Abstract
IN BRIEF After assessing patient perspectives on the success of current diabetes therapies and the factors that have the greatest impact on daily life, we show that time-in-range is a crucial outcome for people with diabetes and that current therapies are falling short on this metric. We also show that patients feel significant stress and worry, and they believe they are falling short in diet, exercise, and weight maintenance. In addition, they believe diet and exercise and in-range blood glucose are the biggest drivers of improved diabetes management and mindset. Together, these findings support the need for therapies that improve outcomes including and beyond A1C.
Although the past 30 years have seen significant innovation in diabetes drug and device development, the economic and human burden of the disease remains enormous. Spending on diabetes in the United States is greater than ever before, yet a staggering number of people continue to develop disabling and life-threatening vascular complications (1). In 2011 alone, about 282,000 people with diabetes in the United States visited an emergency room for hypoglycemia, and about 175,000 visited an emergency room for hyperglycemic crises (2). Diabetes remains a leading cause of kidney failure, lower-limb amputations, and myocardial infarctions (2). People with diabetes also have a 60% higher rate of major depressive disorder, a 123% higher rate of general anxiety disorder, and an 85% higher rate of panic disorder compared to the general population (3).
A1C is currently the metric of choice for assessing the efficacy of new diabetes products, guiding health care providers’ choice of medications, and supporting regulatory approval and reimbursement policies. Although A1C has proven useful for predicting the long-term risk of complications from hyperglycemia, it cannot assess a therapy’s ability to deliver important short-term outcomes that affect patients’ day-to-day experiences (4,5). For this reason, A1C has limited ability to influence patients to effectively use therapies to obtain positive long-term outcomes (4).
Of critical importance, A1C does not capture hypoglycemia, the associated costs of which are momentous for patients and health care systems alike. Recent epidemiologic studies assessing mortality in type 1 diabetes found hypoglycemia to be the reported cause for 5–10% of all deaths (6–8). In 2009, hypoglycemia hospitalizations alone cost the American health care system an estimated $4.7 billion ($0.5 million/hour) at an average estimated cost of $17,654 each (9,10). More than 92% of these hospitalizations were for people with type 2 diabetes, a population that a separate study involving more than 500,000 people found to experience severe hypoglycemic events at a rate of roughly 1 in 20 individuals (11).
Hypoglycemia and fear of hypoglycemia present a challenge to the achievement of near-normal glycemia because the risk of hypoglycemia usually increases in people with well-managed diabetes, despite being present irrespective of the degree of glucose control (12). In a landmark JDRF continuous glucose monitoring (CGM) study, people with diabetes whose A1C levels were <7% spent >90 min/day with glucose levels <70 mg/dL (13). In the more recent IMPACT (An Evaluation of Novel Glucose Sensing Technology on Hypoglycemia in Type 1 Diabetes) study, participants with similarly well-controlled diabetes (A1C 6.7%) spent >200 min/day with blood glucose levels <70 mg/dL at baseline (14).
Another challenge of using A1C as an indicator of glycemic control relates to individual differences in hemoglobin glycation. A recent study demonstrated a range of ∼80 mg/dL in average glucose for the same A1C level (15). Similarly, a 2008 study showed that an A1C value of 7% reflected average blood glucose ranging from 123 to 185 mg/dL; for an A1C of 11%, the range was even greater, at 217–314 mg/dL (16). Moreover, a recent paper by Beck et al. (17) demonstrated that varying patterns of glycemic control are possible even with identical A1C levels and similar mean glucose concentrations. Variations such as these inevitably challenge clinicians titrating therapy for patients and serve as a reminder of the imprecision of A1C as a stand-alone metric.
A1C also does not capture the impact of therapy on daily quality of life, including its impact on stress and worry caused by diabetes. Diabetes is an extremely burdensome, relentless condition that more than doubles the risk of depression, which in turn has been associated with poor medication adherence and an increased risk of complications and mortality (3,18–20). As a result, A1C is of limited value when it comes to developing diabetes products that reduce patient burden and increase therapy adherence.
