Abstract
Background: Breastfeeding has multiple benefits for both mother and infant. Previous studies have shown that Hispanic/Latina women have higher rates of breastfeeding and better health outcomes than non-Hispanic black (NHB) women of similar socioeconomic status. Our primary objective was to explore the association of race/ethnicity with breastfeeding rates and the impact of socioeconomic factors on initiation and continuation of breastfeeding.
Materials and Methods: We performed a hypothesis-generating secondary analysis of a prospective cohort study of perinatal mental health in a diverse sample of 213 mothers. Twenty-eight participants self-identified as non-Hispanic white, 43 as NHB, and 142 as Hispanic/Latina. We examined bivariate relationships and performed logistic regression analysis for a series of maternal, infant, and psychosocial factors to examine their individual effect on the breastfeeding and race/ethnicity relationship odds ratio (OR).
Results: Hispanic/Latina women were more likely to initiate exclusive breastfeeding at delivery compared with NHB women (OR 2.4, 95% confidence interval: 1.2–4.9, p = 0.01). Adjustment for maternal, infant, and psychosocial factors measured did not statistically significantly attenuate the OR for initiation of breastfeeding between NHB and Hispanic/Latina women. Women with a history of sexual abuse were also more likely to initiate exclusive breastfeeding (67%) compared with women without a sexual abuse history (54%, p < 0.05).
Conclusions: In this low socioeconomic status cohort study, Hispanic/Latina women had higher proportions of any amount of breastfeeding compared with their NHB counterparts. This difference was not attenuated by any of the maternal, infant, or psychosocial factors examined, although our secondary analysis of this prospective cohort was limited by the available covariates in the parent study.
Keywords: : breastfeeding, race/ethnicity, Hispanic, Latina, socioeconomic status, abuse history
Introduction
Compared with formula feeding, exclusive breastfeeding has multiple benefits for both mother and infant. Compared with formula-fed infants, those fed breast milk have fewer episodes of otitis media, gastrointestinal and respiratory infections, diabetes, allergies, sudden infant death syndrome, and infant mortality of all causes.1 With this wealth of evidence, the American Academy of Pediatrics and the American College of Obstetrics and Gynecology recommend exclusive breastfeeding for 6 months postpartum.1,2 In addition, cost saving projections suggest that if 90% of women were able to exclusively breastfeed for 6 months and continue through 1 year for each child, the U.S. healthcare system would avert 3,340 deaths and save $3.0 billion annually.3 Despite this evidence, 17.5% of U.S. women do not initiate breastfeeding, and just 24.9% reach 6 months of exclusive breastfeeding.4 Infant feeding is affected by multiple contributing socioeconomic and medical factors including unplanned pregnancy,5 postpartum depression,6 employment,7 parity,8 education status,9,10 support from partner,11 obesity,12 geographic location,13 and maternal age.8,14
Although breastfeeding has proven benefits for both mother and baby, stark differences in breastfeeding rates among race/ethnicity groups exist in the United States. In 2014, 84.8% of Hispanic/Latina and 85.7% of non-Hispanic white (NHW) women ever breastfed their infants at any time in the postpartum period. In comparison, only 68.0% of non-Hispanic black (NHB) ever breastfed their infants.4 In research studies, this difference in breastfeeding rates of Hispanic/Latina women compared with NHB women persists after adjustment for socioeconomic status and extends to multiple other health outcomes.15–18
Researchers have attempted to explain why Hispanic/Latina women in the United States seem to have better health outcomes compared with other women of similar socioeconomic status. Markides and Coreil first described this phenomenon in 1986 and labeled it the “Hispanic paradox.”18 The “Hispanic Paradox” describes the phenomenon that Hispanic/Latina women have better health outcomes than NHB women in multiple areas of health outcomes, despite similar socioeconomic status.19
Several hypotheses exist on why the “Hispanic paradox” exists, including immigration status,20 healthy migrant effect (theory that healthier people migrate to a new country), return migrant effect (theory that sick migrants will return to their country of origin), and ethnic enclave advantage (migrants tend to live in close-knit communities that provide strong social support).19 No consensus has emerged to explain the “Hispanic paradox” advantage in multiple health outcomes, including breastfeeding.20 Our objective was to measure the association between race/ethnicity and breastfeeding and quantify the impact of other socioeconomic factors on initiation and continuation of breastfeeding. We hypothesized that compared with NHB women, Hispanic/Latina women would have higher rates of breastfeeding. We further hypothesized that maternal social support be associated with more breastfeeding, and depression, anxiety, and stress would be associated with reduced breastfeeding.
