Abstract
Background
Each year, around one out of two nursing home (NH) residents are hospitalized in France, and about half to the emergency department (ED). These transfers are frequently inappropriate. This paper describes the protocol of the FINE study. The first aim of this study is to identify the factors associated with inappropriate transfers to ED.
Methods/design
FINE is a case-control observational study. Sixteen hospitals participate. Inclusion period lasts 7 days per season in each center for a total period of inclusion of one year. All the NH residents admitted in ED during these periods are included. Data are collected in 4 times: before transfer in the NH, at the ED, in hospital wards in case of patient's hospitalization and at the patient's return to NH. The appropriateness of ED transfers (i.e. case versus control NH residents) is determined by a multidisciplinary team of experts.
Results
Our primary objective is to determine the factors predisposing NH residents to inappropriate transfer to ED. Our secondary objectives are to assess the cost of the transfers to ED; study the evolution of NH residents' functional status and the psychotropic and inappropriate drugs prescription between before and after the transfer; calculate the prevalence of potentially avoidable transfers to ED; and identify the factors predisposing NH residents to potentially avoidable transfer to ED.
Discussion
A better understanding of the determinant factors of inappropriate transfers to ED of NH residents may lead to proposals of recommendations of better practice in NH and would allow implementing quality improvement programs in the health organization.
Keywords: Inappropriate transfer, Nursing home resident, Emergency department transfer, Potentially avoidable transfer, Appropriateness of transfer, Inappropriate hospitalization
1. Introduction
According to the data of the French nursing homes (NH) research network, 13.5% of NH residents are hospitalized every 3 months and around 50% per year [1]. These hospitalizations concern for half, transfers to Emergency Departments (ED). Previous works [2], [3], [4], [5] confirm this intense flow between NH and ED.
Transfers to ED potentially expose NH residents to iatrogenic complications such as pressure ulcer, confusion, falls [6], [7], functional decline [5], [8], [9], [10] and an increased risk of death [11]. It could be an excessive risk-taking for the resident, an increased risk of patient's care disruption and also important additional health costs [12]. Thus, in this specific population, transfer to ED may frequently have an unfavorable risk-benefit balance. On the other hand, choosing not to transfer a NH resident, who needs and will benefit of ED care is also an unacceptable loss of opportunity for the resident.
In the FINE pilot study [13] performed in anticipation of this project, we found that 43% of NH residents were transferred to ED for inappropriate reasons.
Inappropriate transfer to ED can be defined by the absence of somatic or psychiatric emergency and/or palliative care known before transferring to ED and/or the presence of advance directives for non-hospitalization in the resident's file. It's a clinical situation that could be managed by other means than transfer to ED without loss of opportunity for the patient.
Previous studies have identified factors determining orientation to ED of NH residents based on variables collected in ED medical charts. This results in a truncated and incomplete vision of the problem. However, the reasons of inappropriate ED transfer of NH resident are multiple and more likely to seek in the NH setting, the organization of the primary health care system and the traditional hospitalization services.
The INTERACT (Interventions to Reduce Acute Care Transfers) project demonstrated that specific tools and strategies designed to assist NH staff can reduce hospital transfers and result in significant cost saving [14]. Recently, the IQUARE intervention study (Impact of a QUAlity approach on the development of practical and functional decline of REsidents in NH) [15] demonstrated that a quality approach and the development of a partnership between medical staff of NH and geriatric hospitals significantly reduces transfers to ED.
Our hypothesis is that inappropriate transfers to the ED of NH residents could be reduced by modulating factors accessible to interventions such as the organization of the NH care system and primary care and/or by improving the management of chronic conditions in NH residents. We also hypothesize that the cost of inappropriate transfers to the ED is considerable.
The first aim of the FINE study is to determine the factors predisposing NH residents to inappropriate transfer to ED. Our secondary objectives are to assess the cost of the transfers to ED; study the evolution of NH residents' functional status, psychotropic and inappropriate drugs prescription between before and after the transfer; calculate the prevalence of potentially avoidable transfers to ED; and identify the factors predisposing NH residents to potentially avoidable transfer to ED.
2. Methods
2.1. Study design
The FINE study has obtained approval from the ethics committee, the “Committee for the Protection of Persons and Competent Authority” (CPP) of Bordeaux (SOOM III, 29 may 2015). In order to identify the factors predisposing NH residents to inappropriate transfer to ED, we carry out an observational, multicenter, case-control study (clinicaltrials.gov, NCT02677272). We include all NH residents referred to ED in the study during inclusion period and an expert team defines the transfers as inappropriate (case) or appropriate (control) after the end of the follow-up of the NH resident. By comparing the characteristics of residents and NH as well as the circumstances of transfer between “cases” and “controls”, we will be able to identify the factors significantly associated with inappropriate transfers.
