Abstract
Background
Acute pain is among the leading causes of referral to the emergency department (ED) in industrialized countries. Its management mainly depends on intensity. Moderate-to-severe pain is treated with intravenous (IV) administered opioids, of which morphine is the most commonly used in the ED. We have estimated the burden of IV administration of morphine in the five key European countries (EU5) using a micro-costing approach.
Scope
A structured literature review was conducted to identify clinical guidelines for acute pain management in EU5 and clinical studies conducted in the ED setting. The data identified in this literature review constituted the source for all model input parameters, which were clustered as analgesic (morphine), material used for IV morphine administration, nurse workforce time and management of morphine-related adverse events and IV-related complications.
Findings
The cost per patient of IV morphine administration in the ED ranges between €18.31 in Spain and €28.38 in Germany. If costs associated with the management of morphine-related adverse events and IV-related complications are also considered, the total costs amount to €121.13–€132.43. The main driver of those total costs is the management of IV-related complications (phlebitis, extravasation and IV prescription errors; 73% of all costs) followed by workforce time (14%).
Conclusions
IV morphine provides effective pain relief in the ED, but the costs associated with the IV administration inflict an economic burden on the respective national health services in EU5. An equally rapid-onset and efficacious analgesic that does not require IV administration could reduce this burden.
Keywords: acute pain, analgesia, cost analysis, emergency departments, Europe, morphine, nurse, opioids, pain management
Introduction
Acute pain is one of the leading causes of referral to an emergency department (ED), accounting for more than two-thirds of these visits [1,2]. Acute pain can be caused by a large spectrum of conditions including trauma, renal colic, abdominal pain and myocardial infarction, among others. Despite all the advances in its diagnosis and treatment, management of acute pain in the ED still remains a challenge; pain is often under-recognized and undertreated, and in busy EDs, initiation of treatment may be delayed [3]. Current guidelines recommend analgesia for moderate and severe pain to be initiated within 20 minutes of arrival in the ED [3], but this is not always feasible. In the French multicenter PALIERS study, the time between arrival at the ED and initiation of treatment with an analgesic drug was 60 minutes for 38% (379/988) of patients with acute pain [4].
Intensity of pain (typically defined as mild, moderate or severe), along with patient need and initial response to analgesia, helps guide its treatment [5]. Although oral analgesia is often used to manage pain that is considered mild to moderate in severity, moderate-to-severe acute pain may frequently be managed with intravenous (IV) administered opioids. Although rectal nonsteroidal anti-inflammatory drugs are also recommended in a regional guideline in the UK for severe pain [6], per regional guidelines from the UK and Spain, IV opioid analgesics remain the mainstay treatment to control acute pain in the ED and when needed, they are supplemented with oral analgesics [6–10]. The need to administer analgesia via the IV route in moderate-to-severe pain can also delay initiation of pain relief, particularly in patients with difficult IV access. Although placement of an IV catheter by a nurse is successfully achieved for the majority of patients, in certain cases such as obesity, elderly patients or vasoconstriction brought on by shock, cannulation may need to be conducted with the assistance of ultrasonographic guidance, which substantially delays IV access. Placement of an IV catheter – which, by its nature, is more time-consuming and complex [11] compared with administration of, for example, orally administered drugs – in these patients may take between 30 minutes and 2 hours [12].
Nurse-administered IV morphine is the most commonly used analgesic method for moderate-to-severe pain in the ED in the five key European countries (EU5 [France, Germany, Italy, Spain and the UK]). However, fewer than a handful of studies have assessed the costs associated with this modality of administering analgesia in the ED setting. The studies conducted to date had either a US [13,14] or Hong Kong [15] perspective; none had a European focus. The aim of this study was to measure the costs associated with nurse-administered IV morphine for the management of acute pain in the ED setting in EU5. Costs were estimated for each of these countries using a micro-costing analysis.
Methods
Costs of IV morphine administration in the ED are not readily available from any public database. Therefore, a structured literature review was conducted to identify all the data needed for the micro-costing analysis. The literature review aimed to identify clinical guidelines for the management of moderate-to-severe acute pain in the ED setting in the EU5 and providing a comprehensive list of the interventional and observational ED studies on acute pain. All searches were performed in PubMed and Google, and included the following concepts: ‘acute pain’, ‘intravenous morphine’ and ‘emergency department or room’. Google searches additionally included use of local languages (e.g. ‘guía práctica del manejo del dolor en urgencias’ [Spain] and ‘prise en charge de la douleur aux urgencies’ [France]).
At the time our search was conducted (2016), we were able to identify six regional and two national European guidelines. Regional guidelines included four from the UK [6,8–10], one from Spain [7] and one from France [16]. National guidelines included one from Spain [17] and one from Italy [18]. The interventional and observational studies that were identified represented a cross-section of European and other countries, including four of the five EU5 countries (France, Italy, Spain and the UK) (Table 1).
Table 1.
Summary of noncosts input parameters.
| Costing input | Input parameter | # Studies | Sample size | Reference source (region) | |
|---|---|---|---|---|---|
| Practice guidelines R=regional N=national |
Clinical studies | ||||
| Drug | |||||
| Morphine | 10-mg dose | 7 | 914 | [6,8–10] (UK–R) [7] (Spain–R) [17] (Spain–N) [16] (France–R) [18] (Italy–N) |
[19–21] (US) [22] (UK) [23] (France) [24] (New Zealand) [25] (Malaysia) |
| Materials | |||||
| IV cannula infusion set | 1.3 units | 7 | 3414 | [12,26] (US) [27–29] (France) [30] (Australia) [31] (Spain) |
|
| Draw-up needles | 2 units | - | - | [6,8–10] (UK–R) [7] (Spain–R) [17] (Spain–N) [16] (France–R) [18] (Italy–N) |
|
| Syringe (10 mL) | 1 unit | - | - | [6,8–10] (UK–R) [7] (Spain–R) [17] (Spain–N) [16] (France–R) [18] (Italy–N) |
|
| Saline (100 mL) for dilution | 1 unit | - | - | [6,8–10] (UK–R) [7] (Spain–R) [17] (Spain–N) [16] (France–R) [18] (Italy–N) |
|
| Prefilled (10 mL) saline syringe | 1 unit | - | - | [6,8–10] (UK–R) [7] (Spain–R) [17] (Spain–N) [16] (France–R) [18] (Italy–N) |
|
| Workforce | |||||
| Cannulation | 5.4 mins | 4 | 1011 | [12,26] (US) [27,28] (France) |
|
| Drug preparation | 7.9 mins | 2 | 121 | [15] (Hong Kong) [32] (UK) |
|
| Flushing | 2.0 mins | 1 | 35 | [33] (Australia) | |
| Drug administration | 14.8 mins | 4 | 720 | [15] (Hong Kong) [19,34,35] (US) |
|
| Patient monitoring | 14.0 mins | - | - | [6,8–10] (UK–R) [7] (Spain–R) |
|
| Management of adverse events (rate) | |||||
| Nausea | 12.1% | 14 | 1443 | [19–21,34–38] (US) [22] (UK) [39–41] (Iran) [42] (France) [43] (Belgium) |
|
| Vomiting | 5.8% | 11 | 906 | [19,21,34,35,37,38] (US) [22] (UK) [42] (France) [40,44] (Iran) [43] (Belgium) |
|
| Hypotension | 2.1% | 8 | 1154 | [20,37,38] (US) [42] (France) [40,44] (Iran) [45] (Australia) [46,47] (Turkey) |
|
| Respiratory depression | 1.1% | 9 | 1710 | [22] (UK) [20,38] (US) [23,41] (France) [24] (New Zealand) [45] (Australia) [46,47] (Turkey) |
|
| IV complication treatment (rate) | |||||
| Phlebitis | 2.6% | 1 | 1498 | [48] (Italy) | |
| Extravasation | 0.4% | 4 | 102,204 | [49,50] (US) [51] (Brazil) [52] (Japan) |
|
| Harmful IV prescribing errors | 1.2% | 1 | 330 | [53] (UK) | |
The data for each input parameter as well as the sources of these data are provided in the table above. The column titled # studies provides the number of studies used as the source of the input parameter. The column titled sample size provides the total number of patients included in the source studies.
