Abstract
Background: The use of telemedicine in the diagnosis and treatment of acute stroke, or telestroke, is a well-accepted method of practice improving geographic disparities in timely access to neurological expertise. We propose that mobile telestroke assessment during ambulance transport is feasible using low-cost, widely available technology. Materials and Methods: We designed a platform including a tablet-based end point, high-speed modem with commercial wireless access, external antennae, and portable mounting apparatus. Mobile connectivity testing was performed along six primary ambulance routes in a rural network. Audiovisual (AV) quality was assessed simultaneously by both an in-vehicle and an in-hospital rater using a standardized 6-point rating scale (≥4 indicating feasibility). We sought to achieve 9 min of continuous AV connectivity presumed sufficient to perform mobile telestroke assessments. Results: Thirty test runs were completed: 93% achieved a minimum of 9 min of continuous video transmission with a mean mobile connectivity time of 18 min. Mean video and audio quality ratings were 4.51 (4.54 vehicle; 4.48 hospital) and 5.00 (5.13 in-vehicle; 4.87 hospital), respectively. Total initial cost of the system was $1,650 per ambulance. Conclusions: In this small, single-centered study we maintained high-quality continuous video transmission along primary ambulance corridors using a low-cost mobile telemedicine platform. The system is designed to be portable and adaptable, with generalizability for rapid assessment of emergency conditions in which direct observational exam may improve prehospital diagnosis and treatment. Thus mobile telestroke assessment is feasible using low-cost components and commercial wireless connectivity. More research is needed to demonstrate clinical reliability and efficacy in a live-patient setting.
Key words: : acute stroke, telemedicine, telestroke, mobile health, emergency medical services
Introduction
The use of telemedicine in the assessment and treatment of acute stroke (or telestroke) has greatly impacted the fields of neurology and emergency medicine over the last two decades.1 Stroke is an incredibly time-sensitive emergency that requires rapid access to neurological expertise and neuroimaging, both of which are limited in rural and underserved areas.2 The conventional telestroke hub-and-spoke model allows for the dissemination of neurological expertise and an increase in timely diagnosis and treatment of acute stroke through the use of stationary telemedicine end points.3 However, traditional telestroke models are unable to address the potentially lengthy time preceding a patient's arrival at the hospital.4,5
Numerous initiatives, including the American Heart Association/American Stroke Association's (AHA/ASA) Target: Stroke program, advocate innovative approaches to prehospital stroke care.6 Hospital prenotification by emergency medical services (EMS) is associated with more rapid administration of the clot-busting drug, intravenous tissue plasminogen activator (IV–tPA), in patients with acute ischemic stroke.7–11 However, current methods of EMS stroke screening and triage via telephone communication alone are widely variable and show limited accuracy and reliability.7,12–15 Moreover, recent clinical trial evidence has placed new emphasis on possible selective routing of stroke patients with more severe deficits who may qualify for endovascular therapy in addition to IV–tPA, which is only available at specialized stroke centers.16
To address these gaps, telestroke research has explored mobile platforms—bringing a stroke specialist remotely to the patient during ambulance transport.17–21 In 2009, a position statement by the AHA/ASA acknowledged the potential benefits of a viable platform to facilitate mobile stroke assessment in the prehospital setting but stipulated more research to address feasibility given the technology at the time.22
The purpose of this report is to describe a mobile telemedicine platform developed using low-cost, off-the-shelf technology and high-speed wireless connectivity to perform prehospital stroke assessments. The system was developed in conjunction with a clinical research protocol titled the Improving Treatment with Rapid Evaluation of Acute stroke via mobile Telemedicine (iTREAT) study.23
Materials and Methods
System Components
We designed our mobile telemedicine platform around an in-ambulance, tablet-based end point (iPad® 2 with retina display; Apple, Inc., Cupertino, CA). Audiovisual (AV) transmission was facilitated via a Health Insurance Portability and Accountability Act–secure videoconferencing application (Jabber® video for iPad; Cisco, Inc., San Jose, CA). Protected health information across video streaming was channeled through the University of Virginia Health System firewall using a 128-bit advance encryption standard. To achieve high-speed mobile connectivity in the ambulance, we designed a portable Wi-Fi system using a wireless modem/router (COR IBR600 LE-VZ; CradlePoint®, Boise, ID) with a Verizon Wireless© (New York, NY) network SIM card and two magnetic, external multiple-input–multiple-output antennae (AP-CW-M-S22-RP2-BL and AP-CG-S22-BL; Antenna Plus, Scottsdale, AZ). We worked with Verizon Wireless, which is the largest provider of fourth generation long-term evolution (4G LTE) coverage in our catchment area.