A1C is a useful and validated metric, but other outcomes may be of equal or greater interest to patients and may gauge diabetes therapy success more comprehensively than A1C alone, especially with the advent of accurate and reliable new technology such as CGM. Numerous studies have attempted to analyze patients’ perspectives on diabetes management, yet few have investigated the foremost factors affecting their daily lives and well-being (21–29). This study aims to address this gap to better understand patients’ perspectives on the success of current diabetes therapies, the factors having the greatest impact on their daily lives, and the drivers of diabetes and mindset improvement.
Research Design and Methods
Participants
This study was conducted through an online survey. Participants were members of the dQ&A (San Francisco, Calif.) Patient Panel, a proprietary research panel of people with type 1 or type 2 diabetes. Panel members are invited to respond to quarterly market research tracking surveys and occasional one-time or single-topic surveys.
Procedures
The invitation email mentioned the survey topic, explaining that the results would be presented at a U.S. Food and Drug Administration workshop on diabetes outcome measures beyond A1C. Overall, the survey was in the field from 17 August through 22 August 2016. Respondents received $5.00 USD for completing the survey.
Questionnaire
The online survey presented respondents with 25 questions (Supplementary Table S1). One part of the survey assessed patients’ perceptions of the success of current diabetes drugs and devices across six categories: 1) blood glucose management, 2) complications and comorbidities, 3) freedom from stress and worry, 4) burden of diabetes care, 5) family and relationships, and 6) social interactions. The survey also investigated which factors have the biggest impact on patients’ daily lives and which changes would have the biggest positive impact on diabetes management and mindset. Other sections of the survey covered mental well-being, quality of life, desired improvements for future therapies, relationships with health care providers, and the concerns of loved ones.
Survey questions were developed by several of the authors, based on their personal and professional experiences with diabetes. To further enrich the data and provide a fuller picture of the respondents, survey data were collated with respondents’ demographics, drug and device usage, and health data, which were collected in a quarterly tracking survey 2 months earlier (Supplementary Table S2). The survey was programmed and fielded through Qualtrics (Provo, Utah).
Data Analysis
Respondents were segmented into three groups for analysis: people with type 1 diabetes (T1), people with type 2 diabetes on insulin therapy (T2I), and people with type 2 diabetes not on insulin therapy (T2NI). Data were analyzed using MarketSight software (MarketSight LLC, Newton, Mass.) and Microsoft Excel (Microsoft, Inc., Redmond, Wash.). Statistical significance was tested using a z test at the 95% confidence level.
Results
Baseline Demographics
The survey invitation was received by 4,701 people living with type 1 or type 2 diabetes. Of these, 3,461 respondents completed the survey—a 74% response rate (80% for T1, 72% for T2). The survey responses were stratified into three groups: T1 (30% of respondents, n = 1,026, mean age 52.1 years [SD 13.5 years]), T2I (33% of respondents, n = 1,154, mean age 62.2 years [SD 9.7 years]), and T2NI (37% of respondents, n = 1,281, mean age 62.7 years [SD 10.0 years]). Women made up 62% of the total study population (65% for T1, 59% for T2I, 63% for T2NI). Caucasian respondents made up 92% of the study population, and individuals between the ages of 55 and 64 years made up 34% of the population. Complete demographic data is shown in Supplementary Table S2.
Impact on Daily Life
Food choices was rated as having a “big impact” on daily life by the highest percentage of respondents in each of the three groups (T1, T2I, and T2NI) (Table 1). Of outcomes that can be used to assess diabetes therapies, time-in-range was the highest-ranking one believed to have a “big impact” on daily life by all groups (57% of T1, 45% of T2I, and 41% of T2NI), second only to food choices in all instances. However, nearly as many T2 respondents (44% of T2I and 41% of T2NI) rated A1C as a “big impact” factor, indicating roughly equal relative importance of time-in-range and A1C for these two groups. By contrast, unexpected blood glucose numbers (42%) and dosing insulin (37%) were both believed by T1 respondents to have a larger impact on daily life than A1C (30%); hypoglycemia (30%) was approximately on par with A1C. Moreover, nondiabetes health issues were more commonly scored as a “big impact” factor by T2I and T2NI respondents than by those in the T1 group (Table 1). See full results in Supplementary Figure S1.
TABLE 1.
