Abstract
Objective
To assess the epidemiology and outcome of patients with cirrhosis following critical care unit (CCU) admission.
Design
Retrospective cohort study.
Setting
CCUs in England, Wales and Northern Ireland participating in the United Kingdom Intensive Care National Audit and Research Centre (ICNARC) Case Mix Programme (CMP)
Patients
31,363 patients with cirrhosis identified out of 1,168,650 total CCU admissions (2.7%) admitted to UK CCUs between 1998 and 2012.
Interventions
none
Measurements and main results
10,936 patients had alcohol-related liver disease (ARLD, 35%). 1.6% of CCU admissions in 1998 had cirrhosis rising to 3.1% in 2012. The crude CCU mortality of patients with cirrhosis was 41% in 1998 falling to 31% in 2012 (p<0.001). Crude hospital mortality fell from 58% to 46% over the study period (p<0.001). Mean(SD) APACHE II score in 1998 was 20.3(8.5) and 19.5(7.1) in 2012. Mean APACHE II score for patients with ARLD in 2012 was 20.6(7.0) and 19.0(7.2) for non-ARLD (p<0.001). In adjusted analysis ARLD was associated with increased risk of death (Odds ratio(OR) 1.51 (95%CI 1.42-1.62, p<0.001) with a year-on-year reduction in hospital mortality (adjusted-OR 0.95/yr, (0.94-0.96, p<0.001)).
Conclusions
More patients with cirrhosis are being admitted to CCUs but with increasing survival rates. Patients with ARLD have reduced survival rates partly explained by higher levels of organ failure on admission. Patients with cirrhosis and organ failure warrant a trial of organ support and universal prognostic pessimism is not justified.
Keywords: intensive care, mortality, acute-on-chronic liver failure, liver failure, prognosis, organ support, ICNARC
Introduction
The incidence of liver cirrhosis is rising worldwide with expected increases in hospital admissions and liver-related deaths (1, 2). Patients with cirrhosis are prone to decompensation and extra-hepatic organ failure, requiring hospital treatment and admission to the critical care unit (CCU), with high short-term mortality (3) and significant economic cost (4, 5).
Studies describing the mortality of critically-ill patients with cirrhosis suggest overall mortality ranges between 40 and 80%, with a progressive increase dependent upon the number of organ systems failing (6–9). Earlier reports noted that more than 80% of patients with 2 or more organs in failure by the third day of CCU admission did not survive to hospital discharge(7).
Marked improvements in survival have been noted in patients with acute decompensation (AD) of cirrhosis and organ failure admitted to specialist liver transplant (LT) centres (10, 11) over the last decade. This improvement can partly be explained by reductions in admission organ failure scores as patients were admitted earlier during their critical illness. In cohorts from the Royal Free Hospital, London(10) and King's College Hospital, London(11) the aetiology of underlying cirrhosis was not associated with a survival difference. Furthermore, patients admitted following gastrointestinal haemorrhage had lower mortality rates compared to those with multi-organ failure. Patients with cirrhosis and significant acute organ dysfunctions have recently been classified by international consensus as suffering from the distinct clinical entity of acute-on-chronic liver failure (ACLF)(3).
The background survival for all-comers admitted to CCUs has been increasing for many years. In the United Kingdom, the present expectation is that more than 80% of patients admitted to CCUs will survive to hospital discharge. This reduced mortality trend also occurs in other patient groups where multi-organ failure are common and historical reports suggest poor survival rates, such as sepsis(12), poly-trauma, chronic obstructive airways disease(13) and haematological malignancy(14).
This increasing survival may relate to organisational improvements, protocols to reduce catheter-related bloodstream infections and ventilator associated pneumonia rates and training in critical care. Whether this also occurs in patients with AD or ACLF is unknown. Liver-specific treatments such as liver-assist devices have not been shown to improve outcome(15), and use of liver transplantation for patients with cirrhosis and organ failure is rare. Prognostic pessimism has persisted on the benefit of organ support for patients with cirrhosis, especially outside LT centres (16). Nevertheless recent evidence from the USA suggests that survival for a hospital admission for decompensated cirrhosis is improving (17) although this study did not look at patients admitted ACLF.
Recent UK policy declarations reflect both the increasing numbers of patients with cirrhosis requiring treatment and potential deficiencies in care of patients with liver disease, particularly alcohol related liver disease (18, 19). It is not known whether the provision of critical care support is variable nationally in terms of numbers or patients admitted or in the resulting survival rates. It is an important moment to delineate the role of organ support in patients with cirrhosis given the recent re-evaluation of the care of these patients being undertaken(19). While outcomes for critically ill patients have improved markedly in recent decades, whether this is also the case for ACLF patients is less well defined outside specialist liver centres.
Here, we examine a large population of patients with cirrhosis requiring organ support in CCUs in England, Wales and Northern Ireland. Our aim was to describe the trends in outcome over time at a national level to guide clinical decision and policy making. We also compared the effect of alcohol as an aetiology on survival to hospital discharge and on whether readmission to critical care within the same hospital stay lead to similar survival rates.