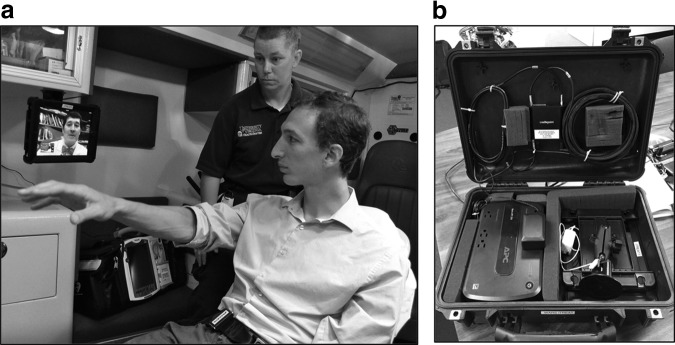
The iPad was secured in a protective case (Defender series; OtterBox®, Fort Collins, CO) and anchored using a positionable twist-lock suction mount with tablet-mounting cradle (RAM-B-166U and RAM-HOL-TAB3U; RAM MOUNTS®, Seattle, WA). An Uninterruptible Power Supply® (BE350G; APC Schneider Electric, West Kingston, RI) was added to ensure a redundant power source within the ambulance. All system components were stored in a protective case (1500 Case®; Pelican©, Torrance, CA) for portability and ease of storage (Fig. 1).
Fig. 1.
The Improving Treatment with Rapid Evaluation of Acute stroke via mobile Telemedicine (iTREAT) mobile telestroke platform. (a) The tablet end point deployed in an ambulance with the neurologist examining a simulated patient. (b) System components mounted to the storage case.
Initial Cost and Running Cost
The initial cost of our mobile telestroke platform includes individual hardware components and a commercial network contract with Verizon Wireless for unlimited data. The total setup cost per ambulance unit is approximately $1,650 (U.S.) (Table 1). We did not include the cost of the Cisco Jabber videoconferencing application as this is currently licensed and supported through our medical center for other telehealth services. Running costs include a per unit monthly data fee for the Verizon Network SIM card, which is currently $50/month.
Table 1.
iTREAT Mobile Telestroke Platform Component List with Associated Undiscounted Costs
| COMPONENT | COST (USD) |
|---|---|
| Apple II iPad with retina display | 500.00 |
| iPad protective case | 54.95 |
| RAM mount | 20.07 |
| RAM tablet cradle | 16.99 |
| Antennae | 240.00 |
| Uninterruptible power supply | 54.99 |
| CradlePoint modem | 599.99 |
| CradlePoint 6-foot cable | 14.49 |
| Modem set-up | 35.00 |
| SIM card | 8.00 |
| Pelican case | 111.95 |
| Total | 1,656.43 |
USD, U.S. dollars.
System Development
Initial development of the platform began in June 2013 with connectivity testing of the technology being conducted during the first 2 months of development. Initial connectivity testing determined AV quality of the video stream transmission during multiple test runs along primary transport routes to the University of Virginia Medical Center within the Thomas Jefferson EMS Council, Inc. of central Virginia. After consulting our partnering EMS departments about travel routes from their respective counties, we designated six primary ambulance routes along main corridors. All designated routes had roughly 20 min or more of transport time, and supported counties designated as rural by the Health Resources Services Administration and the Federal Communications Commission. Given the average time of 5–8 min necessary to complete the National Institutes for Health Stroke Scale (NIHSS),24 the standard screening tool for acute stroke diagnosis, we prespecified 9 min to be the target continuous video transmission time during test calls.
