Abstract
OBJECTIVES
Pre-procedural CT angiography (CTA) assists in evaluating vascular morphology, disease distribution and treatment planning in patients with lower extremity peripheral artery disease (PAD). The aim of the study was to determine the predictive value of radiographic findings on CTA and technical success of endovascular revascularization of occlusions in the superficial femoral-popliteal (SFA-pop) region.
METHODS
Medical records and available imaging studies were reviewed for patients undergoing endovascular intervention for PAD between January 2013 and December 2015 at a single academic institution. Radiologists reviewed pre-operative CTAs of patients with occlusions in the SFA-pop region. Radiographic criteria previously used to evaluate chronic occlusions in the coronary arteries were used. Technical success, defined as restoration of inline flow through the SFA-pop region with < 30% stenosis at the end of the procedure, and intra-operative details were evaluated.
RESULTS
From 2013–2015, 407 patients underwent 540 endovascular procedures for PAD. Pre-procedural CTAs were performed in 217 patients (53.3%), and 84 occlusions in the SFA-pop region were diagnosed. Ten occlusions were excluded as no endovascular attempt to cross the lesion was made due to extensive disease or concomitant iliac intervention. Of the remaining 74 occlusions in the SFA-pop region, 59 were successfully treated (80%), 15 unsuccessfully crossed (20%). The indications for revascularization were claudication in 57% of patients with the remaining for critical limb ischemia. Tasc A, B and C occlusions were treated with 87% success while Tasc D occlusions were treated with 68% success, P=.047. There were 9 occlusions with 100% vessel calcification which was associated with technical failure (P=.014). Longer lengths of occlusion were also associated with technical failure (P=.042). Multiple occlusions (P=.55), negative remodeling (P=.69), vessel runoff (P=.56), and percentage of vessel calcification (P=.059) were not associated with failure. On multivariable analysis 100% calcification remained the only significant predictor of technical failure (OR 9.0, 95% CI 1.8–45.8, P=.008).
CONCLUSIONS
Analysis of pre-operative CTAs shows 100% of calcification as the best predictor of technical failure of endovascular revascularization of occlusions in the SFA-pop region. Further studies are needed to determine the cost effectiveness of obtaining pre-operative CTA for lower extremity PAD.
Introduction
Recent improvements in computed tomography angiography (CTA) have increased image quality and decreased acquisition time1–3. As the distribution of disease is often found in multiple arteries, CTA can evaluate peripheral artery disease (PAD) from the abdomen to the feet in a single study. Disease burden can be assessed according to lesion length, location, and vascular morphology.1 This information allows the operator to plan for intervention with regard to patient positioning, access site(s), and treatment approach.4 Studies regarding the clinical utility of CTA prior to endovascular intervention are limited; in current practice physical exam, duplex ultrasound (DUS) and overall clinical judgement generally determine the need for additional imaging prior to intervention.5–6
This study sought to evaluate whether pre-operative CTAs are predictive of endovascular technical success in treating occlusions in the superficial femoral and popliteal arteries (SFA-pop). Previous work regarding chronic occlusions (CTO) in the coronary arteries evaluated coronary CT findings and the ability to predict lesion crossing difficulty based pre-operative radiographic findings.7,8 We evaluated the radiographic characteristics of occlusions in the SFA-pop region with regards to endovascular treatment outcomes.
Methods
This retrospective observational study at a single academic institution evaluated lower extremity CTA prior to endovascular intervention. This study was performed after obtaining approval from our institution's IRB. Patient consent was waived given the retrospective nature of the study. Between January 2013 and December 2015 a review of medical records and available imaging studies was performed for patients undergoing endovascular intervention for PAD. Patient demographics, prior interventions, pre-operative CTA scans, intra-operative details and imaging, as well as follow-up records were collected and analyzed.
Pre-operative CTA evaluation
We collected all records for patients undergoing endovascular intervention for PAD during the study period. Interventions for acute limb ischemia were excluded. Patients were included if a CTA was performed within 13 months of intervention and was available for radiographic review. Intra-operative angiograms were then evaluated to see if the intervention included an occlusive lesion in the SFA-pop region, defined as absence of contrast through part or entire length of the vessel. The corresponding CTAs were then reviewed by radiologists. Patients without an occlusion in the SFA-pop region on intra-operative angiogram were excluded from further analysis.
CTA methodology
Radiographic records were queried to determine if pre-operative CTA scans were performed at the study institution. Timing of CTA scans prior to endovascular intervention were noted. Radiation exposure in the form of milliGray (mGy) as well as iodinated contrast volumes were noted. At the study institution, it is routine to perform CTA of the abdomen with runoff from just above the celiac artery to the feet. Initial non-contrast 3 mm axial images are acquired through the abdomen and pelvis. A bolus contrast injection followed by a saline flush is administered through a peripheral IV and contiguous axial images are acquired through the abdomen and pelvis with bilateral lower extremity runoff during the systemic arterial phase at 1 mm and 5 mm slice thicknesses. Maximum intensity projection, curved planer, and 3-D reformations are performed at an independent workstation.
