Abstract
Purpose
A laparoscopic approach for emergency appendectomy is increasingly used, in pediatric patients as well. The objective of this study is to audit the current state of diagnostic work-up, surgical techniques and its outcome in children with acute appendicitis.
Methods
A prospective consecutive observational cohort study was carried out in a 2-month study period. All patients under 18 years that were operated for suspected acute appendicitis were included. Primary outcome was the infectious complication rate after open and laparoscopic approach; secondary outcomes were preoperative use of imaging and post-operative predictive value of imaging, normal appendix rate and children with a postoperative ileus.
Results
A total of 541 children were operated for suspected acute appendicitis in 62 Dutch hospitals. Preoperative imaging was used in 98.9% of children. The normal appendix rate was 3.1%. In 523 children an appendectomy was performed. Laparoscopy was used in 61% of the patients and conversion rate was 1.7%. Complicated appendicitis was diagnosed in 29.4% of children. Overall 30-day complication rate was 11.9% and similar after open and laparoscopic. No difference was found in superficial surgical site infections, nor in intra-abdominal abscesses between the open and laparoscopic approach. Complicated appendicitis is an independent risk factor for infectious complications.
Conclusion
The laparoscopic approach is most frequently used, except for young children. Superficial surgical site infections are more frequent after open surgery only in patients with complicated appendicitis. The normal appendix rate is low, most likely because of routine preoperative imaging.
Keywords: Appendicitis, Children, Appendectomy, Pediatric
Introduction
In children, emergency appendectomy is the most performed acute surgical procedure [1].
Two options are available to perform an appendectomy: the open approach through a gridiron incision first described by McBurney in 1894 [2], and the laparoscopic approach described by de Kok [3] in 1977.
Almost 25% of all appendectomies are performed in children and appendicitis has a lifetime incidence of 7–8% with a peak in adolescents [4]. Diagnostic workup and treatment can be different in children and adults.
Over recent years overall diagnostic work-up and treatment are changing. There is an increased use of preoperative imaging to reduce the negative appendectomy rate and new imaging techniques are implemented. Regarding treatment, laparoscopy is more frequently used, but is still not universally accepted as standard of care in the treatment of appendicitis in children. In children, a recent meta-analysis showed a broad equivalence in uncomplicated appendicitis and an increased risk of intra-abdominal abscess in laparoscopy in case of complicated appendicitis [5].
Recently the idea is endorsed that, instead of being a progressive disease starting with uncomplicated stage and evolving to a complicated form, complicated and uncomplicated appendicitis are now considered as two different entities [6]. This has led to new studies evaluating the conservative treatment with antibiotics of uncomplicated appendicitis in children as well as adults [7, 8].
As a part of a nationwide cohort study on surgical treatment of acute appendicitis in The Netherlands [9] this study’s objectives were to evaluate the national guideline and to assess the variation in practice and outcome in the treatment of acute appendicitis in children. Emphasis will be on infectious complications and its clinical consequences after open and laparoscopic appendectomy.
Methods
Study design
A consecutive observational cohort study (snapshot) was performed in hospitals in the Netherlands. All hospitals that provided acute surgical care were invited to participate. This included academic, pediatric and general community hospitals (teaching and non-teaching). The study was designed and led by surgical residents, who together with house officers collected the data.
All consecutive patients undergoing surgery for suspected acute appendicitis were included between June and July 2014. This period was preceded by a pilot phase in May in 8 hospitals in the Amsterdam region. Only pediatric patients (age below 18 years) were analyzed in this study. Patients were excluded if they underwent an elective appendectomy (either interval or as a routine procedure, for instance, in patients with malrotation). Furthermore, patients initially treated non-operatively were also excluded, even though some of them underwent a subsequent appendectomy. All patients that underwent diagnostic laparoscopy without removal of the appendix, or patients that had a different procedure, but were initially operated for suspected appendicitis were included to evaluate the normal appendix rate. A normal appendix was diagnosed by the operating surgeon when there was no sign of inflammation (rigid appendix, prominent vascularization, free fluid, perforation).
Patients were treated according to the local protocol of the participating hospitals, based on the national guideline. No adjustments on treatment were imposed for participating hospitals. No additional follow-up or contribution was asked for the patients.
Primary outcome was complication rate, mainly infectious complications [superficial surgical site infection (SSI) and intra-abdominal abscess (IA)] after open and laparoscopic appendectomy. Secondary outcomes were preoperative use of imaging and post-operative predictive value of imaging, normal appendix rate and children with a postoperative ileus. SSI was defined as the clinical suspicion for a SSI that required additional interventions (either antibiotics or drainage). IA was defined as an intra-abdominal fluid collection that required antibiotics or drainage procedures (surgical or percutaneous). Ileus was defined as no resumption of diet within 5 days [10]. Preoperative definition of complicated appendicitis consisted of signs of perforation in the radiology report, i.e., free fluid, free air or abscess. Intra-operative definition of complicated appendicitis consisted of the presence of perforation or necrosis of the appendix.
