Abstract
OBJECTIVE
To test for differential weight loss response to Low-Fat (LF) vs. Low-Carbohydrate (LC) diets by insulin resistance status with emphasis on overall quality of both diets.
METHODS
Sixty-one adults, BMI 28-40 kg/m2, were randomized in a 2X2 design to LF or LC by insulin resistance status in this pilot study. Primary outcome was 6-month weight change. Participants were characterized as more insulin resistant (IR) or more insulin sensitive (IS) by median split of baseline insulin-area-under-the-curve from an oral glucose tolerance test. Intervention consisted of 14 one-hour class-based educational sessions.
RESULTS
Baseline % carb:% fat:% protein was 44:38:18. At 6m the LF group reported 57:21:22 and the LC group reported 22:53:25 (IR and IS combined). Six-month weight loss (kg) was 7.4 ± 6.0 (LF-IR), 10.4 ± 7.8 (LF-IS), 9.6 ± 6.6 (LC-IR), and 8.6 ± 5.6 (LC-IS). No significant main effects were detected for weight loss by diet group or IR status; no significant diet X IR interaction. Significant differences in several secondary outcomes were observed.
CONCLUSION
Substantial weight loss was achieved overall, but a significant diet X IR status interaction was not observed. Opportunity to detect differential response may have been limited by the focus on high diet quality for both diet groups and sample size.
Keywords: Weight loss, insulin resistance, hyperinsulinemia, low-fat diet, low-carbohydrate diet, obesity
INTRODUCTION
Obesity is related to increased risk of heart disease, stroke, type II diabetes, and some cancers (1). Moderately obese individuals with insulin resistance have a greater metabolic risk profile for these chronic diseases than those with greater insulin sensitivity, even at the same weight (2). Weight loss improves insulin sensitivity and lowers cardiovascular risk (3). However, most people find successful weight loss challenging. The weight loss diet traditionally recommended by health professionals has been a low-fat (Low-Fat), calorie restricted diet (4), which may be particularly inappropriate for insulin resistant individuals, and has been challenged by proponents of alternative dietary strategies, particularly low-carbohydrate (Low-Carb) (5-7).
Several weight loss diet studies have examined whether differences in glucose and insulin dynamics (e.g., differential insulin secretion or insulin resistance status) are a mediating factor for successful weight loss on Low-Fat vs. Low-Carb diets (8-12). These studies have consistently observed that overweight adults with higher insulin secretion or insulin resistance lose more weight on Low-Carb than Low-Fat diets. In contrast, lower insulin secretion or the more insulin sensitive individuals in these trials had more or comparable success with a Low-Fat diet. McClain et al. observed that participants with higher baseline fasting insulin concentrations had lower adherence than participants with lower fasting insulin concentrations when assigned Low-Fat, even when unaware of their baseline fasting insulin status (10). Several proposed mechanisms support the plausibility of greater weight loss on a low carbohydrate diet among insulin resistant individuals, including increased fatty acid uptake, inhibition of lipolysis, and effects on hunger, snacking, and energy intake (12-18).
The current study objective was to conduct a pilot study continuing the research on the potential mediating effects of insulin resistance status on weight loss responses to Low-Fat vs. Low-Carb diets. Particular emphasis was placed on maximizing the fat vs. carbohydrate differentials on the two diets, and on overall nutritional quality.
METHODS
Participants
Participants were recruited from the local community primarily through media advertisements. Pre-menopausal women and men ages 18-50 years were invited to enroll if BMI was 28-40 kg/m2, body weight was stable over the previous 2 months, and medications were stable for ≥ 3 months. Potential participants were excluded if they self-reported: hypertension (except for those stable on anti-hypertension medications), type I or II diabetes mellitus, heart, renal, or liver disease, cancer or active neoplasms, hyperthyroidism unless treated and under control, taking any medications known to affect weight/energy expenditure, smoking, alcohol intake ≥ 3 drinks/day, pregnancy, lactation, no menstruation for the previous 12 months, or plans to become pregnant within the next year. Race/ethnicity data were collected by self-report. All study participants provided written informed consent. The study was approved by the Stanford University Human Subjects Committee.
Study Design
The study employed a 2 X 2 design: Low-Fat vs. Low-Carb diets, and more insulin resistant (IR) vs. more insulin sensitive (IS). We suggest the terms “insulin resistance” and “insulin sensitivity” here be interpreted cautiously as we used a proxy measure for this, rather than a direct measure (expanded discussion in Section 1 of Supplemental Material). The method of determining relative insulin resistance was to calculate an area under the curve of insulin concentrations (AUC-INS) from a four blood samples taken during an oral glucose tolerance test (OGTT) (time 0, 30, 60 and 120 minutes) conducted prior to randomization. Median AUC-INS was determined separately for women and men. Those above the median were considered to be relatively more insulin resistant, and those below were considered relatively more insulin sensitive.
A random number generator (Microsoft Excel) was used to stratify the randomization to Low-Fat vs. Low-Carb by insulin resistance status and gender. The duration of the intervention was 6 months, and the primary outcome was 6-month weight change.
Intervention
The intervention was a class-based education program led by a single health educator (RC). Participants were assigned to groups of 14-16 per class to follow either a Low-Fat or Low-Carb diet. There were 14 one-hour classes over 6 months; once/week for 8 weeks, then once every other week for 8 weeks, and then once/month for 8 weeks.