IV, intravenous; mins, minutes; UK, United Kingdom; US, United States.
The model developed in Microsoft Excel estimated the costs associated with the management of an average patient with moderate-to-severe acute pain of any origin with nurse-administered IV morphine in the ED from a national health service perspective. The input categories were as follows: analgesic administered IV, workforce time spent on IV morphine administration and monitoring the patient, material needed for the IV administration, adverse events reported during administration of IV morphine and complications of IV administration (Table 1). Unit prices and costs included in the model were country-specific and adjusted to 2016 euros (Table 2). The only exception was costs for management of respiratory depression [54] and of IV prescription errors [55], which were derived from US costs because no data were identified in the literature review for Europe.
Table 2.
Summary of costs data inputs.
| Costs per unit in 2016 euros | |||||
|---|---|---|---|---|---|
| FR | DE | IT | ES | UK | |
| Drug | |||||
| Morphine (10 mg) | 0.88 | 1.56 | 0.63 | 0.30 | 1.20 |
| Material | |||||
| Cannula infusion seta | 0.21 | 1.13 | 0.41 | 1.36 | 0.85 |
| Draw-up needlea | 0.12 | 0.08 | 0.05 | 0.04 | 0.07 |
| Syringea | 0.29 | 0.24 | 0.03 | 0.08 | 0.04 |
| Saline for dilutiona | 3.12 | 2.76 | 2.00 | 1.56 | 1.49 |
| Prefilled saline syringe for line flushinga | 0.80 | 1.07 | 0.67 | 0.28 | 0.43 |
| Workforce | |||||
| Cost per minute of nurse time | 0.46 | 0.49 | 0.48 | 0.32 | 0.25 |
| Adverse events | |||||
| Nauseab | 9.41 | 11.76 | 9.24 | 6.11 | 5.13 |
| Vomitingb | 17.09 | 19.81 | 17.22 | 11.45 | 9.23 |
| Hypotensionb | 5.00 | 5.17 | 6.22 | 3.85 | 3.66 |
| Respiratory depressionb,c | 796 | 796 | 796 | 796 | 796 |
| IV complications | |||||
| Phlebitisb | 2.79 | 4.14 | 3.15 | 3.54 | 2.48 |
| IV prescription errorsb,c | 7622 | 7622 | 7622 | 7622 | 7622 |
| Extravasationb | 2.79 | 4.14 | 3.15 | 3.54 | 2.48 |
Costs are given as 2016 euros adjusted costs.
Costs are given per unit.
Costs are given per episode.
These costs were derived from US sources unlike all other costs which were country-specific.
DE, Germany; ES, Spain; FR, France; IT, Italy; IV, intravenous; UK, United Kingdom.
Based on seven ED studies (914 patients) [19–25] and in line with recommendations from the regional and national European guidelines [6–10,16–18], patients received up to 10 mg of morphine in the model (Table 1). The cost of morphine included in the model was its ex-VAT public selling price in 2016 in EU5. The model considers that morphine is administered as four doses as part of a typical dose-titration procedure [6–10,16–18]. IV morphine is prepared by the dilution of 1 mL morphine (10 mg/mL) with 9 mL saline (0.9%), in a syringe.
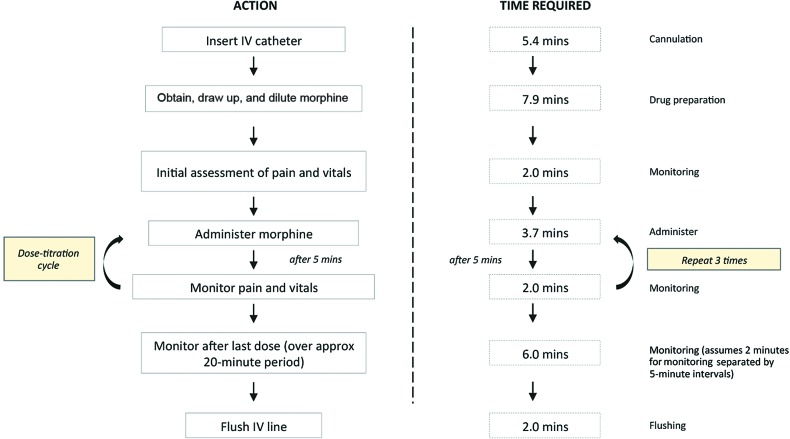
Regarding workforce (i.e. nurses), the time needed to administer IV morphine was estimated based on the regional clinical guidelines from the UK [6,8–10], Spain [7] and ED studies [12,15,19,26–28,32–35] identified in the structured literature review. The inputs that constituted the cost of workforce in the micro-costing model were the costs of nursing time for the following procedures: cannulation, drug preparation, drug administration, patient monitoring and flushing of the IV line (Figure 1). The per-minute cost of nurse time was calculated from available annual, monthly or hourly salaries based on the assumption that 40 hours per week were worked for 47 weeks per calendar year. Salaries were adjusted to 2016 using each country’s consumer price index (Table 1). We assume that nurses spend an average of 4.1 minutes per IV cannulation attempt, based on four ED studies (1011 subjects) [12,26–28]. Also based on ED studies (n=3414 patients) [12,26–31], we assume that each patient has 1.3 IV attempts. Nurses spend 7.9 minutes for drug preparation based on two studies that assessed the average time required to prepare a solution for IV injection via a syringe [15,32]. The amount of time spent by a nurse on drug administration (i.e. 3.7 minutes) was derived from four studies (720 subjects) that monitored the amount of time needed to administer a single IV bolus of morphine in the ED [15,19,34–35]. This time is in line with the 4 to 5 minutes recommended in the label of morphine [56]. None of the identified clinical studies detailed the time needed for patient monitoring, therefore, assumptions based on regional clinical guidelines from the UK [6,8–10] and Spain [7] were made. According to these guidelines, patients’ vital signs (including heart rate, blood pressure, oxygen saturation and respiratory rate) and pain relief should be monitored before, during and after morphine administration. We estimated that a nurse would spend 2 minutes checking a patient’s vital signs and/or pain levels. As shown in Figure 1, the time spent monitoring would be 2 minutes prior to the first morphine dose, an additional 2 minutes before each dose during dose titration and 2 minutes every 5 minutes over a 22-minute period after the last morphine dose. The average amount of time spent by a nurse on IV flushing was derived from one Australian study [33] that assessed the time required by nurses to prepare and administer prefilled saline flush solutions to 35 patients in a laboratory setting; an average of 2 minutes was reported. We consider that flushing is performed only once, before the first dose of morphine is administered and that the nurse needs 2 minutes. When considering all the steps where nurses time themselves, the total nurse time needed for each IV morphine administration including time to monitor the patient is 44 minutes.
Figure 1.
Procedure of IV morphine administration in the ED setting.
All time values in the figure correspond to those required per patient. Example, it was assumed that time for cannulation is 4.1 minutes, but given that patients would have an average of 1.3 attempts, the total time for cannulation is 5.4 minutes per patient.
ED, emergency department; IV, intravenous; mins, minutes.
The inputs that constituted the cost of materials in the micro-costing model were for the following items: a cannula infusion set, draw-up needles, a syringe, saline and a prefilled saline flush syringe. For each of these materials, costs taken were based on prices paid by EU5 hospitals. Where this was not possible, prices were obtained from medical equipment suppliers, which is one of the limitations of our analysis. A cannula infusion set was assumed to be required per attempt. Therefore, a total of 1.3 cannulation sets was required per patient. In addition, two draw-up needles (one for saline and one for morphine) and a single 10 mL syringe were required to prepare the morphine solution per patient. To prepare the solution, one 100 mL bag of saline (the smallest common pack size in countries within scope) was estimated per patient; consequently, this cost includes wastage for saline. In contrast, a prefilled saline flush syringe was used for flushing.