CTA evaluation
A cardiovascular radiologist reviewed all pre-operative CTA scans with occlusions in the SFA-pop region and findings were confirmed by a second cardiovascular radiologist. Scans were blinded to the results of endovascular technical success to treat the occlusive lesion in the SFA-pop region. Radiographic findings previously described to characterize chronic occlusions (CTOs) in the coronary arteries were adapted for evaluation of the occlusions in the SFA-pop region.7,8 Trans-Atlantic Score (TASC) II scores6, lesion length, negative remodeling, percentage of vessel calcification, multiple occlusions and tibial vessel runoff were noted during the evaluation. Negative remodeling was noted as the ratio of the minimum diameter in the occlusive lesion divided by the adjacent patent normal vessel (i.e. without lumen compromise) diameter. Percentage of vessel calcification notes the highest percentage of calcium occupying the cross-sectional area of the occluded vessel segment. The length of multiple occlusions was the additive lengths of occluded vessel segments.
Intra-operative outcomes
Our primary outcome was technical success in crossing the occlusion with restoring inline flow and <30% of residual stenosis on angiography at the end of the procedure. Patients for which no attempt to cross the lesion were excluded from analysis of this outcome. We also collected the total procedure time, fluoroscopy time, radiation exposure in the form of mGy, and contrast volume used during each endovascular procedure. If a concomitant common femoral endarterectomy or iliac intervention was performed this was also recorded. The use of re-entry devices, non-catheter based crossing devices, as well as distal retrograde access was also evaluated.
Short-term procedural patency
Primary and cumulative patencies were investigated in patients who underwent successful endovascular intervention for occlusions in the SFA-pop region. We defined primary patency as freedom from follow-up DUS findings of peak systolic velocity ratio ≥ 2.5 or lack of flow.9 Cumulative patency is noted as either primary patency or patency after a secondary intervention performed to preserve or restore inline flow through the SFA-pop region.
Statistical analysis
Independent variables between groups were evaluated with t-test or Wilcoxon rank-sum for continuous variables and Chi-squared or Fisher exact tests for categorical variables. Variables associated with differences in successful crossing of the occlusion by univariate analysis were included in a multivariate analysis to determine factors independently associated with successful lesion crossing. Statistical analysis was performed using Stata version 14 (College Station, TX). P-values <.05 were considered significant.
Results
During the study period, 407 patients underwent 540 endovascular procedures for lower extremity PAD. Pre-operative CTAs were performed in 217 patients (53.6%), and of these 84 of these found occlusions in the SFA-pop region that were available for review. Of these 84 occlusions, 10 were not attempted to be treated endovascularly due to extensive disease or concomitant iliac intervention. Characteristics of these patients are noted in Supplemental Table 1. The remaining 74 occlusions were attempted to be treated in 66 patients who define the study population. Fifty-nine of the 74 occlusions were successfully crossed and treated (80%), see Figure 1.
Figure 1.
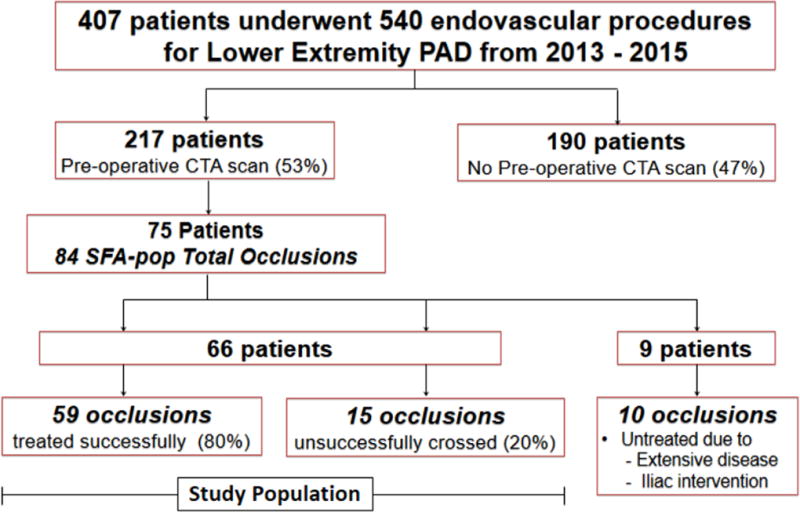
Study population of patients undergoing endovascular interventions with and without pre-operative CTAs
Demographics for the patients who underwent an attempted crossing for 74 SFA-pop occlusions are noted in Table 1. The average age of treated patients was 67.1 years and 65% were male. No statistical difference was found regarding co-morbidities, prior interventions, or indications for procedure for patients with successful or unsuccessful endovascular intervention. Pre-operative CTA scans were performed at median of 1.2 months (IQR 0.3–3.1) prior to intervention with 46% performed within 1 month and 71% performed within 3 months. Sixty-four percent of the CTA scans were performed at the study institution with the remaining scans performed at outside institutions. Pre-operative CTA scans used a median of 145 cc of iodinated contrast (IQR 125–150). The median radiation exposure was 41.6 mGy (IQR 26.1–71.4).
