Summary
The 2012 World Heart Federation (WHF) criteria for echocardiographic diagnosis of rheumatic heart disease (RHD) identify that the finding of ‘pathological’ mitral regurgitation (MR) in a screened individual increases the likelihood of detecting underlying RHD. Cases of isolated ‘pathological MR’ are thus identified as ‘borderline RHD’. A large-scale echocardiographic screening program (Echo in Africa) in South Africa has identified that inter-scallop separations of the posterior mitral valve leaflet (PMVL) can give rise to ‘pathological’ MR. The authors propose that this entity in isolation should be identified and excluded from the WHF ‘borderline RHD’ category. In this case report, we present two examples of ‘pathological’ MR related to inter-scallop separation from the Echo in Africa image database. We further provide screening tips for the accurate identification of this entity.
Keywords: rheumatic heart disease, echocardiography, screening, ‘pathological’ MR, inter-scallop separation of the posterior mitral valve leaflet
Learning points:
Posterior mitral valve leaflet inter-scallop separations are an important entity to identify as a potential cause of haemodynamically insignificant yet WHF ‘pathological’ MR.
Cases of inter-scallop separations with ‘pathological’ MR remain an important finding in RHD screening and those without any other morphological features of RHD should be excluded from the WHF ‘borderline RHD’ group.
Careful interrogation of the mitral valve in both PSLAX and PSSAX views is required to identify the underlying mechanism of MR.
Further study is needed in our study population to describe the prevalence and clinical relevance of inter-scallop separations.
Background
Rheumatic heart disease (RHD) is responsible for significant morbidity and mortality in developing nations and underserved communities in the developed world (1). Sub Saharan Africa has been identified as an area with endemic RHD with an estimated 10 per 1000 population living with RHD (2).
The consensus-derived diagnostic criteria established in 2012 – the ‘World Heart Federation criteria for echocardiographic diagnosis of rheumatic heart disease’ (3) – represent an important milestone in the standardization of diagnostic parameters and the reporting of RHD.
However, the criteria are potentially weakened by the incorporation of a non-specific Doppler-based evaluation of regurgitant valvular lesions that could erroneously include cases with ‘congenital MR’ into the ‘borderline RHD’ group (4, 5, 6, 7).
A large-scale RHD screening program in both high- and low-risk RHD communities in the Western Cape, South Africa (unpublished data from the Echo in Africa (EIA) program) has identified that a normal variant of the posterior mitral valve leaflet (PMVL) – so-called ‘prominent posterior leaflet inter-scallop separation’ (5) – may be responsible for a proportion of screened cases identified as ‘borderline RHD’ with isolated WHF ‘pathological’ MR.
These separations, ‘indentations’ or ‘slits’, have been described in anatomical cardiology texts dating back to the 1950s (8, 9, 10, 11). They are known to exclusively affect the PMVL with marked heterogeneity relating to their location, number (between 0 and 5 separations in a single PMVL) and depth of excursion into the PMVL (8, 11). Victor & Nayak propose in their autopsy series that these separations are a normal finding in the PMVL and play an important role in allowing the PMVL to ‘change in contour and size during atrial and ventricular systole’ (11).
To the best of our knowledge, there is no echocardiographic data that highlight this entity and document its particular relevance to RHD screening.
Case presentation
We present two cases selected from the EIA database of ‘borderline RHD’ with isolated ‘pathological’ MR attributable to prominent inter-scallop separations of the PMVL. Both cases met all 4 Doppler criteria for WHF ‘pathological’ MR.
Investigation
Participants in the Echo in Africa program are screened by experienced RHD sonographers using the General Electric (GE) Vivid I laptop unit. Screening studies are captured in accordance with a minimum standard dataset as stipulated by the British Society for Echocardiography (12).
Case 1 is a screening study obtained from an individual living in a high-risk RHD community (low socio-economic status (SES) and with no access to private medical care). Videos 1, 2, 3 and 4 have been selected from the initial screening study to demonstrate the relevant findings.
Parasternal long axis view (PSLAX) demonstrating a normal mitral valve (normal anterior mitral valve leaflet (AMVL) thickness, no RHD-related restriction of either MV leaflets. View Video 1 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-1.