Ranking of Factors That Have a “Big Impact” on Daily Life With Diabetes by Respondents’ Diabetes Type and Therapy
| Rank* | Diabetes/Therapy Type |
||
|---|---|---|---|
| T1 | T2I | T2NI | |
| 1 | Food choices (63%) | Food choices (67%) | Food choices (64%) |
| 2 | Time-in-range (57%) | Time-in-range (45%) A1C (44%) |
Time-in-range (41%) A1C (41%) |
| 3 | Unexpected blood glucose numbers (42%) | Nondiabetes health issues (36%) Dosing insulin (34%) |
Nondiabetes health issues (31%) |
| 4 | Dosing insulin (37%) | Unexpected blood glucose numbers (28%) | Unexpected blood glucose numbers (20%) |
| 5 | Hypoglycemia (30%) A1C (30%) Nondiabetes health issues (27%) |
Symptoms of complications (24%) | Symptoms of complications (15%) |
This table depicts the percentage of survey respondents within each group who scored a particular factor (e.g., food choices) as having a “big impact” on daily life with diabetes. To better understand the relative importance of these factors, they have been grouped and ranked according to measurable breaks of 4%. In each group food choices was the highest-ranking “big impact” factor and was followed by a measurable break in all instances. Whereas a measurable break also follows time-in-range (defined in the survey as “time spent in the ideal blood glucose range”) for T1 respondents, time-in-range and A1C fell within the same group for all T2 respondents, regardless of whether they were on insulin therapy, indicating roughly equal relative importance. In contrast, a far smaller proportion of T1 respondents considered A1C to have as big of an impact as time-in-range in their daily life. Because food choices cannot be used to assess diabetes therapies, time-in-range emerged as the measurable therapy outcome that had the biggest impact on daily life with diabetes for all groups of respondents. Note that differences across diabetes/therapy type groups are not necessarily significant (see Supplementary Figure S1 for full data).
Current Therapy Success on Time-in-Range Measures
In the survey’s blood glucose management category, questions assessing therapeutic efficacy for time-in-range measures received the lowest percentage of “very successful” responses (full results in Supplementary Table S3). This was consistent for each of the three groups.
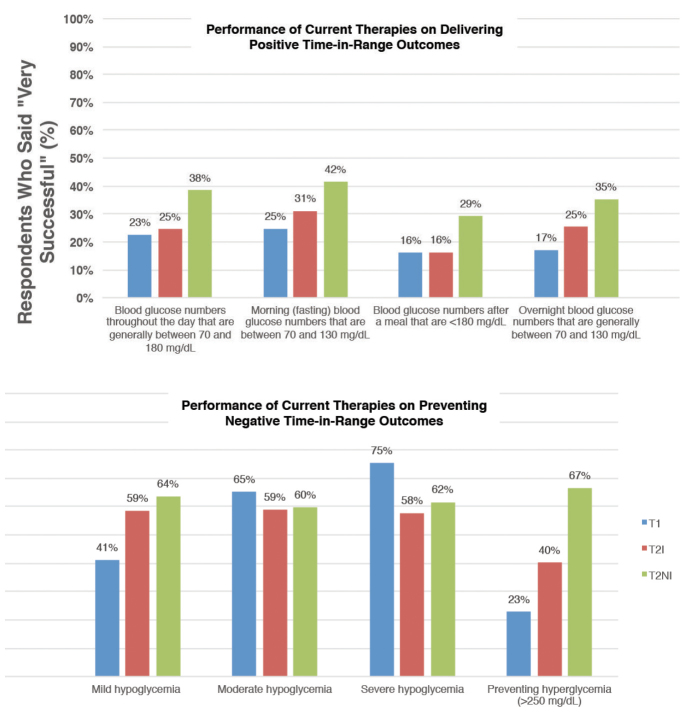
A minority of respondents perceived their current diabetes care regimen to be “very successful” at delivering positive time-in-range outcomes: in-range blood glucose throughout the day, in the morning, after meals, and overnight (Figure 1). Lower perceptions of treatment success were especially evident for respondents on insulin, with only 16–25% of T1 and 16–31% of T2I respondents perceiving their current therapy to be “very successful” on the positive time-in-range measures evaluated. For T2NI respondents, whose overall perception of current therapy success was higher, 29–42% perceived their current therapy to be “very successful” at delivering positive outcomes for the measures evaluated. Across all diabetes and therapy types, the lowest percentage of respondents found their current therapy to be “very successful” at delivering blood glucose numbers <180 mg/dL after a meal.
FIGURE 1.