Methods
Case Mix Programme Database
The Case Mix Programme (CMP) is the national clinical audit for adult critical care in England, Wales and Northern Ireland. The Case Mix Programme Database (CMPD) contains pooled case mix, resource use and outcome data on consecutive admissions to participating units (both intensive care and combined intensive/high dependency units). Data are collected to precise rules and definitions, by trained data collectors, and undergo extensive local and central validation prior to pooling. Details of the data collection and validation have been reported previously(20). The CMPD has been independently assessed to be of high quality(21) and support for the collection and use of patient-identifiable data without consent or need for institutional review board approval has been obtained under Section 251 of the NHS Act 2006 (approval number PIAG 2–10(f)/2005).
Selection of patients
Data were extracted for admissions to critical care between 1 January 1998 and 31 December 2012. Reason(s) for admission to critical care are coded using the ICNARC Coding Method (ICM), a hierarchical coding method specifically designed for coding reasons for admission to critical care(22). Cirrhosis cases were identified where primary, secondary or ultimate primary reason for admission were coded as variceal bleeding, alcoholic cirrhosis, acute alcoholic hepatitis, chronic cirrhosis (cause not defined) or portal hypertension, or where biopsy proven cirrhosis, portal hypertension or hepatic encephalopathy were reported in the past medical history (as per Acute Physiology And Chronic Health Evaluation (APACHE) II definitions(23)). The hierarchical method prevents patients with non-cirrhotic liver disease being included in this analysis.
Of the cirrhosis cases, four subgroups were identified. Alcohol related liver disease (ALRD) cases were identified where primary, secondary or ultimate primary reason for admission were either alcohol withdrawal seizures, alcoholic cirrhosis, acute alcoholic hepatitis, alcohol-induced chronic pancreatitis, self-poisoning with alcohol, alcohol overdose, delirium tremens or alcohol dependence and are compared to non-alcohol related cases. Haemorrhage cases were identified where primary, secondary or ultimate primary reason for admission were variceal bleeding and are compared to non-haemorrhage cases.
Cirrhosis cases were categorised into the following five geographical areas for analysis: South England, Midlands, North England, Wales and Northern Ireland
Case mix
Data were extracted for age, gender, ethnicity, deprivation, acute severity of illness, serum creatinine and blood lactate measurements. Liver function tests and liver specific prognostic score are not routinely captured in the CMP. Ethnicity was reported using the NHS ethnic codes, and categorized as White, Asian, Black and Other ethnic group. Deprivation was assessed with the Index of Multiple Deprivation (IMD) 2010(24). Acute severity of illness was assessed with the ICNARC physiology score(25) [6], APACHE II Acute Physiology Score (APS) and APACHE II score(23). The ICNARC Physiology Score, APS and APACHE II score each encompass a weighting for acute physiology defined by derangement from the normal range for 12 physiological variables in the first 24 hours following admission to the critical care unit. The APACHE II score additionally encompasses a weighting for age and for severe conditions in the past medical history.
Outcome
Data were extracted for status at discharge from the CCU and status at discharge from acute hospital. Data on any readmissions to critical care within the same hospital stay were also extracted.
Analyses
Data were trended by year (1998 to 2012) or 5-year subgroups thereof. Case mix, outcomes and resource use, as defined above, were described per year for each of the following groups: all cirrhosis cases, ARLD and non-ARLD, haemorrhage cases and non-haemorrhage cases, as well as the five geographical subgroups. Categorical data were summarised as number and percentage; continuous data as mean (standard deviation, SD) or median (interquartile range, IQR).
Odds ratios for hospital mortality were calculated using multi-level logistic regression modelling, adjusting for age, gender, CPR prior to admission, location prior to admission, IMD quintile, ICNARC score, ARLD and year of admission with unit as a random effect.
A statistical analysis plan was agreed a priori. The analyses were performed using Stata 13 (Statacorp LP, TX, USA).
Results
Incidence
31,363 patients with cirrhosis were identified in the study period out of 1,168,650 total admissions (2.7%). 558 patients out of a total 34,024 identified admissions (1.6%) in 1998 had cirrhosis rising to 4,207 out of 136,351 (3.1%) in 2012. Although coverage in the CMP did increase over this time, the extrapolated numbers show an increase from 1,450 out of 87,900 (1.6%) to 4750 out of 153,600 (3.1%). These admission rates are presented per 10000 population in Figure 1. The mean (SD) age of patients was 52.3 (12.7) years and 64.5% were male.