To maximize the representativeness of the sample of NH residents (rural and urban), the Toulouse University Hospital and a representative sample of hospitals (n = 15/25) of the Midi-Pyrénées region [Corresponding to the greatest General Hospital Centers of this region] participate in recruitment. Inclusion period lasts 28 days in each center (7 days per season) for a total period of inclusion of one year. In order to respect the daily, weekly and seasonal variations, the study is conducted over 7 days (24 h a day, including a Monday, a Tuesday, a Wednesday, a Thursday, a Friday, a Saturday and a Sunday) per season. During the inclusion period, all the NH residents admitted in ED are included in the FINE study. Data collection is carried out by clinical research technicians specifically allocated to this task.
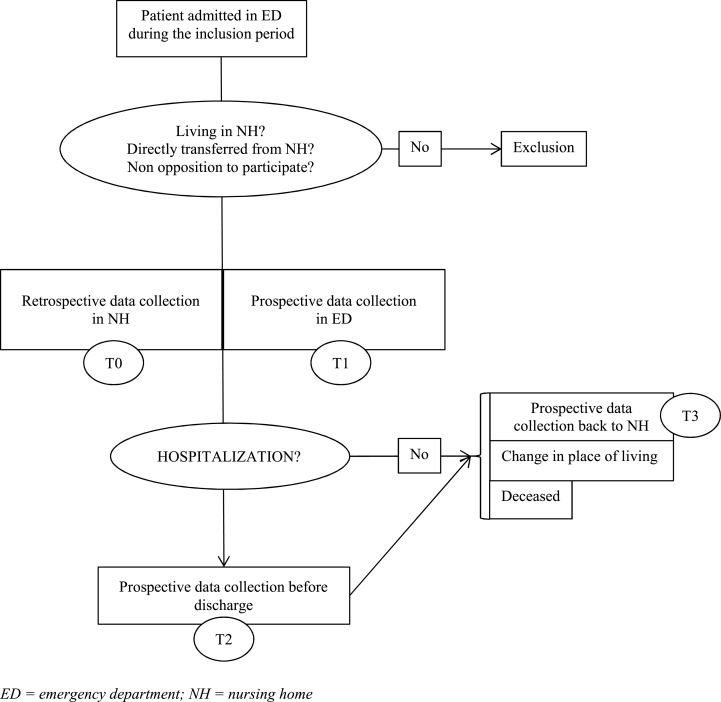
For each resident included, medical and non-medical data are collected in 4 times (Fig. 1): before transfer to ED in the NH (T0), at the ED (T1), in hospital wards (in case of patient's hospitalization) (T2) and at the patient's return to NH (T3). The reports and documents about the circumstances of residents' transfer made by NH and emergency medical assistance (transfer letter, emergency liaison record, drug prescription, transporter form) and reports made by ED and other hospital wards are collected exhaustively.
Fig. 1.
FINE study data collection procedure.
Residents participate in the study according to the length of their stay in hospital (emergency arrival until discharge from the hospital) and 7 days after their return to NH. This duration may vary from a few hours in case of an ED visit to several days if the resident is hospitalized. If the resident deceases during his participation in the study, the cause of death is collected.
2.2. Participants
All patients living in NH admitted directly to ED of the hospitals participating in the study during the inclusion period are included in the study. The non-inclusion criteria are: living in structures other than NH (i.e. sheltered housing, seniors' residences, housing homes, retirement homes, and long-term care units) or in the community; not being transferred directly from NH to ED; have been previously included in FINE study; opposition to participate. As FINE is an observational study, patient's informed consent is not required. Participants are informed and included in case of non-opposition. The inclusion period started in January 2016 with an expected duration of 12 months. The exhaustive recruitment of all NH residents transferred to the ED of the 16 hospitals participating in the FINE study during the inclusion period is estimated at 1004 patients.
2.3. Data collection
The variables are collected at 4 times (Fig. 1): retrospectively by phone call to the NH for T0, and prospectively at ED (T1), in hospital wards if concerned (T2) and back to NH (T3). List of the variables collected during FINE are summarized in Table 1. Our aim is to obtain extensive knowledge of the whole resident's care pathway.
Table 1.
Variables collected at the 4 times.
|
T0 Before transfer retrospective |
|
|
T1 At ED (inclusion) prospective |
|
|
T2 In hospital ward (If concerned) prospective |
|
|
T3 Back to NH prospective |
|
ACSD = Ambulatory Care-Sensitive Diagnosis; ADL = Activities of Daily Living [individuals' ability to execute 6 activities of daily living – score ranges from 0 (low function, dependent) to 6 (not disabled, independent)]; ED = emergency department; GP = general practitioner; NH = nursing home.