Table 1.
Patient Demographics
| Total n= 74 | Successful n=59 | Unsuccessful = 15 | P-value | |
|---|---|---|---|---|
| Age (σ) | 67.1 (11.2) | 67.4 (11.0) | 65.9 (12.4) | .45 |
| Male Gender | 48 (65) | 37 (63) | 11 (73) | .55 |
| Never smoker | 18 (24) | 16 (27) | 2 (13) | .33 |
| HTN | 63 (85) | 49 (83) | 14 (93) | .44 |
| HLD | 46 (62) | 35 (59) | 11 (73) | .38 |
| DM | 32 (43) | 26 (44) | 6 (40) | 1.0 |
| CAD | 37 (50) | 29 (49) | 8 (53) | 1.0 |
| CKD | 6 (8) | 6 (10) | 0 (0) | .34 |
| ESRD | 8 (11) | 5 (8) | 3 (20) | .35 |
| CHF | 15 (20) | 10 (17) | 5 (33) | .17 |
| COPD | 6 (8) | 5 (8) | 1 (7) | 1.0 |
| CVA | 12 (16) | 9 (15) | 3 (20) | .70 |
| Prior Intervention | ||||
| Endovascular | 11 (15) | 8 (14) | 3 (20) | .68 |
| Open | 3 (4) | 2 (3) | 1 (7) | .50 |
| Indication | ||||
| Claudication | 42 (57) | 32 (54) | 10 (67) | .81 |
| Rest Pain | 6 (8) | 5 (8) | 1(7) | |
| Wound | 26 (35) | 22 (37) | 4 (27) |
HTN - Hypertension, HLD - Hyperlipidemia, DM - Diabetes Mellitus, CAD - Coronary Artery Disease, CKD - Chronic Kidney Disease, ESRD - End Stage Renal Disease, CHF - Congestive Heart Failure, COPD - Chronic Obstructive Pulmonary Disease, CVA - Cerebral Vascular Accident
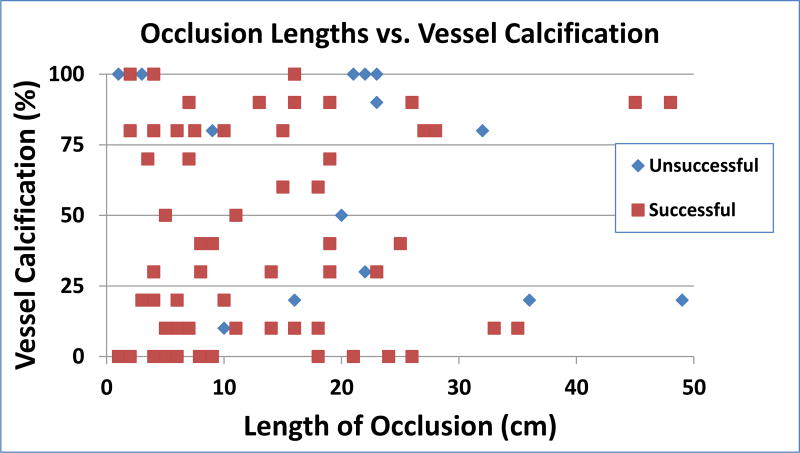
The characteristics of the SFA-pop occlusions are reported in Table 2. There were 5 TASC A occlusions and 14 TASC B occlusions that were treated with 100% success rate. There were 27 TASC C occlusions; 21 of which were treated successfully (78%). Of the 28 TASC D occlusions 19 were treated successfully (68%). Overall technical success for TASC A, B, and C occlusions was 87% compared to 66% for TASC D occlusions, P=.047. Longer length of occlusion (P=.024) was associated with technical failure by univariate analysis. Increased circumferential calcification of the occluded vessel (P=.059) did not reach statistical significance; however, 100% circumferential vessel calcification was associated with technical failure, (P=.014). Representative findings of 100% calcification of SFA-pop occlusions are shown in Figure 2. Multiple occlusions (P=.55), negative remodeling (P=.69), and vessel runoff (P=.56) were not associated with technical failure. Technical success with regard to length of lesion and vessel calcification is shown in Figure 3.
Table 2.