Materials and Methods
Setting and participants
This is a secondary analysis of a longitudinal cohort study performed at the University of North Carolina at Chapel Hill. The primary aim of the parent study was to quantify the association between thyroid function and postpartum depression.21 Participants were enrolled in the initial study if they were in their third trimester of pregnancy and receiving prenatal care from the Wake County Health Department in Raleigh, NC. Exclusion criteria included abnormal thyroid function, history of mental disorders or substance abuse, body mass index (BMI) >35 or <18, heavy smoking, and other serious medical complications. Details of the inclusion and exclusion criteria have been previously published.21 Participants were assessed at enrollment, in the third trimester (35–36 weeks gestation), 6 weeks postpartum, and 12 weeks postpartum. After enrollment, all subsequent visits were conducted in the participant's home. All study staff who conduced visits were fluent in both English and Spanish, and all questionnaires were available in both languages. All participants with available breastfeeding outcomes and known race/ethnicity from the original study were included (N = 213) in this secondary analysis (Fig. 1). Eighty-seven participants were excluded due to missing values for either race/ethnicity (n = 7), missing breastfeeding status at delivery (n = 70), or not self-identifying as NHB, NHW, or Hispanic [Asian (n = 3), American Indian (n = 2), or other (n = 3)] due to small numbers. Excluded women were more likely to speak English, have a lower BMI, and have lower parity than included women (p < 0.05 for comparisons).
FIG. 1.
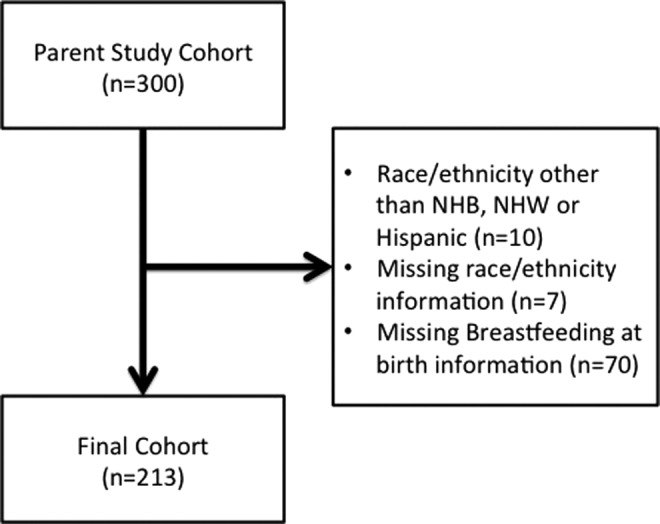
Flow diagram for inclusion into secondary analysis. NHB, non-Hispanic black; NHW, non-Hispanic white.
Variables
Our primary outcome was breastfeeding initiation at delivery. Our secondary outcomes included breastfeeding at 6 and 12 weeks postpartum. Race/ethnicity was self-identified by the participants as Hispanic/Latina, NHB, or NHW.
Breastfeeding
Breastfeeding data were collected at two time points. At 6 weeks postpartum, women were asked how they fed their infants at delivery and how they were currently feeding. At 12 weeks postpartum, women were how they were currently feeding. The questions were phrased as “When your baby was first born, did you breast or bottle (formula) feed?” and “Are you currently breast or bottle (formula) feeding your baby?” with options for breast fed only, bottle fed only, and both breast and bottle fed. Exclusive breastfeeding at each time point was defined as participants who reported “breast fed only.” Any breastfeeding was defined as participants who reported “breast fed only” or “both breast and bottle fed.”
Maternal demographic characteristics
Additional demographic characteristics collected included age (in years), income (in thousands of dollars), marital status (single/divorced versus in an intimate relationship), education (in years), and postpartum employment or schooling. Information collected about pregnancy included gestational age at first visit (in weeks), gestational age at delivery (in weeks), birth weight of the infant (in grams), cesarean section or vaginal delivery, whether the pregnancy was desired, and if it was planned. Desired pregnancy was assessed at the third trimester visit with the following question: “At the time you found out you were pregnant, was this pregnancy wanted or unwanted?” Planned pregnancy was assessed by asking the following question: “At the time you became pregnant, were you actually trying to get pregnant or did it just ‘happen’?”