Perceived success of current therapies on time-in-range measures. Survey respondents were asked to rate the success of current diabetes therapies on a variety of time-in-range metrics, including positive outcomes (e.g., blood glucose levels of 70–180 mg/dL throughout the day, <180 mg/dL after meals, and fasting and overnight glucose levels of 70–130 mg/dL) and negative outcomes (e.g., mild, moderate, and severe hypoglycemia and severe hyperglycemia). In most cases, perceived success was lower in insulin users (T1 and T2I) than in noninsulin users (T2NI). Therapies were rated as the least successful for delivering postmeal blood glucose levels <180 mg/dL. Therapies scored highest for preventing severe hypoglycemia. Survey respondents tended to perceive greater therapy success in preventing negative time-in-range outcomes than in delivering positive time-in-range outcomes.
A higher percentage of respondents found their current diabetes care regimen to be “very successful” at preventing negative time-in-range outcomes: mild, moderate, or severe hypoglycemia or hyperglycemia (Figure 1). More than half of T2NI respondents reported their therapies were “very successful” at preventing each of these negative time-in-range outcomes. Insulin users gave therapies much lower success ratings for preventing hyperglycemia (blood glucose >250 mg/dL) (T1, 23%; T2I, 40%) relative to noninsulin users (T2NI, 67%).
Current Therapy Success on Delivering Freedom From Worry
In addition to the low perceptions of current therapy success on time-in-range measures (Figure 1), freedom from stress and worry was strikingly low across all diabetes and therapy types (Supplementary Table S3). There was not a single question on freedom from stress and worry for which a majority of any group (T1, T2I, or T2NI) said their current care was “very successful” (e.g., at preventing/limiting negative feelings or freeing them from worry about diabetes).
Current therapies received particularly low success scores on the following questions:
“How successful is your current diabetes care regime at freeing you from worry about your glucose numbers during the day?” “Very Successful” was indicated by 16% of T1, 21% of T2I, and 33% of T2NI respondents.
“How successful is your current diabetes care regime at freeing you from worry about the longer-term outlook for your health?” “Very Successful” was indicated by 19% of T1, 19% of T2I, and 27% of T2NI respondents.
“How successful is your current diabetes care regime at preventing or limiting frustration or discouragement about your diabetes?” “Very Successful” was indicated by 17% of T1, 21% of T2I, and 32% of T2NI respondents.
In aggregating responses in the freedom from stress and worry category, an average of 22% of T1 respondents found their current therapies to be “very successful.” For T2I respondents, this average was only slightly higher at 24%, compared to 34% for T2NI respondents. In sum, these data highlight the stress and worry perceived by people with diabetes on insulin therapy. The added burden of insulin therapy is further highlighted in Supplementary Table S3; about half as many insulin users (T1 and T2I) found current therapies to be “very successful” at “limiting the mental effort needed to manage your diabetes.” Similar disparities emerged between insulin users and noninsulin users on the time required to manage diabetes.
Other Categories: Complications, Burden, Relationships, Social Interactions
Supplementary Table S3 contains success scores for other categories. The results generally parallel those discussed above, with lower success among insulin users. However, the T1 and T2I/T2NI groups varied in their lowest and highest success ratings.
For T1, only 16% said their therapies were “very successful” at “minimizing the amount of ‘diabetes stuff’ you need to keep with you.” The greatest reported success was for preventing kidney problems caused by diabetes; 70% perceived their therapies as “very successful” at doing so.
For T2I and T2NI, only 10 and 17%, respectively, said their therapies were “very successful” at reaching or maintaining a healthy weight. The greatest reported success was for “preventing you from feeling embarrassed about having diabetes”; 54 and 68%, respectively, said their therapies were “very successful” at doing so.
Potential Drivers of Diabetes Improvement
A substantial proportion of respondents in each group (26% T1, 35% T2I, 50% T2NI) reported that a change in diet and exercise would have the biggest positive impact on their diabetes, likely resulting in a “big improvement” in their health (Table 2). Notably, for both T2I and T2NI respondents, this was the highest ranked driver of diabetes improvement; for T1 respondents, it ranked as the second most impactful driver of diabetes improvement, after “medical devices” (Table 2). This aligns with the low success scores for weight maintenance in T2I and T2NI, noted above. After diet and exercise, medications, then emotional state, were ranked by the highest percentage of respondents in each group (T1, T2I, and T2NI) as the biggest driver of diabetes improvement.