Data collection
Data were collected from presentation at the emergency room until 30 days after surgery.
Data were anonymized and entered into a web-based database by a single local investigator. Data were extracted from the electronic patient database system, admission charts and operative reports or directly from the operating surgeon when details were unclear. To identify complications during follow-up, the electronic patient database system was monitored to detect postoperative attendance to the emergency department, unscheduled outpatient clinic visits, hospital readmissions, imaging or intervention. Additional checking of admission diagnosis and surgical procedures in the study months identified any possible missing patients.
Statistics
Statistical analysis was performed using SPSS® version 22 (IBM, Armonk, New York, USA).
All normally distributed variables were analyzed using Student’s t test. χ2 test or Fisher’s exact test where appropriate were used in dichotomous outcomes. Univariable odds ratios were calculated to compare complications between laparoscopic and open appendectomy.
Analysis was performed according to the intention to treat principle and converted patients were therefore analyzed in the laparoscopic group.
Results
Included patients
A total of 541 patients were included from 62 Dutch hospitals, including all 7 pediatric hospitals.
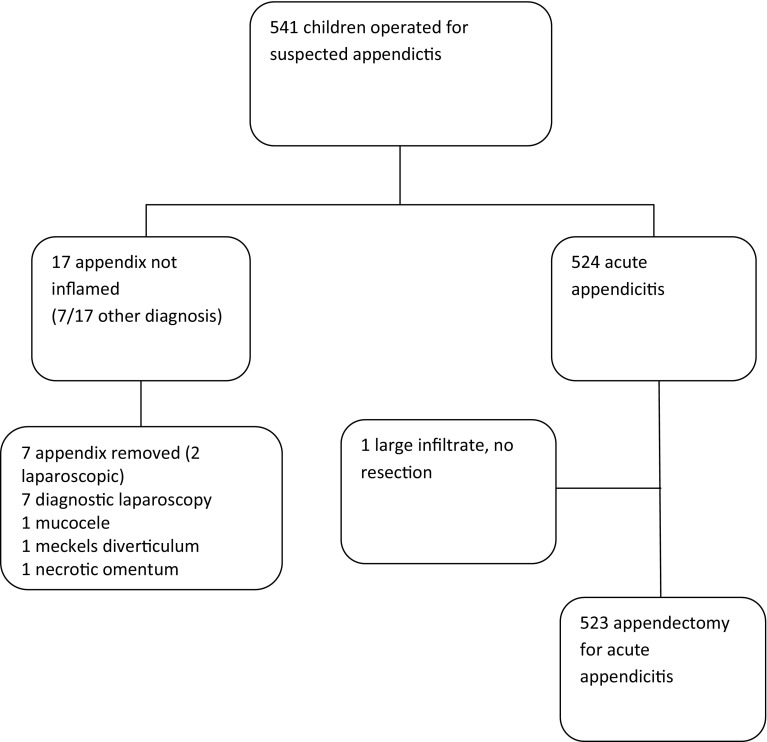
Number of children ranged from 1 to 27 per hospital. In 17 patients the appendix was peroperatively not inflamed (3.1%), an alternative diagnosis was noted in 7 of them (41.2%), and all of them had preoperative imaging. The appendix from only 7 of the 17 patients was removed mainly because of the open approach. Unexpectedly, in 3 of these patients the pathology report stated uncomplicated appendicitis. One of the patients with an acute appendicitis was treated without appendectomy, leaving a total of 523 patients that underwent an appendectomy for suspected appendicitis (Fig. 1). The outcomes of these procedures were examined.
Fig. 1.
Flow diagram
Preoperative data and imaging
Demographic and imaging characteristics are displayed in Table 1. The majority of the children were boys (60%) and the median age was 12 years. As expected, appendicitis under the age of 6 was rare; only 28 patients (5.4%). The majority was treated in a general community hospital, teaching or non-teaching (91.6%). 8.4% in a pediatric (academic) hospital, of which 16.1% children under the age of 6.
Table 1.