Maternal psychosocial factors
Participants enrolled in the parent study completed several validated questionnaires to measure psychosocial factors. Mental health factors collected included the Edinburgh Postnatal Depression Scale (EPDS) score,22 the Medical Outcomes Study (MOS) social support survey,23 Mini-International Neuropsychiatric Interview (MINI),24 history of sexual abuse, and history of physical abuse.25 The abuse history was assessed as part of a comprehensive 55-question survey about trauma and abuse history. For example, one of the questions about sexual abuse stated, “Did anyone ever make you have sexual intercourse (vaginal or anal intercourse) by using force or threatening to harm you?” Baseline EPDS score was defined as the mean of the third trimester scores (screening and baseline scores). Major and minor depression diagnoses were determined at baseline and 12 weeks postpartum by using the modified MINI Plus 5.0.0 International Neuropsychiatric Interview. Inter-rater reliability was measured and deemed acceptable between the trained staff and a board-certified psychiatrist for the psychiatric instruments.21 An expert in trauma trained all staff on administration of the trauma interview and reviewed all recorded trauma.
Analysis
We started by performing analyses to examine distributions and evaluate for outliers in the exposure, outcome, and confounder variables. For categorical variables, we tabulated frequencies, and for continuous variables we calculated mean, range, and standard deviation and examined distributions for skew and collinearity. To examine baseline characteristic distributions by race/ethnicity and breastfeeding outcome, Chi-squared tests were used for categorical variables and one-way analysis of variance tests were used for continuous variables. In cases of cell sizes less than five, we used Fisher's exact tests. Bivariable analyses were used to assess the relationship between race/ethnicity and breastfeeding for mothers who breastfed and those who combined breast and bottle. We performed logistic regression analysis for breastfeeding at delivery by race/ethnicity by adjusting for multiple maternal, infant, and psychosocial factors. Due to the small sample size and inability to control for all covariates, covariates that were significant in the bivariate analyses by race/ethnicity or breastfeeding were included in the final adjusted model. These cofactors included the following: age, income, using federal supplemental nutrition—Women, Infants, and Children (WIC), education, planned pregnancy, gestational age at delivery, birth weight, baseline EPDS score, and history of sexual abuse. (Of note, language was not included in the adjusted model due to the variable's collinearity with race/ethnicity.) All analyses were conducted in STATA/SE 14.1 (StataCorp, Inc., College Station, TX) with alpha level 0.05. The University of North Carolina Institutional Review Board (IRB) and the Wake County Human Services Board approved the original study, and the secondary analysis was deemed exempt from IRB approval by the University of North Carolina IRB.
Results
Of the 213 included women, 28 (13%) were NHW, 43 (20%) were NHB, and 142 (67%) were Hispanic/Latina (Table 1). All continuous variables were normally distributed. As noted in Table 1, our cohort was low income with a high prevalence of receiving government assistance. Median household income was $10,000–$20,000 annually. The majority of participants (92%) were enrolled in the WIC supplemental food program, and participants reported a high proportion (37%) of unplanned and undesired pregnancies.
Table 1.
Baseline Demographic Characteristics and Psychosocial Characteristics by Race/Ethnicity
| Maternal factors | Overall (N = 213) | NHW (N = 28, 13%) | NHB (N = 43, 20%) | Hispanic/Latina (N = 142, 67%) |
|---|---|---|---|---|
| Age (mean, SD)a | 26 (5.6) | 25 (6.2) | 23 (5.0) | 27 (5.4) |
| Income (median income range)a | 10–20K | 20–30K | 10–20K | 10–20K |
| Single/divorced, n (%) | 30 (14) | 4 (14) | 11 (26) | 15 (11) |
| Using WIC,a,bn (%) | 190 (92) | 20 (80) | 37 (88) | 133 (95) |
| Primary language: English,an (%) | 80 (38) | 27 (96) | 43 (100) | 10 (7) |
| Education, years (mean, SD)a | 11 (3.0) | 12 (1.8) | 12 (2.1) | 10 (3.1) |
| GA at first visit, weeks (mean, SD) | 14 (5) | 15 (5) | 14 (5) | 13 (5) |
| Unemployed postpartum,bn (%) | 135 (65) | 14 (56) | 24 (57) | 97 (69) |
| Attitude toward pregnancy,an (%) | ||||
| Planned and desired | 58 (27) | 4 (14) | 5 (12) | 49 (35) |
| Unplanned and desired | 76 (36) | 14 (50) | 17 (40) | 45 (32) |
| Unplanned and undesired | 79 (37) | 10 (36) | 21 (49) | 48 (34) |
| GA at delivery, weeks (mean, SD)a | 39 (1.3) | 40 (1) | 39 (1) | 39 (1) |
| Birth weight, grams (mean, SD)a | 3,372 (474) | 3,571 (492) | 3,202 (432) | 3,384 (468) |
| Cesarean section, n (%) | 36 (17) | 4 (14) | 9 (21) | 23 (16) |
| Social Support MOS baseline score (mean, SD) | 4.0 (0.7) | 4.4 (0.5) | 4.2 (0.6) | 3.8 (0.8) |
| EPDS baseline score (mean, SD)a | 7.1 (4.7) | 5.3 (3.5) | 8.2 (5.0) | 7.2 (4.7) |
| Major depression at baseline on MINI, n (%) | 16 (8) | 1 (4) | 6 (14) | 9 (6) |
| Major depression at 12 weeks on MINI,bn (%) | 12 (6) | 1 (4) | 2 (5) | 9 (6) |
| History of sexual abuse,a,bn (%) | 52 (25) | 12 (48) | 11 (26) | 29 (21) |
| History of physical abuse,bn (%) | 96 (46) | 10 (40) | 14 (33) | 72 (51) |
p = <0.05.