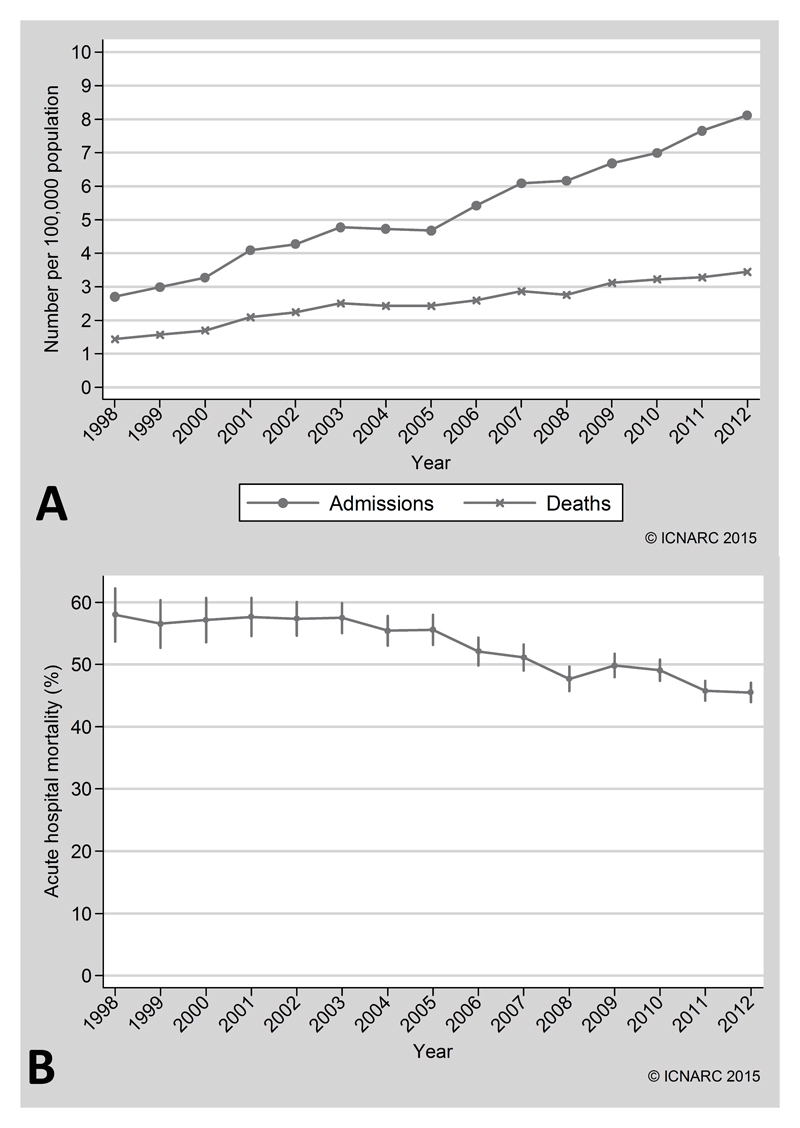
Figure 1.
(A) Extrapolated numbers of cirrhosis admissions and deaths per 100,000 of the population of England, Wales and Northern Ireland. (B) Acute hospital mortality of admissions to United Kingdom critical care units with cirrhosis
Mortality
The crude CCU mortality of patients with cirrhosis was 41.0 (95% CI 38.3-43.5) % in 1998-2002 falling to 32.5 (95% CI 30.6-33.8.1) % in 2008-2012. Crude hospital mortality was 57.4(95% CI 54.9-60.1) % in 1998-2002 and fell to 47.7 (95% CI 44.8-50.1) % in 2008-2012, see Table 1, Supplementary Material and Figures 1A and 1B. The analysis of geographical subgroups, index of deprivation and readmission is presented in the Supplementary Data.
Table 1. Demographics, outcome and critical care unit (CCU) and hospital length of stay (LOS). Years are grouped into 3 eras for ease of comparison, and in graphical form year by year in Figures 1 and 2. APS – acute physiology score, CI – confidence interval, IQR – interquartile range, SD – standard deviation.
| Variable | 1998-2002 | 2003-2007 | 2008-2012 |
|---|---|---|---|
| Number of admissions with cirrhosis | 4577 | 9698 | 17088 |
| Total number of admissions | 220784 | 378995 | 568871 |
| Incidence of patients with cirrhosis/% (95% CI) | 2.0 (1.9-2.1) | 2.6(2.5-2.7) | 3.0(2.9-3.1) |
| Males (%) | 2793 (61) | 5908 (61) | 10580 (62) |
| Age / years (SD) | 51.1 (12.4) | 52.6(12.9) | 53.2(12.3) |
| Alcohol-related N/ % (95% CI) | 1571 33 (28.8-37.3) |
3869 40 (38.8-41.5) |
5496 32 (31.0-33.7) |
| APACHE II Score (SD) | 20.6(8.3) | 20.3(8.1) | 19.6(7.3) |
| APACHE II APS (SD) | 16.2(7.7) | 16.1(7.4) | 14.9(6.6) |
| ICNARC Score (SD) | 23.5(11.5) | 23.1(11) | 21.9(10.1) |
| CCU LOS / days (IQR) | 2.1 (0.8-5.5) | 2.4 (1.0-6.3) | 2.6(1.2-6.8) |
| Survivors | 2.0 (0.9-5.0) | 2.6 (1.2-6.4) | 3.0(1.5-6.8) |
| Non-survivors | 2.1 (0.8-6.2) | 2.1 (0.8-6.2) | 2.4 (0.8-6.7) |
| Hospital LOS / days (IQR) | 14(8-25) | 16(8-28) | 15 (6-27) |
| Survivors | 22 (13-41) | 22 (12-40) | 19 (10-36) |
| Non-survivors | 8 (3-18) | 9 (3-19) | 9 (3-20) |
| CCU Mortality/% (95%CI) | 41.0 (38.3-43.5) | 37.8 (35.6-41.9) | 32.5(30.6-33.8) |
| Hospital Mortality/% (95%CI) | 57.4(54.9-60.1) | 55.4(52.9-57.3) | 47.7(44.8-50.1) |
Severity of illness at presentation
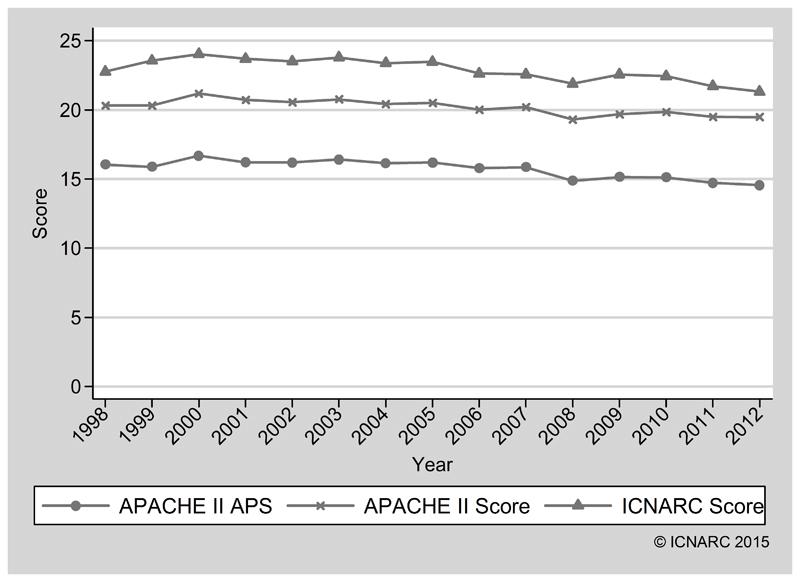