TABLE 2.
Ranking of Factors That Would Most Drive Diabetes Improvement by Respondents’ Diabetes Type and Therapy
| Rank* | Diabetes/Therapy Type |
||
|---|---|---|---|
| T1 | T2I | T2NI | |
| 1 | Medical devices (35%) | Diet and exercise (35%) | Diet and exercise (50%) |
| 2 | Diet and exercise (26%) | Medications (22%) | Medications (18%) |
| 3 | Medications (14%) Emotional state (12%) |
Emotional state (15%) | Emotional state (12%) HCP care (9%) |
| 4 | HCP care (5%) | HCP care (10%) Medical devices (10%) |
Medical devices (4%) |
This table depicts the percentage of survey respondents within each group who ranked a particular factor (e.g., diet and exercise) as what would have the biggest positive impact on diabetes. To better understand the relative importance of these factors, they have been grouped and ranked according to measurable breaks of 4%. For both groups of T2 respondents (T2I, T2NI), diet and exercise was the factor most believed to be the biggest driver of diabetes improvement, followed by medications. For T1 respondents, these highest-ranking factors were medical devices, followed by diet and exercise. HCP, health care provider.
Potential Drivers of a Positive Mindset
For 54% of T1 and 36% of T2I respondents (those taking insulin), “Your blood glucose numbers are on-target all day” ranked as the highest driver of a positive mindset. This factor was ranked second for T2NI respondents, after “You take your diabetes medications exactly as prescribed” (Table 3).
TABLE 3.
Ranking of Factors That Would Most Contribute to a Positive Frame of Mind by Respondents’ Diabetes Type and Therapy
| Rank* | Diabetes/Therapy Type |
||
|---|---|---|---|
| T1 | T2I | T2NI | |
| 1 | Your blood glucose numbers are on-target all day (54%) | Your blood glucose numbers are on-target all day (36%) | You take your diabetes medications exactly as prescribed (29%) |
| 2 | You are relaxed and taking your diabetes in stride (15%) You get the exercise you need or want (14%) |
You take your diabetes medications exactly as prescribed (27%) | Your blood glucose numbers are on-target all day (22%) |
| 3 | You eat healthy food at every meal (9%) You take your diabetes medications exactly as prescribed (8%) |
You are relaxed and taking your diabetes in stride (14%) You eat healthy food at every meal (12%) You get the exercise you need or want (10%) |
You eat healthy food at every meal (18%) You are relaxed and taking your diabetes in stride (16%) You get the exercise you need or want (14%) |
This table depicts the percentage of survey respondents within each group who ranked a particular statement (e.g., “Your blood glucose numbers are on-target all day”) as being most likely put them in a positive frame of mind about their diabetes and health. To better understand the relative importance of these factors, they have been grouped and ranked according to measurable breaks of 3%. For both groups of insulin users (T1, T2I), “Your blood glucose numbers are on-target all day” was the statement most commonly ranked by respondents as what they believed most likely to put them in a positive frame of mind. For T2I and T2NI respondents, “You take your diabetes medications exactly as prescribed” was also selected by many as the factor they believed most likely to contribute to a positive frame of mind; it was the highest-ranking factor for the T2NI group and second highest for the T2I group.
Conclusions
The primary objective of this study was to evaluate patient perspectives on the success of current diabetes therapies, the factors having the greatest impact on daily life, and the drivers of improved diabetes management and mindset. Results from the survey collectively suggest the need for diabetes treatment development and regulation that more expansively evaluate what matters to patients and that better align outcomes with patient challenges and priorities.
Our results underscore the need to consider the full spectrum of patients’ daily glycemia rather than simply the 3-month average, as measured by A1C. “Time spent in the ideal blood glucose range” was rated as having a “big impact” by all three groups surveyed, second only to food choices in all instances and on par with A1C for T2 respondents. Although central to daily diabetes management, food choices is not a metric for assessing diabetes therapies; therefore, time-in-range emerged as the top outcome measure that both reflects patients’ priorities and can be used to quantitatively evaluate treatment efficacy.