Radiographic Characteristics from Pre-operative CTAs of Successful vs Unsuccessful Endovascular Intervention in SFA-pop occlusions
| Total (n = 74) |
Successful (n=59) |
Unsuccessful (n =15) |
P – value | |
|---|---|---|---|---|
| TASC | ||||
| A/B/C (%) | 46 (62) | 40 (87) | 6 (13) | .047 |
| D (%) | 28 (38) | 19 (68) | 9 (32) | |
| Total length of occlusion - cm (IQR) | 14 (6–21) | 11 (6–19) | 21 (13–23) | .042 |
| Multiple occlusion (%) | 27 (36) | 23 (39) | 4 (27) | .55 |
| Negative remodeling* (IQR) | .80 (.60–.80) | .80 (.60–80) | .80 (.60–.95) | .69 |
| Percentage of vessel calcification - (IQR) | 40 (10–80) | 40 (10–80) | 80 (20–100) | .059 |
| 100% Vessel calcification (%) | 9 (12) | 4 (7) | 5 (33) | .014 |
| Tibial vessel runoff (σ) | 2.3 (.7) | 2.3 (0.8) | 2.5 (0.6) | .56 |
| Location of occlusion | ||||
| SFA (%) | 61 (82) | 49 (83) | 12 (80) | .72 |
| Pop (%) | 42 (57) | 31 (53) | 11 (69) | .24 |
| Both (%) | 29 (39) | 21 (36) | 8 (53) | .25 |
Negative remodeling - minimum diameter in lesion/ normal vessel diameter
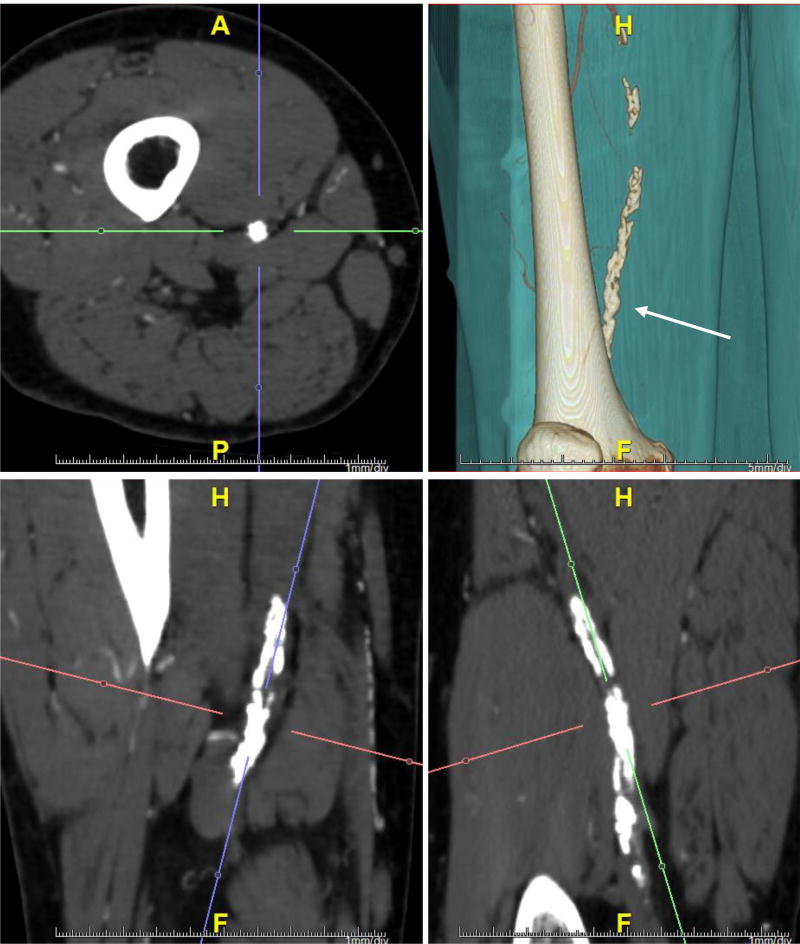
Figure 2.
Example of a 100% calcified lesion in a patient at the level of right Hunter’s adductor channel (arrow). Axial, coronal, sagittal planes and volume rendered CT are shown. Vessel lumen completely obstructed by calcification with no residual flow or thrombus.
Figure 3.
Comparison of length and vessel calcification in successful and unsuccessful endovascular interventions
On multivariable analysis 100% calcification remained the only significant predictor of technical failure with an odds ratio of 9.0 (95% CI 1.8–45.8, P=.008). After accounting for the presence of circumferential calcification, TASC D occlusions (OR 1.86, 95% CI .48–7.18, P=.369) or total length of lesion occlusion (OR 1.05, CI 1.00–1.12, P=.063) were no longer found to be significantly associated with technical failure.
The intra-operative details of the successful and unsuccessful procedures are noted in Table 3. Procedure time, fluoroscopy time, radiation exposure and contrast use were similar between the successful and unsuccessful groups. Femoral endarterectomy and concomitant iliac intervention was also similar between the two groups. There was one use of distal retrograde access used in the unsuccessful cohort, compared to zero in the successful group. A distal re-entry devices and ultrasound guided crossing devices was used in the successful group and a distal re-entry device was used once in the unsuccessful cohort.
Table 3.