Download Video 1 (1.6MB, mov)
PSLAX view with color Doppler demonstrating MR that measures 2.2 cm in length. The jet met the additional requirements to deem it pathological (seen in 2 views, CW maximum velocity >3 m/s and a pansystolic jet). View Video 2 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-2.
Download Video 2 (2.2MB, mov)
Parasternal short axis (PSSAX) view of the mitral valve, demonstrating a PMVL inter-scallop separation in the P2 position. View Video 3 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-3.
Download Video 3 (2.3MB, mov)
PSSAX with color Doppler confirming a P2 inter-scallop separation as the underlying cause of the MR. View Video 4 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-4.
Download Video 4 (1.3MB, mov)
Case 2 is from an individual living in a low-risk RHD community (high SES with access to private medical care). Videos 5, 6, 7 and 8 have been selected from the initial screening study to demonstrate the relevant findings.
Parasternal long axis view (PSLAX) demonstrating a normal mitral valve (normal anterior mitral valve leaflet (AMVL) thickness, no RHD-related restriction of either MV leaflets. View Video 5 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-5.
Download Video 5 (913.4KB, mov)
PSLAX view with color Doppler demonstrating MR that measured 2.2 cm in length. The jet met the additional requirements to deem it pathological (seen in 2 views, CW maximum velocity >3 m/s and a pansystolic jet). View Video 6 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-6.
Download Video 6 (473.6KB, mov)
PSSAX view of the mitral valve, demonstrating a subtler case of an inter-scallop separation in the P2/P3 position. View Video 7 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-7.
Download Video 7 (972.1KB, mov)
PSSAX with color Doppler confirming a P2/P3 inter-scallop separation as the underlying cause of the MR. View Video 8 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-8.
Download Video 8 (359.1KB, mov)
Tips for the echocardiographic diagnosis of inter-scallop separations in screening
Parasternal long axis
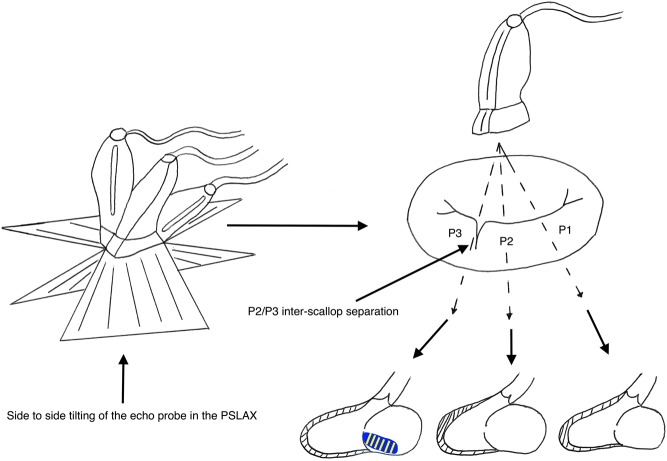
Dynamic scanning with color Doppler is used to identify the segment of the PMVL where the regurgitant jet is seen to be maximal and thus coinciding with the inter-scallop separation. The so-called ‘parasternal sweep’ is performed by tilting the probe up (more lateral portion – P2/P1) and then tilting downwards (more medial portion – P2/P3) (Fig. 1).
Suspect an inter-scallop separation as a cause of MR particularly when the MR jet is centrally directed and shown to emanate from below the coaptation point of the PMVL with the anterior mitral valve leaflet (AMVL) (Video 9). This feature however cannot be solely relied upon as regurgitant jets can be posteriorly directed (Video 2) and can therefore mimic the classic ‘pseudoprolapse’ mechanism of chronic rheumatic MR in terms of jet direction (Videos 10 and 11).
Figure 1.
Parasternal sweep: sweeping from commissure to commissure (tilting the echo probe from side to side in the PSLAX) with focused color Doppler over the MV will identify, which segment is likely to have an inter-scallop separation.
A screened case from the EIA database with ‘pathological MR’ from an inter-scallop separation of the PMVL. This video from the PSLAX view with focused color Doppler over the MV demonstrates central MR with its origin below the coaptation point of the MV leaflets (i.e. body of the PMVL). View Video 9 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-9.