Notably, nearly double the number of T1 respondents scored “time spent in the ideal blood glucose range” as having a “big impact” on daily life with diabetes than those scoring A1C as having a “big impact,” whereas T2 respondents (T2I and T2NI) indicated roughly equal relative importance of these two outcomes (Table 1). Furthermore, respondents taking insulin (T1 and T2I) rated “your blood glucose numbers are on-target all day” as the highest driver of a positive mindset; T2NI respondents rated it as the second-highest driver (Table 3). Together, these results suggest that time-in-range is an important mental and emotional consideration for people with diabetes, and particularly for those taking insulin. The results also serve as a testament to the daily reality of living with diabetes, which is experienced as a physical and psychological battle between hypoglycemia and hyperglycemia. Patients may perceive more daily time-in-range as having greater success with their diabetes, whereas A1C is not likely to have the same daily relevance or result in the equivalent feelings of personal or therapeutic success.
Despite highlighting the “big impact” that time-in-range can have on daily life with diabetes, <50% of respondents reported that their current therapy was “very successful” at achieving positive time-in-range outcomes. Taken together, these data suggest that current therapies are not delivering on time-in-range for most respondents.
Success scores were also low for preventing weight gain and allowing diet and exercise flexibility (Supplementary Table S3), suggesting that lifestyle modification strategies are a major unmet need for people with diabetes. In fact, food choices was rated as having a “big impact” by the highest percentage of T1, T2I, and T2NI respondents (Table 1). All three groups also reported that changing their diet and exercise would be a stronger driver of diabetes improvement than changing their medications, emotional state, or the care they get from health care providers (Table 2).
Throughout, our survey highlights the misalignment between the short-term factors that people with diabetes experience (e.g., food selection, hypo- and hyperglycemia, and weight loss) and how their management is evaluated by many health care providers, regulatory authorities, manufacturers, and payers, which is on a longer-term basis, by A1C and the rate of hyperglycemia-induced complications.
Several limitations are noteworthy. First, all answers were self-reported and collected online, and demographic, health, and drug and device usage data were collected 2 months before the survey administration. Second, although we surveyed a robust and diverse population, our panel is not nationally representative; respondents recruited from online diabetes communities tend to skew toward those who may be more engaged in their diabetes management and have the resources to seek support online (30,31). This suggests that, although respondents overall reported low success, results from a more nationally representative population might demonstrate even lower success scores. Moreover, representation of ethnic minorities in the panel is lower than in the general diabetes population.
Nevertheless, our survey demonstrates that patients do not believe their current therapies are very successful at achieving a host of physical, psychological, and social outcomes (Supplementary Table S3). Few people with diabetes (T1 or T2) reported feeling “very successful” in areas they perceived to have the biggest impact on their daily life—notably, food choices and time-in-range. Freedom from stress and worry—a crucial component of quality of life—also ranked particularly low across the board (Supplementary Table S3C). Collectively, these results showcase significant unmet needs in current diabetes outcomes and care.
Although decades of innovation have advanced certain aspects of diabetes management, the economic and human costs of diabetes remain high (1–4), and therapies are still not succeeding on what matters most to patients. Perhaps most promising is the prospect of capturing information on time-in-range with newer and more accurate CGM devices. We hope the results of this survey motivate manufacturers to evaluate time-in-range more frequently during clinical testing of new diabetes therapies to assess safety and efficacy in a way that reflects what matters most to patients and better reflects daily diabetes management. Moreover, we hope this work prompts future exploration of the psychosocial and behavioral factors that have a big impact on daily life with diabetes (e.g., freedom from stress and worry and food choices), as well as how such priorities can be better incorporated into patient care, product research and development, regulatory risk-benefit decisions, and health care systems to advance real-world diabetes therapy performance and health outcomes.
Supplementary Material
Acknowledgments
The authors thank Lilly Diabetes, Dexcom, and The Apple Pickers Foundation for providing funding in support of this research.
Funding
This dQ&A study was commissioned by The diaTribe Foundation. Lilly Diabetes, Dexcom, and The Apple Pickers Foundation contributed funds that were used for the project.