Intra-operative Findings
| Successful n = 59 | Unsuccessful n = 15 | P-value | |
|---|---|---|---|
| Procedure Time - min (IQR) | 93 (79–120) | 85 (76–100) | .14 |
| Fluoroscopy Time - min (IQR) | 25.2 (18.4–34.9) | 25.4 (22.4–34.6) | .75 |
| Radiation exposure – mGy (IQR) | 499 (228–901) | 229 (191–303) | .09 |
| Iodinated contrast - cc (IQR) | 44 (30–60) | 40 (35 – 49) | .65 |
| Femoral endarterectomy (%) | 7 (12) | 4 (27) | .22 |
| Iliac Intervention (%) | 18 (31) | 3 (20) | .53 |
| Balloon angioplasty alone (%) | 17 (29) | N/A | -- |
| Balloon angioplasty + stent (%) | 42 (71) | N/A | -- |
Median follow-up for the study population was 15.8 months (IQR 8.6–27.8). There were six patient deaths during the follow-up period at an average of 13.6 months (range 0.6–20) from initial endovascular intervention. Forty-six of the successfully treated occlusions (78%) were evaluated for patency at six-months and 35 occlusions (59%) were evaluated for patency at 1 year. The primary patency rates of SFA-pop occlusions treated successfully at 6-month and 1-year intervals were 78% and 49%, respectively. The cumulative patency of SFA-pop occlusions treated successfully at 6-month and 1-year intervals was 96% and 86%, respectively. The 6-month primary patency for 100% calcified occlusions was 100% at 6 months and 67% at 1 year compared to 76% at 6-months and 48% 1-year primary patency occlusions with <100% vessel calcification.
Discussion
This study demonstrates pre-operative CTA findings are associated with technical success in endovascular treatment of occlusions in SFA-pop region. Our main findings show 100% calcified occlusions in the SFA-pop region were approximately nine times more likely to be associated with technical failure compared with lesser extent of calcification using basic catheter and wire endovascular techniques. The TASC II classification for femoral-popliteal lesions considers heavy calcification as part of the criteria; however, no quantitative definition of heavily calcified lesions was described.5 As CTA provide additional information compared to catheter based angiography, non-invasive imaging may guide future treatment options with improvement to CTA technology.
Previous work of CTOs in the coronary arteries demonstrated vessel calcification as a predictor of technical failure of catheter based treatment. This was first described by Mollet and colleagues when describing calcification of coronary arteries found on pre-operative CTA.10 Their series of 47 lesions found that calcification of >50% of the vessel cross sectional area was an independent predictor of guidewire crossing failure. Similar follow-up studies of coronary CTA confirmed these findings regarding vessel calcification.11–13 In a study of subintimal revascularization of occlusions in the SFA-pop region, Marks and colleagues found that grayscale findings on DUS at the distal re-entry point was predictive of technical failure.14 Risk factors for developing vessel calcification include diabetes and chronic renal disease.15
The length of the occlusive lesion was associated with technical failure in univariate analysis but not statistically significant in multi-varriate regression. We found there were two short occlusions that were 1 and 3 cm in length that were 100% calcified that not treated successfully, suggesting that for our cohort 100% calcification rather than length of occlusion was more associated with technical failure. These two unsuccessful short occlusive were found at the tibial trifurcation (TASC D definition) showing that the location of the lesion also contribute technical success. Other radiographic findings such as multiple occlusions, negative remodeling, or vessels runoff were not found to be independent risk factors for technical failure.
A recently developed scoring system with the Japanese CTO registry (J-CTO) utilized CTA findings to predict technical success and guidewire crossing times < 30 minutes.7. The coronary CTO lesion received a total score and was as assigned as easy, intermediate, difficult, or very difficult lesion. In our study we did not attempt to create a scoring system given the limited number of patients but developing a scoring criteria based on CTA findings to predict failure remains an interesting area of future work. Although we note that difficult occlusions, including highly calcified occlusions, may be able to crossed with retrograde techniques, crossing devices, and intravascular ultrasound16–17 CTA findings may be useful in predicting when these techniques may be necessary.
Our study also highlights that pre-procedural CTA was used in approximately half of patients prior to endovascular intervention. This is considerably higher than reported literature of approximately 2% of patients who underwent or expected angiography during the same inpatient stay with a large range between individual hospital and geographic region.18 The large difference is due to the majority of the patients receiving pre-operative CTA scans during an outpatient setting or imaging done at another facility. As nearly half of patients had claudication symptoms, intervention was not performed immediately as a walking regimen was recommended as first line therapy. Currently, there are no recommendations regarding indications for additional non-invasive imaging prior to intervention. As there are advantages to DUS, CTA, and MRA individual patient factors as well as imaging resource availability need to be considered.19–20 We were unable to compare DUS and CTA findings, as many patients with a pre-operative CTA did not undergo additional DUS scanning. Correlating ultrasound and CT findings may assist in determining the utility of additional imaging prior to intervention.