The micro-costing model also included the cost of management of key adverse events associated with IV administration of morphine. The adverse events included in the model were nausea, vomiting, hypotension and respiratory depression. Probability of experiencing any of these events was derived from ED studies where a comparable IV morphine dose was administered also in the ED. As shown in Table 1, the probability of nausea was derived from 14 studies (1443 patients) [19–22,34–43], vomiting from 11 studies (906 patients) [19,21,22,34,35,37,38,40,42–44], hypotension from nine studies (1154 patients) [20,37,38,40,42,44–47] and severe respiratory depression from nine studies (1710 patients) [20,22–24,38,41,45–47]. These probabilities were 0.121, 0.058, 0.021 and 0.011, respectively. Onset of nausea and/or vomiting was treated with antiemetic therapy. For simplicity, all patients with nausea or vomiting received metoclopramide in our model. Based on its label [57], 10 mg (one 2 mL ampoule of 5 mg/mL) of metoclopramide was given IV. This administration required two draw-up needles (one for metoclopramide and one for saline), one 10 mL syringe and one prefilled saline flush syringe. No additional costs were included for the saline needed for preparing the metoclopramide solution, as it is assumed that saline is taken from the 100 mL bag used for preparing the morphine solution. Nursing time associated with the treatment of IV-morphine induced nausea and vomiting was derived from Eberhart et al. [58], a German study (149 subjects) that measured the time spent by nurses to treat episodes of nausea and/or vomiting in a general ward. Time for management of nausea and vomiting was 16.9 and 33.4 minutes, respectively. Management of hypotension consisted of administering saline [20]. The cost of one 1000 mL saline bag for infusion was included in the model. We assumed that the saline administration required 5.4 minutes from a nurse [59]. Finally, the cost of management of severe respiratory depression was derived from Kane-Gill et al. [54].
Complications associated with IV administration of drugs were also included in our model. The inputs that constituted the cost of IV-related complications in the micro-costing model were the costs associated with the risk of developing the following complications due to IV administration: phlebitis, extravasation and the harmful events following IV prescribing errors. No studies that assessed the incidence of phlebitis in the ED were identified. In lieu of this data, the incidence of phlebitis was derived from one clinical study (1498 subjects) [48] where the occurrence of phlebitis within 24 hours of catheter insertion was monitored across medical and surgical wards (the emergency room was not considered as a ‘location’) in an Italian hospital. Based on this study, the probability of phlebitis was set as 0.026 in the model. Probability of extravasation after morphine administration was derived from four clinical studies (102,204 subjects) [49–52] that assessed extravasation after the administration of either IV contrast or chemotherapeutics. The probability was 0.004. Probability of IV morphine prescribing errors is based on the findings of Davies et al. [53], which examined prescription errors across type of opioid and route of administration. The authors report an incidence of 1.2% for potentially lethal prescribing errors. In the model, we assume that management of phlebitis and extravasation consists of inserting a new IV catheter. The costs associated with phlebitis and extravasation included both the materials and workforce costs of inserting a new IV catheter. The cost of treating harmful medication errors was derived from Abraham et al. [55].
The materials used during management of adverse events or IV complications are not included in the costs of materials, as they are already included in the costs of management of adverse events. Similarly, costs of nurse time dedicated in the management of adverse events and IV complications are considered in the costs of adverse events and IV complications, respectively, and not in the costs of workforce time.
Results
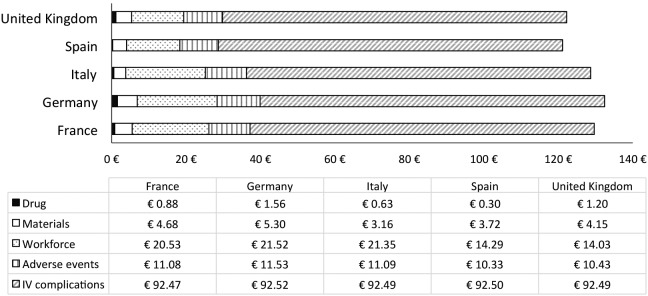
As shown in Table 3 and Figure 2, the costs for all model input parameters were comparable across the EU5 countries. The costs of IV administration of morphine ranged from €18.31 per patient in Spain to €28.38 per patient in Germany. Of these costs, those associated with the time nurses spend to administer the morphine and monitor patients during and after morphine administration are the highest (between €14 [€14.03 in the UK and €14.29 in Spain] and €21–€22 [€21.35 in Italy and €21.52 in Germany]). In terms of workforce costs, the prominent ones were the costs associated with drug administration (€4.71 per patient in the UK to €7.23 per patient in Germany) and monitoring of the patient (€4.45 per patient in the UK to €6.83 per patient in Germany). The costs of morphine were the lowest ones in all countries with a cost ranging between €0.30 per patient in Spain and €1.56 per patient in Germany. Costs of material ranged between €3.16 in Italy and €5.30 in Germany (per patient).
Table 3.
Average cost per patient.
| Costing input | Cost in 2016 euros | ||||
|---|---|---|---|---|---|
| FR | DE | IT | ES | UK | |
| Drug | |||||
| Morphine | 0.88 | 1.56 | 0.63 | 0.30 | 1.20 |
| Materials | |||||
| IV cannula infusion set | 0.28 | 1.51 | 0.55 | 1.79 | 1.46 |
| Draw-up needles | 0.25 | 0.16 | 0.10 | 0.07 | 0.17 |
| Syringe (10 mL) | 0.29 | 0.24 | 0.03 | 0.08 | 0.06 |
| Saline (100 mL) for dilution | 3.06 | 2.32 | 1.81 | 1.50 | 1.91 |
| Prefilled (10 mL) saline syringe | 0.80 | 1.07 | 0.67 | 0.27 | 0.56 |
| Workforce | |||||
| Cannulation | 2.51 | 2.63 | 2.61 | 1.75 | 1.71 |
| Drug preparation | 3.68 | 3.85 | 3.82 | 2.56 | 2.51 |
| Flushing | 0.93 | 0.98 | 0.97 | 0.65 | 0.64 |
| Drug administration | 6.90 | 7.23 | 7.17 | 4.80 | 4.71 |
| Patient monitoring | 6.52 | 6.83 | 6.78 | 4.54 | 4.45 |
| Management of adverse events | |||||
| Nausea | 1.13 | 1.42 | 1.11 | 0.74 | 0.79 |
| Vomiting | 1.00 | 1.16 | 1.01 | 0.67 | 0.69 |
| Hypotension | 0.10 | 0.11 | 0.13 | 0.08 | 0.10 |
| Respiratory depression | 8.84 | 8.84 | 8.84 | 8.84 | 8.84 |
| IV complications treatment | |||||
| Phlebitis | 0.07 | 0.11 | 0.08 | 0.09 | 0.08 |
| Extravasation | 0.01 | 0.02 | 0.01 | 0.01 | 0.01 |
| Harmful IV prescribing errors | 92.39 | 92.39 | 92.39 | 92.39 | 92.39 |
| Aggregated costs | |||||
| Drug administrationa | 26.09 | 28.38 | 25.14 | 18.31 | 19.37 |
| Adverse events and IV complications | 103.56 | 104.04 | 103.58 | 102.83 | 102.91 |
| Total | 129.64 | 132.43 | 128.72 | 121.13 | 122.28 |
Drug administration costs include the costs of drug, material and workforce and exclude any costs due to management of adverse events or IV-related complications.
DE, Germany; ES, Spain; FR, France; IT, Italy; IV, intravenous; UK, United Kingdom.
Figure 2.
Average costs per patient and country.