Demographic and imaging
| Total (N = 523) | Laparoscopy (ITT) (N = 319) | Open (N = 204) | P* | |
|---|---|---|---|---|
| Age | < 0.001 | |||
| 0–5 | 28 (5.4) | 10 (3.1) | 18 (8.8) | |
| 6–11 | 212 (40.5) | 105 (32.9) | 107 (52.5) | |
| 12–17 | 283 (54.1) | 204 (63.9) | 79 (38.7) | |
| Gender | 0.005 | |||
| Male | 314 | 177 (55.5) | 137 (67.2) | |
| Female | 209 | 142 (44.5) | 67 (32.8) | |
| Day since onset complaints | 0.347 | |||
| Median | 1 | 1 | 1 | |
| <3 days | 240 (77.4) | 161 (79.3) | ||
| ≥ 3 days | 70 (22.6) | 42 (20.7) | ||
| Missing | 10 | |||
| Institution | ||||
| Academical/childrens | 44 (8.4) | 32 (10.0) | 12 (5.9) | |
| Community | 479 (91.6) | 287 (90.0) | 192 (94.1) | |
| Imaging | 0.399 | |||
| Ultrasound only | 481 (92) | 288 (90.3) | 193 (94.6) | |
| Ultrasound + CT-scan | 7 (1.3) | 6 (1.9) | 1 (0.5) | |
| Ultrasound + MRI scan | 28 (5.4) | 20 (6.3) | 8 (3.9) | |
| MRI only | 1 (0.2) | 1 (0.3) | 0 (0) | |
| No imaging | 6 (1.1) | 4 (1.3) | 2 (1.0) | |
| Imaging conclusion | 0.012 | |||
| Uncomplicated | 293 (76) | 238 (75.6) | 155 (76.7) | |
| Complicated | 77 (14.9) | 40 (12.7) | 37 (18.3) | |
| Not conclusive | 47 (9.1) | 37 (11.7) | 10 (5.0) |
*χ2 test or Fisher’s exact test where appropriate
In nearly all patients preoperative imaging was performed, (98.9%). Ultrasound was used as the only imaging modality in 92%. Complementary CT-scan or MRI scan was obtained in 1.3 and 5.4%, respectively. Complicated appendicitis was suspected preoperatively in 14.9% of the patients. An inconclusive result from preoperative imaging was in 9.1% of patients. Complex (or complicated) appendicitis on imaging was defined as signs of perforation described in the radiology report, e.g., free fluid or abscess formation.
Intraoperative data
Intraoperative data are displayed in Table 2. A laparoscopic appendectomy was performed in 319 children (61%), although in 1.7% of these procedures it was necessary to convert to open appendectomy. The distribution of the application of laparoscopy for each age group is as follows: 35.7% of children under 6, between 6 and 11 years in 49.5 and 72.1% of children between 12 and 18 years. Conversion rates were 0, 1.4 and 2.1%, respectively.
Table 2.
Operative data
| Total (N = 523) | Laparoscopic (N = 319) | Open (N = 204) | P* | |
|---|---|---|---|---|
| Conversion | 9 (1.7) | |||
| Surgeon | 0.380 | |||
| Consultant or resident under supervision | 452 (86.4) | 274 (85.9) | 178 (87.3) | |
| Resident alone | 71 (13.6) | 45 (14.1) | 26 (12.7) | |
| Operating time (mean, min) | 39.34 | 42.90 | 33.40 | 0.001# |
| Hospital stay (median, days) | 2 | 2 | 2 | 0.473# |
| (Range) | (1–30) | (1–16) | (1–30) | |
| Intraoperative diagnosis | 0.457 | |||
| Simple | 369 (70.6) | 224 (70.2) | 145 (71.1) | |
| Complicated | 154 (29.4) | 95 (29.8) | 59 (28.9) | |
| Antibiotics | 0.603 | |||
| No prophylaxis | 12 (2.3) | 9 (2.8) | 3 (1.5) | |
| Intraoperative | 374 (71.5) | 227(71.2) | 147 (72.1) | |
| Continued | (26.2) | 83 (26.0) | 54 (26.5) | |
| Histology | 0.302 | |||
| Normal | 14 (2.7) | 12 (3.8) | 2 (1.0) | |
| Simple | 404 (77.2) | 244 (76.5) | 160 (78.4) | |
| Necrosis | 42 (8.0) | 26 (8.2) | 16 (7.8) | |
| Perforation | 43 (8.2) | 23 (7.2) | 20 (9.8) | |
| Neoplasm | 3 (0.6) | 2 (0.6) | 1 (0.5) | |
| Other | 9 (1.7) | 5 (1.6) | 4 (2.0) | |
| No pathology | 8 (1.5) | 7 (2.2) | 1 (0.5) |
*χ2 test or Fisher’s exact test where appropriate
#Mann–Whitney U test
A laparoscopic operation was performed in 56.4% of the boys and in 67.9% of the girls.
In patients with preoperative suspicion of uncomplicated appendicitis on imaging, 83.7% were diagnosed with uncomplicated appendicitis during operation. In patients with preoperative suspicion of complicated appendicitis on imaging, 71.4% were diagnosed with complicated appendicitis during operation.
Intraoperatively, in 29.4% of the patients, complicated appendicitis was diagnosed. In 5.2% of patients with complicated appendicitis undergoing a laparoscopic appendectomy conversion was necessary.
Complicated appendicitis was diagnosed significantly more frequent in children < 6-years-old compared to children 6–11 years old and between 12 and 18 years old; 67.9 vs 29.7 vs 25.4%, respectively (P < 0.001).
The overall complication rate after an appendectomy for acute appendicitis was 11.9% during the 30-day follow-up. The rates between laparoscopic and open approaches were comparable (OR 1.064; 95% CI 0.620–1.828; P = 0.462). In complicated appendicitis overall complication rate was 28.6% (OR 7.800; 95% CI 4.329–14.053; P = 0.001). Pediatric surgeons had similar laparoscopic approach rates (OR 1.584; 95% CI 0.645–3.890) and complication rates (OR 0.644; 95% CI 0.213–1.949) as other surgeons.