Download Video 9 (868KB, mov)
PSLAX view demonstrating a rheumatic mitral valve with suggestive RHD-related restriction of the AMVL and PMVL. The A2 segment of the AMVL is seen to ‘prolapse’ past the P2 segment of the PMVL. This mechanism is more correctly termed ‘pseudoprolapse’ as the AMVL is in its normal position at end systole. The impression of A2 prolapse is rather thought to be related to PMVL systolic restriction with resultant malcoaptation of the PMVL and AMVL during systole. This generates the characteristic posteriorly directed jet of rheumatic MR. View Video 10 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-10.
Download Video 10 (908.5KB, mov)
PSLAX view with focused color Doppler over the MV – this video demonstrates the characteristic posterior MR jet encountered in chronic rheumatic MR. View Video 11 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-11.
Download Video 11 (549.8KB, mov)
Parasternal short axis
Tilt to view leaflet tips of PMVL without color – try to identify the separate scallops and the separations that demarcate them (Video 12). Inter-scallop separations are identified as visible linear defects extending a variable depth into the posterior leaflet from the coaptation line. The inter-scallop area is often seen to ‘open up’ during diastole when the scallop edges part in this region.
Color Doppler is used to confirm site of regurgitation (often below coaptation line of the two mitral leaflets) (Video 13) The color jet origin is typically confined to the inter-scallop region and the jet origin spreads predominantly vertically down the height of the PMVL rather than across the coaptation line between the AMVL and PMVL.
PSSAX view of a screened case from the EIA database with ‘pathological MR’. The screener should ensure that the leaflet tips are adequately sectioned to identify potential inter-scallop separation(s). This video demonstrates an inter-scallop separation in the P2/P3 position. View Video 12 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-12.
Download Video 12 (882.7KB, mov)
PSSAX of the same case presented in Video 12: focused color Doppler over the MV confirms a P2 inter-scallop separation as the underlying cause of the MR. View Video 13 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-13.
Download Video 13 (1,019.9KB, mov)
Discussion
In this case report we describe a known anatomical feature of the PMVL, so-called inter-scallop separation, which can be attributed to cause WHF ‘pathological MR’ in screened cases from both a high- and low-risk RHD community.
Identifying alternative ‘congenital’ causes of MR is an important step in the screening process and specifically stipulated by the WHF in an attempt to curb misidentification of non-rheumatic cases. Included among these are congenital anomalies related to leaflet clefts or apparent clefts.
Among the mimics of mitral leaflet clefts are entities that can be readily differentiated from true clefts such as the trileaflet mitral valve. In this entity, the identification of an additional papillary muscle aids in diagnosis (13). True, isolated AMVL clefts (not related to atrio-ventricular septal defects) are a rare finding (14, 15), but due to an absence of anatomical scallops of the AMVL, these entities are not confused with inter-scallop separations and readily identified as congenital abnormalities.
The same does not hold true for cleft-like defects identified in the PMVL. As early as the 1950s, there was contention as to what constitutes the PMVL and importantly, no consistent anatomical nomenclature was agreed on to define its variable divisions (8, 10, 11, 16). This lack of agreement persists, and there is no consensus on what features differentiate the normal anatomical variant of an inter-scallop separation from a cleft or even whether a separation of the entities is warranted. Two strategies of identifying true clefts from among inter-scallop separations have been to look at either the size of the defect or functional consequence thereof. A recent study describing the prevalence and impact of clefts in mitral valve prolapse (MVP) identified clefts as defects that extend >50% of the height of the posterior leaflet and are visible during systole and diastole (17). The authors conclude that these clefts may play an important role in the development and mechanism of prolapse but acknowledge that they likely reflect one end of the spectrum of normality, having also been identified in their control population (17).
In contrast to this, Wyss et al. propose that a cleft is defined as a ‘complete split up to the annulus and has some degree of regurgitation’ (18), choosing instead to incorporate a functional deficit into the definition.
The addition of this functional aspect does not appear to be strongly rooted in a fundamental difference in pathology identified, and it is our contention that PMVL clefts, something previously considered rare (19, 20, 21) is perhaps only one end of the spectrum of normal inter-scallop separation (17).