IV, intravenous.
When we include the contribution of costs associated with management of adverse events and of IV complications, the total costs associated with morphine IV administration for moderate-to-severe acute pain in the ED setting ranged between €121.13 per patient in Spain to €132.43 per patient in Germany. Costs of management of IV complications were the main driver of our model and account for 73% of the total costs (Figure 3). Regarding these costs, the prominent component was the costs of IV prescription errors (€92.39 per patient). Costs of phlebitis (€0.07– €0.11 per patient) and extravasation (€0.01–€0.02 per patient) were only marginal.
Figure 3.
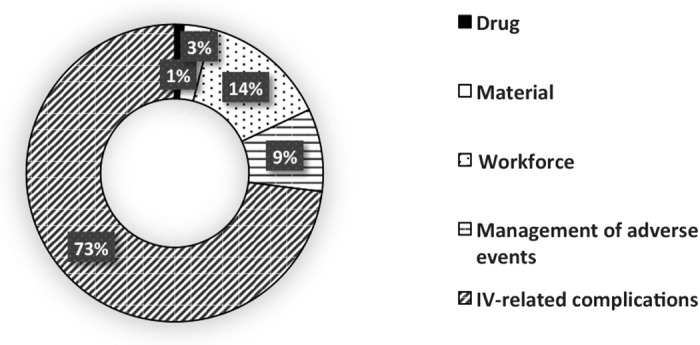
Contribution of the different model components.
IV, intravenous.
The total costs associated with the management of key adverse events of IV morphine, including phlebitis, injection site pain and infections associated with IV administration, ranged between €10.33 per patient in Spain to €11.53 per patient in Germany. The adverse event associated with highest costs was severe respiratory depression (€8.84 per patient). Costs of nausea and vomiting were significantly lower than those of respiratory depression and primarily driven by the time nurses spend to manage these patients.
Discussion
The current micro-costing analysis highlights the economic burden inflicted by administration of IV morphine for moderate-to-severe acute pain in the ED setting in the EU5 countries. The cost of IV morphine administration for acute pain in the ED ranged between €18 and €28 per patient in the EU5 when considering the costs of the analgesic, material and workforce (which includes nursing time, training and effort). These costs amount to between €121 and €132 per patient when also including the contribution of management of adverse events and IV complications.
Although acute pain is one of the leading causes of referral to ED, very few studies have assessed the economic burden of its management in this setting, with only three of these studies focusing on nurse-administered IV analgesia [13–15]. The approach and input parameters estimated in these three studies differ from ours and also among themselves. The first study compares the costs of nurse-administered IV ketorolac and IV morphine in the ED [15]. The study conducted in the ED of a large hospital in Hong Kong included the costs of drugs, nurse workforce time and adverse events collected in their hospital [15]. Similar to our analysis, Rainer et al. considered nausea, vomiting and phlebitis as adverse events of interest, but they also estimated the economic impact of treating drowsiness, sleeping and dizziness in their model [15]. The mean costs per person when excluding subsequent hospital admission was $HK228.80 (€37.13, 2016 values) for patients who received nurse-titrated IV morphine. These costs were $HK43.60 (€7.08, 2016 values) for patients randomized to IV ketorolac. The average total costs estimated by Rainer et al. were lower than ours due to Rainer et al. not considering the cost of the material used for IV administration and importantly, failing to include the contribution of respiratory depression and IV prescription errors [15]. Total costs estimated by Rainer et al. were lower than ours, despite a higher incidence of patients with nausea, vomiting and phlebitis in Rainer et al. Of these adverse events, incidence of phlebitis after IV morphine administration was particularly high in Rainer et al. (27 vs 2.6% in our model).
The second study providing costs for IV morphine was commissioned by Medical Developments International Limited and aimed at comparing the costs of using Penthrox (methoxyflurane given through an inhaler) to those of IV morphine for the treatment of acute pain in the ED [13]. Costs associated with IV morphine amounted to US$33.18 (2008 values; €23.80 when inflated to 2016 values). Costs were estimated based on published literature and primary interviews with ED staff. The input parameters in their model included costs of analgesia, material, workforce time and management of two adverse events (nausea and vomiting). These costs were similar to ours when we excluded costs of respiratory depression and IV prescription errors. However, costs estimated by Medical Developments International Limited [13] were significantly lower than those currently estimated by Palmer et al. [14]. In the model by Palmer et al., the cost of the IV infusion pump (US$37±29; €33.59±26.33; 2016 values) was included, and this was the most costly component [14]. However, the use of infusion pumps is not included in regional and national European clinical guidelines and thus this additional cost burden may likely not be incurred by countries in Europe. In our own personal communications with ED staff from the EU5 countries, infusion pumps, unlike in the United States, are not readily used in the ED for administering IV morphine in Europe.
The adverse events included in our analysis differ from those considered in the other economic studies. To simplify our model, we restricted the adverse events to nausea, vomiting, hypotension and respiratory depression. It can be argued that the latter is more uncommon than the other three. The ED studies identified in the literature showed an incidence of 12.1% for nausea, 5.8% for vomiting, 2.1% for hypotension and 1.1% for respiratory depression. However, despite its low incidence, respiratory depression is one of the most serious adverse events associated with the use of IV morphine and can have devastating outcomes. In line with the clinical relevance of this adverse event, the costs associated with its management, such as nursing costs, monitoring of vital signs and monitoring of oxygen saturation, were the highest among all the modeled adverse events. The other three adverse events were associated with only marginal costs, particularly, hypotension. In our model, we estimate that the cost of treating an episode of nausea would range between €5 and €12 in the EU5 and between €9 and €20 for an episode of vomiting. These costs are lower than those estimated by Eberhart et al. in Germany [58]. The authors estimated the cost of an episode of nausea and/or vomiting that occurred during or after administration of opioid drug, based on the data from 462 inpatients in 16 German hospitals. The costs for an episode of nausea and/or vomiting was estimated as €31±22 when including both the workforce time (€18±14) and materials (€14±13) [58]. The higher costs in Eberhart et al., compared with our estimates, are partly due to inclusion in Eberhart et al. of the costs of material, such as IV lines or gastric tubes, that had to be replaced because of nausea and/or vomiting. These costs were not included in our model.
The main driver of our model was the cost of IV-related complications. Of these, the cost of IV prescription errors had the highest contribution to the total costs. According to the Institute for Safe Medication Practices, opioids are considered to be high-risk medications and medication errors associated with opioids can have serious consequences [60]. Prescription errors are common in hospitals and in the case of opioids, these errors are particularly likely, given the wide variety of drugs, preparations and doses available. The incidence we have modeled for these errors is based on the findings of Davies et al. based on the review of inpatient drug charts in a large UK University teaching hospital [53]. In our model we took a conservative approach and only considered life-threatening errors. In line with this conservative approach, we limited the errors to the prescription ones (e.g. inappropriate opioid) and excluded any dosing errors from nurses. No European-specific data were identified in the literature review regarding the costs of prescription errors for morphine or other types of opioids. Only US costs were identified and these are the ones applied to our analysis. Although the most costly component was IV infusion pumps, which are more commonly used in United States than in Europe, they do represent possible costs in Europe, as EDs become more specialized [61]. These costs were taken from the poster presented by Abraham et al. at the 20th annual meeting of the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) [55]. The authors provide only limited information regarding how these costs were derived from the original estimated by Meissner et al. [62]. Meissner et al. estimated the costs associated with the management of the consequences of different types of errors based on clinical assumptions validated by an expert advisory panel.