Infectious complications
After an appendectomy the overall rate of SSI was 1.7%, of IA was 5.9% and of an ileus was 2.5%.
In Table 3, the overall complication rates for laparoscopic and open appendectomy are displayed. No statistical difference could be detected for SSI, 0.9 vs 2.9% (OR 3.192; 95% CI 0.790–12.91; P = 0.087). There was also no significant difference in IA, 6.0 vs 5.9%, respectively (OR 0.987; 95% CI 0.468–2.079; P = 0.560), nor could it be detected in ileus, 2.2 vs 2.9% (OR 1.351; 95% CI 0.447–4.077; P = 0.395).
Table 3.
Overall 30 day complications
| Total | Laparoscopic | Open | Odds ratio (95% CI) | P* | |
|---|---|---|---|---|---|
| Any complication | 62 (11.9) | 37 (11.6) | 25 (12.3) | 1.064 (0.620–1.828) | 0.462 |
| Infectious complication | |||||
| Any infectious | 39 (7.5) | 22 (6.9) | 17 (8.3) | 2.364 (0.633–2.364) | 0.331 |
| Superficial surgical site infection | 9 (1.7) | 3 (0.9) | 6 (2.9) | 3.192 (0.790–12.91) | 0.087 |
| Intra-abdominal abscess | 31 (5.9) | 19 (6.0) | 12 (5.9) | 0.987 (0.468–2.079) | 0.560 |
| Ileus | 13 (2.5) | 7 (2.2) | 6 (2.9) | 1.351 (0.447–4.077) | 0.395 |
| Hospital stay (days) (median) | 541 | 2 (1–17) | 2 (1–31) | 0.835# | |
| Hospital re-admittance | 30 (5.7) | 20 (6.3) | 10 (4.9) | 1.682 (0.353–1.682) | 0.326 |
| Re-operation | 13 (2.5) | 10 (3.1) | 3 (1.5) | 0.461 (0.125–1.696) | 0.184 |
*χ2 test or Fisher’s exact test where appropriate
#Mann–Whitney U test
We have displayed the outcome in specific disease severity group in Table 4. In complicated appendicitis the overall rate of SSI was 2.6%, of IA was 18.2% and of an ileus was 8.4% of the patients. We noticed that the SSI rate in the laparoscopic appendectomy group was significantly lower compared to the open appendectomy group; 0 vs 6.8% (OR 1.030; 95% CI 0.170–6.242; P = 0.020). No statistical difference was found for IA; 17.9 vs 18.6% (OR 1.051; 95% CI 0.454–4.434; P = 0.535), nor for ileus, 7.4 vs 10.2% (OR 1.423; 95% CI 0.454–4.461; P = 0.372).
Table 4.
30-day complications in complicated appendicitis
| Total | Laparoscopic | Open | Odds ratio (95% CI) | P* | |
|---|---|---|---|---|---|
| Any complication | 44 (28.6) | 25 (26.3) | 19 (32.2) | 1.330 (0.653–2.710) | 0.466 |
| Infectious complication | |||||
| Any infectious | 32 (20.8) | 17 (17.9) | 15 (24.4) | 1.564 (0.712–3.435) | 0.180 |
| Superficial surgical site infection | 4 (2.6) | 0 (0.0) | 4 (6.8) | 1.030 (0.170–6.242) | 0.020 |
| Intra-abdominal abscess | 28 (18.2) | 17 (17.9) | 11 (18.6) | 1.051 (0.454–2.434) | 0.535 |
| Ileus | 13 (8.4) | 7 (7.4) | 6 (10.2) | 1.423 (0.454–4.461) | 0.372 |
| Hospital re-admittance | 21 (13.6) | 14 (14.7) | 7 (11.9) | 0.779 (0.295–2.058) | 0.401 |
| Re-operation | 10 (6.5) | 8 (8.4) | 2 (3.4) | 0.382 (0.078–1.862) | 0.187 |
*χ2 test or Fisher’s exact test where appropriate
Factors of increasing the risk of any infectious complication are listed in Table 5. Children under 6 had a higher chance of developing an IA (P = 0.002). No difference in infectious complications was found in the other age groups. There was no difference in open or laparoscopic approach with regard to developing an IA (P = 1.000).
Table 5.