Mean (SD) APACHE II score in 1998-2002 was 20.6(8.3) and 19.6(7.3) in 2008-2012. The mean (SD) acute physiology component was 16.2(7.7) in 1998-2002 and 14.9 (6.6) in 2008-2012. The mean (SD) ICNARC score in 1998-2002 was 23.5(11.1) and 21.9 (10.2) in 2008-2012 (see per year in Table 2 and Figure 2). Mean (SD) highest serum creatinine for the cohort in 1998 was 176.9 (151.6) µmol/l and 148.0(136.7) µmol/l in 2012. Highest blood lactate was only available from 2008 where it was 4.5(4.4) mmol/l and 4.4 (4.2) mmol/l in 2012. The APACHE II risk of death for patients in 1998 was 47.6% and this was unchanged by 2012. Therefore, the observed mortality to expected risk of death discrepancy fell markedly during the study period.
Table 2. Resource use in this cohort in the final 5 years (where data were available). See Supplementary Material for definitions of the forms of support. Duration refers to median days of therapy received (IQR – interquartile range).
| Variable | 2008 | 2009 | 2010 | 2011 | 2012 |
|---|---|---|---|---|---|
| Advanced respiratory support | |||||
| Number, n (%) | 1,849 (72.0) | 2,022 (69.1) | 2,342 (68.2) | 2,589 (65.5) | 2,706 (64.3) |
| Duration / days (IQR) | 3 (2-7) | 3 (2-8) | 3 (2-7) | 3 (2-7) | 3 (2-7) |
| Basic cardiovascular support | |||||
| Number, n (%) | 2,199 (85.6) | 2,522 (86.2) | 2,947 (85.9) | 3,440 (87.0) | 3,694 (87.8) |
| Duration / days (IQR) | 3 (2-6) | 4 (2-7) | 3 (2-7) | 3 (2-6) | 3 (2-7) |
| Advanced cardiovascular support | |||||
| Number, n (%) | 1,098 (42.7) | 986 (33.7) | 1,064 (31.0) | 1,216 (30.8) | 1,161 (27.6) |
| Duration / days (IQR) | 2 (1-3) | 2 (1-3) | 2 (1-3) | 2 (-,3) | 2 (1-4) |
| Renal support | |||||
| Number, n (%) | 702 (27.3) | 580 (19.8) | 614 (17.9) | 735 (18.6) | 747 (17.8) |
| Duration median (IQR) | 3 (2-6) | 3 (2-6) | 4 (2-8) | 3 (2-6) | 3 (2-6) |
Figure 2.
Physiology scores for cirrhosis admissions (APACHE II (Acute Physiology and Chronic Health Evaluation) and ICNARC (Intensive care national audit and research council) models, APS (acute physiology score).
Alcohol
10,936 patients were identified as having alcohol as the primary aetiological factor (35%). For patients with ARLD, crude hospital mortality fell from 66.7 (95% CI 58.9-73.6) % in 1998 to 58.1 (55.3-60.8) % in 2012. Crude CCU mortality fell from 50.9 (95% CI 43.3-58.5) % in 1998 to 41.9 (95% CI 39.3-44.6)% in 2012. Mean (SD) APACHE II score for patients with ARLD in 2012 was 20.6 (7.0) and 19.0 (7.2) for patients with a non-ARLD. Patients with ARLD had higher peak serum creatinine levels during the CCU stay (mean (SD) 161(150) μmol/l v 142(130) μmol/l for non-ARLD in 2012).