We also included two additional types of IV-related complications: extravasation and phlebitis. The costs associated with their management were significantly lower than the costs of IV prescription errors. Morphine is not an irritant drug and therefore, extravasation does not cause any tissue damage [63]. When extravasation occurs, the only action needed is to place a new IV catheter. Regarding phlebitis, we took a conservative approach and assumed that all cases of phlebitis were uncomplicated and therefore, would only require placement of a new IV line. Unlike Rainer et al. [15], who considered phlebitis an adverse event, we included it as an IV-related complication. As already mentioned, in Rainer et al., the incidence of phlebitis was particularly high (27 vs 2.6% in our model) for the ED setting [15]. We have considered that the reported incidence for phlebitis in Rainer et al. is too high to reflect current clinical practice and therefore, this study was not included in the calculation of the incidence of phlebitis.
Limitations of the study
Similar to other economic models, our analysis has a number of limitations. The analysis we have conducted was restricted to morphine only. Although morphine is still the most commonly used opioid for management of moderate-to-severe acute pain in the ED in EU5, more potent opioids such as hydromorphone and fentanyl are gaining popularity [64]. However, these opioids are more expensive than morphine; therefore, the real economic burden of the use of IV opioids as analgesics for acute pain is likely to exceed our estimates. Similarly, we also took a conservative approach by assuming that all patients with an episode of nausea and/or vomiting receive 10 mg of IV metoclopramide rather than more costly antiemetics (e.g. ondansetron), which are also used for opioid-related nausea and vomiting [65]. In contrast, the rebate applied to hospitals for material was not available for all materials and for all countries. When unavailable, we used the costs from suppliers, which may have overestimated these costs. While this is a limitation, it has only a marginal impact, given that material-related costs accounted for less than 5% of the total costs.
While this model did include workforce costs, it is possible these costs were underestimated. Setting up an IV and administering and monitoring opioids may lead to a delay in care for other patients. Delays in patient treatment can lead to increases in patient stay, overcrowding in the ED, increases in adverse events and an overall increase in cost [66]. Therefore, there may be additional tangential costs in IV morphine administration that were not accounted for in this model.
The model was simplified by assuming all patients reach pain relief with a dose of morphine equal or lower than 10 mg. In clinical practice, patients often receive supportive treatment with oral analgesics and in a considerable percentage of patients, doses higher than 10 mg of morphine are needed [6–10,16–18]. An additional limitation of our model is the reduced number of adverse events (n=4) and IV-related complications (n=3) included in the analysis. The model does not reflect the contribution of other adverse events, such as sedation or pruritus, or IV-related complications, such as needle stick injuries. Their inclusion would have equally increased the costs of IV-administered morphine.
Lack of real-world costs for IV administration of morphine in the ED setting in the countries of interest prompted us to conduct a structured literature review to identify all the data needed to calculate these costs. In order to simulate clinical practice in these countries as closely as possible, we prioritized data from observational studies conducted in the ED setting (including in the UK and in France) and the available regional and/or national clinical guidelines in the UK, Spain, Italy and France for the dose of opioids administered in the ED and workforce time. One real but often overlooked cost not included in our model is the time it takes nurses to waste unused morphine. In many institutions, nurses must also take the time to find a second healthcare provider to witness and cosign the proper destruction of the opioid, which likely adds several more minutes for parenteral administration. In addition, all data related to adverse events for IV morphine originated from ED studies where the dose of administered morphine was comparable to that used in our model and related to short exposure to morphine in the ED setting. All costs used in the model were country-specific and inflation adjusted, when needed, to 2016 using each country’s consumer price index. As previously mentioned, there were two exceptions (costs for management of respiratory depression and of opioid prescription errors) because no data were identified in the literature review for the ED in Europe. The costs of respiratory depression were derived from US costs and the modeled rate of prescription errors originates from a single study conducted in a UK University teaching hospital. The authors report rates of prescription errors in wards rather than in the ED [53]. Therefore, this study may not be representative of all EU5 countries. Further, this study did not compare routes of administration; however, a study by Beaudoin et al. showed that the IV administration of opioids in the ED resulted in more medical errors (and harm due to medical errors) than did oral administration [67]. As previously mentioned, the costs for prescription errors in the current study come from a US study [55]. It can be argued that US costs are higher than European costs; however, this was offset by excluding nonharmful events from our analysis. Given these limitations, the costs of prescription errors should be taken with caution.
Our model measures the average cost in the EU5. Although we prioritized inclusion of published data specific for the ED setting, these data may not take into account variability within and across countries. However, our model provides the cost ranges based on European regional and national guidelines [6–10,16–18], as well as studies from four of the five EU5 (France [23,27,28,41,42], Spain [31], the UK [22,53], Italy [48]) and other countries. Costs of administering IV morphine in the ED are likely to be between €10.90–€17.50 (for those patients who are easily cannulated and for whom vitals are not affected) and €18.30–€28.40 (for those patients with difficult IV access and with underlying conditions that may require additional monitoring).
Conclusion
Our model is a simplified representation of actual clinical practice; it informs on the economic burden, including the time and effort required, of nurse-administered IV analgesia with morphine in the ED setting. Nurse time spent on IV administration is the second most important driver in our model after the costs of IV-related complications, even when we use the lowest reported workforce time values. The use of an equally rapid-onset and efficacious analgesic that can be administered using a less burdensome route (e.g. oral, sublingual or inhaled) may reduce the costs of analgesia for moderate-to-severe acute pain in the ED setting.
Acknowledgements
The abstract of this paper was presented at the ISPOR 19th Annual European Congress in Vienna, as a poster presentation with interim findings. The poster’s abstract was published in ‘Poster Abstracts’ in Value Health 2016;19(7):A582; available at http://www.valueinhealthjournal.com/article/S1098-3015(16)32726-7/abstract. Editing assistance was provided by BlueMomentum, an Ashfield Company, part of UDG Healthcare plc and was funded by AcelRx.
Footnotes
Contributions: KD conceived and designed the study, MC and MH conducted the structured literature review and micro-costing analysis. MC drew the outline of the manuscript, and KD, LB, GP, MC and MH drafted the manuscript. All authors analyzed and interpreted the data, critically revised successive drafts of the manuscript and have approved the final version.
Disclosure and potential conflicts of interest: The research described in this article, the drafting of this manuscript and its publication were funded by AcelRx. KD is an employee of AcelRx. The work of IQVIA was funded by AcelRx. MC and MH are consultants to AcelRx. LB and GP are physicians. LB reports honorarium from BBraun Italia, Medtronic and MSD, and GP from AcelRx. The International Committee of Medical Journal Editors (ICMJE) Potential Conflicts of Interests form for the authors are available for download at: http://www.drugsincontext.com/wp-content/uploads/2018/03/dic.212524-COI.pdf
Funding declaration: This research was funded exclusively by AcelRx.
Correct attribution: Copyright © 2018 Casamayor M, DiDonato K, Hennebert M, Brazzi L, Prosen G. https://doi.org/10.7573/dic.212524. Published by Drugs in Context under Creative Commons License Deed CC BY NC ND 4.0.
Provenance: submitted; externally peer reviewed.
Peer review comments to author: 12 February 2018
Drugs in Context is published by BioExcel Publishing Ltd. Registered office: Plaza Building, Lee High Road, London, England, SE13 5PT.
BioExcel Publishing Limited is registered in England Number 10038393. VAT GB 252772009.
