Abstract
Objectives
To identify the success attributions of high-performing Australian general practices and the enablers and barriers they envisage for practices wishing to emulate them.
Design
Qualitative study using semi-structured interviews and content analysis of the data. Responses were recorded, transcribed verbatim and coded according to success characteristics of high-performing clinical microsystems.
Setting
Primary healthcare with the participating general practices representing all Australian states and territories, and representing metropolitan and rural locations.
Participants
Twenty-two general practices identified as high performing via a number of success criteria. The 52 participants were 19 general practitioners, 18 practice managers and 15 practice nurses.
Results
Participants most frequently attributed success to the interdependence of the team members, patient-focused care and leadership of the practice. They most often signalled practice leadership, team interdependence and staff focus as enablers that other organisations would need to emulate their success. They most frequently identified barriers that might be encountered in the form of potential deficits or limitations in practice leadership, staff focus and mesosystem support.
Conclusions
Practice leaders need to empower their teams to take action through providing inclusive leadership that facilitates team interdependence. Mesosystem support for quality improvement in general practice should focus on enabling this leadership and team building, thereby ensuring improvement efforts are converted into effective healthcare provision.
Keywords: primary care, qualitative research, quality in health care, organisational development, human resource management
Strengths and limitations of this study.
The study focused on high-performing general practices identified through objective criteria.
The study included general practitioner, practice manager and practice nurse perspectives.
All practices had participated in the Australian Primary Care Collaboratives Programme, which may restrict the generalisability of the findings.
Introduction
Rising healthcare costs and ageing populations with chronic diseases stretch the resources of health budgets everywhere. Cardiovascular disease, cancers, chronic respiratory diseases and diabetes are the world’s biggest killers causing 14 million deaths annually in people between the ages of 30 and 70 years. WHO member states have agreed to reduce non-communicable diseases by 25% by 2025.1
General practice plays a major role in prevention by promoting smoking cessation, identification and management of risks for diabetes and cardiovascular disease.2 Not surprisingly, governments have made efforts to improve the performance of general practice. Over the last 25 years, we have seen mesolevel Primary Healthcare Organisations (PHOs) developing in Australia, Canada, the Netherlands, New Zealand, the UK and the USA. The purpose of these mesolevel PHOs is to implement governmental health policies locally by supporting general practices. Evidence about their effectiveness in supporting change in general practice is mixed.3–9
Other initiatives have included learning collaborative approaches, which were first tried in the UK primary care and later in Australia, Canada and north-west Europe.10 11 They proved successful but funding was short lived. By comparison with total health expenditure, organisational developmental efforts have been small and mostly directed at providing individual education opportunities even though there is growing recognition that training individuals does not result in improvement unless organisational culture itself also changes.12
The aims of this study were to identify success characteristics in high-performing Australian general practices and to note enablers and barriers that other organisations wishing to achieve similar success should consider. These were categorised according to known success characteristics of high-performing microsystems.13 Clinical microsystems are the smallest clinical unit where patients and their families access care, for example, a general practice. The performance of the mesosystem can be no better than the sum of the performances of the microsystems, its building blocks. The microsystem concept has roots in the work of Deming, Senge and Wheatley, who applied systems thinking to organisational development, leadership and improvement.13 Quinn in 199214 applied the idea of a ‘smallest replicable unit’ (p.13)13 to high-performing service organisations whom he saw successfully organised around and engineered their frontline interface with individual customer needs, opening the way for its application within healthcare.13
The success characteristics of high-performing clinical microsystems were identified in a study of 20 best-quality, best-value small clinical units in North America.13 Work in applying the microsystem concept in North America and in Europe has resulted in a set of tools to drive quality improvement through team and organisational development.15 The success characteristics included leadership, mesosystem support of the microsystems, patient focus, community and market focus, staff focus, education and training, interdependence of the care team, information and information technology, process improvement and performance results. These characteristics formed the basis of our analysis of high-performing Australian general practices.
Methods
The study was designed to elicit individual perspectives on reasons for the success of high-performing practices. We were interested in how these success factors aligned with a pre-existing framework of success characteristics in clinical microsystems.13 The study applied an interpretive theoretical approach. Interpretive studies ‘assume that people create and associate their own subjective and intersubjective meanings as they interact with the world around them’ (p. 5)16 and in this study we accept that this includes both participants and researchers. Ethics approval for the study was obtained from the Flinders University Social and Behavioural Research Ethics Committee.
Study sample and recruitment
Several filters were used to select high-performing general practice clinical microsystems. A national purposive sample of 26 practices was selected using the following: (1) identification of award winners by Australian General Practice Accreditation Limited (AGPAL), a provider of accreditation and quality improvement for general practices. Awards were for safety, innovation, consumer participation and practice of the year. We also sought recommendation from AGPAL staff based on surveyors’ practice accreditation visits or ‘Best within Best’ from AGPAL nominations of high-performing practices over and above the prize winners. AGPAL states ’Practices across Australia continue to implement quality improvements within their practice to improve efficiencies, processes, staff and patient engagement. We share these industry achievements with other practices and stakeholders to recognise, cultivate and maintain a community of quality’.17 (2) Performance in the Australian Primary Care Collaboratives (APCC) supported by recommendations from APCC staff. Entry to the Collaboratives required practices to already have managers, nurses, computer systems and evidence of interest in quality improvement. Hence, our consideration of quality was by virtue of reputation and participation in quality processes.