Six missing values.
EPDS, Edinburgh Postpartum Depression Scale; GA, gestational age; MINI, Mini International Neuropsychiatric Interview; MOS, Medical Outcomes Study; NHB, non-Hispanic black; NHW, non-Hispanic white; SD, standard deviation; WIC, Women, Infants, and Children.
Baseline characteristics by race/ethnicity
Hispanic/Latina women were significantly older than the NHB participants (27 ± 5 versus 23 ± 5 years, p < 0.001) (Table 1). NHB participants were more likely to be single or divorced compared with NHW or Hispanic/Latina women (26% versus 14% versus 11%, p = 0.054). NHW and NHB women were less likely to have planned and desired pregnancies compared with Hispanic/Latina women (14%, 12%, and 35%, p = 0.01). A higher proportion of Hispanic/Latina women (95%) were using WIC compared with NHW (80%) and NHB (88%, p = 0.02). Mean baseline EPDS scores were lowest in the NHW women (5.3 ± 3.5) compared with the NHB (8.2 ± 5.0) and Hispanic/Latina (7.2 ± 4.7, p = 0.03) women.
Baseline characteristics by infant feeding
Age, income, marital status, gestational age at delivery, depression scores, and planned pregnancy did not vary among the exclusive breastfeeding, exclusive bottlefeeding, and both breastfeeding and bottlefeeding groups (Table 2). Primary language also varied by feeding group, with 35% English speakers in the exclusive breastfeeding group and 57% English speakers in the bottlefeeding-only group. Compared with women without sexual or physical abuse, women with a history of sexual or physical abuse were more likely to exclusively breastfeed (54% versus 67%, p = 0.049; and 51% versus 65%, p = 0.055, respectively).
Table 2.
Baseline Demographic Characteristics and Psychosocial Characteristics by Breastfeeding Outcome Immediately Postpartum
| Exclusive breastfeeding (N = 124, 58%) | Bottlefeeding (N = 46, 22%) | Both (N = 43, 20%) | |
|---|---|---|---|
| Age (mean, SD) | 26 (5.6) | 25 (6.0) | 26 (5.3) |
| Income (median income range) | 10–20K | 10–20K | 10–20K |
| Single/divorced, n (%) | 16 (13) | 5 (11) | 9 (21) |
| Using WIC, n (%)a | 107 (90) | 43 (96) | 40 (93) |
| Primary language: English, n (%)b | 43 (35) | 26 (57) | 11 (26) |
| Education (mean, SD) | 11 (3.0) | 11 (3.3) | 11 (2.8) |
| GA at first visit (mean, SD) | 14 (4.9) | 14 (5.5) | 13 (5.5) |
| Unemployed postpartum, n (%)a | 76 (56) | 27 (20) | 32 (24) |
| Attitude toward pregnancy | |||
| Planned and desired, n (%) | 32 (26) | 10 (22) | 16 (37) |
| Unplanned and desired, n (%) | 42 (34) | 17 (37) | 17 (40) |
| Unplanned and undesired, n (%) | 50 (40) | 19 (41) | 10 (23) |
| GA at delivery in weeks (mean, SD) | 39 (1.2) | 39 (1.4) | 40 (1.2) |
| Birth weight, grams (mean, SD)b | 3,387 (423) | 3,231 (502) | 3,478 (547) |
| Cesarean section, n (%) | 17 (14) | 8 (17) | 11 (26) |
| Social Support MOS baseline score (mean, SD) | 4.0 (0.8) | 4.0 (0.7) | 3.9 (0.8) |
| EPDS baseline score (mean, SD) | 7.3 (4.8) | 7.3 (4.9) | 6.6 (4.0) |
| Major depression at baseline on MINI, n (%) | 7 (6) | 7 (15) | 2 (5) |
| Major depression at 12 weeks on MINI,an (%) | 10 (8) | 2 (4) | 0 |
| History of sexual abuse,a,bn (%) | 35 (29) | 5 (11) | 12 (28) |
| History of physical abuse,an (%) | 62 (52) | 14 (31) | 20 (47) |
Six missing values.
p = <0.05.