Dietary strategy
There were four central components to the dietary strategy. The first was “How Low Can You Go” (Limbo). Low-Fat participants were instructed to cut back to 20 grams/day of total fat, and for Low-Carb to 20 grams/day of digestible carbohydrate. The goal was to achieve the lowest level of fat or carbohydrate intake within the first eight weeks. The second stage (Titrate) was to slowly add fat or carbohydrate back to the diet in increments of five grams/day (e.g., from 20 to 25 grams/day) and then hold it at that amount for 1-4 weeks before adding another 5 grams/day. The third component was to identify the lowest level of fat or carbohydrate intake participants felt could be maintained long term, potentially for the rest of their lives. The fourth strategy was to promote high nutrient density (Quality). Other Quality concepts included “real food,” “minimally processed,” “seasonal,” “organic,” “grass-fed,” “whole grain,” and “pasture-raised,” depending on diet assignment. Both diet groups received similar instructions to drink water and to minimize added sugars, refined white flour products, and sources of trans fats. Participants on the Low Carb diet were asked to consume half an avocado each day (approximately 160 Kcal), as well choosing other sources of plant-based fats, including olive oil, nuts and seeds, and nut butters. Hass avocados were provided by the Hass Avocado board and were distributed to the participants. All participants were encouraged to take an active role in making food choices; by preparing their own foods at home, reading labels, and asking for appropriate modifications for restaurant menu items.
In summary, the diet strategy for both Low-Fat and Low-Carb was a “Limbo-Titrate-Quality” approach designed to motivate participants to achieve the lowest possible level of fat or carbohydrate intake with maximal overall nutritional quality and a dietary pattern that could be continued for a lifetime.
Beyond fat and carbohydrate lowering
Notably, there were no calorie restriction targets in the intervention. Participants were encouraged to track their intake using daily food journals and computer tracking programs. While the first 8 weeks of classes focused specifically on separate strategies to lower fat or carbohydrate intake, the subsequent four months of classes addressed more global topics for both diet groups, similarly, such as mindful eating, adequate sleep, body acceptance, and sugar addition.
Physical activity
All participants were encouraged to be physically active. Participants who were already physically active at baseline were encouraged to maintain or increase their activity. Those who were sedentary at baseline were encouraged to begin moderate exercise. All participants were given pedometers (Omron HJ-112 Digital Pocket Pedometer).
Data Collection
All data were collected at baseline, 3, and 6 months. Clinic and laboratory staff members were blinded to treatment assignment. Participants were blinded as to their baseline OGTT results.
Diet and physical activity data
Three telephone-administered 24-hour recall interviews were conducted at each time point using Nutrition Data System for Research (NDS-R) software [Nutrition Coordinating Center (NCC), University of Minnesota, versions 4.05.33 (2011) and 4.06.34 (2012)]. Interviews were conducted on two weekdays and one weekend day, non-consecutive whenever possible, unannounced, during a two-week window. Average daily energy expenditure was assessed using the Stanford 7-day physical activity recall (19).
Anthropometric data
Height was measured to the nearest millimeter using a standard wall-mounted stadiometer. Body weight was measured to the nearest 0.1 kg on a calibrated clinical scale. Waist circumference was measured to the nearest millimeter at the umbilicus.
Metabolic measures
Blood samples were collected after ≥10 hour fast. Plasma total cholesterol and triglycerides (free glycerol blank subtracted) were measured enzymatically using established clinical chemistry laboratory established methods (Northwest Lipid Laboratory, Seattle, WA) (20, 21). High density lipoprotein cholesterol (HDL-C) was measured by liquid selective detergent followed by enzymatic determination of cholesterol (22). Low density lipoprotein cholesterol (LDL-C) was calculated according to Friedewald (23). Total plasma insulin in serum was measured by radioimmunoassay (24), blood glucose was measured using a modification of the glucose oxidase/peroxidase method (25, 26) (Diabetes Research Center, Washington University, St Louis, MO). Resting blood pressure was assessed three times at 2-minute intervals as described elsewhere (27); the initial reading was discarded and the last two readings were averaged.
Statistical Methods
The primary objective was to test whether there was a significant interaction in weight loss on Low-Fat vs. Low-Carb diets by insulin resistance status as estimated by AUC-INS. Dietary composition data (energy, % carbohydrate, fat, and protein, and grams of fiber, added sugars, and saturated fat) are presented as raw, unadjusted means (± sd) (i.e., no imputation for missing data).
For the main analysis, data were multiply imputed with the MICE package in R 3.0 using 5 imputation steps and 5 imputed data sets. Each imputed data set was fit to a linear regression model using change in weight at six months as the outcome and with subject height, diet, insulin resistance-insulin sensitivity (IR-IS) status and an interaction term between diet and IR-IS status as predictors. Resulting variance estimates were pooled to account for the additional variability induced by the imputation process. In a sensitivity analysis we repeated these models after replacing the dichotomous IR-IS status with continuous baseline insulin AUC. Other exploratory analyses included the use of INS-30, INS-120, and Glu-AUC0-30 X Ins-AUC0-30. We also fit models where, instead of adjusting for baseline height, we adjusted for baseline BMI.
We also explored longitudinal differences between risk factors across the four diet X IR-IS groups (e.g. Low-Fat IR, Low-Carb IR, Low-Fat IS, and Low-Carb IS). For each risk factor, a mixed effect model was fit with the corresponding risk factor as the outcome and group, time point and group time point interaction as predictors. Models were either linear or logistic, depending on the nature of the risk factor. For risk factors with significant interaction term p values, additional pairwise comparisons between the four groups were made using Tukey’s HSD test. All statistical tests were two-tailed using a significance level of 0.05.
RESULTS
Participants were enrolled from February to April, 2012. Sixty-one eligible participants were randomized into four groups – two classes of Low-Fat, and two classes of Low-Carb, with approximately 50% IR and 50% IS in each classes (Figure 1). Baseline characteristics are presented in Table 1. By design INS-AUC (and the highly correlated fasting insulin), were higher for IR vs. IS. As expected, BMI was higher among the more IR vs. IS participants with a trend for higher triglycerides and blood pressure, lower HDL-C, and a higher percentage of metabolic syndrome in the IR group.