Twenty-six practices were approached to participate in the staff interviews via email and phone by a medically trained, male postdoctoral fellow with no prior relationship with the practices. Twenty-two of the 26 practices agreed to participate. The interviews were conducted by the postdoctoral fellow (alone), with limited prior experience of the topic; he in turn was supported by three members of the research team steeped in the research and practice of quality improvement in primary care.
Data collection and analysis
The research team developed an interview schedule to focus on four broad areas: the contribution of the APCC on team dynamics and practice nurse roles, characteristics of high-performing general practices and leadership and cultural characteristics associated with high performance (see questionnaire in online supplementary appendix A). Participants were apprised of the aims of the research and gave written informed consent. Semi-structured interviews ranging from 20 to 60 min duration were conducted in a confidential manner at each participating practice by the postdoctoral fellow. Interviews were audio recorded and transcribed verbatim. Field notes were made only sporadically and offered brief impressions of practice environments and interactions. Cognisant of the time demands on participants, interviews were not returned to participants for comment and no repeat interviews were carried out. The time frame of the study meant that the data collection had to be completed before data analysis could progress.
bmjopen-2017-020552supp001.pdf (233KB, pdf)
The approach to content analysis was to use the a priori framework of the research questions as well as to apply a microsystems framework to categorise emergent concepts. The focal question for this study centred on participant perspectives of why their practices might be considered ‘high performing’ and, if time permitted, most participants were also asked about the enablers and barriers that other practices would need to consider if they were to replicate their model:
What are the things that this practice does that has enabled you to achieve this level of performance?
What do you think it would take to replicate what you are doing? What do you think are the key factors to your success —the key lessons for others who would like to replicate what you have done?
What are the major barriers to replicating this elsewhere? What barriers have you overcome?
The first author coded the transcripts using a deductive approach based on the success characteristics of high-performing clinical microsystems.13 QSR International’s NVivo V.11 Software was used to facilitate coding and indexing the data.18
Results
Twenty-two practices participated in the study. The interviewer conducted 52 interviews with 19 general practitioners (GPs), 15 practice nurses and 18 practice managers from April to December 2013. All Australian states and territories were represented in the study (table 1).
Table 1.
Participating general practices
| No. | RRMA* | State | High performance filters | Practice business model† | Participants | Total participants |
||
| GP | PN | PM | ||||||
| 1 | 4 | VIC | APCC, nomination | GP | 1 | 1 | 1 | 3 |
| 2 | 1 | VIC | APCC, award | GP | 1 | 1 | 1 | 3 |
| 3 | 1 | QLD | APCC, high score | GP | 1 | 1 | 0 | 2 |
| 4 | 1 | QLD | APCC nomination | GP | 1 | 1 | 1 | 3 |
| 5 | 1 | QLD | APCC, AGPAL, award, nomination | GP | 1 | 2 | 1 | 4 |
| 6 | 4 | QLD | APCC, AGPAL, award | GP | 1 | 0 | 1 | 2 |
| 7 | 2 | QLD | APCC, AGPAL, award | GP | 1 | 1 | 1 | 3 |
| 8 | 4 | QLD | APCC, AGPAL nomination | GP | 1 | 1 | 1 | 3 |
| 9 | 4 | NSW | APCC, award | GP | 1 | 1 | 1 | 3 |
| 10 | 1 | SA | APCC, AGPAL | GP | 1 | 1 | 1 | 3 |
| 11 | 1 | SA | APCC, AGPAL, award | GP | 0 | 0 | 1 | 1 |
| 12 | 1 | SA | APCC, AGPAL, nomination | GP | 1 | 0 | 1 | 2 |
| 13 | 5 | VIC | APCC, award, nomination | GP | 1 | 1 | 1 | 3 |
| 14 | 5 | TAS | APCC, AGPAL, award, AGPAL nomination | GP | 1 | 1 | 1 | 3 |
| 15 | 1 | NSW | APCC, nomination | GP | 0 | 1 | 1 | 2 |
| 16 | 1 | NSW | APCC, award | CB | 1 | 0 | 0 | 1 |
| 17 | 1 | NSW | APCC, nomination | GP | 1 | 0 | 0 | 1 |
| 18 | 4 | WA | APCC, AGPAL, award | GP | 1 | 1 | 1 | 3 |
| 19 | 1 | WA | APCC, award | GP | 1 | 1 | 1 | 3 |
| 20 | 1 | WA | APCC, AGPAL, award | GP | 1 | 0 | 1 | 2 |
| 21 | 1 | ACT | APCC, nomination | C | 1 | 0 | 0 | 1 |
| 22 | 5 | NT | APCC, AGPAL, award | C | 0 | 0 | 1 | 1 |
| Total | 19 | 15 | 18 | 52 | ||||
*RRMA refers to the Rural, Remote and Metropolitan Areas classification. 1=capital cities, 2=other metropolitan areas, 3=large rural areas, 4=small rural areas, 5=other rural (not including remote).
†Business model refers to practice ownership: corporate (C), community board (CB) or GP owned (GP).
AGPAL, Australian General Practice Accreditation Limited; APCC, Australian Primary Care Collaboratives; GP, general practitioner; PM, practice manager; PN, practice nurse.