This raises important challenges in the RHD screening environment. Whereas the impact of PMVL ‘clefts’ have been explored in cohorts with overt valve pathology, their role remains undefined in healthy asymptomatic children undergoing RHD screening. Inter-scallop separation, a normal anatomical entity, has not been identified as a potential confounder in the current WHF diagnostic criteria. Consequently, if not recognized and excluded from analysis, could falsely increase the prevalence of ‘borderline RHD’ detected in any RHD screening program. In addition, failure to exclude these cases could further distort the findings of long-term studies documenting the outcome of ‘borderline RHD’ as progression of MR from this entity remains unexplored (22, 23, 24).
Therefore, in the absence of compelling RHD-related morphological changes of the AMVL or the aortic valve (AV), we do not advocate diagnosing cases with RHD where the mechanism of WHF pathological MR is clearly related to an inter-scallop separation. To what extent these cases are currently inflating the size of the Borderline group is an important question that needs to be further studied.
Given the ubiquitous nature of PMVL inter-scallop separations, it is inevitable that screening programs will encounter individuals with true RHD features of their mitral valve in addition to their normal variation of the PMVL (inter-scallop separation with MR). What remains unclear is what specific features of the mitral valve in cases of ‘presumed normal PMVL variants’ will alert the screener to consider a diagnosis of concurrent RHD.
Further research is required to describe the prevalence and natural history of inter-scallop separations in both high- and low-risk RHD populations and the effect that the RHD process has on this underlying normal PMVL variant.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of this case report.
Funding
The Echo in Africa program is supported through an ‘Every heartbeat matters’ Edwards Lifesciences Foundation grant (#35526255).
Patient consent
The Echo in Africa program has received ethical approval from the Health Research Ethics Committee of Stellenbosch University (N14/04/038). Participants in this study are required to provide adequate assent/consent prior to study enrollment. This includes the use of relevant images/data for publication. Studies are de-identified prior to data analysis to ensure participant anonymity.
Author contribution statement
L H screened the participants and wrote the manuscript with input from all the authors. All authors provided critical feedback and helped shape the research, analysis and manuscript.
References
- 1.Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, Charlson F, Davis A, Degenhardt L, Dicker D, et al Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015. 386 743–800. ( 10.1016/S0140-6736(15)60692-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watkins DA, Johnson CO, Colquhoun SM, Karthikeyan G, Beaton A, Bukhman G, Forouzanfar MH, Longenecker CT, Mayosi BM, Mensah GA, et al Global, regional, and national burden of rheumatic heart disease, 1990–2015. New England Journal of Medicine 2017. 377 713–722. ( 10.1056/NEJMoa1603693) [DOI] [PubMed] [Google Scholar]
- 3.Remenyi B, Wilson N, Steer A, Ferreira B, Kado J, Kumar K, Lawrenson J, Maguire G, Marijon E, Mirabel M, et al World Heart Federation criteria for echocardiographic diagnosis of rheumatic heart disease – an evidence-based guideline. Nature Reviews Cardiology 2012. 9 297–309. ( 10.1038/nrcardio.2012.7) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hunter LD, Monaghan M, Lloyd G, Pecoraro AJK, Doubell AF, Herbst PG. Screening for rheumatic heart disease: is a paradigm shift required? Echo Research and Practice 2017. 4 R43–R52. ( 10.1530/ERP-17-0037) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Herbst P. Screening for asymptomatic rheumatic heart disease : understanding the mechanisms key to the diagnostic criteria. SA Heart 2015. 12 134–144. [Google Scholar]
- 6.Dougherty S, Khorsandi M, Herbst P. Rheumatic heart disease screening : current concepts and challenges. Annals of Pediatric Cardiology 2017. 10 39–49. ( 10.4103/0974-2069.197051) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Webb RH, Wilson NJ, Lennon DR, Wilson EM, Nicholson RW, Gentles TL, O’Donnell CP, Stirling JW, Zeng I, Trenholme AA. Optimising echocardiographic screening for rheumatic heart disease in New Zealand: not all valve disease is rheumatic. Cardiology in the Young 2011. 21 436–443. ( 10.1017/S1047951111000266) [DOI] [PubMed] [Google Scholar]