2.4. Outcome measures
2.4.1. Primary outcome measure
The first aim of the study is to identify the factors predisposing NH residents to inappropriate transfer to ED. To properly identify these factors, the very important and critical step is the classification of transfers in inappropriate (case) and appropriate (control) groups. In the FINE study, the classification is realized by a panel of experts. Currently, no validated tool or scale exists to define the appropriateness of an ED transfer. Thus, in our work, the appropriateness of the ED transfers of all centers is determined in a standardized approach by a unique expert team composed of eight members: two geriatricians, two emergency physicians, two general practitioners working in NH (coordinating physicians) and two pharmacists. The team can start appraising the transfers, if at least one member of each specialty is present. To avoid variation of judgment based on the members present, one of the geriatricians (AP) is inevitably present in all meetings.
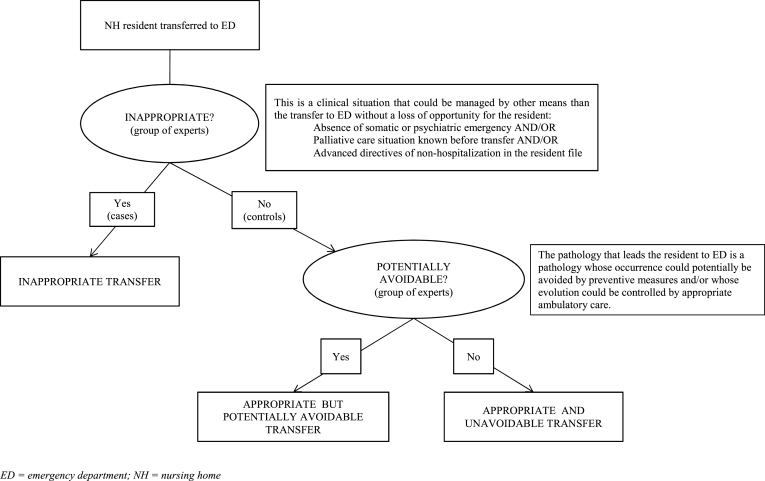
Inappropriate transfer to ED is defined in the FINE study as the absence of somatic and psychiatric emergency conditions and/or palliative care known before decision to transfer and/or the presence of advance directives of non-hospitalization in the resident's medical NH chart. This is a clinical situation that could be managed by other means than the transition to ED without loss of opportunity for the resident.
To judge the appropriateness of the transfer to ED, the group of experts uses, as a support, a standardized procedure (Fig. 2). The expert group has only access to the information concerning the NH resident that is available to the emergency physicians. It contains very necessary NH resident's medical information before transfer at T0 (like his/her medical history and treatment excluding contextual and NH organization data which are the variables of central interest in this study) and the information related to the time spent in the ED at T1. To avoid influencing the ranking, the expert group will not have access to the variables collected at T2 and T3. Thus, the appropriateness of an ED transfer is defined without knowledge of the potential determinants analyzed.
Fig. 2.
Appropriateness and potential avoidability of the NH resident transfer to ED.
In practice, the meetings are held every two weeks. The data about each ED transfer are analyzed by the group. Individual and independent rating divergences are discussed to reach a concerted evaluation of the clinical situation by the group and to score the ED transfer as appropriate or inappropriate. In case of lack of full agreement, vote is taken. Reasons for disagreement between experts are collected.
2.4.2. Secondary outcome measures
2.4.2.1. Cost of transfers to ED
The costs of transfers to ED will be assessed by the direct medical costs (inpatient stay, medical and paramedical acts, medication) and some non-medical costs (transportations) associated with the transfer to the ED. Moreover, the patients' healthcare cost will be recorded over a 12-month period (6 months before and 6 months after the first ED transfer). The economic evaluation will be carried out from the point of view of the payer, health insurance. Medical costs will be obtained from the French National Healthcare Insurance System.
2.4.2.2. Evolution of NH residents' functional status
Residents' functional status is assessed using Katz’ Activity of Daily Living (ADL) scale [16]. The data are collected prior to the acute episode that resulted in the transfer to the emergency department (T0), at the end of the hospitalization (if the resident is hospitalized) (T2) and within 7 days after the patient's return to the NH (T3). The evolution of the ADL score will be assessed between before (T0) and after the ED transfer (T3) separately in each group.
2.4.2.3. Evolution of psychotropic drugs and inappropriate drugs prescription
Medical prescriptions are collected at T0, T1, T2 and T3. A specific focus is done on psychotropic and inappropriate drugs prescription. The evolution of the number of psychotropic and inappropriate drugs prescribed before (T0) and after the ED transfer (T3) will be assessed separately in each group. The inappropriate drugs for elderly are identified according to the Summary of Product Characteristics (SPC), the EU(7) PIM-list [17], the good clinical practice guidelines for the elderly from the French Health Agencies [18] and the Alert and Mastering Indicators of Iatrogenesis [19].