Identifying success characteristics
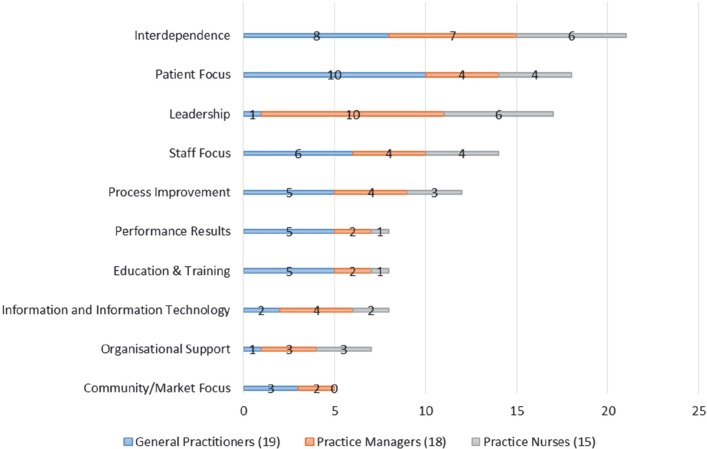
Interview transcripts were coded according to the clinical microsystem success characteristics (see table 2 for representative quotes); (see also online supplementary appendix B for further summaries of responses for each characteristic). Once completed, the attributions coded to each specific microsystem success characteristic were summed and classified according to profession (figure 1).
Table 2.
Clinical microsystems success characteristics and representative verbatim quotes
| Success characteristic13 15 | Representative quote |
| 1. Leadership: the role of leaders is to balance setting and reaching collective goals, and to empower individual autonomy and accountability, through building knowledge, respectful action, reviewing and reflecting. | “I think, my gut feeling is vision. They’ve always cared about the quality of service. They’ve always wanted to do better. They’ve always wanted to improve. They’ve always wanted to explore and see what else is out there and how we can do things differently”. (PM, RRMA 5) |
| 2. Organisational support: the larger organisation looks for ways to support the work of the microsystem and coordinate the hand-offs between microsystems. | “I think, primarily, being involved with the APCC (Australian Primary Care Collaboratives). …Well that’s my impression, because I’ve been involved with it heavily. I think it allowed us to develop the systems you’ve touched on to make things a little more streamlined, a little more efficient… to improve patient care…” (GP, RRMA 4) |
| 3. Staff focus: there is selective hiring of the right kind of people. The orientation process is designed to fully integrate new staff into culture and work roles. Expectations of staff are high regarding performance, continuing education, professional growth and networking. | “You can create a nice environment, nice place … but unless you’ve got the right people, it doesn’t work, yeah”. (GP, RRMA 1) |
| 4. Education and training: all clinical microsystems have responsibility for the ongoing education and training of staff and for aligning roles with training competencies. Academic clinical microsystems have the additional responsibility of training students. | “Also it’s a teaching practice with medical students and nursing students. So, you are constantly teaching people, so you have to always be kind of like on top of best practice and what’s going on to facilitate that, I think”. (PN, RRMA 5) |
| 5. Interdependence: the interaction of staff is characterised by trust, collaboration, willingness to help each other, appreciation of complementary roles, respect and recognition that all contribute individually to a shared purpose. | “I think it’s the team effort… I think everybody’s got jobs and everybody does their jobs, but if you can’t do your own job and you ask for help, it’s given…It’s not just one person, and it’s not just one doctor, and it’s, it’s a whole group of us that want to see out the patient quality of care. And we’ve all got great ideas”. (PN, RRMA 1) |
| 6. Patient focus: the primary concern is to meet all patient needs—caring, listening, educating and responding to special requests, innovating to meet patient needs and smooth service flow. | “I think we’ve always looked at the patient as the whole patient rather than just a quick fix”. (PN, RRMA 4) |
| 7. Community and market focus: the microsystem is a resource for the community; the community is a resource to the microsystem; the microsystem establishes excellent and innovative relationships with the community. | “We have a good community sort of contact. We’re regularly involved in council sort of stuff. Yeah, we donate to council, we donate to the school, breakfast clubs and things like that… we’re pretty good with our community ties. I think that’s one thing that keeps us in good stead with everyone”. (GP, RRMA 4) |
| 8. Performance results: performance focuses on patient outcomes, avoidable costs, streamlining delivery, using data feedback, promoting positive competition and frank discussions about performance. | “We have targets that we all agree on. We get on well; so we talk, and if someone has a problem, we will talk about it usually with our colleagues. We’re comfortable to actually discuss our mistakes. I think it’s important”. (GP, RRMA 4) |
| 9. Process improvement: an atmosphere for learning and design is supported by the continuous monitoring of care, use of benchmarking, frequent tests of change and a staff that has been empowered to innovate. | “Every day there’s something that happens that we think, ‘how can we change that to make it better?’ …as recently as yesterday, you know; we’re always sort of constantly improving”. (PM, RRMA 4) |
| 10. Information and information technology: information is THE connector—staff to patients, staff to staff, needs with actions to meet needs. Technology facilitates effective communication and multiple formal and informal channels are used to keep everyone informed all the time, listen to everyone’s ideas and ensure that everyone is connected on important topics. | With patients: “We use patient-held records and I think that is really valuable. So it, the patient-held record is about the patients knowing what their results are, what their condition is, it’s about having education and it’s also about then having the ability to share the information with the appropriate people outside the practice”. (GP, RRMA 4) Providers and staff: “So, if we recruit new staff, especially GPs, they’re aware of what needs to go into data…. Because everything, all the information (is) in the notes, if someone’s not here, they can just pick it up and look at it and they know. So, they, those kinds of things flow on”. (PM, RRMA 1) Integration of information with technology: “I mean we still use the pen tool… it becomes habit it becomes policy, it just becomes part of the way that we practice… ah and I think now that people are actually starting to see the value of the quality of data”. (PM RRMA 1) |
*Pen Tool is an automated data aggregation program marketed by Pen Computing Systems and provided to GP clinics by mesolevel organisations such as Medicare Locals.