Duality of Interest
The authors from Close Concerns (A.S.B., A.E.D., B.J.L., S.A.O., and K.L.C.) report that some academic institutions, government bodies, and pharmaceutical and device companies in the diabetes field subscribe to the company’s fee-based newsletter Closer Look. The authors from The diaTribe Foundation (A.S.R., L.K., A.S.B., and K.L.C.) report that their organization receives donations from some pharmaceutical and device companies in the diabetes field. The authors from dQ&A Market Research Inc. (S.P.K. amd R.W.) report that that company’s clients include several pharmaceutical and device companies in the diabetes field. I.B.H. independently consults for Abbott Diabetes Care, Adocia, BigFoot Biomedical, Intarcia, and Roche. No other potential conflicts of interest relevant to this article were reported.
Author Contributions
R.W., K.L.C., A.S.B., and S.P.K. developed the study protocol, provided statistical analysis, and contributed to data interpretation. A.S.R., L.K., A.E.D., B.J.L., V.S.I., S.A.O., and I.B.H. contributed to data interpretation and wrote the manuscript. All authors reviewed the manuscript and accept responsibility for the contents of this report. R.W. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation
Portions of the study findings were presented at the U.S. Food and Drug Administration’s Public Workshop: Diabetes Outcome Measures Beyond Hemoglobin A1c (HbA1c) in August 2016, in a late-breaking poster at the American Diabetes Association’s 77th Scientific Sessions in June 2017, and at The diaTribe Foundation’s meeting on Glycemic Outcomes Beyond A1c: Implementation and Standardization in July 2017.
Footnotes
This article contains supplementary data online at http://clinical.diabetesjournals.org/lookup/suppl/doi:10.2337/cd17-0094/-/DC1
References
- 1.American Diabetes Association Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1033–1046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention National diabetes statistics report, 2014. Available from CDC.gov. https://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed 20 December 2016
- 3.Lin EH, Rutter CM, Katon W, et al. . Depression and advanced complications of diabetes: a prospective cohort study. Diabetes Care 2010;33:264–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DCCT Research Group. Diabetes Control and Complications Trial (DCCT): results of feasibility study. Diabetes Care 1987;10:1–19 [DOI] [PubMed] [Google Scholar]
- 5.King P, Peacock I, Donnelly R. . The UK Prospective Diabetes Study (UKPDS): clinical and therapeutic implications for type 2 diabetes. Br J Clin Pharmacol 1999;48:643–648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Writing Group for the DCCT/EDIC Research Group; Orchard TJ, Nathan DM, Zinman B, et al. . Association between 7 years of intensive treatment of type 1 diabetes and long-term mortality. JAMA 2015;313:45–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lung TW, Petrie D, Herman WH, et al. . Severe hypoglycemia and mortality after cardiovascular events for type 1 diabetic patients in Sweden. Diabetes Care 2014;37:2974–2981 [DOI] [PubMed] [Google Scholar]
- 8.Livingstone SJ, Levin D, Looker HC, et al. . Estimated life expectancy in a Scottish cohort with type 1 diabetes, 2008–2010. JAMA 2015;313:37–44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singh G, Mithal A, Mannalithara A, et al. . Hospitalizations due to severe hypoglycemia in patients with type 2 diabetes: a U.S. national perspective (Abstract 279-OR). Diabetes 2013;62(Suppl.1):A72 [Google Scholar]
- 10.Quilliam BJ, Simeone JC, Ozbay AB, Kogut SJ. The incidence and costs of hypoglycemia in type 2 diabetes. Am J Manag Care 2011;17:673–680 [PubMed] [Google Scholar]
- 11.Edridge CL, Dunkley AJ, Bodicoat DH, et al. . Prevalence and incidence of hypoglycaemia in 532,542 people with type 2 diabetes on oral therapies and insulin: a systematic review and meta-analysis of population based studies. Plos One 2015;10:e0126427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lipska KJ, Warton EM, Huang ES, et al. . HbA1c and risk of severe hypoglycemia in type 2 diabetes: the Diabetes and Aging Study. Diabetes Care 2013;36:3535–3542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.JDRF Research Foundation Continuous Glucose Monitoring Study Group; Tamborlane WV, Beck RW, Bode BW, et al. . Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med 2008;359:1464–1476 [DOI] [PubMed] [Google Scholar]