2.4.2.4. Prevalence of potentially avoidable transfers to ED
The prevalence of potentially avoidable transfers to ED will be reported. When a transfer is considered appropriate, it also can be considered as potentially avoidable, if adequate preventive measures have not been implemented to prevent the transfer. When a transfer is considered inappropriate, it is always considered as potentially avoidable (Fig. 2).
The transfer is considered potentially avoidable if the pathology that leads the resident to ED is a pathology whose occurrence could potentially be avoided by implementation of preventive measures and/or whose evolution could be controlled by appropriate ambulatory care. It may be an acute episode or a chronic disease decompensating. The Ambulatory Care Sensitive Conditions (ACSC-9) list (Table 2) is usually used in the literature [20] to characterize hospitalizations as potentially avoidable. This list has been widely used to define potentially avoidable hospitalization. We use this list to characterize the transfers to ED as potentially avoidable. Based on our previous works (FINE pilot) and because the ACSC is not specifically dedicated for ED transfer of NH resident, we have completed this list by conditions frequently reported in NH residents and which are potentially avoidable: falls, fractures, iatrogenic drug effects, inadequate treatments, suboptimal palliative treatment.
Table 2.
Ambulatory care-sensitive conditions.
| Medical condition | ICD-9-CM |
|---|---|
| Grand mal seizure disorders | 780.3; 345 |
| Severe ear, nose, and throat infections | 382; 462; 463; 465; 472.1 |
| Tuberculosis | 011–018 |
| Chronic obstructive pulmonary disease | 491; 492; 494; 496; 466 |
| Bacterial pneumonia | 481; 482.2; 482.3; 482.9; 483; 468 |
| Asthma | 493 |
| Congestive heart failure | 428; 518.4 |
| Hypertension | 401.0; 401.9; 402.0; 402.1; 402.9 |
| Angina | 411.1; 411.8; 413 |
| Cellulitis | 681; 682; 683; 686 |
| Diabetes with ketoacidosis or hyperosmolar coma | 250.1–250.3 |
| Diabetes with specified complications | 250.8–250.9 |
| Diabetes without specified complications | 250.0 |
| Hypoglycemia | 251.2 |
| Gastroenteritis | 558.9 |
| Kidney/urinary tract infection | 590; 599.0; 599.9 |
| Dehydration | 276.5 |
| Iron-deficiency anemia | 280.1; 280.8; 280.9 |
| Nutritional deficiency | 260-262; 268.0–268.1 |
| Dental conditions | 521-523; 525; 528 |
Source: Adapted from Millman M (Ed.): Access to Health Care in America. Committee on Monitoring Access to Personal Health Care Services. Institute of Medicine. Washington, DC: National Academy Press, 1993.
This task is performed by the expert group and is based on the final diagnosis at ED. If the final diagnosis at ED has no link with the reason for transfer, the expert group assessment is based on the associated diagnosis linked to the reason for transfer. Reasons for disagreement between experts are collected.
3. Statistical analysis
Statistical analyses will be performed using STATA software 11.2 (STATA Corp., College Station, TX, USA).
3.1. Sample size
In the FINE pilot study [13], 43% of transfers to the ED of NH residents were considered inappropriate. The exhaustive recruitment of all NH residents transferred to the ED of the 16 hospitals participating in the FINE study during the inclusion period is estimated at 1004 patients. Thus, 432 transfers to ED out of 1004 estimated should be observed as inappropriate (cases). This number is compatible with a robust analysis of the factors independently associated with inappropriate transfers to the ED, in accordance with the methodological standards that recommend a minimum of 10 inappropriate transfers by variable of the multivariate model [21], [22]. Indeed, the power sample size will authorize the analysis of 43 factors.
3.2. Analysis of the main objective
The analysis of factors predisposing to inappropriate transfer to ED will be based, first, on the comparison, between cases and controls, of percentages (chi2 or Fisher exact test according to expected numbers) for qualitative variables and on the comparison of means (Student test if normality and equal variances) or distributions (nonparametric Mann-Whitney test) for quantitative variables (in bivariate analysis). Factors that will be assessed were listed in Table 1 (variables measured at T0 concerning NH data, resident data with functional status and the circumstances of transfer with day of the week, time of the day and season).
Then, in order to assess independent factors predisposing to inappropriate transfer to ED, we will conduct logistic regression models. The initial logistic regression model will be composed of variables found associated with an inappropriate transfer to ED with a P-value <0.20 in bivariate analysis. A backward analysis will be then applied until only variables significantly and independently associated with an inappropriate transfer to ED (P-value <0.05) remained. Interactions between independent covariates will be tested in each backward selection step. All reported P-values were two-sided and the significance threshold was set at <0.05. None imputation has been planned in case of missing data. Nevertheless, missing data will be coded as missing data for the logistic regression model in order to not penalize the power of the analyses.