GP, general practitioner; PM, practice manager; PN, practice nurse; RRMA, Rural, Remote and Metropolitan Areas.
Figure 1.
Attributions for success by professional group.
Frequency of attributions for success and differences by professional group
Overall, the most frequently coded success characteristic was interdependence which was referred to in similar proportions by the three professional groups. This was followed closely by patient focus. The least coded success characteristic was community and market focus.
Practice nurses’ attributions of success were equally most frequently coded under leadership and interdependence. Practice managers followed a similar pattern with their explanations coded most frequently under leadership, followed by interdependence. The most frequently coded success characteristic among GPs was patient focus followed by interdependence. The least coded success characteristic for practice nurses was community and market focus, while performance results, community and market focus and education and training featured equally the least for practice managers. The least cited success characteristics for GPs were leadership and organisational support.
‘We are not perfect’
While most participants readily accepted their ‘high-performing’ label, there were a couple of exceptions. The first noted the importance of continuous learning:
I’m going to be honest: we’re not perfect …Some I think are more up to date than others and that’s a reflection of maybe professional development, teaching students, courses, conferences; some will do more than others. (GP, RRMA 4)
Another while dodging the label ‘high-performing’ highlighted the importance of being focused on patient care:
I didn’t know that we were so high performing, let’s put it that way. I guess what we want to do is we want to achieve the maximum of the patient outcomes, you know, patient care. That’s what we’re all there for, you know, all the doctors are there for. We don’t want to be just ticking along and doing a job and going home. (GP RRMA 5)
Identifying enablers and barriers
Of the 52 participants, 41 individuals representing 18 practices were asked questions about barriers and enablers that might impact on other practices wishing to emulate their success. Enablers and barriers were coded under the clinical microsystems success characteristics (see table 3 for representative quotes). Barriers were couched in terms of deficits in, or limitations of the success characteristics. Further summaries of the responses can be found in online supplementary appendix C.
Table 3.
Identified enablers and barriers coded according to clinical microsystems success characteristics and representative verbatim quotes
| Success characteristics13 15 | Representative quotes | |
| Enablers | Barriers | |
| 1. Leadership: the role of leaders is to balance setting and reaching collective goals, and to empower individual autonomy and accountability, through building knowledge, respectful action, reviewing and reflecting. | “You do have to have, as an absolute minimum, you have to have one person who has both the vision and the position to be able to make things change. Ok"? (GP, RRMA 5) | “…having some degree of buy in from the partners I think was crucial, and times when there wasn’t that buy in nothing moved”. (GP, RRMA 1) |
| 2. Organisational support: the larger organisation looks for ways to support the work of the microsystem and coordinate the hand-offs between microsystems. | “I think being involved in more than one wave of the APCC is terrific, because one wave [Interviewer: So your comment is not one wave, go further…]…Yeah I love it, I miss it and I always learn an enormous amount…. Even being part of their, you know, communication…. There’s email communication between practices… so hopefully they’ll keep getting funding and keep doing different ideas”. (GP, RRMA 1) | “You know a lot of doctors are a bit suspicious, thinking, even they think the APCC is a government plan to get to know their numbers… and I was amazed when I spoke and I heard this, you know, they were really suspicious. So, I think that’s one barrier they have got to get through”. (GP, RRMA 1) |
| 3. Staff focus: there is selective hiring of the right kind of people. The orientation process is designed to fully integrate new staff into culture and work roles. Expectations of staff are high regarding performance, continuing education, professional growth and networking. | “Making sure that all the staff are trained in what is expected of them: understand their role; understand their limitations, understand the reporting procedures; have an open door policy; … and make sure people, make sure staff aren’t frightened to say something, because …they’re frightened that they’ll get a negative response whatever: an open door policy”. (PM, RRMA 2) | “The practice will pay for certain professional development things. Whereas I know some general practices don’t have that…that whoever’s the boss doesn’t want to pay for anything”. (PN, RRMA 1) |
| 4. Education and training: all clinical microsystems have responsibility for the ongoing education and training of staff and for aligning roles with training competencies. Academic clinical microsystems have the additional responsibility of training students. | “I would say, what general practice is doing at a training level, in terms of interns and medical students and registrars. That… starting with that cohort, you can actually influence how they will end up practicing as GPs and that might be something that you start back at this level that it actually flows through over a period of time”. (PM, RRMA 4) | “I think there’s an ongoing pressure from external organisations to keep providing services, because they’re short of examiners, short of teachers, short of people to run intern placements, and so there’s a continuous drive to keep us doing those, those external activities. And it comes down in the end to the doctors making a lifestyle choice, and how much time they want to prioritise their general practice and their other interests”. (GP, RRMA 1) |