Bidirectional AV quality was assessed simultaneously and independently by both an in-vehicle and an in-hospital rater during live, mobile teleconferencing. Raters were members of the stroke service, including an attending physician and fellow, or analysts from the Center for Telehealth. The in-vehicle rater measured prehospital transport time and distance using the MotionX® GPS application (Fullpower Technologies, Santa Cruz, CA) and manually logged sections of poor quality during runs. Overall transmission quality was assessed throughout the entirety of the test run.
A standardized, 6-point scale adapted from Liman et al.18 was used to assess quality between 1 (uninterpretable transmission) and 6 (fully fluid and comprehensible) (Fig. 2). For the purposes of the study, “fluid” video and audio were defined as video transmission with consistent, smooth frame rates and audio without clipping or lag, respectively. A rating of ≥4 was prespecified as being of sufficient AV quality to perform a remote neurological assessment. Following completion of a test call, each rater designated independent audio and video quality ratings. Ratings were automatically compiled into the dataset by recreating the rating sheet as an online form. Raters were blinded to transmission quality scoring submitted by their paired rater.
Fig. 2.
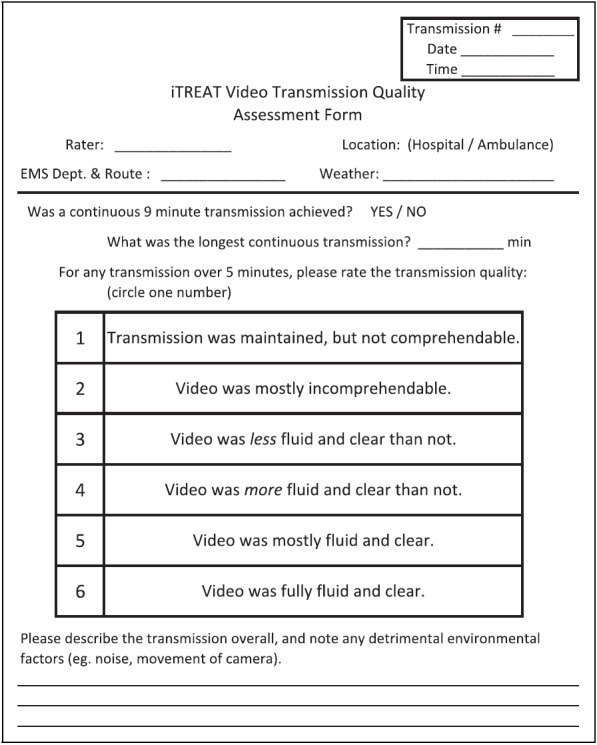
A sample video transmission rating form for test calls. This video transmission rating form with scale was converted to an online form for use by the raters. A similar audio quality rating form was created as well, with the same terminology and descriptors used in the video rating scale. EMS, emergency medical services; iTREAT, Improving Treatment with Rapid Evaluation of Acute stroke via mobile Telemedicine.
Data Analysis
Standardized rating of transmission quality was charted between raters. Results are presented as mean ratings and percentages. Additionally, manual GPS logs of route sections with unacceptable AV connectivity were overlaid to construct a basic connectivity map for our ambulance routing network, with the goal of highlighting consistent dead zones along routes.
Ethical Considerations
This feasibility study was conducted with protocol approval from local Institutional Review Boards. All study investigators completed Collaborative Institutional Training Initiative certification in accordance with ethical standards for human subjects research.