We note that pre-operative CTAs are useful for a variety of reasons including treatment planning. We note six of the ten patients with SFA-pop occlusions did not undergo attempted SFA-pop crossing due to concomitant iliac interventions and/or common femoral endarterectomies. This underscores the importance of considering all patient factors including frailty, co-morbidities, along with disease distribution and severity when choosing the appropriate treatment approach for each patient. Pre-operative CTAs can also influence providers to forego an endovascular approach and proceed directly with bypass in the case of severe disease. Shue and colleagues found that there was no effect in lower extremity bypass outcomes with CTA or MRA as the main pre-operative image modaility,21 highlighting that tibial vessel targets are readily seen on CTA excluding the need for conventional angiogram. In addition, recent work found CTAs were accurate in vein mapping the size and quality of the saphenous vein thereby eliminating the need for additional DUS vein mapping.22
Whether pre-operative CTA scans help with technical success and long term outcomes is an area of future research. In a previous study of MRA prior to renal artery balloon angioplasty and stenting, interventions with pre-operative imaging showed reduced diagnostic angiographic runs and iodinated contrast use.23 As non-invasive imaging continues to improve and becomes more available the increased clinical utility may elucidated over time. It is also important to note when deciding whether to obtain a pre-procedural CTA scan cost, radiation exposure, and contrast dye also need to be considered. On average CTA scans used contrast volumes of 145 cc compared to 41 cc during our endovascular interventions and this may preclude patients with advanced kidney disease not yet on hemodialysis or patients with severe iodine allergies.
Our endovascular technical success rates are similar to published reports. Previous reports have shown an approximately of 80–90% success rate of treating occlusions in the SFA-pop segment.13, 24–25 We found that TASC C/D occlusions had poorer technical success rates compared to TASC A/B occlusions which were treated with 100% success. These findings also show vascular surgeons are also being more aggressive with endovascular based interventions for TASC C/D occlusions with recent endovascular advances and operator experience. As more physicians are incorporating an “endovascular first” treatment approach more challenging occlusions are being aggressively treated.26–28
This study contains limitations that warrant further discussion. First, the small number of failures makes it difficult to draw broad conclusions regarding CTA findings and endovascular technical success. As both patient presentation and distribution of arterial disease vary considerably these findings may be difficult to apply to each individual patient. For example, patient’s vessel size, multiple levels of disease and proximal vessel tortuosity can affect procedure outcomes. Furthermore, each surgeon’s approach, technique, and experience can lead to varying outcomes. As vascular surgeons are able to treat the same disease with an open bypass this also could have affected technical success outcomes with less aggressive attempts.
This study focused solely on occlusions in the SFA-pop region given the higher success rate of iliac interventions and difficulty in assessing tibial vessels.29 We focused on the SFA-pop region as this was a vessel segment that did not involve arterial branches and minimal tortuosity. Occlusions of the tibial arteries are difficult to analyze given the small vessel caliber, timing of contrast dye, and varying anatomy. However, recent work by Kang and colleagues showed that calcification is also predictor of technical failure in the tibial artery region reinforcing our findings.30
Lastly, we note it is difficult to predict long-term patency of successfully treated occlusions in the SFA-pop region. We found that there was a higher primary patency at 6 months and 1 year of successfully treated 100% calcified occlusions compared to occlusions with <100% calcification, therefore showing it may be reasonable to attempt endovascular treatment of 100% calcified vessels. However, this conclusion is limited given the small number of successfully treated lesions. Heterogeneity regarding patient factors, occlusion characteristics, operator technique and treatment choice (e.g. balloon angioplasty versus drug eluting stent) make it difficult to predict long term outcomes according to CTA findings. As post-operative CTAs are not routinely performed to evaluate changes in vessel flow, this also makes it difficult to study long term patency. As with most studies, a larger evaluation of patients with pre-operative CTA and similar radiographic characteristics may help guide future endovascular treatment recommendations.
Conclusions
This study demonstrated 100% vessel calcification as the best predictor of technical failure in endovascular treatment of occlusions in the SFA-pop region. As advances in catheter based technology and non-invasive radiographic imaging continue to evolve, future guidelines may consider non-invasive imaging in the pre-operative assessment to help guide treatment strategies.
Supplementary Material
Supplemental Table 1. Characteristics from Pre-operative CTAs of Untreated SFA-pop occlusions
Footnotes
Presented at the poster session of the Society of Vascular Surgery, Vascular Annual Meeting, Washington DC, June 2016; Western Vascular Surgery Plenary Presentation, Colorado Springs, CO, September 2016.