Resource use
For patients admitted from 2008 it was possible to capture the rates of patients undergoing advanced respiratory, renal or cardiovascular support. Advanced respiratory support was provided in 72.0% of cases in 2008 and 64.3% of cases in 2012. Advanced cardiovascular support was given in 42.7% of cases in 2008 falling to 27.6% in 2012. Renal support was given to 27.3% of patients in 2008 falling to 17.8% of patients in 2012. Mean CCU length of stay in 1998 was 3.8 (5.6) days and 5.7 (7.6) days in 2012, see Table 2.
In 2008 72.0% of patients with ARLD received advanced respiratory support while 67.4% did in 2012. Renal support was provided to 29.5% of patients with ARLD in 2008 and to 19.4% in 2012. There was a similar reduction in the number of cases receiving advanced cardiovascular support (45.8% in 2008 and 28.4% in 2012, see supplementary material).
Detailed data on liver assist devices was not possible within the ICNARC dataset but use of such devices (including MARS(26)) is not expected to have a significant impact on the outcome data described in this study (further details in Supplementary Material).
Multivariate analysis
Logistic regression analysis using hospital survival as the outcome variable and adjusting for age, sex, ICNARC score, year of admission, admission source location, index of deprivation, requirement for CPR prior to admission and alcohol as aetiology is shown in Table 3. This gave an odds ratio (OR) of 0.95 for year of admission (95% CI 0.94 to 0.96; p<0.001), showing a decrease in mortality over time after adjusting for confounders. Alcohol as an aetiology for cirrhosis was associated with increased mortality (OR 1.51; 95% CI 1.42 to 1.61; p<0.001). The AUROC for the logistic regression model was 0.831 (95% CI 0.827 to 0.836), the Hosmer-Lemeshow χ2 statistic was 90 (8 df, p<0.001). Observed and predicted mortality were within +/-4% across the 10 categories.
Table 3. Multivariate logistic regression for acute hospital mortality. The analysis includes year of critical care unit (CCU) admission and is adjusted for age, gender, cardiopulmonary resuscitation (CPR) prior to admission, location prior to admission, alcohol related cirrhosis, index of multiple deprivation (IMD) quintile and Intensive Care National Audit and Research Centre (ICNARC) score, with random effects for unit* [N=28,449].
| Variable | Odds ratio (95% confidence interval) | p value |
|---|---|---|
| Age | 1.02 (1.02,1.03) | <0.001 |
| Gender (male) | 1.01 (0.95,1.07) | 0.71 |
| CPR prior to admission | 1.87 (1.61,2.18) | <0.001 |
| Location prior to admission | ||
| A&E/Other/Not in hospital | 1.00 (-) | - |
| ICU/HDU | 1.26 (1.12,1.41) | <0.001 |
| Theatre (elective) | 0.38 (0.32,0.44) | <0.001 |
| Theatre (emergency) | 0.81 (0.73,0.89) | <0.001 |
| Ward | 1.64 (1.52,1.77) | <0.001 |
| Alcohol related cirrhosis | 1.51 (1.42,1.61) | <0.001 |
| IMD quintile | ||
| 1 (least deprived) | 1.00 (-) | - |
| 2 | 1.02 (0.91,1.14) | 0.70 |
| 3 | 1.06 (0.95,1.18) | 0.30 |
| 4 | 1.08 (0.97,1.20) | 0.16 |
| 5 (most deprived) | 1.07 (0.97,1.19) | 0.16 |
| ICNARC score | 1.13 (1.13,1.14) | <0.001 |
| Year of ICU admission | 0.95 (0.94,0.96) | <0.001 |
rho=0.02 (0.02,0.03)
Discussion
These results demonstrate that patients with cirrhosis and organ failure have substantially improved survival in the modern era of critical care provision. Most patients admitted to critical care with cirrhosis in the UK are now expected to survive.
For decades the combination of a past medical history of cirrhosis and multi-organ failure has been perceived as having prohibitive mortality statistics and that organ support is futile(27). Survival to hospital discharge in patients with non-hepatic reasons for admissions have been increasing recently(12) due to a combination of factors including management of sepsis, attention to prevention of nosocomial infections (e.g. ventilator-associated pneumonia and catheter-related bloodstream infections) and organisation of CCUs. While individual factors are difficult to identify causally with decreasing mortality the background increasing survival rate is clear.
Tertiary liver centres with access to specialist hepatology, transplantation and hepatobiliary surgical expertise have demonstrated improved survival even when transplantation was discounted(11). The management of portal hypertensive bleeding especially has improved significantly. Several centres have reported decreasing mortality rates in patients with or without gastrointestinal haemorrhage as the primary indication for admission (10, 11). Both centres note a reduction in admission APACHE II score suggesting earlier admission to CCUs prior to irreversible MOF as a useful strategy. Furthermore, both transplant centres note that alcohol is not associated with a worse mortality compared to other aetiologies.