Figure 1.
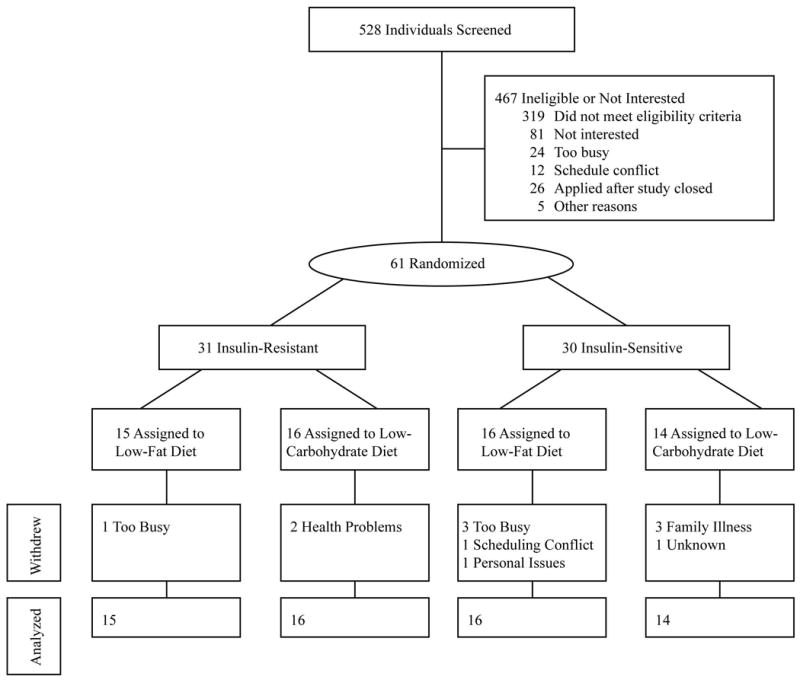
Participant flow through the trial
Table 1.
Baseline Participant Characteristics*
| Variable | Insulin Resistant | Insulin Sensitive | ||
|---|---|---|---|---|
| Low-Fat (n=15) | Low-Carbohydrate (n=16) | Low-Fat (n=16) | Low-Carbohydrate (n=14) | |
| Percent women | 60% | 63% | 63% | 64% |
|
| ||||
| Age (years) | 44 ± 5 | 42 ± 6 | 41 ± 6 | 43 ± 7 |
|
| ||||
| Education (years) | 16.0 ± 2.0 | 16.4 ± 1.8 | 15.9 ± 3.3 | 16.1 ± 1.9 |
|
| ||||
| Percent non-white | 13% | 13% | 25% | 0% |
|
| ||||
| Anthropometrics | ||||
|
| ||||
| BMI (kg/m2) | 35.0 ± 2.4 | 34.2 ± 3.8 | 32.6 ± 2.9 | 31.2 ± 1.9 |
|
| ||||
| Waist circumference | 1.1 ± 0.1 | 1.1 ± 0.1 | 1.0 ± 0.1 | 1.1 ± 0.1 |
|
| ||||
| Cardiovascular disease risk factors | ||||
|
| ||||
| LDL-C (mg/dL) | 118 ± 20 | 108 ± 19 | 111 ± 30 | 113 ± 34 |
|
| ||||
| HDL-C (mg/dL) | 43 ± 10 | 44 ± 13 | 51 ±17 | 49 ± 14 |
|
| ||||
| Triglycerides (mg/dL) | 146 ±58 | 156 ± 68 | 117 ± 59 | 136 ± 99 |
|
| ||||
| Fasting insulin (μU/mL) | 21 ± 5.9 | 27.7 ± 11.4 | 13.4 ± 3.1 | 13.4 ± 3.1 |
|
| ||||
| Fasting glucose (mg/dL) | 100.9 ± 11.2 | 102.5 ±11.8 | 102.7 ± 11.6 | 99.1 ± 7.5 |
|
| ||||
| Insulin AUC (μU × min/ml) | 130.9 ± 54 | 144 ± 49.5 | 65 ± 19 | 58 ± 18.4 |
|
| ||||
| Blood Pressure (mm Hg) | ||||
|
| ||||
| Systolic | 122 ± 12 | 125 ± 10 | 116 ± 13 | 117 ±12 |
|
| ||||
| Diastolic | 81 ± 8 | 83 ± 8 | 77 ± 9 | 78 ± 7 |
|
| ||||
| Percent Metabolic Syndrome | 46.67% | 56.25% | 18.75% | 35.71% |
|
| ||||
| Physical activity (Kcal/kg/day) | 33.2 ± 0.9 | 32.7 ± 1.2 | 34.0 ± 1.7 | 33.6 ± 1.4 |
Abbreviations: HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol
Data are expressed as mean ± SD unless otherwise indicated
Average class attendance was 81 ± 13% (mean ± SD) for the Low-Fat classes and 85 ± 11% for the Low-Carb classes. Of 61 participants enrolled, 49 (80%) completed the 6-month protocol; data were missing at six months from six participants in each diet group.