| 5. Interdependence: the interaction of staff is characterised by trust, collaboration, willingness to help each other, appreciation of complementary roles, respect and recognition that all contribute individually to a shared purpose. | “Culture… is hard to replicate. I think we have a good culture. I think people are engaged; they’re happy. And it’s not all perfect, don’t get me wrong, you know, you do have issues, but I think people genuinely feel that they make a difference and they are allowed to make a difference, and they have input. So, something all our staff have is input, come up with an idea, we’ll look at it”. (PM, RRMA 5) | “My experience from going out to conferences and networking with other nurses in other practices is that the nurses don’t have a lot of freedom from the doctors. The doctors like to have a very tight rein on what’s going on in their practice and the nurses nearly of just do those clinical tasks of supporting the doctor, you know? … And don’t really get to use their skills that they have”. (PN, RRMA 5) |
| 6. Patient focus: the primary concern is to meet all patient needs—caring, listening, educating and responding to special requests, innovating to meet patient needs and smooth service flow. | “When I set the practice up, I had certain aims: one was to have a high quality practice. One where I and my staff liked to work and one where my patients felt comfortable to come and felt better when they left than when they arrived. So, you know, if you’re going to sit in a stinking waiting room and everyone’s loud and noisy, you leave the surgery feeling worse than when you arrived”. (GP, RRMA 4) | “I think that the (macro)system is designed to reward individual, quick medicine, ah dealing with a small number of problems, and … doesn’t support good team based chronic disease management; a lot of the stuff that our nurses do…there’s no item number for that. It frees up our time and it gives better care to our patients, but it’s not financially rewarding”. (GP, RRMA 4) |
| 7. Community and market focus: the microsystem is a resource for the community; the community is a resource to the microsystem; the microsystem establishes excellent and innovative relationships with the community. | “We have a particular stable patient base, if you like, we know our patients very well… we work as a family and the community is very much a community and the doctors have values about looking after that community…” (PM, RRMA 4) | “Doctors…are not in it to make money necessarily; they are in it to care for the community. So, there’s a different approach to the whole billing side of things…that may not work for some practices”. (PM, RRMA 4) |
| 8. Performance results: performance focuses on patient outcomes, avoidable costs, streamlining delivery, using data feedback, promoting positive competition and frank discussions about performance. | “You have to be obsessive and say ‘I have to do this…’ ‘we’re trying to get HbA1c better’, ‘we want to get the blood pressure better’…. And so, constantly chasing the target”. (GP, RRMA 1) | ‘I think once all the systems are set up, it’s all easy…It’s just having the time to set them up”. (PM, RRMA 1) |
| 9. Process improvement: an atmosphere for learning and design is supported by the continuous monitoring of care, use of benchmarking, frequent tests of change and a staff that has been empowered to innovate. | “Even any little improvement is good, you know, so I think that’s how to start practice off, … small changes monthly are, are really good”. (GP, RRMA 1) | “If you try to do five things, they’ll all flop, and when they all flop people are disenchanted and then you’re trying to and they say, ‘oh but we tried that last time’”. (PM, RRMA 1) |
| 10. Information and information technology: information is THE connector—staff to patients, staff to staff, needs with actions to meet needs. Technology facilitates effective communication and multiple formal and informal channels are used to keep everyone informed all the time, listen to everyone’s ideas and ensure that everyone is connected on important topics. | “We now get information on the percentage of medications printed in the last 6 months. You know, the number of diagnoses, even though our patient load is going up we’re trying to get the number of diagnoses down. So everything there is relevant, and we’ve also marked everything there as confidential, so that when we do upload an electronic health history, only relevant stuff, is there”. (GP, RRMA 1) | “…With the e-health, it does take a lot of time. Even the registration, we found that, you know quite difficult and to get to the state of uploading histories is time consuming: getting rid of old diagnoses; making sure medications are in date, we’ve done a lot of work on that, you know, making sure their over-the-counter medicine is up to date”. (GP, RRMA 1) |
GP, general practitioner; PM, practice manager; PN, practice nurse; RRMA, Rural, Remote and Metropolitan Areas.
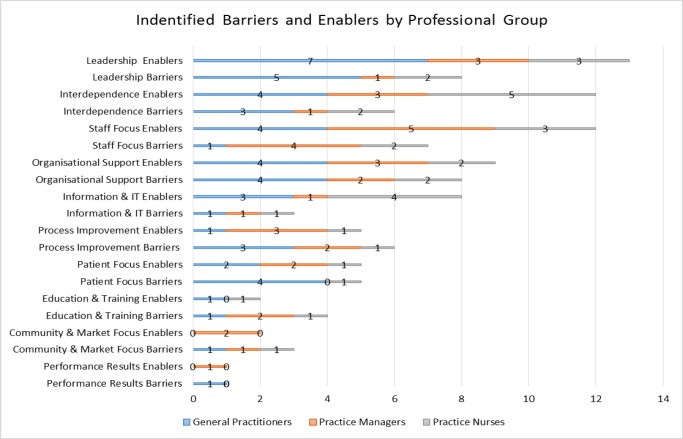
Enabler responses were most frequently coded under leadership, interdependence and staff focus; the least frequently coded were performance results, community and market focus and education and training (figure 2). GP nominated enablers were most frequently coded under leadership (in contrast to their attributions for success); practice managers’ enablers were most frequently coded under staff focus, while for practice nurses, interdependence was most frequently coded.