Results
Av Quality Testing
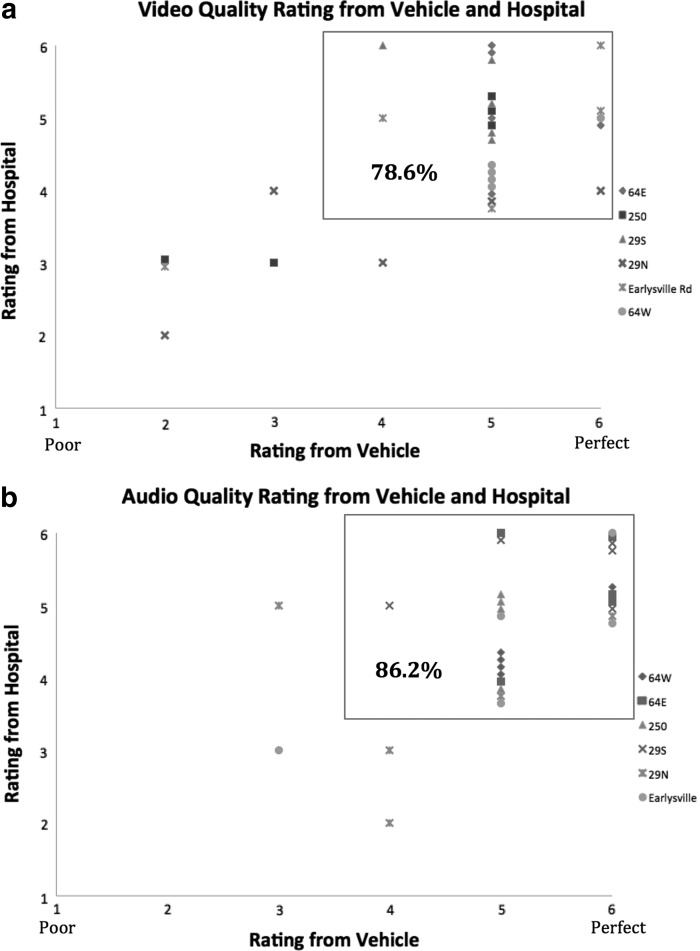
Five test runs were completed along each of the six designated transport corridors for a total of 30 test runs. The platform achieved a mean video quality rating of 4.51 (4.54 vehicle; 4.48 hospital) and a mean audio quality rating of 5.00 (5.13 in-vehicle; 4.87 hospital). Both raters deemed audio and video quality as acceptable, good, or excellent for 86% and 79% of all runs, respectively (Fig. 3). Excluding one route with poor transmission quality, 87.5% of test calls achieved bidirectional AV quality with paired ratings of 4 or higher. AV rating averages for the individual transport routes are listed in Figure 4. The most common complaint associated with poor video quality scores by raters was freezing of the image, with raters mentioning pixilation and loss of fluidity as the main problem in two other poorly scored runs. Poor audio scoring was mainly associated with lag in the audio stream.
Fig. 3.
Test run audiovisual quality ratings: (a) video and (b) audio quality rating from the vehicle and the hospital. “Acceptable” audiovisual quality transmissions are denoted by the box. Data points represent paired quality ratings from in-ambulance and in-hospital raters for each test run along the designated ambulance routes.
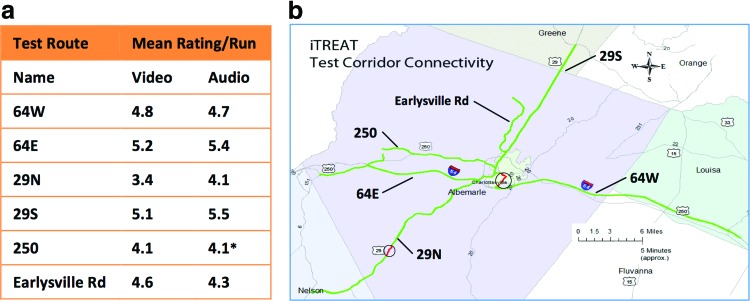
Fig. 4.
(a) Audiovisual quality rating averages for designated emergency medical services routes and (b) GPS map of mobile videoconferencing dead zones on routes. (a) Values are averages of individual test run ratings by both in-hospital and in-vehicle raters. *Average audio quality rating for this route contains one less data point compared with the others as one rating was missing. (b) This map displays the six designated test routes. Zones of consistently poor connectivity across multiple test runs are shown inside the circles. iTREAT, Improving Treatment with Rapid Evaluation of Acute stroke via mobile Telemedicine. Color images available online at www.liebertpub.com/tmj
Remote Assessment Feasibility Testing
During connectivity testing, 93% of test runs achieved a minimum 9 min of continuous, live video transmission with a mean mobile connectivity time of 18 min. All test runs were completed during daytime hours, with 43% of runs between 8 a.m. and 12 p.m. and 57% between 12 p.m. and 5 p.m. Weather was also recorded, with 53% clear/sunny, 43% cloudy/overcast, and 3% stormy. Based off of manual GPS mapping of connectivity along transport corridors, only two short sections demonstrated consistently poor transmission quality (Fig. 4).