Dietary Adherence and Physical Activity
Participants in both Low-Fat and Low-Carb made substantial dietary changes as assessed at 3- and 6-months, relative to baseline (Figure 2). With average baseline energy intake percentages of 44:38:18 from carbohydrate:fat:protein, the two diet groups shifted to an average ratio of approximately 58:22 carbohydrate:fat for Low-Fat, and 21:53 for Low-Carb (average at 6 months), with protein being relatively similar, particularly at 6 months. Between the 3- and 6-month time points there was modest recidivism in the Low-Carb group while macronutrient ratios were more stable for Low-Fat during this phase. Average energy intake from alcohol ranged from 1-4 percent of energy in the four Low-Fat and Low-Carb classes (energy intake from alcohol excluded from Figure 2 data). Reported energy intake suggested an average ~600 kcal/day decrease at 3 and 6 months relative to baseline (~30% energy). An expanded presentation of macronutrient distribution for all four subgroups at all three time points is available in the Supplemental Material, Section 2 and Table S1.
Figure 2.
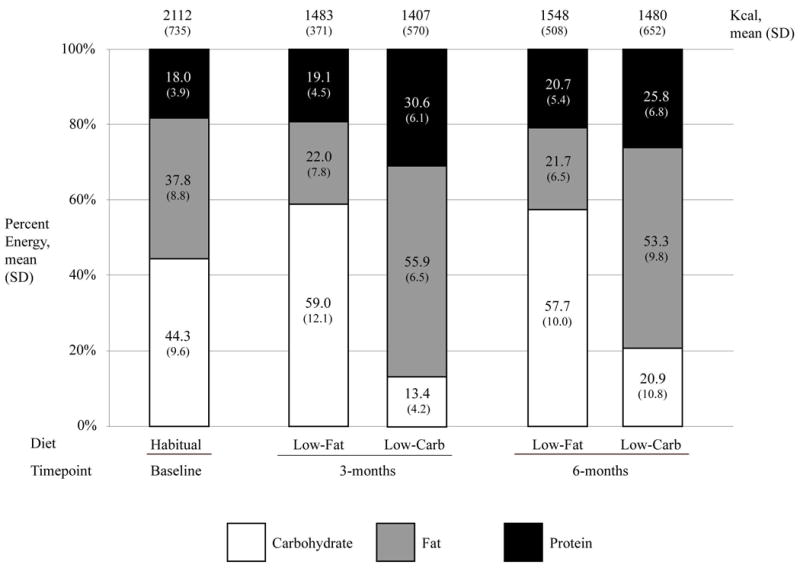
Dietary assessment: proportions of carbohydrates, fats, and proteins for each diet at baseline, 3-months, and 6-months
On average the Low-Fat group decreased absolute amounts (grams) of added sugar intake by ~50% and saturated fat by ~66% while increasing fiber intake by ~25% relative to baseline; the Low-Carb group decreased added sugar intake by ~70%, fiber by ~40% and increased saturated fat by ~10% (Table 2). These were changes of absolute intake amounts in the context of a general ~30% reduction of overall energy intake.
Table 2.
Selected Dietary Components (mean ± SD)*
| Low-Fat | Low-Carbohydrate | |
|---|---|---|
| Total Fiber (g/1000 Kcal) | ||
| Baseline | 9 ± 4 | 12 ± 5 |
| 3-months | 18 ± 8 | 9 ± 3 |
| 6-months | 16 ± 7 | 10 ± 4 |
| Added Sugars (g/1000 Kcal) | ||
| Baseline | 20 ± 10 | 19 ± 10 |
| 3-months | 16 ± 11 | 4 ±4 |
| 6-months | 16 ± 13 | 7 ± 6 |
| Saturated fat (g/1000 Kcal) | ||
| Baseline | 15 ± 4 | 13 ± 4 |
| 3-months | 7 ± 3 | 20 ± 5 |
| 6-months | 7 ± 3 | 19 ± 6 |
Sample sizes: Baseline Low-Fat n=31, Low-Carbohydrate n=30; 3-months n=26 each diet group; 6-months n=25 each group.
Energy expenditure increased modestly and similarly for both diet groups. Baseline energy expenditure for the Low-Fat group was 33.7 ± 1.4 kcal/kg/day, which increased at three and six months to 34.2 ± 1.6 and 34.6 ± 2.6 kcal/kg/day, respectively. In parallel, baseline energy expenditure for the Low-Carb group was 32.7 ± 0.9 kcal/kg/day, which increased at three and six months to 33.5 ± 1.3 and 33.8 ± 1.9 kcal/kg/day, respectively.
Six-Month Weight Loss for Four Groups
Average weight loss after 6 months for the n=49 that completed the protocol was 9.0 ± 6.5 kg (19.8 ± 14.3 lbs), which represented 8.9 ± 5.7% of baseline weight. The 6-month weight loss results by Diet Type-Insulin Resistance Status group were 7.5 ± 6.0 kg for Low-Fat-IR, 10.4 ± 7.8 kg for Low-Fat-IS, 9.6 ± 6.6 kg for Low-Carb-IR, and 8.6 ± 5.6 kg for Low-Carb-IS (Figure 3). A significant interaction between diet assignment and insulin resistance status was not detected, and there were no significant main effect differences in weight loss detected by diet group or by insulin resistance status. We found no meaningful differences in estimate direction or significance between the models where baseline height was a confounder and models where baseline BMI was a confounder, or when using INS-30, INS-120 or Glu-AUC0-30 X Ins-AUC0-30 in the models.
Figure 3.