- 8.Ranganathan N, Lam JH, Wigle ED, Silver MD. Morphology of the human mitral valve. II. The value leaflets. Circulation 1970. 41 459–467. ( 10.1161/01.CIR.41.3.459) [DOI] [PubMed] [Google Scholar]
- 9.Chiechi M, Lees W, Thompson R. Functional anatomy of the normal mitral valve. Journal of Thoracic Surgery 1956. 32 378–398. [PubMed] [Google Scholar]
- 10.Rusted I, Scheifley C, Edwards J. Studies of the mitral valve. I. Anatomic features of the normal mitral valve and associated structures. Circulation 1952. 6 825–831. ( 10.1161/01.CIR.6.6.825) [DOI] [PubMed] [Google Scholar]
- 11.Victor S, Nayak VM. Definition and function of commissures, slits and scallops of the mitral valve: analysis in 100 hearts. Asia Pacific Journal of Thoracic and Cardiovascular Surgery 1994. 3 10–16. ( 10.1016/1324-2881(94)90050-7) [DOI] [Google Scholar]
- 12.Wharton G, Steeds R, Allen J, Phillips H, Jones R, Kanagala P, Lloyd G, Masani N, Mathew T, Oxborough D, et al A minimum dataset for a standard adult transthoracic echocardiogram: a guideline protocol from the British Society of Echocardiography. Echo Research and Practice 2015. 2 G9–G24. ( 10.1530/ERP-14-0079) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Rensburg A, Pecoraro A, Kyriakakis C, Herbst P, Doubell A. Trileaflet mitral valves – when lightning strikes thrice. SA Heart 2016. 13 36–37. [Google Scholar]
- 14.Perier P, Clausnizer B. Isolated cleft mitral valve: valve reconstruction techniques. Annals of Thoracic Surgery 1995. 59 56–59. ( 10.1016/0003-4975(94)00613-C) [DOI] [PubMed] [Google Scholar]
- 15.Timóteo A, Galrinho A, Fiarresga A, Branco L, Banazol N, Leal A, Fragata J, Quininha J. Isolated cleft of the anterior mitral valve leaflet. European Journal of Echocardiography 2007. 8 59–62. [DOI] [PubMed] [Google Scholar]
- 16.Harken D, Ellis LB, Dexter L, Farrand RE, Dickson JF. The responsibility of the physician in the selection of patients with mitral stenosis for surgical treatment. Circulation 1952. 5 349–362. ( 10.1161/01.CIR.5.3.349) [DOI] [PubMed] [Google Scholar]
- 17.Ring L, Rana BS, Ho SY, Wells FC. The prevalence and impact of deep clefts in the mitral leaflets in mitral valve prolapse. European Heart Journal: Cardiovascular Imaging 2013. 14 595–602. [DOI] [PubMed] [Google Scholar]
- 18.Wyss CA, Enseleit F, Van Der Loo B, Grünenfelder J, Oechslin EN, Jenni R. Isolated cleft in the posterior mitral valve leaflet: a congenital form of mitral regurgitation. Clinical Cardiology 2009. 32 553–560. ( 10.1002/clc.20608) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McEnany MT, English TA, Ross DN. The congenitally cleft posterior mitral valve leaflet: an antecedent to mitral regurgitation. Annals of Thoracic Surgery 1973. 16 281–292. ( 10.1016/S0003-4975(10)64995-8) [DOI] [PubMed] [Google Scholar]
- 20.Creech O, Ledbetter M, Reemtsma K. Congenital mitral insufficiency with cleft posterior leaflet. Circulation 1962. 25 390–394. ( 10.1161/01.CIR.25.2.390) [DOI] [PubMed] [Google Scholar]
- 21.Amin A, Davis M, Auseon A. Isolated cleft posterior mitral valve leaflet: an uncommon cause of mitral regurgitation. European Journal of Echocardiography 2009. 10 173–174. ( 10.1093/ejechocard/jen212) [DOI] [PubMed] [Google Scholar]
- 22.Zühlke L, Engel ME, Lemmer CE, Van De Wall M, Nkepu S, Meiring A, Bestawros M, Mayosi BM. The natural history of latent rheumatic heart disease in a 5 year follow-up study : a prospective observational study. BMC Cardiovascular Disorders 2016. 16 46 ( 10.1186/s12872-016-0225-3) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rémond M, Atkinson D, White A, Brown A, Carapetis J, Remenyi B, Roberts K, Maguire G. Are minor echocardiographic changes associated with an increased risk of acute rheumatic fever or progression to rheumatic heart disease? International Journal of Cardiology 2016. 198 117–122. ( 10.1016/j.ijcard.2015.07.005) [DOI] [PubMed] [Google Scholar]
- 24.Beaton A, Aliku T, Dewyer A, Jacobs M, Jiang J, Longenecker CT, Lubega S, McCarter R, Mirabel M, Mirembe G, et al Latent rheumatic heart disease: identifying the children at highest risk of unfavorable outcome. Circulation 2017. 136 2233–2244. ( 10.1161/CIRCULATIONAHA.117.029936) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Parasternal long axis view (PSLAX) demonstrating a normal mitral valve (normal anterior mitral valve leaflet (AMVL) thickness, no RHD-related restriction of either MV leaflets. View Video 1 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-1.