Breastfeeding by race/ethnicity
Exclusive breastfeeding
Compared with NHB women, Hispanic/Latina women were more likely to exclusively breastfeed immediately postpartum (61% versus 40%, p = 0.002, Table 3). This relationship remained consistent at 6 and 12 weeks (20% versus 14%, p < 0.001; 16% versus 5%, p < 0.001, respectively). Compared with NHB women, the unadjusted odds ratio (OR) and 95% confidence interval (CI) for exclusive breastfeeding were greater for both NHW and Hispanic/Latina women (NHW: 3.8, CI: 1.4–10.6, p = 0.01; Hispanic/Latina: 2.4, CI: 1.2–4.9, p = 0.01, respectively). Of the Hispanic/Latina women, 32% planned to exclusively breastfeed and 61% did exclusively breastfeed at delivery. In the group of NHB women, 30% planned to exclusively breastfeed and 40% did exclusively breastfeed at delivery.
Table 3.
Breastfeeding Outcomes by Race/Ethnicity at Each Time Period
| Postpartum time period | Race/ethnicity | Exclusively breastfeeding, n (%) | Bottle, n (%) | Both, n (%) | Unadjusted odds ratio for exclusive breastfeeding versus bottlefeeding or both | Unadjusted odds ratio for any breastfeeding versus bottlefeeding only |
|---|---|---|---|---|---|---|
| Immediately postpartuma | NHB | 17 (40) | 18 (42) | 8 (19) | Reference | Reference |
| NHW | 20 (71) | 5 (18) | 3 (11) | 3.8 (1.4–10.6) | 3.3 (1.1–10.4) | |
| Hispanic/Latina | 87 (61) | 23 (16) | 32 (23) | 2.4 (1.2–4.9) | 3.7 (1.8–7.9) | |
| 6 Weeksa | NHB | 6 (14) | 28 (65) | 9 (21) | Reference | Reference |
| NHW | 12 (43) | 9 (32) | 7 (25) | 4.6 (1.5–14.5) | 3.9 (1.4–10.8) | |
| Hispanic/Latina | 28 (20) | 27 (19) | 87 (61) | 1.5 (0.6–3.9) | 8.0 (3.7–16.9) | |
| 12 Weeksa,b | NHB | 2 (5) | 33 (79) | 7 (17) | Reference | Reference |
| NHW | 11 (42) | 13 (50) | 2 (8) | 14.7 (2.9–74.0) | 3.7 (1.3–10.6) | |
| Hispanic/Latina | 23 (16) | 38 (27) | 79 (56) | 3.9 (0.89–17.4) | 9.8 (4.3–22.5) |
Fisher's exact test p-value <0.01.
Six missing values.
Any breastfeeding
At delivery, compared with NHB women, Hispanic/Latina women were more likely to report any breastfeeding (combined breastfeeding and both breastfeeding and bottlefeeding groups; 84% versus 59%, p < 0.001). This disparity persisted through the immediate postpartum period to 6 and 12 weeks postpartum when Hispanic/Latina women continued to have higher breastfeeding proportions compared to NHB (Table 3). Compared with NHB women, the unadjusted OR and 95% CI for any breastfeeding at delivery was significantly greater for both NHW and Hispanic/Latina women (NHW: 3.3, CI: 1.1–10.4, p = 0.04; and Hispanic/Latina: 3.7, CI: 1.8–7.9, p = 0.001, respectively).
Logistic regression modeling
After adjustment for multiple covariates, the odds of exclusive breastfeeding in NHW and Hispanic/Latina women at delivery was more than three times higher than NHB women (NHW adjusted OR 3.2, CI: 1.0–10.3, p = 0.047; and Hispanic/Latina 3.5, CI: 1.5–8.3, p = 0.004, Table 4) in our sample. For any breastfeeding at delivery, NHW have 1.4 (CI: 0.4–5.2, p = 0.6) times the odds of any breastfeeding compared with NHB women after adjustment for multiple maternal, infant, and psychosocial factors. Hispanic/Latina women have more than five times the odds (5.1, CI: 1.9–13.8, p = 0.001) of any breastfeeding at delivery compared with NHB women after adjustment. Due to casewise deletion, the adjusted models include 207 women, with 6 women dropped from the multivariate analysis due to missing covariates.
Table 4.