Figure 2.
Identified enablers and barriers by professional group.
The barriers identified by participants were most frequently coded under leadership and organisational support, followed by staff focus, with performance results, education and training and community and market focus mentioned least (figure 2). Leadership was again the most frequently coded characteristic for GPs; for practice manager responses, staff focus was the most frequently used code; barriers identified by practice nurses were equally most frequently coded under leadership, organisational support, staff focus and interdependence.
Discussion
When asked what made them a high-performing practice, participants most frequently articulated ideas that were strongly related to interdependence, patient focus and leadership (followed by staff focus). Nominated enablers were also attributed most frequently to leadership, followed by interdependence and staff focus. While the focus on these human characteristics might demonstrate social desirability bias (the desire to answer in a way that would be perceived favourably) and self-serving bias (aiming to maintain and enhance self-esteem) by highlighting participants’ own role in accomplishing success, the significant role that each plays in ensuring continuous improvement needs to be recognised. The honesty and trust demonstrated in references to the importance of interdependence have helped to create cultures of learning and improvement where they can collectively improve things and where hierarchical boundaries need not apply so widely.19 20 Inclusive teams require the inclusive leadership described by Nembhard and Edmondson21:
Our research suggest leader inclusiveness—words and deeds by leaders that invite and approve others’ contributions—can take nature off its course, helping them to overcome status’ inhibiting effects on psychological safety…. We thus suggest that active, inclusive behaviour on the part of physician leaders may be an essential means of facilitating others’ meaningful engagement in team-based quality improvement work. (p. 958)
Leadership holds a prominent place in our collective consciousness and has been recognised as a way in which we understand and make sense of organisations.22 Gerstner and Day describe an employee’s relationship with their leader, supervisor or boss as ‘a lens through which the entire work experience is viewed’ (p. 840).23 Those who were not positioned as overall practice leaders (most practice managers and practice nurses), were much more likely to provide reasons for success that could be coded to leadership. Leadership may be a salient success characteristic for practice managers in particular as they depend on the support of the practice leadership to initiate organisational change. GPs may have omitted to mention this success factor because they assume it, or are reticent to ‘talk themselves up’. GPs most frequently nominated leadership as an enabler demonstrating that they do not underestimate its importance, while they most frequently attributed success to having a patient focus. This patient focus may also be communicated in other ways including as a vision to inspire their teams to high performance, a characteristic indicative of effective leadership styles such as transformational leadership.24 25 At the same time, the leader-consciousness of team members other than GPs is a reminder of the need for practice leaders to demonstrate and set the tone for inclusiveness.
While we do emphasise the importance of leadership in this section, all team members in effect, contribute to success and this is underlined by attributions made by all roles to ‘interdependence’. We also acknowledge that leadership was referred to in terms of the GP role and attributed to other staff who headed up various teams within the practice, for example, practice nurses. Healthcare transformation is said to emerge from the persistent accumulation of small gains made at the microsystem level, the result of internal design work carried out by a multidisciplinary team.26 Those teams need to be empowered to lead change efforts, to create shared norms and values aligned with organisational goals and to incorporate routinised processes of change that involve a shared vocabulary and understanding.26 As Bohmer notes ‘in effect, instead of taking their work context as a given, staff actively create the local system needed to provide the best possible care’ (p. 711).26
Practice leaders could also note that while participants often acknowledged barriers to success in terms of the cost and time involved in various initiatives, they also tended to frame these costs as a necessary ‘investment’ in order to achieve long-term returns. Examples included educating medical staff for future roles as GPs and investments of time or finance made across a number of practice areas. This tendency might illustrate the optimism and ‘calculated risk taking’ that are said to comprise resilience, a noted habit of ‘improvers’.27 This mindset may be a key enabler for those wishing to model themselves on these high-performing practices.