Discussion
As a first step in the iTREAT study, we developed a novel platform for conducting mobile telemedicine assessments during ambulance transport. In our initial round of field-testing, we achieved continuous mobile AV connectivity along ambulance routes with reproducible quality using a commercial cellular network. As noted in prior pilot studies of ambulance-based telestroke, technical feasibility depends on the availability of high-speed broadband.17–21 Our platform utilizes a commercial 4G LTE network while remaining low cost with widely available components. By using a commercially prevalent tablet as the mobile end point, a single ambulance can be outfitted for less than $2,000. Additionally, the suction mounting system allows flexibility in placement of the mobile end point to accommodate differing ambulance layouts and engineering safety specifications. These design elements maximize portability and adaptability in order to make mobile telemedicine generalizable to various EMS systems.
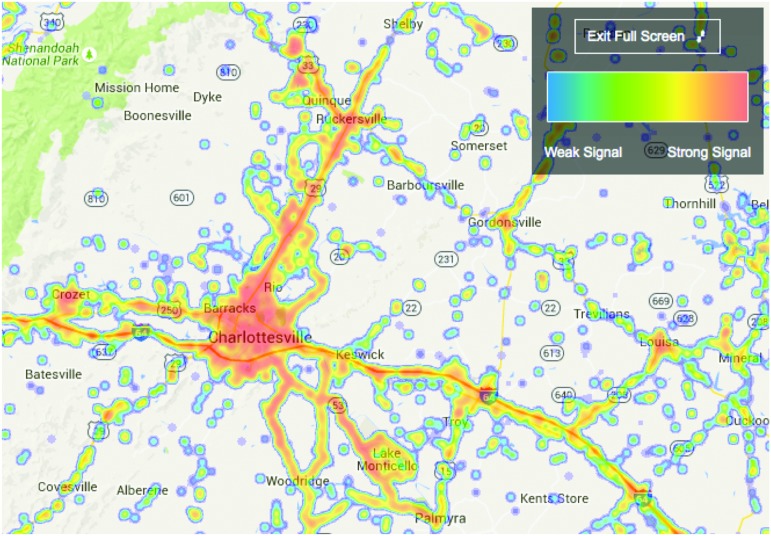
Adapting mobile telemedicine within a rural system of care brings unique challenges, including the possibility of a more limited broadband infrastructure. However, in our system, most ambulances travel along mainstream corridors for the majority of transport time during which high-quality AV connectivity is viable due to greater cell tower density. For hospital systems with longer EMS routes, understanding geographic patterns within the commercial broadband network is crucial to achieve ambulance-based telemedicine. The validity of our connectivity results is substantiated in comparison with a publicly available network connectivity map as depicted in Figure 5. Of note is that our least consistent ambulance route during initial field testing was shown to have lowest overall connectivity via the third-party cellular density map. If we excluded this single route from the analysis, the percentage of test runs achieving consistently high-quality video transmission approached 90%. Findings from this initial study were relayed to our contacts at Verizon Wireless; however, the current connectivity results displayed in Figure 5 should reflect any improvements made since our communication with the network providers. We hope continued collaboration with our wireless network representatives will further improvements along EMS routes and expect that similar collaborations would be necessary for translation to other regions.
Fig. 5.