Adjusted Odds Ratio for Breastfeeding Immediately Postpartum
| Race/ethnicity | Unadjusted | Fully adjusted modela | |
|---|---|---|---|
| Exclusive breastfeeding versus bottlefeeding or both | NHB | Reference | Reference |
| NHW | 3.8 (1.4–10.6) | 3.2 (1.0–10.3) | |
| Hispanic/Latina | 2.4 (1.2–4.9) | 3.5 (1.5–8.3) | |
| Any breastfeeding versus bottlefeeding only | NHB | Reference | Reference |
| NHW | 3.3 (1.1–10.4) | 1.4 (0.4–5.2) | |
| Hispanic/Latina | 3.7 (1.8–7.9) | 5.1 (1.9–13.8) |
Adjusted for age, income, using federal supplemental nutrition—WIC, education, planned pregnancy, gestational age at delivery, birth weight, baseline EPDS score, and history of sexual abuse.
Discussion
Our objective was to examine the association between race/ethnicity and exclusive breastfeeding, as well as to evaluate the impact of other socioeconomic factors on initiation and continuation of exclusive breastfeeding in this low-income cohort. We hypothesized that compared with NHB women, Hispanic/Latina women would have a higher prevalence of exclusive breastfeeding. We also hypothesized that higher levels of social support would increase exclusive breastfeeding, and depression and anxiety would decrease exclusive breastfeeding. We elected to use this parent study to explore and refine these hypotheses due to its in-depth assessment of a diverse subset of women, including detailed trauma interview, multiple psychosocial measures, and high percentage of Hispanic women with interviews in their native language.
Our findings extend early work on breastfeeding rates between Hispanic and NHB women. In 2014, 84.8% of Hispanic/Latina and 85.7% of NHW women ever breastfed their infants at any time in the postpartum period. In comparison, only 68.0% of NHB ever breastfed their infants.26 Our results supported this hypothesis as we observed a higher rate of exclusive breastfeeding among Hispanic/Latina women compared with NHB women immediately postpartum through 12 weeks postpartum.
Unplanned pregnancy,5 postpartum depression risk,6 employment,7 parity,8 education status,9,10 support from partner,11 obesity,12 geographic location,13 and maternal age8,14 are all factors that affect breastfeeding outcomes. Contrary to past research, in our cohort, baseline depression and anxiety in the late antepartum period were not associated with differences in breastfeeding.6,27 However, baseline depression was uncommon in our sample (16/213, 7.5%), limiting our power to detect an association. In addition, as our primary outcome was initiation of breastfeeding at delivery, we did not adjust for major depression in the postpartum period due to temporality of the measures.
We had hypothesized that the difference in breastfeeding rates among Hispanic and NHB women resulted from differences in social support or other psychosocial factors. However, after adjustment for each of the statistically significant psychosocial and demographic covariates in our sample, Hispanic/Latina women continued to have higher odds of breastfeeding compared with NHB women immediately postpartum in our cohort. In addition, despite statistically significant lower social support and higher rates of physical abuse in our cohort, Hispanic/Latina women exclusively breastfed at higher rates than NHB women. These findings suggest that socioeconomic status, social support, and mental health status do not fully explain the Hispanic paradox of higher breastfeeding rates in Hispanic/Latina women compared to NHB women. A larger sample size with more episodes of postpartum depression would allow for a complete mediation analysis to examine this possible causal pathway.