References
- 1.Met R, Bipat S, Legemate DA, Reekers JA, Koelemay MJ. Diagnostic performance of computed tomography angiography in peripheral arterial disease: a systematic review and meta-analysis. JAMA. 2009 Jan 28;301(4):415–24. doi: 10.1001/jama.301.4.415. [DOI] [PubMed] [Google Scholar]
- 2.Napoli A, Anzidei M, Zaccagna F, Cavallo Marincola B, Zini C, Brachetti G, et al. Peripheral arterial occlusive disease: diagnostic performance and effect on therapeutic management of 64-section CT angiography. Radiology. 2011 Dec;261(3):976–86. doi: 10.1148/radiol.11103564. [DOI] [PubMed] [Google Scholar]
- 3.Schernthaner R, Fleischmann D, Stadler A, Schernthaner M, Lammer J, Loewe C. Value of MDCT angiography in developing treatment strategies for critical limb ischemia. AJR Am J Roentgenol. 2009 May;192(5):1416–24. doi: 10.2214/AJR.08.1078. [DOI] [PubMed] [Google Scholar]
- 4.Thukkani AK, Kinlay S. Endovascular intervention for peripheral artery disease. Circ Res. 2015 Apr 24;116(9):1599–613. doi: 10.1161/CIRCRESAHA.116.303503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Society for Vascular Surgery Lower Extremity Guidelines Writing Group. Conte MS, Pomposelli FB, Clair DG, Geraghty PJ, McKinsey JF, Mills JL, et al. Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: management of asymptomatic disease and claudication. J Vasc Surg. 2015 Mar;61(3 Suppl):2S–41S. doi: 10.1016/j.jvs.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 6.Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG TASC II Working Group. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) J Vasc Surg. 2007 Jan;45(Suppl S):S5–67. doi: 10.1016/j.jvs.2006.12.037. [DOI] [PubMed] [Google Scholar]
- 7.Morino Y, Abe M, Morimoto T, Kimura T, Hayashi Y, Muramatsu T, et al. J-CTO Registry Investigators. Predicting successful guidewire crossing through chronic total occlusion of native coronary lesions within 30 minutes: the J-CTO (Multicenter CTO Registry in Japan) score as a difficulty grading and time assessment tool. JACC Cardiovasc Interv. 2011 Feb;4(2):213–21. doi: 10.1016/j.jcin.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 8.Opolski MP, Achenbach S, Schuhbäck A, Rolf A, Möllmann H, Nef H, et al. Coronary computed tomographic prediction rule for time-efficient guidewire crossing through chronic total occlusion: insights from the CT-RECTOR multicenter registry (Computed Tomography Registry of Chronic Total Occlusion Revascularization) JACC Cardiovasc Interv. 2015 Feb;8(2):257–67. doi: 10.1016/j.jcin.2014.07.031. [DOI] [PubMed] [Google Scholar]
- 9.Rosenfield K, Jaff MR, White CJ, Rocha-Singh K, Mena-Hurtado C, Metzger DC, et al. Trial of a Paclitaxel-Coated Balloon for Femoropopliteal Artery Disease. N Engl J Med. 2015 Jul 9;373:145–53. doi: 10.1056/NEJMoa1406235. [DOI] [PubMed] [Google Scholar]
- 10.Mollet NR, Hoye A, Lemos PA, Cademartiri F, Sianos G, McFadden EP, et al. Value of preprocedure multislice computed tomographic coronary angiography to predict the outcome of percutaneous recanalization of chronic total occlusions. Am J Cardiol. 2005;95:240–3. doi: 10.1016/j.amjcard.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Soon KH, Cox N, Wong A, Chaitowitz I, Macgregor L, Santos PT, et al. CT coronary angiography predicts the outcome of percutaneous coronary intervention of chronic total occlusion. J Interv Cardiol. 2007;20:359–66. doi: 10.1111/j.1540-8183.2007.00275.x. [DOI] [PubMed] [Google Scholar]
- 12.García-García HM, van Mieghem CA, Gonzalo N, Meijboom WB, Weustink AC, Onuma Y, et al. Computed tomography in total coronary occlusions (CTTO registry): radiation exposure and predictors of successful percutaneous intervention. EuroIntervention. 2009;4:607–16. doi: 10.4244/eijv4i5a102. [DOI] [PubMed] [Google Scholar]
- 13.Martín-Yuste V, Barros A, Leta R, Ferreira I, Brugaletta S, Pujadas S, et al. Factors determining success in percutaneous revascularization of chronic total coronary occlusion: multidetector computed tomography analysis. Rev Esp Cardiol. 2012;65:334–40. doi: 10.1016/j.recesp.2011.11.009. [DOI] [PubMed] [Google Scholar]
- 14.Marks NA, Ascher E, Hingorani AP, Shiferson A, Puggioni A. Gray-scale median of the atherosclerotic plaque can predict success of lumen re-entry during subintimal femoral-popliteal angioplasty. J Vasc Surg. 2008 Jan;47(1):109–15. doi: 10.1016/j.jvs.2007.09.039. discussion 115–6. [DOI] [PubMed] [Google Scholar]