3.3. Analysis of secondary objectives
The estimated cost of transfers (i.e. appropriate and inappropriate) and the costs of care 6 months before and 6 months after the first transfer will be described by the mean, standard deviation and extreme values. Moreover, a comparison of care costs before and after the first transfer will be achieved. It will be based on the use of statistical tests in paired series (Student test or Wilcoxon).
The comparison of the residents' functional status (score ADL) between before and after the transfer to ED will be based on tests in paired series (Student test or Wilcoxon).
The number of psychotropic and inappropriate drugs will be compared between before (T0) and after the transfer to ED (T3) using statistical tests in paired series (Student test or Wilcoxon).
The estimation of the prevalence of NH residents' potentially avoidable transfers to ED will be expressed with its 95% confidence interval. The analysis of factors predisposing to a potentially avoidable ED transfer will be based on the same methodology as used for the analysis of the main objective.
All reported P-values will be two-sided and a p-value < 0.05 will be considered significant.
4. Discussion
Avoiding inappropriate transfer to ED of the NH resident may reduce the risk of hospital-acquired conditions such as functional decline, morbi-mortality and health care expenditure. FINE will result in better understanding of the determinants factors of inappropriate transfers to ED of NH residents. Based on these results, FINE final objective is to initiate quality improvement measures to reduce the number of unnecessary ED transfer and promote better care for NH resident. FINE is an essential requirement to implement an optimization of the flow of residents between NH and ED and thus improve the care system. The originality of our project is to consider the entire trajectory of NH residents, from NH, before their transfer to ED, in the ED and hospital unit, and back to the NH. The second strength of FINE is to accurately determine the cost of transfers to ED of NH residents. We believe that FINE will allow us to lead targeted actions with health regulators/competent authorities and health policy makers. Finally, the analysis of potentially avoidable transfers will also allow recommending preventive intervention and better practice to implement in NH.
Numerous studies have investigated the rate and reason of inappropriate hospitalization (IH) or potentially avoidable/preventable hospitalization (PAH/PPH) of NH residents. IH or PAH/PPH are usually defined by opinion of an expert panel [23], [24], coding of diagnosis (ACSD) [12], [25], [26], [27], [28], the appreciation of an emergency doctor [29] or a primary care physician [30]. All these approaches are open to criticisms (administrative data approach, assessment based on one physician opinion). These works usually highlighted the high rate of IH or PAH/PPH. The various definitions result in prevalence of IH up to 40% [23] and between 13.1% [31] to 67% for PAH/PPH [32].
On the other hand, the studies that investigated the reasons of inappropriateness of the transfers to ED of NH residents are scare and none have been performed in France.
Numerous definitions for inappropriate or avoidable/preventable transfer to ED are available. Some authors used emergency criteria to judge the appropriateness such as transfer classification of the ambulance transfer and emergency physician opinion [33]. Stephens et al. studied ED visit and ACSC ED visit in subgroups of NHR [34], [35]; Bergman considered in his study [29] that only ED transfers leading to hospitalization were appropriate.
The lack of consensual definition of appropriateness of transfers to ED of NH resident is a potential limitation of our research. However, our approach is based on current available data of the literature and we believe that the methodological protocol and the tools used by the expert panel will result in clinically relevant characterization of the NH residents. In a population of 54 NH residents in the FINE pilot study, we found a rate of inappropriate transfers to ED of NH residents of 43%. This rate is similar to the one reported by Saliba et al., in 2000 [23] in the United States. Various factors related to inappropriate hospitalization have been reported in the literature. Factors are related to the patient's condition like functional status, comorbidities or cognitive impairment [18], [36], [37], [38]. Other factors are related to contextual conditions: strong request of hospitalization from the formal or informal caregiver, poor assessment of care in nursing homes, lack of collegial decision recorded on reasonable limitation of care, detrimental nature of hospitalization for patient comfort [39] or financial considerations [40]. In the FINE pilot study, we demonstrated in a small sample of NH resident transferred to the ED that poor functional status, pressure ulcer, short life expectancy, lack of technical means in NH for monitoring and treatment and urgent need for complementary exams were statistically significant factors that may be improved by adequate quality improvement measures. We believe that the current FINE study will confirm these encouraging results and investigate a larger number of factors that may also be accessible to future intervention to reduce the number of inappropriate ED transfers.
The FINE study is an observational study that not allows the demonstration of causality association. Over-interpretation of our results will be discussed and mitigated in regards to the current knowledge. The strength of FINE is to be able to investigate in a large sample of NH residents and probably a large number of factors potentially accessible to intervention. The health economic variables collected in this research could give further arguments to improve this health care organization. FINE may open the discussion about redistribution of financial resources to NH and optimize the upstream care pathway and the NH residents care management.
Inappropriate transfers of NH resident to ED should be avoided to reduce the risk of pejorative events and the health related cost associated with these inadequate cares. We believe that the FINE study would contribute to implement new strategies of care for NH residents. The results of the FINE study would facilitate new programs, and reduce unnecessary risk of iatrogenic complications, functional decline and mortality.