Download Video 1 (1.6MB, mov)
PSLAX view with color Doppler demonstrating MR that measures 2.2 cm in length. The jet met the additional requirements to deem it pathological (seen in 2 views, CW maximum velocity >3 m/s and a pansystolic jet). View Video 2 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-2.
Download Video 2 (2.2MB, mov)
Parasternal short axis (PSSAX) view of the mitral valve, demonstrating a PMVL inter-scallop separation in the P2 position. View Video 3 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-3.
Download Video 3 (2.3MB, mov)
PSSAX with color Doppler confirming a P2 inter-scallop separation as the underlying cause of the MR. View Video 4 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-4.
Download Video 4 (1.3MB, mov)
Parasternal long axis view (PSLAX) demonstrating a normal mitral valve (normal anterior mitral valve leaflet (AMVL) thickness, no RHD-related restriction of either MV leaflets. View Video 5 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-5.
Download Video 5 (913.4KB, mov)
PSLAX view with color Doppler demonstrating MR that measured 2.2 cm in length. The jet met the additional requirements to deem it pathological (seen in 2 views, CW maximum velocity >3 m/s and a pansystolic jet). View Video 6 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-6.
Download Video 6 (473.6KB, mov)
PSSAX view of the mitral valve, demonstrating a subtler case of an inter-scallop separation in the P2/P3 position. View Video 7 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-7.
Download Video 7 (972.1KB, mov)
PSSAX with color Doppler confirming a P2/P3 inter-scallop separation as the underlying cause of the MR. View Video 8 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-8.
Download Video 8 (359.1KB, mov)
A screened case from the EIA database with ‘pathological MR’ from an inter-scallop separation of the PMVL. This video from the PSLAX view with focused color Doppler over the MV demonstrates central MR with its origin below the coaptation point of the MV leaflets (i.e. body of the PMVL). View Video 9 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-9.
Download Video 9 (868KB, mov)
PSLAX view demonstrating a rheumatic mitral valve with suggestive RHD-related restriction of the AMVL and PMVL. The A2 segment of the AMVL is seen to ‘prolapse’ past the P2 segment of the PMVL. This mechanism is more correctly termed ‘pseudoprolapse’ as the AMVL is in its normal position at end systole. The impression of A2 prolapse is rather thought to be related to PMVL systolic restriction with resultant malcoaptation of the PMVL and AMVL during systole. This generates the characteristic posteriorly directed jet of rheumatic MR. View Video 10 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-10.
Download Video 10 (908.5KB, mov)
PSLAX view with focused color Doppler over the MV – this video demonstrates the characteristic posterior MR jet encountered in chronic rheumatic MR. View Video 11 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-11.
Download Video 11 (549.8KB, mov)
PSSAX view of a screened case from the EIA database with ‘pathological MR’. The screener should ensure that the leaflet tips are adequately sectioned to identify potential inter-scallop separation(s). This video demonstrates an inter-scallop separation in the P2/P3 position. View Video 12 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-12.
Download Video 12 (882.7KB, mov)
PSSAX of the same case presented in Video 12: focused color Doppler over the MV confirms a P2 inter-scallop separation as the underlying cause of the MR. View Video 13 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-18-0010/video-13.
Download Video 13 (1,019.9KB, mov)



 This work is licensed under a
This work is licensed under a