in VA and the United States, and to help patients improve their personal well-being, not just manage their numbers” (13).
Acknowledgments
The authors wish to acknowledge all the members of the VHA CW-HSI workgroup for their ongoing support of the initiative; all VHA medical centers, clinicians, and patients who have embraced the CW-HSI; and the VHA Office of Quality, Safety & Value for hosting the CW-HSI Internet site and endorsing the database for the project.
Funding and Support
This unfunded initiative was developed, implemented, and evaluated by existing VHA staff. This project was deemed to be operations and not research by the Edward Hines, Jr. VA Hospital Institutional Review Board. This work was supported in small part by a grant (SCE 12-181) from the VHA Health Services Research & Development Service/Quality Enhancement Research Initiative (QUERI) to author D.C.A.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
Author Contributions
S.M.W. wrote the manuscript, researched data, contributed to the discussion, and reviewed/edited the manuscript. S.C.H., M.M., and L.M.P. wrote the manuscript, contributed to the discussion, and reviewed/edited the manuscript. B.V.B. wrote the manuscript, researched data, and reviewed/edited the manuscript. S.A.W. and D.C.A. contributed to the discussion and reviewed/edited the manuscript. D.M.L. reviewed/edited the manuscript. S.M.W. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the views of the Department of Veterans Affairs or the U.S. government.
Previous Presentations
A description of the CW-HSI and selected data were presented at the AcademyHealth Concordium 2016 on 13 September 2016 in Arlington, Va.; the 2016 Guidelines International Network Conference on 28 September 2016 in Philadelphia, Pa.; the 2016 CMS Quality Conference on 14–15 December 2016 in Baltimore, Md.; and at the Food and Drug Administration, Center for Drug Evaluation and Research, Professional Affairs and Stakeholder Engagement Staff (PASES) public workshop on Reducing the Risk of Preventable Adverse Drug Events Associated With Hypoglycemia in the Older Population on 12 September 2017 in Silver Spring, Md.
References
- 1.Aron DC. No “black swan”: unintended but not unanticipated consequences of diabetes performance measurement. Jt Comm J Qual Patient Saf 2013;39:106–108 [DOI] [PubMed] [Google Scholar]
- 2.Lipska KJ, Ross JS, Wang Y, et al. . National trends in U.S. hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, 1999 to 2011. JAMA Intern Med 2014;174:1116–1124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ACCORD Study Group Nine-year effects of 3.7 years of intensive glycemic control on cardiovascular outcomes. Diabetes Care 2016;39:701–708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hayward RA, Reaven PD, Wiitala WL, et al.; VADT Investigators . Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2015;372:2197–2206 [DOI] [PubMed] [Google Scholar]
- 5.Zoungas S, Chalmers J, Neal B, et al.; ADVANCE-ON Collaborative Group . Follow-up of blood-pressure lowering and glucose control in type 2 diabetes. N Engl J Med 2014;371:1392–1406 [DOI] [PubMed] [Google Scholar]
- 6.Pogach LM, Brietzke SA, Cowan CL Jr, Conlin P, Walder DJ, Sawin CT; VA/DoD Diabetes Guideline Development Group . Development of evidence-based clinical practice guidelines for diabetes: the Department of Veterans Affairs/Department of Defense guidelines initiative. Diabetes Care 2004;27(Suppl. 2):B82–B89 [DOI] [PubMed] [Google Scholar]
- 7.U.S. Department of Veterans Affairs Shared decision making with the patient with diabetes [Internet]. Available from https://www.healthquality.va.gov/guidelines/CD/diabetes/cpgSDMDMPOCKETFinalPRESS022513.pdf. Accessed 24 April 2017
- 8.ABIM Foundation American Geriatrics Society: avoid using medications other than metformin to achieve hemoglobin A1c<7.5% in most older adults; moderate control is generally better [Internet]. Available from http://www.choosingwisely.org/clinician-lists/american-geriatrics-society-medication-to-control-type-2-diabetes/. Accessed 24 April 2017
- 9.American Geriatrics Society Expert Panel on Care of Older Adults with Diabetes Mellitus; Moreno G, Mangione CM, Kimbro L, Vaisberg E. Guidelines abstracted from the American Geriatrics Society guidelines for improving the care of older adults with diabetes mellitus: 2013 update. J Am Geriatr Soc 2013;61:2020–2026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Inzucchi SE, Bergenstal RM, Buse JB, et al.; American Diabetes Association; European Association for the Study of Diabetes . Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012;35:1364–1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Canadian Diabetes Association Clinical Practice Guidelines Expert Committee; Cheng AY Canadian Diabetes Association 2013 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes 2013;37(Suppl. 1):S1–S216 [DOI] [PubMed] [Google Scholar]
- 12.U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion National Action Plan for Adverse Drug Event Prevention. Washington, D.C., U.S: Department of Health and Human Services, 2014 [Google Scholar]
- 13.U.S. Department of Veterans Affairs VA implements national hypoglycemic safety initiative [Internet]. Available from https://www.va.gov/opa/pressrel/includes/viewPDF.cfm?id=2666. Accessed 24 April 2017