The data we present here demonstrate a different pattern. While mortality is falling, the acuity of critical illness on admission measured by APACHE II score (and predicted risk of death) did not change significantly. Admission ICNARC score fell by a small amount over the study period but after adjusting for this on multivariate analysis the year by year fall in mortality retained statistical significance. This suggests that while earlier admission is useful to manage impending organ failure, patients should not be denied admission based on organ failure score alone and that the excess mortality associated with chronic liver disease (in addition to physiological APACHE score) is diminishing.
Our findings here confirm a more positive outlook for patients with cirrhosis and ACLF. While other authors have reported mortality rates of up to 80% in patients with ACLF-3 (3, 28) this was in the context of care outside of CCUs whereas all the patients in our study were cared for in CCUs. We would urge early admission to CCU to prevent irreversible organ failure occurring.
Overall this registry study represents the largest dataset of patients with cirrhosis managed in CCUs yet reported and therefore sets the benchmark of outcomes now expected in this patient group. It companions the epidemiological data in ALF(29) but for the first time demonstrates the improving outlook at population level for this important and more common subgroup of liver patients who require organ support.
While there may be country specific aspects in terms of interaction with liver transplantation services we expect these to impact the minority of patients given the access to LT in patients with ACLF has been limited in the past. This is because we exclude patients with ALF and transplantation is predominantly an elective procedure in patients with cirrhosis in most countries. Recent reports are challenging the dogma of whether LT is useful in patients with ACLF(30) which may lead to higher admission rates and greater access to LT services. As the UK moves to an organ allocation system based on wait list mortality it would be interesting to observe the impact on outcomes of patients after this change as those with organ failures will be more likely to receive an offer. In countries where MELD based allocation is already in use(31) it would be interesting to see if the outcomes of patients with cirrhosis and organ failure in general is different to what we report here.
In contrast to LT units we found that alcohol appears to be associated with an excess independent mortality risk even when confounders are addressed (although they tend to present with higher levels of organ (particularly renal) dysfunction). This discrepancy may be related to acute alcoholic hepatitis, which is associated with ongoing alcohol use and a high mortality. Our data would not allow clear delineation of this as retrospective allocation of diagnosis would require access to liver function tests, history of abstinence, imaging or liver biopsy data. We would not suggest that patients with ARLD be denied access to CCUs based on prohibitively high mortality until the underlying reason for this higher attributable mortality is identified. The number of patients receiving LT during the index admission in this dataset would be exceedingly small.
Doubt over appropriateness over the use of critical care services in actively drinking patients with ARLD may lead to delays in admission. Other investigators have noted an increased mortality in patients with ARLD who were consuming alcohol up to hospital admission (3). Of note we see a lower incidence of ALRD compared to other aetiologies in contrast to recent reports from the UK (1) which may be related to ARLD being defined from the reason for admission in the ICNARC dataset. This may represent under reporting or a reduced admission rate for ARLD outside LT centres.
This study has several limitations. We are unfortunately unable to calculate MELD, ACLF grade or CLIF-SOFA scores (or apply SOFA organ failure definitions) retrospectively from this data as the CMP was set up as a general CCU dataset with a strong focus on resource use. This is a weakness which does not allow prognostic scoring systems to be compared or validated in this otherwise very large cohort. The level of detail is sufficient to give guidance on the pattern of survival over time, corrected for general ICU severity measures, which is nevertheless still useful in overcoming prognostic pessimism about admission of patients with cirrhosis to CCUs.
We are unable to demonstrate definitively which patients were listed for LT following acute admission to the CCU for organ support. However, this is likely to be a small number compared to the overall cohort. It has been demonstrated previously in analysis of the UK national database of NHS Blood and Transplant that between 2011 to 2016 only 65 patients underwent LT following an acute hospitalisation with extra-hepatic organ failure(32). At present we are unable to demonstrate whether an unlisted patient was declined certain organ support modalities due to concerns over futility. This may occur for example in suspected HRS where bridging to LT was deemed futile. Further analysis will be required linking critical care and transplantation data sources to address these aspects in future studies.
The ICNARC dataset was not originally envisaged with liver disease as a primary aspect of study and so we are unable to give granular data beyond alcohol related liver disease in terms of aetiology. This limits the description of the major other aetiologies such as viral hepatitis or non-alcohol related fatty liver disease (NAFLD) or rarer causes such as autoimmune hepatitis. In future NAFLD is likely to increase as a cause for cirrhosis and viral hepatitis will decrease rapidly given the effective treatments for hepatitis C. Future studies should focus on this aspect of the increasing burden of metabolic liver disease with more detailed aetiological descriptions.
We do not have information on long-term survival as although patients may survive the critical care or hospital stay their risk of death is still high and many will not survive the year following admission. However, these data provide further impetus for expedited transplant assessments in those patients who survive CCU admission.
In conclusion, the rising incidence of cirrhosis in the general population is reflected in increasing numbers of patients with cirrhosis admitted to CCUs. As critical care services expand it is vital that these patients are given access to organ support as the majority will survive to hospital discharge.
