Left ventricular ejection fraction (LVEF) is an important predictor of cardiovascular (CV) mortality in patients with heart failure (HF), and cause of death varies with ejection fraction.1–3 Nevertheless, the influence of LVEF on cause-specific death in HF with preserved ejection fraction (HFpEF) patients is not well described.
We evaluated the influence of LVEF on CV and non-CV deaths in the Treatment of Preserved Cardiac Function Heart Failure with an Aldosterone Antagonist (TOPCAT) study. The TOPCAT trial enrolled HFpEF patients with LVEF ≥45% and assessed the effect of spironolactone on a composite outcome of CV death, aborted cardiac arrest, and hospitalization for HF, over a median follow-up of 42 months.4 LVEF was determined at each site by echocardiography (96.7%), radionuclide ventriculography (2.3%), or angiography (1%).
All endpoints were adjudicated centrally by a blinded clinical endpoint committee. Deaths were classified into three categories: CV, non-CV, and unknown. Cardiovascular deaths were further classified as sudden cardiac death (SCD), and death due to myocardial infarction (MI), pump failure, stroke, or another CV cause. Death was considered non-CV if an unequivocal and documented non-CV cause could be established as the primary cause of death. Cause of death was considered unknown when insufficient data were available to determine the reason to be CV or non-CV.5 We divided the range of LVEFs across the entire TOPCAT trial into four separate categories: ≤47% 48–52% 53–57% and ≥58%. Each of these categories was centered around a multiple of 5, as we observed a substantial ‘digit preference’ for LVEF values in multiples of 5, which has been seen in previous trials.2 Baseline characteristics were summarized for each group, and compared using trend tests.
Unadjusted and age/sex-adjusted incidence rates of cause-specific mortality were calculated across LVEF categories using Poisson regression models. The incident rates and proportions of cause-specific death were compared between the lowest LVEF category vs. others. All these analyses were conducted in the Americas (n=1767) owing to previously noted substantial regional differences in patient demographics, outcomes, and response to spironolactone in the TOPCAT trial.6
Among patients enrolled in Americas, LVEF ranged from 44% to 85% (mean 58%, median 58%, 25th-75th percentile 53–61%). Baseline characteristics varied considerably by LVEF. Patients in higher LVEF categories were older, more likely to be female, and have a history of hypertension, and less likely to be current smokers or have a history of MI, percutaneous coronary intervention, coronary artery bypass graft surgery, or be on beta-blocker, angiotensin-converting enzyme inhibitor/angiotensin receptor blocker, than those with lower LVEFs (all P < 0.05). The crude and age/sex-adjusted annualized rates of all-cause mortality, CV mortality and SCD were highest in the lowest LVEF category as compared to other categories (P <0.001 for all components). Crude and age/sex-adjusted annualized rates of pump failure, MI related, stroke related, non-CV death and unexplained death did not vary across LVEF categories (Figure 1). However, compared to patients with LVEF ≥48% the proportion of SCD in the lowest LVEF category was significantly higher (33% vs. 17% P = 0.007) and numerically higher for CV death (69% vs. 56%, P = 0.11) and lower for non-CV death (22% vs. 33%, P = 0.13).
Figure 1.
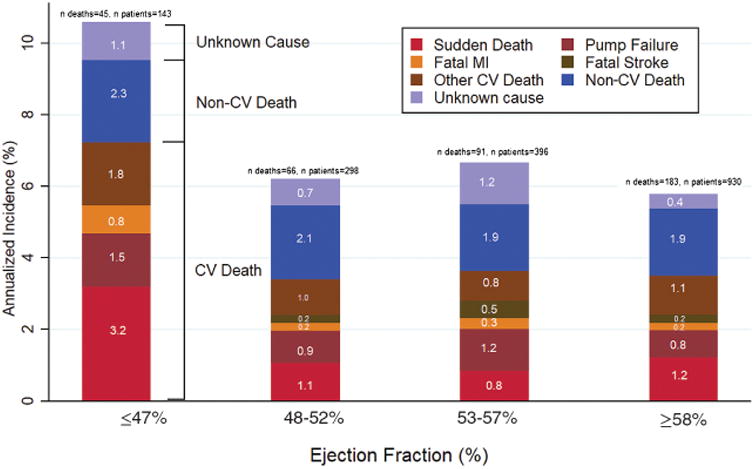
Age- and sex-adjusted annualized incidence of components of death by left ventricular ejection fraction in TOPCAT-Americas. CV, cardiovascular; MI, myocardial infarction.
The cause-specific breakdown of CV and non-CV death was not reported by earlier smaller randomized controlled trials (RCTs) among (DIG-ancillary and PEP-CHF) HFpEF patients; the more recent RCTs including TOPCAT and I-PRESERVE have reported these details on the mode of death among enrolled patients. Most HFpEF patients in these RCTs die of CV causes (60–70%) but none of the recent RCTs have evaluated the influence of LVEF on cause-specific deaths. We have shown that the rates of cause-specific mortality in HFpEF patients vary by LVEF. The differences in cause of death across the LVEF spectrum in this HFpEF population may in part be explained by substantial variation in baseline characteristics across LVEF categories. HFpEF patients with lower LVEF had a higher proportion of coronary artery disease history and behaved more like HF with reduced ejection fraction, perhaps accounting for higher rates of CV death and SCD in lower-LVEF HFpEF patients. On the other hand, patients in the higher LVEF categories had a lower burden of CV morbidities, thus explaining the higher proportion of non-CV deaths in these individuals. The proportion of deaths attributable to pump failure were quite low, while not unexpected, have potential implications for future investigation of non-HF therapies among these patients.