Infectious complication causes
| Superficial surgical site infection | P* | Intra-abdominal abscess | P* | |
|---|---|---|---|---|
| Approach | 0.087 | 0.566 | ||
| Laparoscopic | 3 (0.9) | 19 (6.0) | ||
| Open | 6 (2.9) | 12 (5.9) | ||
| Age | 0.448 | 0.002 | ||
| 0–5 | 1 (3.6) | 6 (21.4) | ||
| 6–11 | 5 (2.4) | 12 (5.7) | ||
| 12–17 | 3 (1.1) | 13 (4.6) | ||
| Gender | 0.334 | |||
| Male | 6 (1.9) | 17 (5.4) | ||
| Female | 3 (1.4) | 14 (6.7) | ||
| Day since onset complaints median | 0.352 | 0.001 | ||
| <3 days | 6 (1.5) | 13 (3.2) | ||
| ≥ 3 days | 3 (2.5) | 18 (14.8) | ||
| Migration of pain | 0.753 | 0.223 | ||
| Yes | 3 (1.4) | 8 (3.8) | ||
| No | 6 (2.0) | 22 (7.5) | ||
| Temperature | 0.632 | 0.100 | ||
| ≤37.4 | 3 (1.2) | 7 (2.9) | ||
| >37.4 | 5 (2.0) | 23 (9.2) | ||
| Leucocytes (mmol/ml) | 0.219 | 0.142 | ||
| ≤ 13.6 | 1 (0.5) | 7 (3.5) | ||
| > 13.6 | 8 (2.5) | 24 (7.5) | ||
| CRP | 0.235 | 0.001 | ||
| ≤ 39 | 3 (1.0) | 5 (1.6) | ||
| > 39 | 6 (2.9) | 26 (12.6) | ||
| Imaging conclusion | 0.035 | 0.001 | ||
| Uncomplicated | 5 (1.3) | 13 (3.3) | ||
| Complicated | 4 (5.2) | 13 (16.9) | ||
| Not conclusive | 0 (0) | 4 (8.5) | ||
| Intra-operative diagnosis | 0.256 | 0.001 | ||
| Complicated | 4 (2.6) | 28 (18.2) | ||
| Simple | 5 (1.4) | 4 (0.8) | ||
| Surgeon | 0.266 | 0.371 | ||
| Consultant or resident with supervision | 9 (2.0) | 28 (6.2) | ||
| Resident alone | 0 (0.0) | 3 (4.2) | ||
| Operating time | 0.714 | 0.002 | ||
| < 60 min | 8 (1.9) | 18 (4.2) | ||
| ≥ 60 min | 1 (1.6) | 9 (14.8) | ||
| Missing | 0 | 4 (11.4) | ||
| Antibiotics | 0.427 | 0.001 | ||
| No | 0 (0.0) | 0 (0.0) | ||
| Perioperative < 24 h | 5 (1.3) | 3 (0.8) | ||
| Prolonged for complicated appendicitis | 4 (2.9) | 28 (20.4) |
*χ2 test or Fisher’s exact test where appropriate
In binary logistic regression analysis no difference was found in overall incidence of surgical site infections (OR 0.313; 95% CI 0.77–1.267; P = 0.104) or intra-abdominal abscesses (OR 1.013; 95% CI 0.481–2.135; P = 0.972) between the laparoscopic or open approach.
In multivariate analysis, complicated appendicitis shows to be the only independent risk factor for any infectious complication, Table 6.
Table 6.
Multivariate analysis for infectious complications
| OR | 95% CI | P | |
|---|---|---|---|
| Approach | 0.900 | 0.409–1.982 | 0.794 |
| Age < 6 | 2.614 | 0.829–8.241 | 0.101 |
| Complicated appendicitis | 10.770 | 3.978–29.157 | 0.001 |
| Imaging results | 1.856 | 0.815–4.229 | 0.141 |
Multivariate binary logistic regression
Discussion
This national cohort study shows that since the introduction of our national guideline, the majority of children undergo preoperative imaging studies. This has led to a low normal appendix rate of 3.1%. Furthermore, there was no significant overall difference in SSI and IA between the laparoscopic and open approach in children with acute appendicitis. However, we found a significant difference in infectious complications between complicated and uncomplicated appendicitis. Our study shows less SSI in the laparoscopic approach with no increase in the IA for patients with complicated appendicitis. Complicated appendicitis is identified as the sole risk factor for any infectious complication.
In literature, inconsistent results have been published both in the adult and pediatric population regarding the potential benefits and harms of laparoscopic appendectomy. A Cochrane review reported a slightly lower incidence of superficial surgical site infections in the laparoscopic technique, but an increased risk (nearly twofold) of IA after laparoscopic appendectomy, although results should be interpreted with care due to the quality of this studies [11]. In children, the same hazard of IA is noted after laparoscopic appendectomy after complicated appendicitis in several meta-analysis although large, well-designed RCTs on this subject in children are needed [5, 12]. Our results are comparable with other studies mentioning that the surgical approach does not affect the incidence of intra-abdominal abscesses, but the severity of the appendicitis (uncomplicated versus complicated) does [13].
We showed a low normal appendix rate. This is most likely due to the high level of preoperative imaging and accuracy. The Dutch appendicitis guideline was implemented in 2010. In our study, the first post guideline, almost all children had preoperative imaging and, in accordance with these national guidelines, ultrasound was most commonly used. Before implementation of the guidelines a baseline survey showed a normal appendix rate of 15.9%, it also showed that preoperative imaging was performed in only 44.2% [14]. Although appendicitis scoring systems like the Alvarado score can be of aid, they are known to be not accurate enough to predict acute appendicitis in children [15].