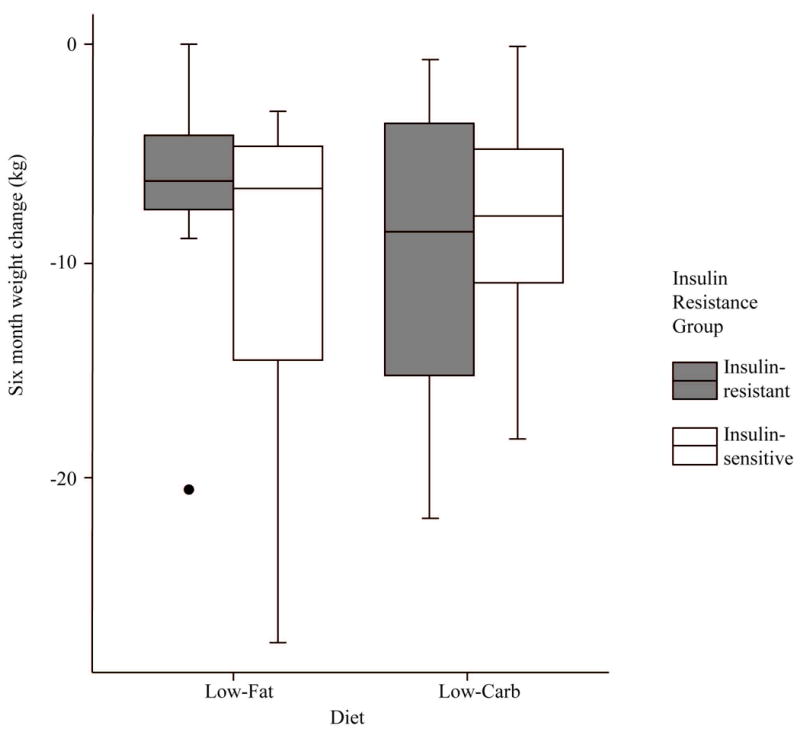
Six month weight change by diet and insulin resistance group, n=49. Six-month weight loss (kg) was 7.4 ± 6.0 (LF-IR), 10.4 ± 7.8 (LF-IS), 9.6 ± 6.6 (LC-IR), and 8.6 ± 5.6 (LC-IS).
Risk Factor Changes
With few exceptions, risk factors changed in a beneficial way across all groups (Table 3). Triglyceride concentrations dropped by ~25% across the four groups combined. Both diastolic and systolic blood pressure decreased for all four groups. HDL-C concentrations increased by almost 10% in three of the four groups, with a negligible overall change in the Low-Fat-IS group. Fasting glucose decreased modestly, on average, in three of the four groups, with a negligible 6-month change in the Low-Carb-IS group. At baseline 40% of participants met metabolic syndrome criteria, which was down to 15% overall at 6 months. No significant 6-month change differences were detected among groups for any of the above risk factors.
Table 3.
Risk Factor Changes and Metabolic Syndrome Prevalence by Diet Group-Insulin Resistance Status
| Insulin Resistant | Insulin Sensitive | P Value | |||
|---|---|---|---|---|---|
| Low-fat (n=15§) | Low-carbohydrate (n=16§) | Low-fat (n=16§) | Low-carbohydrate (n=14§) | Time X Treatment Group* | |
| LDL-C (mg/dL) | |||||
|
| |||||
| 3 month | -13.2 (20.1) | 12.6 (21.0) | -16.2 (27.8) | 23.9 (46.6) | |
| 6 month | -14.4 (23.8)a,b | 6.5 (25.7)a,b | -20.8 (26.1)a | 17.8 (40.8)b | 0.006 |
|
| |||||
| HDL-C (mg/dL) | |||||
|
| |||||
| 3 month | -2.6 (6.0) | 0.1 (4.8) | -3.5 (6.5) | 2.1 (6.6) | |
| 6 month | 3.7 (5.9) | 4.3 (3.7) | 0.6 (5.8) | 4.4 (7.0) | 0.273 |
|
| |||||
| Triglycerides (mg/dL) | |||||
|
| |||||
| 3 month | -8.1 (39.5) | -40.1 (77.9) | -12.8 (23.0) | -20.9 (33.9) | |
| 6 month | -34.1 (30.1) | - 35.1 (67.4) | -9.6 (27.9) | -32.2 (41.4) | 0.588 |
|
| |||||
| Fasting Insulin (μU/mL) | |||||
|
| |||||
| 6 month | -8.2 (5.6)a,b | -12.7 (8.1)a | -4.5 (4.4)b | -3.8 (3.8)b | 0.003 |
|
| |||||
| Fasting Glucose (mg/dL) | |||||
|
| |||||
| 3 month | -5.0 (10.3) | -4.6 (12.9) | -8.1 (10.7) | 0.8 (8.7) | |
| 6 month | -2.8 (10.0) | -5.7 (13.6) | -3.6 (16.5) | 3.8 (7.8) | 0.125 |
|
| |||||
| Insulin AUC (μU x min/ml) | |||||
|
| |||||
| 3 month | -65.8 (4.9) | -68.3 (50.1) | -27.5 (25.4) | -11.2 (23.6) | |
| 6 month | -57.6 (38.4)a,c | -67.5 (49.3)a | -15.1 (32.7)b | -18.3 (20.5)b,c | <0.0001 |
|
| |||||
| Blood Pressure Systolic (mm Hg) | |||||
|
| |||||
| 3 month | -1.1 (5.2) | -6.7 (11.9) | -3.8 (6.3) | -6.0 (7.4) | |
| 6 month | -2.2 (9.0) | -8.8 (10.1) | -6.9 (10.2) | -4.4 (8.1) | 0.165 |
|
| |||||
| Blood Pressure Diastolic (mm Hg) | |||||
|
| |||||
| 3 month | -0.7 (3.8) | -3.8 (7.3) | -3.7 (4.3) | -3.8 (4.3) | |
| 6 month | -2.4 (6.8) | -5.3 (7.5) | -6.4 (7.1) | -4.3 (5.6) | 0.311 |
|
| |||||
| Metabolic Syndrome (percent) | |||||
|
| |||||
| 3 month | 46.7 | 18.8 | 6.3 | 14.3 | |
| 6 month | 20.0 | 12.5 | 12.5 | 7.1 | 0.508 |
Data are expressed as mean (standard deviation), except for Metabolic Syndrome (percent).