The participating general practice teams show innovation, creativity, motivation and high morale, but they would be the first to say that there is room for improvement. Our study suggests that consideration of community and market focus may be least in the minds of even high-performing practices. There was some frustration expressed about the lack of mesolevel support for community outreach initiatives. Information technology was also cited infrequently as a reason for success, although cited moderately frequently as an enabler. There is frustration with the performance of information technology in Australian general practice which while solving some problems, is also seen to generate others28 and there is a perception of low levels of support for this area from mesoorganisations.29 Perhaps then it is no surprise that organisational (or mesosystem) support was the second least coded reason for success. Indeed, support was not attributed to the mesoorganisation but to APCC and AGPAL. The support offered by the APCC in the form of training and development, and support for improvement and innovation was mentioned frequently as an enabler. While acknowledged as a significant resource, participants also identified perceived and real barriers to participation in this programme for other practices. Unfortunately, the most significant barrier is that funding for the APCC has been discontinued since the time when the interviews were conducted, leaving a gap in the system which needs to be filled especially as APCC was so valued by practices. The lack of mesosystem support was also illustrated in terms of time and cost barriers identified for many of the ‘success characteristics’. While many of the participants were committed to investment of both resources with a view to long-term positive outcomes, these still pose very real obstacles and may indicate ‘outmoded theories of control’.3 Alternative strategies may be called for. In response to the burden from chronic disease, a number of countries including Australia, Canada, New Zealand and the USA are moving towards patient-centred medical homes also known as healthcare homes.30 A similar Dutch development has been made through bundled payments.9 One US study found that many practices were not yet ready to perform as patient-centred medical homes31 and the situation may not be any better in other countries. A look to alternative models might address unsatisfactory mesosystem support, something that is considered a weak link in delivery of high-performing primary care.32
The findings of this study acknowledge that while more satisfactory mesosystem support to facilitate improved performance is desirable, it is not enough; these strategies do not guarantee operational change at the microsystem level; it is the structures and processes at practice level that ultimately govern delivery of care.26 The success characteristics of high-performing microsystems provide a template for guiding general practices towards structures and processes that are likely to result in effective provision of care. General practices can assess themselves using the Microsystem Assessment Tool and set their own priorities for development.15 Mesoorganisations should consider internal training to better facilitate practices in line with microsystem success characteristics. One such training programme is the Dartmouth Clinical Microsystem Curriculum.13
All our high-performing practices had been part of the APCC programme, limiting the generalisability of our findings. The interviewer may have been subject to an observer-expectancy effect that may have resulted in subconsciously prompting participant responses of particular success characteristics, even though participants were not given access to the microsystem success characteristics when giving their responses. A single coder analysed the data and the decision to take a deductive approach may evoke a confirmation bias, whereby interview text was possibly coded incorrectly in order to confirm the expected validity of the clinical microsystems success characteristics. While the responses given by participants were categorised according to the clinical microsystems success characteristics, other salient characteristics may exist, for example, some of the demographic factors outlined in table 1. Context is important in health systems. Answers given by these Australian practices may vary from the views in other countries, especially in relation to the performance of mesolevel organisations and IT.
We acknowledge that the attributions of these high-performing practices are still subjective explanations. As mentioned previously, the tendency to nominate human characteristics as the reasons for success may be due to social desirability and self-serving bias. Other parts of the interview used in this study consistently yielded information about improvements or innovations practices had made that seem to support the external recognition given to them, and these accounts are planned for a later publication. These included, for example, finding new ways to serve the needs of their community to greater efficiencies in handling information and to giving all practice personnel a voice in decision making. In addition, while the attributions made would seem to indicate likely contributions to success, if we were to also include poor performing practices in our study we might find that they too report some of the same characteristics that high-performing practices do, while their weaker performance on other characteristics impinge on their overall performance. As in the case of the participating practices, poor performing practices will not be strong in all of the success characteristics. It may be that the areas they are weak in (eg, leadership) undermine the strengths they do have. Furthermore, there may be other characteristics that can be attributed for the success of these practices that were not known or articulated by participants in the study. Finally, while we have tried to provide an external benchmark of high-performing general practices through the criteria described earlier in this paper, we acknowledge that there are other definitions of high performance that might lead to other general practices being included in such a study. For example, a patient and consumer group’s view of what constitutes high performance in general practice is an obvious consideration for future research.
The study’s results suggests that human dynamics remain at the forefront of our thinking in change management initiatives with learning and development approaches that harness these dynamics effectively as paramount. The key ingredients for success are a clinical microsystem consisting of inclusive leadership and an interdependent team who are committed to ‘improvement and innovation’ and who are empowered to accomplish just that.
Supplementary Material
Acknowledgments
The authors acknowledge AGPAL and the APCCP for their assistance in recruiting participants and the general practices that participated in this study.
Footnotes
Contributors: Study conceived by JAD, JKJ, JF, MM and DF who also developed the interview questions. AHD analysed the data. AHD and JAD drafted the manuscript. AHD, JAD, JKJ, JF, MM and DF all commented on the manuscript.
Funding: The research reported in this article was funded by a grant from the Australian Government Department of Health.
Disclaimer: The information and opinions contained in it do not necessarily reflect the views or policy of the Australian Primary Health Care Research Institute (APHCRI), the Australian Government or the Department of Health.
Competing interests: None declared.
Patient consent: Not required.
Ethics approval: Flinders University Social and Behaviour Ethics Committee (Project No. 5609).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Supplementary data consisting of appendices will be made available.