CT, and in children mainly MRI, are known for high sensitivity in diagnosing appendicitis [16, 17]. But costs, radiation exposure with potential negative effects from CT-scan and availability need to be considered. New combined diagnostic strategies are being developed to increase sensitivity as far as possible with respect to cost and availability [18], and recent studies show that mandatory imaging in suspected appendicitis is cost efficient [19, 20].
In 50% of children with a intraoperative normal appendix the preoperative imaging was inconclusive for appendicitis, therefore surgery, in particular laparoscopy, can be seen as part of the diagnostic algorithm.
Our study is in line with other studies that showed that decreasing age comes with an increase in complicated appendicitis, this could be because of a diagnostic challenge in very young children [21, 22], or because complicated appendicitis is a different entity and more frequently seen in young children. As a consequence the IA rate is also profoundly increased in this group.
Our study shows that although the majority of all children are operated laparoscopically, the open approach is mostly applied in children under 6-years-old. The difference in approach in the youngest age group might be because of use of specific pediatric instruments, or expected difficulty of procedures. Although the laparoscopic approach has therapeutic and diagnostic advantages in the general population [23, 24], in young children these advantages have so far never been proved although faster recovery is frequently reported in laparoscopy [25]. The high percentage of boys in our population (60%), was a surprise and cannot satisfactorily be explained.
Nowadays complicated appendicitis is believed to be a different entity than uncomplicated appendicitis [6]. In this cohort 28.7% of cases were defined as complicated appendicitis, and it was the only independent risk factor for infectious complications. Complicated appendicitis was equally divided between laparoscopic and open approach, as was the preoperative suspicion of complicated appendicitis on imaging and the final histological conclusion. In complicated appendicitis a higher rate of SSI was found in the open technique, but no difference in IA. In our opinion this is explained by the fact that during open appendectomy the layers of the abdominal wall are exposed to the inflamed appendix and in some cases also purulent fluid. In the laparoscopic approach the abdominal wall is protected. Other complications were equally distributed. Overall conversion rate was very low, 1.7%, and in complicated appendicitis a 5.2%. Conversion rate is much lower than historical cohorts reported [26, 27], this could be because in these historical cohorts surgeons may still have been in there learning curve. Conversion in our study was mostly because of a large abscess or infiltrate with insufficient overview.
More and more studies are being published on conservative treatment of acute appendicitis, comparing initial non-operative treatment with antibiotics versus appendectomy in uncomplicated appendicitis, which might be a safe option [7, 28, 29]. To start the appropriate treatment regime, correct preoperative discrimination between uncomplicated and complicated appendicitis with the help of imaging studies is crucial. In this prospective cohort study all consecutive children undergoing appendectomy for suspected acute appendicitis were included. This provides a veracious overview of the current treatment of appendicitis and the complications of appendectomy for acute appendicitis, whereas randomized trials use strict in and exclusion criteria. The downsides of this cohort study, a wide variety of treatment modalities were used in the participating centers, and the risk of inter observer variation due to the multiple operating surgeons were minimized by the appointment of one local researcher. This local researcher was responsible for data collection and entry.
Our study shows that laparoscopic approach in pediatric appendicitis is safe, with no overall differences in infectious complications compared to the open approach.
The routine use of preoperative imaging, as dictated by national guidelines, most likely results in a low normal appendix rate in children. Although imaging accuracy was acceptable, it was, in multivariable analysis, not able to predict complicated appendicitis. This needs to be improved to safely expand studies of non-operative treatment regimes.
Complicated appendicitis is identified as the only independent risk factor for infectious complications and the laparoscopic, when compared to the open approach in complicated appendicitis, causes less SSI and an equal incidence of IA.
Acknowledgements
Snapshot Appendicitis Collaborative Study Group: Van AckerGJ, Akkermans B, AkkersdijkGJ, Algie GD, Allema JH, Andeweg CS, Appeldoorn N, van Baal JG, den Bakker CM, Bartels SA, van den Berg C, Boekestijn, B, den Boer FC, Boerma D, van den Boom AL, Boute MC, Bouwense SA, Bransen J, van Brussel FA, Busch OR, de Castro SM, Cense HA, Croese, C, van dalen T, Dawson I, van Dessel E, Dettmers R, DharN, Dohmen FY, van Dongen KW, van Duijvendijk P, DulferRR, Dwars BJ, Eerenberg JP, van der Elst M, van den Ende E, Fassaert LM, Fikkers JT, Foppen, JW, Furnee, EJ, Garssen FP, Gerhards MF, van Goor H, de Graaf JS, Graat LJ, Grootr J, van der Ham AC, Hamming JF, Hamminga JT, van der Harst E, Heemskerk J, Heijne A, Heikens JT, Heineman E, Hertogs R, van Heurn E, van den Hil LC, Hooftwijk AG, Hulsker CC, Hunen DR, Ibelings MS, Klaase JM, Klicks R, Knaapen L, Kortekaas RT, Kruyt F, Kwant S, Lases SS, LettingaT, Loupatty A, Matthijsen RA, Minnee RC, Mirck B, Mitalas L, Moes D, Moorman AM, Nieuwenhuijs VB, Nieuwenhuizen GA, Nijk PD, Omloo JM, Ottenhof AG, Palamba HW, van der Peet DL, Pereboom IT, Plaisier PW, van der Ploeg AP, Raber MH, Reijen MM, Rijna H, Rosman C, Roumen RM, Scmitz RF, Schouten van der Velden AP, Scheurs WH, Sigterman TA, Smeets HJ, Sonnevled DJ, Sosef MN, Spoor SF, Stassen LP, van Steensel L, Stortelder E, Straatman J, van Susante HJ, Suykerbuyk de Hoog DE, Terwisscha van Scheltinga C, Toorenvliet BR, Verbeek PC, Verseveld M, Volders JH, Vriens MR, Vriens PW, Vrouenraets BC, van de wall BJ, Wegdam JA, WesterduinE, Wever JJ, Wijfels NA, Wijnhoven BP, Winkel TA, van der Zee DC Zeillemaker AM, Zietse C.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was waived by the institutional review board of the Academic Medical Centre Amsterdam. For reason of the audit design of the study.