Other important possible factors that we were unable to analyze in this analysis include culture, acculturation status, and family support of breastfeeding. Singh et al. have demonstrated an association with breastfeeding status and immigration status.17 Additional factors that contribute to the decision for NHB women to breastfeed include social support and family members' attitudes toward breastfeeding. Having a first-degree relative or close friend who has experience with breastfeeding increases the likelihood of breastfeeding.28
Our analysis was notable for the relatively high proportion of history of physical abuse in the Hispanic/Latina participants (51%) as well as an overall mean of 25% of sexual abuse history for entire cohort, which is comparable to nationwide survey data.29 Despite this history of physical and sexual abuse, women with an abuse history were more likely to breastfeed compared with women who did not have a history of physical or sexual abuse. Although our cohort was small, this association has been reported in other studies. Prentice et al. noted in a nationwide sample of 1,220 mothers that mothers with a history of sexual abuse had over 2.5 times the odds of breastfeeding initiation than those without a history of abuse.30 Kendall-Tackett et al. noted that hours of sleep were higher and depression scores were lower in women with a history of sexual assault who breastfed.31 It has been proposed that this association may be due to parenting attitudes and the desire for a woman with a history of sexual or physical abuse to consciously parent differently,30 leading to an increased breastfeeding rate. On the other hand, other studies have noted that women with history of sexual abuse have higher rates of breastfeeding complications32 and earlier cessation of breastfeeding.33
Our study has several strengths, including a racially and ethnically diverse cohort of participants with a large proportion of Hispanic/Latina women and a comprehensive questionnaire designed to capture detailed trauma and mental health data. However, our findings must be interpreted in the context of the study design and be viewed as hypothesis generating. The main limitation of our secondary analysis was the small sample size of NHB women that precluded predictive modeling and interaction analysis. An a priori sample size calculation was not performed, as this was a secondary analysis of a parent study. In addition, information on acculturation status was not collected, precluding consideration of this confounder in our analysis. The parent study enrolled women with low socioeconomic status, and thus our results cannot be generalized to high-income women. In addition, approximately one-fourth of the participants were excluded from the final analysis due to lack of breastfeeding information, which limits generalizability. Potential misclassification is an important limitation: breastfeeding initiation at delivery was collected retrospectively postpartum, potentially introducing recall bias, and information on timing of introduction of formula or breastfeeding cessation between study assessments was not collected. However, the 6- and 12-week infant feeding patterns were collected prospectively, and higher rates of exclusive breastfeeding and any breastfeeding were noted in Hispanic/Latina women compared to NHB women. Also, participants who were feeding exclusively with pumped breast milk might have selected bottlefeeding as their mode of feeding, although the questions did specify bottlefeeding as formula feeding. Participants might also have been supplementing the breast milk with other solids or liquids other than formula, as this was not specifically addressed.
Conclusion
In conclusion, in this low socioeconomic status cohort, Hispanic/Latina women had higher rates of exclusive breastfeeding compared to their NHB counterparts, which was not explained by the maternal, infant, or psychosocial factors we examined. Due to the fact that this was a secondary data analysis of a small prospective cohort study, these findings should be seen as hypothesis generating rather than interpreted as defining a causal relationship. Future prospective studies are needed, which assess breastfeeding intention, outcomes, and acculturation status. In addition, women with a history of physical or sexual abuse had higher rates of exclusive breastfeeding initiation at delivery than women who did not experience abuse. This finding underscores the importance of individualizing care and tailoring our approach to the specific needs of each woman.
Disclosure Statement
No competing financial interests exist.
References
- 1.American Academy of Pediatrics. Breastfeeding and the use of human milk. Pediatrics 2012;129:e827–e841 [DOI] [PubMed] [Google Scholar]
- 2.American College of Obstetricians and Gynecologists. Committee Opinion No. 658: Optimizing support for breastfeeding as part of obstetric practice. Obstet Gynecol 2016;127:e86–e92 [DOI] [PubMed] [Google Scholar]
- 3.Bartick MC, Schwarz EB, Green BD, et al. Suboptimal breastfeeding in the United States: Maternal and pediatric health outcomes and costs. Matern Child Nutr 2017;13:e12366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. U.S. National Immunization Survey—National and state breastfeeding rates. Available at www.cdc.gov/breastfeeding/data/nis_data Published 2014 (accessed December6, 2017)
- 5.Taylor JS, Cabral HJ. Are woman with an unintended pregnancy less likely to breastfeed? J Fam Pract 2002;51:431–436 [PubMed] [Google Scholar]