5. Conclusion
A better understanding of the determinants of inappropriate transfers to ED of NH residents would allow implementing quality improvement program. The final objective of the FINE study is to optimize the flow of residents between NH and ED and thus to improve the health care policy. Reasons of the dysfunction are certainly multiple. The strength and originality of our project is first to consider the entire trajectory of the NH residents, from NH to the ED, during the hospitalization, until return to NH. Second, the medico-economic study will provide relevant information to health regulators/competent authorities and health policy makers, which may lead to proposals of recommendations of best practice in NH. First results are expected in 2018.
Funding
This study was supported by a grant from the French Ministry of Health (Programme de recherche sur la performance du système de soins; PREPS 2014, 14-0185).
Sponsor's role
The Toulouse University Hospital Center is the sponsor of the FINE study (CHU Toulouse; 15 7464 06) and is responsible of regulatory affairs and contracts with study sites.
Competing interest
The authors have no conflict of interest to declare that could appear to have influenced this submitted work.
Acknowledgements
The authors thank the Midi-Pyrenees Regional Direction of Medical Service, the Midi-Pyrenees Regional Health Agency and the Research and Innovation Direction of the Toulouse University Hospital. They also thank all the geriatrician investigators, emergency physicians and clinical research associates who participated to this research: Albi Hospital Center (W. Bouzid PhD, S. Laborie MD, J. Meunier MD); Auch Hospital Center (M. Camallières MD, V. Sarda MD); Ariège Couserans Hospital Center (F. Castéra MD, F. Del Mazo MD); Bigorre Hospital Center (S. Benech MD, F. Huchet MD, Y. Gasnier MD, C. Périssé); Cahors Hospital Center (V. Kostek MD, C. Quénec'hdu, M. Oberlin MD); Castelsarrasin Moissac Hospital Center (M. Bersou MD, L. Brignol MD); Castres-Mazamet Hospital Center (N. Boulogne, MN. Cufi MD, N. Lagoutte MD); Jean Coulon Hospital Center (A. Hustache MD, J. Mac MD); Lannemezan Hospital Center (S. Bordes MD, L. Dugas MD); Lavaur Hospital Center (C. Blatge MD, C. Lapasse, A. Sebbane MD); Lourdes Hospital Center (S. Cottin MD, M. Péré-Saun MD); Montauban Hospital Center (C. Iché MD, N. Lafarge, V. Régniez, A. Roustan MD); Rodez Hospital Center (D. Kaya-Vaur MD, A. Pereira MD); Saint Gaudens Hospital Center (E. Deweerdt MD, P. Montastier MD); Toulouse University Hospital Center (E. Paez, D. Pennetier PhD, A. Lendrieux); Val d’Ariège Hospital Center (L. Bories MD, ES. Friederich MD, Y. Herades). They also thank all the nursing home professionals who contributed to this study.
References
- 1.Rolland Y., Abellan van Kan G., Hermabessiere S., Gerard S., Guyonnet Gillette S., Vellas B. Descriptive study of nursing home residents from the REHPA network. J. Nutr. Health Aging. 2009;13:679–683. doi: 10.1007/s12603-009-0197-4. [DOI] [PubMed] [Google Scholar]
- 2.Briggs R., Coughlan T., Collins R., O'Neill D., Kennelly S.P. Nursing home residents attending the emergency department: clinical characteristics and outcomes. QJM. 2013;106:803–808. doi: 10.1093/qjmed/hct136. [DOI] [PubMed] [Google Scholar]
- 3.Jensen P.M.1, Fraser F., Shankardass K., Epstein R., Khera J. Are long-term care residents referred appropriately to hospital emergency departments? Can. Fam. Physician. 2009;55:500–505. [PMC free article] [PubMed] [Google Scholar]
- 4.Ingarfield S.L., Finn J.C., Jacobs I.G., Gibson N.P., Holman C.D., Jelinek G.A., Flicker L. Use of emergency departments by older people from residential care: a population based study. Age Ageing. 2009;38:314–318. doi: 10.1093/ageing/afp022. [DOI] [PubMed] [Google Scholar]