- 14.ABIM Foundation VA Choosing Wisely task force helps elderly veterans with diabetes [Internet]. Available from http://www.choosingwisely.org/resources/updates-from-the-field/va-choosing-wisely-task-force-helps-elderly-veterans-with-diabetes/. Accessed 25 April 2017
- 15.Tseng CL, Soroka O, Maney M, Aron DC, Pogach LM. Assessing potential glycemic overtreatment in persons at hypoglycemic risk. JAMA Intern Med 2014;174:259–268 [DOI] [PubMed] [Google Scholar]
- 16.Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med 2011;365:2002–2012 [DOI] [PubMed] [Google Scholar]
- 17.Miller ME, Bonds DE, Gerstein HC, et al.; ACCORD Investigators . The effects of baseline characteristics, glycaemia treatment approach, and glycated haemoglobin concentration on the risk of severe hypoglycaemia: post hoc epidemiological analysis of the ACCORD study. BMJ 2010;340:b5444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Punthakee Z, Miller ME, Launer LJ, et al.; ACCORD Group of Investigators; ACCORD-MIND Investigators . Poor cognitive function and risk of severe hypoglycemia in type 2 diabetes: post hoc epidemiologic analysis of the ACCORD trial. Diabetes Care 2012;35:787–793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.U.S. Department of Veterans Affairs Management of diabetes mellitus in primary care (2017): VA/DoD clinical practice guidelines [Internet]. Available from https://www.healthquality.va.gov/guidelines/CD/diabetes/. Accessed 25 April 2017
- 20.U.S. Department of Veterans Affairs Diabetes health survey [Internet]. Available from https://www.hsrd.minneapolis.med.va.gov/PDF/Diabetes_Health_Survey.pdf. Accessed 8 June 2017
- 21.Self-Management Resource Center English evaluation tools: hypoglycemia [Internet]. Available from http://www.selfmanagementresource.com/resources/evaluation-tools/english-evaluation-tools. Accessed 8 June 2017
- 22.U.S. Department of Veterans Affairs Privacy Act of 1974: a notice by the Veterans Affairs Department on 01/27/2014. Federal Register 2014;79:4377–4382. Available from https://www.gpo.gov/fdsys/pkg/FR-2014-01-27/pdf/2014-01497.pdf. Accessed 11 December 2017 [Google Scholar]
- 23.U.S. Department of Veterans Affairs Quality, safety & value: hypoglycemia safety initiative (HSI) [Internet]. Available from https://www.qualityandsafety.va.gov/ChoosingWiselyHealthSafetyInitiative/HypoglycemiaSite/Hypoglycemia.asp. Accessed 25 April 2017
- 24.U.S. Department of Veterans Affairs My HealtheVet veterans health library [Internet]. Available from http://www.veteranshealthlibrary.org/. Accessed 1 June 2017
- 25.Vimalananda VG, DeSotto K, Chen T, et al. . A quality improvement program to reduce potential overtreatment of diabetes among Veterans at high risk of hypoglycemia. Diabetes Spectr 2017;30:211–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care 2006;29:823–829 [DOI] [PubMed] [Google Scholar]
- 27.Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr 2010;140:304–310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang ES, Brown SE, Ewigman BG, Foley EC, Meltzer DO. Patient perceptions of quality of life with diabetes-related complications and treatments. Diabetes Care 2007;30:2478–2483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pathak RD, Schroeder EB, Seaquist ER, et al.; SUPREME-DM Study Group . Severe hypoglycemia requiring medical intervention in a large cohort of adults with diabetes receiving care in U.S. integrated health care delivery systems: 2005–2011. Diabetes Care 2016;39:363–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rushmer R, Davies HT. Unlearning in health care. Qual Saf Health Care 2004;13(Suppl. 2):ii10–ii15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gupta DM, Boland RJ Jr, Aron DC. The physician’s experience of changing clinical practice: a struggle to unlearn. Implement Sci 2017;12:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Greenhalgh T, Robert G, Bate P, Kyriakidou O, Macfarlane F, Peacock R. How to spread good ideas: a systematic review of the literature on diffusion, dissemination and sustainability of innovations in health service delivery and organization. Report for the National Co-ordinating Centre for NHS Service Delivery and Organisation R & D (NCCSDO), 2004. Available from http://www.netscc.ac.uk/hsdr/files/project/SDO_FR_08-1201-038_V01.pdf. Accessed 11 December 2017 [Google Scholar]
- 33.Caverly TJ, Fagerlin A, Zikmund-Fisher BJ, et al. . Appropriate prescribing for patients with diabetes at high risk for hypoglycemia: national survey of Veterans Affairs health care professionals. JAMA Intern Med 2015;175:1994–1996 [DOI] [PubMed] [Google Scholar]
- 34.Aron DC, Lowery J, Tseng CL, Conlin P, Kahwati L. De-implementation of inappropriately tight control (of hypoglycemia) for health: protocol with an example of a research grant application. Implement Sci 2014;9:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.U.S. Food and Drug Administration Reducing the risk of preventable adverse drug events associated with hypoglycemia in the older population [Internet]. Available from https://www.fda.gov/Drugs/NewsEvents/ucm538666.htm. Accessed 11 May 2017