- 15.Chen NX, Moe SM. Vascular Calcification: pathophysiology and risk factors. Curr Hypertens Rep. 2012;14:228–37. doi: 10.1007/s11906-012-0265-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.White CJ, Gray WA. Endovascular therapies for peripheral arterial disease: an evidence-based review. Circulation. 2007 Nov 6;116(19):2203–15. doi: 10.1161/CIRCULATIONAHA.106.621391. [DOI] [PubMed] [Google Scholar]
- 17.Panico A, Jafferani A, Shah F, Dieter RS. Advances in peripheral arterial disease endovascular revascularization. Cardiol Clin. 2015 Feb;33(1):89–98. doi: 10.1016/j.ccl.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 18.de Vos MS, Hawkins AT, Hevelone ND, Hamming JF, Nguyen LL. National variation in the utilization of alternative imaging in peripheral arterial disease. J Vasc Surg. 2014 May;59(5):1315–22. e1. doi: 10.1016/j.jvs.2013.11.059. [DOI] [PubMed] [Google Scholar]
- 19.Chan D, Anderson ME, Dolmatch BL. Imaging evaluation of lower extremity infrainguinal disease: role of the noninvasive vascular laboratory, computed tomography angiography, and magnetic resonance angiography. Tech Vasc Interv Radiol. 2010 Mar;13(1):11–22. doi: 10.1053/j.tvir.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 20.Owen AR, Roditi GH. Peripheral arterial disease: the evolving role of non-invasive imaging. Postgrad Med J. 2011 Mar;87(1025):189–98. doi: 10.1136/pgmj.2009.082040. [DOI] [PubMed] [Google Scholar]
- 21.Shue B, Damle RN, Flahive J, Kalish JA, Stone DH, Patel VI, et al. The increased use of computed tomography angiography and magnetic resonance angiography as the sole imaging modalities prior to infrainguinal bypass has had no effect on outcomes. Ann Vasc Surg. 2015 Aug;29(6):1245–54. doi: 10.1016/j.avsg.2015.03.039. [DOI] [PubMed] [Google Scholar]
- 22.deFreitas DJ, Love TP, Kasirajan K, Haskins NC, Mixon RT, Brewster LP, et al. Computed tomography angiography-based evaluation of great saphenous vein conduit for lower extremity bypass. J Vasc Surg. 2013 Jan;57(1):50–5. doi: 10.1016/j.jvs.2012.06.077. discussion 55. [DOI] [PubMed] [Google Scholar]
- 23.Sharafuddin MJ, Stolpen AH, Dixon BS, Andresen KJ, Sun S, Lawton WJ. Value of MR angiography before percutaneous transluminal renal artery angioplasty and stent placement. J Vasc Interv Radiol. 2002 Sep;13(9 Pt 1):901–8. doi: 10.1016/s1051-0443(07)61773-4. [DOI] [PubMed] [Google Scholar]
- 24.Laxdal E, Jenssen GL, Pedersen G, Aune S. Subintimal angioplasty as an treatment of femoropopliteal occlusions. Eur J Vasc Endovasc Surg. 2003;25:578–82. doi: 10.1053/ejvs.2002.1899. [DOI] [PubMed] [Google Scholar]
- 25.Surowiec SM, Davies MG, Eberly SW, Rhodes JM, Illig KA, Shortell CK, et al. Percutaneous angioplasty and stenting of the superficial femoral artery. J Vasc Surg. 2005;41:269–78. doi: 10.1016/j.jvs.2004.11.031. [DOI] [PubMed] [Google Scholar]
- 26.Jaff MR, White CJ, Hiatt WR, Fowkes GR, Dormandy J, Razavi M, et al. An update on methods for revascularization and expansion of the TASC lesion classification to include below-the-knee arteries: A supplement to the inter-society consensus for the management of peripheral arterial disease (TASC II): The TASC steering committee. Catheter Cardiovasc Interv. 2015 Oct;86(4):611–25. doi: 10.1002/ccd.26122. [DOI] [PubMed] [Google Scholar]
- 27.Olin JW, White CJ, Armstrong EJ, Kadian-Dodov D, Hiatt WR. Peripheral Artery Disease: Evolving Role of Exercise, Medical Therapy, and Endovascular Options. J Am Coll Cardiol. 2016 Mar 22;67(11):1338–57. doi: 10.1016/j.jacc.2015.12.049. [DOI] [PubMed] [Google Scholar]
- 28.Antoniou GA, Chalmers N, Georgiadis GS, Lazarides MK, Antoniou SA, Serracino-Inglott F, et al. A meta-analysis of endovascular versus surgical reconstruction of femoropopliteal arterial disease. J Vasc Surg. 2013 Jan;57(1):242–53. doi: 10.1016/j.jvs.2012.07.038. [DOI] [PubMed] [Google Scholar]
- 29.Yacyshyn VJ, Thatipelli MR, Lennon RJ, Bailey KR, Stanson AW, Holmes DR, Jr, et al. Predictors of failure of endovascular therapy for peripheral arterial disease. Angiology. 2006;57:403–17. doi: 10.1177/0003319706290732. [DOI] [PubMed] [Google Scholar]
- 30.Kang IS, Lee W, Choi BW, Choi D, Hong MK, Jang Y, Ko YG. Semiquantitative assessment of tibial artery calcification by computed tomography angiography and its ability to predict infrapopliteal angioplasty outcomes. J Vasc Surg. 2016 Jul 15; doi: 10.1016/j.jvs.2016.04.047. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. Characteristics from Pre-operative CTAs of Untreated SFA-pop occlusions