- 5.Rolland Y., Andrieu S., Crochard A. Psychotropic drug consumption at admission and discharge of nursing home residents. J. Am. Med. Dir. Assoc. 2012;13 doi: 10.1016/j.jamda.2011.12.056. 407.e7-407.e12. [DOI] [PubMed] [Google Scholar]
- 6.Rothschild J.M., Bates D.W., Leape L.L. Preventable medical injuries in older patients. Arch. Intern Med. 2000;160:2717–2728. doi: 10.1001/archinte.160.18.2717. [DOI] [PubMed] [Google Scholar]
- 7.Sari A.B., Cracknell A., Sheldon T.A. Incidence, preventability and consequences of adverse events in older people: results of a retrospective case-note review. Age Ageing. 2008;37:265–269. doi: 10.1093/ageing/afn043. [DOI] [PubMed] [Google Scholar]
- 8.Wilber S.T., Blanda M., Gerson L.W., Allen K.R. Short-term functional decline and service use in older emergency department patients with blunt injuries. Acad. Emerg. Med. 2010;17:679–686. doi: 10.1111/j.1553-2712.2010.00799.x. [DOI] [PubMed] [Google Scholar]
- 9.Creditor M.C. Hazards of hospitalization of the elderly. Ann. Intern Med. 1993;118:219–223. doi: 10.7326/0003-4819-118-3-199302010-00011. [DOI] [PubMed] [Google Scholar]
- 10.Covinsky K.E., Palmer R.M., Fortinsky R.H. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J. Am. Geriatr. Soc. 2003;51:451–458. doi: 10.1046/j.1532-5415.2003.51152.x. [DOI] [PubMed] [Google Scholar]
- 11.Launay C.P., Annweiler C., de Decker L., Kabeshova A., Fantino B., Beauchet O. Risk of in-hospital mortality following emergency department admission: results from the geriatric EDEN cohort study. J. Nutr. Health Aging. 2014;18:83–86. doi: 10.1007/s12603-013-0038-3. [DOI] [PubMed] [Google Scholar]
- 12.Grabowski D.C., 0'Malley A.J., Barhydt N.R. The costs and potential savings associated with nursing home hospitalizations. Health Aff. 2007;26:1753–1761. doi: 10.1377/hlthaff.26.6.1753. [DOI] [PubMed] [Google Scholar]
- 13.Binot I., Tavassoli N., Berard E., Perrin A., Bismuth S., Giovanni E., Lafourcade A., Vellas B., Rolland Y. Nursing home residents in emergency department: risk factors of inappropriate or potentially avoidable transfers. Results of FINE pilot study. J. Nurs. Home Res. 2017;3:28–37. [Google Scholar]
- 14.Ouslander J.G., Lamb G., Tappen R. Interventions to reduce hospitalizations from nursing homes: evaluation of the INTERACT II collaborative quality improvement project. J. Am. Geriatr. Soc. 2011;59:745–753. doi: 10.1111/j.1532-5415.2011.03333.x. [DOI] [PubMed] [Google Scholar]
- 15.de Souto Barreto P., Lapeyre-Mestre M., Mathieu C., Piau C., Bouget C., Cayla F., Vellas B., Rolland Y. A multicentric individually-tailored controlled trial of education and professional support to nursing home staff: research protocol and baseline data of the IQUARE study. J. Nutr. Health Aging. 2013;17:173–178. doi: 10.1007/s12603-013-0008-9. [DOI] [PubMed] [Google Scholar]
- 16.Katz S., Ford A., Moskowitz R. The index of ADL: a standardised measure of biological and psychosocial function. JAMA. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 17.Renom-Guiteras A., Meyer G., Thürmann P.A. The EU(7)-PIM list: a list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur. J. Clin. Pharmacol. 2015;71:861–875. doi: 10.1007/s00228-015-1860-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fiche points clés, organisation des parcours : prendre en charge une personne âgée polypathologique en soins primaires. HAS. 2015 http://www.has-sante.fr/portail/upload/docs/application/pdf/2015-04/fiche_parcours_polypathologie_du_sujet_age.pdf (accessed september 29 2016) [Google Scholar]
- 19.The Alert and Mastering Indicators of Iatrogenesis (AMI) proposed by HAS. http://www.has-sante.fr/portail/jcms/c_1250626/fr/indicateurs-de-pratique-clinique-ipc-pmsa. (accessed september 29 2016).