Supplementary Material
Financial Support
MJWM is grateful to the Wellcome Trust, UK for support in the form of a Postdoctoral Research Training Fellowship during part of the period in which this article was produced. He is also grateful to the NIHR Biomedical Research Centres at both Imperial College London and Kings College London for infrastructure support.
List of abbreviations
- ACLF
acute on chronic liver failure
- ARLD
Alcohol related liver disease
- APACHE
Acute Physiology and Chronic Health Evaluation
- CCMDS
critical care minimal data set
- CMP
Case Mix Programme
- CCU
critical care unit
- CLIF
chronic liver failure
- HDU
high dependency unit
- ICNARC
Intensive Care National Research Centre
- ICU
intensive care unit
- SOFA
sequential organ failure assessment
Footnotes
Conflicts of interest
The authors have no conflicts of interest relevant to this manuscript.
Copyright form disclosure: Dr. McPhail received support for article research from the Wellcome Trust/COAF. Dr. Bernal received funding from Vital Therapies Inc. The remaining authors have disclosed that they do not have any potential conflicts of interest.
References
- 1.Thomson SJ, Westlake S, Rahman TM, et al. Chronic liver disease--an increasing problem: a study of hospital admission and mortality rates in England, 1979-2005, with particular reference to alcoholic liver disease. Alcohol Alcohol. 2008;43(4):416–422. doi: 10.1093/alcalc/agn020. [DOI] [PubMed] [Google Scholar]
- 2.Roberts SE, Goldacre MJ, Yeates D. Trends in mortality after hospital admission for liver cirrhosis in an English population from 1968 to 1999. Gut. 2005;54(11):1615–1621. doi: 10.1136/gut.2004.058636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moreau R, Jalan R, Gines P, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology. 2013;144(7):1426–1437. doi: 10.1053/j.gastro.2013.02.042. 1437 e1421-1429. [DOI] [PubMed] [Google Scholar]
- 4.Shawcross DL, Austin MJ, Abeles RD, et al. The impact of organ dysfunction in cirrhosis: survival at a cost? J Hepatol. 2012;56(5):1054–1062. doi: 10.1016/j.jhep.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 5.Aggarwal A, Ong JP, Younossi ZM, et al. Predictors of mortality and resource utilization in cirrhotic patients admitted to the medical ICU. Chest. 2001;119(5):1489–1497. doi: 10.1378/chest.119.5.1489. [DOI] [PubMed] [Google Scholar]
- 6.Das V, Boelle PY, Galbois A, et al. Cirrhotic patients in the medical intensive care unit: early prognosis and long-term survival. Critical care medicine. 2010;38(11):2108–2116. doi: 10.1097/CCM.0b013e3181f3dea9. [DOI] [PubMed] [Google Scholar]
- 7.Arabi Y, Ahmed QA, Haddad S, et al. Outcome predictors of cirrhosis patients admitted to the intensive care unit. Eur J Gastroenterol Hepatol. 2004;16(3):333–339. doi: 10.1097/00042737-200403000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Cholongitas E, Senzolo M, Patch D, et al. Risk factors, sequential organ failure assessment and model for end-stage liver disease scores for predicting short term mortality in cirrhotic patients admitted to intensive care unit. Aliment Pharmacol Ther. 2006;23(7):883–893. doi: 10.1111/j.1365-2036.2006.02842.x. [DOI] [PubMed] [Google Scholar]
- 9.Levesque E, Hoti E, Azoulay D, et al. Prospective evaluation of the prognostic scores for cirrhotic patients admitted to an intensive care unit. J Hepatol. 2012;56(1):95–102. doi: 10.1016/j.jhep.2011.06.024. [DOI] [PubMed] [Google Scholar]
- 10.Theocharidou E, Pieri G, Mohammad AO, et al. The Royal Free Hospital score: a calibrated prognostic model for patients with cirrhosis admitted to intensive care unit. Comparison with current models and CLIF-SOFA score. Am J Gastroenterol. 2014;109(4):554–562. doi: 10.1038/ajg.2013.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McPhail MJ, Shawcross DL, Abeles RD, et al. Increased Survival for Patients with Cirrhosis and Organ Failure in Liver Intensive Care and Validation of the Chronic Liver Failure-Sequential Organ Failure Scoring System. Clin Gastroenterol Hepatol. 2015;13(7):1353–1360. doi: 10.1016/j.cgh.2014.08.041. [DOI] [PubMed] [Google Scholar]
- 12.Kaukonen KM, Bailey M, Suzuki S, et al. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA : the journal of the American Medical Association. 2014;311(13):1308–1316. doi: 10.1001/jama.2014.2637. [DOI] [PubMed] [Google Scholar]
- 13.Wildman MJ, Sanderson C, Groves J, et al. Implications of prognostic pessimism in patients with chronic obstructive pulmonary disease (COPD) or asthma admitted to intensive care in the UK within the COPD and asthma outcome study (CAOS): multicentre observational cohort study. Bmj. 2007;335(7630):1132. doi: 10.1136/bmj.39371.524271.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bird GT, Farquhar-Smith P, Wigmore T, et al. Outcomes and prognostic factors in patients with haematological malignancy admitted to a specialist cancer intensive care unit: a 5 yr study. British journal of anaesthesia. 2012;108(3):452–459. doi: 10.1093/bja/aer449. [DOI] [PubMed] [Google Scholar]