Footnotes
The Snapshot Appendicitis Collaborative Study Group collaborators are listed in Acknowledgements section.
References
- 1.Blakely ML, Spurbeck WW, Lobe TE. Current status of laparoscopic appendectomy in children. Semin Pediatr Surg. 1998;7(4):225–227. doi: 10.1016/S1055-8586(98)70035-6. [DOI] [PubMed] [Google Scholar]
- 2.McBurney C. The incision made in the abdominal wall in cases of appendicitis, with a description of a new method of operating. Ann Surg. 1894;20:38–43. doi: 10.1097/00000658-189407000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Kok HJ. A new technique for resecting the non-inflamed not-adhesive appendix through a mini-laparotomy with the aid of the laparoscope. Arch Chirurgicum Neerlandicum. 1977;29(3):195–198. [PubMed] [Google Scholar]
- 4.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132(5):910–925. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 5.Markar SR, Blackburn S, Cobb R, Karthikesalingam A, Evans J, Kinross J, et al. Laparoscopic versus open appendectomy for complicated and uncomplicated appendicitis in children. J Gastrointest Surg. 2012;16(10):1993–2004. doi: 10.1007/s11605-012-1962-y. [DOI] [PubMed] [Google Scholar]
- 6.Livingston EH, Woodward WA, Sarosi GA, Haley RW. Disconnect between incidence of nonperforated and perforated appendicitis: implications for pathophysiology and management. Ann Surg. 2007;245(6):886–892. doi: 10.1097/01.sla.0000256391.05233.aa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gorter RR, van der Lee JH, Cense HA, Kneepkens CM, Wijnen MH, In ‘t Hof KH, et al. Initial antibiotic treatment for acute simple appendicitis in children is safe: Short-term results from a multicenter, prospective cohort study. Surgery. 2015;157(5):916–923. doi: 10.1016/j.surg.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 8.Di Saverio S, Sibilio A, Giorgini E, Biscardi A, Villani S, Coccolini F, et al. The NOTA Study (Non Operative Treatment for Acute Appendicitis): prospective study on the efficacy and safety of antibiotics (amoxicillin and clavulanic acid) for treating patients with right lower quadrant abdominal pain and long-term follow-up of conservatively treated suspected appendicitis. Ann Surg. 2014;260(1):109–117. doi: 10.1097/SLA.0000000000000560. [DOI] [PubMed] [Google Scholar]
- 9.van Rossem CC, Bolmers MD, Schreinemacher MH, van Geloven AA, Bemelman WA. Prospective nationwide outcome audit of surgery for suspected acute appendicitis. Br J Surg. 2016;103(1):144–151. doi: 10.1002/bjs.9964. [DOI] [PubMed] [Google Scholar]
- 10.Vather R, Trivedi S, Bissett I. Defining postoperative ileus: results of a systematic review and global survey. J Gastrointest Surg. 2013;17(5):962–972. doi: 10.1007/s11605-013-2148-y. [DOI] [PubMed] [Google Scholar]
- 11.Sauerland S, Jaschinski T, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 2010(10):Cd001546 [DOI] [PubMed]
- 12.Zhang S, Du T, Jiang X, Song C. Laparoscopic appendectomy in children with perforated appendicitis: a meta-analysis. Surg Laparosc Endosc Percutan Tech. 2017;27(4):262–266. doi: 10.1097/SLE.0000000000000411. [DOI] [PubMed] [Google Scholar]
- 13.Nataraja RM, Teague WJ, Galea J, Moore L, Haddad MJ, Tsang T, et al. Comparison of intraabdominal abscess formation after laparoscopic and open appendicectomies in children. J Pediatr Surg. 2012;47(2):317–321. doi: 10.1016/j.jpedsurg.2011.11.023. [DOI] [PubMed] [Google Scholar]
- 14.Bakker OJ, Go PM, Puylaert JB, Kazemier G, Heij HA. Guideline on diagnosis and treatment of acute appendicitis: imaging prior to appendectomy is recommended. Nederlands tijdschrift voor geneeskunde. 2010;154:A303. [PubMed] [Google Scholar]