- 6.Pitonyak JS, Jessop AB, Pontiggia L, et al. Life course factors associated with initiation and continuation of exclusive breastfeeding. Matern Child Health J 2016;20:240–249 [DOI] [PubMed] [Google Scholar]
- 7.Ogbuanu C, Glover S, Probst J, et al. The effect of maternity leave length and time of return to work on breastfeeding. Pediatrics 2011;127:e1414–e1427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hundalani SG, Irigoyen M, Braitman LE, et al. Breastfeeding among inner-city women: From intention before delivery to breastfeeding at hospital discharge. Breastfeed Med 2013;8:68–72 [DOI] [PubMed] [Google Scholar]
- 9.van Rossem L, Oenema A, Steegers EAP, et al. Are starting and continuing breastfeeding related to educational background? The generation R study. Pediatrics 2009;123:e1017–e1027 [DOI] [PubMed] [Google Scholar]
- 10.Heck KE, Braveman P, Cubbin C, et al. Socioeconomic status and breastfeeding initiation among California mothers. Public Health Rep 2006;121:51–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pisacane A, Continisio GI, Aldinucci M, et al. A controlled trial of the father's role in breastfeeding promotion. Pediatrics 2005;116:e494–e498 [DOI] [PubMed] [Google Scholar]
- 12.Martinez JL, Chapman DJ, Perez-Escamilla R. Prepregnancy obesity class is a risk factor for failure to exclusively breastfeed at hospital discharge among Latinas. J Hum Lact 2016;32:258–268 [DOI] [PubMed] [Google Scholar]
- 13.Belanoff CM, Mcmanus BM, Carle AC, et al. Racial/ethnic variation in breastfeeding across the US: A multilevel analysis from the National Survey of Children's Health, 2007. Matern Child Heal J 2012;16:514–526 [DOI] [PubMed] [Google Scholar]
- 14.Jones JR, Kogan MD, Singh GK, et al. Factors associated with exclusive breastfeeding in the United States. Pediatrics 2011;128:1117–1125 [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Progress in increasing breastfeeding and reducing racial/ethnic differences—United States, 2000–2008 births. MMWR 2013;62:77–80 [PMC free article] [PubMed] [Google Scholar]
- 16.Jones KM, Power ML, Queenan JT, et al. Racial and ethnic disparities in breastfeeding. Breastfeed Med 2015;10:186–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh GK, Kogan MD, Dee DL. Nativity/immigrant status, race/ethnicity, and socioeconomic determinants of breastfeeding initiation and duration in the United States, 2003. Pediatrics 2007;119(Suppl 1):S38–S46 [DOI] [PubMed] [Google Scholar]
- 18.Markides KS, Coreil J. The health of Hispanics in the southwestern United States: An epidemiologic paradox. Public Health Rep 1986;101:253–265 [PMC free article] [PubMed] [Google Scholar]
- 19.Valles SA. The challenges of choosing and explaining a phenomenon in epidemiological research on the “Hispanic Paradox.” Theor Med Bioeth 2016;37:129–148 [DOI] [PubMed] [Google Scholar]
- 20.Gibson-Davis CM, Brooks-Gunn J. Couples' immigration status and ethnicity as determinants of breastfeeding. Am J Public Health 2006;96:641–646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pedersen C, Leserman J, Garcia N, et al. Late pregnancy thyroid-binding globulin predicts perinatal depression. Psychoneuroendocrinology 2016;65:84–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987;150:782–786 [DOI] [PubMed] [Google Scholar]
- 23.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med 1991;32:705–714 [DOI] [PubMed] [Google Scholar]
- 24.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The Development and Validation of a Structured Diagnostic Psychiatric Interview for DSM-IV and ICD-10, Vol 59 Physicians Postgraduate Press, 1998. Available at www.psychiatrist.com/jcp/article/Pages/1998/v59s20/v59s2005.aspx (accessed March7, 2017) [PubMed]
- 25.Leserman J, Pence BW, Whetten K, et al. Relation of lifetime trauma and depressive symptoms to mortality in HIV. Am J Psychiatry 2007;164:1707–1713 [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control. Breastfeeding among U.S. children born 2000–2013. National Immunization Survey. Available at www.cdc.gov/breastfeeding/data/nis_data/rates-any-exclusive-bf-socio-dem-2013.htm (accessed March29, 2017)
- 27.Dennis C-L, McQueen K. The relationship between infant-feeding outcomes and postpartum depression: A qualitative systematic review. Pediatrics 2009;123:e736–e751 [DOI] [PubMed] [Google Scholar]
- 28.DeVane-Johnson S, Woods-Giscomb C, Thoyre S, et al. Integrative literature review of factors related to breastfeeding in African American women: Evidence for a potential paradigm shift. J Hum Lact 2017;33:435–447 [DOI] [PubMed] [Google Scholar]
- 29.Breiding MJ, Smith SG, Basile KC, et al. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization—National intimate partner and sexual violence survey, United States, 2011. MMWR Surveill Summ 2014;63:1–18 [PMC free article] [PubMed] [Google Scholar]
- 30.Prentice JC, Lu MC, Lange L, et al. The association between reported childhood sexual abuse and breastfeeding initiation. J Hum Lact 2002;18:219–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kendall-Tackett K, Cong Z, Hale TW. Depression, sleep quality, and maternal well-being in postpartum women with a history of sexual assault: A comparison of breastfeeding, mixed-feeding, and formula-feeding mothers. Breastfeed Med 2013;8:16–22 [DOI] [PubMed] [Google Scholar]
- 32.Elfgen C, Hagenbuch N, Görres G, et al. Breastfeeding in women having experienced childhood sexual abuse. J Hum Lact 2017;33:119–127 [DOI] [PubMed] [Google Scholar]
- 33.Sørbø MF, Lukasse M, Brantsæter A-L, et al. Past and recent abuse is associated with early cessation of breast feeding: Results from a large prospective cohort in Norway. BMJ Open 2015;5:e009240. [DOI] [PMC free article] [PubMed] [Google Scholar]