For all manuscript and submissions enquiries, contact the Editorial office dic.editorial@bioexcelpublishing.com
For all permissions, rights and reprints, contact David Hughes david.hughes@bioexcelpublishing.com
References
- 1.Cordell WH, Keene KK, Giles BK, Jones JB, Jones EH, Brizendine EJ. The high prevalence of pain in emergency medical care. Am J Emerg Med. 2002;20:165–9. doi: 10.1053/ajem.2002.32643. http://dx.doi.org/10.1053/ajem.2002.32643. [DOI] [PubMed] [Google Scholar]
- 2.Todd KH, Ducharme J, Choiniere M, Crandall CS, Fosnocht DE, Homel P, Tanabe P PEMI Study Group. Pain in the emergency department: results of the pain and emergency medicine initiative (PEMI) multicenter study. J Pain. 2007;8:460–6. doi: 10.1016/j.jpain.2006.12.005. https://doi.org/10.1016/j.jpain.2006.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Todd KH, Sloan EP, Chen C, Eder S, Wamstad K. Survey of pain etiology, management practices and patient satisfaction in two urban emergency departments. CJEM. 2002;4:252–6. doi: 10.1017/s1481803500007478. https://doi.org/10.1017/s1481803500007478. [DOI] [PubMed] [Google Scholar]
- 4.Boccard E, Adnet F, Gueugniaud PY, Filipovics A, Ricard-Hibon A. Prise en charge de la douleur chez l’adulte dans des services d’urgences en France en 2010. Ann Fr Med Urgence. 2011;1:312–9. https://doi.org/10.1007/s13341-011-0094-4. [Google Scholar]
- 5.Macintyre PE, Schug SA, Scott DA, Visser EJ, Walker SM APM: SE Working Group of the Australian and New Zealand College of Anaesthetists and Faculty of Pain Medicine. Acute Pain Management: Scientific Evidence. 3rd ed. Melbourne: ANZCA & FPM; 2010. [Google Scholar]
- 6.Cardiff and Vale University Health board. Pain service guidelines (adult) 2015. [Last accessed 27 March 2018]. Available at https://sydney.edu.au/medicine/pmri/pdf/Acute-pain-management-scientific-evidence-third-edition.pdf.
- 7.Comisión de Farmacia e Terapeutica. Protocolo de morfina parenteral urgencias de atención primaria. 2003. [Last accessed 27 March 2018]. Available at: http://www.sergas.es/gal/documentacionTecnica/docs/Farmacia/XapOurense/InformacionFarmacoTerapeutica/sergaV3N2MorfinaParenteral.PDF. 2003.
- 8.Royal Cornwall Hospitals NHS Trust. Clinical guideline for intravenous morphine administration in clinical areas for adults. 2015. [Last accessed 27 March 2018]. Available at https://doclibrary-rcht.cornwall.nhs.uk/documentslibrary/royalcornwallhospitalstrust/clinical/pain/intravenousmorphineadministrationinclinicalar.pdf.
- 9.Salisbury NHS Foundation Trust. Administration of bolus dose intravenous morphine. 2016. [Last accessed 27 March 2018]. Available at http://www.icid.salisbury.nhs.uk/ClinicalManagement/Pain/Pages/AdministrationofMorphine.aspx.
- 10.Worcestershire Acute Hospitals NHS Trust. Clinical guidelines – Acute Pain Control WAHT-ANA-007.2015. [Last accessed 27 March 2018]. Available at http://www2.worcsacute.nhs.uk/healthprofessionals/clinical-guidelines/?ignoreeveryonegroup=0&assetdet906991=21632&search=acute+pain+control&searchcontent=0.
- 11.ENA. Emergency Nurses Association. Clinical Practice Guideline: Difficult intravenous access. 2015. [Last accessed 27 March 2018]. Available at https://www.ena.org/docs/default-source/resource-library/practice-resources/cpg/difficultivaccesscpg.pdf?sfvrsn=9944da58_8.
- 12.Witting MD. IV access difficulty: incidence and delays in an urban emergency department. J Emerg Med. 2012;42:483–7. doi: 10.1016/j.jemermed.2011.07.030. https://doi.org/10.1016/j.jemermed.2011.07.030. [DOI] [PubMed] [Google Scholar]
- 13.NIHR HSRIC. Horizon Scanning Review. Birmingham: NIHR Horizon Scanning Research & Intelligence Centre; 2016. [Last accessed 27 March 2018]. Methoxyflurane (Penthrox) for emergency relief of moderate to severe pain. Available at http://www.io.nihr.ac.uk/topics/methoxyflurane-penthrox-for-emergency-relief-of-moderate-to-severe-pain/ [Google Scholar]
- 14.Palmer PP, Walker JA, Patanwala AE, Hagberg CA, House JA. Cost of intravenous analgesia for the management of acute pain in the emergency department is substantial in the United States. [Last accessed 27 March 2018];JHEOR. 2017 5:1–15. doi: 10.36469/9793. https://www.jheor.org/other-conditions/237-cost-of-intravenous-analgesia-for-the-management-of-acute-pain-in-the-emergency-department-is-substantial-in-the-united-states. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rainer TH, Jacobs P, Ng YC, Cheung NK, Tam M, Lam PK, Wong R, Cocks RA. Cost effectiveness analysis of intravenous ketorolac and morphine for treating pain after limb injury: double blind randomised controlled trial. BMJ. 2000;321:1247–51. doi: 10.1136/bmj.321.7271.1247. https://doi.org/10.1136/bmj.321.7271.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Galinski M, Adnet F. Prise en charge de la douleur aiguë en médecine d’urgence [Acute pain management in emergency medicine] [Last accessed 9 March 2018];Réanimation. 2007 16:652–9. Available at https://www.srlf.org/wp-content/uploads/2015/11/0711-12-Reanimation-Vol16-N7-8-p652_659.pdf. [Google Scholar]
- 17.Blanco-Tarrío E. Tratamiento del dolor agudo. [Treatment of acute pain]. Medicina de Familia. SEMERGEN. 2010;36:392–8. https://doi.org/10.1016/j.semerg.2010.05.003. [Google Scholar]
- 18.Savoia G, Coluzzi F, Di Maria C, Ambrosio F, Della Corte F, Oggioni R, Messina A, Constantini A, Launo C, Consalvo Mattia, Paoletti F, Lo Presti C, Bertini L, Vito Peduto A, De Iaco F, Schiraldi F, Bussani F, De Vito L, Giagnorio G, Marinangeli F, Coaccioli S, Aurilio C, Valenti F, Bonetti C, Piroli A, Paladini A, Ciccozzi A, Matarazzo T, Marraro G, Paolicchi A, Martino A, De Blasio E, Cerchiari E, Radeschi G. Raccomandazioni Intersocietarie Italiane (SIAARTI, SIMEU, SIS 118, AISD, SIARED, SICUT, IRC) sulla gestione del dolore in emergenza. [Last accessed 9 March 2018]. Available at http://www.aisd.it/e107_files/downloads/raccintersocietarie_it_complete31052014.pdf.