Table column headings indicate sample size used in statistical testing (see below). Values reflect actual data from those who completed the 6-month protocol: n=14, n=14, n=11 and n=10, respectively.
Intention-to-treat analysis, with baseline data carried forward for missing values. P value for time X diet group interaction for 6-month change determined using mixed-model and autoregressive covariance structure.
For 6-month risk factors with time X group p<0.05, pair-wise differences are indicated by superscripts; pairs with a shared superscript are not different.
Six-month changes in LDL-C concentrations were statistically different among groups, with increases for Low-Carb and decreases for Low-Fat, regardless of IR status. Fasting insulin concentrations dropped significantly more for the two IR groups than the two IS groups, although by definition the IR groups had higher baseline insulin levels and thus greater capacity for improvement. Overall average fasting insulin concentrations decreased for all four groups. This same pattern was observed for INS-AUC.
Discussion
In this pilot study we investigated whether there was a differential weight loss response to Low-Fat vs. Low-Carb diets by baseline insulin resistance status, using INS-AUC as a proxy measure, among non-diabetic overweight adults and adults with obesity who were otherwise in general good health. Overall, participants experienced substantial weight loss: an average of 9.0 ± 6.5 kg, which represented 8.9 ± 5.7% of baseline weight. However, a significant interaction between diet assignment and insulin resistance status was not detected for weight loss. Dietary assessment indicated substantial diet differentiation between the Low-Fat and Low-Carb groups, which was supported by observed changes in secondary metabolic outcomes including fasting insulin, LDL-C, HDL-C and triglycerides. In addition, the dietary assessment data indicate that the substantial dietary changes achieved by mid-study were largely maintained to the end of the study at 6 months.
Several other studies have reported a statistically significant interaction in weight loss between diet type and insulin resistance status, including a previous investigation by our own research group (8-10, 12). Two of the studies were feeding studies, of 4-6 month duration with small samples sizes of 4-8 per treatment arm (8, 12). These studies, perhaps because of the more rigorous control of diet, and the 30% restriction of energy intake, achieved greater weight loss overall than the two free-living studies which used an ad libitum approach (9, 10). However, the free-living studies had larger sample sizes and longer durations than the feeding studies. Notably, the four previous studies used three different methods to assess insulin and glucose dynamics. Compared to this set of four previous studies, in the current free-living study the magnitude of overall weight loss was comparable to the feeding studies and substantially higher than the other two free-living studies while using an ad libitum approach to energy intake. The INS-AUC method used in the current study to differentiate greater insulin resistant from greater insulin sensitive individuals was different than all of the other studies, and was more a measure of hyperinsulinemia than a direct measure of insulin resistance. In absolute numbers, the average weight loss results in the current study paralleled the findings from the other studies – the more insulin resistant group lost slightly more weight on Low-Carb, and the insulin sensitive group lost slightly more weight on Low-Fat, but the differences were not statistically or clinically significant. With so many differences among the previous four studies and the current study, which all address the same general research question, we are not able to determine whether we failed to detect a true effect that the other studies correctly identified, or if we truly and accurately identified no effect in our study population using the design described.
There are multiple mechanisms that could be responsible for a potential differential weight loss response to Low-Fat vs. Low-Carb diets by variability in insulin and glucose dynamics including differential hunger /satiety, energy expenditure, fatty-acid metabolism, lipolysis, and adipogenesis. Several groups of investigators have observed one or more factors along a continuum that suggest Low-Fat relative to Low-Carb diets cause greater excursions in postprandial glucose and insulin metabolism, may increase 24-hour hunger, and may subsequently increase overall energy intake due to their higher glycemic load (11, 28-31). Related research suggests that diets with a higher glycemic index can affect hormones regulating metabolism (13-15). Under these conditions insulin resistant individuals may feel less satiated and experience stronger physiologically driven urges to consume more food after consuming a lower fat/higher carbohydrate meal compared to insulin sensitive individuals.
In separate experiments with humans, one a parallel design and another a cross-over, the lab group of Ludwig et al., found that substantial weight loss achieved by or followed by isocaloric diets differing in glycemic load led to differential changes in resting energy expenditure and total energy expenditure; the observed results favored greater energy expenditure on the lower glycemic load/lower carbohydrate diets (17, 32). Although insulin resistance status was not addressed as a potential covariate in these analyses, it is plausible that the more insulin resistant individuals who were on higher glycemic load/higher carbohydrate diets would experience an even greater decrease in energy expenditure than the more insulin sensitive individuals on the same diet, making it more difficult to achieve or maintain weight loss.
Further discussion of the observed changes and lack of changes in some of the risk factors in Table 3 is presented in the Supplemental Material Section 3.
The study design and conduct included several important strengths. One was the high degree of dietary differentiation achieved for those assigned to Low-Fat vs. Low-Carb. In many weight loss diet studies, the combination of modest dietary goals and substantial recidivism over time (i.e., weak treatment fidelity) can lead to a lack of physiologically meaningful dietary differences between treatment arms. The differences in proportions of energy intake from fat vs. carbohydrate achieved and maintained out to 6 months in the two diet groups of the current study involved a substantial shift of approximately 25% of energy intake. The use of three unannounced 24-hour recalls and NDS-R for dietary assessment at three time points, and the high rate of completion of these assessments was an important methodological strength. Other strengths included the relatively high retention rate of 80% and the identical drop-out rates in both diets. Stratifying the randomization by insulin resistance status was an important design component, and the use of INS-AUC from OGTTs to identify and differentiate participants who were more insulin resistant vs. more insulin sensitive was superior to fasting measures that could have been used (e.g., fasting insulin or TG/HDL-C ratio).