Our analyses have several limitations. LVEFs were measured at the sites in TOP-CAT and verified on a fraction of enrolled subjects (27%) by the core laboratory. The core lab LVEFs were significantly greater by ∼1.6 units than site reported LVEFs. There is substantial geographic variation in baseline characteristics and event rates in TOPCAT among patients enrolled in Russia and the Republic of Georgia as compared to the Americas.6,7 Therefore, we have restricted these analyses to the Americas, in which we are more certain of the diagnosis of HF.
In summary, we found that baseline characteristics and event rates of cause-specific mortality in HFpEF vary by LVEF. These findings may have implications for future trials in HFpEF as the burden of disease modifiable by specific therapies may vary by LVEF.
Acknowledgments
Funding: This work was supported by National Institutes of Health grant 5T32HL094301-07 (Navkaranbir S. Bajaj).
Footnotes
Conflict of interest: none declared.
References
- 1.Butler J, Fonarow GC, Zile MR, Lam CS, Roessig L, Schelbert EB, Shah SJ, Ahmed A, Bonow RO, Cleland JG, Cody RJ, Chioncel O, Collins SP, Dunnmon P, Filippatos G, Lefkowitz MP, Marti CN, McMurray JJ, Misselwitz F, Nodari S, O'Connor C, Pfeffer MA, Pieske B, Pitt B, Rosano G, Sabbah HN, Senni M, Solomon SD, Stockbridge N, Teerlink JR, Georgiopoulou VV, Gheorghiade M. Developing therapies for heart failure with preserved ejection fraction: current state and future directions. JACC Heart Fail. 2014;2:97–112. doi: 10.1016/j.jchf.2013.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Solomon SD, Anavekar N, Skali H, McMurray JJ, Swedberg K, Yusuf S, Granger CB, Michelson EL, Wang D, Pocock S, Pfeffer MA Candesartan in Heart Failure Reduction in Mortality (CHARM) Investigators. Influence of ejection fraction on cardiovascular outcomes in a broad spectrum of heart failure patients. Circulation. 2005;112:3738–3744. doi: 10.1161/CIRCULATIONAHA.105.561423. [DOI] [PubMed] [Google Scholar]
- 3.Solomon SD, Claggett B, Lewis EF, Desai A, Anand I, Sweitzer NK, O'Meara E, Shah SJ, McKinlay S, Fleg JL, Sopko G, Pitt B, Pfeffer MA TOPCAT Investigators. Influence of ejection fraction on outcomes and efficacy of spironolactone in patients with heart failure with preserved ejection fraction. Eur Heart J. 2016;37:455–462. doi: 10.1093/eurheartj/ehv464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pitt B, Pfeffer MA, Assmann SF, Boineau R, Anand IS, Claggett B, Clausell N, Desai AS, Diaz R, Fleg JL, Gordeev I, Harty B, Heitner JF, Kenwood CT, Lewis EF, O'Meara E, Probstfeld JL, Shaburishvili T, Shah SJ, Solomon SD, Sweitzer NK, Yang S, McKin-lay SM TOPCAT Investigators. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370:1383–1392. doi: 10.1056/NEJMoa1313731. [DOI] [PubMed] [Google Scholar]
- 5.Desai AS, Lewis EF, Li R, Solomon SD, Assmann SF, Boineau R, Clausell N, Diaz R, Fleg JL, Gordeev I, McKinlay S, O'Meara E, Shaburishvili T, Pitt B, Pfeffer MA. Rationale and design of the treatment of preserved cardiac function heart failure with an aldosterone antagonist trial: a randomized, controlled study of spironolactone in patients with symptomatic heart failure and preserved ejection fraction. Am Heart J. 2011;162:966–972.e10. doi: 10.1016/j.ahj.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 6.Pfeffer MA, Claggett B, Assmann SF, Boineau R, Anand IS, Clausell N, Desai AS, Diaz R, Fleg JL, Gordeev I, Heitner JF, Lewis EF, O'Meara E, Rouleau JL, Probstfield JL, Shaburishvili T, Shah SJ, Solomon SD, Sweitzer NK, McKinlay SM, Pitt B. Regional variation in patients and outcomes in the Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist (TOPCAT) trial. Circulation. 2015;131:34–42. doi: 10.1161/CIRCULATIONAHA.114.013255. [DOI] [PubMed] [Google Scholar]
- 7.de Denus S, O'Meara E, Desai AS, Claggett B, Lewis EF, Leclair G, Jutras M, Lavoie J, Solomon SD, Pitt B, Pfeffer MA, Rouleau JL. Spironolactone metabolites in TOPCAT - new insights into regional variation. N Engl J Med. 2017;376:1690–1692. doi: 10.1056/NEJMc1612601. [DOI] [PMC free article] [PubMed] [Google Scholar]