- 15.Banares R, Catalina MV, Vaquero J. Molecular adsorbent recirculating system and bioartificial devices for liver failure. Clin Liver Dis. 2014;18(4):945–956. doi: 10.1016/j.cld.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 16.Berry PA, Thomson SJ, Rahman TM, et al. Review article: towards a considered and ethical approach to organ support in critically-ill patients with cirrhosis. Aliment Pharmacol Ther. 2013;37(2):174–182. doi: 10.1111/apt.12133. [DOI] [PubMed] [Google Scholar]
- 17.Schmidt ML, Barritt AS, Orman ES, et al. Decreasing mortality among patients hospitalized with cirrhosis in the United States from 2002 through 2010. Gastroenterology. 2015;148(5):967–977 e962. doi: 10.1053/j.gastro.2015.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Measuring the Units: A review of patients who died with alcohol-related liver disease. National Confidential Enquiry into Patient Outcome and Death. 2013 [Google Scholar]
- 19.Williams R, Aspinall R, Bellis M, et al. Addressing liver disease in the UK: a blueprint for attaining excellence in health care and reducing premature mortality from lifestyle issues of excess consumption of alcohol, obesity, and viral hepatitis. Lancet. 2014;384(9958):1953–1997. doi: 10.1016/S0140-6736(14)61838-9. [DOI] [PubMed] [Google Scholar]
- 20.Harrison DA, Brady AR, Rowan K. Case mix, outcome and length of stay for admissions to adult, general critical care units in England, Wales and Northern Ireland: the Intensive Care National Audit & Research Centre Case Mix Programme Database. Crit Care. 2004;8(2):R99–111. doi: 10.1186/cc2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Catalogue NI. Information Catalogue – Directory of Clinical Databases. 2007 http://www.icapp.nhs.uk/docdat/.
- 22.Young JD, Goldfrad C, Rowan K. Development and testing of a hierarchical method to code the reason for admission to intensive care units: the ICNARC Coding Method. Intensive Care National Audit & Research Centre. British journal of anaesthesia. 2001;87(4):543–548. doi: 10.1093/bja/87.4.543. [DOI] [PubMed] [Google Scholar]
- 23.Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Critical care medicine. 1985;13(10):818–829. [PubMed] [Google Scholar]
- 24.Government DfCaL. English indices of deprivation. 2010 [Google Scholar]
- 25.Harrison DA, Parry GJ, Carpenter JR, et al. A new risk prediction model for critical care: the Intensive Care National Audit & Research Centre (ICNARC) model. Critical care medicine. 2007;35(4):1091–1098. doi: 10.1097/01.CCM.0000259468.24532.44. [DOI] [PubMed] [Google Scholar]
- 26.Banares R, Nevens F, Larsen FS, et al. Extracorporeal albumin dialysis with the molecular adsorbent recirculating system in acute-on-chronic liver failure: the RELIEF trial. Hepatology. 2013;57(3):1153–1162. doi: 10.1002/hep.26185. [DOI] [PubMed] [Google Scholar]
- 27.O'Brien AJ, Welch CA, Singer M, et al. Prevalence and outcome of cirrhosis patients admitted to UK intensive care: a comparison against dialysis-dependent chronic renal failure patients. Intensive care medicine. 2012;38(6):991–1000. doi: 10.1007/s00134-012-2523-2. [DOI] [PubMed] [Google Scholar]
- 28.Gustot T, Fernandez J, Garcia E, et al. Clinical Course of acute-on-chronic liver failure syndrome and effects on prognosis. Hepatology. 2015;62(1):243–252. doi: 10.1002/hep.27849. [DOI] [PubMed] [Google Scholar]
- 29.Bernal W, Hyyrylainen A, Gera A, et al. Lessons from look-back in acute liver failure? A single centre experience of 3300 patients. J Hepatol. 2013;59(1):74–80. doi: 10.1016/j.jhep.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 30.Artru F, Louvet A, Ruiz I, et al. Liver transplantation in the most severely ill cirrhotic patients: A multicenter study in acute-on-chronic liver failure grade 3. J Hepatol. 2017;67(4):708–715. doi: 10.1016/j.jhep.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 31.Nekrasov V, Matsuoka L, Kaur N, et al. Improvement in the Outcomes of MELD >/= 40 Liver Transplantation: An Analysis of 207 Consecutive Transplants in a Highly Competitive DSA. Transplantation. 2017;101(10):2360–2367. doi: 10.1097/TP.0000000000001738. [DOI] [PubMed] [Google Scholar]
- 32.Bernal W. Improving Outcomes for Transplantation of Critically Ill Patients with Cirrhosis? Clinical Liver Disease. 2017;10(1):25–28. doi: 10.1002/cld.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.