- 15.Macco S, Vrouenraets BC, de Castro SM. Evaluation of scoring systems in predicting acute appendicitis in children. Surgery. 2016;160(6):1599–1604. doi: 10.1016/j.surg.2016.06.023. [DOI] [PubMed] [Google Scholar]
- 16.Koning JL, Naheedy JH, Kruk PG. Diagnostic performance of contrast-enhanced MR for acute appendicitis and alternative causes of abdominal pain in children. Pediatr Radiol. 2014;44(8):948–955. doi: 10.1007/s00247-014-2952-x. [DOI] [PubMed] [Google Scholar]
- 17.Thieme ME, Leeuwenburgh MM, Valdehueza ZD, Bouman DE, de Bruin IG, Schreurs WH, et al. Diagnostic accuracy and patient acceptance of MRI in children with suspected appendicitis. Eur Radiol. 2014;24(3):630–637. doi: 10.1007/s00330-013-3044-2. [DOI] [PubMed] [Google Scholar]
- 18.Atema JJ, van Rossem CC, Leeuwenburgh MM, Stoker J, Boermeester MA. Scoring system to distinguish uncomplicated from complicated acute appendicitis. Br J Surg. 2015;102(8):979–990. doi: 10.1002/bjs.9835. [DOI] [PubMed] [Google Scholar]
- 19.Lahaye MJ, Lambregts DM, Mutsaers E, Essers BA, Breukink S, Cappendijk VC, et al. Mandatory imaging cuts costs and reduces the rate of unnecessary surgeries in the diagnostic work-up of patients suspected of having appendicitis. Eur Radiol. 2015;25(5):1464–1470. doi: 10.1007/s00330-014-3531-0. [DOI] [PubMed] [Google Scholar]
- 20.Boonstra PA, van Veen RN, Stockmann HB. Less negative appendectomies due to imaging in patients with suspected appendicitis. Surg Endosc. 2015;29(8):2365–2370. doi: 10.1007/s00464-014-3963-2. [DOI] [PubMed] [Google Scholar]
- 21.Lee SL, Stark R, Yaghoubian A, Shekherdimian S, Kaji A. Does age affect the outcomes and management of pediatric appendicitis? J Pediatr Surg. 2011;46(12):2342–2345. doi: 10.1016/j.jpedsurg.2011.09.030. [DOI] [PubMed] [Google Scholar]
- 22.Nance ML, Adamson WT, Hedrick HL. Appendicitis in the young child: a continuing diagnostic challenge. Pediatr Emerg Care. 2000;16(3):160–162. doi: 10.1097/00006565-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Wei HB, Huang JL, Zheng ZH, Wei B, Zheng F, Qiu WS, et al. Laparoscopic versus open appendectomy: a prospective randomized comparison. Surg Endosc. 2010;24(2):266–269. doi: 10.1007/s00464-009-0563-7. [DOI] [PubMed] [Google Scholar]
- 24.Larsson PG, Henriksson G, Olsson M, Boris J, Stroberg P, Tronstad SE, et al. Laparoscopy reduces unnecessary appendicectomies and improves diagnosis in fertile women. A randomized study. Surg Endosc. 2001;15(2):200–202. doi: 10.1007/s004640000255. [DOI] [PubMed] [Google Scholar]
- 25.Aziz O, Athanasiou T, Tekkis PP, Purkayastha S, Haddow J, Malinovski V, et al. Laparoscopic versus open appendectomy in children: a meta-analysis. Ann Surg. 2006;243(1):17–27. doi: 10.1097/01.sla.0000193602.74417.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andersson RE. Short-term complications and long-term morbidity of laparoscopic and open appendicectomy in a national cohort. Br J Surg. 2014;101(9):1135–1142. doi: 10.1002/bjs.9552. [DOI] [PubMed] [Google Scholar]
- 27.Masoomi H, Nguyen NT, Dolich MO, Mills S, Carmichael JC, Stamos MJ. Laparoscopic appendectomy trends and outcomes in the United States: data from the Nationwide Inpatient Sample (NIS), 2004–2011. Am Surg. 2014;80(10):1074–1077. [PubMed] [Google Scholar]
- 28.Svensson JF, Patkova B, Almstrom M, Naji H, Hall NJ, Eaton S, et al. Nonoperative treatment with antibiotics versus surgery for acute nonperforated appendicitis in children: a pilot randomized controlled trial. Ann Surg. 2015;261(1):67–71. doi: 10.1097/SLA.0000000000000835. [DOI] [PubMed] [Google Scholar]
- 29.Georgiou R, Eaton S, Stanton MP, Pierro A, Hall NJ. Efficacy and safety of nonoperative treatment for acute appendicitis: a meta-analysis. Pediatrics. 2017;139(3):e20163003. doi: 10.1542/peds.2016-3003. [DOI] [PubMed] [Google Scholar]