- 19.Birnbaum A, Schechter C, Tufaro V, Touger R, Gallagher EJ, Bijur P. Efficacy of patient-controlled analgesia for patients with acute abdominal pain in the emergency department: a randomized trial. Acad Emerg Med. 2012;19:370–7. doi: 10.1111/j.1553-2712.2012.01322.x. http://dx.doi.org/10.1111/j.1553-2712.2012.01322.x. [DOI] [PubMed] [Google Scholar]
- 20.Fleischman RJ, Frazer DG, Daya M, Jui J, Newgard CD. Effectiveness and safety of fentanyl compared with morphine for out-of-hospital analgesia. Prehosp Emerg Care. 2010;14:167–75. doi: 10.3109/10903120903572301. https://doi.org/10.3109/10903120903572301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Silverman ME, Shih RD, Allegra J. Morphine induces less nausea than meperidine when administered parenterally. J Emerg Med. 2004;27:241–3. doi: 10.1016/j.jemermed.2004.04.011. https://doi.org/10.1016/j.jemermed.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 22.Evans E, Turley N, Robinson N, Clancy M. Randomised controlled trial of patient controlled analgesia compared with nurse delivered analgesia in an emergency department. Emerg Med J. 2005;22:25–9. doi: 10.1136/emj.2002.004614. http://dx.doi.org/10.1136/emj.2002.004614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lvovschi V, Aubrun F, Bonnet P, Bouchara A, Bendahou M, Humbert B, Hausfater P, Riou B. Intravenous morphine titration to treat severe pain in the ED. Am J Emerg Med. 2008;26:676–82. doi: 10.1016/j.ajem.2007.10.025. https://doi.org/10.1016/j.ajem.2007.10.025. [DOI] [PubMed] [Google Scholar]
- 24.O’Connor A, Schug SA, Cardwell H. A comparison of the efficacy and safety of morphine and pethidine as analgesia for suspected renal colic in the emergency setting. J Accid Emerg Med. 2000;17:261–4. doi: 10.1136/emj.17.4.261. http://dx.doi.org/10.1136/emj.17.4.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rahman NH, DeSilva T. A randomized controlled trial of patient-controlled analgesia compared with boluses of analgesia for the control of acute traumatic pain in the emergency department. J Emerg Med. 2012;43:951–7. doi: 10.1016/j.jemermed.2012.02.069. https://doi.org/10.1016/j.jemermed.2012.02.069. [DOI] [PubMed] [Google Scholar]
- 26.Costantino TG, Parikh AK, Satz WA, Fojtik JP. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med. 2005;46:456–61. doi: 10.1016/j.annemergmed.2004.12.026. https://doi.org/10.1016/j.annemergmed.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 27.Lapostolle F, Catineau J, Garrigue B, Monmarteau V, Houssaye T, Vecci I, Tréoux V, Hospital B, Crocheton N, Adnet F. Prospective evaluation of peripheral venous access difficulty in emergency care. Intensive Care Med. 2007;33:1452–7. doi: 10.1007/s00134-007-0634-y. https://doi.org/10.1007/s00134-007-0634-y. [DOI] [PubMed] [Google Scholar]
- 28.Minville V, Pianezza A, Asehnoune K, Cabardis S, Smail N. Prehospital intravenous line placement assessment in the French emergency system: a prospective study. Eur J Anaesthesiol. 2006;23:594–7. doi: 10.1017/S0265021506000202. https://doi.org/10.1017/S0265021506000202. [DOI] [PubMed] [Google Scholar]
- 29.Sebbane M, Claret PG, Lefebvre S, Mercier G, Rubenovitch J, Jreige R, Edledjam JJ, de La Coussaye JE. Predicting peripheral venous access difficulty in the emergency department using body mass index and a clinical evaluation of venous accessibility. J Emerg Med. 2013;44:299–305. doi: 10.1016/j.jemermed.2012.07.051. https://doi.org/10.1016/j.jemermed.2012.07.051. [DOI] [PubMed] [Google Scholar]
- 30.Carr PJ, Rippey JC, Budgeon CA, Cooke ML, Higgins N, Rickard CM. Insertion of peripheral intravenous cannulae in the Emergency Department: factors associated with first-time insertion success. J Vasc Access. 2015;17:182–90. doi: 10.5301/jva.5000487. https://doi.org/10.5301/jva.5000487. [DOI] [PubMed] [Google Scholar]
- 31.Gonzalez López JL, Arribi Vilela A, Fernández del Palacio E, Olivares Corral J, Benedicto Martí C, Herrera Portal P. Indwell times, complications and costs of open vs closed safety peripheral intravenous catheters: a randomized study. J Hosp Infect. 2014;86:117–26. doi: 10.1016/j.jhin.2013.10.008. https://doi.org/10.1016/j.jhin.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 32.Adapa RM, Mani V, Murray LJ, Degnan BA, Ercole A, Cadman B, Williams CE, Gupta AK, Wheeler DW. Errors during the preparation of drug infusions: a randomized controlled trial. Br J Anaesth. 2012;109:729–34. doi: 10.1093/bja/aes257. https://doi.org/10.1093/bja/aes257. [DOI] [PubMed] [Google Scholar]
- 33.Keogh S, Marsh N, Higgins N, Davies K, Rickard C. A time and motion study of peripheral venous catheter flushing practice using manually prepared and prefilled flush syringes. J Infus Nurs. 2014;37:96–101. doi: 10.1097/NAN.0000000000000024. https://doi.org/10.1097/NAN.0000000000000024. [DOI] [PubMed] [Google Scholar]
- 34.Bijur PE, Schechter C, Esses D, Chang AK, Gallagher EJ. Intravenous bolus of ultra-low-dose naloxone added to morphine does not enhance analgesia in emergency department patients. J Pain. 2006;7:75–81. doi: 10.1016/j.jpain.2005.08.008. https://doi.org/10.1016/j.jpain.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 35.Birnbaum A, Esses D, Bijur PE, Holden L, Gallagher EJ. Randomized double-blind placebo-controlled trial of two intravenous morphine dosages (0.10 mg/kg and 0.15 mg/kg) in emergency department patients with moderate to severe acute pain. Ann Emerg Med. 2007;49:445–53. doi: 10.1016/j.annemergmed.2006.06.030. https://doi.org/10.1016/j.annemergmed.2006.06.030. [DOI] [PubMed] [Google Scholar]
- 36.Beaudoin FL, Lin C, Guan W, Merchant RC. Low-dose ketamine improves pain relief in patients receiving intravenous opioids for acute pain in the emergency department: results of a randomized, double-blind, clinical trial. Acad Emerg Med. 2014;21:1193–202. doi: 10.1111/acem.12510. https://doi.org/10.1111/acem.12510. [DOI] [PubMed] [Google Scholar]
- 37.Chang AK, Bijur PE, Meyer RH, Kenny MK, Solorzano C, Gallagher EJ. Safety and efficacy of hydromorphone as an analgesic alternative to morphine in acute pain: a randomized clinical trial. Ann Emerg Med. 2006;48:164–72. doi: 10.1016/j.annemergmed.2006.03.005. https://doi.org/10.1016/j.annemergmed.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 38.Chang AK, Bijur PE, Baccelieri A, Gallagher EJ. Efficacy and safety profile of a single dose of hydromorphone compared with morphine in older adults with acute, severe pain: a prospective, randomized, double-blind clinical trial. Am J Geriatr Pharmacother. 2009;7:1–10. doi: 10.1016/j.amjopharm.2009.02.002. https://doi.org/10.1016/j.amjopharm.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 39.Behzadnia MJ, Javadzadeh HR, Saboori F. Time of admission, gender and age: challenging factors in emergency renal colic – a preliminary study. [Last accessed 27 March 2018];Trauma Mon. 2012 17:329–32. doi: 10.5812/traumamon.6800. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860620/pdf/traumamon-17-329.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Soleimanpour H, Hassanzadeh K, Vaezi H, Golzari SE, Esfanjani RM, Soleimanpour M. Effectiveness of intravenous lidocaine versus intravenous morphine for patients with renal colic in the emergency department. BMC Urol. 2012;12:13. doi: 10.1186/1471-2490-12-13. https://doi.org/10.1186/1471-2490-12-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zare MA, Ghalyaie AH, Fathi M, Farsi D, Abbasi S, Hafezimoghadam P. Oral oxycodone plus intravenous acetaminophen versus intravenous morphine sulfate in acute bone fracture pain control: a double-blind placebo-controlled randomized clinical trial. Eur J Orthop Surg Traumatol. 2013;24:1305–9. doi: 10.1007/s00590-013-1392-x. https://doi.org/10.1007/s00590-013-1392-x. [DOI] [PubMed] [Google Scholar]