Verizon cellular network connectivity in the emergency medical services triage network. This third-party connectivity map is derived from the connectivity levels of private users as relayed by a smartphone application. Data were compiled and presented by OpenSignal.com Color images available online at www.liebertpub.com/tmj
We designed iTREAT with an emphasis on advancing prehospital stroke care, including the potential for more accurate diagnosis, improved routing and triage, and timelier treatment. Mobile telemedicine may also assist in EMS research facilitating informed consent and investigation of novel prehospital treatments.25 Moreover, a low-cost, adaptable mobile telemedicine platform may translate well to other emergency, time-sensitive conditions in which a visual assessment has value. These might include trauma, neonatal care, or other cardiovascular conditions.26–29
The results of this initial feasibility study have several limitations. Although we did not specifically incorporate patient examination into field testing, we did specify and achieve at least 9 min of high-quality, continuous videoconferencing, which is ample time to complete a screening neurological assessment. Additionally, we were only able to show high-fidelity bidirectional AV quality in approximately 80% of test runs. The fact that our results boosted dramatically with the exclusion of one ambulance route suggests that an individualized and geographic approach to troubleshooting is necessary. Given that testing was performed in only one region, these results may not be generalizable to other health systems. For instance, urban systems may have great cellular traffic or impedance affecting transmission quality. High-density EMS systems may also have shorter transport times during which meaningful prehospital telemedicine assessment would be less valuable.
Although individual test run characteristics were recorded, the small number of test runs completed limited the ability to analyze differences in transmission quality due to weather, time of day/year, or vehicle. We limited field testing to daytime hours as a matter of convenience, which may neglect variations in cellular transmission, traffic patterns, or EMS personnel.
From a methodological point of view, this is a small observational study, and results are hypothesis generating. Quality ratings to determine feasibility were subjective and may have been biased, although simultaneous in-vehicle and in-hospital ratings were blinded. Additionally, measures of inter-rater reliability were not achieved. However, we have observed favorable results correlating the NIHSS in simulated stroke scenarios using our mobile telestroke platform, and we are proceeding with testing in live patient encounters.30 We are also working on a correlation study between subjective AV quality and objective transmission metrics, including jitter and packet loss, which may determine minimum performance standards for a quality mobile telemedicine encounter.
The iTREAT system is an evolving clinical application, and additional steps are underway to determine reliability and efficacy in live patient encounters. As a novel application of mobile telemedicine, our platform is representative of the growing field of mobile health, or m-health. According to the business and technology news outlet Business Insider, mobile is the only U.S. consumer media that is growing, and mobile devices have far surpassed desktop computers in global sales and Internet usage from 2009 to 2013.31 Applications of m-health are rapidly growing as a result of this increased societal presence, and this is especially true in the treatment and prevention of cardiovascular disease.32,33 As an example in acute stroke care, the NIHSS has been validated for use with both the iPhone and iPad for bedside testing.24,34,35 This further supports the feasibility of our system for translation to clinical practice.
Conclusions
Mobile, prehospital assessment of acute stroke patients via ambulance-based videoconferencing is feasible and can be achieved using low-cost components and commercial data networks. More research is necessary to determine reliability and practical efficacy of our mobile telemedicine system. Developing mobile telehealth applications with a focus on portability and adaptability is widely generalizable for rural and underserved areas, as well as a range of emergency medical conditions.
Acknowledgments
The authors acknowledge the following support: AHA Student Scholarship in Cerebrovascular Disorders and Stroke, NINDS Clinical Trials Methodology Course R25 NS088248, Health Resources and Services Administration grant GO1RH27869-01-00, the University of Virginia Neuroscience Center of Excellence, the Virginia Alliance for Emergency Medicine Research, the Thomas Jefferson EMS Council, Inc., and Verizon Wireless, Inc.
Disclosure Statement
The authors have obtained U.S. Provisional Patent Application Serial number 61/867,477, filed on August 19, 2013. B.B.W. is the Associate Editor of Neurology®, and A.M.S. is the Deputy Section Editor of Neurology® Podcast and a Speaker for America's Essential Hospitals.