- 20.Becker M.A., Boaz T.L., Andel R. Predictors of preventable nursing home hospitalizations: the role of mental disorders and dementia. Am. J. Geriatr. Psychiatry. 2010;18:475–482. doi: 10.1097/JGP.0b013e3181b2145a. [DOI] [PubMed] [Google Scholar]
- 21.Concato J., Feinstein A.R., Holford T.R. The risk of determining risk with multivariable models. Ann. Intern Med. 1993;118:201–210. doi: 10.7326/0003-4819-118-3-199302010-00009. [DOI] [PubMed] [Google Scholar]
- 22.Harrel F.E., Jr., Lee K.L., Matchar D.B. Regression models for prognostic prediction: advantages, problems, and suggested solutions. Cancer Treat. Rep. 1985;69:1071–1077. [PubMed] [Google Scholar]
- 23.Saliba D., Kington R., Buchana J. Appropriateness of the decision to transfer nursing facility residents to hospital. J. Am. Geriatr. Soc. 2000;48:154–163. doi: 10.1111/j.1532-5415.2000.tb03906.x. [DOI] [PubMed] [Google Scholar]
- 24.Ouslander J.G., Perloe M., Givens J.H. Reducing potentially avoidable hospitalizations of nursing home residents: results of a pilot quality improvement project. J. Am. Med. Dir. Assoc. 2009;10:644–652. doi: 10.1016/j.jamda.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 25.Intrator O., Zinn J., Mor V. Nursing home characteristics and potentially preventable hospitalizations of long-stay residents. J. Am. Geriatr. Soc. 2004;52:1730–1736. doi: 10.1111/j.1532-5415.2004.52469.x. [DOI] [PubMed] [Google Scholar]
- 26.Walker J.D., Teare G.F., Hogan D.B. Identifying potentially avoidable hospital admissions from Canadian long-term care facilities. Med. Care. 2009;47:250–254. doi: 10.1097/MLR.0b013e3181847588. [DOI] [PubMed] [Google Scholar]
- 27.Young Y., Inamdar S., Dichter B.S. Clinical and nonclinical factors associated with potentially preventable hospitalizations among nursing home residents in New York State. J. Am. Med. Dir. Assoc. 2011;12:364–371. doi: 10.1016/j.jamda.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 28.Becker M., Boaz T., Andel R. Predictors of avoidable hospitalizations among assisted living residents. J. Am. Med. Dir. Assoc. 2012;13:355–359. doi: 10.1016/j.jamda.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 29.Bergman H., Clarfield M. Appropriateness of patient transfer from a nursing home to an acute-care hospital: a study of emergency room visits and hospital admissions. J. Am. Geriatr. Soc. 1991;45:302–306. doi: 10.1111/j.1532-5415.1991.tb03568.x. [DOI] [PubMed] [Google Scholar]
- 30.Hanger H.C., Fletcher V., Sidwell A. Acute medical admissions for older people from residential care facilities: are they appropriate? N. Z. Med. J. 2011;124:24–32. [PubMed] [Google Scholar]
- 31.Finn J.C., Flicker L., Mackenzie E. Interface between residential aged care facilities and a teaching hospital emergency department in Western Australia. Med. J. Aust. 2006;184:432–435. doi: 10.5694/j.1326-5377.2006.tb00313.x. [DOI] [PubMed] [Google Scholar]
- 32.Ouslander J.G., Lamb G., Perloe M. Potentially avoidable hospitalizations of nursing home residents: frequency, causes, and costs. J. Am. Geriatr. Soc. 2010;58:627–635. doi: 10.1111/j.1532-5415.2010.02768.x. [DOI] [PubMed] [Google Scholar]
- 33.Jones J.S., Dwyer P.R., White L.J. Patient transfer from nursing home to emergency department: outcomes and policy implications. Acad. Emerg. Med. 1997;4:908–915. doi: 10.1111/j.1553-2712.1997.tb03818.x. [DOI] [PubMed] [Google Scholar]
- 34.Stephens C.E., Newcomer R., Blegen M. Emergency department use by nursing home residents: effect of severity of cognitive impairment. Gerontologist. 2012;52:383–393. doi: 10.1093/geront/gnr109. [DOI] [PubMed] [Google Scholar]
- 35.Stephens C.E., Sackett N., Govindarajan P., Lee S.J. Emergency department visits and hospitalizations by tube-fed nursing home residents with varying degrees of cognitive impairment: a national study. BMC Geriatr. 2014;4:35. doi: 10.1186/1471-2318-14-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Payne R.A., Abel G.A., Guthrie B. The effect of physical multimorbidity, mental health conditions and socioeconomic deprivation on unplanned admissions to hospital: a retrospective cohort study. CMAJ. 2013;185:E221–E228. doi: 10.1503/cmaj.121349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Somme D., Cauterman M., Huet B., Durand-Gasselin B., Saint-Jean O. Inappropriateness of hospital use in two acute geriatrics department: description of the phenomenon and analysis of risk factors. Rev. Med. Interne. 2007;28:818–824. doi: 10.1016/j.revmed.2007.05.034. [DOI] [PubMed] [Google Scholar]
- 38.Somme D., Saint-Jean O., Cauterman M., Huet B., Durand-Gasselin B. Appropriateness of hospitalisation use: about the difference between productivity and health efficiency. Rev. Med. Interne. 2008;29:437–438. doi: 10.1016/j.revmed.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 39.Ouslander J.G., Berenson R.A. Reducing unnecessary hospitalizations of nursing home residents. N. Engl. J. Med. 2011;365:1165–1167. doi: 10.1056/NEJMp1105449. [DOI] [PubMed] [Google Scholar]
- 40.Grabowski D.C., Stewart K.A., Broderick S.M. Predictors of nursing home hospitalization: a review of the literature. Med. Care Res. Rev. 2008;65:3–39. doi: 10.1177/1077558707308754. [DOI] [PubMed] [Google Scholar]