- 42.Galinski M, Dolveck F, Borron SW, Tual L, Van Laer V, Lardeur JY, Lapostolle F, Adnet F. A randomized, double-blind study comparing morphine with fentanyl in prehospital analgesia. Am J Emerg Med. 2005;23:114–9. doi: 10.1016/j.ajem.2004.03.010. http://dx.doi.org/10.1016/j.ajem.2004.03.010. [DOI] [PubMed] [Google Scholar]
- 43.Vergnion M, Degesves S, Garcet L, Magotteaux V. Tramadol, an alternative to morphine for treating posttraumatic pain in the prehospital situation. Anesth Analg. 2001;92:1543–6. doi: 10.1097/00000539-200106000-00039. https://doi.org/10.1097/00000539-200106000-00039. [DOI] [PubMed] [Google Scholar]
- 44.Azizkhani R, Pourafzali SM, Baloochestani E, Masoumi B. Comparing the analgesic effect of intravenous acetaminophen and morphine on patients with renal colic pain referring to the emergency department: a randomized controlled trial. J Res Med Sci. 2013;18:772–6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3872585/ [PMC free article] [PubMed] [Google Scholar]
- 45.Fry M, Holdgate A. Nurse-initiated intravenous morphine in the emergency department: efficacy, rate of adverse events and impact on time to analgesia. Emerg Med (Fremantle) 2002;14:249–254. doi: 10.1046/j.1442-2026.2002.00339.x. https://doi.org/10.1046/j.1442-2026.2002.00339.x. [DOI] [PubMed] [Google Scholar]
- 46.Serinken M, Eken C, Turkcuer I, Elicabuk H, Uyanik E, Schultz CH. Intravenous paracetamol versus morphine for renal colic in the emergency department: a randomised double-blind controlled trial. Emerg Med J. 2012;29:902–5. doi: 10.1136/emermed-2011-200165. https://doi.org/10.1136/emermed-2011-200165. [DOI] [PubMed] [Google Scholar]
- 47.Bektas F, Eken C, Karadeniz O, Goksu E, Cubuk M, Cete Y. Intravenous paracetamol or morphine for the treatment of renal colic: a randomized, placebo-controlled trial. Ann Emerg Med. 2009;54:568–74. doi: 10.1016/j.annemergmed.2009.06.501. https://doi.org/10.1016/j.annemergmed.2009.06.501. [DOI] [PubMed] [Google Scholar]
- 48.Cicolini G, Manzoli L, Simonetti V, Flacco ME, Comparcini D, Capasso L, Di Baldassarre A, Eltaji Elfarouki G. Phlebitis risk varies by peripheral venous catheter site and increases after 96 hours: a large multi-centre prospective study. J Adv Nurs. 2014;70:2539–49. doi: 10.1111/jan.12403. https://doi.org/10.1111/jan.12403. [DOI] [PubMed] [Google Scholar]
- 49.Rupp JD, Ferre RM, Boyd JS, Turer RW, Self WH. Contrast extravasation prevalence in emergency department patients with ultrasound-guided peripheral intravenous catheters. Ann Emerg Med. 2015;66(4):S98. Abstract 273. https://doi.org/10.1016/j.annemergmed.2015.07.307. [Google Scholar]
- 50.Hardie AD, Kereshi B. Incidence of intravenous contrast extravasation: increased risk for patients with deep brachial catheter placement from the emergency department. Emerg Radiol. 2014;21:235–8. doi: 10.1007/s10140-013-1185-x. https://doi.org/10.1007/s10140-013-1185-x. [DOI] [PubMed] [Google Scholar]
- 51.Adami NP, de Gutiérrez MG, da Fonseca SM, de Almeida EP. Risk management of extravasation of cytostatic drugs at the adult chemotherapy outpatient clinic of a university hospital. J Clin Nurs. 2005;14:876–82. doi: 10.1111/j.1365-2702.2005.01124.x. https://doi.org/10.1111/j.1365-2702.2005.01124.x. [DOI] [PubMed] [Google Scholar]
- 52.Watanabe H, Ikesue H, Yoshida M. Protection against the extravasation of anticancer drugs by standardization of the management system. Hosp Pharm. 2008;43:571–6. https://doi.org/10.1310/hpj4307-571. [Google Scholar]
- 53.Davies DE, Schneider F, Childs S, Hucker T, Krikos D, Peh J, McGowan C, Stone P, Cashman J. A prevalence study of errors in opioid prescribing in a large teaching hospital. Int J Clin Pract. 2011;65:923–9. doi: 10.1111/j.1742-1241.2011.02705.x. https://doi.org/10.1111/j.1742-1241.2011.02705.x. [DOI] [PubMed] [Google Scholar]
- 54.Kane-Gill SL, Rubin EC, Smithburger PL, Buckley MS, Dasta JF. The cost of opioid-related adverse drug events. J Pain Palliat Care Pharmacother. 2014;28:282–93. doi: 10.3109/15360288.2014.938889. https://doi.org/10.3109/15360288.2014.938889. [DOI] [PubMed] [Google Scholar]
- 55.Abraham J, Ogden K, Wang Y, Jones J. An economic analysis of postoperative pain management with fentanyl iontophoretic transdermal system. [Last accessed 27 March 2018];Value Health. 2015 18:A295. Available at http://www.valueinhealthjournal.com/article/S1098-3015(15)01778-7/pdf. [Google Scholar]
- 56.Morphine sulphate injection 10mg per ml summary of product characteristics. [Last accessed 28 March 2018]. Available at https://www.medicines.org.uk/emc/medicine/21357.
- 57.Metoclopramide 5 mg/ml Injection summary of product characteristics. [Last accessed 28 March 2018]. Available at https://www.medicines.org.uk/emc/medicine/20906.
- 58.Eberhart L, Koch T, Kranke P, Rüsch D, Torossian A, Nardi-Hiebl S. Activity-based cost analysis of opioid-related nausea and vomiting among inpatients. J Opioid Manag. 2014;10:415–22. doi: 10.5055/jom.2014.0238. https://doi.org/10.5055/jom.2014.0238. [DOI] [PubMed] [Google Scholar]
- 59.Abbey M, Chaboyer W, Mitchell M. Understanding the work of intensive care nurses: a time and motion study. Aust Crit Care. 2012;25:13–22. doi: 10.1016/j.aucc.2011.08.002. https://doi.org/10.1016/j.aucc.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 60.Institute for Safe Medication Practices. ISMP list of high alert medications. [Last accessed 28 March 2018]. Available at https://ismp.org/Tools/highalertmedications.pdf.
- 61.Totten V, Bellou A. Development of emergency medicine in Europe. Acad Emerg Med. 2013;20:514–21. doi: 10.1111/acem.12126. https://doi.org/10.1111/acem.12126. [DOI] [PubMed] [Google Scholar]
- 62.Meissner B, Nelson W, Hicks R, Sikirica V, Gagne J, Schein J. The rate and costs attributable to intravenous patient-controlled analgesia errors. Hosp Pharm. 2009;44:312–24. https://doi.org/10.1310/hpj4404-312. [Google Scholar]
- 63.Lake C, Beecroft CL. Extravasation injuries and accidental intra-arterial injection. [Last accessed 9 April 2018];Contin Educ Anaesth Crit Care Pain. 2010 10:109–13. https://academic.oup.com/bjaed/article/10/4/109/381097. [Google Scholar]
- 64.Patanwala AE, Keim SM, Erstad BL. Intravenous opioids for severe acute pain in the emergency department. Ann Pharmacother. 2010;44:1800–9. doi: 10.1345/aph.1P438. https://doi.org/10.1345/aph.1P438. [DOI] [PubMed] [Google Scholar]
- 65.Swegle JM, Logemann C. Management of common opioid-induced adverse effects. [Last accessed 27 March 2018];Am Fam Physician. 2006 74:1347–54. https://www.aafp.org/afp/2006/1015/p1347.pdf. [PubMed] [Google Scholar]
- 66.Huang Q, Thind A, Dreyer JF, Zaric GS. The impact of delays to admission from the emergency department on inpatient outcomes. BMC Emerg Med. 2010;10(1):16. doi: 10.1186/1471-227X-10-16. https://doi.org/10.1186/1471-227X-10-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Beaudoin FL, Merchant RC, Janicki A, McKaig DM, Babu KM. Preventing iatrogenic overdose: a review of in–emergency department opioid-related adverse drug events and medication errors. Ann Emerg Med. 2015;65(4):423–31. doi: 10.1016/j.annemergmed.2014.11.016. https://doi.org/10.1016/j.annemergmed.2014.11.016. [DOI] [PubMed] [Google Scholar]