References
- 1.Levine SR, Gorman M. “Telestroke”: The application of telemedicine for stroke. Stroke 1999;30:464–469 [DOI] [PubMed] [Google Scholar]
- 2.Mullen MT, Judd S, Howard VJ, et al. Disparities in evaluation at certified primary stroke centers: Reasons for geographic and racial differences in stroke. Stroke 2013;44:1930–1935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schwamm LH, Audebert HJ, Amarenco P, et al. Recommendations for the implementation of telemedicine within stroke systems of care: A policy statement from the American Heart Association. Stroke 2009;40:2635–2660 [DOI] [PubMed] [Google Scholar]
- 4.Kleindorfer D, Kissela B, Schneider A, et al. Eligibility for recombinant tissue plasminogen activator in acute ischemic stroke: A population-based study. Stroke 2004;35:e27–e29 [DOI] [PubMed] [Google Scholar]
- 5.Kwan J, Hand P, Sandercock P. A systematic review of barriers to delivery of thrombolysis for acute stroke. Age Ageing 2004;33:116–121 [DOI] [PubMed] [Google Scholar]
- 6.Fonarow GC, Smith EE, Saver JL, et al. Improving door-to-needle times in acute ischemic stroke: The design and rationale for the American Heart Association/American Stroke Association's Target: Stroke initiative. Stroke 2011;42:2983–2989 [DOI] [PubMed] [Google Scholar]
- 7.Lin CB, Peterson ED, Smith EE, et al. Patterns, predictors, variations, and temporal trends in emergency medical service hospital prenotification for acute ischemic stroke. J Am Heart Assoc 2012;1:e002345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin CB, Peterson ED, Smith EE, et al. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes 2012;5:514–522 [DOI] [PubMed] [Google Scholar]
- 9.Patel MD, Rose KM, O'Brien EC, Rosamond WD. Prehospital notification by emergency medical services reduces delays in stroke evaluation: Findings from the North Carolina Stroke Care Collaborative. Stroke 2011;42:2263–2268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abdullah AR, Smith EE, Biddinger PD, Kalenderian D, Schwamm LH. Advance hospital notification by EMS in acute stroke is associated with shorter door-to-computed tomography time and increased likelihood of administration of tissue-plasminogen activator. Prehosp Emerg Care 2008;12:426–431 [DOI] [PubMed] [Google Scholar]
- 11.Desai JA, Smith EE. Prenotification and other factors involved in rapid tPA administration. Curr Atheroscler Rep 2013;15:337. [DOI] [PubMed] [Google Scholar]
- 12.Crocco TJ, Grotta JC, Jauch EC, et al. EMS management of acute stroke—Prehospital triage (resource document to NAEMSP position statement). Prehosp Emerg Care 2007;11:313–317 [DOI] [PubMed] [Google Scholar]
- 13.Rajajee V, Saver J. Prehospital care of the acute stroke patient. Tech Vasc Interv Radiol 2005;8:74–80 [DOI] [PubMed] [Google Scholar]
- 14.Studnek JR, Asimos A, Dodds J, Swanson D. Assessing the validity of the Cincinnati prehospital stroke scale and the medic prehospital assessment for code stroke in an urban emergency medical services agency. Prehosp Emerg Care 2013;17:348–353 [DOI] [PubMed] [Google Scholar]
- 15.Brandler ES, Sharma M, McCullough F, et al. Prehospital stroke identification: Factors associated with diagnostic accuracy. J Stroke Cerebrovasc Dis 2015;24:2161–2166 [DOI] [PubMed] [Google Scholar]
- 16.Powers WJ, Derdeyn CP, Biller J, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2015;46:3020–3035 [DOI] [PubMed] [Google Scholar]
- 17.LaMonte MP, Xiao Y, Hu PF, et al. Shortening time to stroke treatment using ambulance telemedicine: TeleBAT. J Stroke Cerebrovasc Dis 2004;13:148–154 [DOI] [PubMed] [Google Scholar]
- 18.Liman TG, Winter B, Waldschmidt C, et al. Telestroke ambulances in prehospital stroke management: Concept and pilot feasibility study. Stroke 2012;43:2086–2090 [DOI] [PubMed] [Google Scholar]