The major limitations of this pilot study were the duration and sample size. Given a consistent pattern of maximal weight loss at six months followed by weight stabilization and often regain across a range of published studies, it is more optimal to include follow-ups of a year or more in weight loss studies. Also, given the substantial heterogeneity of inter-group weight loss typical of these types of trials, large sample sizes are a preferred design component; the null finding for an interaction between insulin resistance status and diet assignment for weight loss difference in this study may have been attributable to a lack of adequate statistical power. However, a primary objective of this pilot study was to test the approach undertaken to achieve greater differentiation of diets and treatment fidelity for the purpose of incorporating this approach in a future, larger, longer trial; that follow-up trial, with a sample size of 600 and a duration of one year is currently underway. An expanded discussion of study limitations is presented in the Supplemental Material Section 4. Despite the limitations of the pilot study, we believe the high degree of apparent treatment diet differentiation, the relatively high average weight loss across both treatment arms, and the interesting findings of risk factor changes at 3 and 6 months are results worthy of dissemination.
In conclusion, our pilot study achieved substantial differentiation of Low-Fat vs. Low-Carb study diets in a free-living population that led to an average weight loss of 9% body weight over 6 months in overweight adults and adults with obesity. Our findings did not detect differential effects by diet, by insulin resistance status, or the interaction of these conditions. Further research on a larger study population for a longer period of time is warranted using the novel dietary intervention approach developed here.
Supplementary Material
What is already known about this subject?
In the majority of published weight loss studies contrasting low-fat to low-carbohydrate diets, when participants are simply randomized to one of the two diets, the reported weight loss differences are often similar.
In a small number of studies, when baseline insulin resistance status was taken into consideration, a differential weight loss response to low-fat vs. low-carbohydrate diets has been reported.
Dietary adherence, differentiation of study diets, more than minimal weight loss achievement, and study retention are challenging aspects of diet weight loss studies.
What does this study add?
This study used a novel approach to dietary achievement that resulted in a high degree of study diet differentiation and treatment adherence, as well as high and equal study retention in both diet groups.
The average weight loss of 9% body weight in this free-living study population was higher than that achieved in many other free-living population studies.
Unlike many previous studies, both the low-fat and the low-carbohydrate groups were given equally challenging goals, with an equal and strong emphasis on overall dietary quality; and all participants were assessed for glucose and insulin dynamics by oral glucose tolerance test both pre- and post-intervention.
In this pilot study there was no statistically significant difference in weight loss by diet group, insulin resistance status, or in the interaction of diet and insulin resistance status. Given that substantial average weight loss was achieved on both diets, this may be explained by the strong emphasis on diet quality (e.g., avoidance of added sugar and refined carbohydrate) for both diet groups, and/or the small sample size.
Acknowledgments
RC and CG conceived and carried out the study. KK, LO and JH analyzed the data. All authors contributed to writing the paper and had final approval of the submitted and published versions. Additionally we would like to acknowledge Antonella Dewell, Josephine Hau and Taylor Saunders for coordinating the implementation of the study and for data collection, Jessica Kubo for her contribution to statistical analysis and data management, Alana Koehler for her technical support, and all of the research participants without whom the study would not have been possible.
Grant Support:
This investigation was supported by funds from the Hass Avocado Board, by NIH grant 1 K12 GM088033, by an unrestricted grant from the Nutrilite Health Institute, and by Human Health Service grant M01-RR00070, General Clinical Research Centers, National Center for Research Resources, National Institutes of Health.
Clinicaltrials.gov: NCT01661426
Footnotes
Mr. Kapphahn and Ms. Cherin have nothing to disclose.
References
- 1.Centers for Disease Control and Prevention. Overweight and obesity [Webpage] 2014 [updated September 9, 2014]. Available from: http://www.cdc.gov/obesity/data/adult.html.
- 2.McLaughlin T, Abbasi F, Lamendola C, Reaven G. Heterogeneity in the prevalence of risk factors for cardiovascular disease and type 2 diabetes mellitus in obese individuals: effect of differences in insulin sensitivity. Arch Intern Med. 2007;167:642–648. doi: 10.1001/archinte.167.7.642. [DOI] [PubMed] [Google Scholar]
- 3.Reaven GM. The insulin resistance syndrome: definition and dietary approaches to treatment. Annu Rev Nutr. 2005;25:391–406. doi: 10.1146/annurev.nutr.24.012003.132155. [DOI] [PubMed] [Google Scholar]
- 4.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res. 1998;6(Suppl 2):51S–209S. [PubMed] [Google Scholar]
- 5.Agatston A. The South Beach Diet. St Martin’s Griffin; 2005. [Google Scholar]
- 6.Atkins RC. Dr Atkins’ New Diet Revolution. Harper; 2009. [Google Scholar]
- 7.Sears B. The Zone: A Dietary Road Map. Regan Books; 1995. [Google Scholar]