- 14.Bolinder J, Antuna R, Geelhoed-Duijvestijn P, Kröger J, Weitgasser R. Novel glucose-sensing technology and hypoglycaemia in type 1 diabetes: a multicentre, non-masked, randomised controlled trial. Lancet 2016;388:2254–2263 [DOI] [PubMed] [Google Scholar]
- 15.Bergenstal RM, Gal RL, Connor CG, et al. . Racial differences in the relationship of glucose concentrations and hemoglobin A1c levels. Ann Intern Med 2017;167:95–102 [DOI] [PubMed] [Google Scholar]
- 16.Nathan DM, Kuenen J, Borg R, Zheng H, Schoenfeld D, Heine RJ. Translating the A1C assay into estimated average glucose values. Diabetes Care 2008;31:1473–1478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beck RW, Connor CG, Mullen DM, Wesley DM, Bergenstal RM. The fallacy of average: how using HbA1c alone to assess glycemic control can be misleading. Diabetes Care 2017;40:994–999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gonzalez JS, Safren SA, Cagliero E, et al. . Depression, self-care, and medication adherence in type 2 diabetes: relationships across the full range of symptom severity. Diabetes Care 2007;30:2222–2227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Groot MD, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med 2001;63:619–630 [DOI] [PubMed] [Google Scholar]
- 20.Fisher L, Skaff MM, Mullan JT, Arean P, Glasgow R, Masharani U. A longitudinal study of affective and anxiety disorders, depressive affect and diabetes distress in adults with type 2 diabetes. Diabetic Med 2008;25:1096–1101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reaney M, Elash CA, Litcher-Kelly L. Patient reported outcomes (PROs) used in recent phase 3 trials for type 2 diabetes: a review of concepts assessed by these PROs and factors to consider when choosing a PRO for future trials. Diabetes Res Clin Pract 2016;116:54–67 [DOI] [PubMed] [Google Scholar]
- 22.Vieta A, Badia X, Sacristán JA. A systematic review of patient-reported and economic outcomes: value to stakeholders in the decision-making process in patients with type 2 diabetes mellitus. Clin Ther 2011;33:1225–1245 [DOI] [PubMed] [Google Scholar]
- 23.Engström MS, Leksell J, Johansson U-B, Gudbjörnsdottir S. What is important for you? A qualitative interview study of living with diabetes and experiences of diabetes care to establish a basis for a tailored patient-reported outcome measure for the Swedish National Diabetes Register. BMJ Open 2016;6:e010249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vanstone M, Rewegan A, Brundisini F, Dejean D, Giacomini M. Patient perspectives on quality of life with uncontrolled type 1 diabetes mellitus: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser 2015;15:1–29 [PMC free article] [PubMed] [Google Scholar]
- 25.Keely E, Traczyk L, Liddy C. Patients’ perspectives on wait times and the referral-consultation process while attending a tertiary diabetes and endocrinology centre: is econsultation an acceptable option? Can J Diabetes 2015;39:325–329 [DOI] [PubMed] [Google Scholar]
- 26.Joensen LE, Filges T, Willaing I. Patient perspectives on peer support for adults with type 1 diabetes: a need for diabetes-specific social capital. Patient Prefer Adherence 2016;10:1443–1451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Polonsky WH, Fisher L, Hessler D, Bruhn D, Best JH. Patient perspectives on once-weekly medications for diabetes. Diabetes Obes Metab 2011;13:144–149 [DOI] [PubMed] [Google Scholar]
- 28.Sullivan-Bolyai S, Bova C, Johnson K, et al. . Engaging teens and parents in collaborative practice. Diabetes Educ 2014;40:178–190 [DOI] [PubMed] [Google Scholar]
- 29.Nadal JF, Barba EL, Garcia CG, Buil-Cosiales P, Millaruelo JM, Peña MLO. Patient-reported outcomes in type 2 diabetes mellitus: patients’ and primary care physicians’ perspectives in the Spanish health care system. Patient Prefer Adherence 2015;8:1413–1422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goldberg M, Chastang JF, Leclerc A, et al. . Socioeconomic, demographic, occupational, and health factors associated with participation in a long-term epidemiologic survey: a prospective study of the French GAZEL cohort and its target population. Am Journal Epidemiol 2001;154:373–384 [DOI] [PubMed] [Google Scholar]
- 31.Browne JL, Holmes-Truscott E, Ventura AD, et al. . Cohort profiles of the cross-sectional and prospective participant groups in the second Diabetes MILES—Australia (MILES-2) study. BMJ Open 2017;7:e012926. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.