References
- 1. World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013- 2020. Geneva: World Health Organization, 2013. [Google Scholar]
- 2. Macinko J, Starfield B, Shi L. The contribution of primary care systems to health outcomes within Organization for Economic Cooperation and Development (OECD) countries, 1970-1998. Health Serv Res 2003;38:831–65. 10.1111/1475-6773.00149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Berwick DM. Improvement, trust, and the healthcare workforce. Qual Saf Health Care 2003;12(Suppl 1):448–52. 10.1136/qhc.12.6.448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gauld R, Mays N. Are New Zealand’s new primary health organisations fit for purpose? BMJ 2006;333:1216–8. 10.1136/bmj.39029.493542.94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dunbar JA. When big isn’t beautiful: lessons from England and Scotland on primary health care organisations. Med J Aust 2011;195:219–21. [DOI] [PubMed] [Google Scholar]
- 6. Naylor C, Curry N, Holder H, et al. . Supporting improvement in general practice? London: the King’s fund, 2013. [Google Scholar]
- 7. Sorrell BR, Rosen R, Smith J. GP commissioning: insights from the medical groups in the United States. London: Nuffield Trust, 2011. [Google Scholar]
- 8. Abou Elnour A, Dunbar J, Ford D, et al. . General practices' perspectives on medicare locals' performance are critical lessons for the success of primary health networks. Australas Med J 2015;8:320–4. 10.4066/AMJ.2015.2508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Struijs JN, Baan CA. Integrating care through bundled payments--lessons from The Netherlands. N Engl J Med 2011;364:990–1. 10.1056/NEJMp1011849 [DOI] [PubMed] [Google Scholar]
- 10. Oldham J. Sic Evenit ratio ut componitur: the small book about large system change. Chichester: Kingsham Press, 2004. [Google Scholar]
- 11. Knight AW, Caesar C, Ford D, et al. . Improving primary care in Australia through the Australian primary care collaboratives program: a quality improvement report. BMJ Qual Saf 2012;21:948–55. 10.1136/bmjqs-2011-000165 [DOI] [PubMed] [Google Scholar]
- 12. Dunbar JA, Reddy P, McAvoy B, et al. . The contribution of approaches to organisational change in optimising the primary health care workforce. Canberra: Australian Primary Health Care Research Institute, 2007. [Google Scholar]
- 13. Nelson EC, Batalden PB, Huber TP, et al. . Success characteristics of high performing microsystems: learning from the best : Nelson EC, Batalden PB, Godfrey MM, Quality by design: a clinical microsystems approach. San Francisco: Jossey Bass, 2007. [Google Scholar]
- 14. Quinn JB. Intelligent enterprise: A knowledge and service based paradigm for industry. New York: Free Press, 1992. [Google Scholar]
- 15. Johnson JK. Clinical microsystem assessment tool. Microsystem academy. 2003. http://clinicalmicrosystem.org/wp-content/uploads/2014/07/microsystem_assessment.pdf (accessed Jan 2018).
- 16. Orlikowski WJ, Baroudi JJ. Studying information technology in organizations: research approaches and assumptions. Inf Syst Res 1991;2:1–28. 10.1287/isre.2.1.1 [DOI] [Google Scholar]
- 17. AGPAL. Celebrating practice achievements. https://www.agpal.com.au/practice-accreditation/ (accessed Jan 2018).
- 18. QSR International Pty Ltd. NVivo qualitative data analysis software. Version 11, 2015. [Google Scholar]
- 19. Edmondson AC, Dillon JR, Roloff KS. Three perspectives on team learning. Acad Manag Ann 2007;1:269–314. 10.1080/078559811 [DOI] [Google Scholar]
- 20. Schein EH, Schein P. Organisational culture and leadership. 5th edn Hoboken, NJ: Wiley, 2017. [Google Scholar]
- 21. Nembhard IM, Edmondson AC. Making it safe: the effects of leader inclusiveness and professional status on psychological safety and improvement efforts in health care teams. J Organ Behav 2006;27:941–66. 10.1002/job.413 [DOI] [Google Scholar]
- 22. Meindl JR, Ehrlich SB, Dukerich JM. The romance of leadership. Adm Sci Q 1985;30:78–102. 10.2307/2392813 [DOI] [Google Scholar]
- 23. Gerstner CR, Day DV. Meta-analytic review of leader–member exchange theory: correlates and construct issues. J Appl Psychol 1997;82:827–44. 10.1037/0021-9010.82.6.827 [DOI] [Google Scholar]
- 24. Avolio BJ. Full leadership development: Building the vital forces in organizations. Thousand Oaks, CA: Sage, 1999. [Google Scholar]
- 25. Bass BM, Avolio BJ. The implications of transactional and transformational leadership for individual, team, and organizational development. ROCD 1990;4:231–72. [Google Scholar]
- 26. Bohmer RM. The hard work of health care transformation. N Engl J Med 2016;375:709–11. 10.1056/NEJMp1606458 [DOI] [PubMed] [Google Scholar]
- 27. Lucas B, Nacer H. The habits of an improver: thinking about learning for improvement in healthcare. London: Health Foundation, 2015. [Google Scholar]
- 28. Henderson J, Miller G, Britt H, et al. ; The effect of computerisation on the quality of care in Australian general practice. Final report to the royal Australian college of general practitioners. Sydney: University of Sydney, 2007. [Google Scholar]
- 29. Ghosh A, McCarthy S, Halcomb E. Perceptions of primary care staff on a regional data quality intervention in Australian general practice: a qualitative study. BMC Fam Pract 2016;17:50 10.1186/s12875-016-0445-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Janamian T, Jackson CL, Glasson N, et al. . A systematic review of the challenges to implementation of the patient-centred medical home: lessons for Australia. Med J Aust 2014;201(3 Suppl):69–73. 10.5694/mja14.00295 [DOI] [PubMed] [Google Scholar]
- 31. Hollingsworth JM, Saint S, Sakshaug JW, et al. . Physician practices and readiness for medical home reforms: policy, pitfalls, and possibilities. Health Serv Res 2012;47(1 Pt 2):n/a–508. 10.1111/j.1475-6773.2011.01332.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rosen R, Kumpunen S, Curry N, et al. . Is bigger better? Lessons for large-scale general practice. Research report: Nuffield Trust, 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-020552supp001.pdf (233KB, pdf)