- 8.Cornier MA, Donahoo WT, Pereira R, Gurevich I, Westergren R, Enerback S, et al. Insulin sensitivity determines the effectiveness of dietary macronutrient composition on weight loss in obese women. Obes Res. 2005;13:703–709. doi: 10.1038/oby.2005.79. [DOI] [PubMed] [Google Scholar]
- 9.Ebbeling CB, Leidig MM, Feldman HA, Lovesky MM, Ludwig DS. Effects of a low-glycemic load vs low-fat diet in obese young adults: a randomized trial. JAMA. 2007;297:2092–2102. doi: 10.1001/jama.297.19.2092. [DOI] [PubMed] [Google Scholar]
- 10.McClain AD, Otten JJ, Hekler EB, Gardner CD. Adherence to a low-fat vs. low-carbohydrate diet differs by insulin resistance status. Diabetes Obes Metab. 2013;15:87–90. doi: 10.1111/j.1463-1326.2012.01668.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McLaughlin T, Carter S, Lamendola C, Abbasi F, Yee G, Schaaf P, et al. Effects of moderate variations in macronutrient composition on weight loss and reduction in cardiovascular disease risk in obese, insulin-resistant adults. Am J Clin Nutr. 2006;84:813–821. doi: 10.1093/ajcn/84.4.813. [DOI] [PubMed] [Google Scholar]
- 12.Pittas AG, Das SK, Hajduk CL, Golden J, Saltzman E, Stark PC, et al. A low-glycemic load diet facilitates greater weight loss in overweight adults with high insulin secretion but not in overweight adults with low insulin secretion in the CALERIE Trial. Diabetes Care. 2005;28:2939–2941. doi: 10.2337/diacare.28.12.2939. [DOI] [PubMed] [Google Scholar]
- 13.Boden G, Sargrad K, Homko C, Mozzoli M, Stein TP. Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes. Ann Intern Med. 2005;142:403–411. doi: 10.7326/0003-4819-142-6-200503150-00006. [DOI] [PubMed] [Google Scholar]
- 14.Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA. 2002;287:2414–2423. doi: 10.1001/jama.287.18.2414. [DOI] [PubMed] [Google Scholar]
- 15.Ludwig DS, Majzoub JA, Al-Zahrani A, Dallal GE, Blanco I, Roberts SB. High glycemic index foods, overeating, and obesity. Pediatrics. 1999;103:E26. doi: 10.1542/peds.103.3.e26. [DOI] [PubMed] [Google Scholar]
- 16.Pawlak DB, Kushner JA, Ludwig DS. Effects of dietary glycaemic index on adiposity, glucose homoeostasis, and plasma lipids in animals. Lancet. 2004;364:778–785. doi: 10.1016/S0140-6736(04)16937-7. [DOI] [PubMed] [Google Scholar]
- 17.Pereira MA, Swain J, Goldfine AB, Rifai N, Ludwig DS. Effects of a low-glycemic load diet on resting energy expenditure and heart disease risk factors during weight loss. JAMA. 2004;292:2482–2490. doi: 10.1001/jama.292.20.2482. [DOI] [PubMed] [Google Scholar]
- 18.Rodin J. Insulin levels, hunger, and food intake: an example of feedback loops in body weight regulation. Health Psychol. 1985;4:1–24. doi: 10.1037//0278-6133.4.1.1. [DOI] [PubMed] [Google Scholar]
- 19.Sallis JF, Haskell WL, Wood PD, Fortmann SP, Rogers T, Blair SN, et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 20.Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. Clin Chem. 1974;20:470–475. [PubMed] [Google Scholar]
- 21.Sampson EJ, Demers LM, Krieg AF. Faster enzymatic procedure for serum triglycerides. Clin Chem. 1975;21:1983–1985. [PubMed] [Google Scholar]
- 22.Warnick GR, Albers JJ. A comprehensive evaluation of the heparin-manganese precipitation procedure for estimating high density lipoprotein cholesterol. J Lipid Res. 1978;19:65–76. [PubMed] [Google Scholar]
- 23.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 24.Morgan CR, Lazarow A. Immunoassay of insulin: two antibody system: plasma insulin levels in normal, sub diabetic, and diabetic rats. Diabetes. 1963;12:115–126. [Google Scholar]
- 25.Lott JA, Turner K. Evaluation of Trinder’s glucose oxidase method for measuring glucose in serum and urine. Clin Chem. 1975;21:1754–1760. [PubMed] [Google Scholar]
- 26.Trinder P. Determination of blood glucose using an oxidase-peroxidase system with a non-carcinogenic chromogen. J Clin Pathol. 1969;22:158–161. doi: 10.1136/jcp.22.2.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.King AC, Sallis JF, Dunn AL, Simons-Morton DG, Albright CA, Cohen S, et al. Overview of the Activity Counseling Trial (ACT) intervention for promoting physical activity in primary health care settings. Activity Counseling Trial Research Group. Med Sci Sports Exerc. 1998;30:1086–1096. doi: 10.1097/00005768-199807000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Arumugam V, Lee JS, Nowak JK, Pohle RJ, Nyrop JE, Leddy JJ, et al. A high-glycemic meal pattern elicited increased subjective appetite sensations in overweight and obese women. Appetite. 2008;50:215–222. doi: 10.1016/j.appet.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Lennerz BS, Alsop DC, Holsen LM, Stern E, Rojas R, Ebbeling CB, et al. Effects of dietary glycemic index on brain regions related to reward and craving in men. Am J Clin Nutr. 2013;98:641–647. doi: 10.3945/ajcn.113.064113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu AG, Most MM, Brashear MM, Johnson WD, Cefalu WT, Greenway FL. Reducing the glycemic index or carbohydrate content of mixed meals reduces postprandial glycemia and insulinemia over the entire day but does not affect satiety. Diabetes Care. 2012;35:1633–1637. doi: 10.2337/dc12-0329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shikany JM, Margolis KL, Pettinger M, Jackson RD, Limacher MC, Liu S, et al. Effects of a low-fat dietary intervention on glucose, insulin, and insulin resistance in the Women’s Health Initiative (WHI) Dietary Modification trial. Am J Clin Nutr. 2011;94:75–85. doi: 10.3945/ajcn.110.010843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ebbeling CB, Swain JF, Feldman HA, Wong WW, Hachey DL, Garcia-Lago E, et al. Effects of dietary composition on energy expenditure during weight-loss maintenance. JAMA. 2012;307:2627–2634. doi: 10.1001/jama.2012.6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