- 19.Bergrath S, Reich A, Rossaint R, et al. Feasibility of prehospital teleconsultation in acute stroke—A pilot study in clinical routine. PloS One 2012;7:e36796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Hooff RJ, Cambron M, Van Dyck R, et al. Prehospital unassisted assessment of stroke severity using telemedicine: A feasibility study. Stroke 2013;44:2907–2909 [DOI] [PubMed] [Google Scholar]
- 21.Wu TC, Nguyen C, Ankrom C, et al. Prehospital utility of rapid stroke evaluation using in-ambulance telemedicine: A pilot feasibility study. Stroke 2014;45:2342–2347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwamm LH, Holloway RG, Amarenco P, et al. A review of the evidence for the use of telemedicine within stroke systems of care: A scientific statement from the American Heart Association/American Stroke Association. Stroke 2009;40:2616–2634 [DOI] [PubMed] [Google Scholar]
- 23.Chapman S, Lippman J, Gunnell B, et al. Mobile telestroke during ambulance transport is feasible in a rural EMS setting—Pilot data from the Improving Treatment With Rapid Evaluation Of Acute Stroke Via Mobile Telemedicine (iTREAT) Study [abstract S5.002]. Neurology 2014;82(Suppl 5):S5.002 [Google Scholar]
- 24.Anderson ER, Smith B, Ido M, Frankel M. Remote assessment of stroke using the iPhone 4. J Stroke Cerebrovasc Dis 2013;22:340–344 [DOI] [PubMed] [Google Scholar]
- 25.Ahluwalia A, Starkman S, Sanossian N, et al. Enrolling patients in ambulance stroke trials using mobile televideo consent: Preliminary experience [abstract S5.004[. Neurology 2014;82(Suppl 5):S5..004. [Google Scholar]
- 26.Bergrath S, Czaplik M, Rossaint R, et al. Implementation phase of a multicentre prehospital telemedicine system to support paramedics: Feasibility and possible limitations. Scand J Trauma Resusc Emerg Med 2013;21:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Qureshi A, Shih E, Fan I, et al. Improving patient care by unshackling telemedicine: Adaptively aggregating wireless networks to facilitate continuous collaboration. AMIA Annu Symp Proc 2010;2010:662–666 [PMC free article] [PubMed] [Google Scholar]
- 28.Chu Y, Ganz A. A mobile teletrauma system for rural trauma care. Conf Proc IEEE Eng Med Biol Soc 2004;5:3282–3285 [DOI] [PubMed] [Google Scholar]
- 29.Amadi-Obi A, Gilligan P, Owens N, O'Donnell C. Telemedicine in pre-hospital care: A review of telemedicine applications in the pre-hospital environment. Int J Emerg Med 2014;7:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Padrick MM, Chapman Smith SN, McMurry TL, et al. NIH Stroke Scale assessment via iPad-based mobile telestroke during Ambulance transport is feasible—Pilot data from the Improving Treatment with Rapid Evaluation of Acute Stroke via Mobile Telemedecine (iTREAT) Study [abstract 90]. Stroke 2015;46:A90 [Google Scholar]
- 31.Blodget H, Danova T. The future of mobile! March 21, 2014. Available at www.businessinsider.com/future-of-mobile-slides-2014-3 (last accessed August19, 2015)
- 32.Waegemann CP. mHealth: The next generation of telemedicine? Telemed J E Health 2010;16:23–25 [DOI] [PubMed] [Google Scholar]
- 33.Burke LE, Ma J, Azar KM, et al. Current science on consumer use of mobile health for cardiovascular disease prevention: A scientific statement from the American Heart Association. Circulation 2015;132:1157–1213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gonzalez MA, Hanna N, Rodrigo ME, Satler LF, Waksman R. Reliability of prehospital real-time cellular video phone in assessing the simplified National Institutes of Health Stroke Scale in patients with acute stroke: A novel telemedicine technology. Stroke 2011;42:1522–1527 [DOI] [PubMed] [Google Scholar]
- 35.Binz S, Khatri R, Carroll J, Prusakov P, Chang F-L. The feasibility of iPad technology for remote acute ischemic stroke assessment [abstract P05.203]. Neurology 2013;80:P05.203 [Google Scholar]